Highlights
-
•
Pseudoaneurysm of the cystic artery following acute cholecystitis is rare.
-
•
It can be safely managed laparoscopically with simultaneous cholecystectomy.
-
•
This avoids multiple invasive procedures and decreases morbidity associated with open surgery.
Keywords: Laparoscopic, Cystic artery, Pseudoaneurysm, Calculus cholecystitis
Abstract
INTRODUCTION
Pseudoaneurysm of the cystic artery is very rare. In the majority of cases it has been reported as a post-operative complication of laparoscopic cholecystectomy, however it has also been associated with the presence of acute cholecystitis or pancreatitis.
When these pseudoaneurysms rupture they can lead to intraperitoneal bleeding, haemobilia and upper gastrointestinal haemorrhage. Radiological as well as open surgical approaches have been described for control of this rare pathology.
PRESENTATION OF CASE
We report the laparoscopic surgical management of an incidental, unruptured cystic artery pseudoaneurysm in a patient presenting with acute cholecystitis.
DISCUSSION
Cystic artery pseudoaneurysm is a rare entity and as such there is no consensus on the clinical management of this condition. A variety of treatment strategies have been reported in the literature including radiological selective embolisation and coiling, open cholecystectomy with ligation of the aneurysm, or a two-step approach involving radiological management of the pseudoaneurysm followed by an elective cholecystectomy.
CONCLUSION
In this report we have demonstrated that laparoscopic management of a cystic artery pseudoaneurysm with simultaneous laparoscopic cholecystectomy is feasible and safe. This avoids multiple invasive procedures and decreases morbidity associated with open surgery.
1. Background
Aneurysmal dilatation of an otherwise normal artery in the background of an inflammatory process or previous trauma differentiates a pseudoaneurysm from a true aneurysm. Pseudoaneurysm of the cystic artery is rare. The majority of cases are complications of biliary surgery or angiographic intervention due to injury to the vascular wall [1]. Pseudoaneurysms secondary to acute or chronic calculous cholecystitis are rare despite the high incidence of cholecystitis. To the best of our knowledge less than 25 such cases have been reported in the literature [2–25].
The pathophysiology of aneurysmal dilatation of the cystic artery in the presence of calculous cholecystitis is not clear but it is thought that the artery is eroded either by direct pressure of gallstones or inflammation of the arterial wall. This consequently leads to damage of the adventitia with localised weakness in the vessel wall and formation of a pseudoaneurysm.
Clinical presentation is usually with a ruptured pseudoaneurysm. Patients may suffer intraperitoneal bleeding and shock, acute haemorrhagic cholecystitis or rarely haemobilia and Quincke's triad – gastrointestinal bleeding, right upper quadrant pain and jaundice.
The unruptured pseudoaneurysm is detected as an ‘incidentaloma’ on radiological investigations of the biliary system. The appearance of an enhancing ‘nodule’ on the cystic artery or embedded in the inflamed gallbladder wall, should raise the suspicion of a pseudoaneurysm.
We hereby describe our case of an unruptured cystic artery aneurysm in the context of acute calculous cholecystitis, which was detected incidentally on biliary imaging and was treated laparoscopically with simultaneous cholecystectomy. To our knowledge there is only one further report of this in the literature [2].
2. Case presentation
A 61-year-old female presented with a 24-h history of right upper and lower quadrant abdominal pain and vomiting. At the time of presentation she was afebrile and haemodynamically stable. She did not have any haematemesis or malaena. Her past medical history included a hiatus hernia, hypertension, asthma and a hysterectomy. Her medications included lansoprazole, bendroflumethiazide, ventolin and seretide.
On examination she was tender over the right side of the abdomen with guarding in the right upper quadrant.
3. Investigations
Her laboratory investigations revealed: haemoglobin 14.5, white cell count 18.1, C-reactive protein 8, bilirubin 9, ALP 57, AST 20, ALT 17 and an amylase of 49.
At this point the patient underwent contrast enhanced computed tomography (CECT) and an ultrasound scan (USS) of the abdomen. The CECT revealed extensive cholecystitis with pericholecystic fluid collection and a small amount of fluid in the pelvis (Figs. 1 and 2). A 12 mm × 15 mm × 8 mm cystic artery pseudoaneurysm (Figs. 1 and 2) was also identified with no evidence of rupture. The rest of the intra-abdominal organs were unremarkable. A limited USS revealed multiple calculi within the gallbladder lumen. There was no intra or extra-hepatic duct dilatation. The cystic artery pseudoaneurysm was not visualised on USS.
Fig. 1.

CT – cross section. Arrow: cystic artery pseudoaneurysm enhancing with contrast. Arrow head: gallbladder with pericholecystic fluid.
Fig. 2.

CT – coronal section. Arrow: cystic artery pseudoaneurysm enhancing with contrast. Arrow head: gallbladder with pericholecystic fluid.
4. Differential diagnosis
She was admitted under the surgical team with the working diagnosis of acute cholecystitis or appendicitis.
Antibiotics were given for treatment of acute cholecystitis. The case was discussed in our hepato-biliary multi-disciplinary meeting. The decision was to treat the acute episode of cholecystitis and subsequently admit the patient within 4–6 weeks for an elective simultaneous laparoscopic cholecystectomy and proximal control of the cystic artery aneurysm.
5. Treatment
The procedure was jointly performed by an upper gastrointestinal and a hepatopancreatobiliary surgeon with extensive laparoscopic experience. The patient had standard pre-operative checks and was cross-matched two units of red cells. This operation was conducted under general anaesthetic. A standard laparoscopic cholecystectomy set was used with the addition of a Harmonic® scalpel. A major laparotomy and a vascular instrument set were kept on stand-by.
Pneumoperitoneum was induced through the umbilicus using an open technique and the standard 4-port laparoscopic cholecystectomy approach utilised.
The gallbladder had inflammatory adhesions to the omentum and duodenum, which were released by energised dissection (Fig. 3). A posterior window of safety was created followed by dissection of a secondary window between the cystic artery and cystic duct. After a combination of careful blunt and energised dissection, the anatomy was clearly defined.
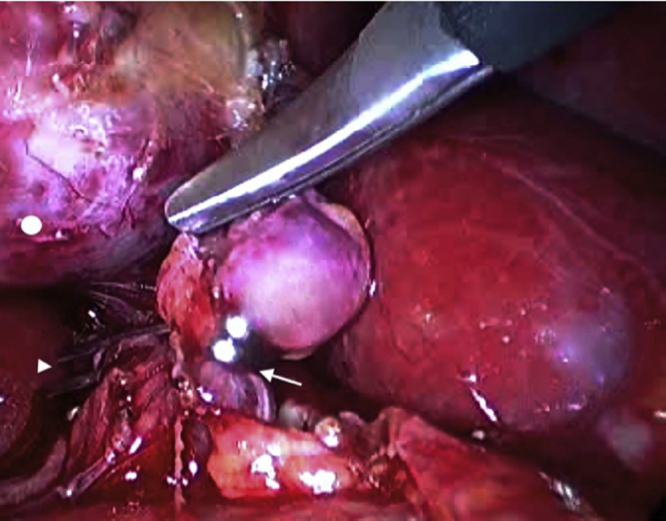
Fig. 3.

Arrow: gallbladder with inflammatory adhesions.
The cystic duct was short and approximately 10 mm in diameter. The neck of the gallbladder contained a 8 mm gallstone. Both the anterior and posterior branches of the cystic artery were identified. The pseudoaneurysm arose from the anterior branch of the cystic artery. Through careful blunt dissection this was freed from adhesions to the gallbladder wall.
At this point we opted to control the pseudoaneurysm. The proximal part of the cystic artery was carefully dissected to allow the application of clips. Two 10 mm titanium clips were applied proximally to the pseudoaneurysm and one applied distally adjacent to the gallbladder. Using the Harmonic scalpel the artery was divided just proximal to the distal clip, over the pseudoaneurysm (Fig. 4). The posterior branch of the cystic artery was similarly clipped and divided with two proximal and one distal 10 mm clip.
Fig. 4.
Arrow: cystic artery pseudoaneurysm with proximal control with clips on anterior branch of cystic artery. Arrow head: clips on posterior branch of cystic artery. Circle: gallbladder.
The short cystic duct contained a stone, which was ‘milked’ into the gallbladder.
Extra-large Hem-o-lok® were used to clip the cystic duct; two proximally and one distally followed by division of the duct (Fig. 5).
Fig. 5.
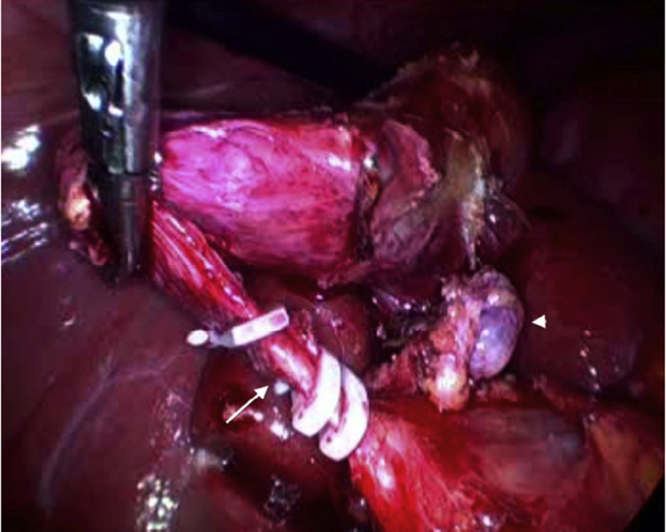
Arrow: cystic duct with Hem-o-lok® applied. Arrow head: clipped cystic artery pseudoaneurysm.
The gallbladder was dissected off the liver bed using standard technique and retrieved using a disposable tissue retrieval bag. Haemostasis was ensured and a local wash with normal saline was performed. A 14 French suction drain was left in the subhepatic space.
6. Outcome
The patient made an uneventful recovery and was discharged the following morning after confirmation of normal liver function tests and haemoglobin levels.
7. Discussion
We have described a case of an unruptured cystic artery pseudoaneurysm, which was managed laparoscopically. We have to assume that the cause of the pseudoaneurysm in our case was acute calculous cholecystitis as no other potential risk factors were identified. Furthermore, appearances on imaging as well as intra-operative inspection of the cystic artery were in keeping with an otherwise normal vessel. Of additional interest is the impacted gallstone at the gallbladder neck, which was seen intraoperatively. Therefore, it is possible that in addition to the acute inflammation of cholecystitis, the direct pressure effect by the gallstone on the cystic artery accelerated the formation of the pseudoaneurysm.
The diagnosis of a bleeding pseudoaneurysm in an unstable patient should be prompt.
Ultrasound with or without Doppler used in combination with cross sectional imaging such as CECT are usually adequate in making the diagnosis. Magnetic resonance imaging (MRI) can additionally be used in equivocal cases.
A literature search identified 24 reports of cystic artery pseudoaneurysm associated with cholecystitis. In 22 of these reports the patients had presented with an already ruptured pseudoaneurysm and features of gastrointestinal bleeding. Interestingly, only two cases reported an unruptured cystic artery pseudoaneurysm being diagnosed as ‘incidentalomas’ making our case the third in the literature. One of those was managed with open cholecystectomy and ligation of the cystic artery [8] while the other was managed laparoscopically [2].
Cystic artery pseudoaneurysm is a rare entity and as such there is no consensus on the clinical management of this condition. A variety of treatment strategies have been reported in the literature including radiological selective embolisation and coiling, open cholecystectomy with ligation of the aneurysm, or a two-step approach involving radiological management of the pseudoaneurysm followed by an elective cholecystectomy.
In high risk patients with active bleeding angiographic embolisation has been performed successfully [7]. The definitive management of these patients is cholecystectomy and ligation of the pseudoaneurysm. Therefore, embolisation and coiling can be seen as a ‘bridge’ to surgery in an attempt to stabilise the patient and avoid an emergency laparotomy.
Because of the high risk of pseudoaneurysm rupture surgeons have avoided the laparoscopic approach. In this report we have demonstrated that laparoscopic management of a cystic artery pseudoaneurysm with simultaneous laparoscopic cholecystectomy is feasible and safe. Surgeons that undertake such tasks need advanced laparoscopic skills and the necessary support.
Conflict of interest
None.
Funding
None.
Consent
Obtained. Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contributions
The four authors were involved in all aspects including:
Conception and design, acquisition of data or analysis and interpretation of data.
Drafting the article or revising it critically for important intellectual content.
Final approval of version published.
Research registry
researchregistry265.
Guarantor
All authors.
Learning points.
-
•
Pseudoaneurysm of the cystic artery following acute cholecystitis is rare.
-
•
It can be safely managed laparoscopically with simultaneous cholecystectomy.
-
•
This avoids multiple invasive procedures and decreases morbidity associated with open surgery.
References
- 1.Baker K.S., Tisnado J., Cho S.R., Beachley M.C. Splanchnic artery aneurysms and pseudoaneurysms: transcatheter embolization. Radiology. 1987;163:135–139. doi: 10.1148/radiology.163.1.3823426. [DOI] [PubMed] [Google Scholar]
- 2.Dewachter L., Dewaele T., Rosseel F., Crevits I., Aerts P., De Man R. Acute cholecystitis with pseudoaneurysm of the cystic artery. J. Belg. Radiol. – Belg. Tijdschr. Radiol. 2012;95(May–June (3)):136–137. doi: 10.5334/jbr-btr.584. [DOI] [PubMed] [Google Scholar]
- 3.Chong J.J., O’Connell T., Munk P.L., Yang N., Harris A.C. Case of the month #176: pseudoaneurysm of the cystic artery. Can. Assoc. Radiol. J. 2012;63(May (2)):153–155. doi: 10.1016/j.carj.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 4.Siddiqui N.A., Chawla T., Nadeem M. Cystic artery pseudoaneurysm secondary to acute cholecystitis as cause of haemobilia. BMJ Case Rep. 2011:2011. doi: 10.1136/bcr.07.2011.4480. PMCID: PMC3185451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hague J., Brennand D., Raja J., Amin Z. Cystic artery pseudoaneurysms in hemorrhagic acute cholecystitis. Cardiovasc. Interv. Radiol. 2010;33(December (6)):1287–1290. doi: 10.1007/s00270-010-9861-7. [DOI] [PubMed] [Google Scholar]
- 6.Desai A.U., Saunders M.P., Anderson H.J., Howlett D.C. Successful transcatheter arterial embolisation of a cystic artery pseudoaneurysm secondary to calculus cholecystitis: a case report. J. Radiol. Case Rep. 2010;4(2):18–22. doi: 10.3941/jrcr.v4i2.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mullen R., Suttie S.A., Bhat R., Evgenikos N., Yalamarthi S., McBride K.D. Microcoil embolization of mycotic cystic artery pseudoaneurysm: a viable option in high-risk patients. Cardiovasc. Interv. Radiol. 2009;32(November (6)):1275–1279. doi: 10.1007/s00270-009-9590-y. [DOI] [PubMed] [Google Scholar]
- 8.Machida H., Ueno E., Shiozawa S., Fujimura M., Tsuchiya A., Kim D.H., Ogawa K., Aiba M. Unruptured pseudoaneurysm of the cystic artery with acute calculous cholecystitis incidentally detected by computed tomography. Radiat. Med. 2008;26(July (6)):384–387. doi: 10.1007/s11604-008-0243-x. [DOI] [PubMed] [Google Scholar]
- 9.Radouane B., Jidal M., El Fenni J., Chaouir S., Amil T., Hanine A., Benameur M. Pseudoaneurysm of the cystic artery complicating calculous cholecystitis: a case report. J. Radiol. 2008;89(March (3 Pt. 1)):345–346. doi: 10.1016/s0221-0363(08)93010-9. [DOI] [PubMed] [Google Scholar]
- 10.Saluja S.S., Ray S., Gulati M.S., Pal S., Sahni P., Chattopadhyay T.K. Acute cholecystitis with massive upper gastrointestinal bleed: a case report and review of the literature. BMC Gastroenterol. 2007;7(March):12. doi: 10.1186/1471-230X-7-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Akatsu T., Tanabe M., Shimizu T., Handa K., Kawachi S., Aiura K., Ueda M., Shimazu M., Kitajima M. Pseudoaneurysm of the cystic artery secondary to cholecystitis as a cause of hemobilia: report of a case. Surg. Today. 2007;37(5):412–417. doi: 10.1007/s00595-006-3423-2. [DOI] [PubMed] [Google Scholar]
- 12.Lee J.W., Kim M.Y., Kim Y.J., Suh C.H. CT of acute lower GI bleeding in chronic cholecystitis: concomitant pseudoaneurysm of cystic artery and cholecystocolonic fistula. Clin. Radiol. 2006;61(July (7)):634–636. doi: 10.1016/j.crad.2006.02.007. [DOI] [PubMed] [Google Scholar]
- 13.Pérez-Castrillón J.L., Mendo M., Calero H. Hemorrhage into the gallbladder caused by pseudoaneurysm of the cystic artery. Endoscopy. 2006;38(Suppl. 2):E50. doi: 10.1055/s-2006-944681. [DOI] [PubMed] [Google Scholar]
- 14.Joyce M.R., Donnolly M., O'Shea L., Jeffers M., O’Riordain D. Pseudoaneurysm of the cystic artery: a diagnostic dilemma and rare cause of haemobilia. Ir. J. Med. Sci. 2006;175(January–March (1)):81. doi: 10.1007/BF03169011. [DOI] [PubMed] [Google Scholar]
- 15.Gutiérrez G., Ramia J.M., Villar J., Garrote D., Ferron A., Ruiz E. Cystic artery pseudoaneurism from an evolved acute calculous cholecystitis. Am J Surg. 2004;187(April (4)):519–520. doi: 10.1016/j.amjsurg.2003.12.033. [DOI] [PubMed] [Google Scholar]
- 16.Maeda A., Kunou T., Saeki S., Aono K., Murata T., Niinomi N., Yokoi S. Pseudoaneurysm of the cystic artery with hemobilia treated by arterial embolization and elective cholecystectomy. J. Hepatobiliary Pancreat. Surg. 2002;9(6):755–758. doi: 10.1007/s005340200105. [DOI] [PubMed] [Google Scholar]
- 17.Nakajima M., Hoshino H., Hayashi E., Nagano K., Nishimura D., Katada N., Sano H., Okamoto K., Kato K. Pseudoaneurysm of the cystic artery associated with upper gastrointestinal bleeding. J. Gastroenterol. 1996;31(October (5)):750–754. doi: 10.1007/BF02347630. [DOI] [PubMed] [Google Scholar]
- 18.Wu T.C., Liu T.J., Ho Y.J. Pseudoaneurysm of the cystic artery with upper gastrointestinal hemorrhage. Case report. Acta Chir. Scand. 1988;154(February (2)):151–152. [PubMed] [Google Scholar]
- 19.Reddy S.C. Pseudoaneurysm of cystic artery with upper gastrointestinal hemorrhage. South Med. J. 1983;76(January (1)):85–86. doi: 10.1097/00007611-198301000-00023. [DOI] [PubMed] [Google Scholar]
- 20.Barba C.A., Bret P.M., Hinchey E.J. Pseudoaneurysm of the cystic artery: a rare cause of hemobilia. Can. J. Surg. 1994;37(February (1)):64–66. [PubMed] [Google Scholar]
- 21.Smague E.A., Schulte F., Guse S. Recurrent hemobilia caused by a ruptured pseudoaneurysm of the cystic artery in the gallbladder. Chirurg. 1990;61(March (3)):199–200. [PubMed] [Google Scholar]
- 22.Strickland S.K., Khoury M.B., Kiproff P.M., Raves J.J. Cystic artery pseudoaneurysm: a rare cause of hemobilia. Cardiovasc. Interv. Radiol. 1991;14(May–June (3)):183–184. doi: 10.1007/BF02577726. [DOI] [PubMed] [Google Scholar]
- 23.Miura K., Hoshino T., Komatsu M., Ono T., Sato T., Tanaka J., Masamune O. A case of hemorrhage into the gallbladder probably due to rupture of pseudoaneurysm formed by cystic artery. Nippon Shokakibyo Gakkai Zasshi. 1998;95:450–454. [PubMed] [Google Scholar]
- 24.Kaman L., Kumar S., Behera A., Katariya R.N. Pseudoaneurysm of the cystic artery: a rare cause of hemobilia. Am. J. Gastroenterol. 1998;93:1535–1537. doi: 10.1111/j.1572-0241.1998.475_y.x. [DOI] [PubMed] [Google Scholar]
- 25.Morioka D., Ueda M., Baba N., Kubota K., Otsuka Y., Akiyama H. Hemobilia caused by pseudoaneurysm of the cystic artery. J. Gastroenterol. Hepatol. 2004;19:724–726. doi: 10.1111/j.1440-1746.2004.03461.x. [DOI] [PubMed] [Google Scholar]


