TO THE EDITOR:
The Affordable Care Act (ACA) expanded Medicaid coverage to adults with incomes up to 133% of the federal poverty level, but a subsequent Supreme Court ruling determined Congress could give states the option to expand. In September of 2013, the state of Michigan approved expansion. Beginning in April 2014, more than 400,000 adults will be newly eligible for Medicaid enrollment in the state.1
The impact of this influx of patients on surgical care and hospital costs in Michigan is unknown. Previous national studies of Medicaid patients undergoing surgery have shown worse outcomes2 and increased costs.3 Given the ACA also mandates a reduction in payments to disproportionate share hospitals (DSH),4 increased Medicaid enrollment could have substantial clinical and financial implications for hospitals facing expansion. To better understand this change, we examined the surgical outcomes and resource use of Medicaid patients in Michigan the year prior to implementation of the ACA using a statewide clinical registry.
METHODS
We studied all non-elderly adults undergoing inpatient general surgery within the 52-hospital Michigan Surgical Quality Collaborative (MSQC) in the year prior to approval of Medicaid expansion (July 2012 to June 2013). Medicare patients and those ≥65 years old were excluded. Details of prospective data collection, case sampling, and definitions of comorbidities and outcomes have been previously described.5 We calculated descriptive statistics and rates of unadjusted surgical outcomes for patients stratified by insurance status. Hospitals were ranked according to the proportion of Medicaid patients served, and divided into quintiles. For all statistical tests, p-values are two-tailed, and alpha is set at 0.05. Analyses were performed using STATA version 13.1 (StataCorp, College Station, TX). This study was ruled exempt by the Institutional Review Board.
RESULTS
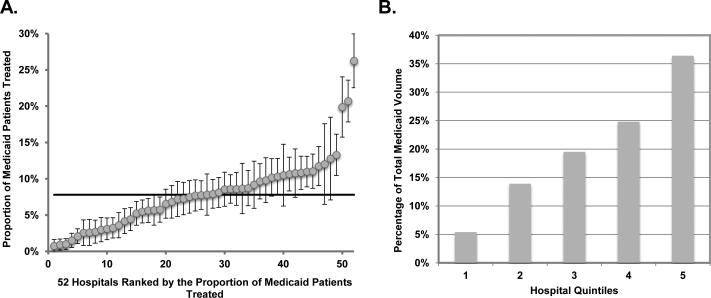
The final cohort included 13,887 patients undergoing general surgery during the study period. Patient demographics, surgical outcomes, and resource use of Medicaid patients, compared to private insurance patients, are shown in Table 1. Medicaid patients were younger and more likely to be female and non-white. Rates of smoking (49%), chronic obstructive pulmonary disease (10%), and peripheral vascular disease (7%) were twice those seen in the privately insured. Medicaid patients underwent 21% more emergent operations, experienced 67% more serious complications, and utilized 50% more resources. Examination of hospitals revealed wide variability in the proportion of Medicaid patients treated (Figure 1A). The highest two hospital quintiles accounted for 61.2% of all Medicaid patients treated (Figure 1B).
Table 1.
Patient demographics, procedure mix, postoperative outcomes, and resource use in private insurance and Medicaid patients undergoing surgery during the period July 2012 to June 2013 (IQR: interquartile range; BMI: body mass index).
| Private Insurance (n=11,763) | Medicaid (n=2,124) | p-value | |
|---|---|---|---|
| Descriptive Statistics | |||
| Age, median (IQR), years | 49 (28 - 70) | 41 (17 - 65) | <0.01 |
| Female sex | 7,205 (61) | 1,462 (68) | <0.01 |
| BMI, mean (SD), kg/m2 | 31 (18) | 31 (9) | 0.30 |
| Non-white race | 1,938 (16) | 715 (34) | <0.01 |
| Current smoker | 2,882 (25) | 1,052 (49) | <0.01 |
| Urgent/Emergent operation | 4,541 (39) | 989 (47) | <0.01 |
| Comorbidities | |||
| Hypertension | 3,816 (32) | 693 (33) | 0.87 |
| Diabetes mellitus | 1,167 (10) | 284 (13) | <0.01 |
| Chronic obstructive pulmonary disease | 457 (4) | 214 (10) | <0.01 |
| Coronary artery disease | 676 (6) | 170 (8) | <0.01 |
| Peripheral vascular disease | 347 (3) | 143 (7) | <0.01 |
| Dependent functional status | 151 (1) | 91 (4) | <0.01 |
| Common Operations | |||
| Laparoscopic cholecystectomy | 3,397 (29) | 617 (29) | 0.87 |
| Laparoscopic appendectomy | 1,877 (16) | 268 (13) | <0.01 |
| Ventral hernia repair | 587 (5) | 92 (4) | 0.19 |
| Postoperative Outcomes | |||
| Any complication | 912 (8) | 264 (12) | <0.01 |
| Major complications | 699 (6) | 204 (10) | <0.01 |
| Mortality | 46 (1) | 19 (1) | <0.01 |
| Resource Utilization | |||
| Length of stay, median (IQR), days | 2 (0 - 6) | 3 (0 - 8) | <0 01 |
| Readmission | 662 (6) | 193 (9) | <0.01 |
* All values are number (percentage) unless otherwise noted
** All outcomes are measured at 30 days or in-hospital (for durations longer than 30 days).
Figure 1.
A.) Proportion of Medicaid patients treated by each of Michigan's 52 hospitals, and B.) Percentage of total Medicaid volume treated within each hospital quintile, during the period July 2012 to June 2013.
COMMENT
Medicaid patients undergoing surgery in Michigan represent a significant challenge to the healthcare system. These patients have worse health status, experience more complications, and utilize more resources than privately insured patients. The proportion of Medicaid patients served varies substantially, and a small subset of hospitals cares for a large percentage of the state's Medicaid population. Given the findings above, the ACA mandated decrease in DSH payments could place this subset of hospitals at risk for financial insolvency.
This analysis is limited by small sample size. However this study represents the most current data available, and uses an internally-validated clinical registry. Though this data is limited to a single state, there is no reason to believe there are systematic differences between our cohort and the national Medicaid population.
To ensure high quality care, legislators and hospitals must adapt to meet the needs of this patient population. In Michigan, the legislation to expand Medicaid also funded an advisory committee to study the cost and quality of care delivered to these patients.1 Existing regional quality collaboratives, such as the MSQC, have the infrastructure necessary to address these issues, and have been shown to improve outcomes.6 State legislatures considering expansion should partner with these organizations to ensure increased access is met with high-value surgical care.
Acknowledgement
We would like to thank John Z. Ayanian, MD, MPP for his helpful comments.
Funding/Support: None.
Footnotes
Author Contributions: SAW and KHS had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Waits, Reames, Sheetz. Acquisition of data: Waits, Sheetz. Analysis and interpretation of data: All Authors. Drafting of the manuscript: Waits, Reames, Sheetz. Critical revision of the manuscript for important intellectual content: All Authors. Statistical analysis: Sheetz. Obtained funding: N/A. Administrative, technical, or material support: Campbell. Study supervision: Campbell.
Conflict of Interest Disclosures: The authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Dr. Campbell is Program Director of the Michigan Surgical Quality Collaborative. SAW, BNR, KHS, and MJE have no conflicts of interest to disclose.
References
- 1.Ayanian JZ. Michigan's Approach to Medicaid Expansion and Reform. New England Journal of Medicine. 2013;369(19):1773–1775. doi: 10.1056/NEJMp1310910. [DOI] [PubMed] [Google Scholar]
- 2.LaPar DJ, Bhamidipati CM, Mery CM, et al. Primary payer status affects mortality for major surgical operations. Ann Surg. 2010 Sep;252(3):544–550. doi: 10.1097/SLA.0b013e3181e8fd75. discussion 550-541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bradley CJ, Dahman B, Bear HD. Insurance and inpatient care: differences in length of stay and costs between surgically treated cancer patients. Cancer. 2012 Oct 15;118(20):5084–5091. doi: 10.1002/cncr.27508. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Medicare and Medicaid Services Medicaid program; state disproportionate share hospital allotment reductions. Final rule. Federal register. 2013 Sep 18;78(181):57293–57313. [PubMed] [Google Scholar]
- 5.Waits SA, Sheetz KH, Campbell DA, et al. Failure to rescue and mortality following repair of abdominal aortic aneurysm. Journal of vascular surgery. 2013 Dec 21; doi: 10.1016/j.jvs.2013.10.078. In Press. [DOI] [PubMed] [Google Scholar]
- 6.Share DA, Campbell DA, Birkmeyer N, et al. How a regional collaborative of hospitals and physicians in Michigan cut costs and improved the quality of care. Health affairs. 2011 Apr;30(4):636–645. doi: 10.1377/hlthaff.2010.0526. [DOI] [PubMed] [Google Scholar]