Abstract
An intra-abdominal bronchogenic cyst (BC) is a very rare congenital anomaly caused by abnormal budding of the developing tracheobronchial tree. Intra-abdominal BCs are reported as retroperitoneal masses in most cases, many of which are located on the left side of the midline, the perigastric area, the left adrenal gland, or the superior body of the pancreas. Intra-abdominal BCs are frequently misdiagnosed due to the rarity, location, and variable cystic content. We report five patients with intra-abdominal BCs who underwent surgery in a single institution.
Keywords: Bronchogenic cyst, Pancreatic neoplasms, Retroperitoneal neoplasms, Cysts, Abdominal
INTRODUCTION
Bronchogenic cysts (BCs) are rare benign congenital anomalies caused by abnormal budding of the developing tracheobronchial tree within the primitive foregut during early embryogenesis.1 BCs are usually located in the pulmonary parenchyma or in the mediastinum. BCs can also occur outside of the thoracic cavity, including the skin, subcutaneous tissue, shoulder, and neck.1 However, intra-abdominal BCs are very rare, and in most cases, are reported as retroperitoneal masses. Only 51 cases of retroperitoneal BCs have been reported in the English literature. Indeed, intra-abdominal BCs are frequently misdiagnosed due to its rare occurrence.
We report the clinical, radiologic, surgical, and pathologic findings of five patients with intra-abdominal BCs who underwent surgery in our institution.
CASE
Five patients with intra-abdominal BCs who underwent surgery at the Samsung Medical Center in Seoul, Korea, between 2 May 2000 and 3 October 2008 were retrospectively reviewed. After the surgery, a histopathologic diagnosis of BC was established for all of the patients.
Patient 1
A 61-year-old male underwent total gastrectomy for gastric cancer in the cardia portion of the stomach. A 3.5×2-cm cyst was identified incidentally during surgery and included in the specimen.
Patient 2
A 62-year-old female underwent esophagogastroduodenoscopy for epigastric pain. She had chronic gastritis in the antrum of the stomach, and a mass suggestive of a gastric submucosal tumor was demonstrated at the esophagogastric junction during endoscopy. The mass was thought to be a neurogenic tumor based on the pre-operative computed tomography (CT) findings. She underwent a wedge resection of the stomach.
Patient 3
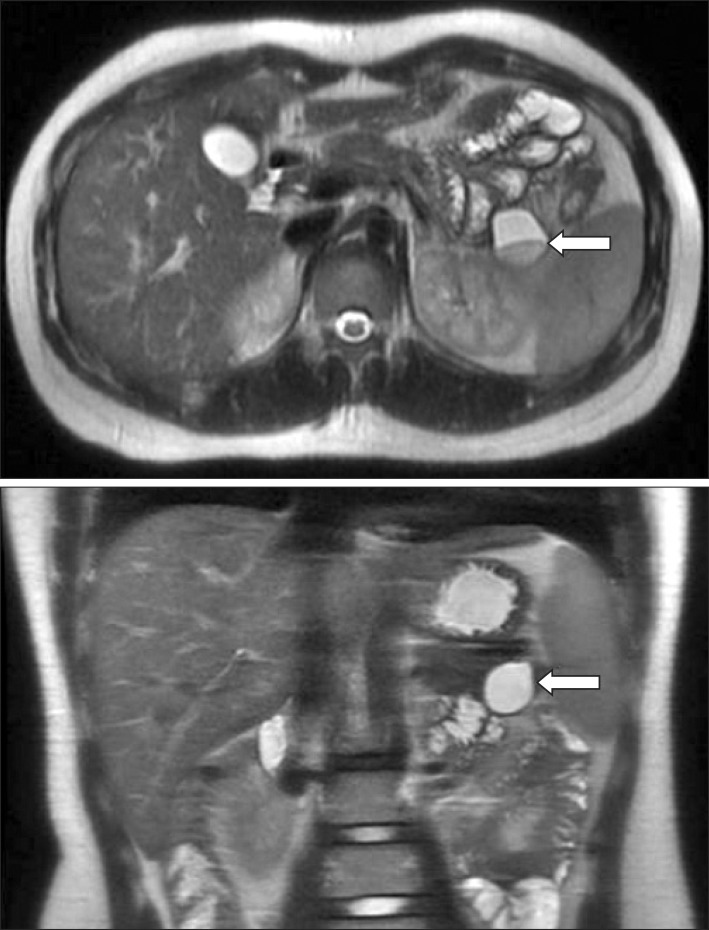
A 17-year-old male sought evaluation at the hospital due to right lower quadrant abdominal pain. A magnetic resonance image (MRI) revealed a tumor in the tail of the pancreas with an oligocyst or pseudocyst (Fig. 1). On CT, the tumor appeared to be a mucinous cystic tumor, solid pseudopaillary tumor, or a pseudocyst. The patient underwent a distal pancreatectomy.
Fig. 1. Magnetic resonance image (MRI), including vertical and horizontal sections. The cystic mass shows a fluid level and high-signal intensity on the T2-weighted image (arrows).
Patient 4
A 45-year-old female had intermittent abdominal discomfort. A CT revealed an 8-cm left adrenal gland tumor which was suggestive of a neurogenic tumor or lymphangioma. The tumor was excised. Four years after the surgery, she sought evaluation in the outpatient clinic for intermittent back pain. A CT scan was performed, but no abnormal findings were noted. The symptoms were relieved without intervention.
Patient 5
A 45-year-old female had a regular medical examination and a 3.6-cm tumor was noted incidentally between the tail of the pancreas and the stomach on CT which was consistent with a neurogenic tumor or lymphangioma (Fig. 2). Positron emission tomography was performed to rule out a malignancy. The mass had the appearance of a photon-defect lesion, which was consistent with a benign tumor. An endoscopic ultrasonographic fine-needle aspiration biopsy was performed, but was non-contributory with the exception of inflammatory cells in a proteinaceous background. She underwent excision of the tumor. The mass was 3.6 cm in size and consisted of a cyst, including turbid white fluid. Several episodes of blood pressure fluctuation occurred intra-operatively, but the surgery was completed without other complications. The pathologic diagnosis was shown to be a BC (Fig. 3).
Fig. 2. Computed tomography of the abdomen shows a circumscribed 3.6-cm cystic mass between the left adrenal gland and the distal pancreas (arrows). The mass was thin-walled, had a smooth margin, and was homogeneous.
Fig. 3. (A) Cut surface shows a unilocular cystic lesion (arrow) with focal yellow wall thickening (arrow head) containing serous, but turbid fluid. (B) Under light microscopic examination, the cystic lesion was shown to be lined by pseudostratified ciliated (respiratory) epithelium (inset; hematoxylin and eosin, ×200). (C) The focus of the thickened wall was shown to be a xanthogranulomatous inflammation with a collection of foamy histiocytes and lymphocytic infiltration (hematoxylin and eosin, ×200).
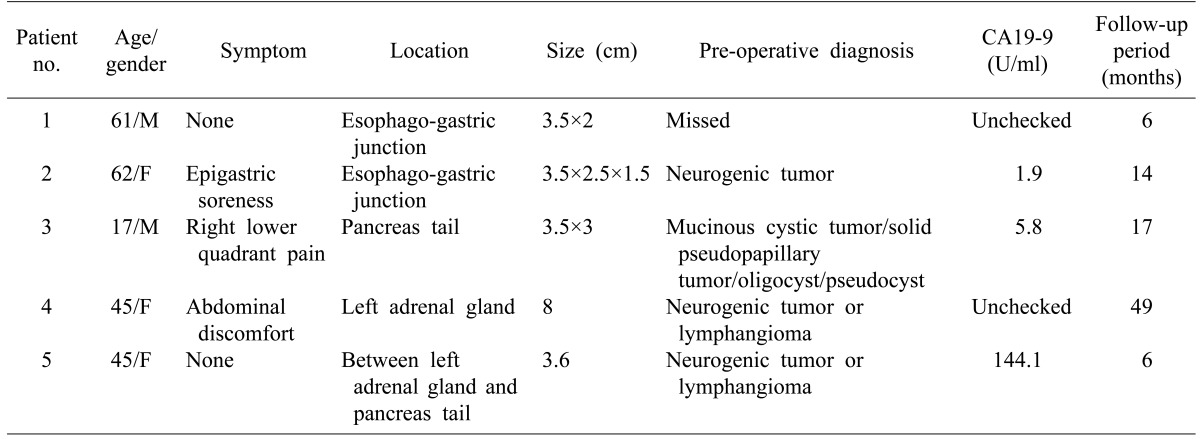
All patients were discharged uneventfully after surgery. There was no tumor recurrence during the follow-up period. The demographics and pre-operative diagnosis of each patient, including the imaging study findings and carbohydrate antigen 19-9 level, are presented in Table 1.
Table 1. Demographics and pre-operative diagnoses of each patient.
DISCUSSION
A BC is thought to be a foregut malformation.1 BCs arise from an abnormal budding of the tracheobronchial rudiment of the primitive foregut during the 3rd-7th weeks of embryologic development.1 When attachment to the primitive foregut persists, the cyst is usually associated with the tracheobronchial tree or the esophagus. If complete separation occurs, the cyst may occur in other unusual locations, presumably by migration.1 The subdiaphragmatic BC is extremely rare and accounts for 0.03% of all retroperitoneal tumors.2 The possible explanation for this condition is as follows: during the fusion of the pleura-peritoneal membranes, the abnormal budding of the tracheobronchial tree may be pinched off in the abdominal cavity.3 The subdiaphragmatic BC can be differentiated as intra or retro-peritoneal.
According to the largest review of cases, 76.5% of subdiaphragmatic BCs were located in the retroperitoneal space and 81% were located on the left side of the midline, perigastric area, left adrenal gland, or superior body of the pancreas.4 Our results are in agreement with previous reports with respect to location. These typical locations of BCs can lead to a misdiagnosis. The retroperitoneal space consists of many co-adjacent organs. Therefore, the exact location of the tumor can be easily confused with another condition, such as a gastric submucosal tumor, pancreatic cystic tumor, adrenal tumor, splenic tumor, enteric cyst, or retroperitoneal tumor.
Retroperitoneal BCs have been reported to occur in both genders equally, and in a wide age range.4 The reported average size of a BC is 5.72 cm, but can vary.4 Most patients with BCs have vague, non-specific abdominal symptoms.4 As more patients undergo routine medical evaluations, the incidental detection of BCs has correspondingly increased. However, large BCs can produce symptoms related to infections or compression of adjacent organs.1 Amongst our patients, three had atypical symptoms. Only patient #4 had symptoms associated with BCs.
Among the previously reported cases, there was a patient with a BC who had pheochromocytoma-like symptoms attributed to compression of the adrenal gland by the cyst with secondary release of catecholamines by the gland.5 Patient #5 had blood pressure fluctuations intra-operatively, but the relationship, if any, with the BC was not clear.
The CT images of sub-diaphragmatic BCs show sharply demarcated cystic masses with thin walls.4,6 CT attenuation of cystic content is water or soft-tissue attenuation according to the amount of protein-rich mucus (watery to a viscous fluid), and this is another factor which can cause confusion in the pre-operative diagnosis.4,6 MRI findings of BCs are described as a cystic mass slightly hyper or iso-intense to skeletal muscle on T1-weighted images.4,6 On T2-weighted images, most sub-diaphragmatic BCs present as cystic tumors hyper or iso-intense with cerebrospinal fluid.4,6 Despite these radiologic diagnostic features, the retroperitoneal BC is frequently confused with other types of retroperitoneal masses such as a lymphangioma, neuroendocrine tumor, mucinous cystic tumor, epidermoid cyst, or solid and pseudopapillary tumor. None of the patients in the current series were diagnosed with a BC based on radiologic modalities.
The identification of ciliated columnar epithelial cells in an endosonographically-guided fine needle aspiration biopsy is the only way to confirm a BC pre-operatively. However, it is very difficult to target the thin wall of a BC exactly. Therefore, in spite of a successful case using this method of diagnosis, an endosonographically-guided fine needle aspiration biopsy does not appear to be a reliable diagnostic test.7
The definitive diagnosis of a BC can be achieved histopathologically. The cyst wall is composed of pseudostratified ciliated columnar or cuboidal epithelium.1,6
The natural course is unknown, but the post-operative prognosis is good in patients with subdiaphragmatic BCs.4 Although most patients are asymptomatic, surgical excision is recommended to establish the diagnosis, treat any symptoms, and prevent complications. In addition, infections may occur and the rare but documented risk of malignant transformation exists.4,8 When a subdiaphragmatic BC is excised, less invasive surgery, such as enucleation or simple excision (rather than extensive excision), is suggested.
In summary, although subdiaphragmatic BCs are rare, a subdiaphragmatic BC should be considered in the differential diagnosis of a retroperitoneal mass, particularly in the case of a cystic tumor in the region of the distal pancreas, left adrenal gland, or upper portion of the stomach.
References
- 1.Coselli MP, de Ipolyi P, Bloss RS, et al. Bronchogenic cysts above and below the diaphragm: report of eight cases. Ann Thorac Surg. 1987;44:491–494. doi: 10.1016/s0003-4975(10)62106-6. [DOI] [PubMed] [Google Scholar]
- 2.Menke H, Röher HD, Gabbert H, et al. Bronchogenic cyst: a rare cause of a retroperitoneal mass. Eur J Surg. 1997;163:311–314. [PubMed] [Google Scholar]
- 3.Sumiyoshi K, Shimizu S, Enjoji M, et al. Bronchogenic cyst in the abdomen. Virchows Arch A Pathol Anat Histopathol. 1985;408:93–98. doi: 10.1007/BF00739965. [DOI] [PubMed] [Google Scholar]
- 4.Ubukata H, Satani T, Motohashi G, et al. Intra-abdominal bronchogenic cyst with gastric attachment: report of a case. Surg Today. 2011;41:1095–1100. doi: 10.1007/s00595-010-4398-6. [DOI] [PubMed] [Google Scholar]
- 5.Doggett RS, Carty SE, Clarke MR. Retroperitoneal bronchogenic cyst masquerading clinically and radiologically as a phaeochromocytoma. Virchows Arch. 1997;431:73–76. doi: 10.1007/s004280050071. [DOI] [PubMed] [Google Scholar]
- 6.Kim EY, Lee WJ, Jang KT. Retroperitoneal bronchogenic cyst mimicking a pancreatic cystic tumour. Clin Radiol. 2007;62:491–494. doi: 10.1016/j.crad.2006.10.012. [DOI] [PubMed] [Google Scholar]
- 7.Sato M, Irisawa A, Bhutani MS, et al. Gastric bronchogenic cyst diagnosed by endosonographically guided fine needle aspiration biopsy. J Clin Ultrasound. 2008;36:237–239. doi: 10.1002/jcu.20425. [DOI] [PubMed] [Google Scholar]
- 8.Sullivan SM, Okada S, Kudo M, et al. A retroperitoneal bronchogenic cyst with malignant change. Pathol Int. 1999;49:338–341. doi: 10.1046/j.1440-1827.1999.00869.x. [DOI] [PubMed] [Google Scholar]