Abstract
Introduction
Neurosurgery remains among the highest malpractice risk specialties. This study aimed to identify areas in neurosurgery associated with litigation, attendant causes and costs.
Methods
Retrospective analysis was conducted of 42 closed litigation cases treated by neurosurgeons at one hospital between March 2004 and March 2013. Data included clinical event, timing and reason for claim, operative course and legal outcome.
Results
Twenty-nine claims were defended out of court and twelve were settled out of court. One case required court attendance and was defended. Of the 42 claims, 28, 13 and 1 related to spinal (0.3% of caseload), cranial (0.1% of caseload) and peripheral nerve (0.07% of caseload) surgery respectively. The most common causes of claims were faulty surgical technique (43%), delayed diagnosis/misdiagnosis (17%), lack of information (14%) and delayed treatment (12%), with a likelihood of success of 39%, 29%, 17% and 20% respectively. The highest median payouts were for claims against faulty surgical technique (£230,000) and delayed diagnosis/misdiagnosis (£212,650). The mean delay between clinical event and claim was 664 days.
Conclusions
Spinal surgery carries the highest litigation risk versus cranial and peripheral nerve surgery. Claims are most commonly against faulty surgical technique and delayed diagnosis/misdiagnosis, which have the highest success rates and payouts. In spinal surgery, the most common cause of claims is faulty surgical technique. In cranial surgery, the most common cause is lack of information. Claims may occur years after the clinical event, necessitating thorough contemporaneous documentation for adequate future defence. We emphasise thorough patient consultation and meticulous surgical technique to minimise litigation in neurosurgical practice.
Keywords: Litigation, Closed claims, Legal outcome, Neurosurgery, Payout
Neurosurgery remains among the highest malpractice risk specialties in medicine1 owing to the risk of morbidity and mortality from both operative intervention and the natural history of the clinical conditions treated. In the US, a continuing trend of ‘defensive medicine’ has been observed among neurosurgeons whereby clinically unnecessary diagnostic imaging and consultations may be conducted and high risk procedures may be avoided to satisfy a perceived legal risk.2 A similar trend may be seen in the UK3 against a background of a recent doubling of clinical negligence costs against National Health Service (NHS) hospitals.4
Good risk management is essential to limit litigation in neurosurgery and this mandates knowledge about the areas of highest risk. There have been studies on litigation in other specialties5,6 but these data are lacking in neurosurgery. Individual pathologies such as cauda equina syndrome have been analysed medicolegally7,8 but not the spectrum of conditions across neurosurgery as a whole. There are very few data on high risk areas of practice, causes of claims or costs. Such data in neurosurgery are important to maintain quality patient care, reduce litigation costs in increasingly cost conscious NHS hospitals and limit the individual surgeon’s risk at a time when insurance premiums for neurosurgeons are at their highest.2
This is the first analysis of medicolegal claims related to the breadth of UK neurosurgical practice over the last decade. The aim of the study was to identify areas of practice associated with the highest risk of litigation, attendant causes and costs.
Methods
With permission from the senior neurosurgeons and the legal department at St George’s Hospital, all consecutive cases of closed claims (ie claims with outcomes) in neurosurgery between 1 March 2004 and 1 March 2013 were identified from the institution’s risk management system (Datix, London, UK). Data were collected retrospectively on patient demographics, clinical event, timing and reason for claim (delayed diagnosis/misdiagnosis, delayed treatment, faulty surgical technique, lack of information, surgical infection, inadequate follow-up), subspecialty (cranial surgery, spinal surgery, peripheral nerve surgery), operative course and legal outcome (settled or defended, out-of-court or in-court, payout cost where settled).
Results
Over the period between March 2004 and March 2013, 42 closed litigation claims in neurosurgery were identified. The mean delay between clinical event and a claim was 664 days (range: 23–1,880 days). The distribution of claims by neurosurgical subspecialty is shown in Table 1.
Table 1.
Case volume and closed medicolegal claims by neurosurgical subspecialty
| Neurosurgical subspecialty | Case volume | Medicolegal claims |
|---|---|---|
| Cranial | 13,251 | 13 (0.1%) |
| Spinal | 9,411 | 28 (0.3%) |
| Peripheral nerve | 1,428 | 1 (0.07%) |
There was a higher proportion of claims in spinal surgery (0.3% of caseload) than in cranial (0.1% of caseload) or peripheral nerve surgery (0.07% of caseload). Twenty-three claims involved elective surgery (0.3% of elective caseload) and nineteen involved emergency surgery (0.2% of emergency caseload). The proportion of claims was similar across vascular, tumour, trauma and cerebrospinal fluid diversion subgroups.
The causes of claims were distributed differently for cranial, spinal and peripheral nerve surgery (Fig 1). The leading cause of claims against spinal procedures was faulty surgical technique (54% versus 23% for cranial and 0% for peripheral nerve procedures). In contrast, the leading cause of claims against cranial procedures was lack of information (31% versus 7% for spinal and 0% for peripheral nerve procedures). The one claim against peripheral nerve surgery was for inadequate follow-up.
Figure 1.
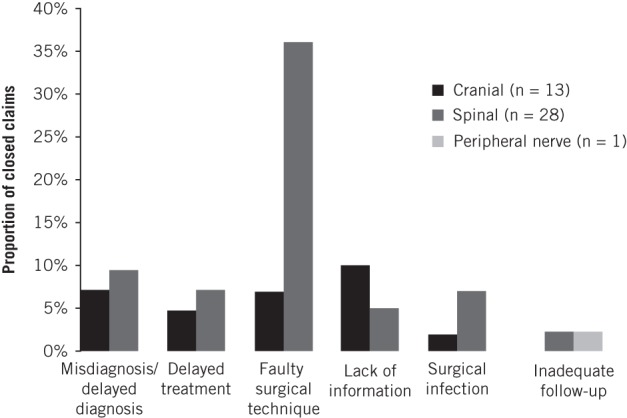
Distribution of closed claims by neurosurgical subspecialty and cause
The total payout to 12 successful claimants was £3 million, with a median payout of £203,158. Claims against faulty surgical technique received the highest median payout of £230,000 (Fig 2). The next highest payouts were against misdiagnosis/delayed diagnosis (£212,650) and delayed treatment (£198,000). The lowest median payouts were against lack of information (£77,000) and surgical infection (£35,000). The likelihood of successful claims was highest against faulty surgical technique (39%), misdiagnosis/delayed diagnosis (29%) and surgical infection (26%), and it was lowest against delayed treatment (20%), lack of information (17%) and inadequate follow-up (0%) (Fig 2).
Figure 2.
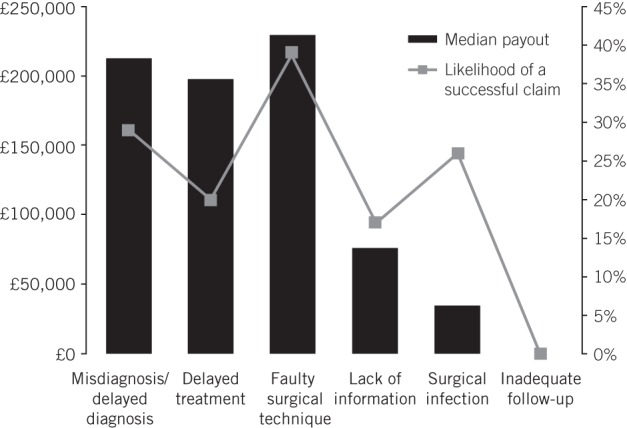
Median payout and likelihood of success for the causes of litigation
Of 13 claims against cranial surgery, 3 misdiagnoses or delayed diagnoses were noted: misdiagnosis of cerebellar abscess following foramen magnum decompression, delayed diagnosis of hydrocephalus and delayed diagnosis of viral encephalitis following decompressive craniectomy for presumed malignant left middle cerebral artery infarction. There were two claims against delayed treatment: one case of delay in commencement of dexamethasone for meningioma and one case of delay in performing foramen magnum decompression surgery in a symptomatic patient with Arnold–Chiari type I malformation. Faulty surgical technique was claimed in three cases: misplaced drain during evacuation of a subdural haematoma resulting in a non-reversible neurological deficit, misplaced distal catheter of a ventriculoperitoneal shunt resulting in obstructive hydrocephalus and reoperation, and incomplete resection of a meningioma. Surgical infection occurred in one case of subdural empyema following removal of an arachnoid cyst. Lack of information on treatment risks was identified in four cases: inadequately discussed risk of motor deficit (2), dysphasia (1) and side effect profile of dexamethasone (1).
Of 28 claims against spinal surgery, there were 4 cases of delayed diagnosis, which included 3 cases of cauda equina syndrome secondary to a herniated disc and one case of myelopathy secondary to postoperative epidural haematoma. Faulty surgical technique was detected in 15 cases: nerve root damage (5), lumbar discectomy at the wrong level (4), misplacement of a pedicle screw (4), tear of a common iliac vein during discectomy (1) and inadequate discectomy (1). There were three claims against delayed treatment: delayed admission of spinal cord injured patients from their local hospital (2) and delayed lumbar laminectomy despite progressive symptoms (1). Surgical infection was noted in three cases: following lumbar laminectomy (1) and laminectomy with pedicle screw fixation (2). Lack of information about the risk of worsening neurology after lumbar discectomy was found in two cases. There was also one claim against inadequate follow-up of a patient with persistent radiculopathy following lumbar laminectomy.
There was only one claim against peripheral nerve surgery. This was for inadequate follow-up of a patient with recurrent symptoms following carpal tunnel decompression.
Discussion
While there have been a number of medicolegal studies in neurosurgery conducted in European countries and North America,9–12 there have been none to date reflecting UK practice. Our analysis is the first to review cases of litigation across the breadth of UK neurosurgery. It is important to note that our data relate to claims both defended as well as successful and therefore reflect the extent of neurosurgeons’ involvement in giving evidence in litigation cases rather than solely demonstrating proven negligence.
Overall, the most common cause of claims was faulty surgical technique (43%), which was defined as an avoidable surgical error that did not meet the expected standard of care. Detailed data were collected on the reasons for successful claims, based on review of legal and medical notes. There were seven successful claims identified against faulty surgical technique and in all cases, poor surgical technique alone was implicated. There was no evidence in these cases of lack of informed consent regarding risks of surgery. Claims against failure to provide information regarding the risks of treatment (operative or non-operative) in patients who subsequently developed complications were categorised accordingly under ‘lack of information’.
Claims against cranial surgery
We have shown that cranial surgery carries a litigation risk of approximately 1 in 1,000 cases, of which the leading cause was lack of information (10%) followed by delayed diagnosis/misdiagnosis (7%) and faulty surgical technique (7%). Three of the four claims of lack of information related to failure to discuss operative risks including motor deficit and dysphasia, high impact factors on quality of life. Recent studies show the importance of thorough patient consultation not only preoperatively with informed consent, to guide surgical decision making and reduce patient anxiety, but especially postoperatively, to enable patients to participate effectively in their own recovery.13,14 In all settings, thorough consultation with patients and their families is critical in neurosurgery to achieve good patient care and to mitigate claims related to what are potentially high morbidity and mortality procedures.
One claim against lack of information regarding side effects of dexamethasone treatment was identified. An alert and orientated inpatient with meningioma was started on oral 8mg dexamethasone twice a day and, subsequently, over the period of a week developed significant weight gain, hypertriglyceridaemia and impaired glucose metabolism. These effects are all established risks of corticosteroid treatment but they had not been discussed with the patient prior to starting treatment. Discussion with the patient about drug risks and benefits may be lacking in the setting of prescription decisions made during time pressed ward rounds by hasty junior doctors at busy neurosurgical centres and, given the rarity of severe side effects, the importance of consulting with the patient before starting therapy is not always appreciated. This claim was successful and serves to highlight to neurosurgeons at all levels of training that good patient consultation encompasses discussion of non-operative as well as operative management.
There were two successful claims against faulty surgical technique in cranial surgery: misplaced drain in brain cortex during evacuation of a subdural haematoma, resulting in a non-reversible neurological deficit, and incomplete meningioma removal. In the latter case, immediate postoperative imaging demonstrated more than 60% of residual tumour and the patient’s preoperative neurological deficit had not resolved. ‘Redo’ craniotomy and resection of the residual meningioma was undertaken, which led to a protracted hospital stay complicated by wound infection and hospital acquired pneumonia. It was conceded by the attending neurosurgeon that intraoperative imaging had not been utilised, and that this represented inappropriate practice, falling short of the expected standard of care, and resulted directly in a misplaced craniotomy flap that was inadequate for good tumour access and resection. The settlement for this claim was £350,000.
Claims against spinal surgery
We have shown that spinal surgery carries the highest risk of litigation (approximately 1 in 300 cases), of which the leading cause by far is faulty surgical technique, with the highest likelihood of success and financial payout. This was followed by delayed diagnosis/misdiagnosis and surgical infection. These findings are consistent with the few medicolegal studies published on spinal procedures.9,10
Of spinal claims against faulty surgical technique, lack of consultant supervision was implicated in 6/15 cases (40%), which included 3/5 cases of nerve root damage. This highlights the importance of intraoperative expertise as opposed to simply competence in reducing surgical error. Two-thirds of these claims occurred in the last five years. Structural changes to service and neurosurgical training in the NHS, in part due to the European Working Time Regulations, may have resulted in competent but less experienced registrars performing cases versus their predecessors a decade ago.15 Over a quarter of cases of faulty surgical technique were due to wrong site surgery, emphasising the importance of intraoperative imaging after exposure and marking of a fixed anatomic structure.16 Minimising medicolegal risk in spinal surgery must evidently focus on reducing faulty surgical technique, given its high incidence, high likelihood of success and potential costs.
Of five successful claims against faulty surgical technique in spinal surgery, four were due to wrong level surgery secondary to inadequate use of intraoperative x-ray guidance to check the vertebral level. The standard of care in spinal surgery includes operating at the correct site of the lesion using imaging guidance. Surgical technique did not meet this standard in the four cases of wrong level spinal surgery and resulted directly in postoperative neurological deficits in these patients.
One of the successful claims against faulty surgical technique due to wrong level surgery was made four years following the procedure. In this case, the verdict highlighted the deficient recording of the patient’s preoperative neurological deficits in the medical notes, which meant that the neurosurgeon could not construct an adequate defence when explaining postoperative outcomes. Given the time delay between surgery and the claim, we emphasise the importance of thorough contemporaneous documentation in reducing the risk of future litigation.
There was one successful claim against faulty surgical technique due to complete severance of the right L5 nerve root during an L4/5 microdiscectomy for cauda equina syndrome. This resulted directly in a complete irreversible right foot drop, which impacted the patient’s mobility and quality of life. A combination of three factors led to successful litigation in this case.
First, the procedure was performed by an unsupervised junior registrar out of hours when the standard of care would have been that the responsible consultant either perform or supervise the procedure. Second, the surgeon had inappropriately used a craniotome to perform the laminectomy prior to disc removal. He had had no prior experience using this surgical tool in spinal surgery and did not therefore recognise his own limitations. Complete wrapping and severing of the right L5 nerve root around the rotating drill component of the craniotome occurred as a result. The standard of care for a junior surgeon with limited experience would have been to use a Kerrison upward cutting rongeur, with which he did have experience but which he did not use. Third, at the time of iatrogenic injury, no senior help was requested by the junior surgeon, indicating that no serious attempt was made to remedy the gross surgical error. This case serves to highlight that neurosurgical trainees must recognise their limitations and utilise an adequate support structure in case of technical difficulty.
Delayed or wrong diagnosis was the second most common claim against spinal procedures. The neurosurgical centre ultimately treating the patient (which has access to and expertise in sophisticated neuroimaging techniques as well as neurological observation) was not always implicated but rather the referring local hospital to which the patient first presented. In the context of clinical emergencies, delay in diagnosis or referral from the local hospital presents a high risk to patient safety and can be associated with costly litigation.
One case in our study illustrates this point. A 54-year-old patient presented to a local hospital with a 5-week history of lower back pain and bilateral leg weakness, which had worsened over the previous 48 hours to the point where she was no longer able to walk. She did not have any urinary symptoms. Although the emergency department physician considered a diagnosis of cauda equina syndrome, magnetic resonance imaging (MRI) to confirm the diagnosis was only requested on an urgent rather than emergent basis, resulting in a 24-hour delay in performing the scan. Following the imaging, there was a further 24-hour delay in radiological review and referral to the neurosurgical centre for surgery. During the combined 48 hours of delay, the patient developed established urinary retention and worsened leg weakness. Following decompression surgery for a large central L3/4 disc prolapse at the neurosurgical centre, she had a limited recovery in bladder function and has been receiving complex treatment to improve this for the last two years.
The payout relating to this case was £1,525,000 against the local hospital. This was the largest single payout in our study. In clinical emergencies with a level of diagnostic uncertainty (eg cauda equina syndrome), immediate MRI to confirm the diagnosis and early consultation with a neurosurgical centre are crucial to ensure timely referral for surgical intervention, and therefore also to ensure quality care and reduced risk of litigation.
The rate of claims against surgical infection was 7% in spinal surgery compared with 2% in cranial surgery. This difference may in part be owing to patient related factors or changing institutional factors with time (eg infection control protocols or different perioperative antibiotic use). Another hypothesis is that there is a higher risk of cerebrospinal fluid leak from spinal as compared with cranial procedures, especially when performed by unsupervised neurosurgical registrars.
Claims against peripheral nerve surgery
There was one claim against peripheral nerve surgery (0.07% of caseload, approximately 1 in 1,500 cases) due to inadequate follow-up after carpal tunnel decompression. The lower incidence of claims in this subspecialty compared with cranial and spinal surgery may reflect the relatively lower complexity of operative management involved and the lower attendant morbidity. As a result, patients are less likely to suffer adverse outcomes and pursue legal action.
Study limitations
This study was based solely on those claims recorded in our hospital’s risk management system. No data were obtained directly from other major sources such as the NHS Litigation Authority or medical defence organisations. Using such sources may have increased the sample size.
Conclusions
In UK neurosurgical practice, spinal surgery carries the highest litigation risk versus cranial and peripheral nerve surgery. Overall, the most common causes of claims are faulty surgical technique and delayed diagnosis/misdiagnosis, which have the highest likelihood of success and cost of payout, and together represent 60% of claims. In spinal surgery, the most common cause of claims is faulty surgical technique, whereas within cranial surgery the most common cause is lack of information. Claims may occur years after the clinical event, which suggests that thorough contemporaneous documentation will be vital to a future defence. We emphasise thorough patient consultation and meticulous surgical technique to minimise litigation in daily neurosurgical practice.
Acknowledgements
The authors would like to thank Shanti Kelly of St George’s Hospital legal department for kindly extracting all closed claims in neurosurgery from the hospital’s Datix risk management system.
The material in this paper was presented at the autumn meeting of the Society of British Neurological Surgeons held in Colchester, September 2013.
The authors would like to thank Afra Rafique of St George’s Hospital for her role in early data collection and as a recognised author of the poster presentation titled ‘Why do neurosurgeons get sued? A 9-year review of medicolegal claims in neurosurgery’ delivered at the Society of British Neurosurgeons Autumn Meeting, Colchester, UK held on 25th September 2013.
References
- 1.Jena AB, Seabury S, Lakdawalla D, Chandra A. Malpractice risk according to physician specialty. N Engl J Med 2011; 365: 629–636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nahed BV, Babu MA, Smith TR, Heary RF. Malpractice liability and defensive medicine: a national survey of neurosurgeons. PLoS One 2012; 7: e39237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Palmer R. Medical negligence – causes, trends and lessons. Health Care Risk Report 1998. (October) 1–2. [Google Scholar]
- 4.NHS Litigation Authority. Factsheet 2: Financial Information London: NHSLA; 2013. [Google Scholar]
- 5.Campbell WB, France F, Goodwin HM. Medicolegal claims in vascular surgery. Ann R Coll Surg Engl 2002; 84: 181–184. [PMC free article] [PubMed] [Google Scholar]
- 6.Goodwin H. Litigation and surgical practice in the UK. Br J Surg 2000; 87: 977–979. [DOI] [PubMed] [Google Scholar]
- 7.Daniels EW, Gordon Z, French K et al. Review of medicolegal cases for cauda equina syndrome: what factors lead to an adverse outcome for the provider? Orthopedics 2012; 35: e414–e419. [DOI] [PubMed] [Google Scholar]
- 8.Todd NV. Causes and outcomes of cauda equina syndrome in medico-legal practice: a single neurosurgical experience of 40 consecutive cases. Br J Neurosurg 2011; 25: 503–508. [DOI] [PubMed] [Google Scholar]
- 9.Emery E, Balossier A, Mertens P. Is the medicolegal issue avoidable in neurosurgery? A retrospective survey of a series of 115 medicolegal cases from public hospitals. World Neurosurg 2013. January 10 [Epub ahead of print.] [DOI] [PubMed] [Google Scholar]
- 10.Epstein NE. A review of medicolegal malpractice suits involving cervical spine: what can we learn or change? J Spinal Disord Tech 2011; 24: 15–19. [DOI] [PubMed] [Google Scholar]
- 11.Sughrue ME, Rutkowski MJ, Shangari G et al. Risk factors for the development of serious medical complications after resection of meningiomas. J Neurosurg 2011; 114: 697–704. [DOI] [PubMed] [Google Scholar]
- 12.Santiago-Sáez A, Perea-Pérez B, Labajo-González E et al. Analysis of judicial sentences against neurosurgeons resolved in second court of justice in Spain in the period from 1995 to 2007. Neurocirugia 2010; 21: 53–60. [PubMed] [Google Scholar]
- 13.Rozmovits L, Khu KJ, Osman S et al. Information gaps for patients requiring craniotomy for benign brain lesion: a qualitative study. J Neurooncol 2010; 96: 241–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Díaz JL, Barreto P, Gallego JM et al. Proper information during the surgical decision-making process lowers the anxiety of patients with high-grade gliomas. Acta Neurochir 2009; 151: 357–362. [DOI] [PubMed] [Google Scholar]
- 15.Canter R. Impact of reduced working time on surgical training in the United Kingdom and Ireland. Surgeon 2011; 9: S6–S7. [DOI] [PubMed] [Google Scholar]
- 16.Devine J, Chutkan N, Norvell DC, Dettori JR. Avoiding wrong site surgery: a systematic review. Spine 2010; 35: S28–S36. [DOI] [PubMed] [Google Scholar]


