Abstract
Microwave assisted liver resection is a useful technique, especially when haemostasis could be difficult to achieve with conventional methods. However, prolonged administration of microwaves can be responsible for intraoperative haemoglobinuria. We describe the first case of acute haemolysis secondary to microwave assisted liver resection.
Keywords: Microwaves, Complications, Liver
Case history
Radiofrequency assisted liver resection is nowadays a widely used technique both in open and laparoscopic surgery. 1 Conversely, microwave assisted liver resection has been seldom reported. 2–4
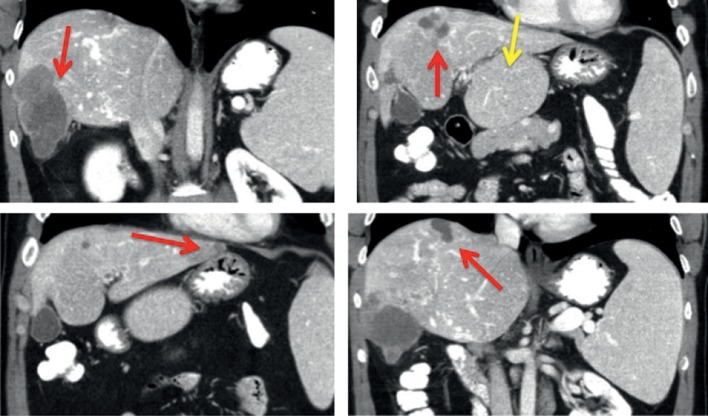
We describe a case of a 41-year-old patient who presented with sigmoid cancer and bilobar large liver metastases. He was treated initially with chemotherapy (FOLFOX + bevacizumab, 28 courses) but he developed complete portal vein thrombosis at the hilum. He also developed portal hypertension with superior mesenteric vein thrombosis, a low platelet count and hypersplenism, with a huge hypertrophy of segment I. His post-treatment computed tomography (CT) showed a significant reduction in size of the liver metastasis (Fig 1) with complete radiological and endoscopic response of the rectal tumour.
Figure 1.
Preoperative computed tomography showing bilobar colorectal liver metastasis (red arrows) with portal vein thrombosis and huge hypertrophy of caudate lobe (yellow arrow)
However, the intrahepatic vascular shunts and the presence of portal hypertension were considered a contraindication for an extended hepatectomy and also risk factors for intraoperative bleeding. We therefore decided to resect the largest right lobe liver lesion and the small superficial left lobe lesion using a microwave assisted technique (Fig 2), and to ablate the other lesions in order to obtain an R0 resection.
Figure 2.
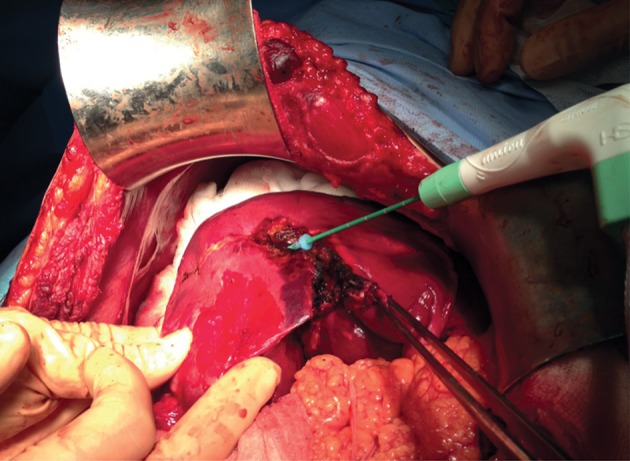
Intraoperative photograph of microwave assisted liver resection. The microwave needle is introduced in the liver parenchyma under echographic guidance.
The AMICA™ microwave tissue ablation system (HS Hospital Service, Rome, Italy) consists of a 2.45GHz generator, with power output settings ranging from 20W to 80W, and a percutaneous 14G cooled antenna with ‘mini-choke’ technology.
The microwave needle was first introduced in the liver parenchyma under echographic guidance at a distance of 2cm from the resectable liver metastasis so as to obtain clear margins. Following the ablation, the liver was transected progressively with a knife within the ablated margin. We performed eight ablations (3 minutes, 80W each, estimated ablation area 4cm × 3cm each) to resect the large liver metastasis and three additional ablations for the remaining two lesions (5 minutes, 80W, estimated area 5cm × 3.5cm each).
During the operation, at completion of the liver resection and after the ablation of the last liver metastasis, the patient’s urine suddenly turned dark (Fig 3) and his blood haemoglobin concentration dropped from 13g/dl to 6g/dl in the absence of any intraoperative blood loss. His body temperature also increased to 38.5°. Intraoperative urine analysis confirmed haemoglobinuria and a diagnosis of acute intravascular haemolysis was made. The serum bilirubin level peaked at 14g/dl during the following 24 hours and returned to normal after 48 hours, and the patient received two units of red blood cells. CT performed on postoperative day 7 showed no residual liver disease (Fig 4). He was discharged on day 10 with no other complications.
Figure 3.

Intraoperative photograph of urine bag showing haemoglobinuria
Figure 4.
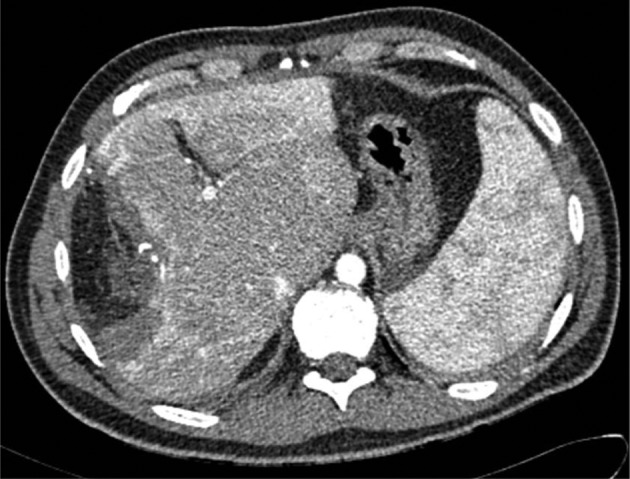
Computed tomography on postoperative day 7 showing no residual disease
Discussion
Few cases of acute intraoperative haemolysis have been reported as a complication of radiofrequency liver ablation. 5 This is the first reported case of acute intravascular haemolysis following microwave ablation. When compared with radiofrequency, microwave ablation has the advantage of avoiding the heat sink effect, which can compromise the oncological efficacy of liver ablation, especially in cases of portal hypertension. However, this report shows that when used for repeated ablations, microwaves can cause severe haemoglobinuria and renal function must be monitored carefully.
References
- 1. Pai M, Frampton AE, Mikhail S et al. Radiofrequency assisted liver resection: analysis of 604 consecutive cases. Eur J Surg Oncol 2012; 38: 274–280. [DOI] [PubMed] [Google Scholar]
- 2. Percivale A, Griseri G, Gastaldo A et al. Microwave assisted liver resection: clinical feasibility study and preliminary results. Minerva Chir 2012; 67: 415–420. [PubMed] [Google Scholar]
- 3. Satoi S, Kamiyama Y, Matsui Y et al. Clinical outcome of 214 liver resections using microwave tissue coagulation. Hepatogastroenterology 2005; 52: 1,180–1,185. [PubMed] [Google Scholar]
- 4. Simo KA, Sereika SE, Newton KN, Gerber DA. Laparoscopic-assisted microwave ablation for hepatocellular carcinoma: safety and efficacy in comparison with radiofrequency ablation. J Surg Oncol 2011; 104: 822–829. [DOI] [PubMed] [Google Scholar]
- 5. Li H, Li B, Wei Y, Liu F. Hemolysis as a complication of radiofrequency ablation for hepatocellular carcinoma must be paid more attention. Dig Dis Sci 2011; 56: 3,391–3,392. [DOI] [PubMed] [Google Scholar]