Highlights
-
•
Early pregnancy sonographic examination helps in early detection of uterine anomalies.
-
•
Close follow up of the pregnancy in a BU is essential to early recognize adverse outcomes.
-
•
Uterine rupture can occur in early pregnancy in patients with uterine anomaly.
Keywords: Bicornuate uterus, Pregnancy, Rupture
Abstract
Introduction
Bicornuate uterus (BU) is a rare uterine anomaly result from incomplete fusion of the two Müllerian ducts during embryogenesis. BU very rarely can lead to rupture of the uterus during the early pregnancy with high mortality and morbidity rates.
Presentation Of Case
A primigravida in the first trimester (9 weeks) presented complaining of epigastric pain and vomiting for one day. Ultrasound scan was performed at the 7th week of pregnancy and showed a BU with single intrauterine gestational sac in the right horn. On presentation, the patient was pale and irritable. Urgent ultrasound scan showed viable fetus in the right horn, free fluids in Morrison’s pouch. Laparotomy showed BU with pregnancy in the ruptured right horn. The defect in the uterus was repaired. Postoperatively, the patient was advised to use contraceptive pills for one year.
Discussion
Our patient has a sonographic diagnosis of BU at the 7th gestational week. At that stage, nothing was done except close follow up of the pregnancy. When she developed severe epigastric pain, initially, we thought of peptic ulcer disease complications. Even after deterioration of the patients’ condition, the diagnosis was not clear as the urgent ultrasound showed a viable fetus. Blood and fluid replacement therapy, and exploratory laparotomy were essential to save the patient’s life.
Conclusion
This case highlights the fact that uterine rupture can occur in early pregnancy when associated with uterine anomaly. Early sonographic diagnosis has a major contribution in evaluation and management.
1. Introduction
The female reproductive organs develop from the fusion of the bilateral paramesonephric (Müllerian) ducts to form the uterus, cervix, and upper two-thirds of the vagina. Bicornuate uterus (BU) is a rare uterine anomaly result from incomplete fusion of the two Müllerian ducts during embryogenesis. This leads to varying degrees of separation between two symmetrical uterine cavities ranging from partial separation to complete separation with no communication between the two cavities [1,2]. Kidney and other urinary tract abnormalities are often associated with Müllerian ducts anomalies [3]. Rupture of the gravid uterus is a rare obstetric catastrophe with high mortality and morbidity. It is more common in multigravida or in scarred uterus and usually occurs at labor [4]. BU is associated with adverse reproductive outcomes and very rarely can lead to rupture uterus during the pregnancy [4]. Herein, we report a case of primigravida with first trimester rupture of bicornuate uterus. BU was diagnosed before rupture by ultrasound scan at the 7th week of gestation.
2. Case report
A 24-year-old primigravida in the first trimester (9 weeks) presented to the Emergency Department complaining of severe epigastric pain and vomiting for one day. The patient had recurrent attacks of epigastric pain during the last 3 weeks and she was receiving medications for peptic ulcer disease. There was no history of bleeding per vagina. Ultrasound scan performed at the 7th week of pregnancy has shown a BU with single intrauterine gestational sac and viable fetal pole in the right horn (Fig. 1). No renal abnormality was detected by the ultrasound scan. On examination, the patient was pale and irritable. She was a febrile, her pulse rate was 94 bpm, blood pressure 100/65 mmHg, and respiratory rate was 20/min. Abdomen was soft with tenderness in the epigastric area. Blood investigation has shown hemoglobin of 109 g/L, total white blood cell count of 11.3 × 10/L and platelets of 223 × 10/L. An emergency abdominal ultrasound scan of the abdomen and pelvis was performed. It showed viable fetus with positive heart activity in the right horn of the BU with gestational age of 9 weeks, free fluids in Morrison’s pouch, and free fluids in the pelvis. In the next 3 h the pain increased and CT scan of the abdomen showed increased free fluid in the peritoneal cavity (Fig. 2). The patient became restless with pulse rate of 120 bpm, blood pressure 110/70 mmHg, and hemoglobin dropped to 6.8 g/l. Blood substitution and fluid resuscitation were started immediately and the patient underwent exploratory laparotomy. About 2.5 liters of hemorrhagic fluid was removed from the peritoneal cavity. The uterus was found to be bicornuate with a pregnancy in the right rudimentary horn. The uterus was ruptured through a 5 × 3 cm opening in the superior-lateral region (right cornu of the uterus) with continuous bleeding from the edges (Fig. 3). Placental tissues and a fetus with crown-rump length of about 2.5 cm were seen in the peritoneal cavity. Both the ovaries and the fallopian tubes were normal. The defect was repaired using 3/0 vicryl suture. Four units of packed red blood cells were transfused for the patient. The post-operative period was uneventful and the patient was discharged on the 4th postoperative day. She was advised to use contraceptive piles for at least one year.
Fig. 1.
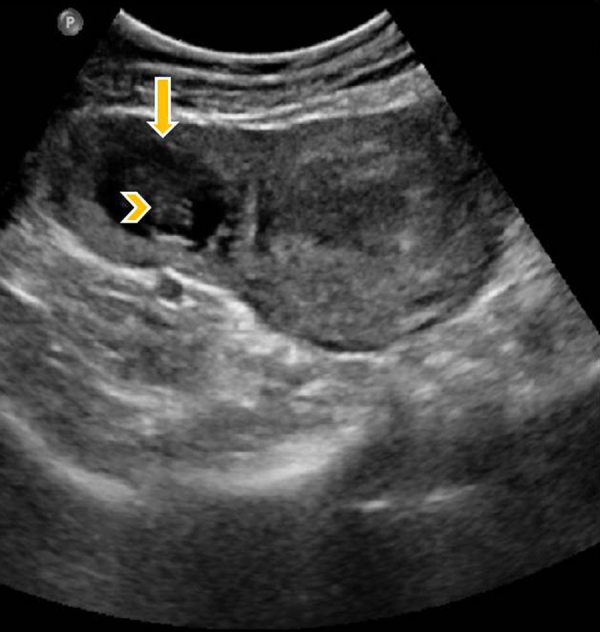
Ultrasound of the pelvis at the 7th week of pregnancy shows bicornuate uterus with a gestational sac in the smaller right horn (arrow). Fetal pole is seen within the sac (arrow head).
Fig. 2.

CT abdomen coronal section shows gravid uterus with gestational sac towards the right side (arrow). Moderate amount of free fluid in the abdomen especially around the liver (arrow head).
Fig. 3.
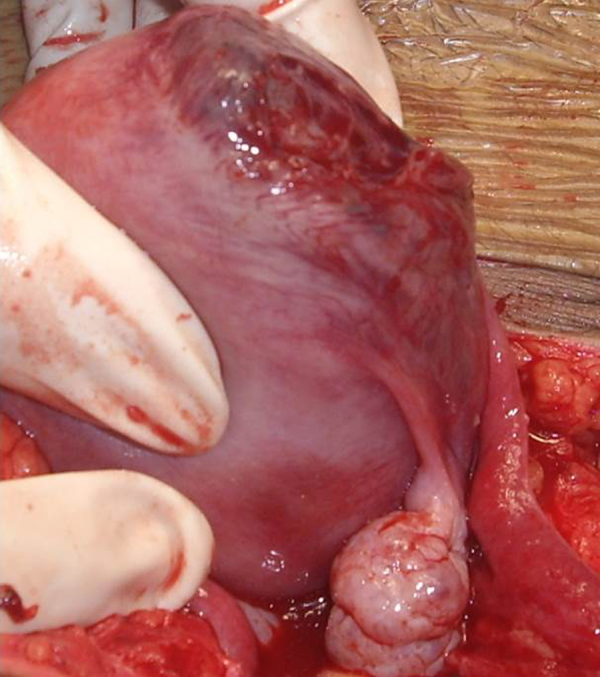
Laparotomy shows rupture of right cornual pregnancy of the uterus with intact right ovary and fallopian tube.
3. Discussion
Pregnancy in a BU has a poor reproductive potential and requires close monitoring [1]. In asymptomatic women, the presence of bicornuate uterus may not be detected until during pregnancy or delivery [4,5]. Our patient has a sonographic diagnosis of BU at the 7th gestational week of her first pregnancy with no history of infertility or previous abortions. At that stage nothing had been done except close follow up of the pregnancy. When she developed the severe epigastric pain, initially, we thought that it was a complication of her peptic ulcer disease. An urgent ultrasound examination had shown viable fetus before the actual rupture of the uterus and fetal death. Even after deterioration of the patients’ condition, dropping of her hemoglobin, and CT scan finding of increased free intraperitoneal fluid, the diagnosis was not clear. Immediate blood and fluid replacement therapy, and exploratory laparotomy were essential to save the patient’s’ life [6,7]. Obstetrical outcomes are generally reported to be better in cases of bicornuate uterus than in unicornuate uterus [2].
The cornual pregnancy has been used in the literature to indicate pregnancy in a horn of an anomalous uterus [8]. However, the terms interstitial and cornual pregnancies, have been used interchangeably, cornual implantation describes those in the upper lateral uterine cavity (as we think the case in this report), whereas, interstitial denotes those implanted within the proximal intramural portion of the tube [8]. The thin muscular wall of the pregnant horn increases the risk of the horn ruptures [9].
Diagnosis of early first trimester prerupture is rare and remains challenging. Ultrasound in early pregnancy has a major rule in the early diagnosis. MRI can be a useful noninvasive diagnostic tool [9]. Due to the scar following the uterine rupture, pregnancy is suggested to be avoided at least for one year [4]. The subsequent pregnancy should be carefully monitored [10].
4. Conclusion
This case highlights the fact that uterine rupture can occur in early pregnancy when associated with uterine anomaly. The clinician should be aware of this potentially life-threatening condition. Early sonographic diagnosis has a major contribution in evaluation and management.
Conflicts of interest
Authors have no conflict of interest.
Sources of funding
Nothing to declare.
Ethical approval
Not required ethical approval.
Consent of patient
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contributions
Ashraf F. Hefny: study concept data collection, interpretation, writing the first draft and editing the paper.
Fathima T. Kunhivalappil: study concept, interpretation, editing the paper.
Ritu Nambiar: study concept, interpretation, editing the paper.
Masoud O. Bashir: study concept, interpretation, editing the paper.
Guarantor
All the authors are responsible for the article.
References
- 1.Chan Y.Y., Jayaprakasan K., Tan A., Thornton J.G., Coomarasamy A., Raine-Fenning N.J. Reproductive outcomes in women with congenital uterine anomalies: a systematic review. Ultrasound Obstet. Gynecol. 2011;38:371–382. doi: 10.1002/uog.10056. [DOI] [PubMed] [Google Scholar]
- 2.Reichman D.E., Laufer M.R. Congenital uterine anomalies affecting reproduction. Best Pract. Res. Clin. Obstet. Gynaecol. 2010;24:193–208. doi: 10.1016/j.bpobgyn.2009.09.006. [DOI] [PubMed] [Google Scholar]
- 3.Elyan A., Saeed M. Mullerian duct anomalies: clinical concepts. Ain Shams J. Obstetr. Gynecol. 2004;1:11–20. [Google Scholar]
- 4.Singh N., Singh U., Verma M.L. Ruptured bicornuate uterus mimicking ectopic pregnancy: a case report. J. Obstet. Gynaecol. Res. 2013;39:364–366. doi: 10.1111/j.1447-0756.2012.01914.x. [DOI] [PubMed] [Google Scholar]
- 5.Jayaprakash S., Muralidhar L., Sampathkumar G., Sexsena R. Rupture of bicornuate uterus. BMJ Case Rep. 2011;28(October) doi: 10.1136/bcr.08.2011.4633. pii:0820114633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hassan C.H., Karim A.K., Ismail N.A., Omar M.H. Case report of ruptured non-communicating right rudimentary horn pregnancy: an acute emergency. Acta Medica (Hradec Kralove) 2011;54:125–126. doi: 10.14712/18059694.2016.34. [DOI] [PubMed] [Google Scholar]
- 7.Elsayegh A., Nwosu E.C. Rupture of pregnancy in the communicating rudimentary uterine horn at 34 weeks. Hum. Reprod. 1998;13:3566–3568. doi: 10.1093/humrep/13.12.3566. [DOI] [PubMed] [Google Scholar]
- 8.Arleo E.K., DeFilippis E.M. Cornual, interstitial, and angular pregnancies: clarifying the terms and a review of the literature. Clin. Imaging. 2014;38:763–770. doi: 10.1016/j.clinimag.2014.04.002. [DOI] [PubMed] [Google Scholar]
- 9.Tsafrir A., Rojansky N., Sela H.Y., Gomori J.M., Nadjari M. Rudimentary horn pregnancy: first-trimester prerupture sonographic diagnosis and confirmation by magnetic resonance imaging. J. Ultrasound Med. 2005;24:219–223. doi: 10.7863/jum.2005.24.2.219. [DOI] [PubMed] [Google Scholar]
- 10.Kochar S., Prakash P. An unusual case of rupture of right horn of bicornuate uterus at eighteen weeks of gestation. J. Obstet. Gynaecol. India. 2012;62:694–695. doi: 10.1007/s13224-012-0160-x. [DOI] [PMC free article] [PubMed] [Google Scholar]


