Abstract
Noma is a gangrenous disease of the orofacial region that leads to severe facial tissue destruction and is a significant cause of death among children. With the advent of modern antibiotics and improved nutrition, children with noma may survive into adulthood, but must face the challenge of undergoing repair of the sequelae of noma. This report describes a case of bony fusion of the maxilla and mandible in a 28-year-old female patient, which was a sequelae of a childhood case of noma.
Keywords: Noma; Jaw Diseases; Tomography, X-ray Computed
The term 'noma' is derived from the Greek word nomein, meaning 'to devour,' which is an allusion to the rapidly destructive course of gangrene.1,2 Hippocrates first described noma in the fifth century BC, and the disease continued to be reported throughout Europe until World War II.3 Noma is not distributed uniformly over the world, and predominantly affects children in the sub-Saharan countries of Senegal, Niger, Nigeria, Mauritania, Chad, Sudan, Mali, and Ethiopia. Occasionally, rare cases are reported in other African countries, as well as in Asia and Latin America.4
The aetiology of noma includes poor oral hygiene in children, poor nutrition, a weak immune system, and a history of measles, scarlet fever, typhoid, bacillary dysentery, malaria, whooping cough, tuberculosis, malignancy, or HIV. The pathogenicity is mainly related to the high bacterial load of normal microorganisms in the oral cavity, which may break down the resistance of the immune system. This results in gangrene that rapidly invades the facial tissues and results in the severe disfigurement of the face.5
The infection causes perforating wounds of the lips, cheek, nose, palate, mandible, and maxilla. Healing occurs with the formation of contractures and fibrosis. The sequelae of noma include salivary leakage, facial mutilation, trismus, and facial asymmetry that may lead to fibrous and bony fusion of the jaws.6 Ankylosis of the jaws and bony fusion of the maxilla and mandible are the most disabling sequelae of noma. Bony ankylosis not only results in difficulty with speech and mastication, but also prevents social eating habits and the maintenance of oral hygiene. It may cause imbalance in facial growth, distorted dental development, and malocclusion.7
Cases of noma are rarely reported in developing countries such as India, and the sequelae of bony fusion of the jaws is extremely rare. In a series of 76 patients with ankylosis of the mandible from various causes, 48.7% of cases were found to be due to noma. Bony ankylosis of the mandible and maxilla has been found to occur in 30%-43% of cases of noma, according to several case series.6 This report describes a rare case of noma that resulted in bony fusion of the maxilla and mandible.
Case Report
A 28-year-old female patient presented to the Department of Oral Medicine and Radiology of the Institute for Technology and Sciences Dental College, Muradnagar, Ghaziabad, India with a chief complaint of inability to open her mouth for 23 years. The patient's history revealed that ulceration on the tongue occurred when she was five years of age, in association with a fever. The ulcer quickly expanded to involve the adjacent structure of the jaw, cheek, and face, perforating the skin and exposing the internal structures. She was treated with indigenous medicine. Although the wound healed within one to two months, a severe scar was left during the healing of the soft tissue defect, and gradually she became unable to open her mouth due to the fusion of both jaws on one side. The patient suffered for almost 23 years, unable to eat or chew food. She also reported swallowing her exfoliated deciduous teeth, as she was unable to spit.
The patient's past dental and medical history was otherwise unremarkable. The patient lived in a remote village and had not undergone any prior medical check-ups. Her personal history revealed that she had always been on a semi-solid or a liquid diet through a straw placed into small openings between the teeth on the right side of her mouth. She experienced no developmental delays and achieved all milestones normally. The patient was poorly built and poorly nourished, with a normal gait, and all her vital signs were within normal limits.
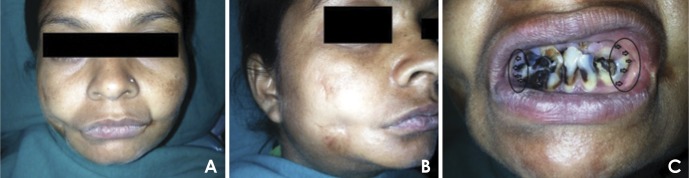
An extra-oral examination revealed facial asymmetry that became more pronounced with age (Fig. 1A). She did not have normally comprehensible speech. The patient could speak relatively uninterruptedly but the words were not completely clear. Her mouth opening was completely restricted, with no movements of the jaw possible on either side. On inspection, a single, roughly oval shaped scar was present on the right lower third of the face, measuring approximately 2 cm×3 cm, extending anteroposteriorly 2 cm behind the right lip commissure to 4 cm in front of the right tragus, and superoinferiorly 5 cm below the outer canthus to the lower border of the mandible on the right side (Fig. 1B). Posterior to the left angle of the mouth, a similar scar was noted. The scars were completely adherent to the mandible. No lateral motion of her temporomandibular joints was observed. An intraoral examination demonstrated that her lips parted and that the opening of her mouth was completely restricted. The labial and buccal mucosa and vestibule were completely adherent to the alveolar ridges on both sides. The remaining teeth visibly present were the lower central and lateral incisors, canine, and premolar, which were grossly decayed (Fig. 1C).
Fig. 1. A. A frontal extraoral photograph shows the scars on both right and left cheeks. B. An extraoral photograph on the right side reveals the scar. C. An intraoral photograph shows grossly decayed anterior teeth with no mouth opening.
On the basis of the clinical findings, a provisional diagnosis of severe trismus was made, with a differential diagnosis of intra-articular fusion, extra-articular fusion with superadded infection, and congenital syngnathia. The patient was then further assessed with a blood examination, a liver and renal function test, an ultrasound of the neck, and a radiological examination, including a panoramic radiograph and three-dimensional computed tomography scan. The complete blood profile and liver and renal function tests were within normal limits. The ultrasound of the neck revealed normal bilateral parotid and submandibular lymph nodes, and no lymph nodes were seen along levels II, IV, and V.
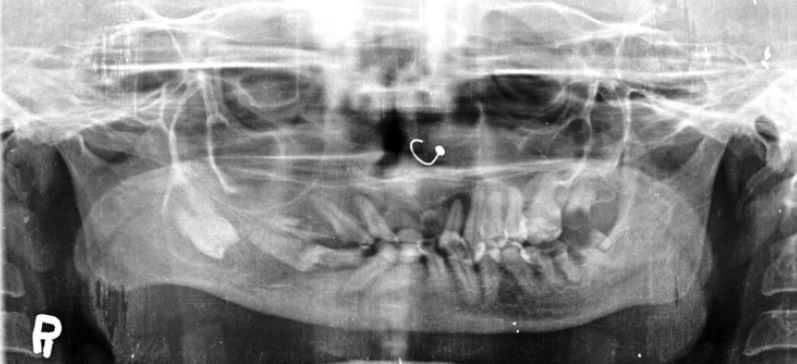
The panoramic radiograph showed that the fusion of the maxilla and mandible extended from the right upper second premolar to the tip of the coronoid process of mandible. The second maxillary molar and the first and second premolars were merged in the bony fusion on the right side. The panoramic radiograph clearly demonstrated the absence of a union of the head of the condyle with the temporal fossa. The right antegonial notch was deep compared to the left side (Fig. 2).
Fig. 2. A panoramic radiograph reveals the fusion of the maxilla and mandible extending from the right upper second premolar to the tip of coronoid process of mandible.
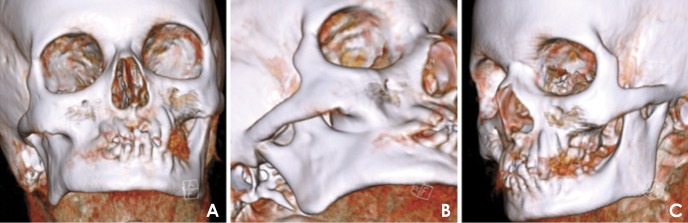
A non-contrast multi-detector computed tomography scan of the head and neck was carried out. Volume data was post-processed in the coronal and axial planes. Three-dimensional volume-rendered images were generated from the acquired data. The multi-detector computed tomography scan showed a bony fusion of the right lateral half of the maxilla with the mandible, extending medially up to the right second premolar and laterally to the base of the proximal aspect of the coronoid process. The length of the fusion was approximately 5 cm. The central portion of the fused area was mildly radiolucent (low density), and the outer margins were dense. (Figs. 3 and 4)
Fig. 3. A. An axial CT image shows the continuous fusion between the maxilla and mandible on the right side. B. A coronal CT image shows the similar features of axial section. C. A coronal CT image shows no fusion of the condylar head of both sides.
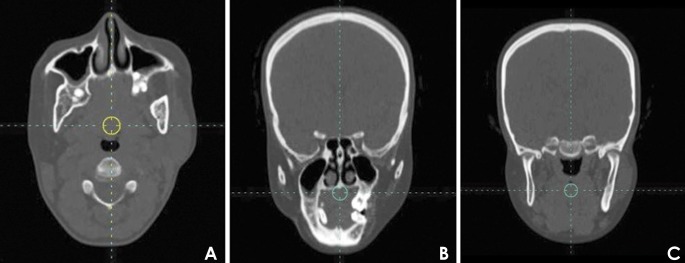
Fig. 4. Three-dimensional CT images. A. Anterior facial area reveals the fused bone. B. Right oblique anterior view indicates bony fusion extending from the right premolar region to the anterior border of ramus of mandible. C. Left oblique anterior view shows no bony fusion.
Based on these findings and the patient's history of illness, the final diagnosis was fusion of the maxilla and mandible on the right side as a sequelae of noma.
Surgical treatment was performed to completely excise the bony fusion of the right arch through an extra-oral approach. The patient was operated on under general anaesthesia. A single extra-oral incision was made from behind the ear and angle of the mandible, splitting the lower lip on the right side. The bony fusion was removed and the right side was closed with a galea flap that was introduced intra-orally by making a tunnel over the zygomatic arch and sutured to make buccal mucosa. A lateral tongue flap was used to make the buccal and lingual vestibules. The decayed anterior and posterior teeth, along with bone and calculus, were removed. Considerably more opening between the arches was noted (Fig. 5). The recovery was uneventful, and the patient was satisfied with the surgical goal of increasing the size of the pathway for eating.
Fig. 5. Post-operative follow-up after 3 month reveals 25 mm mouth opening.

Discussion
Cancrum oris or noma is still a major health problem in many developing countries. The triad of malnutrition, poor oral hygiene, and debilitating disease contributes to its continued presence. Although the precise prevalence of noma is unknown, it ranges from 30,000 to 140,000 cases.8 In high-income countries, noma is now extremely rare. In contrast, noma still persists in the poorest developing countries, predominantly in Africa.3 The epidemiology of noma shows a similar pattern, although the mortality rate has been drastically reduced from 90% to approximately 8%-10% due to modern antibiotics.9 Although noma can affect infants, children, and adults,1 a slight predilection may exist for females over males.6
The direct cause of noma remains a mystery.8 It has been postulated that the disease is triggered by a consortium of microorganisms, of which Fusobacterium necrophorum is a key component.10 The most common predisposing factors are poor oral hygiene, dehydration, malnutrition, and concomitant illnesses, such as measles, scarlet fever, or tuberculosis, malignancies, especially leukaemia, and immunodeficiency disorders, such as AIDS.11
The infection may begin as acute necrotizing ulcerative gingivitis.6 The lesion may then ulcerate and spread to the buccal or lingual sulcus and to the mucosa of the lip or cheek. The progression of the destructive process results in extension to the skin. The greater involvement of the interior of the oral cavity with lesser involvement of the overlying skin has resulted in the lesion being described as a 'cone gangreneux'. Once the slough separates, sequestration of the exposed bone and teeth occurs. The process of defect formation is rapid and is typically well-defined.12 Gangrene of the soft tissues may then be gradually followed by scar tissue repair of the resulting defect. The appearance of false fibrosis occurs. Fibrous ankylosis often sets in before the oral wound is completely healed, due to the contraction of scar tissue in the periphery of the defect. The fibrosis progresses in some patients to true bony fusion between the mandible and maxilla, and sometimes also to the temporomandibular joint.7 The facial bones, jaws, and teeth may be affected to varying degrees.10 The presenting clinical features are similar to those reported by our patient. The site of the cancrum oris ulcer can be identified as a dimple in the smooth contour of the cheek due to ulcer scarring.11 Oluwasanmi et al.7 reported 15 patients with cheek defects, of whom eight had a tell-tale cheek scar overlying the area of the defect, similar to what was found in our patient.
Several studies have shown that the clinicopathological features of cancrum oris are complicated by trismus. If the ankylosis of the jaws is intra-articular, the bony fusion is situated at the temporomandibular joint, and if it is extra-articular, the bony fusion involves the jaws.11 However, the ankylosis in our case involved the maxilla and mandible rather than the temporomandibular joint, which is a rare finding in noma cases. Bony fusion of the mandible is serious and is the most disabling type of fusion. Difficulty with mastication, impairment of speech, poor oral hygiene, and facial asymmetry result in physical and psychological disabilities, particularly in young children with a complete inability to open the mouth.7,13 These problems were observed in our case.
Oluwasanmi et al.7 reported changes in the temporomandibular joint in two patients who had diminished joint space, whereas in two patients, widening was observed in one plane and narrowing in another plane. In our case, no fusion of the condyles was observed, but a reduced joint could be clearly seen in the coronal section of the computed tomography scan.
Diseases occasionally confused with noma that could have been considered in the differential diagnosis of this case include visceral leishmaniasis, yaws, gangosa, syphilis, midline lethal granuloma, tuberculosis, leprosy, lupus erythematous, mucormycosis, agranulocytic ulceration, clostridia gangrene, some tropical fungal infections, oral cancer, and physical trauma. However, these diseases do not generally occur in young children, do not have a rapid progression that would fit the history described by our patient, or do not produce the extent of tissue destruction seen here.6,14
Eating is a major problem for patients with ankylosis. In a series of 17 patients, 57% were found to be anaemic, with haemoglobin levels of under 75% of normal (12 g/dL); levels as low as 19%-30% of normal were not uncommon. Malnutrition and undernutrition occur in many cases; growth retardation may be so severe that an adolescent of 15 years may have the stature of a child of eight years.7 This dynamic was observed in our patient. Although the age of our patient was 28 years, she weighed 37.1 kg, had a height of 146 cm, and had a very low basal metabolic rate of 975 calories.
In extra-articular ankylosis due to cancrum oris, the bony changes are associated with the destruction of the maxilla, the malar bone, and a portion of the mandible. The remaining bone is characterized by areas of sclerosis or rarefaction and the distortion of the normal configuration with loss of the trabecular pattern.13
Further three-dimensional computed tomography imaging in our case was a step forward in being able to clearly visualize the exact architecture of the area of ankylosis prior to surgery, making a much better surgical plan possible.
Antibiotics are mainly indicated for the acute and fulminating early stage of the disease, while surgical intervention is required for the chronic and disfiguring late stage. The eventual plastic and reconstructive operations are designed to reflect individual needs. In order to improve the overall health status of the patients during the acute stage, vitamins can be administered and ionic and acid-base imbalances can be corrected. The surgical correction of noma deformities can be challenging due to the unique patterns of destruction in each case. Hence, no standard surgical procedure is common to all noma cases.1,15 The fused bridges are identified and excised by extra-oral approaches, and scars on the mucosa and the skin are also excised and removed using the same approach.4
This patient presented to us after 23 years of suffering. Her history showed that she was from a remote area. She could not preserve data relevant to the diagnosis of her illness or information that would establish which infection led to complete trismus and the bony fusion of the maxilla and mandible. We were not able to establish the nature of the infection that she suffered from. However, based on the history, oral examination, radiologic examination, and the literature, bony fusion of the maxilla and mandible was considered to be a sequelae of noma. We hypothesized that the massive soft tissue necrosis probably extended into the periosteum and bone, leading to bony fusion of the maxilla and mandible, which is a rare sequelae of noma. Even in a developing country like India, cases of noma may arise in remote areas, and complications involving fusion may occur due to a lack of awareness, misdiagnosis, and negligence. The oral diagnostician should take the necessary steps after diagnosing cases of noma and provide a level of follow-up appropriate for avoiding complications like those observed in this case.
References
- 1.Ogbureke KU, Ogbureke EI. NOMA: a preventable "Scourge" of African children. Open Dent J. 2010;4:201–206. doi: 10.2174/1874210601004010201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Woon CY, Sng KW, Tan BK, Lee ST. Case report journey of a noma face. Eplasty. 2010;10:e49. [PMC free article] [PubMed] [Google Scholar]
- 3.Baratti-Mayer D, Gayet-Ageron A, Hugonnet S, François P, Pittet-Cuenod B, Huyghe A, et al. Risk factors for noma disease: a 6-year, prospective, matched case-control study in Niger. Lancet Glob Health. 2013;1:e87–e96. doi: 10.1016/S2214-109X(13)70015-9. [DOI] [PubMed] [Google Scholar]
- 4.Marck KW, Bruijn HP. Surgical treatment of noma. Oral Dis. 1999;5:167–171. doi: 10.1111/j.1601-0825.1999.tb00084.x. [DOI] [PubMed] [Google Scholar]
- 5.Bello SA, Aluko Olokun B, Olaitan AA, Ajike SO. Aetiology and presentation of ankylosis of the temporomandibular joint: report of 23 cases from Abuja, Nigeria. Br J Oral Maxillofac Surg. 2012;50:80–84. doi: 10.1016/j.bjoms.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 6.Deeb GR, Yih WY, Merrill RG, Lundeen RC. Noma: report of a case resulting in bony ankylosis of the maxilla and mandible. Dentomaxillofac Radiol. 1999;28:378–382. doi: 10.1038/sj/dmfr/4600475. [DOI] [PubMed] [Google Scholar]
- 7.Oluwasanmi JO, Lagundoye SB, Akinyemi OO. Ankylosis of the mandible from cancrum oris. Plast Reconstr Surg. 1976;57:342–350. doi: 10.1097/00006534-197603000-00011. [DOI] [PubMed] [Google Scholar]
- 8.Marck KW. Noma: a neglected enigma. Lancet Glob Health. 2013;1:e58–e59. doi: 10.1016/S2214-109X(13)70035-4. [DOI] [PubMed] [Google Scholar]
- 9.Oginni FO, Oginni AO, Ugboko VI, Otuyemi OD. A survey of cases of cancrum oris seen in Ile-Ife, Nigeria. Int J Paediatr Dent. 1999;9:75–80. doi: 10.1046/j.1365-263x.1999.00110.x. [DOI] [PubMed] [Google Scholar]
- 10.Wazir SM, Khan SU. Cancrum oris. J Pak Assoc Dermatol. 2008;18:110–112. [Google Scholar]
- 11.Lagundoye SB, Oluwasanmi JO. Radiologic examination of trismus as a complication of cancrum oris. Oral Surg Oral Med Oral Pathol. 1975;39:812–820. doi: 10.1016/0030-4220(75)90043-2. [DOI] [PubMed] [Google Scholar]
- 12.Lazarus D, Hudson DA. Cancrum oris - a 35-year retrospective study. S Afr Med J. 1997;87:1379–1382. [PubMed] [Google Scholar]
- 13.Adekeye EO. Ankylosis of the mandible: analysis of 76 cases. J Oral Maxillofac Surg. 1983;41:442–449. doi: 10.1016/0278-2391(83)90129-5. [DOI] [PubMed] [Google Scholar]
- 14.Enwonwu CO, Falkler WA, Jr, Phillips RS. Noma (cancrum oris) Lancet. 2006;368:147–156. doi: 10.1016/S0140-6736(06)69004-1. [DOI] [PubMed] [Google Scholar]
- 15.Giessler GA, Schmidt AB, Deubel U, Cornelius CP. Free flap transfer for closure and interposition-arthroplasty in noma defects of the lateral face associated with bony ankylosis. J Craniofac Surg. 2004;15:766–773. doi: 10.1097/00001665-200409000-00013. [DOI] [PubMed] [Google Scholar]