Abstract
Backgrounds/Aims
We aimed to to evaluate the feasibility of laparoscopic common bile duct exploration (LCBDE) in patients with previous upper abdominal surgery.
Methods
Retrospective analysis was performed on data from the attempted laparoscopic common bile duct exploration in 44 patients. Among them, 5 patients with previous lower abdominal operation were excluded. 39 patients were divided into two groups according to presence of previous upper abdominal operation; Group A: patients without history of abdominal operation. (n=27), Group B: patients with history of upper abdominal operation. Both groups (n=12) were compared to each other, with respect to clinical characteristics, operation time, postoperative hospital stay, open conversion rate, postoperative complication, duct clearance and mortality.
Results
All of the 39 patients received laparoscopic common bile duct exploration and choledochotomy with T-tube drainage (n=38 [97.4%]) or with primary closure (n=1). These two groups were not statistically different in gender, mean age and presence of co-morbidity, mean operation time (164.5±63.1 min in group A and 134.8±45.2 min in group B, p=0.18) and postoperative hospital stay (12.6±5.7 days in group A and 9.8±2.9 days in group B, p=0.158). Duct clearance and complication rates were comparable (p>0.05). 4 cases were converted to open in group A and 1 case in group B respectively. In group A (4 of 27 (14.8%) and 1 of 12 (8.3%) in group B, p=0.312) Trocar or Veress needle related complication did not occur in either group.
Conclusions
LCBDE appears to be a safe and effective treatment even in the patients with previous upper abdominal operation if performed by experienced laparoscopic surgeon, and it can be the best alternative to failed endoscopic retrograde cholangiopancreatography for difficult cholelithiasis.
Keywords: Laparoscopic common bile duct exploration, Previous surgery
INTRODUCTION
Traditionally, the management of common bile duct (CBD) stones required open laparotomy and bile duct exploration which was first performed by Courvoisier and Thomton separately in 1889.1 Since the introduction of endoscopic retrograde cholangiopancreatography (ERCP) and endoscopic sphincterotomy (EST) in the 1970s, endoscopic management of CBD stones has gained popularity.2,3 After the introduction of laparoscopic cholecystectomy (LC) from France in 1987, the mainstream treatment of CBD stones with gallbladder stones is ERCP combined with LC.2,3 But, this is generally performed in two stages, which makes the patients uncomfortable not only in clinical but also in an economical respect. It also can result in the need for repeated procedures if it fails, and sometimes surgery is needed.
Recently, laparoscopic skills have developed quite rapidly. In the case of CBD stones, there are many reports involving laparoscopic procedures. Since the introduction of laparoscopic CBD exploration (LCBDE) in 1991, a single-stage approach without attempting ERCP has been suggested. These days, the majority of patients suffering from concomitant gallstones and CBD stones have been managed by a single-stage approach. It has been proven not only feasible but also effective in many reports. This procedure appears to be shorter hospital stay and a similar stone clearance rate, relative cost-effectiveness while preserving the function of the sphinter of Oddi and less ERCP-related complications.4,5 But, in cases with history of prior abdominal operation, the laparoscopic approach had potential difficulties - manipulation of instruments, potential risks of general anesthesia in patients who had medical problems, and technical demands.6,7,8,9,10,11
Previous abdominal surgery has been considered as a relative contraindication for laparoscopy.12,13,14 With development of surgical skills and instruments recently, the laparoscopic procedures were performed as a common treatment in CBD stones even in complicated cases. The usefulness of LCBDE has been reported with success rates in the range of 93.3-100% in general patients.12 The impact of previous abdominal operations on LC and urologic procedures has been studied, and the outcomes were not found to be affected by prior surgery.12,13,14,15,16 However, only a few reports about the impact of previous abdominal operations on LCBDE have been published. We aimed to evaluate the feasibility of LCBDE even in patients with previous abdominal surgery by a single surgeon who experienced LC from over 200 cases in patients with upper abdominal operations.
METHODS
Patients and grouping
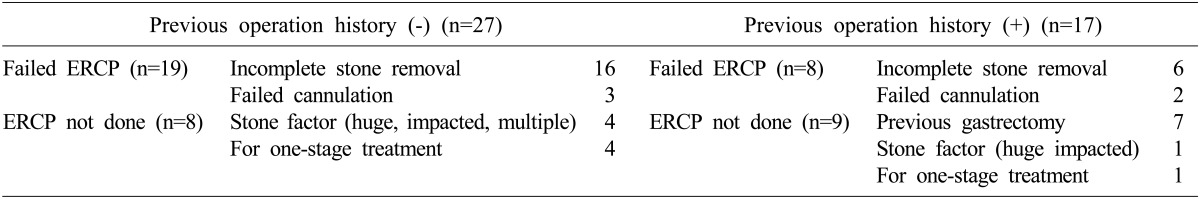
From December 2003 to March 2012, 44 patients with a diagnosis of CBD stone underwent LCBDE at the Department of Surgery, Boramae Medical Center, Seoul, Korea. All patients were diagnosed with abdominal computed tomography (CT), received ERCP or magnetic resonance cholangiopancreatography (MRCP), and informed about their health conditions. Among them, 27 patients were without history of previous abdominal surgery, while 17 patients had received various kinds of abdominal operation before. LCBDE were applied to (1) the patients with failed ERCP (n=27): incomplete stone removal (n=22), failed cannulation (n=5), and (2) the patients who did not have ERCP (n=17): stone factor (multiple, huge, impacted) (n=5), anatomic variation came from gastric resection (n=7), for one-stage treatment (n=5) (Table 1). Among them, we excluded the 5 patients with previous lower abdominal operations who did not meet the criteria in this study.
Table 1. Indications of laparoscopic common bile duct exploration.
We divided the remaining 39 patients into two groups; 27 patients without any history of previous abdominal operation were in Group A and 12 patients who underwent previous upper abdominal surgery were in Group B. Both groups were compared to each other with respect to their clinical characteristics (sex, age, body weight and co-morbidity), operation time, postoperative hospital stay, postoperative complication and conversion rate to open surgery.
Operation techniques
Under general anesthesia, the patient was laid in a 15 degree back up and 15 degree right tilt position. We used a four-trocar technique; 11-mm infra-umbilical port for laparoscope, one 11-mm port in subxiphoid for working port and future choledochoscope, one 5-mm port 5cm inferior to the right subcostal margin on the right midclavicular line, one 5 mm post on the right flank for assistance. If the previous incision scar was more than 3 cm far from the umbilicus, we used an infra-umbilical port, otherwise we made a camera port 3 cm right lateral to the umbilicus. After exposure of the rectus fascia, upward lifting of the full thickness of the rectus fascia with a Cocher clamp was followed by a careful insertion of a Veress needle. Access into the peritoneal cavity by a Veress needle could be confirmed by free dropping of normal saline and initial low intraabdominal pressure. After insufflations of CO2 gas to 10 mmHg, we incised the anterior rectus fascia to expose the peritoneal layer. Regurgitation of insufflated CO2 gas with simple puncture of peritoneum could assure the access to the intra-abdominal cavity. Finger dissection was a safe and useful method for clearance of adhesion without bowel injury.
After the identification of CBD, choledochotomy was performed with a vertical incision approximately 1 to 1.5 cm in length with electrocautery. Both edges of the opened common bile duct were stitched-up with Vicryl suture and retracted in the opposite direction for easy entrance of choledochoscope. Through the 5-mm flexible choledochoscope, we identified the CBD stones, and removed them by flushing method with sterile saline, a stone basket, and sometimes crashed them by electrohydraulic lithotripsy.
The choledochotomy site was closed by continuous suture, using vicryl 3-0 with T-tube insertion and cholecystectomy was performed. We ended the operation with a Jackson-Pratt drain insertion into the operation site. All the operations were performed by a single surgeon.
Statistical analysis
Statistical significance was analyzed using the Chi-square test, Student's t-tests. A p-value<0.05 was considered significant.
RESULTS
During the study period, a total number of 44 patients underwent LCBDE initially for CBD stones in our hospital. This population comprised 24 (54.5%) males and 20 (45.5%) females with a mean age of 67.5±14.0 years (range, 34 to 90 years). There were 17 cases with previous operation history. Of 17 cases, 10 had upper abdominal operation for gastric disease (n=9) and temporary jejunostomy (n=1), 2 underwent laparoscopic cholecystectomy and another 5 cases had gynecologic procedures via low midline incision (n=2) and open appendectomy with McBurney incision (n=3) which were excluded in this study (Table 2).
Table 2. Types of previous abdominal operations in group B.
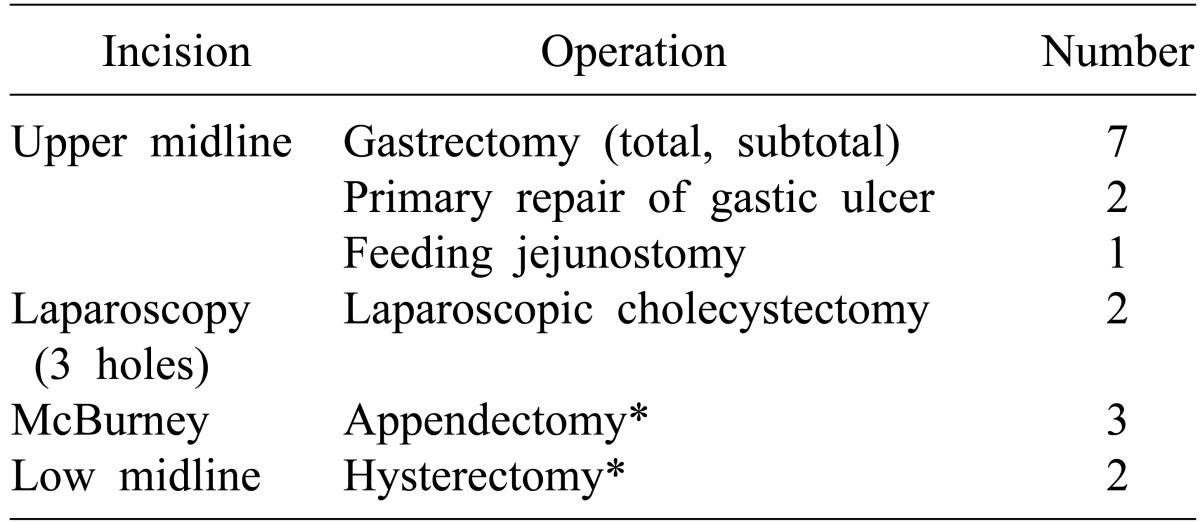
Group B, presence of upper abdominal operation
*Not included in this study
Preoperative status is presented in Table 3. In terms of male to female ratio, mean age, body weight, there were no significant differences. 15 cases in group A and 10 cases in group B had an additional underlying disease such as hypertension, cerebral disease, diabetes mellitus, chronic liver diseases, pulmonary disease like tuberculosis or pneumonia without a significant difference between the two groups (p=0.151).
Table 3. Characteristics of patients in both groups.
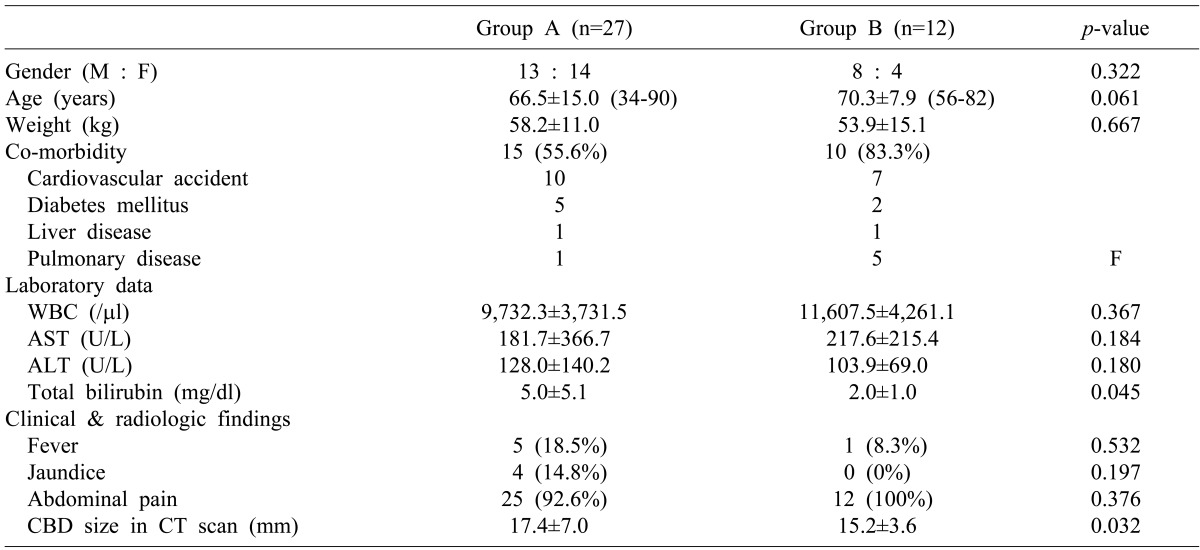
Group A, absence of previous abdominal operation; Group B, presence of upper abdominal operation; AST, aspartate transaminase; ALT, alanine transaminase; CBD, common bile duct; CT, computed tomography
The mean operation time was 164.5±63.1 minutes in group A and 134.8±45.2 minutes in group B, but there was no significant difference (p=0.180). For estimated blood loss (EBL), there was no significant difference (79.6±205.4 ml in group A and 31.3±36.6 ml group B, p=0.103) though it showed more blood loss in group A than in group B. No significant difference in the postoperative hospital stay was observed between the two groups (p=0.158). There were no complications due to port placement in either group. In 3 patients, minor bile leakage was shown during postoperative cholangiography at postoperative 7 days. But no additional procedure was needed for the management of the minor bile leakage. There was no mortality and no postoperative bleeding or bowel leakage A total of 5 cases were converted to open surgery (4 in group and 1 in group B). The reasons for open conversion in group A were severe intra-abdominal adhesion in 2 cases, an excessively small size of the abdominal cavity which impeded manipulation of the laparoscopic instrument, and lastly for possible unexpected injury to CBD during dissection. In group B, just one case was converted to open surgery due to severe inflammation (Table 4 and 5).
Table 4. Comparison of operative results in both groups.
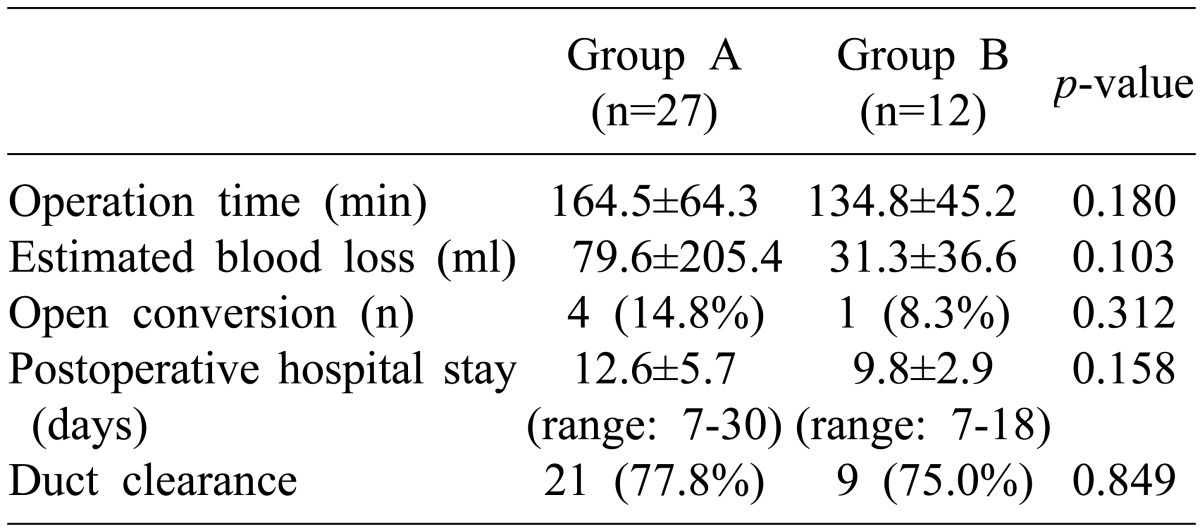
Group A, absence of previous abdominal operation; Group B, presence of upper abdominal operation
Table 5. Postoperative complications.
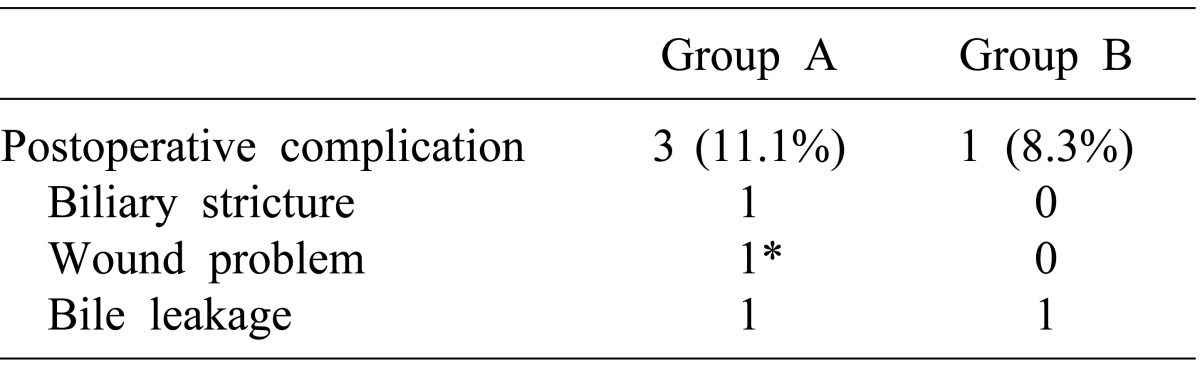
Group A, absence of previous abdominal operation; Group B, presence of upper abdominal operation
*A case of open conversion
DISCUSSION
As LC has became the gold standard for treatment of benign gallbladder disease with the development of skills and devices for laparoscopic procedures, the trend of treatment for CBD stones has changed and various options are now prevalent. These options are ERCP with or without EST, LCBDE or open CBD exploration and radiologic intervention. With the advances in endoscopic and laparoscopic technology, ERCP followed by LC has become the mainstream treatment for patients with concomitant GB and CBD stones in most centers.
However, ERCP has potential serious complications such as pancreatitis, cholangitis, duodenal perforation and life-threatening hemorrhage.17 The stone clearance rate of ERCP is reported as 75% notwithstanding the repeated sessions and additional procedures for the difficult CBD stones. Moreover, ERCP fails in 3% to 10% of all patients. The superiority of the LCBDE with LC exists in the context of a single session procedure for concomitant GB and CBD stone and preservation of the function of sphincter of Oddi which prevents ERCP related complications and post-procedural pain. Therefore, LCBDE can be the best alternative to failed ERCP for difficult cholelithiasis,18,19 although an experienced laparoscopic surgeon is mandatory. LCBDE is well indicated in 'difficult cholelithiasis' which was defined by Tai et al.17 as a failure of endoscopic stone retrieval for the following reasons; (1) access and cannulation difficulty, (2) difficult nature of CBD stones in the aspect of number or size, (3) the presence of ERCP-related complications, and (4) contraindication of EST.
In the early period of laparoscopic surgery, the laparoscopic approach was contraindicated for patients with history of prior abdominal operation. However, not only with the development of surgical skills and instruments but with the accumulated experience of laparoscopic surgeons, complicated laparoscopic procedures can be overcome with or without previous operations.20,21,22 Several concerns that make surgeons hesitate about the laparoscopic approach in previously operated abdomen include (1) possible risk of injury to organs adjacent to the previous incision wound during insertion of the Veress needle or trocar (2) curtain-like severe adhesion that prevent access to the target organ from the prior operation as well as present inflammatory processes in spite of barely establishing pneumoperitoneum (3) risk of bowel injury during adhesiolysis and (4) higher probability of conversion to open surgery.
Site selection for the initial trocar is of importance with respect to both patient's safety and exposure of the biliary tract. Li et al.20 reported that the blind puncture of a Veress needle is safe if the previous scar is more than 3 cm from the umbilicus, whereas the Hasson (open) technique is recommended if the scar is less than 3 cm from the umbilicus. In addition, we think the blind access with the trocar is not recommended even more than 3 cm from the previous scar, because the small bowel can be adherent to the innocent abdominal wall more than 3 cm from the previous incision in our experience. We applied the Veress needle method in almost all cases even less than 3 cm from the previous scar. Grasping the full layer of fascia of the rectus muscle with a Kocher clamp can facilitate abdominal wall lifting for safe insertion of the Veress needle. Confirmation of safe access into the peritoneal cavity can be achieved by free dropping of normal saline through the Veress needle followed by identifying initial low intraabdominal pressure after connecting CO2 gas. Mechanical insufflation of CO2 gas can detach multiple loose adhesions of bowel loops from the abdominal wall, which prevents possible injury to other organs not adherent to the previous scar. As usual, a simple puncture with the Veress needle to the adherent small bowel does not appear to cause serious problems, and injury from the Veress needle seems to be easily healed unless the bowel loop is severely distended. Hanney et al.23 reported two cases of aortic injury during use of the Hasson cannula and supported the Veress needle technique. Dunne et al.24 compared the Veress needle and Hasson technique for establishing pneumoperitoneum, which showed no significant difference between the technique chosen and incidence of complications. As aforementioned, we utilized an open technique with finger dissection after establishing pneumoperitoneum with a Veress needle (modified Hasson technique), which enabled avoidance of serious complications possibly encountered at the stage of entrance to the abdominal cavity.
As noninvasive methods, Viscera slide ultrasound and magnetic resonance imaging (MRI) have been suggested, and they can be considered for detecting intra-abdominal adhesions to the abdominal wall and adhesion-free areas so as to prevent injuries during the creation of pneumoperitoneum.22,25 They may serve as a diagnostic tool for future planning of laparoscopic surgery assuming that the clinical efficiency and economic feasibility are verified.
Once the abdominal cavity has been accessed, adhesiolysis should be performed enough to insert a second trocar to aid in acquisition of a view around the initial port, followed by retraction, and further dissection. Rather than adhesiolysis of all intra-abdominal adhesions, it is recommended to remove the adhesions interfering with the approach to the operative field or laparoscopic procedures. Excessive use of electrocautery should be refrained to prevent unwitting burn injury during dissection. Additionally, it should be considered that imprudent dissection with mere presumption of adhesion pattern beyond the visible area may give rise to unexpected injury to organs.
Once an upper gastrointestinal operation has been performed, especially biliary tract operations, dense adhesions around the hepatoduodenal ligament and upward adhesion of the 2nd portion of the duodenum are usually observed during re-exploration in laparoscopic fashion. Identification of the gallbladder is most crucial for sequential dissection along the right side of the common bile duct for bile duct exploration. If cholecystectomy has been performed in a previous operation, hepatic hilum should be approached by freeing the lateral parietes and beginning dissection on the right side along the lateral inferior border of the liver.20 Resultant down positioning of the transverse colon and duodenum enables finding of the common bile duct, hence the following procedure can be continued. In our opinion, complete dissection of the left side of the common bile duct is not recommended for prevention of injury to hepatic artery or portal vein injury. Clearance of the anterior aspect of the common bile duct seems to be enough for the exploration with choledochoscopy and other procedures for stone removal. We usually stitch up the opened edge of the bile duct for lateral retraction in the opposite direction, and this procedure fixes the common bile duct and allows easy access of choledochoscope into the bile duct lumen.
In some cases, we encountered rather tedious situations owing to abundant muddy stones spilled out through the opened bile duct. It took much operation time to clear up the sludge and stones from the abdominal cavity and the patient would suffer from postoperative fever. Accordingly, a patient with a highly fragile stone does not appear to be indicated for LCBDE.
The problem of T-tube insertion is still debatable and primary closure of the bile duct after exploration with or without biliary stent is in vogue at the moment.19,26,27,28,29,30 We inserted T-tubes in all cases as a route for identification and removal of the possible residual stones.
In summary, postoperative data of LCBDE in the patients with previous upper abdominal operation on operation time, conversion rate, postoperative complication rate was comparable to those in the patients without previous history. With these results, LCBDE can be described as safe, minimally invasive procedures in the patient with previous abdominal operation as far as an experienced laparoscopic surgeon is available, and it can be the best alternative to failed ERCP for difficult cholelithiasis.
References
- 1.Beal JM. Historical perspective of gallstone disease. Surg Gynecol Obstet. 1984;158:181–189. [PubMed] [Google Scholar]
- 2.Soper NJ. Laparoscopic general surgery--past, present, and future. Surgery. 1993;113:1–3. [PubMed] [Google Scholar]
- 3.Crawford DL, Phillips EH. Laparoscopic common bile duct exploration. World J Surg. 1999;23:343–349. doi: 10.1007/pl00012308. [DOI] [PubMed] [Google Scholar]
- 4.Vandervoort J, Soetikno RM, Tham TC, et al. Risk factors for complications after performance of ERCP. Gastrointest Endosc. 2002;56:652–656. doi: 10.1067/mge.2002.129086. [DOI] [PubMed] [Google Scholar]
- 5.Poulose BK, Arbogast PG, Holzman MD. National analysis of in-hospital resource utilization in choledocholithiasis management using propensity scores. Surg Endosc. 2006;20:186–190. doi: 10.1007/s00464-005-0235-1. [DOI] [PubMed] [Google Scholar]
- 6.Franklin ME, Jr, Pharand D, Rosenthal D. Laparoscopic common bile duct exploration. Surg Laparosc Endosc. 1994;4:119–124. [PubMed] [Google Scholar]
- 7.Lezoche E, Paganini AM. Single-stage laparoscopic treatment of gallstones and common bile duct stones in 120 unselected, consecutive patients. Surg Endosc. 1995;9:1070–1075. doi: 10.1007/BF00188989. [DOI] [PubMed] [Google Scholar]
- 8.Millat B, Fingerhut A, Deleuze A, et al. Prospective evaluation in 121 consecutive unselected patients undergoing laparoscopic treatment of choledocholithiasis. Br J Surg. 1995;82:1266–1269. doi: 10.1002/bjs.1800820936. [DOI] [PubMed] [Google Scholar]
- 9.Rhodes M, Nathanson L, O'Rourke N, et al. Laparoscopic exploration of the common bile duct: lessons learned from 129 consecutive cases. Br J Surg. 1995;82:666–668. doi: 10.1002/bjs.1800820533. [DOI] [PubMed] [Google Scholar]
- 10.Urbach DR, Khajanchee YS, Jobe BA, et al. Cost-effective management of common bile duct stones: a decision analysis of the use of endoscopic retrograde cholangiopancreatography (ERCP), intraoperative cholangiography, and laparoscopic bile duct exploration. Surg Endosc. 2001;15:4–13. doi: 10.1007/s004640000322. [DOI] [PubMed] [Google Scholar]
- 11.Rhodes M, Sussman L, Cohen L, et al. Randomised trial of laparoscopic exploration of common bile duct versus postoperative endoscopic retrograde cholangiography for common bile duct stones. Lancet. 1998;351:159–161. doi: 10.1016/s0140-6736(97)09175-7. [DOI] [PubMed] [Google Scholar]
- 12.Karayiannakis AJ, Polychronidis A, Perente S, et al. Laparoscopic cholecystectomy in patients with previous upper or lower abdominal surgery. Surg Endosc. 2004;18:97–101. doi: 10.1007/s00464-003-9001-4. [DOI] [PubMed] [Google Scholar]
- 13.Parsons JK, Jarrett TJ, Chow GK, et al. The effect of previous abdominal surgery on urological laparoscopy. J Urol. 2002;168:2387–2390. doi: 10.1016/S0022-5347(05)64151-1. [DOI] [PubMed] [Google Scholar]
- 14.Schirmer BD, Dix J, Schmieg RE, Jr, et al. The impact of previous abdominal surgery on outcome following laparoscopic cholecystectomy. Surg Endosc. 1995;9:1085–1089. doi: 10.1007/BF00188992. [DOI] [PubMed] [Google Scholar]
- 15.Yu SC, Chen SC, Wang SM, et al. Is previous abdominal surgery a contraindication to laparoscopic cholecystectomy? J Laparoendosc Surg. 1994;4:31–35. doi: 10.1089/lps.1994.4.31. [DOI] [PubMed] [Google Scholar]
- 16.Law WL, Lee YM, Chu KW. Previous abdominal operations do not affect the outcomes of laparoscopic colorectal surgery. Surg Endosc. 2005;19:326–330. doi: 10.1007/s00464-004-8114-8. [DOI] [PubMed] [Google Scholar]
- 17.Tai CK, Tang CN, Ha JP, et al. Laparoscopic exploration of common bile duct in difficult choledocholithiasis. Surg Endosc. 2004;18:910–914. doi: 10.1007/s00464-003-8216-8. [DOI] [PubMed] [Google Scholar]
- 18.Shin HS, Chun KS, Song IS. Laparoscopic common bile duct exploration in patients with failed endoscopic stone extraction. Korean J Hepatobiliary Pancreat Surg. 2009;13:164–170. [Google Scholar]
- 19.Park YC, Jeong JS, Jeong JG, et al. The clinical outcome of laparoscopic common bile duct exploration for the primary treatment of choledocholithiasis. Korean J Hepatobiliary Pancreat Surg. 2011;15:13–18. [Google Scholar]
- 20.Li LB, Cai XJ, Mou YP, et al. Reoperation of biliary tract by laparoscopy: experiences with 39 cases. World J Gastroenterol. 2008;14:3081–3084. doi: 10.3748/wjg.14.3081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tang CN, Tsui KK, Yang GP, et al. Laparoscopic exploration of common bile duct in post-gastrectomy patients. Hepatogastroenterology. 2008;55:846–849. [PubMed] [Google Scholar]
- 22.Zinther NB, Zeuten A, Marinovskij E, et al. Detection of abdominal wall adhesions using visceral slide. Surg Endosc. 2010;24:3161–3166. doi: 10.1007/s00464-010-1110-2. [DOI] [PubMed] [Google Scholar]
- 23.Hanney RM, Carmalt HL, Merrett N, et al. Vascular injuries during laparoscopy associated with the Hasson technique. J Am Coll Surg. 1999;188:337–338. doi: 10.1016/s1072-7515(99)00005-8. [DOI] [PubMed] [Google Scholar]
- 24.Dunne N, Booth MI, Dehn TC. Establishing pneumoperitoneum: Verres or Hasson? The debate continues. Ann R Coll Surg Engl. 2011;93:22–24. doi: 10.1308/003588411X12851639107557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chung HJ, Park IY. Ultrasound can prevent visceral injuries during the creation of pneumoperitoneum in patients with previous abdominal surgery. J Korean Soc Endosc Laparosc Surg. 2006;9:45–48. [Google Scholar]
- 26.Wu JS, Soper NJ. Comparison of laparoscopic choledochotomy closure techniques. Surg Endosc. 2002;16:1309–1313. doi: 10.1007/s004640080016. [DOI] [PubMed] [Google Scholar]
- 27.El-Geidie AA. Is the use of T-tube necessary after laparoscopic choledochotomy? J Gastrointest Surg. 2010;14:844–848. doi: 10.1007/s11605-009-1133-y. [DOI] [PubMed] [Google Scholar]
- 28.Zhang WJ, Xu GF, Wu GZ, et al. Laparoscopic exploration of common bile duct with primary closure versus T-tube drainage: a randomized clinical trial. J Surg Res. 2009;157:e1–e5. doi: 10.1016/j.jss.2009.03.012. [DOI] [PubMed] [Google Scholar]
- 29.Chen CC, Wu SD, Tian Y, et al. Sphincter of Oddi-preserving and T-tube-free laparoscopic management of extrahepatic bile duct calculi. World J Surg. 2011;35:2283–2289. doi: 10.1007/s00268-011-1193-5. [DOI] [PubMed] [Google Scholar]
- 30.Jameel M, Darmas B, Baker AL. Trend towards primary closure following laparoscopic exploration of the common bile duct. Ann R Coll Surg Engl. 2008;90:29–35. doi: 10.1308/003588408X242295. [DOI] [PMC free article] [PubMed] [Google Scholar]


