Highlights
-
•
Few reports deal with shunt-related complications during carotid endarterectomy.
-
•
We present a complication of shunting, consisting of internal carotid artery rupture at the distal tip of the shunt.
-
•
The management consisted of successful arterial repair via a saphenous vein patch.
Keywords: Carotid endarterectomy, Carotid shunt, Shunt-related complications
Abstract
Introduction
Shunting is a well-accepted method of maintaining cerebral perfusion during carotid endarterectomy (CEA). Nonetheless, shunt insertion may lead to complications including arterial dissection, embolization, and thrombosis. We present a complication of shunt insertion consisting of arterial wall rupture, not reported previously.
Presentation of case
A 78-year-old woman underwent CEA combined with coronary artery bypass grafting (CABG). At the time of shunt insertion an arterial rupture at the distal tip of the shunt was detected and was repaired via a small saphenous vein patch. Eversion CEA and subsequent CABG completed the procedure whose postoperative course was uneventful.
Discussion
Shunting during combined CEA-CABG may be advisable to assure cerebral protection from possible hypoperfusion due to potential hemodynamic instability of patients with severe coronary artery disease. Awareness and prompt management of possible shunt-related complications, including the newly reported one, may contribute to limiting their harmful effect.
Conclusion
Arterial wall rupture is a possible, previously not reported, shunt-related complication to be aware of when performing CEA.
1. Introduction
The benefit of carotid artery revscularization to prevent stroke has been recognized for both symptomatic and asymptomatic, hemodynamically significant carotid artery stenoses [1–4]. The insertion of an indwelling shunt is a widely accepted method to prevent cerebral hypoperfusion during carotid artery revascularization [5,6]. Indications for shunting vary among surgeons, with proponents of routine shunting [7] and proponents of selective shunting [8,9]. The major issue supporting selective shunting is the observation that the vast majority of intraoperative neurologic complications are due to thrombo–embolic episodes or technical errors, rather than to cerebral hypoperfusion related to carotid clamping [10], and the absence of significant differences between routine and selective shunting in terms of perioperative neurologic mortality and morbidity [11,12]. A further element favoring selective over routine shunting is the possible occurrence of shunt-related complications, which include intimal injury followed by dissection with thrombosis and embolization, pseudoaneurysm, distal embolization during shunt insertion, shunt malfunction with inadequate cerebral perfusion, and visual exposure limitation [5,13–15]. The present report deals with a complication of carotid shunt insertion, to our knowledge not previously reported, consisting of a focal rupture of the internal carotid artery (ICA).
2. Presentation of case
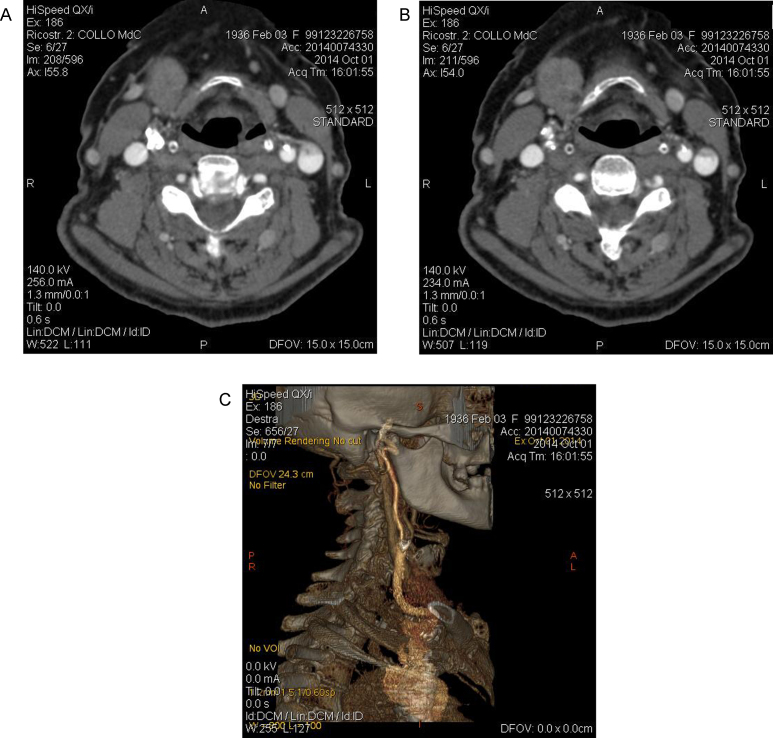
A 78-year-old woman was admitted to undergo coronary artery bypass grafting (CABG) for the elective treatment of triple vessel coronary artery disease (CAD). At preoperative duplex ultrasound scanning of the supraortic trunks (SAT), an asymptomatic, 80% stenosis of the right internal carotid artery (ICA) was detected. The stenosis was confirmed at a spiral CT scan of the SAT (Fig. 1A–C). The contralateral carotid artery presented a hemodynamically non-significant, calcified plaque. The vertebral arteries were equivalent, both injected the basilar artery and did not present hemodynamically significant lesions. The patient was scheduled for combined eversion carotid endarterectomy (CEA) and CABG. The combined carotid and coronary artery revascularization was considered an indication for systematic shunting during CEA [16]. At operation, after exposing the right carotid bifurcation and gently mobilizing the distal ICA, the ICA itself was sectioned at its origin and a Pruitt-Inahara shunt (Le Maitre Vascular Inc., Burlington, MA) was inserted. Immediately after shunt insertion, an intense bleeding was observed from beneath the digastric muscle, due to a 2-mm diameter rutpture of the ICA at the tip of the shunt. The ICA was controlled more distally and the shunt was gently repositioned beyond the lesion. A segment of greater saphenous vein, already harvested for CABG, was tailored to perform a small patch repair of the arterial lesion with the shunt in place (Fig. 2). Eversion endarterectomy completed the procedure, which was followed by CABG. The patient made an uneventful recovery and returned home on postoperative day 12, with a regularly patent ICA revascularization at control duplex ultrasound, performed before discharge from the hospital.
Fig. 1.
Preoperative CT scanning of the supraaortic trunks (SAT) showing an 80% stenosis of the right internal carotid artery at horizontal sections (A,B) and 3-D reconstruction (C).
Fig. 2.

Intraoperative picture showing repair of the internal carotid artery (ICA) with a small saphenous vein patch (arrow).
3. Discussion
Shunt-related complications during CEA may occur essentially through two different mechanisms: inadequate perfusion despite shunt patency due to distal thrombosis or embolization, and mechanical injury to the arterial wall, during shunt insertion or retrieval [5]. To our knowledge, this is the first case of ICA rupture due to shunt insertion. Adventitial injury occurring during freeing of the distal ICA and thinning of the arterial wall may have contributed to enhance the traumatic action of the shunt. In the patient object of the present report, the severe ICA stenosis was asymptomatic and detected at systematic duplex ultrasound of SAT, performed as part of preoperative workup of patients candidates for elective CABG. Combined carotid and myocardial revascularization was decided based on the evidence of significantly better neurologic results of CABG in patients with associated, severe carotid stenosis undergoing prior or combined CEA, compared to those undergoing ICA revascularization after CABG [16]. Although not mandatory, shunting during combined CEA–CABG may be advisable, in selected cases, by the need to ensure cerebral protection from possible hypoperfusion, due to the potential intraoperative hemodynamic instability of patiens with severe CAD. Therefore, based on this assumption and our experience, combined carotid and coronary artery revascularization is for us an indication for systematic shunting during CEA [16]. Other indications for systematic shunting, in our practice, are occlusion of the contralateral ICA or previous ipsilateral stroke. Beside these special settings, we usually perform selective shunting, relying on transcutaneous cerebral oximetry measurement (INVOS, Medtronic, Minneapolis, MN) combined with visual appreciation of distal ICA backbleeding. Based on our previous experience and results, carotid shunting is overall a safe procedure. Nonetheless, as shown in the reported case, the insertion of a shunt is not free from risks [5,13–15]. Awareness of its potential complications followed by prompt recognition and management, may contribute to limit their harmful effect.
4. Conclusion
Disruption of the arterial wall at the time of carotid shunt insertion is a previously not reported complication of shunting itself. The knowledge of its possible occurrence is a further requirement for an always careful insertion of the shunt and the capability to manage the related complications.
Conflicts of interest
No conflicts of interest to be disclosed.
Funding
No sources of funding.
Ethical Approval
Ethical approval was given by the Institutional Ethics Committee.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Study concept and design: G.I., F.C., F.V.
Data collection: F.C., G.P.
Analysis and interpretation: G.I., F.C., G.P., F.V.
Writing the paper: G.I.
Critical revision of the article: G.I., F.C., G.P., F.V.
Final approval of the article: G.I., F.C., G.P., F.V.
Guarantor
Giulio Illuminati, first and corresponding author, takes full responsibility for the work, the conduct of the study, had access to data and controlled the decision to publish.
References
- 1.North American Symptomatic Carotid Endarterectomy Trial Collaborators Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N. Eng. J. Med. 1991;325:445–453. doi: 10.1056/NEJM199108153250701. [DOI] [PubMed] [Google Scholar]
- 2.European Carotid Surgery Trialists Collaborative Group MRC European Carotid Surgery Trial: interim results for symptomatic patients with severe (70–99%) or mild (0–29%) carotid stenosis. Lancet. 1991;337:1235–1243. [PubMed] [Google Scholar]
- 3.European Carotid Surgery Trialists Collaborative Group Randomised trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European Carotid Surgery Trial (ECST) Lancet. 1998;351:1379–1387. [PubMed] [Google Scholar]
- 4.Executive Committee for the Asymptomatic Carotid Atherosclerosis Study Endarterectomy for asymptomatic carotid artery stenosis. JAMA. 1995;273:1421–1428. [PubMed] [Google Scholar]
- 5.Troisi N., Dorigo W., Pulli R., Pratesi C. A cause of traumatic internal carotid artery aneurysm secondary to carotid shunting. J. Vasc. Surg. 2010;51:225–227. doi: 10.1016/j.jvs.2009.08.057. [DOI] [PubMed] [Google Scholar]
- 6.Sundt T.M.J., r E., bersold M.J., Sharbrough F.W., Piepgras D.G., Marsh W.R., Messick J.M. The risk-benefit ratio of intraoperative shunting during carotid endarterectomy. Ann. Surg. 1986;203:196–204. doi: 10.1097/00000658-198602000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Javid H., Julian O.C., Dye W.S., Hunter J.A., Najafi H., Goldin M.D., Serry C., DeLaria G.A. Seventeen-year experience with routine shunting in carotid artery surgery. World J. Surg. 1979;3:167–177. doi: 10.1007/BF01561267. [DOI] [PubMed] [Google Scholar]
- 8.Luzzani L., Bellosta R., Carugati C., Talarico M., Sarcina A. Routine shunting is a safe and reliable method of cerebral protection during carotid endarterectomy. Ann. Vasc. Surg. 2006;20:482–487. doi: 10.1007/s10016-006-9037-8. [DOI] [PubMed] [Google Scholar]
- 9.Woodworth G.F., McGirt M.J., Than K.D., Huang J., Perler B.A., Tamargo R.J. Selective versus routine intraoperative shunting during carotid endarterectomy: a multivariate outcome analysis. Neurosurgery. 2007;61:1170–1177. doi: 10.1227/01.neu.0000306094.15270.40. [DOI] [PubMed] [Google Scholar]
- 10.Riles T.S., Imparato A.M., Jacobowitz G.R., Lamparello P.J., Giangola G., Adelman M.A., Landis R. The cause of perioperative stroke after carotid endarterectomy. J. Vasc. Surg. 1994;19:206–216. doi: 10.1016/s0741-5214(94)70096-6. [DOI] [PubMed] [Google Scholar]
- 11.Chessman R., Patil S., Hassouna A., Kirk J. Shunt use in carotid endarterectomy: a devastating complication. Rev. Vasc. Med. 2014;2:103–105. [Google Scholar]
- 12.Rerkasem K., Rothwell P.M. Routine or selective carotid artery shunting for carotid endarterectomy (and different methods of monitoring in selective shunting) Cochrane Database Syst. Rev. 2009;7(October (4)) doi: 10.1002/14651858.CD000190.pub2. CD000160. [DOI] [PubMed] [Google Scholar]
- 13.Bandyk D.F., Thiele B.L. Safe intraluminal shunting during carotid endarterectomy. Surgery. 1983;93:260–263. [PubMed] [Google Scholar]
- 14.Loftus C.M., Dyste G.N., Reinarz S.J., Hingtgen W.L. Distal cervical carotid dissection after carotid endarterectomy: a complication of indwelling shunt? Neurosurgery. 1986;19:441–445. doi: 10.1227/00006123-198609000-00018. [DOI] [PubMed] [Google Scholar]
- 15.Calhoun T.R., Kitten C.M. Proximal shunt dissection: a potential problem in carotid endarterectomy. Tex Heart Inst. J. 1985;12:359–361. [PMC free article] [PubMed] [Google Scholar]
- 16.Illuminati G., Ricco J.B., Caliò F., Pacilè M.A., Miraldi F., Frati G., Macrina F., Toscano M. Short-term results of a randomized trial examining timing of carotid endarterectomy in patients with severe asymptomatic unilateral carotid stenosis undergoing coronary artery bypass grafting. J. Vasc. Surg. 2011;54:993–999. doi: 10.1016/j.jvs.2011.03.284. [DOI] [PubMed] [Google Scholar]