Abstract
Objectives
Although an association between psychosocial distress (depression, anxiety, somatization, and perceived stress) and voice disorders has been observed, little is known about the relationship between distress and patient-reported voice handicap. Further, the psychological mechanisms underlying this relationship are poorly understood. Perceived control plays an important role in distress associated with other medical disorders. The objectives of this study were to 1) characterize the relationship between distress and patient-reported voice handicap and 2) examine the role of perceived control in this relationship.
Study Design
Cross-sectional study in tertiary care academic voice clinic.
Methods
Distress, perceived stress, voice handicap, and perceived control were measured using established assessment scales. Association was measured with Pearson’s correlation coefficient; moderation was assessed using multiple hierarchical regression.
Results
533 patients enrolled. 34% met criteria for clinically significant distress (i.e., depression, anxiety, and/or somatization). A weak association (r=0.13, p=0.003) was observed between severity of psychosocial distress and vocal handicap. Present perceived control was inversely associated with distress (r=−0.41, p<0.0001), stress (r=−0.30, p<0.0001), and voice handicap (r=−0.30, p<0.0001). The relationship between voice handicap and psychosocial distress was moderated by perceived control (b for interaction term −0.15, p<0.001); greater vocal handicap was associated with greater distress in patients with low perceived control.
Conclusions
Severity of distress and vocal handicap were positively related, and the relation between them was moderated by perceived control. Vocal handicap was more related to distress among those with low perceived control; targeting this potential mechanism may facilitate new approaches for improved care.
INTRODUCTION
A number of studies have drawn attention to psychosocial distress in patients with dysphonia1–3, although subject samples from these investigations have mostly been small and limited to specific laryngeal diagnoses. More recent studies involving larger numbers of patients with broader voice-related diagnoses have observed a startlingly high prevalence of clinically significant distress in patients presenting for voice care.1, 4, 5 Although this association has been consistently observed, limited data are available on the relationship between distress and degree of voice-related handicap. Presumably, greater distress and voice-related handicap would be correlated. However, in the study by Siupsinskiene et al.4, which is to our knowledge the only publication examining this issue, a weak relationship was observed between patient scores on the Hospital Anxiety and Depression Scale (HADS) and the Voice Handicap Index (r=0.17 for depression, 0.23 for anxiety). The relatively weak strength of this association was initially puzzling. One potential explanation was that the HADS does not assess somatic concerns; given our prior observation of a significant somatic component to distress among voice patients,5 we speculated that including an assessment of somatization in addition to anxiety and depression could allow better detection of an association between severity of distress and vocal handicap.
When the correlation between two variables is unexpectedly low it is also useful to look for variables that may be moderating the relationship. A moderator effect is an interaction “whereby the effect of one variable depends on the level of another.”6 This is distinct from a mediator, which explains the relationship between one variable and another rather than identifying when or for whom the relationship is meaningful. In the case of psychosocial distress and voice-related handicap, we speculated that a moderator might allow us to identify patients for whom there was a meaningful relationship between distress and voice-related handicap.
We thus turned our attention to one potential moderator, a psychological construct described in a temporal model of perceived control. Perceived control, an important psychological concept, is defined as “people’s beliefs in their capability to exercise some measure of control over their own functioning and over environmental events.”7 In this context, it would describe the degree to which patients believed that they had control over the voice-related events that occurred in their lives and how they responded or adjusted to them. We were particularly interested in present (as opposed to past or future) perceived control, which is “control [over] some current aspect of the event,”8 and has been shown to be more predictive of decreased distress than past or future perceived control. Present perceived control is linked with better life outcomes and reported physical health in undergraduates with a history of distressing life events.9 Present perceived control was associated with less distress in patients with medical conditions such as tinnitus,10 cardiac problems,11 and breast cancer,12, 13 indicating that although the situation itself may or may not be controllable, the patient’s response to the situation plays an important role in outcomes.
We examined these factors by concurrently assessing distress (including depression, anxiety, somatization, and stress), voice handicap, and degree of present perceived control in patients who presented with voice problems.
The objectives of this study were to assess the strength of association between voice handicap and distress in a sample of heterogeneous voice clinic patients, determine whether present perceived control (PPC) was associated with distress and voice handicap, and determine whether present control moderated the relationship between psychosocial distress and voice handicap.
We hypothesized that
Voice handicap and distress would have a small to moderate correlation4, and
Present perceived control would be negatively associated with distress 10–13 as well as voice handicap.
On an exploratory basis, we also hypothesized that present perceived control would moderate the relationship between distress and voice handicap such that vocal handicap would be more strongly related to distress for those with lower perceived control. This hypothesis, in contrast to those presented above, was based on clinical impressions rather than on existing literature, as there is no prior literature describing the role of perceived control in this context.
MATERIALS AND METHODS
Participants
Consecutive patients presenting to the Voice Clinic at an academic otolaryngology clinic were invited to participate by research staff and were prospectively enrolled for this study. Inclusion criteria included patient report of voice concern(s), age of at least 18, and ability to complete questionnaires independently. Patients completed the instruments before being seen by a provider. Participants were included in the sample regardless of specific voice-related diagnosis to increase sample heterogeneity and the generalizability of the findings. The first 192 patients of the sample presented here were also included in an earlier study of this population.5 Information on demographic and medical characteristics, past medical history, and voice diagnosis was abstracted from the participants’ medical records. All diagnoses were abstracted from the clinic charts as documented by one of two laryngologists, with no independent or separate review, as in previous studies.1, 4 In cases where multiple possible diagnostic categories were invoked, an inclusive approach was taken and all potential or definitive diagnoses from the clinical encounter were recorded. The study was approved by the University of Minnesota Institutional Review Board (IRB# 1201M9533).
Instruments
Overall psychosocial distress, including depression, anxiety, and somatic symptoms, was assessed using the Brief Symptom Inventory-18 (BSI-18).14 The BSI-18 has been used in a variety of patient populations15–17 and has demonstrated strong reliability (0.74–0.89 across subscales).18 Patients with T-scores of at least 63, which are approximately equivalent to a 90th percentile on community norms, were considered to have met case criteria.18 To identify “high risk” patients who did not meet the strict criteria for caseness, a cutoff at the 75%ile (equivalent to a T score of 57) was used.14 The BSI-18 can also be interpreted at the subscale level for depression, anxiety, and somatic concerns. The Cronbach’s alpha coefficient for the BSI-18 scale in this sample was 0.92.
The Perceived Stress Scale (PSS)19 was used to evaluate perceived stress (e.g., “In the past month, how often have you felt nervous or stressed?”). The PSS is the most commonly used measure to evaluate perceptions of stress, and has several different versions, including 14 items, 10 items, and 4 items, which are designed to be contextually nonspecific. Scores on all versions have been demonstrated to have strong internal reliability (ranging from 0.72 to 0.86) and population norms have been established.19–21 The PSS-4 is derived from the four most predictive items from the longer scales and has been shown to have comparable reliability to the 10-item version.19 To minimize participant burden, we used the 4-item scale to assess perceived stress. The Cronbach’s alpha coefficient for the PSS-4 scale in this sample was 0.79.
A scale that measures perceived control (Perceived Control over Stressful Events Scale) has been developed by Frazier et al. and has strong content validity, factor structure, internal consistency, and test-retest reliability.8 For this study we used the present perceived control subscale, as it is the most strongly associated with outcomes.8 The present control subscale is an 8-item measure designed to assess perceptions of present control over specific stressors and was adapted for use in the context of a voice problem. Individuals rated each of the eight items (e.g., “How I deal with this voice problem now is under my control”) on a 4-point scale (1 = strongly disagree to 4 = strongly agree). Higher mean scores indicate greater levels of perceived control. In previous research, Cronbach’s alpha coefficients for the present control scale have ranged from 0.77 to 0.86 and 3-week test-retest reliability was 0.59)8. The Cronbach’s alpha coefficient for the present control scale (PPC-8) in this sample was 0.79.
Patient-reported vocal handicap was used as the primary measure of vocal function. The 10-item version of the Voice Handicap Index22, the VHI-10,23 was used in this study. The VHI-10 has excellent reliability (ranging from 0.88 to 0.97 in voice-disordered patients and in nonclinical samples)23 and normative values have been established.24 Patients were asked to rate their agreement with statements such as “People seem irritated with my voice,” and “I tend to avoid groups of people because of my voice.” The Cronbach’s alpha coefficient for VHI-10 scale in this sample was 0.91.
Data Analysis
Data were analyzed using Statistical Package for the Social Sciences (SPSS 22, Armonk, NY). Initial data analyses revealed no outliers or deviations from normality. In instances where scales were incomplete, mean imputation was used if more than 70% of the scale had been completed (i.e., no more than 3 of 10 items was missing). Scales were excluded from analysis if they were missing more than 30% of responses. Overall, less than 5% of responses to any single item was missing, and only 3% of the scales were excluded from analysis. Means and proportions were used to summarize and describe the data. Pearson’s correlations were calculated to assess the extent to which individuals with higher vocal handicap reported greater distress and perceived stress, as would individuals with lower perceived present control. To investigate the hypothesis that vocal handicap would be more strongly related to distress for patients who perceived less control over their voice problem, we followed recommendations provided by Frazier et al. for testing moderation effects using multiple regression).6 Voice-related handicap (VHI) was the independent variable, perceived present control was the moderator variable, and mental health symptoms and perceived stress were the dependent variables. The predictor and moderator variables were converted to Z scores and entered into the first step of the multiple regression equation. The Predictor×Moderator interaction term was entered in the second step. Moderation was detected if this interaction term was significant. Simple slopes were calculated for groups representing 1 standard deviation above and below the mean of present control and vocal handicap for significant interactions. Effect sizes were derived using the differences between the high and low PPC groups within the high VHI category; the original population mean was used for this derivation.25
RESULTS
Five hundred thirty three patients enrolled in the study (86% of eligible patients); 326 were women (61%) and 207 were men (39%). The predominant self-reported race was white (88%), with 3.4% reporting black race, 0.75% American Indian or Alaska Native, 1.5% Asian, 2% other, 3.4% multiracial, and 1.5% declined to answer. The majority of patients were married (56%). Typical vocal demand widely varied, with 37% reporting routine voice use and 35% reporting extensive or extraordinary vocal demand. Among all participants, 21% reported a prior diagnosis of anxiety and 22% reported a prior diagnosis of depression. The most common voice-related diagnoses were muscle tension dysphonia (49%), benign vocal fold mass/lesion (25%), and irritable larynx (17%). Some patients were included in more than one diagnostic category, as described above.
Prevalence of Voice Handicap and Distress
In line with our previous research, participants reported high levels of voice handicap and distress.5 On the measure of voice handicap, approximately 77% of the sample scored above the cut-off of 11 (mean [M] = 19.39, standard deviation [SD] = 9.49) established by Rosen et al. for dysphonia.23 With regard to distress symptoms, 34% of the patients (n=181) met case criteria either based on BSI total score or by a score that met case criteria for one or more subdomains.18 This included 22% who met criteria for caseness in the somatic subdomain, 18% who met criteria for caseness in the depression subdomain, and 19% who met criteria for caseness in the anxiety subdomain. Moreover, nearly half of all participants (n=266) were identified to be at “high risk” for mental health difficulties based on scoring in the 75%ile percentile or higher on at least one BSI subdomain scale.14 Participants also reported higher levels of perceived stress symptoms (M= 5.24, SD = 3.42) than a normative sample of adults taking part in a smoking cessation program (M = 4.49, SD = 2.96); the between-group effect size was d = 0.25.20 On average, participants reported moderate levels of perceived present control over their stressors (M = 2.94, SD = 0.60).
Relationships between Voice Handicap, Present Control and Distress
Correlations between vocal handicap, perceived present control, mental health symptoms, and perceived stress are presented in Table 1. As predicted, individuals who reported greater vocal handicap reported higher levels of psychological distress (r = 0.13; p = 0.003), higher levels of perceived stress (r = 0.16; p < 0.0001), and lower levels of perceived present control (r = −0.30, p < 0.0001). Individuals who reported lower perceived present control reported higher levels of distress (r = −0.41, p < 0.0001) and higher levels of perceived stress (r = −0.41, p < 0.0001).
Table 1.
Pearson’s correlation coefficients between variables
| VHI-10 | BSI-18 | PSS-4 | |
|---|---|---|---|
| VHI-10 | |||
| BSI-18 | 0.13 (p = 0.003) | ||
| PSS-4 | 0.16 (p < 0.0001) | 0.65 (p < 0.0001) | |
| PPC-8 | −0.30 (p < 0.0001) | −0.41 (p < 0.0001) | −0.41 (p < 0.0001) |
Moderation Analysis
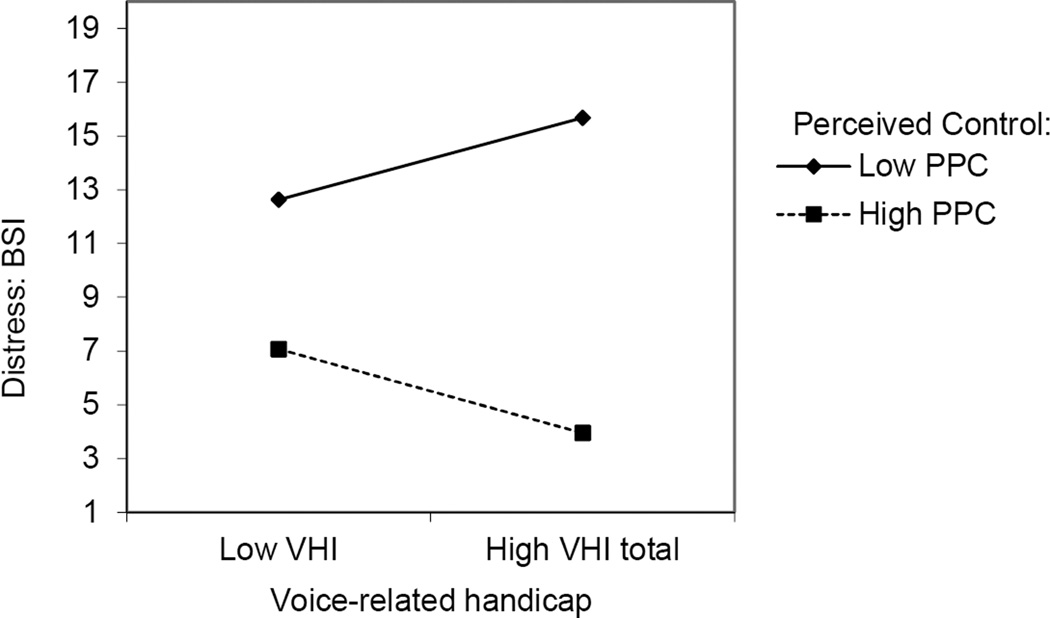
Regression analyses revealed significant interaction effects for perceived present control (see Tables 2). As shown in Figure 1, perceived present control moderated the relationship between vocal handicap and overall psychological distress (t = −3.64, p < 0.001). The simple slope for individuals who reported higher levels of present control (1 SD above the mean) was −1.56 (t = −2.46, p = 0.014) and the simple slope for individuals who reported lower levels of present control (1 SD below the mean) was 1.52 (t = 2.51, p = 0.013). In other words, individuals with lower levels of perceived present control reported greater distress in association with greater voice handicap. For those with high VHI scores, the effect size for the difference in distress between individuals low and high in perceived present control was estimated to be Cohen’s d = 1.08.
Table 2.
Hierarchical regression of BSI-18
| Variable | B | SE(B) | Standardized B |
|---|---|---|---|
| Step 1 | |||
| PPC (Z score) | −4.37 | 0.46 | −0.41*** |
| VHI (Z score) | 0.05 | 0.46 | 0.01 |
| Step 2 | |||
| PPC (Z score) | −4.32 | 0.45 | −0.40*** |
| VHI (Z score) | −0.02 | 0.45 | −0.002 |
| PPC x VHI Interaction | −1.54 | 0.42 | −0.15*** |
= p <0 .001 (two tailed)
Figure 1.
Present control moderated the relationship between vocal handicap and overall psychological distress
[Abbreviations: BSI: Brief Symptom Inventory; VHI: Voice handicap Index; PPC: Present Perceived Control.]
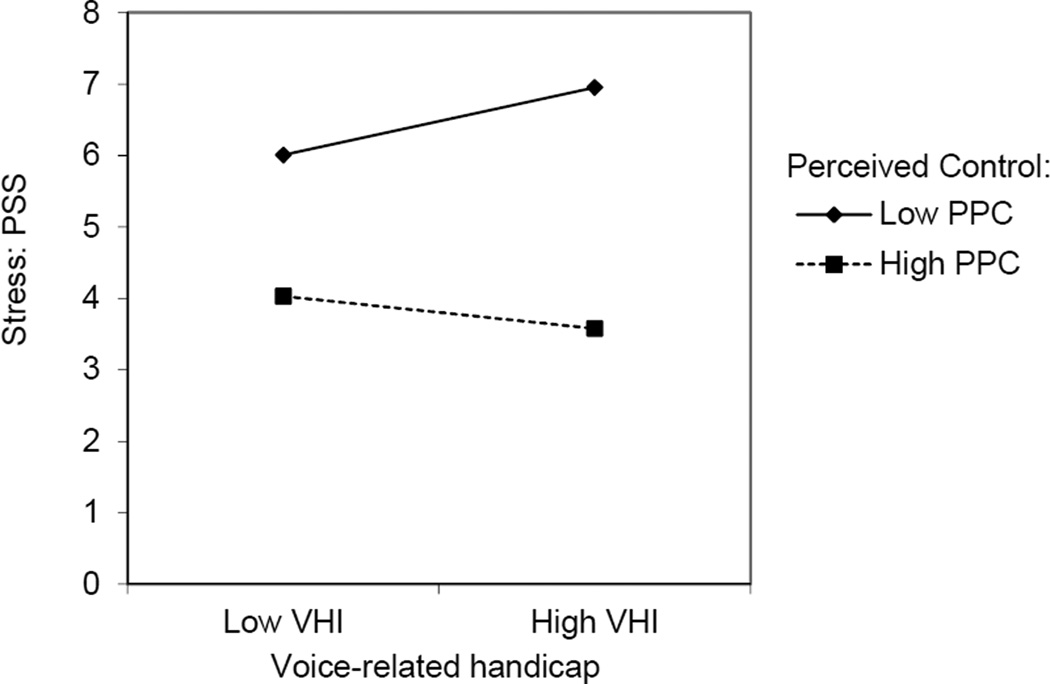
As shown in Table 3 and Figure 2, present control also moderated the relationship between vocal handicap and perceived stress symptoms (t = −2.61, p = 0.01). The simple slope for individuals who reported higher levels of present control (1 SD above the mean was −0.23, which was not significant (t = −1.128, p = 0.26). The simple slope for individuals who reported lower levels of present control (1 SD below the mean) was 0.47 (t = 2.46, p = 0.014). These interactions suggested that vocal handicap was more strongly related to distress and perceived stress among those who perceived less control over stressors related to their voice problems. For those with high VHI scores, the effect size for the difference in perceived stress between individuals low and high in perceived present control was estimated to be Cohen’s d = 0.99.
Table 3.
Hierarchical regression of PSS-4
| Variable | B | SE(B) | Standardized B |
|---|---|---|---|
| Step 1 | |||
| PPC (Z score) | −1.35 | 0.14 | −0.40*** |
| VHI (Z score) | 0.14 | 0.14 | 0.04 |
| Step 2 | |||
| PPC (Z score) | −1.34 | 0.14 | −0.40*** |
| VHI (Z score) | 0.12 | 0.14 | 0.04 |
| PPC X VHI Interaction | −0.35 | 0.13 | −0.11** |
= p < 0. 001 (two tailed),
= p <0 .01 (two tailed)
Figure 2.
Present control moderated the relationship between vocal handicap and perceived stress symptoms
[Abbreviations: PSS: Perceived Stress Scale; VHI: Voice handicap Index; PPC: Present Perceived Control.]
DISCUSSION
We observed a weak but significant correlation (r = 0.13) between severity of distress and voice-related handicap. The strength of this association was similar to the prior findings of Siupsinskiene et al.4 while using a different measure of distress that allowed assessment of somatization in addition to depression and anxiety. Stronger relationships were observed between present perceived control and distress (r = −0.41), and present perceived control and voice-related handicap (r = −0.30), suggesting that perceived control was an important factor for these patients. Moderation analysis provided support for this finding, demonstrating that perceived control moderated the relationship between distress and voice handicap.
The identification of perceived control as a moderator helps to explain the weak magnitude of the overall correlation, which represented a mix of patients for whom there was a strong association between severity of distress and voice handicap and others for whom the two were unrelated. Thus, it appears that the relationship between distress and voice handicap is only strong in some patients, and examining a moderating variable allowed the identification of individuals who may have the greatest risk for difficulty and greatest need for help. This information could be applied to improve clinical assessment and treatment approaches by identifying patients who might need additional resources or treatment options beyond current standard voice care.
Although to our knowledge this is the largest study of distress in voice patients, our findings should be interpreted in the context of several limitations. The participants were care-seeking patients at a tertiary academic medical center and therefore some aspects of these findings may not generalize to other patient groups or community samples. The data were collected in a cross-sectional manner; thus, although these findings allow a more nuanced understanding of the relationship between distress and dysphonia, we could assess only association, not causality. This topic is particularly complex as distress may contribute to dysphonia and dysphonia may contribute to distress. Future work will incorporate longitudinal data collection and analysis to examine causality between these variables.
Strengths of this study include the use of psychometrically sound assessment measures and a high enrollment rate, supporting the potential validity of the findings. The inclusion of a broad range of voice-related diagnoses also indicates that these findings may be relevant for a variety of patients, not just for those with particular voice disorders.
Our findings are clinically significant because perceived control is both directly related to outcomes and is potentially modifiable. Present perceived control is associated with better adjustment even after controlling for coping strategies or locus of control.8 In addition, several studies have demonstrated that interventions targeting perceived control are effective for enhancing control and reducing stress and mental health symptoms.8, 9, 26–29 Adaptation of these interventions for use in the voice patient population, for whom the role of behavioral factors can be especially critical, is in progress, and may provide a useful adjunct to existing treatment options.
CONCLUSIONS
We observed a weak association between severity of psychosocial distress and voice-related handicap. We also observed a moderate inverse relationship between perceived control and distress as well as perceived control and voice handicap. Perceived control moderated the relationship of distress and voice handicap, identifying a subset of patients with low perceived control in whom higher voice handicap was associated with greater distress. These findings suggest that targeting perceived present control may provide an opportunity to improve care for patients with voice problems.
ACKNOWLEDGMENTS
This study was funded through NIH UL1TR000114. We are deeply grateful to Brenna Finley MPH, Meg Her MPH, Kathryn Banks BA, and Patricia Fernandes Boettner DDS MS for study coordination. We appreciate thoughtful input from Lions Voice Clinic members Deirdre D. Michael PhD CCC-SLP, Lisa Butcher MS CCC-SLP, Jesse Hoffmeister MS CCC-SLP, and George S. Goding Jr, MD FACS and from Bevan Yueh MD MPH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Accepted for oral presentation at 2015 Annual Symposium of Voice Foundation
Contributor Information
Stephanie Misono, Assistant Professor, Department of Otolaryngology/Head and Neck Surgery, School of Medicine, 420 Delaware St SE, MMC 396, Minneapolis, MN 55455, smisono@umn.edu, 612-626-5526 (phone), 612-625-2101 (fax).
Liza Meredith, Graduate Research Assistant, Department of Psychology, mere0032@umn.edu.
Carol B. Peterson, Research Associate, Assistant Professor, Department of Psychiatry, School of Medicine, peter161@umn.edu.
Patricia A. Frazier, Professor and Associate Chair, Department of Psychology, pfraz@umn.edu.
REFERENCES
- 1.Dietrich M, Verdolini Abbott K, Gartner-Schmidt J, Rosen CA. The frequency of perceived stress, anxiety, and depression in patients with common pathologies affecting voice. J Voice. 2008;22:472–488. doi: 10.1016/j.jvoice.2006.08.007. [DOI] [PubMed] [Google Scholar]
- 2.Mirza N, Ruiz C, Baum ED, Staab JP. The prevalence of major psychiatric pathologies in patients with voice disorders. Ear Nose Throat J. 2003;82:808–810. 812–814. [PubMed] [Google Scholar]
- 3.Willinger U, Volkl-Kernstock S, Aschauer HN. Marked depression and anxiety in patients with functional dysphonia. Psychiatry Res. 2005;134:85–91. doi: 10.1016/j.psychres.2003.07.007. [DOI] [PubMed] [Google Scholar]
- 4.Siupsinskiene N, Razbadauskas A, Dubosas L. Psychological distress in patients with benign voice disorders. Folia Phoniatr Logop. 2011;63:281–288. doi: 10.1159/000324641. [DOI] [PubMed] [Google Scholar]
- 5.Misono S, Peterson CB, Meredith L, et al. Psychosocial Distress in Patients Presenting With Voice Concerns. J Voice. 2014 doi: 10.1016/j.jvoice.2014.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Frazier PA, Tix AP, Barron KE. Testing Moderator and Mediator Effects in Counseling Psychology Research. Journal of Counseling Psychology. 2004;51:115–134. [Google Scholar]
- 7.Bandura A. SOCIAL COGNITIVE THEORY: An Agentic Perspective. Annual Review of Psychology. 2001;52:1–26. doi: 10.1146/annurev.psych.52.1.1. [DOI] [PubMed] [Google Scholar]
- 8.Frazier P, Keenan N, Anders S, Perera S, Shallcross S, Hintz S. Perceived past, present, and future control and adjustment to stressful life events. Journal of personality and social psychology. 2011;100:749–765. doi: 10.1037/a0022405. [DOI] [PubMed] [Google Scholar]
- 9.Frazier P, Anders S, Shallcross S, et al. Further development of the temporal model of control. J Couns Psychol. 2012;59:623–630. doi: 10.1037/a0029702. [DOI] [PubMed] [Google Scholar]
- 10.Sirois FM, Davis CG, Morgan MS. "Learning to live with what you can't rise above": control beliefs, symptom control, and adjustment to tinnitus. Health psychology : official journal of the Division of Health Psychology, American Psychological Association. 2006;25:119–123. doi: 10.1037/0278-6133.25.1.119. [DOI] [PubMed] [Google Scholar]
- 11.Moser DK, Riegel B, McKinley S, et al. The Control Attitudes Scale-Revised: psychometric evaluation in three groups of patients with cardiac illness. Nursing research. 2009;58:42–51. doi: 10.1097/NNR.0b013e3181900ca0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beckjord EB, Glinder J, Langrock A, Compas BE. Measuring multiple dimensions of perceived control in women with newly diagnosed breast cancer. Psychology & health. 2009;24:423–438. doi: 10.1080/08870440903126447. [DOI] [PubMed] [Google Scholar]
- 13.Tomich PL, Helgeson VS. Cognitive adaptation theory and breast cancer recurrence: Are there limits? Journal of consulting and clinical psychology. 2006;74:980–987. doi: 10.1037/0022-006X.74.5.980. [DOI] [PubMed] [Google Scholar]
- 14.Zabora J, BrintzenhofeSzoc K, Jacobsen P, et al. A new psychosocial screening instrument for use with cancer patients. Psychosomatics. 2001;42:241–246. doi: 10.1176/appi.psy.42.3.241. [DOI] [PubMed] [Google Scholar]
- 15.Imayama I, Alfano CM, Kong A, et al. Dietary weight loss and exercise interventions effects on quality of life in overweight/obese postmenopausal women: a randomized controlled trial. The international journal of behavioral nutrition and physical activity. 2011;8:118. doi: 10.1186/1479-5868-8-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gaylord SA, Palsson OS, Garland EL, et al. Mindfulness training reduces the severity of irritable bowel syndrome in women: results of a randomized controlled trial. The American journal of gastroenterology. 2011;106:1678–1688. doi: 10.1038/ajg.2011.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vangel SJ, Jr, Rapport LJ, Hanks RA. Effects of family and caregiver psychosocial functioning on outcomes in persons with traumatic brain injury. The Journal of head trauma rehabilitation. 2011;26:20–29. doi: 10.1097/HTR.0b013e318204a70d. [DOI] [PubMed] [Google Scholar]
- 18.Derogatis LR. BSI 18 (Brief Symptom Inventory 18): Administration, Scoring, and Procedures Manual. Bloomington, MN: NCS Pearson; 2000. [Google Scholar]
- 19.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of health and social behavior. 1983;24:385–396. [PubMed] [Google Scholar]
- 20.Cohen S, Williamson G. Perceived Stress in a probability sample of the U.S. In: Spapacam S, Oskamp S, editors. The social psychology of health: Claremont Symposium on Applied Social Psychology. 1988. [Google Scholar]
- 21.Cohen S, Janicki-Deverts D. Who's Stressed? Distributions of Psychological Stress in the United States in Probability Samples from 1983, 2006, and 20091. Journal of Applied Social Psychology. 2012;42:1320–1334. [Google Scholar]
- 22.Jacobson BH, Johnson A, Grywalski C, et al. The Voice Handicap Index (VHI): Development and Validation. Am J Speech Lang Pathol. 1997;6:66–70. [Google Scholar]
- 23.Rosen CA, Lee AS, Osborne J, Zullo T, Murry T. Development and validation of the voice handicap index-10. Laryngoscope. 2004;114:1549–1556. doi: 10.1097/00005537-200409000-00009. [DOI] [PubMed] [Google Scholar]
- 24.Arffa RE, Krishna P, Gartner-Schmidt J, Rosen CA. Normative values for the Voice Handicap Index-10. J Voice. 2012;26:462–465. doi: 10.1016/j.jvoice.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 25.Dunlap WP, Cortina JM, Vaslow JB, Burke MJ. Meta-analysis of experiments with matched groups or repeated measures designs. Psychological Methods. 1996;1:170–177. [Google Scholar]
- 26.Hintz S, Frazier PA, Meredith L. Evaluating an Online Stress Management Intervention for College Students. Journal of counseling psychology. 2014 doi: 10.1037/cou0000014. [DOI] [PubMed] [Google Scholar]
- 27.Frazier PA. Perceived control and distress following sexual assault: a longitudinal test of a new model. Journal of personality and social psychology. 2003;84:1257–1269. doi: 10.1037/0022-3514.84.6.1257. [DOI] [PubMed] [Google Scholar]
- 28.Frazier PA, Mortensen H, Steward J. Coping Strategies as Mediators of the Relations Among Perceived Control and Distress in Sexual Assault Survivors. Journal of Counseling Psychology. 2005;52:267. [Google Scholar]
- 29.Frazier P, Meredith L, Greer C, et al. Randomized controlled trial evaluating the effectiveness of a web-based stress management program among community college students. Anxiety, Stress and Coping. doi: 10.1080/10615806.2014.987666. In press. [DOI] [PubMed] [Google Scholar]