ABSTRACT
We report a case of accessory scrotum (AS) in the perineal region with peduncular lipoma, diagnosed prenatally. A male fetus of 31 weeks’ gestation was referred to our department with a perineal mass. Prenatal ultrasonography and magnetic resonance imaging showed a mass of 1.0 × 1.2 cm located posterior to the scrotum. No other abnormalities were noted during pregnancy. The patient was delivered vaginally at 38 weeks of gestation. On physical examination, a soft peduncular mass with a rugged and pigmented swelling was located between the normally developed scrotum and the anus. There were no specific symptoms or any other associated congenital anomalies. We completely excised the mass at one month of age. A histological examination revealed lipoma, with tissue suggestive of scrotum, so a definite diagnosis of AS was made. AS is a rare congenital anomaly of the scrotum. We review the literature.
Key Words: congenital scrotal anomaly, accessory scrotum, perineal lipoma, neonate, prenatal diagnosis
INTRODUCTION
Congenital scrotal anomalies are unusual and include penoscrotal transposition, bifid scrotum, ectopic scrotum, and accessory scrotum (AS). Among these, AS is the least frequent, with only 42 cases reported in the English literature.1-40) AS is characterized by additional scrotal tissue lacking a testis, besides a normally developed scrotum. Various associated anomalies have been reported. In particular, contiguous subcutaneous tumor is the most frequently associated abnormality and is reported to be related to the etiology of AS.
Although prenatal screening techniques have advanced, most reported cases of congenital perineal mass have been identified after birth. We report a rare case of AS with peduncular lipoma diagnosed prenatally.
CASE REPORT
A 28-year-old woman was referred to our hospital for the evaluation of a fetal perineal mass at a gestational age of 31 weeks. Prenatal ultrasonography and magnetic resonance imaging (MRI) showed a mass of 1.0 × 1.2 cm located posterior to the scrotum in a male fetus. (Fig. 1) The likely diagnosis was lipoma and the mass maintained a stable appearance until delivery. No other abnormalities were noted during the whole gestation. The male newborn was delivered vaginally at 38 weeks of gestation and his body weight was 2208 g. There were no specific symptoms after birth.
Fig. 1.
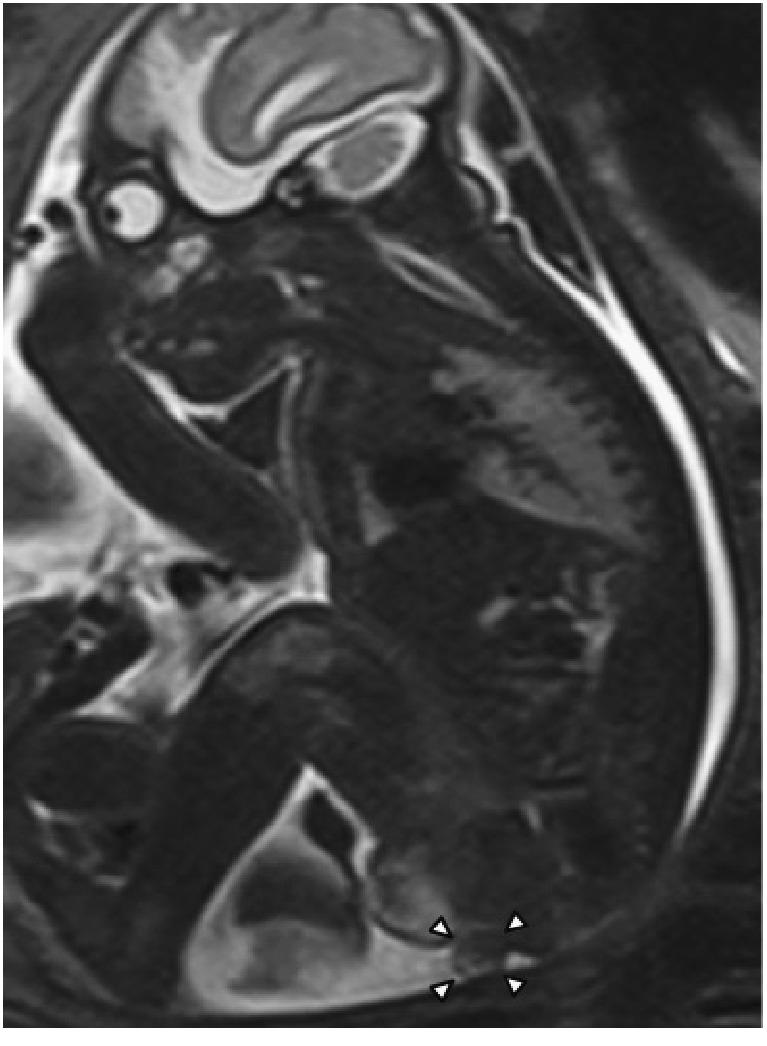
MRI at 31 weeks of gestation.
Arrowheads indicate a 1.0 × 1.2 cm mass located posterior to the scrotum.
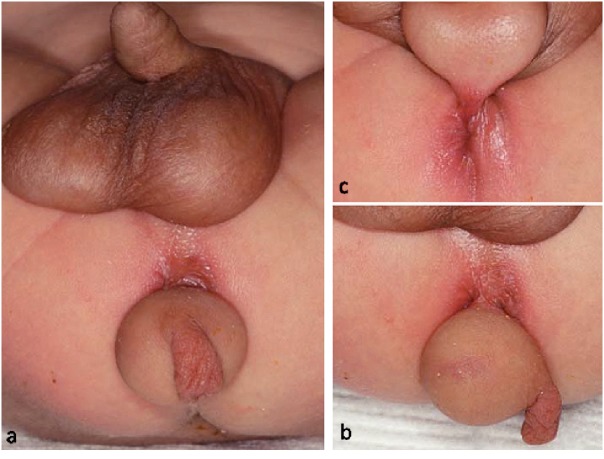
On physical examination, the soft peduncular mass, measuring 2.0 cm in diameter, was attached to a midperineal skin tag. There was also a rugged pigmented swelling on the mass, measuring 0.7 cm in diameter, which resembled the scrotum. (Fig. 2) The normal testes could be palpated in both the developed scrotal sacs. There were no additional abnormalities of the external genitalia. On MRI, the perineal mass showed high signal intensity on T1- and T2- weighted images and the signal intensity was suppressed on fat-suppressed T1-weighted images. MRI revealed no associated abnormalities of the intraabdominal organs, musculoskeletal system, or genitourinary system.
Fig. 2.
a. A soft peduncular mass with a rugged and pigmented swelling is located posterior to the normally developed scrotum.
b. Lateral view.
c. The mass is attached at the midperineum with a skin tag.
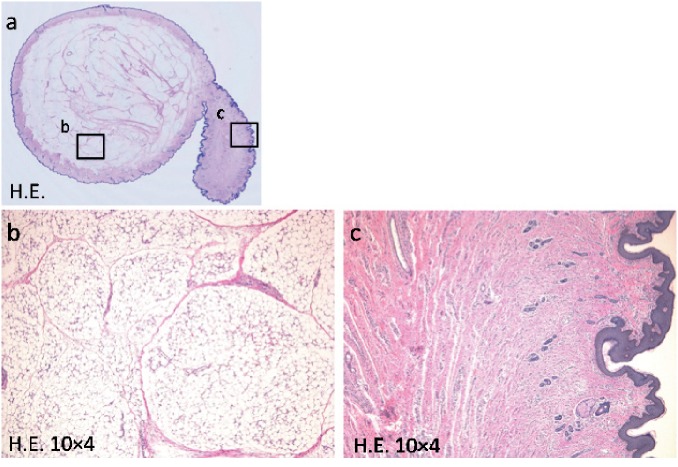
The preoperative diagnosis was AS with perineal lipoma, and we completely excised the mass under general anesthesia at one month of age. The postoperative course was uneventful, and the patient was discharged on the day after the operation. There was no recurrence or functional sequelae within a follow-up period of six months. A histological examination revealed that the peduncular mass consisted of mature adipose tissue. In this case, it was difficult to distinguish between lipoma and normal adipose tissue pathologically. However, our clinical diagnosis was lipoma because the peduncular mass was separated from normal perineal region by the skin tag. The rugged swelling on the peduncular mass showed smooth muscle fibers in the subcutaneous layer, which represented the tunica dartos. (Fig. 3) The swelling was definitively diagnosed as AS.
Fig. 3.
Histological examination.
a. Macroscopic image
b. The peduncular mass consists of mature adipose tissue.
c. Smooth muscle fibers in the subcutaneous layer of the rugged swelling represent the tunica dartos.
DISCUSSION
The scrotum is formed by the fusion of the labioscrotal swellings. These swellings appear at four weeks of gestation and migrate to the caudal portion after 12 weeks of gestation. Abnormal migration or early division of the labioscrotal swellings is possibly related to the etiology of congenital scrotal anomalies.9) The least frequent congenital scrotal anomaly is AS,25) characterized by additional scrotal tissue without a testis, besides a normally developed scrotum. Forty-three cases have been reported, including ours.1-40) (Table)
Table.
Characteristics of accessory scrotum
| n = 43 (1949–2014) | ||
|---|---|---|
| Sex (male) | 100% (43/43) | |
| Age at operation | median (range) | 9 months (4 days–46 years) |
| Prenatal diagnosis | 7.0% (3/34) | |
| Associated anomalies | ||
| Contiguous subcutaneous tumor | 72.5% (29/40) | |
| Hamartoma | 10.3% (3/29) | |
| Lipoblastoma | 3.4% (1/29) | |
| Anorectal malformation | 18.6% (8/43) | |
| Other scrotal anomalies | 16.3% (7/43) | |
| Hypospadias | 9.3% (4/43) | |
| Pseudodiphallia | 4.7% (2/43) | |
| Skeletal abnormalities | 4.7% (2/43) | |
| Renal dysplasia | 4.7% (2/43) | |
| Spina bifida | 4.7% (2/43) | |
| Retrocerebellar arachnoid cyst | 2.3% (1/43) | |
| Vertebral abnormality | 2.3% (1/43) | |
Various anomalies associated with AS have been reported. In particular, contiguous subcutaneous tumor has a high incidence (72.5%) of association with AS. Histologically, one case of subcutaneous tumor was lipoblastoma,13) three cases were hamartoma,1, 12, 21) and the others were consistent with lipoma. (Table) It is assumed that the contiguous subcutaneous tumor is related to the etiology of AS. Sule hypothesized that AS develops when intervening mesenchymal tissue (i.e., the developing subcutaneous tumor) disrupts the continuity of the developing caudal labioscrotal swelling.26) However, the complete etiology of AS is not explained by this hypothesis because AS can occur with no contiguous tumor. Takayasu hypothesized that AS develops from the early division and teratoid growth of pluripotential labioscrotal tissue elements.39) Most ASs including ours were located in the perineal region. However, two cases associated with skeletal abnormalities were located in the pubic area,5, 10) and one case was located on the distal penile shaft.23)
Only three cases, including ours, have been detected prenatally. Our case was detected at a gestational age of 31 weeks, and the other two reported cases were detected at 24 weeks11) and 32 weeks8) of gestation. A congenital perineal mass is unusual in itself, and most reported cases have been diagnosed after birth.41, 42) However, detection is possible with careful prenatal screening. The differential diagnosis of a fetal perineal mass includes lipoma, lipoblastoma, infantile hemangioma, hamartoma, and choristoma.41) If a fetal perineal mass is detected during the antenatal period, it is important to look for any associated congenital anomalies.42)
The prognoses of surgically treated patients are good, and only one has died, from an associated anomaly before surgery.22) The reported ages at surgery range from four days to 46 years (median, nine months), and three adult cases are recorded in the literature. Our patient was operated upon in the neonatal period because the mass was considered to be excisable without complications and the associated subcutaneous tumor had a low probability of malignancy.13)
CONCLUSION
We experienced a rare case of AS with peduncular lipoma. Although a fetal perineal mass is difficult to diagnose, it can be detected with careful prenatal screening. Many ASs are associated with contiguous subcutaneous tumors, which are assumed to be related to the etiology of AS.
CONFLICT OF INTEREST
The authors declare that they have no conflicts of interest.
REFERENCES
- 1).Lee JI, Jung HG. Perineal accessory scrotum with a lipomatous hamartoma in an adult male. J Korean Surg Soc, 2013; 85: 305–308. [DOI] [PMC free article] [PubMed]
- 2).Chatterjee S, Gajbhiye V, Nath S, Ghosh D, Chattopadhyay S, Das SK. Perineal accessory scrotum with congenital lipoma: a rare case report. Case Rep Pediatr, 2012; 757120. [DOI] [PMC free article] [PubMed]
- 3).Kumar PA, Arunachalam P, Kumar PN. Accessory scrotum in the perineum. J Indian Assoc Pediatr Surg, 2011; 16: 169–170. [DOI] [PMC free article] [PubMed]
- 4).Kavecan II, Jovanovic-Privrodski JD, Dobanovacki DS, Obrenovic MR. Accessory scrotum attached to a peduncular perineal lipoma. Pediatr Dermatol, 2012; 29: 522–524. [DOI] [PubMed]
- 5).Gucev Z, Castori M, Tasic V, Popjordanova N, Hasani A. A patient with unilateral tibial aplasia and accessory scrotum: a pure coincidence or nonfortuitous association? Case Rep Med, 2010; 2010: 898636. [DOI] [PMC free article] [PubMed]
- 6).Soccorso G, Ninan GK. A case of perineal lipoma with accessory scrotum and pseudo-diphallia. Eur J Pediatr Surg, 2009; 19: 55–56. [DOI] [PubMed]
- 7).Harada M, Udagawa A, Yoshimoto S, Ichinose M. A case of accessory scrotum with perineal lipoma. J Plast Reconstr Aesthet Surg, 2009; 62: 108–109. [DOI] [PubMed]
- 8).Lee RH, Goodwin TM, Miller D, Songster GS. Accessory scrotum: prenatal sonographic features. Ultrasound Obstet Gynecol, 2007; 30: 118–119. [DOI] [PubMed]
- 9).Park KH, Hong JH. Perineal lipoma in association with scrotal anomalies in children. BJU Int, 2006; 98: 409–412. [DOI] [PubMed]
- 10).Kendirci M, Horasanli K, Miroglu C. Accessory scrotum with multiple skeletal abnormalities. Int J Urol, 2006; 13: 648–650. [DOI] [PubMed]
- 11).Aboodi MM, Al-Jadeed HA. Accessory pseudophallus with accessory pseudoscrotum detected during antenatal sonographic scanning. J Ultrasound Med, 2005; 24: 1163–1166. [DOI] [PubMed]
- 12).Ramzisham AR, Thambidorai CR. Perineal hamartoma with accessory scrotum, anorectal anomaly, and hypospadias—a rare association with embryological significance: case report. Pediatr Surg Int, 2005; 21: 478–481. [DOI] [PubMed]
- 13).Ito M, Hashizume K, Kanamori Y. New phenotype of accessory scrotum with perineal lipoblastoma: coexistence of midperineal and lateral accessory scrotums. Int J Urol, 2004; 11: 125–127. [DOI] [PubMed]
- 14).Ratan SK, Rattan KN, Sehgal T, Ratan J. Perineal accessory scrotum. Indian J Pediatr, 2003; 70: 679–680. [DOI] [PubMed]
- 15).Göktas S, Aydur E, Yildirim I, Sümer F. Accessory scrotum attached to a perineal lipoma in an adult male. Int J Urol, 2003; 10: 501–503. [DOI] [PubMed]
- 16).Budhiraja S, Pandit SK. Accessory scrotum. Urol Int, 1999; 63: 210–211. [DOI] [PubMed]
- 17).Korkmaz A, Tekinalp G, Aygün C, Sahin S. Accessory scrotum: an unusual localization of scrotal skin. Pediatr Dermatol, 1999; 16: 142–143. [DOI] [PubMed]
- 18).Ozcan C, Celik A, Erdener A. Accessory perineal scrotum associated with anorectal malformation. BJU Int, 1999; 83: 729–730. [DOI] [PubMed]
- 19).Kawa G, Kawakita S, Ohara T, Matsuda T. Accessory scrotum with penoscrotal transposition and retrocerebellar arachnoid cyst: a case report. Int J Urol, 1997; 4: 327–328. [DOI] [PubMed]
- 20).Rattan KN, Pandit SK, Budhiraja S. Accessory scrotum with imperforate anus. Pediatr Surg Int, 1997; 12: 217. [PubMed]
- 21).Amann G, Berger A, Rokitansky A. Accessory scrotum or perineal collision-hamartoma. A case report to illustrate a misnomer. Pathol Res Pract, 1996; 192: 1039–1043. [DOI] [PubMed]
- 22).Shoshany G, Gottfied E, Bar-Maor JA. Accessory scrotum and anorectal malformation associated with "pseudo" prune belly in a neonate. J Perinatol, 1996; 16: 224–226. [PubMed]
- 23).Coplen DE, Mikkelsen D, Manley CB. Accessory scrotum located on the distal penile shaft. J Urol, 1995; 154: 1908. [PubMed]
- 24).Komuro Y, Takedai T. Accessory scrotum: a case report and review of the literature. Br J Plast Surg, 1994; 47: 579–580. [DOI] [PubMed]
- 25).Siddiky SA, Das DK, Islam AS. Accessory scrotum. Br J Urol, 1994; 74: 676–677. [DOI] [PubMed]
- 26).Sule JD, Skoog SJ, Tank ES. Perineal lipoma and the accessory labioscrotal fold: an etiological relationship. J Urol, 1994; 151: 475–477. [DOI] [PubMed]
- 27).Spears T, Franco I, Reda EF, Hernandez-Graulau J, Levitt SB. Accessory and ectopic scrotum with VATER association. Urology, 1992; 40: 343–345. [DOI] [PubMed]
- 28).Ferro F, Lais A, Korman R, Caterino S. Accessory perineal scrotum associated with anorectal malformation. A report of 2 cases. S Afr J Surg, 1991; 29: 32–34. [PubMed]
- 29).Shimotake T, Tokiwa K, Yanagihara J, Iwai N. Accessory scrotum with lipoma in an infant. Z Kinderchir, 1990; 45: 255–256. [DOI] [PubMed]
- 30).Balik E, Cetinkurşun S, Oztop F. Accessory scrotum: report of a case. Z Kinderchir, 1990; 45: 253–254. [DOI] [PubMed]
- 31).Rege VM, Deshmukh SS. Accessory perineal scrotum (a case report). J Postgrad Med, 1988; 34: 180–181. [PubMed]
- 32).Kolandaivelu G, Seeniraj K, Bose JC, Rajagopal P. Accessory scrotum. Br J Urol, 1987; 59: 363. [DOI] [PubMed]
- 33).Szylit JA, Grossman ME, Luyando Y, Olarte MR, Nagler H. Becker’s nevus and an accessory scrotum. A unique occurrence. J Am Acad Dermatol, 1986; 14: 905–907. [DOI] [PubMed]
- 34).Yokokawa K, Nakano E, Takaha M. Accessory scrotum: a case report. J Urol, 1986; 135: 593–594. [DOI] [PubMed]
- 35).Redman JF, Morris WD. Accessory perineal scrotum. Urology, 1983; 22: 406–407. [DOI] [PubMed]
- 36).Tripathi FM, Khanna S. Accessory scrotum: a case report. Br J Plast Surg, 1983; 36: 127–128. [DOI] [PubMed]
- 37).Azmy A, Ransley PG. Accessory scrotum. Z Kinderchir, 1981; 33: 373–374. [DOI] [PubMed]
- 38).Hata Y. Accessory scrotum. Plast Reconstr Surg, 1980; 66: 613–616. [DOI] [PubMed]
- 39).Takayasu H, Ueno A, Tsukada O. Accessory scrotum: a case report. J Urol, 1974; 112: 826–827. [DOI] [PubMed]
- 40).Daut WW, Daut RV. Accessory scrotum, posteriorly located; review of the literature and report of a case. J Iowa State Med Soc, 1949; 39: 194. [PubMed]
- 41).Wax JR, Pinette MG, Mallory B, Carpenter M, Winn S, Cartin A. Prenatal sonographic diagnosis of a perineal lipoma. J Ultrasound Med, 2010; 29: 1257–1259. [DOI] [PubMed]
- 42).Ahn KH, Boo YJ, Seol HJ, Park HT, Hong SC, Oh MJ, Kim T, Kim HJ, Kim YT, Kim SH, Lee KW. Prenatally detected congenital perineal mass using 3D ultrasound which was diagnosed as lipoblastoma combined with anorectal malformation: case report. J Korean Med Sci, 2010; 25: 1093–1096. [DOI] [PMC free article] [PubMed]