Abstract
Aims
The aim of the present study was to assess the pharmacokinetics of total and unbound ceftriaxone in intensive care unit (ICU) patients and its protein binding characteristics.
Methods
Twenty patients (m/f 15/5, age 25–86 years, body weight 60–121 kg, APACHE II 7–40, estimated glomerular filtration rate 19–157 ml min–1, albumin 11.7–30.1 g l–1, total bilirubin <0.1–36.1 mg dl–1) treated with intravenous ceftriaxone were recruited from two ICUs. Timed plasma samples were obtained using an opportunistic study protocol. Ceftriaxone concentrations were determined by high-performance liquid chromatography; unbound concentrations were determined after ultrafiltration using a new method which maintains physiological pH and temperature. The pharmacokinetics was described by a one-compartment model, the protein-binding characteristics by Michaelis–Menten kinetics.
Results
For total drug, the volume of distribution was 20.2 l (median; interquartile range 15.6–24.5 l), the half-life 14.5 h (10.0–25.5 h) and the clearance 0.96 l h–1 (0.55–1.28 l h–1). The clearance of unbound drug was 1.91 l h–1 (1.46–6.20 l h–1) and linearly correlated with estimated glomerular filtration rate (slope 0.85, y-intercept 0.24 l h–1, r2 = 0.70). The unbound fraction was higher in ICU patients (33.0%; 20.2–44.5%) than reported in healthy volunteers, particularly when renal impairment or severe hyperbilirubinaemia was present. In all patients, unbound concentrations during treatment with ceftriaxone 2 g once daily remained above the EUCAST susceptibility breakpoint (≤1 mg l–1) throughout the whole dosing interval.
Conclusions
Protein binding of ceftriaxone is reduced and variable in ICU patients due to hypoalbuminaemia, but also to altered binding characteristics. Despite these changes, the pharmacokinetics of unbound ceftriaxone is governed by renal function. For patients with normal or reduced renal function, standard doses are sufficient.
Keywords: albumin, cystatin C, dosing, HPLC, pharmacodynamics, ultrafiltration
WHAT IS ALREADY KNOWN ABOUT THIS SUBJECT
Critical illness can influence the pharmacokinetics of many drugs.
This may include the protein binding of highly bound drugs such as ceftriaxone.
It is assumed that this leads to high drug clearance, low plasma concentrations and therapeutic failure.
WHAT THIS STUDY ADDS
Protein binding of ceftriaxone is reduced in intensive care unit (ICU) patients, not only because of hypoalbuminaemia.
This does not impair the attainment of the pharmacokinetic/pharmacodynamic target ƒT>MIC.
Plasma albumin concentrations and in vitro binding data from healthy volunteers cannot be used to predict unbound concentrations of ceftriaxone correctly in ICU patients.
Introduction
The pharmacokinetic properties of many drugs can be severely altered in special populations such as intensive care unit (ICU) patients [1]. Expansion of the extracellular space by aggressive fluid resuscitation and dysfunction of the eliminating organs are probably the most important factors, but changes in plasma protein binding may also contribute [2]. Although the worldwide spread of extended-spectrum beta-lactamase-producing Enterobacteriaceae has somewhat limited its usefulness, ceftriaxone has still many indications, mainly in the treatment of severe community-acquired infections such as pneumonia, meningitis or intra-abdominal infections.
A particular feature of ceftriaxone is its long elimination half-life due to extensive binding to plasma proteins [3]. Both elimination and antimicrobial activity are limited to the small unbound fraction of the drug. As the relevant pharmacokinetic/pharmacodynamic (PK/PD) index of beta-lactams such as ceftriaxone is the cumulative percentage of a 24-h period that the free/unbound drug concentration exceeds the minimal inhibitory concentration (MIC) at steady state (ƒT>MIC) [4], this behaviour may be advantageous because sustained concentrations above the MIC are preferable to a high peak and then rapidly decreasing concentrations. Direct determination of unbound concentrations is technically demanding and often not carried out. An alternative is determination of total concentrations, and calculation of unbound concentrations using either fixed or model-predicted ratios [5]. However, this approach is most problematic in a special population like critically ill patients when data on protein binding are imputed from healthy volunteers or even preclinical models [6], as the observation of low total concentrations and the assumption of a low unbound fraction (as in healthy volunteers) may erroneously lead to the conclusion that unbound concentrations are insufficient.
In recent works, we demonstrated that inconsistencies reported on unbound drug concentrations of vancomycin and ertapenem are partially due to technical shortcomings of the methods employed [7,8]. We developed a robust ultrafiltration method, which was also validated in vitro for ceftriaxone [9]. In the present study, we applied this method to describe the plasma pharmacokinetics of unbound ceftriaxone and its protein-binding characteristics in ICU patients.
Methods
Patients and clinical samples
The present study included patients from a medical ICU at the University Hospital Regensburg, Germany, and from the surgical ICU of the Charité Universitätsmedizin Berlin – Campus Benjamin Franklin, Berlin, Germany. Both ICUs provide tertiary care and have a focus on gastroenterology, hepatology and infectious diseases (Regensburg), and patients undergoing major general surgery or neurosurgery (Berlin), but basically admit all kinds of patients who require intensive care. The ethics committees responsible gave approval for anonymized analysis of blood samples obtained in the course of the treatment (Regensburg: 98/35; Berlin: EA4/028/13). We used the remains of plasma samples from standard clinical care for blood gas analysis from a point-of-care testing system. Patients or their legal representatives consented to such use in the medical treatment contract (Berlin), or gave informed consent to participate in this study (Regensburg). Clinical data and the dosing history were collected from the patient files prior to anonymization. In both ICUs, ceftriaxone is usually administered as short infusion over 30 min. If no differing period had been documented, this value was used for pharmacokinetic calculations. Eligible patients were identified by periodical chart review of all patients in the ICU. Age ≥18 years and treatment with ceftriaxone were the only inclusion criteria; patients were excluded when renal replacement therapy was applied or when it did not appear feasible to obtain a sufficient number of samples (e.g. due to imminent discharge or death).
The sampling times were chosen opportunistically among available specimens, with the aim of capturing one or two dosing intervals, with three to four samples. Samples in the very early phase after the end of ceftriaxone infusion were deliberately avoided because these measurements might have been less robust and would anyway not have affected ƒT>MIC. Plasma was separated immediately by centrifugation, stored at –70 °C and shipped on dry ice to the laboratory for analysis. Because renal function is an important determinant of ceftriaxone clearance, cystatin C levels, in addition to creatinine levels, were determined for all patients, and used to estimate the glomerular filtration rate (GFR) according to Hoek (eCLHoek) [10]. Because creatinine production in ICU patients is often reduced owing to immobility and muscle wasting, this approach is considered to be more precise than creatinine-based estimations such as the popular Cockcroft–Gault formula (eCLCG) [11].
In total, 69 plasma samples from 20 ICU patients (median three samples per patient, range 1–6) treated with intravenous ceftriaxone 2 g once daily were collected. The number of plasma samples was insufficient (<3) for pharmacokinetic calculations in three patients, but could be used for the analysis of the binding characteristics. Patients' characteristics and laboratory data are described in Table 1. There is no policy to maintain albumin concentrations above a certain threshold, but six patients had received intravenous albumin (12.5–100 g) within the 72 h before plasma samples were obtained.
Table 1.
Characteristics and laboratory data of 20 intensive care unit patients [15 male (M), five female (F)] treated with ceftriaxone
| Patient | Indication, known liver disease | Sex | Age (years) | Weight (kg) | Height (cm) | APACHE II | SAPS II | Creatinine (mg dl–1) | Cystatin C (mg dl–1) | Total bilirubin (mg dl–1) | Albumin (g l–1) | eCLCG (ml min–1) | eCLHoek (ml min–1) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Prophylaxis (postoperative) | F | 27 | 90 | 165 | 15 | 33 | 0.71 | 0.66 | <0.1 | 25.5 | 169 | 134 |
| 2*,‡ | Prophylaxis (gastrointestinal bleeding) | M | 72 | 95 | 175 | 25 | 21 | 8.8 | 3.65 | 0.3 | 21.0 | 10 | 22 |
| 3*,‡ | Community-acquired pneumonia | F | 73 | 75 | 167 | 11 | 26 | 1.56 | 2.01 | 0.2 | 22.7 | 38 | 38 |
| 4 | Infection of unknown origin | M | 54 | 100 | 175 | 8 | 9 | 1.11 | 0.88 | 0.4 | 24.8 | 108 | 108 |
| 5† | Prophylaxis (gastrointestinal bleeding), liver cirrhosis | F | 60 | 60 | 163 | 18 | 27 | 0.77 | 1.13 | 26.5 | 22.4 | 74 | 63 |
| 6* | Prophylaxis (gastrointestinal bleeding) | M | 59 | 103 | 188 | 13 | 8 | 5.43 | 2.47 | 0.4 | 21.4 | 21 | 37 |
| 7* | Prophylaxis (gastrointestinal bleeding) | M | 86 | 80 | 160 | 12 | 11 | 1.65 | 1.79 | 0.2 | 24.6 | 36 | 43 |
| 8* | Nosocomial pneumonia | M | 78 | 72 | 180 | 31 | 28 | 2.63 | 3.79 | 1.3 | 17.2 | 24 | 19 |
| 9*,† | Urosepsis, primary sclerosing cholangitis | M | 25 | 70 | 184 | 12 | 31 | 1.64 | 2.48 | 36.1 | 18.1 | 68 | 31 |
| 10 | Prophylaxis (gastrointestinal bleeding) | M | 65 | 98 | 186 | 7 | 9 | 0.76 | 0.77 | 0.7 | 27.0 | 134 | 129 |
| 11*,‡ | Infection of unknown origin | M | 65 | 121 | 166 | 27 | 19 | 1.87 | 2.6 | 1.9 | 23.4 | 67 | 34 |
| 12* | Endocarditis | M | 74 | 80 | 170 | 22 | 5 | 4.55 | 2.4 | 0.2 | 19.9 | 16 | 32 |
| 13*,‡,† | Urosepsis, liver cirrhosis | M | 61 | 80 | 180 | 12 | 5 | 3.14 | 2.54 | 24.8 | 30.1 | 28 | 32 |
| 14‡ | Urosepsis | M | 63 | 90 | 190 | 34 | 19 | 0.79 | 0.81 | 1.0 | 27.0 | 122 | 120 |
| 15 | Secondary peritonitis | F | 84 | 76 | 156 | 16 | 37 | 0.45 | 0.86 | 0.3 | 13.6 | 112 | 91 |
| 16* | Secondary peritonitis | M | 65 | 70 | 176 | 19 | 43 | 3.21 | 2.05 | 0.7 | 11.7 | 23 | 37 |
| 17* | Nosocomial pneumonia | M | 73 | 90 | 180 | 40 | 78 | 3.79 | 2.39 | 0.7 | 15.5 | 22 | 36 |
| 18‡,†§ | Spontaneous bacterial peritonitis, liver cirrhosis | M | 29 | 95 | 183 | 15 | 16 | 0.55 | 0.62 | 19.4 | 24.5 | 266 | 157 |
| 19§ | Prophylaxis (gastrointestinal bleeding) | M | 77 | 74 | 174 | 19 | 16 | 1.03 | 0.96 | 0.2 | 28.5 | 63 | 86 |
| 20§ | Bacterial tracheobronchitis | F | 58 | 64 | 170 | 25 | 27 | 0.57 | 0.55 | 0.2 | 16.2 | 109 | 143 |
| Median | 65 | 80 | 175 | 17 | 20 | 1.60 | 1.90 | 0.55 | 22.6 | 65 | 40 | ||
| Minimum | 25 | 60 | 156 | 7 | 5 | 0.45 | 0.55 | <0.1 | 11.7 | 10 | 19 | ||
| Maximum | 86 | 121 | 190 | 40 | 78 | 8.80 | 3.79 | 36.1 | 30.1 | 266 | 157 |
Renal impairment (CLHoek<60 ml min–1);
severe hyperbilirubinaemia (>15 mg dl–1);
intravenous administration of albumin within the last 72 h before plasma samples were obtained;
insufficient data for pharmacokinetic analysis – binding studies only. APACHE II, Acute Physiology and Chronic Health Evaluation II; SAPS II, Acute Physiology and Chronic Health Evaluation II.
Analysis of ceftriaxone
Total plasma concentrations of ceftriaxone were determined by adapting previously described validated high-performance liquid chromatography (HPLC) methods for total [12] or unbound [13] ceftriaxone. Sample preparation for total ceftriaxone included protein precipitation with acetonitrile and a wash step with dichloromethane. The chromatographic system and determination of unbound ceftriaxone is described elsewhere [9]. Briefly, plasma was buffered to pH ∼7.4 and ultrafiltered at 1000 g for 20 min at 37 °C using Nanosep Omega 10K filters (VWR, Ismaning, Germany). For total ceftriaxone, linearity has been demonstrated in spiked plasma from healthy volunteers between 1 and 300 mg l–1, and the coefficient of variation (CV) for intra- and inter-assay precision and accuracy was <4% over the whole range. From the lower limit of detection of 30 pg ceftriaxone injected onto the column, a lower limit of quantification of 0.1 mg l–1 total ceftriaxone can be estimated (signal/noise 6/1, injection volume 2 µl). For unbound ceftriaxone, the inter-assay precision of the determination was between 5.5% (300 mg l–1 total ceftriaxone) and 13% (1 mg l–1 total ceftriaxone). The intra-assay precision was about 1% in preliminary experiments, and accordingly was not implemented into the further validation procedure. The CV of intra- and inter-assay precision and accuracy for total ceftriaxone was <4% based on quality control samples (100 mg l–1, 10 mg l–1) incorporated into each run of patient samples (n = 4 runs). The CV of inter-assay precision for unbound ceftriaxone was 5% at 100 mg l–1 and 17% at 10 mg l–1 total ceftriaxone (n = 3 runs). An interfering peak (shoulder) was observed in one patient at the standard detection wavelength of 260 nm. Therefore, quantification was performed at 300 nm, where the signal height was one-third, but the assay still sufficiently sensitive.
Protein-binding studies
The in vitro protein binding of ceftriaxone was characterized in pooled plasma from six healthy volunteers (albumin concentration 42.8 g l–1). Plasma was buffered with 3% (v/v) 3 mol l–1 potassium phosphate, pH 7.5, and spiked with 5% aqueous ceftriaxone solution to obtain final concentrations of 1, 3, 10, 30, 100, 300 and 1000 mg l–1. The sample was then incubated in the preheated centrifuge for 10 min prior to ultrafiltration [9]. In a second experiment, plasma was diluted with an equal volume of saline and processed analogously. Analysis of unbound ceftriaxone was carried out as described above. Protein binding of ceftriaxone was assessed using a Scatchard plot and Michaelis–Menten kinetics. Molar concentrations were calculated from mass concentrations with a molar weight of 554.58 g mol–1 for ceftriaxone and 66,000 g mol–1 for albumin. Because of previous reports of higher unbound concentrations in patients with severe hyperbilirubinaemia or with renal impairment [14–17], patients were analysed separately according to the presence of these conditions (total bilirubin >15 mg dl–1, CLHoek <60 ml min–1).
Pharmacokinetic and statistical analysis
The pharmacokinetics of total and unbound concentrations were analysed separately by fitting a one-compartment model (zero-order input, first-order elimination) with 1/y2 weighting using Phoenix WinNonlin 6.3 (Pharsight/Certara, St Louis, MO, USA). The pharmacokinetic parameters obtained were then used to simulate a full plasma concentration–time course of unbound ceftriaxone for each patient until day 6 of treatment (2 g once daily, infused over 30 min). It was assumed that steady state would be attained after that time, even in patients with a long half-life of about 24 h. Additionally, three virtual patients were simulated to illustrate the influence of changes in the volume of distribution on the concentration–time course and ƒT>MIC. A clearance of 6 l h–1 (representing normal renal function) and volumes of distribution of 20, 50 and 100 l (referring to the values for unbound drug) were chosen, thus covering a greater range than observed among the patients in the present study (24.1–84.2 l).
Prism 6.0f for MacOSX (GraphPad Software, La Jolla, CA, USA) was used for calculating statistics and Michaelis–Menten kinetics. For regression analysis, 1/y2 weighting was applied. Nonparametric [median, range, interquartile range (IQR), percentiles] or parametric (mean, confidence interval) descriptive statistics are provided, as appropriate.
Results
Pharmacokinetics
The concentration–time courses of both total and unbound ceftriaxone could be described adequately by the one-compartment model in 17 patients, as demonstrated by the good agreement between predicted and observed concentrations (Figure1). The pharmacokinetic parameters derived are listed in Table 2. The clearance of total ceftriaxone was weakly correlated with renal function markers (eCLCG: r2 = 0.27; eCLHoek: r2 = 0.18), whereas the clearance of unbound ceftriaxone showed an acceptable to good correlation (eCLCG: r2 = 0.49; eCLHoek: r2 = 0.70). The regression equation for the clearance of unbound ceftriaxone on eCLHoek was CL = 0.85 × eCLHoek + 0.24 l h–1.
Figure 1.
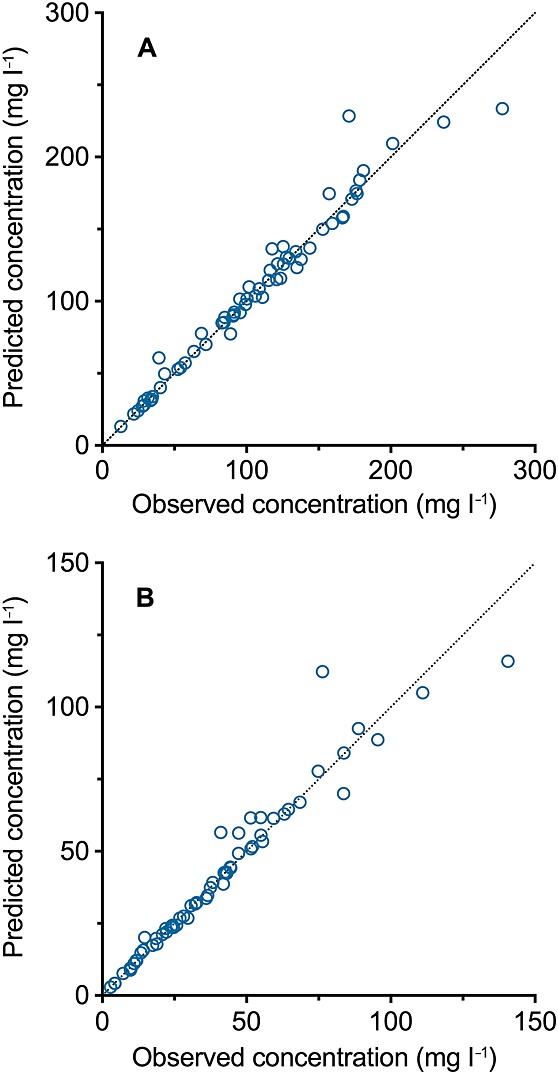
Agreement between observed concentrations and those predicted by a one-compartment model for (A) total ceftriaxone and (B) unbound ceftriaxone
Table 2.
Pharmacokinetic parameters of total and unbound ceftriaxone in 17 intensive care unit patients
| Total drug | Unbound drug | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Patient | Vss (l) | CL (l h–1) | CL/CLHoek | t1/2 (h) | Vss (l) | CL (l h–1) | CL/CLHoek | t1/2 (h) | Unbound fraction‡ average (range) |
| 1 | 10.4 | 1.06 | 0.13 | 6.8 | 47.7 | 6.85 | 0.85 | 4.8 | 15.4% (13.8–20.4%) |
| 2* | 23.5 | 0.54 | 0.41 | 30.4 | 62.8 | 1.77 | 1.37 | 24.6 | 30.3% (30.8–33.7%) |
| 3* | 20.2 | 0.46 | 0.20 | 30.3 | 28.6 | 1.21 | 0.53 | 16.5 | 38.3% (29.9–46.9%) |
| 4 | 16.1 | 1.28 | 0.20 | 8.7 | 79.1 | 7.60 | 1.17 | 7.2 | 16.9% (13.1–19.7%) |
| 5† | 20.0 | 0.95 | 0.25 | 14.5 | 34.1 | 1.79 | 0.47 | 13.2 | 53.4% (43.0–62.0%) |
| 6* | 21.0 | 0.53 | 0.23 | 27.7 | 41.3 | 2.15 | 0.96 | 13.3 | 24.5% (23.3–35.9%) |
| 7* | 13.5 | 0.68 | 0.26 | 13.7 | 46.5 | 3.16 | 1.22 | 10.2 | 21.6% (17.3–24.9%) |
| 8* | 14.2 | 0.52 | 0.47 | 18.8 | 24.1 | 1.19 | 1.07 | 14.0 | 44.0% (37.8–50.7%) |
| 9*,† | 33.4 | 1.68 | 0.90 | 13.8 | 35.6 | 1.86 | 1.00 | 13.3 | 90.2% (84.4–96.8%) |
| 10 | 15.0 | 1.09 | 0.14 | 9.5 | 66.5 | 6.24 | 0.81 | 7.4 | 17.6% (13.0–20.2%) |
| 11* | 17.8 | 0.57 | 0.27 | 21.8 | 49.8 | 1.37 | 0.66 | 25.3 | 41.5% (35.7–44.1%) |
| 12* | 21.2 | 0.63 | 0.33 | 23.3 | 42.2 | 1.91 | 0.99 | 15.3 | 33.0% (26.8–37.3%) |
| 13*,† | 28.0 | 1.00 | 0.53 | 19.5 | 31.2 | 1.38 | 0.73 | 15.6 | 72.0% (61.0–82.8%) |
| 14 | 19.4 | 1.28 | 0.18 | 10.5 | 84.2 | 6.84 | 0.95 | 8.5 | 18.7% (15.0–20.8%) |
| 15 | 21.5 | 1.81 | 0.33 | 8.2 | 58.0 | 6.17 | 1.13 | 6.5 | 29.4% (21.7–37.4%) |
| 16* | 30.7 | 0.61 | 0.27 | 35.0 | 63.6 | 1.54 | 0.69 | 28.6 | 39.5% (43.3–46.8%) |
| 17* | 25.5 | 1.45 | 0.68 | 12.2 | 40.3 | 3.22 | 1.51 | 8.7 | 44.9% (34.2–56.0%) |
| Median | 20.2 | 0.96 | 0.27 | 14.5 | 46.5 | 1.91 | 0.96 | 13.3 | 33.0% (34.2%)§ |
| p25 | 15.6 | 0.55 | 0.20 | 10.0 | 34.9 | 1.46 | 0.71 | 8.0 | 20.2% (21.3%)§ |
| p75 | 24.5 | 1.28 | 0.44 | 25.5 | 63.2 | 6.20 | 1.15 | 16.0 | 44.5% (46.5%)§ |
Renal impairment (CLHoek<60 ml min–1);
severe hyperbilirubinaemia (>15 mg dl–1);
the average unbound fraction was calculated as the ratio of the calculated CL of total drug and unbound drug, whereas the range is provided for the values actually observed among the available plasma samples (not necessarily within a certain concentration range);
median, 25th and 75th percentile of all observed values. CL, clearance; CLHoek, glomerular filtration rate estimated from cystatin C, according to Hoek; p25, 25th percentile; p75, 75th percentile; t1/2, half-life; Vss, volume of distribution in steady state.
The simulated concentration–time courses of unbound ceftriaxone for days 1 and 6 of treatment are shown in Figure2. All but one patient (patient 1) showed unbound trough concentrations >2 mg l–1 (the resistance breakpoint for Enterobacteriaceae and Streptococcus pneumoniae according to European Committee on Antimicrobial Susceptibility Testing (EUCAST)), and >8 mg l–1 (4 × the breakpoint) at the mid-dosing interval. Virtual patients demonstrate clearly that a high volume of distribution has a favourable effect on ƒT>MIC. A patient with a high volume of distribution (100 l) would have low peak concentrations (20–25 mg l–1), but maintain unbound concentrations >4 mg l–1 throughout the whole dosing interval (even after the first dose). By contrast, with a low volume of distribution (20 l), peak concentrations would be very high (∼90 mg l–1), but even an MIC of ≤1 mg l–1 (the susceptibility breakpoint for Enterobacteriaceae) would be exceeded only for two-thirds of the dosing interval.
Figure 2.
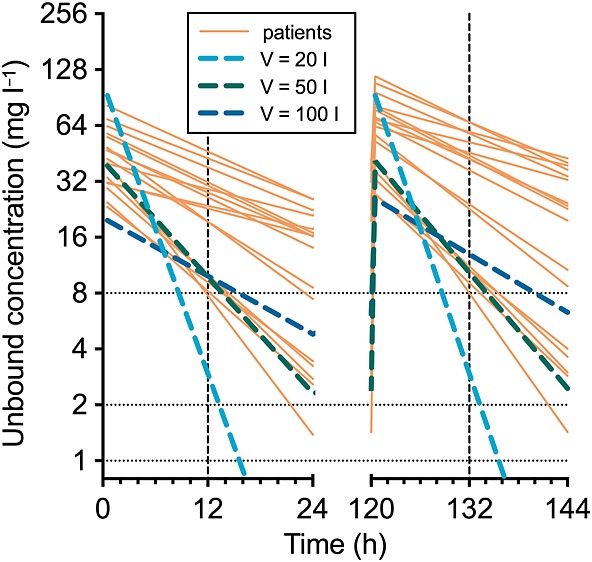
Simulated concentration–time courses of unbound ceftriaxone in 17 intensive care unit patients on days 1 and 6 of therapy (2 g i.v. once daily over 30 min), and in three virtual patients with a clearance of 6 l h–1 and a varying volume of distribution (V). Vertical reference line: mid-interval; horizontal reference lines: susceptibility (≤1 mg l–1), resistance (>2 mg l–1) and 4 × resistance (>8 mg l–1) breakpoints for Enterobacteriaceae according to European Committee on Antimicrobial Susceptibility Testing (EUCAST)
Plasma protein binding
In spiked plasma from healthy volunteers, the unbound fraction was 6–10% at total concentrations below 100 mg l–1, and increased to 65% at 1000 mg l–1 (Figure3). In plasma from ICU patients, the same trend was visible, but unbound fractions were generally much higher. The highest values of about 90% were observed in samples of a patient (patient 9) with severe hyperbilirubinaemia. Among patients with normal bilirubin, those with renal impairment (CLHoek<60 ml min–1) had higher unbound fractions (median 35.9%; IQR 31.1–44.1%; n = 9) than patients with normal renal function (19.5%; 14.7–25.1%; n = 7). Only one slope was apparent in the Scatchard plot for plasma from healthy volunteers, corresponding to one relevant binding site in the investigated concentration range (Figure4). Accordingly, the binding characteristics of ceftriaxone to albumin were described by Michaelis–Menten kinetics (Figure5). The binding curve for plasma from ICU patients without renal impairment was nearly superimposable with that for healthy volunteers. Both affinity and maximal binding capacity were somewhat reduced in patients with renal impairment, and severely reduced in patients with hyperbilirubinaemia (Table 3).
Figure 3.
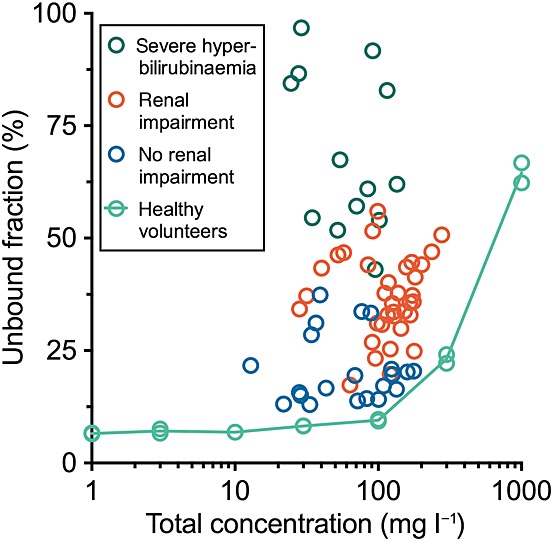
Unbound fraction vs. total concentration of ceftriaxone in plasma from healthy volunteers and from intensive care unit patients
Figure 4.
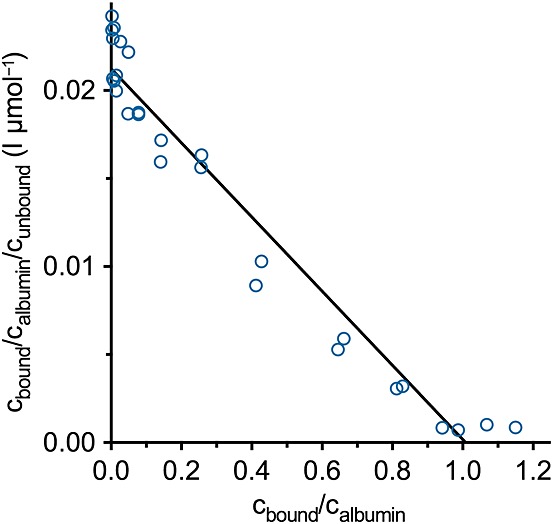
Scatchard plot of ceftriaxone binding in plasma from healthy volunteers. cbound, cunbound, calbumin: molar concentrations of bound and unbound ceftriaxone and of albumin
Figure 5.
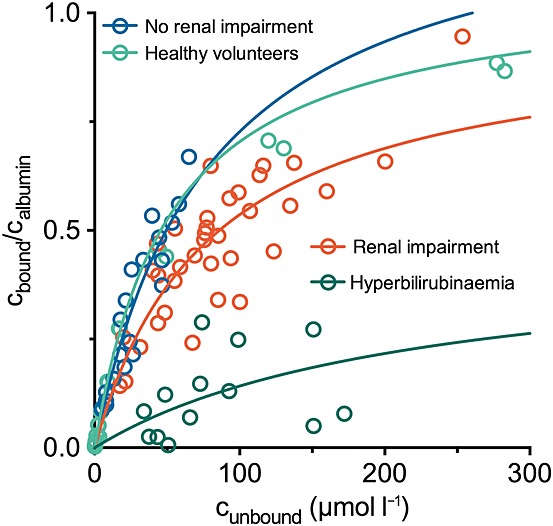
Michaelis–Menten analysis of ceftriaxone binding to plasma from healthy volunteers and intensive care unit patients. cbound, cunbound, calbumin: molar concentrations of bound and unbound ceftriaxone and of albumin
Table 3.
Protein binding characteristics, of ceftriaxone in plasma, normalized to albumin, according to Michaelis–Menten kinetics
| n | kd (µmol l–1) | |||||
|---|---|---|---|---|---|---|
| N | r2 | PE | CI95 | PE | CI95 | |
| Healthy volunteers | 28/* | 0.972 | 1.07 | 0.940–1.20 | 51.8 | 43.7–59.8 |
| Intensive care unit patients | ||||||
| – With normal bilirubin | 56/16 | 0.877 | 0.806 | 0.670–0.941 | 46.4 | 31.7–61.1 |
| – Without renal impairment | 21/7 | 0.907 | 1.31 | 0.588–2.02 | 79.5 | 22.7–136 |
| – With renal impairment | 35/9 | 0.787 | 0.962 | 0.693–1.23 | 79.3 | 38.1–121 |
| – With hyperbilirubinaemia | 13/4 | 0.262 | 0.458 | –1.13–2.05 | 222 | 0–1256 |
Pooled plasma from six healthy volunteers; four independent experiments with seven concentrations each. CI95, 95% confidence interval; kd, dissociation constant; n, maximum binding capacity per albumin molecule; N, number of analysed data points/number of patients; PE, point estimate.
Discussion
In the present study, we report the pharmacokinetics of total and unbound ceftriaxone in 17 ICU patients. As a strength of this study, unbound concentrations were determined directly using a modern ultrafiltration method which has been validated in vitro [9]. Compared with equilibrium dialysis, which was used in older studies [14–18], this technique enables a plasma sample to be separated rapidly into a protein-free aqueous phase, which can be injected directly into the HPLC column. Accordingly, it has been suggested as a simple and fast method for therapeutic drug monitoring of beta-lactams [13]. However, we demonstrated recently that ultrafiltration is susceptible to experimental conditions such as centrifugal force, pH and temperature [7–9], the neglect of which may have contributed to some inconsistent results in the literature [19].
Previous, more extensive in vitro studies have demonstrated the presence of up to three binding sites for ceftriaxone in human plasma [20,21], and complex interactions with displacing drugs which involve conformational changes of the albumin molecule rather than direct competition [3]. Such detailed investigations were beyond the scope of the present study. The precise estimation of protein-binding parameters requires measurements up to very high concentrations, at which saturation is actually observed. These were obtained experimentally in spiked plasma from healthy volunteers (total concentration of 300 mg l–1 and 1000 mg l–1), but were not observed in the clinical samples. Additionally, the statistical interpretation of the data was limited by the small number of patients and by the variable number of data points per patient. However, the presented results illustrate nicely how critical illness can affect the unbound concentration of drugs. Whereas the binding characteristics in patients without severe hyperbilirubinaemia and renal impairment were fairly homogeneous (evidenced by r2 = 0.907 of the model fit) and resembled closely those from healthy volunteers, renal impairment, and, most of all, severe hyperbilirubinaemia, had a strong inhibiting effect on protein binding beyond hypoalbuminaemia (which is corrected for in the Scatchard and Michaelis–Menten analysis). Similar observations have been made previously in vitro in uraemic plasma [22], in patients with acute renal failure [16,17] and in functionally anephric patients [14], as well as in patients with chronic liver disease [15]. Whereas competitive binding of bilirubin and ceftriaxone has been demonstrated [23], only one patient in the former study [15] had severe hyperbilirubinaemia. This means that both renal and hepatic insufficiency are associated with reduced protein binding of ceftriaxone, but the exact mechanisms are probably complex and difficult to predict in an individual patient. This compromises any attempt to calculate unbound concentrations in ICU patients from total concentrations using in vitro binding data from healthy volunteers [5,19].
In an often-cited paper, Benet and Hoener argue convincingly that – with rare exceptions – 'changes in plasma protein binding have little clinical relevance' [24], and cite ceftriaxone as one of the drugs 'for which changes in protein binding have been [erroneously] thought to be important'. In short, initially higher unbound concentrations due to an acute elevation of the unbound fraction are rapidly counteracted by the higher amount of drug cleared from the plasma. In the end, the exposure to unbound drug (in terms of area under the curve) depends only on the clearance of unbound drug, which depends e.g. on renal function but not on the unbound fraction. Accordingly, we observed a linear correlation between the clearance of unbound ceftriaxone and the GFR estimated from plasma cystatin C by the Hoek formula. The high slope (0.85) and the low y-intercept (0.24 l h–1) indicate that dose adjustments proportional to renal function may become necessary, whereas the unbound fraction is irrelevant, as predicted by Benet and Hoener [24]. In the present study, the five patients with the highest eCLHoek (91–134 ml min–1) had the lowest unbound trough concentrations (1.43–4.02 mg l–1), but these were still above the EUCAST susceptibility breakpoint. Only for patients with a further elevated glomerular filtration ('augmented renal clearance' [25]), a higher dose or, preferably, a shorter dosing interval seem advisable.
Changes in the volume of distribution due to altered protein binding can occur if the unbound fraction in plasma and in tissue changes differently [24]. In comparison to studies in healthy volunteers [26,27], the volume of distribution of total drug in the present study was about twice as high (∼20 l compared with ∼10 l), which is in good agreement with results from other studies in critically ill patients [5,17]. Such increased volumes of distribution have been described for many antibiotics with predominantly extracellular distribution [1], including agents with minimal protein binding [28,29], and must therefore be attributed to other factors, e.g. expansion of the extracellular space by fluid administration and oedema formation. For a beta-lactam such as ceftriaxone, a higher volume of distribution might even have a favourable effect on the plasma concentration–time profile during steady state, because lower peak concentrations are presumably without relevance, whereas a longer half-life and higher trough concentrations increase the decisive PK/PD index ƒT>MIC.
Several limitations of the present study should be mentioned. First, the sample size of 20 ICU patients prevents generalizability and extrapolation to different patient groups. No patients with augmented renal clearance were present, which has recently been identified as an important cause for subtherapeutic concentrations of beta-lactam antibiotics [30]. Secondly, the study protocol was generic, and did not follow a specific time schedule. In addition, urine was not collected, which would have allowed a better quantification of renal function (by measuring the endogenous creatinine clearance) and the separate determination of the renal clearance of ceftriaxone. The pharmacokinetic analysis was limited to a simple one-compartment model, although more complex models and nonlinear kinetics (due to the saturable protein binding) have been described for ceftriaxone [5,18]. However, unbound ceftriaxone is responsible for the antibacterial activity and is best described by linear pharmacokinetics [18]. The pharmacokinetics of total ceftriaxone is actually nonlinear [18], but the error may be sufficiently small to permit comparisons with other studies, particularly if these also used linear models and (mostly) the same dose of 2 g once daily [5,16,17]. Overall, we consider the study to provide a meaningful example of the successful application of ultrafiltration to determine unbound ceftriaxone concentrations in a clinically relevant study population.
To summarize, we used ultrafiltration to determine the unbound concentrations of ceftriaxone in plasma, and to describe the protein-binding characteristics and the plasma pharmacokinetics of ceftriaxone in ICU patients. In accordance with previous studies, the volume of distribution and the unbound fraction were elevated, the latter particularly in patients with renal impairment or severe hyperbilirubinaemia. Clearance of unbound ceftriaxone as the dominant pharmacokinetic parameter was proportional to renal function. In patients with normal or reduced renal function, the standard dose (2 g once daily) resulted in sufficient unbound plasma concentrations above the susceptibility breakpoint throughout the whole dosing interval.
Competing Interests
All authors have completed the Unified Competing Interest form at http://www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare no support from any organization for the submitted work, no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years and no other relationships or activities that could appear to have influenced the submitted work.
The authors wish to thank Sebastian G. Wicha, Dept. of Clinical Pharmacy and Biochemistry, Institute of Pharmacy, Freie Universität Berlin, Germany, for help with the analysis of the protein-binding characteristics, and Dr Carsten Gnewuch, Institute for Clinical Chemistry and Laboratory Medicine, University of Regensburg, Germany, for his cooperation. This work was funded by institutional sources only.
Contributors
Bernd Salzberger and Martin G. Kees were responsible for the study concept and design; Michael Schleibinger, Cathérine L. Steinbach, Christoph Töpper, Uwe Liebchen and Martin G. Kees for the acquisition of clinical data; Michael Schleibinger, Alexander Kratzer and Frieder Kees for the drug assays; Martin G. Kees for the pharmacokinetic and statistical analysis and drafting of the manuscript; and Michael Schleibinger, Cathérine L. Steinbach, Christoph Töpper, Alexander Kratzer, Uwe Liebchen, Frieder Kees and Bernd Salzberger for critical revision of the manuscript. All authors read and approved the final manuscript.
References
- 1.Roberts JA, Abdul-Aziz MH, Lipman J, Mouton JW, Vinks AA, Felton TW, Hope WW, Farkas A, Neely MN, Schentag JJ, Drusano G, Frey OR, Theuretzbacher U, Kuti JL. Individualised antibiotic dosing for patients who are critically ill: challenges and potential solutions. Lancet Infect Dis. 2014;14:498–509. doi: 10.1016/S1473-3099(14)70036-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roberts JA, Pea F, Lipman J. The clinical relevance of plasma protein binding changes. Clin Pharmacokinet. 2013;52:1–8. doi: 10.1007/s40262-012-0018-5. [DOI] [PubMed] [Google Scholar]
- 3.McNamara PJ, Trueb V, Stoeckel K. Ceftriaxone binding to human serum albumin: indirect displacement by probenecid and diazepam. Biochem Pharmacol. 1990;40:1247–53. doi: 10.1016/0006-2952(90)90390-7. [DOI] [PubMed] [Google Scholar]
- 4.Mouton JW, Dudley MN, Cars O, Derendorf H, Drusano GL. Standardization of pharmacokinetic/pharmacodynamic (PK/PD) terminology for anti-infective drugs: an update. J Antimicrob Chemother. 2005;55:601–7. doi: 10.1093/jac/dki079. [DOI] [PubMed] [Google Scholar]
- 5.Garot D, Respaud R, Lanotte P, Simon N, Mercier E, Ehrmann S, Perrotin D, Dequin PF, Le Guellec C. Population pharmacokinetics of ceftriaxone in critically ill septic patients: a reappraisal. Br J Clin Pharmacol. 2011;72:758–67. doi: 10.1111/j.1365-2125.2011.04005.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heuberger J, Schmidt S, Derendorf H. When is protein binding important? J Pharm Sci. 2013;102:3458–67. doi: 10.1002/jps.23559. [DOI] [PubMed] [Google Scholar]
- 7.Kees MG, Wicha SG, Seefeld A, Kees F, Kloft C. Unbound fraction of vancomycin in intensive care unit patients. J Clin Pharmacol. 2014;54:318–23. doi: 10.1002/jcph.175. [DOI] [PubMed] [Google Scholar]
- 8.Liebchen U, Kratzer A, Wicha SG, Kees F, Kloft C, Kees MG. Unbound fraction of ertapenem in intensive care unit patients. J Antimicrob Chemother. 2014;69:3108–11. doi: 10.1093/jac/dku226. [DOI] [PubMed] [Google Scholar]
- 9.Kratzer A, Liebchen U, Schleibinger M, Kees MG, Kees F. Determination of free vancomycin, ceftriaxone, cefazolin and ertapenem in plasma by ultrafiltration: impact of experimental conditions. J Chromatogr B. 2014;961:97–102. doi: 10.1016/j.jchromb.2014.05.021. [DOI] [PubMed] [Google Scholar]
- 10.Hoek FJ, Kemperman FAW, Krediet RT. A comparison between cystatin C, plasma creatinine and the Cockcroft and Gault formula for the estimation of glomerular filtration rate. Nephrol Dial Transpl. 2003;18:2024–31. doi: 10.1093/ndt/gfg349. [DOI] [PubMed] [Google Scholar]
- 11.Carlier M, Dumoulin A, Janssen A, Picavet S, Vanthuyne S, Eynde RV, Vanholder R, Delanghe J, Schoenmakere GD, Waele JJD, Hoste EAJ. Comparison of different equations to assess glomerular filtration in critically ill patients. Intensive Care Med. 2015;41:427–35. doi: 10.1007/s00134-014-3641-9. [DOI] [PubMed] [Google Scholar]
- 12.McWhinney BC, Wallis SC, Hillister T, Roberts JA, Lipman J, Ungerer JPJ. Analysis of 12 beta-lactam antibiotics in human plasma by HPLC with ultraviolet detection. J Chromatogr B. 2010;878:2039–43. doi: 10.1016/j.jchromb.2010.05.027. [DOI] [PubMed] [Google Scholar]
- 13.Briscoe SE, McWhinney BC, Lipman J, Roberts JA, Ungerer JPJ. A method for determining the free (unbound) concentration of ten beta-lactam antibiotics in human plasma using high performance liquid chromatography with ultraviolet detection. J Chromatogr B. 2012;907:178–84. doi: 10.1016/j.jchromb.2012.09.016. [DOI] [PubMed] [Google Scholar]
- 14.Stoeckel K, McNamara PJ, Hoppe-Seyler G, Blumberg A, Keller E. Single-dose ceftriaxone kinetics in functionally anephric patients. Clin Pharmacol Ther. 1983;33:633–41. doi: 10.1038/clpt.1983.86. [DOI] [PubMed] [Google Scholar]
- 15.Stoeckel K, Tuerk H, Trueb V, McNamara PJ. Single-dose ceftriaxone kinetics in liver insufficiency. Clin Pharmacol Ther. 1984;36:500–9. doi: 10.1038/clpt.1984.210. [DOI] [PubMed] [Google Scholar]
- 16.Heinemeyer G, Link J, Weber W, Meschede V, Roots I. Clearance of ceftriaxone in critical care patients with acute renal failure. Intensive Care Med. 1990;16:448–53. doi: 10.1007/BF01711224. [DOI] [PubMed] [Google Scholar]
- 17.Joynt GM, Lipman J, Gomersall CD, Young RJ, Wong EL, Gin T. The pharmacokinetics of once-daily dosing of ceftriaxone in critically ill patients. J Antimicrob Chemother. 2001;47:421–9. doi: 10.1093/jac/47.4.421. [DOI] [PubMed] [Google Scholar]
- 18.Stoeckel K, McNamara PJ, Brandt R, Plozza-Nottebrock H, Ziegler WH. Effects of concentration-dependent plasma protein binding on ceftriaxone kinetics. Clin Pharmacol Ther. 1981;29:650–7. doi: 10.1038/clpt.1981.90. [DOI] [PubMed] [Google Scholar]
- 19.Wong G, Briscoe S, Adnan S, McWhinney B, Ungerer J, Lipman J, Roberts JA. Protein binding of β-lactam antibiotics in critically ill patients: can we successfully predict unbound concentrations? Antimicrob Agents Chemother. 2013;57:6165–70. doi: 10.1128/AAC.00951-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Popick AC, Crouthamel WG, Bekersky I. Plasma protein binding of ceftriaxone. Xenobiotica. 1987;17:1139–45. doi: 10.3109/00498258709167406. [DOI] [PubMed] [Google Scholar]
- 21.Nerli B, Romanini D, Picó G. Structural specificity requirements in the binding of beta lactam antibiotics to human serum albumin. Chem Biol Interact. 1997;104:179–202. doi: 10.1016/s0009-2797(97)00024-0. [DOI] [PubMed] [Google Scholar]
- 22.Fiset C, Vallée F, LeBel M, Bergeron MG. Protein binding of ceftriaxone: comparison of three techniques of determination and the effect of 2-hydroxybenzoylglycine, a drug-binding inhibitor in uremia. Ther Drug Monit. 1986;8:483–9. [PubMed] [Google Scholar]
- 23.Fink S, Karp W, Robertson A. Ceftriaxone effect on bilirubin-albumin binding. Pediatrics. 1987;80:873–5. [PubMed] [Google Scholar]
- 24.Benet LZ, Hoener BA. Changes in plasma protein binding have little clinical relevance. Clin Pharmacol Ther. 2002;71:115–21. doi: 10.1067/mcp.2002.121829. [DOI] [PubMed] [Google Scholar]
- 25.Udy AA, Roberts JA, Boots RJ, Paterson DL, Lipman J. Augmented renal clearance: implications for antibacterial dosing in the critically ill. Clin Pharmacokinet. 2010;49:1–16. doi: 10.2165/11318140-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 26.Patel IH, Chen S, Parsonnet M, Hackman MR, Brooks MA, Konikoff J, Kaplan SA. Pharmacokinetics of ceftriaxone in humans. Antimicrob Agents Chemother. 1981;20:634–41. doi: 10.1128/aac.20.5.634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pollock AA, Tee PE, Patel IH, Spicehandler J, Simberkoff MS, Rahal JJ. Pharmacokinetic characteristics of intravenous ceftriaxone in normal adults. Antimicrob Agents Chemother. 1982;22:816–23. doi: 10.1128/aac.22.5.816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Marik PE. Aminoglycoside volume of distribution and illness severity in critically ill septic patients. Anaesth Intensive Care. 1993;21:172–3. doi: 10.1177/0310057X9302100206. [DOI] [PubMed] [Google Scholar]
- 29.Gonçalves-Pereira J, Póvoa P. Antibiotics in critically ill patients: a systematic review of the pharmacokinetics of β-lactams. Crit Care. 2011;15:R206. doi: 10.1186/cc10441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Udy AA, Varghese JM, Altukroni M, Briscoe S, McWhinney BC, Ungerer JP, Lipman J, Roberts JA. Subtherapeutic initial β-lactam concentrations in select critically ill patients: association between augmented renal clearance and low trough drug concentrations. Chest. 2012;142:30–9. doi: 10.1378/chest.11-1671. [DOI] [PubMed] [Google Scholar]


