Abstract
Backgrounds/Aims
In the treatment of complicated cholecystitis, laparoscopic cholecystectomy (LC) has limited efficacy due to its substantial post-operative complications. In addition, the clinical characteristics of complicated cholecystitis (CC) patients were suspected as advanced age with highly risky comorbidity. Percutaneous transhepatic gall bladder (PTGBD) drainage could be an alternative option for successful LC. Hence, this study evaluated the outcome of PTGBD for CC within and after 5 days.
Methods
The medical records of 109 consecutive CC patients who had undergone an LC between January 2007 and December 2011 were retrospectively reviewed and compared with the medical records of CC patients who had undergone an LC within 72 hours of (group I, n=63) or 5 days after PTGBD (group II, n=40). In addition, group I was divided into group Ia (n=46) and group Ib (n=17), according to the patients' development of open-conversion or post-operative complications. The clinical outcomes of the four groups were analyzed.
Results
There was a significantly higher reference to age, the ASA score grading, and predominant comorbidities in group II than in group I. The peri-operative results of group II showed lower blood loss and relatively shorter operating times than those of group I. In the cases of early LC within 72 hours (group Ia vs. group Ib), the difference was statistically insignificant.
Conclusions
The delayed LC after PTGBD for complicated cholecystitis with high clinical risk had better results in this study, although it prolonged the patient's hospital stay.
Keywords: Complicated cholecystitis, Percutaneous transhepatic gallbladder drainage, Early laparoscopic cholecystectomy, Delayed laparoscopic cholecystectomy
INTRODUCTION
In the early days of laparoscopic surgery, the preferred treatment for acute cholecystitis was controversial, due to high incidences of complications and conversions to laparotomy. Currently, however, in the acute setting, laparoscopic cholecystectomy (LC) is recognized as a standard procedure and is performed as early as possible in principle.1,2 In complicated cholecystitis, however, there is still a high rate of complications and open conversions; therefore, careful approach should be taken in the procedure of early laparoscopic cholecystectomy.3
In addition, there are still no clear decision criteria between early surgery and delayed surgery after non-surgical treatment because it is not easy to diagnose accurately before the operation, although approximately 20% of acute cholecystitis patients develop complications, such as empyema, gangrene, and perforation.4 Thus, to improve the quality of the surgery results and the recovery, the pre-operative characteristics of high-risk patients should be identified, and the appropriate timing and methods of the surgery should be determined.
Since the introduction of percutaneous transhepatic gallbladder drainage (PTGBD) by Radder5 in the early 1980s, it has been shown as effective in high-risk patients in the treatment of acute inflammation, and has been deemed beneficial if the underlying disease state is controlled to enable time delay surgery.6,7 The indication and timing of delayed laparoscopic cholecystectomy after PTGBD is still under discussion, however, due to the increased operative difficulty with the worsening of fibrosis and adhesions owing to unremedied inflammation.8
In this study, the patients who had undergone early LC for complicated cholecystitis were compared with those who had undergone delayed LC after PTGBD. Then, the surgical outcomes, such as the clinical relief, development of complications, and length of the hospital stay were compared, and the appropriateness of the timing of the surgery for the pre-operative evaluation of the patients and their clinical significance were evaluated.
METHODS
Between January 2007 and December 2011, 526 patients underwent LC in one medical center. This retrospective study was performed on 109 of such patients, after the exclusion of 417 patients who were diagnosed with minor cholecystitis, simple cholelithiasis, and polyp of the gallbladder.
The diagnosis of complicated cholecystitis was based on a combination of clinical, imaging, and peri-operative findings. The imaging study was conducted on patients who had pain, tenderness, or rebound tenderness in their right upper abdomen, as well as empyema, gangrene, perforation of the gall bladder, or pericholecystic fluid collection. The intra-operative findings included a case of inflammation of the gall bladder with wall thickness (≥4 mm) or with adhesion to surrounding organs, and cases of hydrops, empyema, gangrene, perforation, and abscess periphery. If the diagnosis was accompanied by cholangitis, due to endoscopic retrograde cholangiopancreatography (ERCP) or magnetic resonance cholangiopancreatography (MRCP), the patient was excluded from this study.
High-risk patients who appear to have a moderate degree of inflammation, such as sepsis with complicated cholecystitis, can be offered PTGBD, especially when they have a poor general condition or when there is a need to treat an underlying disease with a priority. After an average of 7.9 days, as well as at least 5 days after the PTBD procedure, LC was performed.
PTGBD was performed in 40 patients of the total of 109 patients with complicated cholecystitis. It was carried out by a radiologist, and the gall bladder was identified via ultrasonography. The aspirated material was sent to a clinical laboratory for culture. Procedure-related complications, such as pigtail conduit dislocation, bile leakage, and intra-abdominal bleeding, were not observed.
In all the cases, general anesthesia was applied, and LC was selected primarily for complicated cholecystitis, using the four-trocar technique. After the introduction of the laparoscope below the navel trocar (12 mm) into the peritoneal cavity, carbon dioxide gas was injected intraperitoneally to maintain a 12-15 mmHg intra-abdominal pressure, and three trocars (5 mm) were additionally inserted.
First, according to the timing of the surgery, the 109 patients with complicated cholecystitis were divided into two groups. The data on the patients who underwent LC within 72 hours of admission (group I, n=63) and on the patients who underwent LC 5 days after PTGBD (group II, n=40) were compared. In addition, group I was divided into group Ia (n=46) and group Ib (n=17), according to the patients' development of open-conversion or post-operative complications. From these, delayed LC was performed after conservative treatment only in 6 cases, without PTGBD.
The pre-operative clinical status of each group was examined by age, sex, weight, American Society of Anesthesiologists (ASA) classification, white blood cell (WBC) count, and C-reactive protein (CRP) value upon the patients' admission. The degree of operative difficulty was quantified by reviewing the operation time, blood loss, and rate of open-conversion. The post-operative results were also analyzed, according to the duration of the patient's hospital stay, the time of resumption, and the occurrence of post-operative complications. Statistical analyses were performed using SPSS Version 20.0 through independent sample t-tests and chi-square tests. The statistical results were considered significant when the p-value was less than 0.05.
RESULTS
Pre-operative characteristics of complicated cholecystitis
The mean age of all the patients in the 109 cases was 65.7 years. The average ages of the patients in the two groups were 60.4 years in group I (n=63) and 72.5 years in group II (n=40). The male-to-female ratios were 1.62 : 1 in group I and 1.35 : 1 in group II.
The mean ASA classifications and the proportions of patients with underlying diseases were 1.78 and 57.14% in group I, and 2.4 and 90.0% in group II, respectively. The clinical patterns of the two groups were also compared. Significant differences were observed between the two groups in terms of age, ASA classifications, and the proportion of patients with underlying diseases (p<0.001). In group II, the number of patients with underlying hypertension and cerebrovascular disease was relatively large (p<0.05).
The mean leukocytosis values were 15.0×1,000/mm3 in group I and 16.8×1,000/mm3 in group II, but they were not statistically significant. The mean CRP values were 13.73 mg/dl in group I and 19.25 mg/dl in group II, which were statistically significant (p<0.05) (Table 1).
Table 1. Pre-operative characteristics of complicated cholecystitis.
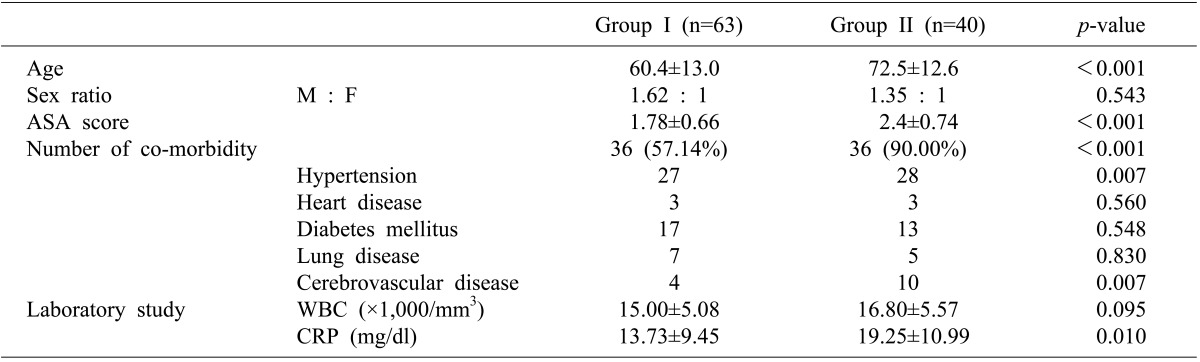
Group I, laparoscopic cholecystectomy underwent within 72 hours; Group II, preoperative percutaneous transhepatic gallbladder drainageand subsequent laparoscopic cholecystectomy underwent after 5 days; ASA, American Society of Anesthesiologists score; WBC, white blood cell; CRP, C-reactive protein
Comparison of the outcomes of the operation on the complicated cholecystitis
The mean operative times were 99.8 minutes in group I and 85.9 minutes in group II, and the mean blood loss values were 361.6 ml in group I and 186.1 ml in group II (Table 2). The numbers of cases in which the open-conversion to laparotomy was performed were seven (11.1%) in group I and only four (8.7%) in group II. In group I, the patients who underwent early LC, the operative time, blood loss volume, and rate of open-conversion were higher, though without statistical significance, except for the intra-operative blood loss volume (p<0.05).
Table 2. Comparison of outcome during operation of complicated cholecystitis.
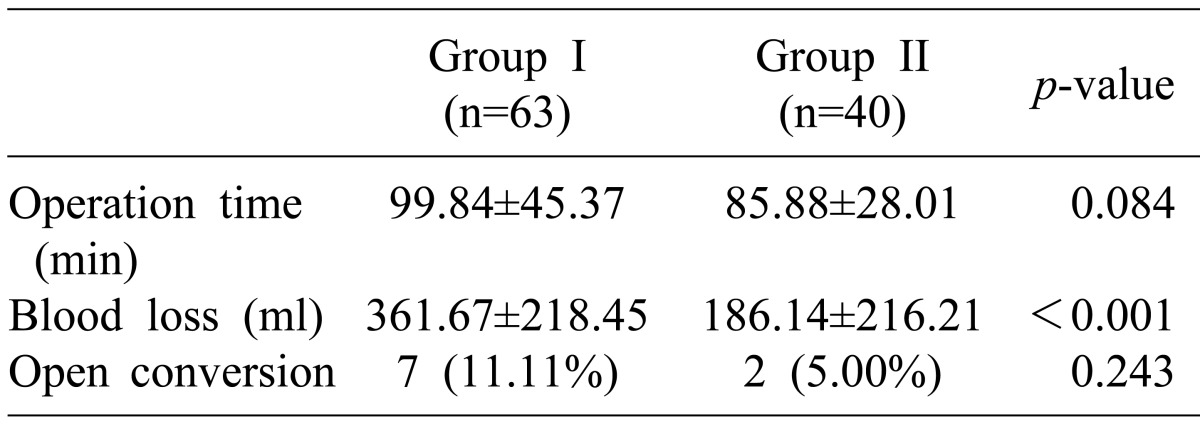
Open conversion, converted from laparoscopic cholecystectomy to open cholecystectomy
Complicated cholecystitis post-operative results
The average durations of the patients' hospital stay were 12.92 days in group I and 20.08 days in group II. Group I patients' hospital stay was significantly shorter (p<0.05). The oral intake was resumed after 2.56 days in group I and after 2.55 days in group II, showing almost no difference.
Post-operative complications occurred in 22 cases (21.36%) in group I and group II among the 103 patients. Of these, the following complications occurred in 15 cases (24.59%) in group I: bile leak in 2 cases, intraperitoneal abscess in 1 case, heart disease in 4 cases, respiratory diseases, such as pneumonia and pulmonary embolism, in 3 cases, and general edema, paralytic ileus, and other complications in 5 cases. The following complications occurred in seven cases (17.5%) in group II: intraperitoneal abscess in 1 case, surgical site bleeding in 1 case, heart disease in 2 cases, and pneumonia and other complications in 2 cases. There was a higher incidence of complications after the surgery in group I than in group II, but the difference between the two groups was statistically insignificant (Table 3). In addition, six patients with delayed LC for more than 5 days after conservative treatment alone showed the highest percentage of underlying diseases (83%) when compared with that of the group I and group II patients. The former patients' WBC count of 12.46×1,000/mm3 and CRP value of 7.66 mg/dl were lower than those of the later. The mean operative time of the six patients was 66 minutes, the mean blood loss was 189 ml, and the mean duration of their hospital stay was 9.7 days. The six patients who underwent LC after 5 days with conservative treatment alone and the patients who underwent LC 5 days after PTGBD did not differ significantly, but the exact statistical significance could not be determined because of the small sample sizes, though it was generally the same as that in the earlier-mentioned study.
Table 3. Postoperative results of complicated cholecystitis.
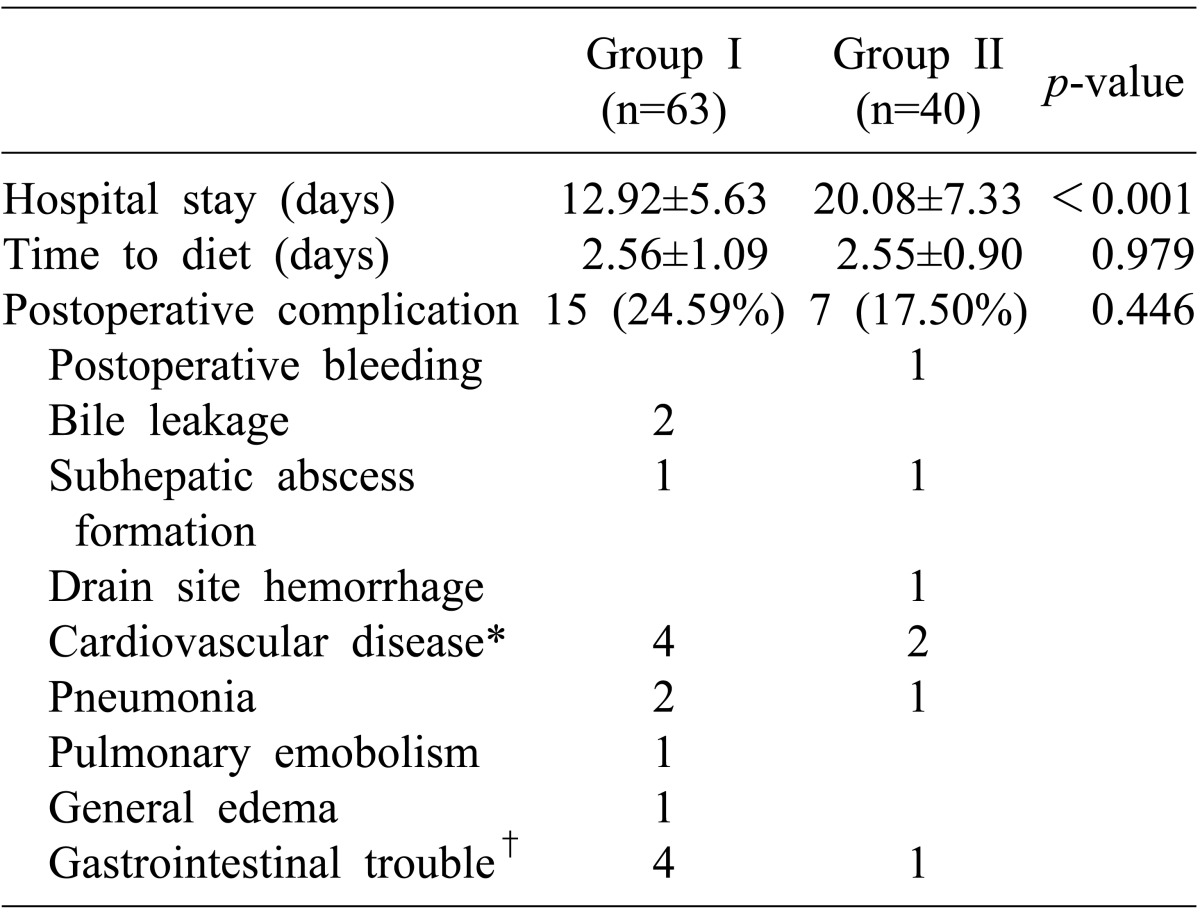
*Worsen existing disease or hypotension or arrhythmia; †Including stress gastritis, ileus, diarrhea
Comparison of the development of peri-operative difficulty or post-operative complications in the early LC group and that in the complicated cholecystitis group
The 63 patients who underwent LC within 72 hours of their hospital admission (group I) were divided into group Ia and group Ib, according to their development of open-conversion to laparotomy or post-operative complications. Within group Ia, there were 46 patients without complications. In comparison, complications (n=15, 73%), including open-conversion (n=7, 27%), occurred in 17 cases in group Ib.
The mean age, mean ASA classifications, and proportion of patients with underlying diseases in group Ia were 59 years, 1.67, and 52.2%, respectively. The mean age, mean ASA classifications, and proportion of underlying diseases in group Ib were 63.9 years, 2.06, and 70.6%, respectively. The mean initial WBCs were 14.5×1,000/mm3 in group Ia and 16.0×1,000/mm3 in group Ib. Group Ia less frequently showed the results of all the features than group Ib, though without statistical significance, except with respect to the ASA classification (p<0.05).
The mean operative times were 185.1 minutes in group Ia and 123.2 minutes in group Ib, and the mean blood loss values were 458.0 ml in group Ia and 435.9 ml in group Ib, which had a statistically insignificant difference. The mean hospital stay durations, however, were 11.3 days in group Ia and 17.2 days in group Ib, which had a statistically significant difference (p<0.001) (Table 4).
Table 4. Comparison on development of perioperative difficulty or postoperative complication between early laparoscopic cholecystectomy of complicated cholecystitis.
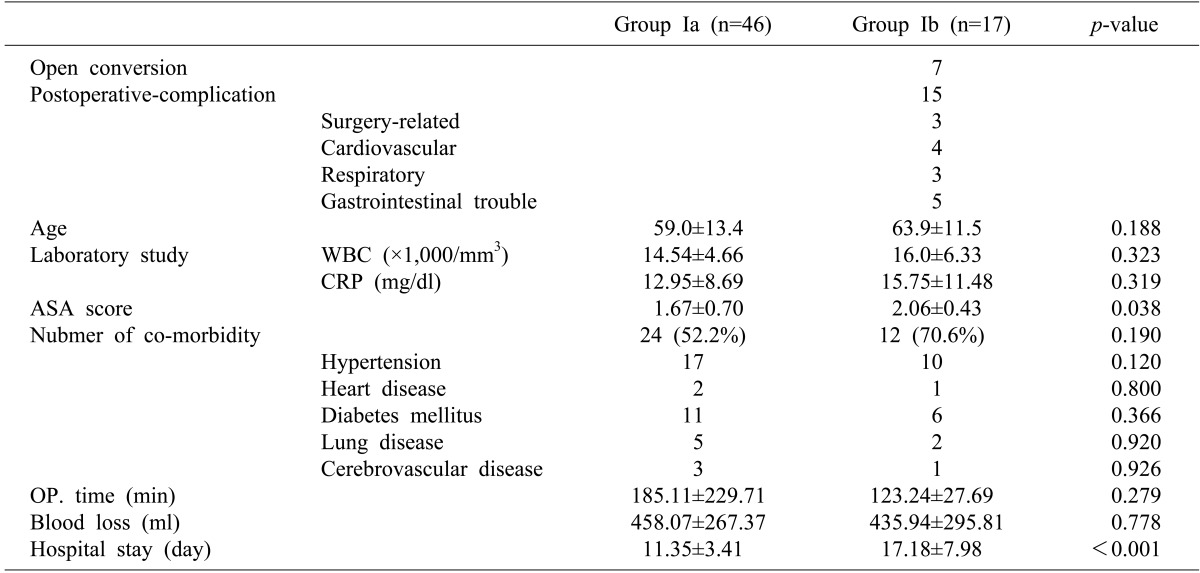
Surgery-related complications included bile leakage and subhepatic abscess formation. Cardiovascular complications included worsen existing disease, hypotension or arrhythmia. Respiratory complications included pneumonia and pulmonary embolism
Group Ia, no development of any complication with early laparoscopic cholecystectomy undergoing within 72 hours; Group Ib, development of some complications or open conversion with early laparoscopic cholecystectomy
DISCUSSION
In the present study, patients with complicated cholecystitis were found to have had moderate to severe inflammation and poor general conditions. Most current surgeons agree that LC is the treatment of choice for complicated cholecystitis. Nevertheless, there are two issues on the high rate of complications after surgery and open-conversion after LC in high-risk patients with complicated cholecystitis. Thus, to reduce the incidence of complications and the open-conversion rate, various studies have been reported on the appropriate timing of the surgery. Eldar et al.9 and Fletcher et al.10 reported that the inflammation intensifies and the rate of post-operative complications is higher in the elderly as risk factors of the development of complicated cholecystitis. Bingener et al.11 and Kanaan et al.12 suggested that as a risk factor associated with open-conversion to laparotomy, the elderly are more susceptible to damage from inflammation of the gall bladder wall deformation. Complicated cholecystitis is accompanied by cardio-respiratory complications in the elderly, so delayed LC that is performed after PTGBD has been reported to have advantages such as relief of inflammation, patient stabilization, and a successful outcome.13,14,15 Many researchers have a contrary opinion, however, that early LC can solve the problem immediately and reduce medical expenses by shortening the patient's hospital stay.16
There have been many reports on the optimal time of LC. The longer the delay in the LC, the more fibrosis and adhesion in the operation field occurs, which makes operation difficult. Therefore, researchers recommend that LC be done within 48 or 72 hours, at least five days after the patient's presentation at the hospital, though their opinions vary. Farooq et al.16 and Daniak et al.17 found that after early surgery within 72 hours, post-operative complications were reduced from the existing 20% to 8%. They reported that the patient's recovery time, length of hospital stay, and medical expenses were cut in half. On the contrary, Kim et al.18 and Shin et al.19 suggested that purulent bile emission after PTGBD can reduce the difficulty of the surgery at least three days after the symptoms subside within about 48 hours, by reducing the intra-abdominal pressure and irritation. It reduced the rate of open-conversion by 5% and 11% in the former and latter studies, respectively.
In this study, the patients' pre-operative clinical factors were analyzed, and observed significantly higher values in group I as the patients underwent LC within 72 hours of their hospital admission than in group II as the patients underwent LC five days after PTGBD, in terms of age, ASA classifications, proportion of underlying diseases, and CRP values (p-value<0.05). The comparison of the surgical procedures showed that group I had only a slightly longer operative time and a slightly higher rate of open-conversion and post-operative complications than in group II, but a more statistically significant edge in average blood loss (p<0.05).
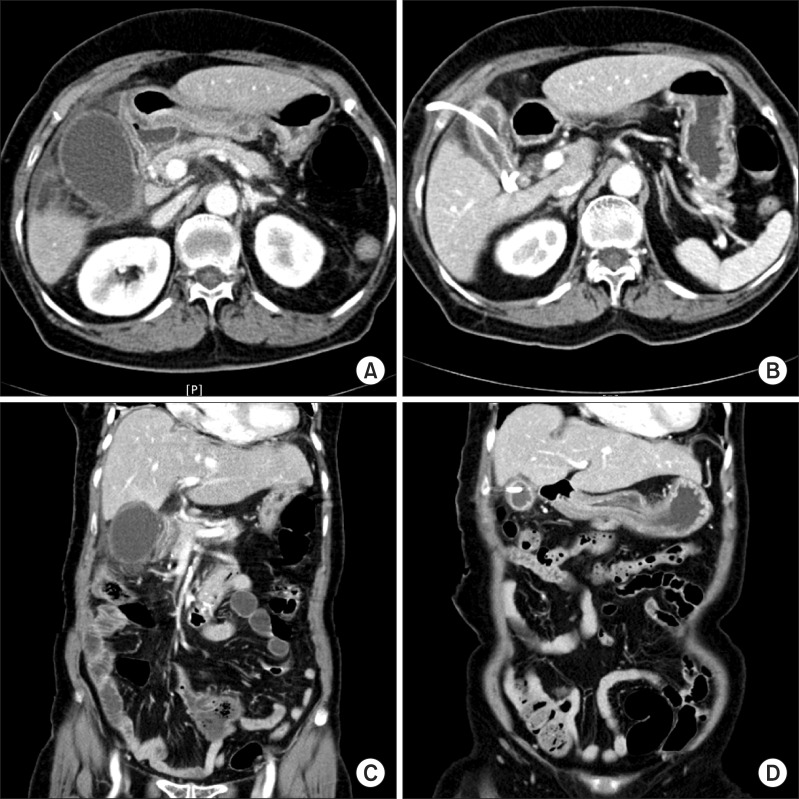
This study offered conflicting results of the peri-operative process in group II patients, who underwent delayed LC because their results were superior to those of group I, despite the more severe pre-operative inflammation and poorer general condition of group II patients than of group I patients who underwent early LC. Recent studies reported advantages of the rapid reduction of the inflammation that affected the surgical difficulty. Cytokines are the most potent stimulants of fibroplasia that affects wound healing, and have strong chemotactic effects on polymorphonuclear neutrophils. Shin et al.19 suggested that early inflammatory emission with reduction of cytokines improves to some extent the excessive fibrosis and adhesions that cause the open-conversion. Lee et al.20 reported the usefulness of PTGBD in relieving inflamed gall bladder adhesions, and its low open-conversion rate through the facilitation of laparoscopic cholecystectomy. They also accounted for the usefulness of PTGBD in providing pre-operative time to identify the patient's underlying disease, and the status of the biliary system can improve the patient's safety. In terms of the results, it can be said that the results are consistent with the outcomes of this study (Fig. 1).
Fig. 1. Axial (A, B) and coronal (C, D) CT images of empyema of the gallbladder in an 82 year-old female patient. (A, C) Computed tomography scan shows a markedly dilated and gallbladder with ascites collection at perihepatic space. (B, D) Follow up CT image obtained 14 days after percutaneous transhepatic gallbladder drainage shows marked resolution of the abscess with drainage tube.
The hospital stay was significantly shorter in group I at 12.9 days than in group II at 20.08 days. After some deliberation, however, the increase in the duration of the hospital stay of about 7 days with the selection of delayed LC was deemed endurable because it could countervail the shortened hospital stay with the early LC, given that surgery was undergone at least 5 days to an average of 7.9 days after PTGBD. In addition, in this study, the surgical procedure and the post-operative complication in group II was relatively more tolerable than in group I, though the difference was insignificant. Thus, it is thought that delayed LC could be tactically considered for high-risk patients in the selection of the appropriate timing of the surgery.21
The comparison of the two groups of patients who underwent early LC showed that the ASA classification of group Ib was relatively higher than that of group Ia (2.06 versus 1.67, p<0.05). In terms of the duration of the hospital stay, the average of 17 days of group Ib was approximately longer than the average of only 6 days of group Ia (p<0.05). Compared with the 20.1 day-mean duration of the hospital stay of the previously analyzed delayed LC group, the result of the early surgical intervention group was dubious, which is the advantage of the shortening of the hospital stay. Then considering that the surgical outcomes of the high-risk patients who underwent delayed LC were better than those of the patients who underwent early LC in terms of their ASA classifications,21,22 the evaluation of the patients in groups Ia and Ib, who underwent early LC, corresponded to the overall evaluation of this study. In the end, the appropriateness of choosing early LC was reconsidered.
The risk factors of complicated cholecystitis have been controversial until recently, as shown with an opinion that age is more important in the early operative process than the presence of an underlying disease.16 There have been issues concerning more comorbid conditions, such as heart disease, as a risk factor of open-conversion to laparotomy.12 Consequently, in patients suspected as complicated cholecystitis during the diagnostic procedure, their clinical status, such as ASA classification and comorbidity, should be evaluated in detail by focusing on them. In this process, to successfully treat complicated cholecystitis, selection of the appropriate timing of surgery is important.
In conclusion, of the 109 patients who were diagnosed with complicated cholecystitis, 63 patients underwent laparoscopic cholecystectomy within 72 hours of admission and 40 patients underwent delayed laparoscopic cholecystectomy after PTGBD. The pre-operative evaluation showed that the underlying disease and the ASA classification posed higher risks in the latter than in the former patients. The delayed-surgery group showed shorter operative time, less blood loss, a lower open-conversion rate, and a lower incidence of post-operative complications than the other groups. Therefore, depending on the clinical state of the complicated cholecystitis patient, it is necessary to determine the appropriate timing of surgery.
ACKNOWLEDGEMENTS
This research was supported by Gwangmyeong Sungae Hospital (2012).
References
- 1.Zucker KA, Flowers JL, Bailey RW, et al. Laparoscopic management of acute cholecystitis. Am J Surg. 1993;165:508–514. doi: 10.1016/s0002-9610(05)80951-1. [DOI] [PubMed] [Google Scholar]
- 2.Knight JS, Mercer SJ, Somers SS, et al. Timing of urgent laparoscopic cholecystectomy does not influence conversion rate. Br J Surg. 2004;91:601–604. doi: 10.1002/bjs.4539. [DOI] [PubMed] [Google Scholar]
- 3.Habib FA, Kolachalam RB, Khilnani R, et al. Role of laparoscopic cholecystectomy in the management of gangrenous cholecystitis. Am J Surg. 2001;181:71–75. doi: 10.1016/s0002-9610(00)00525-0. [DOI] [PubMed] [Google Scholar]
- 4.Kiviluoto T, Sirén J, Luukkonen P, et al. Randomised trial of laparoscopic versus open cholecystectomy for acute and gangrenous cholecystitis. Lancet. 1998;351:321–325. doi: 10.1016/S0140-6736(97)08447-X. [DOI] [PubMed] [Google Scholar]
- 5.Radder RW. Ultrasonically guided percutaneous catheter drainage for gallbladder empyema. Diagn Imaging. 1980;49:330–333. [PubMed] [Google Scholar]
- 6.Klimberg S, Hawkins I, Vogel SB. Percutaneous cholecystostomy for acute cholecystitis in high-risk patients. Am J Surg. 1987;153:125–129. doi: 10.1016/0002-9610(87)90212-1. [DOI] [PubMed] [Google Scholar]
- 7.Sugiyama M, Tokuhara M, Atomi Y. Is percutaneous cholecystostomy the optimal treatment for acute cholecystitis in the very elderly? World J Surg. 1998;22:459–463. doi: 10.1007/s002689900416. [DOI] [PubMed] [Google Scholar]
- 8.Habib FA, Kolachalam RB, Khilnani R, et al. Role of laparoscopic cholecystectomy in the management of gangrenous cholecystitis. Am J Surg. 2001;181:71–75. doi: 10.1016/s0002-9610(00)00525-0. [DOI] [PubMed] [Google Scholar]
- 9.Eldar S, Sabo E, Nash E, et al. Laparoscopic cholecystectomy for acute cholecystitis: prospective trial. World J Surg. 1997;21:540–545. doi: 10.1007/pl00012283. [DOI] [PubMed] [Google Scholar]
- 10.Fletcher DR, Hobbs MS, Tan P, et al. Complications of cholecystectomy: risks of the laparoscopic approach and protective effects of operative cholangiography: a population-based study. Ann Surg. 1999;229:449–457. doi: 10.1097/00000658-199904000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bingener J, Richards ML, Schwesinger WH, et al. Laparoscopic cholecystectomy for elderly patients: gold standard for golden years? Arch Surg. 2003;138:531–535. doi: 10.1001/archsurg.138.5.531. [DOI] [PubMed] [Google Scholar]
- 12.Kanaan SA, Murayama KM, Merriam LT, et al. Risk factors for conversion of laparoscopic to open cholecystectomy. J Surg Res. 2002;106:20–24. doi: 10.1006/jsre.2002.6393. [DOI] [PubMed] [Google Scholar]
- 13.Saxe A, Lawson J, Phillips E. Laparoscopic cholecystectomy in patients aged 65 or older. J Laparoendosc Surg. 1993;3:215–219. doi: 10.1089/lps.1993.3.215. [DOI] [PubMed] [Google Scholar]
- 14.Chikamori F, Kuniyoshi N, Shibuya S, et al. Early scheduled laparoscopic cholecystectomy following percutaneous transhepatic gallbladder drainage for patients with acute cholecystitis. Surg Endosc. 2002;16:1704–1707. doi: 10.1007/s00464-002-9004-6. [DOI] [PubMed] [Google Scholar]
- 15.Kim IG, Jeon JY. Benefits of percutaneous transhepatic gallbladder drainage for laparoscopic cholecystectomy in patients with acute cholecystitis. Korean J Hepatobiliary Pancreat Surg. 2010;14:46–52. [Google Scholar]
- 16.Farooq T, Buchanan G, Manda V, et al. Is early laparoscopic cholecystectomy safe after the "safe period"? J Laparoendosc Adv Surg Tech A. 2009;19:471–474. doi: 10.1089/lap.2008.0363. [DOI] [PubMed] [Google Scholar]
- 17.Daniak CN, Peretz D, Fine JM, et al. Factors associated with time to laparoscopic cholecystectomy for acute cholecystitis. World J Gastroenterol. 2008;14:1084–1090. doi: 10.3748/wjg.14.1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim JM, Kim KS, Kim KH. Percutaneous gallbladder drainage and optimal timing for successful laparoscopic cholecystectomy in acute complicated cholecystitis. J Korean Surg Soc. 2007;73:242–245. [Google Scholar]
- 19.Kim H, Kim HO, Shin JH. Comparison of early versus delayed laparoscopic cholecystectomy after percutaneous transhepatic gallbladder drainage (PTGBD) for patient with complicated acute cholecystitis. J Korean Surg Soc. 2007;73:329–333. [Google Scholar]
- 20.Lee SM, Joe S, Lee MK, et al. Usefullness of preoperative percutaneous transhepatic GB drainage on laparoscopic cholecystectomy in patients with acute chlolecystitis. Korean J Hepatobiliary Pancreat Surg. 2002;6:167–172. [Google Scholar]
- 21.Yun SS, Hwang DW, Kim SW, et al. Better treatment strategies for patients with acute cholecystitis and American Society of Anesthesiologists classification 3 or greater. Yonsei Med J. 2010;51:540–545. doi: 10.3349/ymj.2010.51.4.540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee AB, Lee HK, Min SK, et al. Clinical characteristics of complicated acute cholecystitis and its outcome of laparoscopic cholecystectomy. J Korean Surg Soc. 2006;70:53–58. [Google Scholar]