Abstract
Aims
Educating physicians in the procedural as well as cognitive skills of information technology (IT)-mediated medication management could be one of the missing links for the improvement of patient safety. We aimed to compose a framework of tasks that need to be addressed to optimize medication management in outpatient care.
Methods
Formal task analysis: decomposition of a complex task into a set of subtasks. First, we obtained a general description of the medication management process from exploratory interviews. Secondly, we interviewed experts in-depth to further define tasks and subtasks. Setting: Outpatient care in different fields of medicine in six teaching and academic medical centres in the Netherlands and the United States. Participants: 20 experts. Tasks were divided up into procedural, cognitive and macrocognitive tasks and categorized into the three components of dynamic decision making.
Results
The medication management process consists of three components: (i) reviewing the medication situation; (ii) composing a treatment plan; and (iii) accomplishing and communicating a treatment and surveillance plan. Subtasks include multiple cognitive tasks such as composing a list of current medications and evaluating the reliability of sources, and procedural tasks such as documenting current medication. The identified macrocognitive tasks were: planning, integration of IT in workflow, managing uncertainties and responsibilities, and problem detection.
Conclusions
All identified procedural, cognitive and macrocognitive skills should be included when designing education for IT-mediated medication management. The resulting framework supports the design of educational interventions to improve IT-mediated medication management in outpatient care.
Keywords: education, human factors, IT, medication management, task analysis
WHAT IS ALREADY KNOWN ABOUT THIS SUBJECT
Medication safety might be improved by well-designed education regarding IT-mediated medication management
To inform the design of education an analysis of skills and complicating factors of IT-mediated management is needed
The process of medication management includes reconciliation, prescribing, communicating with the pharmacy, dispensing, administration, monitoring, and patient education.
From this process description, the exact skills to be trained are unclear
WHAT THIS STUDY ADDS
Identification of procedural, cognitive, and macrocognitive skills needed for IT-mediated medication management
Identification of complicating factors for IT-mediated medication management
Directions for the design of education to improve IT-mediated medication management
Introduction
Medications represent a core treatment option for outpatients. However, medication use is frequently complicated by adverse events, many of which are preventable [1–3]. An adverse event is an adverse outcome that can be attributed to an action of a drug [4]. Unnoticed or inadequately managed drug–drug interactions, contraindications, under/overdosing and duplicate therapy have been associated with preventable adverse drug events [3]. Besides these so-called therapeutic medication errors, administrative medication errors, such as errors in readability, drug name and route of administration, also contribute to preventable adverse events [5]. The Institute of Medicine estimated the number of deaths due to medication errors to be one out of every 131 outpatient deaths [6]. Electronic prescribing with computerized physician order entry (CPOE) may reduce medication errors by improving the legibility and completeness of prescriptions as well as by clinical decision support for alerting and managing drug–drug interactions, drug–disease interactions, allergies and past adverse drug events, inappropriate dosing and duplicate medication [7]. On the other hand, use of CPOE may also facilitate new errors, such as selecting the incorrect patient, drug or dose [8].
Education of health care professionals is usually necessary to exploit the full potential of information technology (IT). Financial incentives have been suggested to stimulate the adoption of IT. However, this approach does not provide the necessary new skills and knowledge for meaningful use. These are vital as current IT systems in health care are often unintuitive, have many different components and are used in dynamic medical environments. Adequate education of end-users may be the missing link for further improvements in patient safety by IT. Limited data are available regarding how to design education for physicians on the use of complex IT [9–11].
Intuitively designed educational approaches for the use of IT typically result in teaching physicians (procedural) computer skills. But cognitive skills are often a prerequisite for adequate performance of the procedures. A cognitive skill is, for example, the decision as to whether or not to register an adverse drug event in CPOE and is a prerequisite for the correct (procedural) registration. Task analysis is a technique supporting the explication of these cognitive skills [12]. Task analysis includes the decomposition of a complex task into a set of subtasks, and the exploration of complicating circumstances. When designing education on the basis of a task analysis, the analysed tasks can be converted into learning goals. Analysis of complicating circumstances guides the gradual increase in complexity of instruction. In aviation, this method has been efficacious in designing education. Flying an aeroplane resembles meaningful use of IT in medication management because cognitive skills such as decision making are a prerequisite for the performance of the procedural part of the task in order to reach the destination safely [13].
Physicians play a key role in the outpatient medical process by medication history taking including reconciliation and use of medication, choosing the correct medicine, writing the prescriptions, communicating with the patient about the goals, risks and instructions for administration, and communicating with the pharmacy to ensure correct dispensing [10,14–18]. In this study, we focus on the physician's tasks in the medication process, which we refer to as 'medication management'. The goals of physicians' medication management are to maximize the effectiveness and minimize the risks of treatment, minimize costs and respect patients' choices [19]. This includes paying attention to patients' adherence to medication: do patients take their medication as prescribed [20]? It also includes shared decision making, which is the process of physician and patient jointly participating in a health decision after discussing options, benefits and harms, and explicitly taking the patient's own preferences into account [21]. This differs from patient education, which takes place after the decision is made and the patient is instructed about how and when to use the medication, and when to contact the physician [22].
To provide a sound basis for the design of education, insight into the task to be learned is necessary. The goal of this study was to obtain clear and comprehensive insights into the various procedural and cognitive tasks and complicating circumstances involved in the optimal use of IT in medication management by physicians in the outpatient clinic. We also aimed to create a framework for these tasks.
Methods
Study design
Formal task analysis is scientifically based in human factors engineering techniques [23]. Human factors science is concerned with the interplay between technologies and their use by humans. Technical systems often do not fulfil their promise – sometimes due to the technical content of the system itself, but more often because the technology does not optimally support the human's tasks. Human factors methods clarify this interplay and support improvements by, for example, interface redesign or the education of end-users. Task analysis employs and combines different methods. First, we obtained a general description of the medication management process from the literature and exploratory interviews. Secondly, we interviewed experts in-depth to compose a conceptual framework of tasks and to define complicating circumstances. We acquired ethical approval from the Ethical Review Board of the Dutch Association for Medical Education for this study.
Stage 1: general process description and characteristics of experts
Data collection
The first process description was based on the existing literature, as referred to in the introduction, and interviews with a convenience sample of four health care professionals who had an overview of the field of IT-mediated medication management (Table 1). In a 1-h semi-structured exploratory interview, FvS asked participants whether they recognized the components of the process description from the literature and which components were missing. In the second part of the interview, FvS asked participants to elaborate on the type of experts that should be interviewed to obtain an in-depth analysis of IT-mediated medication management.
Table 1.
Participant characteristics for stage 1
| Participants in exploratory interviews(n = 4) | No. of participants |
|---|---|
| Expertise | |
| Physician and clinical pharmacologist, both >8 years of experience with information technology (IT) for medication management | 2 |
| Hospital pharmacist specialized in IT for medication management | 1 |
| Health care manager responsible for education of physicians in IT-mediated medication management | 1 |
| Hospitals | |
| University Medical Centre, Utrecht, Utrecht, the Netherlands | 3 |
| Erasmus Medical Centre, Rotterdam, the Netherlands | 1 |
Data analysis
For a meaningful categorization of the components of medication management, we applied a general theory of dynamic decision making. This theory states that complex tasks consist of situational awareness, decision making and action [24,25].
Respondents in stage 1 indicated that experts should be physicians practising in outpatient care representing various fields of medicine, and should have an expertise in using medication-related IT plus additional expertise in pharmacotherapy, research, education, policy and/or development of IT. Experts should represent various settings, teaching as well as academic medical centres, and should be using various types of medication-related IT.
Generally, for full expertise, 10 years of engagement in a specific domain is required [26]. Few physicians meet this criterion for the use of medication-related IT. Therefore, we judged interviewees on their reflections on their own performance, which is also a feature of expertise [26].
Stage 2: in-depth expert interviews to analyse tasks and complicating circumstances
Data collection
For the in-depth interviews, we recruited experts in the Netherlands and asked them to suggest other experts, a method called 'snowballing'. Physicians with expertise in research and policy regarding medication-related IT were not available in the Netherlands, so we interviewed experts in the USA (see Table 2 for details about the experts).
Table 2.
Participant characteristics for stage 2
| Participants in-depth expert interviews (n = 20) | No. of participants |
|---|---|
| Specialization of participants: | |
| General internal medicine | 8 |
| Oncology | 2 |
| Nephrology | 2 |
| Haematology | 1 |
| Endocrinology | 1 |
| Gastroenterology | 1 |
| Infectious disease | 1 |
| Rheumatology | 1 |
| Geriatrics | 2 |
| Cardiology | 1 |
| Additional expertise (most had >1) | |
| Clinical pharmacology | 5 |
| Published research regarding medication management IT | 7 |
| Education regarding medication management IT | 18 |
| Development of medication management IT | 5 |
| Policy regarding medication management IT | 4 |
| Hospitals: | |
| University Medical Centre Utrecht, Utrecht (the Netherlands) | 6 |
| Erasmus Medical Centre, Rotterdam (the Netherlands) | 3 |
| Catharina Hospital, Eindhoven (the Netherlands) | 2 |
| Brigham and Women's Hospital, Boston, MA (USA) | 6 |
| Stanford Medical Centre, Stanford, CA (USA) | 2 |
| Palo Alto Medical Foundation, Palo Alto, CA (USA) | 1 |
| IT for medication management used by experts | |
| EZIS-Medicatie (Chipsoft) CPOE/CDSS/integrated with Electronic Health Record (EHR) | 8 |
| EVS-Medicatie (I-soft) CPOE/CDSS/not fully integrated with EHR | 3 |
| EPIC CPOE/CDSS/integrated with EHR | 2 |
| Brigham and Women's home-grown CPOE/CDSS/ integrated with EHR | 6 |
During the in-depth, semi-structured, 1-h face-to-face interviews, experts were asked to imagine themselves in the outpatient clinic with a variety of patients and to elaborate on what they do to manage their patients' medications. To deepen the information, the interviewer (FvS) asked questions about how and when they used IT to perform these tasks, the problems they faced, how they dealt with these problems under time pressure, and what decisions they made. Experts were also asked to describe the most important complicating circumstances (see Appendix 1 for the interview protocol).
Interviews were recorded digitally and transcribed verbatim. In this study, saturation was considered to be accomplished when 90% of the items (i.e. codes) in the framework were defined. On the basis of the literature, we expected saturation after approximately 12 interviews [27]. After saturation, interviews were used for corroboration [27].
Data analysis
First, FvS named all tasks and complicating factors in three interviews, a method called 'open coding'. A hospital pharmacist (JZ) coded one in-depth interview independently using this codebook. FvS and JZ discussed the categorizations and definitions of the codes until a consensus was reached. Subsequently, five Dutch interviews were coded independently by JZ and FvS, and four US interviews were coded independently by FvS and LAM. Pairs of coders discussed disagreements until a consensus was reached, which meant that inter-rater differences were solved after discussion. When a consensus could not be reached, EtB (internist) was consulted.
To indicate whether tasks were procedural (e.g. ' to document') or cognitive (' to evaluate'), Bloom's taxonomy was used [28]. In addition, macrocognitive tasks were identified [29]. These are specific forms of cognitive task performed when acting in complex socio-technical environments, where planning and adaptation to changing situations is paramount [29]. Complicating circumstances were defined as factors that affect the physician's ability adequately to perform IT-mediated medication management [24,25].
The structure of the task was agreed upon after discussion between the three coders (FvS, JZ and LAM), internist (EtB), expert in task analysis (JMS), pharmacist (TE) and biomedical informatics researcher (JA). This resulted in the final version of the codebook. FS coded the remainder of the interviews and discussed uncertainties. The results were verified by five of the previously interviewed experts, a method called 'member checking'. The outcome was a framework of physicians' tasks included in IT-mediated medication management in the outpatient setting.
Results
Participant details are depicted in Tables 1 and 2. For stage 2, we interviewed 22 experts in the Netherlands (n = 12) and USA (n = 10). All participants were physicians practising in outpatient care. Participants had a median of 8 years (range 6–10 years) of experience using IT for medication management and a median of 15 years (range 6–25 years) of prescribing medications. Two of the invited physicians did not meet the standards of expertise, so 20 in-depth interviews were used for analysis. Saturation was reached after eight interviews.
The resulting framework is presented in Figure1. It shows that outpatient IT-mediated medication management comprises three main components: (i) reviewing the medication situation; (ii) composing a treatment plan; and (iii) accomplishing and communicating the treatment and surveillance plan. These components include procedural and cognitive tasks. During the whole process, macrocognitive tasks support a smooth and accurate performance. We also identified complicating circumstances jeopardizing accuracy and safety.
Figure 1.
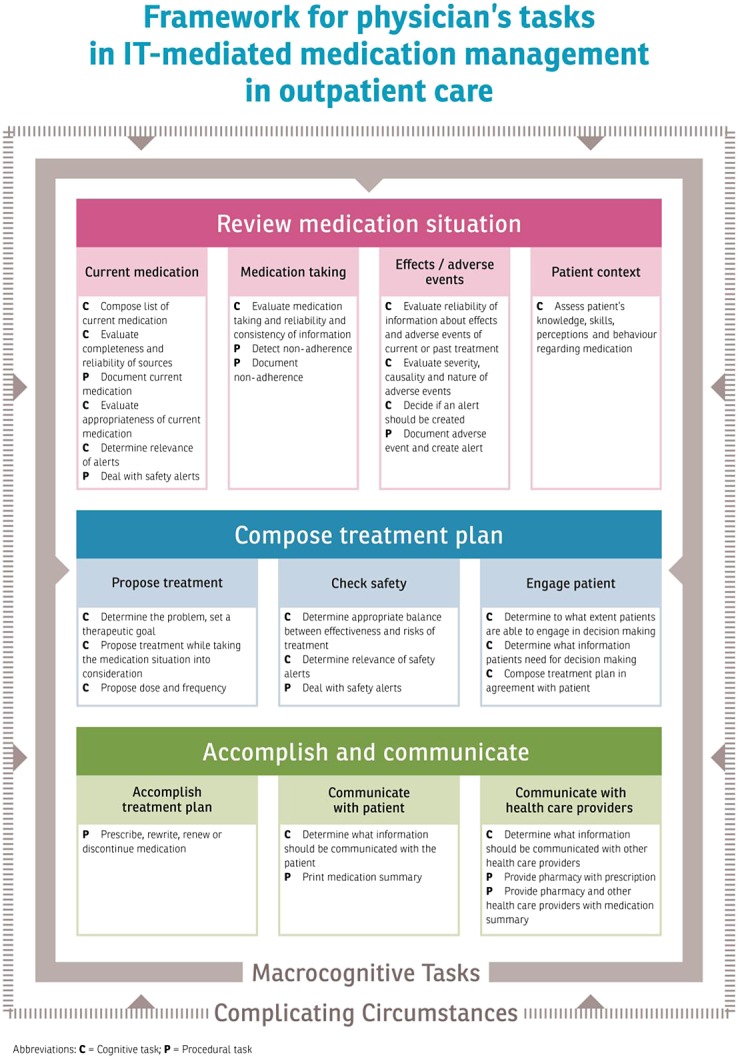
Framework for physician's tasks in IT-mediated medication management in outpatient care
Reviewing the medication situation
Reviewing the medication situation is a component of medication management in which cognitive and procedural tasks alternate. For example, a list of current medications is composed by combining information from several sources and judging their reliability (cognitive tasks), followed by documenting the current medication into the IT system (procedural task) and evaluating the current medications for appropriateness, such as drug–drug interactions.
“Now, a third source of truth, which complicates things further, is the information from the pharmacy. Until recently, we did not have that available. We do now, but it's set up in a way in which you have [to] go through an extra step to get to it and you can't easily look at the whole list, you have to do one medication at the time.” (US14)
Physicians reported that they reviewed whether patients took their medications as prescribed (cognitive task). Where possible, physicians used IT to detect and document non-adherence (procedural).
“ I need to have a sense of what the patient is able to understand and a glimpse [in]to whether they are able to be adherent to the medicine. If they don't know what a medicine is for, they might not be taking it. Or [if] a patient has to take a pill every day and I haven't refilled it since 2010, you know they are not taking it. … Or they say: " Yes, I am taking my medicine," but their cholesterol is still 274… It is educational for me to figure out if somebody actually is taking those medications. And if they are not… why they are not… and if they can open a bottle…” (US17)
Current and past adverse drug events are assessed on reliability, causality and severity (cognitive task). If applicable, adverse events are documented (procedural). Physicians noticed that, among health care providers, there are no universal operational definitions of adverse events and allergies. This complicates the registration of such events and is further complicated by the use of vague terms used within the IT systems themselves.
“We are not done by only using the terms " side effect" and " allergy". An event may be called a side effect by one doctor, and just a medication effect by another… And allergies are also difficult because some think it is not an allergy, but a side effect. And how are you going to document this in the system? The button in the system where I can document adverse events is called " Allergies" ” (NL5)
Assessing patients' knowledge and behaviour regarding medication is a cognitive task. Typically, physicians combine tasks:
“I match the name of the medication with the effect. I will say: I notice that you take tacrolimus for your transplant, twice a day, 1 mg – is that right? … Then I look at their reaction. If they look a little puzzled, this is a sign for me that I have to pay more attention to this.” (NL1)
Composing a treatment plan
Composing a treatment plan consists merely of cognitive tasks. Physicians indicate the problem, take the medication situation into consideration and propose prescribing, rewriting, continuing or discontinuing treatments. When physicians prescribe medications, they consider dosing, frequency and safety issues.
Decision support systems give directions for the appropriateness and safety of the proposed treatment. Physicians determine whether alerts from the system are relevant for their patient. The only procedural task in this component is dealing technically with the alert.
“At that point, I actually use decision support to help me, so I can tell them whether there is any issue around interactions with other medications.” (US19)
Physicians reported that they strived to participate in shared decision making with their patients. In this process, they estimated the extent to which the patient is capable of making a decision about their treatment, and determine what information patients need to participate in the decision-making process.
“I discuss with my patients the reasons for starting the medication. When the patient agrees, I prescribe it on the system… I negotiate with my patients. I discuss with them the nature of the problem and the possibilities for solving it.” (NL4)
Accomplishing and communicating the treatment and surveillance plan
Accomplishing the treatment plan is largely a procedural task that can include prescribing, rewriting, renewing or discontinuing medications on the system.
Cognitive and procedural tasks are intertwined in the communication of the treatment and surveillance plan. Physicians reported that they instructed patients about why, how and when to take the drugs, the nature and time of the expected effect, to be alert to symptoms indicating side effects, and what to do in case of supposed side effects (cognitive tasks). A medication summary is printed to support this communication (procedural).
“I use the process of placing the order, which I do in their presence, to cue me to do all steps. So I literally would say: “I prescribe for you medicine x at this dose” and I speak to them about [it], saying: “this is a starter dose – we may have to escalate it later… You are going to take this once a day and let me tell you something about, we may already [have] talked about [it], the indication for starting that medication”, and at that point I would talk about the side effects and how they will get the medication and then sending the prescription off to their pharmacy.” (US19).
Communication with the community pharmacy and other health care providers consists of a combination of cognitive and procedural tasks. Physicians provide the pharmacy with their prescription and estimate whether it is necessary to provide pharmacy and other health care providers with additional information, such as indications or reasons for discontinuation.
“Sometimes there is medication that has resulted in severe renal or liver insufficiency. Then I think everybody has to know. Then I will document the reason for [its] discontinuation in the IT system, [and] this will be printed on the medication summary.” (NL8)
Macrocognitive tasks
Four macrocognitive tasks were identified: planning, integration, managing uncertainties and responsibilities, and problem detection. Physicians are planning during the whole medication management process. They plan, for example, when and how thoroughly they review and document the current medication:
“I always ask patients: " Has anything changed in the meantime?" I pay more attention to verification of a medication if I am going to prescribe or change it, or when there are symptoms possibly caused by it.” (NL6)
Physicians integrate IT into their workflow and detect possible problems and errors:
“If you do it right, CPOE can dramatically improve the transparency of the process and it allows you to use prescribing as an educational opportunity. I turn the computer screen and, while I write my prescription, I tell them what I am doing – it becomes another opportunity to reinforce [to] them why I am doing it, and it also has the advantage that they can be a safety check.” (US16)
Physicians deal with uncertainties concerning the reliability of information from their patients. In addition, they determine which medication-related tasks are within their area of responsibility, and they may not want to take responsibility for medications that they themselves did not prescribe.
“Especially psychiatric medications… I prefer not to renew these, or only for 1 week. Then I suggest asking their responsible caretaker.” (NL1)
Complicating circumstances
Circumstances that complicate the accurate and safe accomplishment of physicians' tasks are related to: (i) system design (the health care, as well as IT, system); (ii) patients' characteristics; and (iii) workload.
Poor organization of health care systems makes medication management, and especially composing an accurate list of current medications, more complicated.
“Because our system is unfortunately fragmented, there maybe medications from other doctors or maybe they went to an emergency room in another state.” (US17)
Poor IT-system design does not support complex prescriptions, such as medicines that are not in the standard formulary, are taken at different doses a day, are taken according to tapering schemes, consist of half-pills or are taken 'as needed'. Physicians reported that medication management was also more complicated when patients were not able to provide accurate information. This was particularly the case when patients had a low educational level or there was a language barrier.
Physicians' workload increased with the number of patients they treated in a day, resulting in increased time pressure. The number of medications and comorbidities per patient also raised the complexity of decision making. Complexity increased further with the number of other competing tasks, such as giving emotional support or simultaneously caring for other patients.
Discussion
The resulting framework of physicians' tasks is crucial in guiding the future design of educational interventions for the optimal use of IT in medication management in the outpatient clinic. Training should include all identified procedural, cognitive and macrocognitive tasks.
To inform the design of educational interventions, it is vital to analyse the task-to-be-educated as a whole. This implies that all essential aspects of the task should be included in the educational intervention. This acknowledges the complexity of the task, including the context in which it must be performed. Until now, only fragments of the complicated domain of IT-mediated medication management received attention in the literature. Koppel et al. focused on the use of IT by physicians in the inpatient setting and concluded that a wide variety of (near) medication errors were due to interface problems and the incorrect use of IT [8]. Previous research also demonstrated the importance of distinct physician tasks during medication management: medication reconciliation, taking a complete medication history including questions about non-adherence and adverse drug events, and shared decision making [15,21]. Bell et al. [10] and McKibbon et al. [14] proposed a general description of the process of IT-mediated medication management. [10, 14] However, for the design of education, these task descriptions are still either too fragmented, or too general, and make no distinctions between cognitive, macrocognitive and procedural tasks. In health care, the importance of cognitive tasks, such as situation awareness and decision making, and macrocognitive tasks has been acknowledged and analysed in surgery and anaesthesia, and recently a general framework of non-technical skills in health care was proposed [30,31].
This current study analysed the set of tasks in IT-mediated medication management integrating procedural as well as cognitive tasks, providing a sound basis for the design of education.
We hypothesized that, to date, physicians have not been trained sufficiently in the optimal use of IT in medication management. They typically receive only a short introduction to, and demonstration of, some technical procedures. Optimal education with the goal of improving patient safety should also explicitly address the cognitive tasks in medication management, such as: what to do if the medication-related information is unreliable; when an alert should be created for an adverse event; and when to provide extra information to other health care providers. Physicians face these problems on a daily basis.
The analysed complicating circumstances determine the didactical sequence of cases. By starting with easy cases and gradually enhancing the level of difficulty,physicians are enabled to develop their competency steadily [32]. Macrocognition is used increasingly when medication management becomes more complex.
The resulting framework enabled us to design a generic training package for medication management in outpatient care that fosters the optimal use of IT. A sample online module based on the framework is added as a supplement [33]. This sample comprises the most complex module, in which physicians practise a case including non-adherence, incomplete information, multiple comorbidities, complex medications, drug–drug interactions and distractions during prescribing. Macrocognitive strategies for error detection are addressed. All components of IT-mediated medication management, with their cognitive and procedural tasks, are included: the current medication situation is reviewed and a therapeutic plan is composed, accomplished and communicated. However, physicians could first practise with modules that feature easier cases, wherein patients provide complete and reliable information about their medication and need simple prescriptions.
Besides ensuring education about a whole task, analysis of a task also supports the description of the nature of the subcomponents of the task and subsequently determines the appropriate teaching method for this task. For example, learning how to register an adverse drug event in CPOE requires practising with the CPOE system. However, learning how to determine whether an adverse drug event should be registered requires an appropriate rule of thumb, and knowledge about the consequences of registration.
Task analysis may also be a valuable technique for designing education for other health care domains in which IT and clinical practice are highly intertwined, such as the use of electronic health records. Training programmes designed on the basis of these analyses may be useful in undergraduate as well as postgraduate and continuing medical education. Task analysis may also help to improve the interface design of IT for medication management. For interface design, the same technique may be used, but the focus of analysis is more on whether the interface supports all components of the task [23].
This study had several limitations, including the use of self-reported data. This may have introduced social desirability response bias [34]. We took proactive measures to avoid this by asking explicitly what experts do if time is scarce. Another limitation was the use of two sources of information: existing literature and interviews. Observations of physicians might have revealed even more insight. However, the purpose of this study was to compose a framework, rather than understanding exactly how physicians accomplish tasks. Future researchers may undertake observations to specify training goals further and may find our proposed framework helpful in guiding their interpretation.
This study was strengthened by the participation of experts from various hospitals, in two countries, using different medication management IT systems, and allowed for generalization of the results. Additionally, the inclusion of 20 participants reduced potential study bias as it is highly unlikely that major tasks would have been missed after interviewing 20 experts. US interviews mostly corroborated the results from the Dutch interviews. Another strength was the collaboration of multiple disciplines in the research team. The interviewer (FvS) is a physician trained in qualitative research. A clinical information analyst from the USA (LAM) checked codes for the US context. The cognitive psychologist (JMS) contributed employing appropriate methods for the task analysis. The use of various sources of information (literature and interviews), corroboration of findings, coding by three people and member checking further contributed to the reliability of the study results.
Conclusion
Educating physicians in the skills of IT-mediated medication management is an important component of promoting patient safety. We performed a formal task analysis, providing insight into the procedural, cognitive and macrocognitive tasks needed for training physicians to improve their outpatient medication management with optimal use of IT. The study also provided an insight into how to increase the complexity of training by adding complicating circumstances. The resulting framework supports the design of educational interventions to improve IT-mediated medication management in outpatient care.
Appendix 1: Interview protocol
Introduction: The goal of the research is to develop an educational intervention to improve CPOE-medicated medication management in the outpatient clinic. In this interview, we focus on medication verification, the prescribing of medication and medication communication.
Research question: What knowledge and skills are needed for proper CPOE-mediated medication management in the outpatient clinic?
In this interview we focus on the following questions: What are the most important goals, and how are they reached? What are risks and complexities of CPOE-mediated medication management?
Consent: Do you agree to participate in this research? And do you accept digital recording of the interview?
Expertise
I first would like to talk to you about your expertise in this field. For how many years have you used CPOE? How many different systems have you used? Did you participate in the development of your CPOE system? Did you do research in the field of CPOE? Are you also involved in education about CPOE or medication management?
Part 1: Goals and actions
Please picture yourself working in the outpatient clinic. You are seeing a patient, and you are going to verify (prescribe, communicate) his or her medication; what do you do?
Why do you do this?
What do you need (tools, information) to perform medication verification properly?
-
Does medication management differ in different circumstances?
◦ New patient vs. patient you already know.
◦ Old/ disabled patient vs. relatively young and healthy patients, etc.
Part 2: Decisions
At what points of the process do you make decisions? What kind of decisions?
What knowledge and skills do you need to make the right decision?
When do you know that a sub-goal has been reached?
Part 3: Risks and complexities
Which parts of the process are the most error-prone or prone for errors with severe outcomes? Where in the process is patient safety diminished?
What parts of the process take the most time? Why?
What sub-goals are sometimes not reached? Why?
When does CPOE-mediated medication management become complex? / What types of influence make it complex? (e.g. number of medications)
Competing Interests
All authors have completed the Unified Competing Interest form at http://www.icmje.org/coi_disclosure.pdf and declare: EtB and FvS had support from ZonMw (the Netherlands Organization for Health Research and Development) for the submitted work – the design, analysis, interpretation, and reporting of the study are entirely independent of the funder; no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; no other relationships or activities that could appear to have influenced the submitted work.
Contributors
FvS carried out design, data collection, data analysis and writing. JZ and LAM carried out data analysis and reviewing. JA carried out design, data collection, data analysis and reviewing. DB, TvG and PJ carried out data collection and reviewing. JMS and EtB carried out design, data analysis and reviewing. AE carried out data analysis, writing and reviewing.
We thank all interviewees for participating in this study. This research is financed by The Netherlands Organisation for Health Research and Development (ZonMw): the main commissioning organizations for ZonMw are the Dutch Ministry of Health and the Netherlands Organization for Scientific research.
Supporting Information
Additional Supporting Information may be found in the online version of this article at the publisher's web-site:
Module 4.1
Medication management with optimal use of IT
References
- 1.Dornan T, Ashcroft D, Heathfield H, Lewis P, Miles J, Taylor D, Tully M, Wass V. 2009. An in-depth investigation into causes of prescribing errors by foundation trainees in relation to their medical education: EQUIP study. Final report to the General Medical Council. University of Manchester: School of Pharmacy and Pharmaceutical Sciences and School of Medicine. ; Available at: http://www.gmc-uk.org/about/research/25056.asp (last accessed 23 September 2013)
- 2.Gandhi TK, Weingart SN, Borus J, Seger AC, Peterson J, Burdick E, Seger DL, Shu K, Federico F, Leape LL, Bates DW. Adverse drug events in ambulatory care. N Engl J Med. 2003;348:1556–64. doi: 10.1056/NEJMsa020703. [DOI] [PubMed] [Google Scholar]
- 3.Leendertse AJ, Egberts AC, Stoker LJ, van den Bemt PM HARM Study Group. Frequency of and risk factors for preventable medication-related hospital admissions in the Netherlands. Arch Intern Med. 2008;168:1890–6. doi: 10.1001/archinternmed.2008.3. [DOI] [PubMed] [Google Scholar]
- 4.Aronson JK, Ferner RE. Clarification of terminology in drug safety. Drug Saf. 2005;28:851–70. doi: 10.2165/00002018-200528100-00003. [DOI] [PubMed] [Google Scholar]
- 5.van Doormaal JE, van den Bemt PM, Mol PG, Zaal RJ, Egberts AC, Haaijer-Ruskamp FM, Kosterink JG. Medication errors: the impact of prescribing and transcribing errors on preventable harm in hospitalised patients. Qual Saf Health Care. 2009;18:22–7. doi: 10.1136/qshc.2007.023812. [DOI] [PubMed] [Google Scholar]
- 6.Kohn LT, Corrigan JM, Donaldson MS, editors. To Err is Human: Building a Safer Health System. Washington DC: National Academies Press (US); 2000. [PubMed] [Google Scholar]
- 7.van Doormaal JE, van den Bemt PM, Zaal RJ, Egberts AC, Lenderink BW, Kosterink JG, Haaijer-Ruskamp FM, Mol PG. The influence that electronic prescribing has on medication errors and preventable adverse drug events: an interrupted time-series study. J Am Med Inform Assoc. 2009;16:816–25. doi: 10.1197/jamia.M3099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Koppel R, Metlay JP, Cohen A, Abaluck B, Localio AR, Kimmel SE, Strom BL. Role of computerized physician order entry systems in facilitating medication errors. JAMA. 2005;293:1197–203. doi: 10.1001/jama.293.10.1197. [DOI] [PubMed] [Google Scholar]
- 9.Pageler NM, Friedman CP, Longhurst CA. Refocusing medical education in the EMR era. JAMA. 2013;310:2249–50. doi: 10.1001/jama.2013.282326. [DOI] [PubMed] [Google Scholar]
- 10.McKibbon KA, Lokker C, Handler SM, Dolovich LR, Holbrook AM, O'Reilly D, Tamblyn R, J Hemens B, Basu R, Troyan S, Roshanov PS, Archer NP, Raina P. Enabling medication management through health information technology (Health IT) Evid Rep Technol Assess Full Rep. 2011;201:1–951. [PMC free article] [PubMed] [Google Scholar]
- 11.Ross S, Patey R, Flin R. Is it time for a nontechnical skills approach to prescribing? Br J of Clin Pharmacol. 2014;78:681–3. doi: 10.1111/bcp.12252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shepherd A. Hierarchial Task Analysis. London: Taylor & Francis; 2001. [Google Scholar]
- 13.Flin R, O'Connor P, Crichton M. Safety at the Sharp End: A Guide to Non-Technical Skills. Aldershot: Ashgate Publishing Limited; 2008. [Google Scholar]
- 14.Bell DS, Cretin S, Marken RS, Landman AB. A conceptual framework for evaluating outpatient electronic prescribing systems based on their functional capabilities. J Am Med Inform Assoc. 2004;11:60–70. doi: 10.1197/jamia.M1374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Drenth-van Maanen AC, Spee J, van Hensbergen L, Jansen PA, Egberts TC, van Marum RJ. Structured history taking of medication use reveals iatrogenic harm due to discrepancies in medication histories in hospital and pharmacy records. J Am Geriatr Soc. 2011;59:1976–7. doi: 10.1111/j.1532-5415.2011.03610_11.x. [DOI] [PubMed] [Google Scholar]
- 16.Garfield S, Barber N, Walley P, Willson A, Eliasson L. Quality of medication use in primary care –mapping the problem, working to a solution: a systematic review of the literature. BMC Med. 2009;7 doi: 10.1186/1741-7015-7-50. 50-7015-7-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Boockvar KS, Santos SL, Kushniruk A, Johnson C, Nebeker JR. Medication reconciliation: barriers and facilitators from the perspectives of resident physicians and pharmacists. J Hosp Med. 2011;6:329–37. doi: 10.1002/jhm.891. [DOI] [PubMed] [Google Scholar]
- 18.Pippins JR, Gandhi TK, Hamann C, Ndumele CD, Labonville SA, Diedrichsen EK, Carty MG, Karson AS, Bhan I, Coley CM, Liang CL, Turchin A, McCarthy PC, Schnipper JL. Classifying and predicting errors of inpatient medication reconciliation. J Gen Intern Med. 2008;23:1414–22. doi: 10.1007/s11606-008-0687-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barber N. What constitutes good prescribing? BMJ. 1995;310:923–5. doi: 10.1136/bmj.310.6984.923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nieuwlaat R, Wilczynski N, Navarro T, Hobson N, Jeffery R, Keepanasseril A, Agoritsas T, Mistry N, Iorio A, Jack S, Sivaramalingam B, Iserman E, Mustafa RA, Jedraszewski D, Cotoi C, Haynes RB. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. 2014;11 doi: 10.1002/14651858.CD000011.pub4. CD000011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hoffmann TC, Montori VM, Del Mar C. The connection between evidence-based medicine and shared decision making. JAMA. 2014;312:1295–6. doi: 10.1001/jama.2014.10186. [DOI] [PubMed] [Google Scholar]
- 22.de Vries TPGM, Henning RH, Hogerzeil HV, Fresle DA. Guide to Good Prescribing. Geneva: World Health Organization; 1994. [Google Scholar]
- 23.Schraagen JMC. Task analysis. In: Ericsson KA, Charness N, Feltovich PJ, Hoffman RR, editors. The Cambridge Handbook of Expertise and Expert Performance. New York, NY: Cambridge University Press; 2006. pp. 185–202. [Google Scholar]
- 24.Rasmussen J. Information Processing and Human–Machine Interaction: An Approach to Cognitive Engineering. New York, NY: North Holland; 1986. [Google Scholar]
- 25.Endsley MR. Toward a theory of situation awareness in dynamic systems. Hum Factors. 1995;37:32–64. [Google Scholar]
- 26.Ericsson KA. Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Acad Med. 2004;79(10 Suppl):S70–81. doi: 10.1097/00001888-200410001-00022. [DOI] [PubMed] [Google Scholar]
- 27.Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods. 2006;18:59–82. [Google Scholar]
- 28.Krathwohl DR. A revision of Bloom's taxonomy: an overview. Theory Pract. 2002;41:212–8. [Google Scholar]
- 29.Schraagen JM, Klein G, Hoffman RR. The macrocognition framework of naturalistic decision making. In: Schraagen JM, Militello LG, Ormerod T, Lipshitz R, editors. Naturalistic Decision Making and Macrocognition. Aldershot: Ashgate Publishing Limited; 2008. pp. 3–25. [Google Scholar]
- 30.Flin R, Patey R. Non-technical skills for anaesthetists: developing and applying ANTS. Best Pract Res Clin Anaesthesiol. 2011;25:215–27. doi: 10.1016/j.bpa.2011.02.005. [DOI] [PubMed] [Google Scholar]
- 31.Gordon M, Baker P, Catchpole K, Darbyshire D, Schocken D. Devising a consensus definition and framework for non-technical skills in healthcare to support educational design: a modified Delphi study. Med Teach. 2014;22:1–6. doi: 10.3109/0142159X.2014.959910. [DOI] [PubMed] [Google Scholar]
- 32.van Merrienboer JJG, Kirschner PA. Ten Steps to Complex Learning: A Systematic Approach to Four-Component Instructional Design. New York, NY: Taylor & Frances; 2012. [Google Scholar]
- 33.Stiphout van F. 2014. Module 4.1: Medication management with optimal use of IT. Available at http://143.121.209.126/∼lars/mv_utrecht_4.1/story.html (last accessed March 2015)
- 34.Hoffman RR, Crandall B, Shadbolt N. Use of the critical decision method to elicit expert knowledge: a case study in the methodology of cognitive task analysis. Hum Factors. 1998;40:254–76. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Module 4.1
Medication management with optimal use of IT


