Highlights
-
•
Stump appendicitis is a rare presentation and therefore presents as a diagnostic dilemma.
-
•
A PubMed search was conducted to identify cases of stump appendicitis following appendectomy.
-
•
We report a case of a 72 year old female who presents 7 years post appendectomy with stump appendicitis.
-
•
Systematic review of 61 cases were analyzed and outcomes highlighted.
Keywords: Completion appendectomy, Appendectomy, Appendicectomy, Stump appendicitis
Abstract
Introduction
Stump appendicitis is one of the rare delayed complications post appendectomy with a reported incidence of 1 in 50,000 cases. Stump appendicitis can present as a diagnostic dilemma if the treating clinician is unfamiliar with this rare clinical entity. A PubMed search was conducted to identify cases of stump appendicitis following appendectomy. Sixty one cases of SA that were reported in English medical literature were analyzed.
Presentation of case
We report a case of stump appendicitis (SA) with a systematic review and challenges encountered during the management.
Discussion
The interval from original appendectomy to stump appendicitis ranged from 4 days to 50 years. SA followed appendectomy in 58% of open and 31.6% of laparoscopic procedures. SA was frequently misdiagnosed as constipation, gastroenteritis or right sided diverticulitis, therefore leading to a significant delay to surgery. Computerized Tomography diagnosed SA in 56.3% of cases. Perforation with gangrene of the stump occurred in 60%.
Conclusion
Stump appendicitis can represent a diagnostic dilemma if the treating physician is unfamiliar with this uncommon clinical entity. Radiological imaging is required to aid diagnosis and a completion appendectomy is the modality of treatment.
1. Introduction
Stump appendicitis is one of the rare delayed complications post appendectomy with a reported incidence of 1 in 50,000 cases. Stump appendicitis can present as a diagnostic dilemma if the treating clinician is unfamiliar with this rare clinical entity. A PubMed search was conducted to identify cases of stump appendicitis following appendectomy. Sixty one cases of SA that were reported in English medical literature were analyzed. We report a case of stump appendicitis with a systematic review and challenges encountered during the management.
2. Case presentation
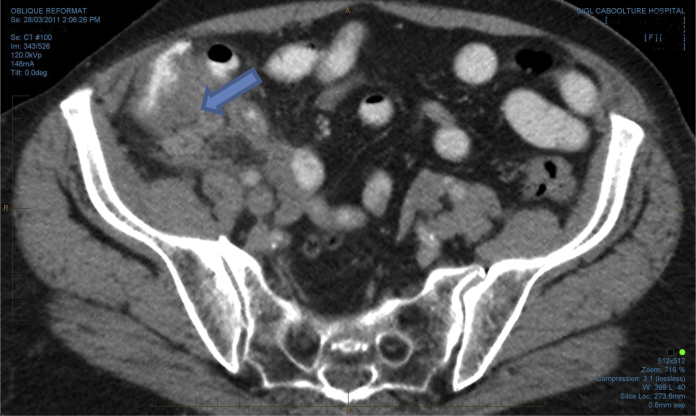
A 72 year old female with a history of laparoscopic appendectomy 7 years ago (2007) was admitted to the emergency department (2011), with ongoing right iliac fossa (RIF) pain. On admission, clinical examination revealed signs of localized tenderness in RIF. The inflammatory markers were normal. She had a White Cell Count of 9.4 × 109/L. Her CT abdomen revealed evidence of stump appendicitis without free gas (Figs. 1 and 2). The patient was on warfarin for atrial fibrillation with an International Normalized Ratio (INR) of 3.2. A clinical decision was made to manage her conservatively with IV antibiotics due to a high INR and having a stable hemodynamic status. The patient had an uneventful recovery and was discharged after 4 days.
Fig. 1.
Arrow indicating appendiceal stump with inflammatory changes.
Fig. 2.

Coronal view with arrow indicating features of stump appendicitis.
She was readmitted again in 2014 with severe RIF pain and fever. Clinical examination showed localized peritonism and biochemistry revealed evidence of an inflammatory response. She had a White Cell Count of 18 × 109/L.
CT abdomen showed gas locules (Fig. 3) around the caecal pole with a mild amount of free fluids and fat stranding suspicious of a perforated caecal diverticulum. The patient underwent a laparotomy and the finding were a perforated appendicular base with an appendicular stump of 2.5 cm, which was confirmed histologically.
Fig. 3.

Gas locules along the caecal pole.
3. Discussion
Appendectomy remains one of the most commonly performed procedures by the general surgeon. More than 250,000 appendectomies are performed each year in America for acute appendicitis, and the lifetime risk of developing appendicitis is 8.6% for men and 6.7% for women [1]. Short-term complications associated with surgery for acute appendicitis include wound infection, deep infection including intraabdominal collections and bleeding. The long term complications are often vague and poorly defined but include hernias, small bowel obstructions and stump appendicitis.
The appendix arises from the posteromedial wall of the cecum about 3 cm below the ileocecal valve. Its variable position and subserous length, combined with acute inflammation, may result in misidentification of the appendicecal junction. Dissecting the recurrent branch of the appendicecal artery and following the tenia coli on the cecum helps in identifying the true appendicular base. Generally, an appendix stump shorter than 5 mm reduces the risk of stump appendicitis [1,2].
The first two documented cases of stump appendicitis were in 1945 by Rose, and since then there have been sixty one cases reported. This number is on the rise likely due to the easy availability and lower threshold to investigate with a CT scan [3]. Stump appendicitis is an under reported and poorly defined condition which could raise significant diagnostic challenges.
Stump appendicitis is one of the rare delayed complications after an appendectomy with a reported incidence of 1 in 50,000 cases [4]. Prompt recognition is important in order to lead to early treatment, thus avoiding serious complications like wound infection, intraabdominal abscess formation, intestinal perforation with peritonitis, bleeding and adhesions with subacute intestinal obstructions.
Stump appendicitis can represent a diagnostic dilemma if the treating physician is unfamiliar with this uncommon clinical entity. Clinically, patients present with signs and symptoms mimicking appendicitis or the acute abdomen along with a previous history of appendectomy as seen in our case. The presence of an appendectomy scar does not rule out the possibility of stump appendicitis [5]. The interval time for onset of symptoms could range anywhere from two weeks to years after an appendectomy.
The incidence and prevalence of stump appendicitis has been increasing in the recent years. It has been reported following both open and laparoscopic appendectomy [6,7]. Whether the laparoscopic technique plays any role in the increased incidence of stump appendicitis is yet to be ascertained. The potential limitation of laparoscopy such as lack of three dimensional vision and absence of tactile feedback has been suggested by some authors to increase the chance of leaving behind a longer stump [8]. However, stump appendicitis has been reported more following open appendectomy. Further advancement in the techniques of laparoscopy, especially the use of angled scopes and high definition cameras, provide good visualization of the surgical field. Accurate visualization of the base of the appendix either in open or laparoscopic appendectomy is a must to minimize the incidence of stump appendicitis. Leaving a longer stump may result in chronic inflammation or serve as a reservoir for faecolith, thus more prone to becoming ischemic and eventually perforate or suppurate. It has been suggested that no appendicular stump longer than 3 mm should be left behind [9].
The common conditions leading to stump appendicitis have been broadly classified as anatomical or surgically related factors. One common denominator is the inappropriate identification of the appendicular base, which is the appendicecal junction.
The anatomical related factors may be positional by means of a retrocecal appendix or subserosal appendix, a duplicated appendix, which is a rare developmental abnormality seen in about 0.004% of appendectomy patients or a diverticulum at the appendicular base [10].
The surgical factors predisposing for stump appendicitis may be inadequate identification of the appendicular base because of severe local inflammation, leaving a long stump due to fear of caecal injury or difficult dissection and local ulcerations due to presence of a faecolith [3,11]. Stump appendicitis has been reported following open appendectomy with stump ligation, open appendectomy with stump inversion and laparoscopic appendectomy where appendicecal stump is either closed with an endoloop or by stapling. Both the surgical techniques i.e., inversion of stump or simple ligation of stump cannot prevent the possibility of stump appendicitis. Radiological evaluation by ultrasound and computed tomography (CT) scan aids in the preoperative diagnosis of stump appendicitis [12,13]. The High incidence of stump appendicitis compared to laparoscopic surgery supports the above practical difficulties faced with the limited access during open surgery.
CT scan of the abdomen is more specific than ultrasound for the accurate diagnosis of stump appendicitis because it excludes other etiologies of the acute abdomen. CT findings may be similar to those seen in acute appendicitis. These include pericecal inflammatory changes, abscess formation, fluid in the right paracolic gutter, caecal wall thickening and an ileocecal mass. In the era of laparoscopy a diagnostic laparoscopy may prove to be the next diagnostic and therapeutic option in the case of ambiguity.
Completion appendectomy either by open or by laparoscopic intervention is the treatment of choice for stump appendicitis [14]. Very rarely, extensive surgery such as ileocolic resection may be necessary if there is significant inflammation around the ileocecal region. It is imperative to adequately visualize the appendicular base and the ileocecal region to ensure that a stump not more than 5 mm remains after appendix removed.
Conflict of interest
There was no financial or personal relationships which could influence bias in this case report and literature review.
Sources of funding
There was no funding requirement for this case report, bar the amount required if the case report is published.
Ethical approval
No ethical approval was required or requested for this case report.
Consent
Verbal consent was obtained from patient. All details of the patient in the images attached with the case report has been deleted and patient remains anonymous.
Author contributions
Rasika Hendahewa — primary author of the case report, literature review, analysis and interpretation of data.
Sujith Ratnayake — Literature review, analysis and interpretation of data.
Ashvini Shekhar — secondary author, editor and correspondence author for case report.
Guarantor
Rasika Hendahewa — General Surgeon, Caboolture Hospital, McKean Street, Caboolture, 4510 Queensland, Australia.
References
- 1.Humes D.J., Simpson J. Acute appendicitis. BMJ. 2006;333(7567):530–534. doi: 10.1136/bmj.38940.664363.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bickell N.A., Aufses A.H., Jr., Rojas M., Bodian C. How time affects the risk of rupture in appendicitis. J. Am. Coll. Surg. 2006;202(3):401–406. doi: 10.1016/j.jamcollsurg.2005.11.016. [DOI] [PubMed] [Google Scholar]
- 3.Rose T. Recurrent appendiceal abscess. Med. J. Aust. 1945;32:659–662. [Google Scholar]
- 4.Harris C.R. Appendiceal stump abscess ten years after appendectomy. Am. J. Emerg. Med. 1989;7(4):411–412. doi: 10.1016/0735-6757(89)90050-8. [DOI] [PubMed] [Google Scholar]
- 5.Devereaux D.A., McDermott J.P., Caushaj P.F. Recurrent appendicitis following laparoscopic appendectomy Report of a case. Dis. Colon. Rectum. 1994;37(7):719–720. doi: 10.1007/BF02054417. [DOI] [PubMed] [Google Scholar]
- 6.Walsh D.C., Roediger W.E. Stump appendicitis–a potential problem after laparoscopic appendicectomy. Surg. Laparosc. En- dosc. 1997;7(4):357–358. [PubMed] [Google Scholar]
- 7.Liang M.K., Lo H.G., Marks J.L. Stump appendicitis: a comprehensive review of literature. Am Surg. 2006;72(2):162–166. [PubMed] [Google Scholar]
- 8.Bickell N.A., Aufses A.H., Jr., Rojas M., Bodian C. How time affects the risk of rupture in appendicitis. J. Am. Coll. Surg. 2006;202(3):401–406. doi: 10.1016/j.jamcollsurg.2005.11.016. [DOI] [PubMed] [Google Scholar]
- 9.Attwood S.E., Hill A.D., Murphy P.G., Thornton J., Stephens R.B. A prospective randomized trial of laparoscopic versus open appendectomy. Surgery. 1992;112(3):497–501. [PubMed] [Google Scholar]
- 10.Wei B., Qi C.L., Chen T.F. Laparoscopic versus open appendectomy for acute appendicitis: a metaanalysis. Surg En- dosc. 2011;25(April (4)):1199–1208. doi: 10.1007/s00464-010-1344-z. Epub 2010 Sep 17. [DOI] [PubMed] [Google Scholar]
- 11.Greenberg J.J., Esposito T.J. Appendicitis after laparoscopic appendectomy: a warning. J. Laparoendosc. Surg. 1996;6(3):185–187. doi: 10.1089/lps.1996.6.185. [DOI] [PubMed] [Google Scholar]
- 12.Somerville P.G., Lavelle M.A. Residual appendicitis following incomplete laparoscopic appendectomy. Br. J. Surg. 1996;83(6):869. doi: 10.1002/bjs.1800830646. [DOI] [PubMed] [Google Scholar]
- 13.Cave A.J. Appendix vermiformis duplex. J. Anat. 1936;70:283–292. (Pt. 2) [PMC free article] [PubMed] [Google Scholar]
- 14.Wallbridge P.H. Double appendix. Br. J. Surg. 1962;50:346–347. doi: 10.1002/bjs.18005022124. [DOI] [PubMed] [Google Scholar]