Abstract
Background:
Respiratory dysfunction often persists in post intensive care unit (ICU) patients and intermediate care facilities have been established to ensure the continuous of appropriate care.
Methods:
The data of patients with difficult weaning from mechanical ventilation admitted to a respiratory intermediate unit (RIU) attached to a pulmonary department of a General Hospital, were retrospectively analyzed. Clinical characteristics, weaning from mechanical ventilation and tracheostomy, ICU readmission and RIU mortality were examined over a period of 18 years (1993- 2010) that was randomly divided into three six-year-periods.
Results:
A total of 548 patients (age 56.7±17.9 years) [mean ± standard deviation (SD)], of whom 80% with tracheostomy in place and 37.6% with pressure ulcers, were examined. The ICU stay was 30.1±24.7 days (mean ± SD) and increased over time (p<0.05). Patients’ baseline disorders were: chronic respiratory disease (41.3%), chronic cardiovascular diseases (10.6%), neuromuscular disease (22.8%) and miscellaneous (25.3%). The length of RIU stay (22.8±19.5 days) was constant over the examined periods but an increase in age and maintenance of tracheostomy were observed; 80% of patients were liberated from mechanical ventilation and 58.5% from tracheostomy, whereas the RIU mortality was 15%.
Conclusion:
In their vast majority patients with chronic respiratory failure, who were admitted to RIU,were weaned from mechanical ventilation, although in a substantial percentage the maintenance of tracheostomy was mandatory after discharge. Hippokratia 2015, 19 (1): 37-40.
Keywords: Respiratory intermediate unit, mechanical ventilation, tracheostomy, RICU, chronic respiratory failure
Introduction
Respiratory failure persists in many patients after their intensive care unit (ICU) hospitalization, while recovering from critical illness, especially if there is a background of chronic respiratory dysfunction. In these patients often tracheostomy remains in place and about 5% of them require prolonged ventilator support1.These factors determine patient’s destination after ICU discharge in order to secure the care they need2.
Existence of the appropriate place to transfer these patients depends on each country’s health system organization and financial support. In the USA and certain European countries, special units, named step down units, intermediate or respiratory intermediate units, have been set up much earlier and official data exist about their functional profile3. In a recent survey about ICU beds in Europe, intermediate care beds are reported in Greece4 but to the best of our knowledge there is no information about the activity of such units and the patients’ destination after ICU discharge.
Aim of this study was to describe the characteristics and outcome of patients with difficulty in weaning from mechanical ventilation after ICU discharge, who were admitted to a Respiratory Intermediate Unit attached to a Pulmonary Department.
Setting
A 6-bed respiratory intermediate unit (RIU), located within the pulmonary department in a district general hospital, was assigned to provide care in post ICU patients with persistent respiratory dysfunction who failed to wean from mechanical ventilation or tracheostomy. The patients were transferred from the ICU of our hospital and from four ICUs of other hospitals mainly in the same district.
The personnel working in the unit consists of a pulmonologist and a trainee in pulmonary medicine, a physiotherapist and two trained nurses during the morning shift, while during the afternoon and evening shifts, the unit is run by the doctors and nurses on call in the pulmonary ward.
Patients and Methods
A retrospective observational study from 1993 to 2010 was performed, regarding data of patients transferred to the RIU. A random division into three six-year-periods was performed in order to study the course of this unit, over time. Admission criteria included difficulty in weaning from mechanical ventilation, consciousness (GSC ≥ 8), stable hemodynamic condition and absence of fever or other signs of acute infectious disease.
Upon admission, a detailed evaluation of the patient’s general condition was performed. Invasive or non invasive mechanical ventilation support was started in a pressure support (PS) mode and oxygen supply was administered according to patient’s needs. A plan of respiratory and physical therapy was scheduled and implemented to all patients. Oral feeding was started after bedside evaluation of swallowing. Weaning from mechanical ventilation was initiated after achievement of clinical stability and included trials on spontaneous breathing and gradually reduced time of mechanical ventilation support, in order to test patient’s ventilator independence. Before decannulation, patient’s ability to tolerate tracheostomy tube capping for 24 hours, was estimated. Cough effectiveness and the ability to speak, were also evaluated. An overnight sleep study with cardiorespiratory parameters recording or an overnight oximetry was performed before tracheostomy tube was finally removed.
Data collected were: age, sex, the underlying disease leading to ICU admission, and the ICU and RIU length of stay. As markers of patient’s severity, we used the presence of tracheostomy and pressure ulcers upon admission to RIU5.
Patients were divided in 4 categories according to their underlying disease: i) chronic pulmonary disease [chronic obstructive pulmonary disease (COPD)], restrictive disease (obesity hypoventilation, kyphoscoliosis, post Tuberculosis sequelae, etc), ii) neuromuscular disease [Duchene muscular dystrophy (DMD), other myopathies and motor neuron diseases], iii) chronic cardiovascular disease, and iv) miscellaneous (surgical patients, major cardiovascular surgery, trauma, and other medical conditions). Clinical outcomes recorded were: i) weaning from mechanical ventilation, defined as the ability to breathe spontaneously upon discharge at least during the day, ii) weaning from the tracheostomy, iii) readmission to ICU, and iv) RIU mortality.
We also estimated the changes in the staff availability during the period studied. The three periods of 6 consecutive years, (1993-98, 1999-2004 and 2005-2010), were studied.
Statistics
Data are presented as mean ± standard deviation (SD), among the three consecutive 6-year periods of time, comparisons were done using Student’s t test and one-way analysis of variance (ANOVA) for quantitative variables and chi-square test for qualitative variables. A p value of <0.05 was considered to be statistically significant.
Results
A total of 548 patients (67% men, mean age 56.7±17.9 years) were included in the study. Upon admission, 80% were already tracheostomized and 37.6% had pressure ulcers (at least grade II). The underlying cause leading to ICU hospitalization was chronic respiratory disease in 41.3% of patients, chronic cardiovascular disease in 10.6%, neuromuscular disease in 22.8% and miscellaneous in 25.3% of patients.
Patients’ characteristics upon admission are presented in Table 1. The mean age and the mean previous ICU stay increased over time (p<0.001 and p<0.05 respectively). The proportion of patients with chronic respiratory and cardiovascular diseases remained constant over time, but the proportion of patients with neuromuscular diseases increased (p<0.01). Significantly more patients were tracheostomized over time and the presence of pressure ulcers increased as well (p<0.01) (Table 1).
Table 1. Patients’ characteristics, upon admission to the respiratory intermediate unit (RIU), for the 548 patients admitted during a period of 18 years (1993 - 2010).
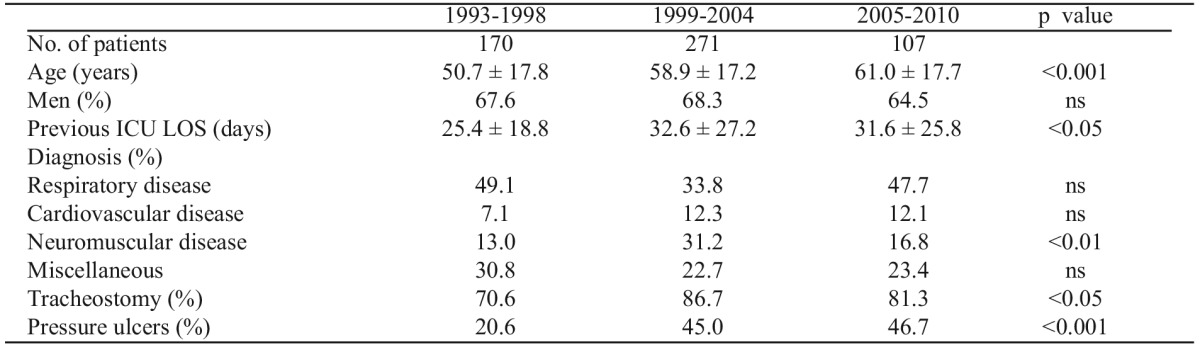
ICU: intensive care unit, LOS: Length of staying, ns: non significant
The clinical outcomes are shown in Table 2. The mean duration of RΙU stay was constant over time. Τhe ICU readmission was 5.8%, without statistical difference among the periods under study.
Table 2. Clinical outcomes in RIU for the 548 patients admitted during a period of 18 years (1993 - 2010).
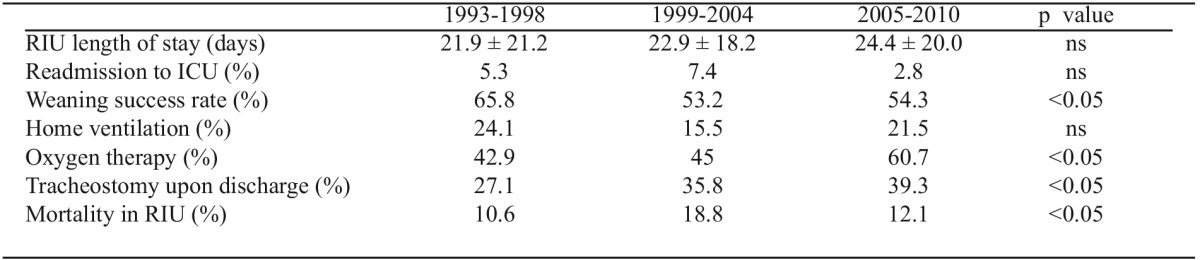
RIU: respiratory intermediate unit, ns: non significant
The proportion of major surgical patients showed a slight reduction between the examined three periods. Weaning from mechanical ventilation was achieved in 80% of patients and in 58.5% of patients the tracheostomy was closed. In 47.2% of patients home oxygen therapy was initiated or continued. The rate of home mechanical ventilation did not change significantly, but the number of patients discharged with tracheostomy or home oxygen therapy increased over time.
The overall RIU mortality was 15%, yet a difference in mortality was observed over time, with an increase over the second period and a decrease in the third period to the same level as it was in the first period (Table 2).
Over time, changes regarding nursing staff availability had occurred: in the first period there was a nurse/patient ratio of 0.5, in the second it was 0.83 and in the third period it declined to 0.33. This decrease recorded in the third period was followed by a reduction of RIU beds from six to three.
Discussion
The results of the current study demonstrate that ICU patients with difficult weaning from mechanical ventilation and persistent respiratory dysfunction were old, spent long time in ICU and as a consequence they had a tracheostomy in place and pressure ulcers upon discharge. For these patients the major underlying disorders were chronic respiratory disease and neuromuscular disorders.
Increased age is a common characteristic of patients transferred from ICU to RIU requiring prolonged ventilator support6,7 and this was an important issue in our study. Persistent respiratory failure seems to be more common in elderly patients, as aging is associated with a high rate of co-morbidities and impaired cardiopulmonary reserves.
The overall weaning success rate, that we observed, was similar to other studies, although weaning success among different centers is difficult to be compared, because of differences in the admitting criteria and the patients’ severity of illness8-10. Weaning from mechanical ventilation ranged between 73%-86.2% with an increase in the third examined period. Over time mechanical support was continued in a constant percentage of patients, mainly suffering from chronic obstructive or restrictive respiratory disorder and a substantial percentage of patients started or continued long term oxygen therapy.
The percentage of tracheostomy in place upon discharge showed a trend to increase over time, a phenomenon reported from other centers, too. In a survey from five Italian RIUs, tracheostomy remained in place upon discharge in a substantial number of weaned patients who had co-morbidities or were over 70 years of age11. We assume that in our patients, the increased age and the increased number of patients with underlying neuromuscular disorders are additional reasons for the tracheostomy maintenance and/or weaning failure upon discharge, because these two conditions predispose to weakness of effective cough and airway clearance.
The reported RIU mortality ranges in various studies between 10-20%, depending on different admission criteria and the severity of patient’s condition7,8,12,13. In our study the overall RIU mortality was 15% without significant difference between the first and third examined period, but with a noticeable increase in the second period. During this second period, the health condition of admitted patients was more complicated as indicated by the increased presence of pressure ulcers, cardiovascular diseases and increased duration of ICU stay.
It is worth noting that the acceptance of patients in RIU declined in the third examined period, mainly due to the fact that during this period there was a reduction in the availability of nursing staff, related to hospital administration policy.
In most European countries as seen in Italy and Spain, patients admitted in RIUswere transferred from emergency departments, suffering from acute respiratory failure and a smaller proportion was after ICU discharge9-13, while in France and Germany RIUs serve exclusively for post intensive care of patients with difficult weaning14. In these units weaning protocols are implemented and also programs for patient and familiy preparation in the case of home ventilator support15,16. Ιn our study, all patients were transferred from ICUs due to persistent respiratory failure requiring prolonged mechanical ventilation.
It is recently reported that tracheostomy in place, after ICU discharge, is associated with increased mortality when patients are transferred to the ward17. There are several reports about the cost effectiveness of such units and their influence in patients’ outcome18-20. There are different proposals about the unit or department of hospitalization in terms of the patients’status which are related to each hospital’s policy. As this group of ICU patients with persistent respiratory dysfunction is expected to increase21, the establishment of a RIU will be crucial for critical bed availability and reduction of their economic burden19,20,22. From this point of view these facilities should be supported by health care professionals as well as health care policies, in order to maintain safe care for ICU patients with resistant respiratory dysfunction, especially nowadays with restricted health resources in countries under financial crisis23. On the other hand the continuum of care for these patients is also emphasized in many reports and these units are proposed to be connected with rehabilitation centers or with regional home care programs24-26.
Limitations of the study
Our study is a retrospective review of post-ICU patients over an 18-year-period. We used routinely collected data which did not allow us to examine the impact of patients’ condition before the acute deterioration of their health status. This variable, in addition to ICU complications, might have contributed to patients’ early outcome and difficulty in weaning. Furthermore, at the time of the study, no registry data about the ICU patients was available concerning the admitting criteria and definition for weaning failure. This limitation prevents from drawing any valid conclusions regarding correlations between outcomes and clinical parameters of patients’ condition.
Conclusion
The current study provides information regarding the clinical characteristics and outcome of ICU patients with persistent respiratory failure and weaning failure transferred to a RIU. Elderly patients with chronic respiratory or cardiovascular diseases, or patients suffering from neuromuscular disorders, could benefit from care provided in appropriate units as, in a considerable rate, ventilator independence can be achieved. For these patients, a RIU attached to a pulmonary department could serve as a proper destination when recovering from critical illness.
Conflict of interest
Authors declare no conflict of interest
References
- 1.MacIntyre NR, Epstein SK, Carson S, Scheinhorn D, Christopher K, Muldoon S, National Association for Medical Direction of Respiratory Care Management of patients requiring prolonged mechanical ventilation: report of a NAMDRC consensus conference. Chest. 2005;128:3937–3954. doi: 10.1378/chest.128.6.3937. [DOI] [PubMed] [Google Scholar]
- 2.da Silva MC, de Sousa RM, Padilha KG. Patient destination after discharge from intensive care units: wards or intermediate care units? Rev Lat Am Enfermagem. 2010;18:224–232. doi: 10.1590/s0104-11692010000200013. [DOI] [PubMed] [Google Scholar]
- 3.Corrado A, Roussos C, Ambrosino N, Confalonieri M, Cuvelier A, Elliott M, et al. Respiratory Society Task Force on epidemiology of respiratory intermediate care in Europe. Respiratory intermediate care units: a European survey. Eur Respir J. 2002;20:1343–1350. doi: 10.1183/09031936.02.00058202. [DOI] [PubMed] [Google Scholar]
- 4.Rhodes A, Ferdinande P, Flaatten H, Guidet B, Metnitz PG, Moreno RP. The variability of critical care bed numbers in Europe. Intensive Care Med. 2012;38:1647–1653. doi: 10.1007/s00134-012-2627-8. [DOI] [PubMed] [Google Scholar]
- 5.Lyder CH, Wang Y, Metersky M, Curry M, Kliman R, Verzier NR, et al. Hospital-acquired pressure ulcers: results from the national Medicare Patient. Safety Monitoring System study. J Am Geriatr Soc. 2012;60:1603–1608. doi: 10.1111/j.1532-5415.2012.04106.x. [DOI] [PubMed] [Google Scholar]
- 6.Bo M, Massaia M, Raspo S, Bosco F, Cena P, Molaschi M, et al. Predictive factors of in-hospital mortality in older patients admitted to a medical intensive care unit. J Am Geriatr Soc. 2003;51:529–533. doi: 10.1046/j.1532-5415.2003.51163.x. [DOI] [PubMed] [Google Scholar]
- 7.Fernández Del Campo R, Lozares Sánchez A, Moreno Salcedo J, Lozano Martínez JI, Amigo Bonjoch R, Jiménez Hernández PA, et al. Age as predictive factor of mortality in an intensive and intermediate care unit. Rev Esp Geriatr Gerontol. 2008;43:214–220. doi: 10.1016/s0211-139x(08)71185-5. [DOI] [PubMed] [Google Scholar]
- 8.Polverino E, Nava S, Ferrer M, Ceriana P, Clini E, Spada E, et al. Patient’s characteristics, hospital course and clinical outcomes in five Italian respiratory care units. Intensive Care Med. 2010;36:137–142. doi: 10.1007/s00134-009-1658-2. [DOI] [PubMed] [Google Scholar]
- 9.Scheinhorn DJ, Hassenpflug MS, Votto JJ, Chao DC, Epstein SK, Doig GS, et al. Post ICU mechanical ventilation at 23 long-term care hospitals. Chest. 2007;131:85–93. doi: 10.1378/chest.06-1081. [DOI] [PubMed] [Google Scholar]
- 10.Wijkstra PJ, Avendano MA, Goldstein RS. Inpatient chronic assisted ventilator care. A 15 year experience. Chest. 2003;124:850–856. doi: 10.1378/chest.124.3.850. [DOI] [PubMed] [Google Scholar]
- 11.Confalonieri M, Gorini M, Ambrosino N, Mollica C, Corrado A. Respiratory intensive care units in Italy: a national census and prospective cohort study. Thorax. 2001;56:373–378. doi: 10.1136/thorax.56.5.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aburto M, Esteban C, Aguirre U, Egurrola M, Altube L, Moraza FJ, et al. A year’s experience in an Intermediate Respiratory Care Unit. Arch Bronconeumol. 2009;45:553–539. doi: 10.1016/j.arbres.2009.04.015. [DOI] [PubMed] [Google Scholar]
- 13.Sala E, Balaguer C, Carrera M, Palou A, Bover J, Agustí A. Activity of an intermediate respiratory care unit attached to a respiratory medicine department. Arch Bronconeumol. 2009;45:168–172. doi: 10.1016/j.arbres.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 14.Nava S, Confalonieri M, Rampulla C. Intermediate respiratory intensive care units in Europe: a European perspective. Thorax. 1998;53:798–802. doi: 10.1136/thx.53.9.798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Simonds AK. Streamlining weaning: protocols and weaning units. Thorax. 2005;60:175–177. doi: 10.1136/thx.2004.028688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kahn JM. The evolving role of dedicated weaning facilities in critical care. Intensive Care Med. 2010;36:8–10. doi: 10.1007/s00134-009-1672-4. [DOI] [PubMed] [Google Scholar]
- 17.Martinez GH, Fernandez R, Casado MS, Cuena R, Lopez-Reina P, Zamora S, et al. Tracheostomy tube in place at Intensive Care Unit: Discharge ιs associated with increased ward mortality. Respir Care. 2009;54:1644–1652. [PubMed] [Google Scholar]
- 18.Seneff Mg, Wagner D, Thompson D, Honeycutt C, Silver MR. The impact of long-term acute care facilities on the outcome and cost of care for patients undergoing prolonged mechanical ventilation. Crit Care Med. 2000;28:342–350. doi: 10.1097/00003246-200002000-00009. [DOI] [PubMed] [Google Scholar]
- 19.Pilcher DV, Bailey MJ, Treacher DF, Hamid S, Williams AJ, Davidson AC. Outcomes cost and long term survival of patients referred to a regional weaning centre. Thorax. 2005;60:187–192. doi: 10.1136/thx.2004.026500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lone NI, Walsh TS. Prolonged mechanical ventilation in critically ill patients: epidemiology, outcomes and modelling the potential cost consequences of establishing a regional weaning unit. Crit Care. 2011;15:R102. doi: 10.1186/cc10117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Esteban A, Anzueto A, Frutos F, et al. Characteristics and outcomes in adult patients receiving mechanical ventilation: a 28-day international study. JAMA. 2002;287:345–355. doi: 10.1001/jama.287.3.345. [DOI] [PubMed] [Google Scholar]
- 22.Robson V, Poynter J, Lawler PG, Baudouin SV. The need for a regional weaning centre, a one year survey of intensive care weaning delay in the Northern Region of England. Anaesthesia. 2003;58:161–182. doi: 10.1046/j.1365-2044.2003.02964_1.x. [DOI] [PubMed] [Google Scholar]
- 23.Morgan D, Astolfi R. Health spending continues to stagnate in many OECD countries. OECD Health Working Papers 2014, 68 OECD Publishing. Available at: http://dx.doi.org/10.1787/5jz5sq5qnwf5-en. Last accessed 3-4-2014.
- 24.Ceriana P, Delmastro M, Rampulla C, Nava S. Demographics and clinical outcomes of patients admitted to a respiratory intensive care unit located in a rehabilitation center. Respir Care. 2003;48:670–676. [PubMed] [Google Scholar]
- 25.Bagley PH, Cooney E. A community based regional ventilator weaning unit. Development and outcomes. Chest. 1997;111:1024–1029. doi: 10.1378/chest.111.4.1024. [DOI] [PubMed] [Google Scholar]
- 26.Carpene N, Vagheggini G, Panait E, Gabbrielli L, Ambrosino N. A proposal of a new model for long term weaning: respiratory intensive care unit and weaning center. Respiratory Medicine. 2010;104:1505–1511. doi: 10.1016/j.rmed.2010.05.012. [DOI] [PubMed] [Google Scholar]


