Abstract
Background
Substantial geographic variation exists in percutaneous coronary intervention (PCI) use across the United States. It is unclear the extent to which high PCI utilization can be explained by PCI for inappropriate indications. The objective of this study was to examine the relationship between PCI rates across regional healthcare markets utilizing hospital referral regions (HRRs) and PCI appropriateness.
Methods
The number of PCI procedures in each HRR was obtained from the 2010 100% Medicare limited data set. HRRs were divided into quintiles of PCI utilization with increasing rates of utilization progressing to quintile 5. NCDR CathPCI Registry® data were used to evaluate patient characteristics, appropriate use criteria (AUC), and outcomes across the HRR quintiles defined by PCI utilization with the study population restricted to HRRs where ≥ 80% of the PCIs were performed at institutions participating in the registry. PCI appropriateness was defined using 2012 AUC by the American College of Cardiology (ACC)/American Heart Association (AHA)/The Society for Cardiovascular Angiography and Interventions (SCAI).
Results
Our study cohort comprised of 380,981 patients treated at 178 HRRs. Mean PCI rates per 1,000 increased from 4.6 in Quintile 1 to 10.8 in Quintile 5. The proportion of non-acute PCIs was 27.7% in Quintile 1 increasing to 30.7% in Quintile 5. Significant variation (p < 0.001) existed across the quintiles in the categorization of appropriateness across HRRs of utilization with more appropriate PCI in lower utilization areas (Appropriate: Q1, 76.53%, Q2, 75.326%, Q3, 75.23%, Q4, 73.95%, Q5, 72.768%; Inappropriate: Q1 3.92%, Q2 4.23%, Q3 4.32%, Q4 4.35%, Q5 4.05%; Uncertain: Q1 8.29%, Q2 8.84%, Q3 8.08%, Q4 9.01%, Q5 8.93%; Not Mappable: Q1 11.26%, Q2 11.67%, Q3 12.37%, Q4 12.69%, Q5 14.34%). There was no difference in risk-adjusted mortality across quintiles of PCI utilization.
Conclusions
Geographic regions with lower PCI rates have a higher proportion of PCIs performed for appropriate indications. Areas that perform more PCIs also appear to perform more elective PCI and many could not be mapped by the AUC.
Introduction
Percutaneous coronary intervention (PCI) is one of the most commonly performed procedures in the United States and is a major contributor to health care cost. Prior studies have reported a 5-fold variation in rates of PCI across geographic regions. [1] As much of this geographic variation is attributable to differences in rates of PCI for non-urgent indications, it is possible that practice variation is a major driver of this dissimilarity. However, it is unknown the extent to which geographic variation in PCI procedures is due to inappropriate use of PCI.
The American College of Cardiology (ACC), American Heart Association (AHA), and The Society for Cardiovascular Angiography and Interventions (SCAI) have developed well-established guidelines for the performance of PCI. [2] In 2009, a multi–society effort resulted in the development of Appropriate Use Criteria (AUC) for Coronary Revascularization [3]. These criteria serve as a standardized tool to assess the likelihood of clinical benefit from a given PCI procedure. Initial studies have indicated that almost all PCIs performed for acute indications are appropriate whereas the rate of inappropriate PCI (in which the expected benefit of treatment is small) is between 12% to 20% for non-acute indications. [4–7]
The objective of this study was to better understand the overall relationship between utilization of PCI across regional healthcare markets across the United States and appropriateness. We hypothesized that previously described geographic variations in PCI rates may be driven by different patterns of use of non-urgent, inappropriate procedures, with little geographic variation in appropriate PCI.
This research was supported by the American College of Cardiology Foundation’s National Cardiovascular Data Registry (NCDR). The views expressed in this manuscript represent those of the authors, and not necessarily represent the official views of the NCDR or its associated professional societies identified at www.ncdr.com.
Methods
Funding and Content
No extramural funding was used to support this work. The authors are solely responsible for the design and conduct of this study, all study analyses, the drafting and editing of the paper and its final contents.
CathPCI Registry
Our study was comprised of patients undergoing PCI in 2010 at hospitals participating in the NCDR CathPCI Registry. The details and design of the NCDR CathPCI Registry, a joint initiative of the American College of Cardiology and the Society for Cardiovascular Angiography and Interventions, have been described previously. [8,9] Briefly, the registry assesses characteristics, treatments, and in-hospital outcomes of patients undergoing diagnostic catheterization or percutaneous intervention at over 1,500 United States sites. The data are collected by trained staff at participating hospitals using standardized data elements. The data collection process, audit and quality checks have been previously described. Waiver of written informed consent and authorization for this study was granted by Chesapeake Research Review Incorporated. Patient records and information was anonymized and de-identified prior to analysis.
Categorizing Procedural Appropriateness
The methodology for the appropriateness criteria for coronary revascularization has been described previously. [3] Briefly, an expert panel from various specialties and subspecialties reviewed a set of 198 prototypical clinical scenarios and adjudicated whether or not the literature and clinical experience supported that the benefits of the procedure, in terms of mortality reduction or symptom relief, outweighed the costs and risks. Each clinical scenario was scored on a numeric scale from 1 indicating the least appropriate and 9 suggesting the most. Scores were further categorized into ratings of appropriate (median score = 7–9), uncertain (4–6), or inappropriate (1–3). The terminology was changed in 2013 to appropriate care, may be appropriate care, and rarely appropriate care; however, the aforementioned terminology was utilized given the application of the 2012 ACC/AHA/SCAI AUC in the current work. [10] Appropriate coronary revascularization is considered generally acceptable and a reasonable approach for the indication that is likely to improve the patients’ outcomes and survival while coronary revascularization is considered inappropriate when it is not generally acceptable and not a reasonable approach for the indication as it is unlikely to improve the patients’ outcomes and survival. Coronary revascularization is considered uncertain when more research or patient information is required to classify as appropriate or inappropriate. Previous work demonstrated minimal rates of inappropriate PCIs in patients being treated for an acute coronary syndrome (ACS), but almost 1 in 8 procedures in the setting of stable coronary artery disease (CAD) were inappropriate and nearly 1 in 6 PCIs were unmappable due to missing data. [4]
Statistical Analysis
Assessing geographical variation in PCI
Geographical variation was assessed by dividing the country into hospital referral regions (HRRs). An HRR is a regional health care market for tertiary care that contains at least one hospital performing major cardiovascular procedures and neurosurgery. [11] The number of PCI procedures in each zip code was obtained by identifying claims with relevant PCI ICD-9 and CPT procedure codes from the 100% Medicare limited data set from 2010 (please see S1Tablefor relevant codes). These data were then aggregated to the HRR level by mapping patient zip code to HRR using zipcode crosswalk files from the Dartmouth Atlas of Health Care (http://www.dartmouthatlas.org/tools/downloads.aspx#crosswalks). The rate of PCI use was calculated at the HRR level by dividing the number of PCIs performed on Fee For Service (FFS) Medicare Patients by the total number of eligible FFS Medicare patients in that HRR. We then divided HRRs into quintiles of PCI utilization with quintile 5 representing the highest utilization rate.
All PCIs (irrespective of payer status) in the NCDR CathPCI registry were then assigned to the respective HRRs and quintiles of utilization (derived using Medicare data) using patient zip code. To avoid misclassification due to incomplete participation in the CathPCI registry, we restricted the analyses to those HRRs in which greater than 80% of the total number of PCIs were performed at hospitals participating in the CathPCI Registry.
Data from the NCDR CathPCI Registry were then used to evaluate patient characteristics, procedural appropriateness, and in-hospital outcomes across the quintiles of PCI utilization. Appropriateness was defined using the 2012 ACC/AHA/SCAI AUC and PCIs were categorized as appropriate, inappropriate, uncertain, or unmappable. Unmappable cases are those in which no stress test was performed and the presentation was non-ACS or for a non-ACS presentation with a positive stress test and an unavailable result. [3,12]
Assessing variation in appropriateness
The difference in appropriateness across quintiles of PCI utilization was compared using a Chi square test. Additionally, a Cochran-Armitage trend test was performed on each level of the appropriate use criteria. To assess for differences in outcome across the areas of varying PCI utilization, observed and adjusted mortality rates across quintiles were calculated. The NCDR mortality risk model was used to adjust for differences in patient mix. [13] The adjusted rates represented the indirect standardized mortality ratio (observed over expected number of deaths) multiplied by the observed overall rate.
The analysis was repeated utilizing only those HRRs with 100% capture (i.e. all PCIs in that HRR were performed at hospitals participating in the CathPCI Registry).
Results
Patient Population
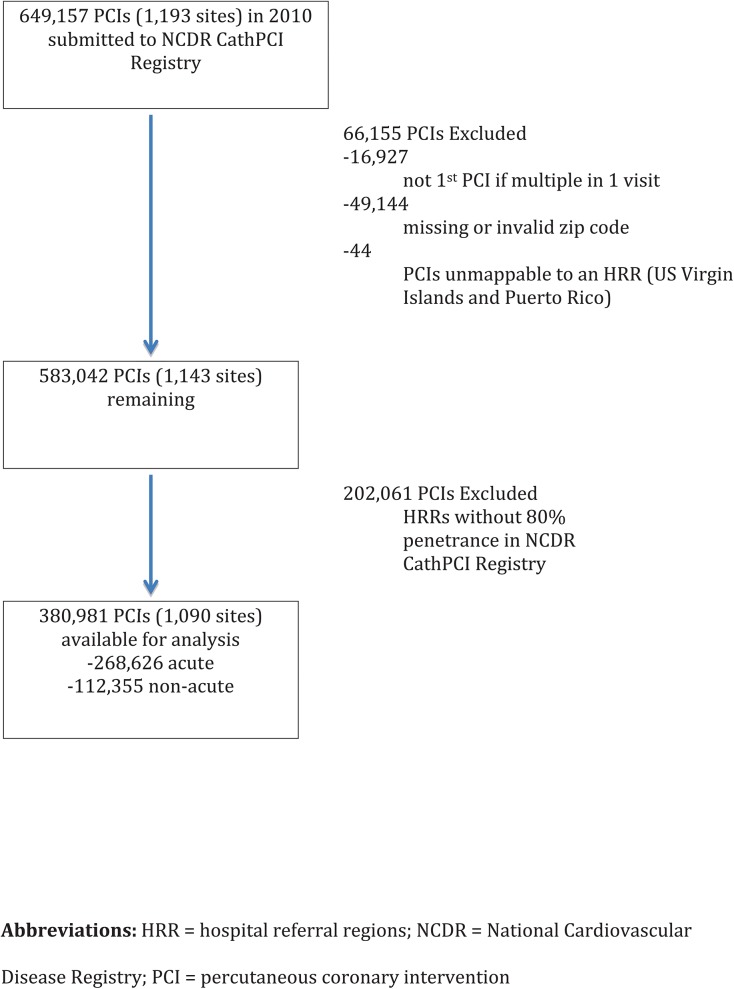
The study population selection is outlined in Fig 1. Of the 306 HRRs spanning the United States, 178 were included in the analysis. Of the 178 HRRs included, 100 HRRs had 100% capture (i.e. all sites within that HRR participating in the NCDR CathPCI Registry) while 78 HRRs had 80–99.9% capture. A total of 380,981 patients underwent their first PCI in 2010 and had a valid zip code that could be mapped to these 178 HRRs with ≥80% penetrance in the NCDR.
Fig 1. Final cohort available for primary analysis.
Shown is the final cohort for the primary analysis and the PCIs that were excluded.
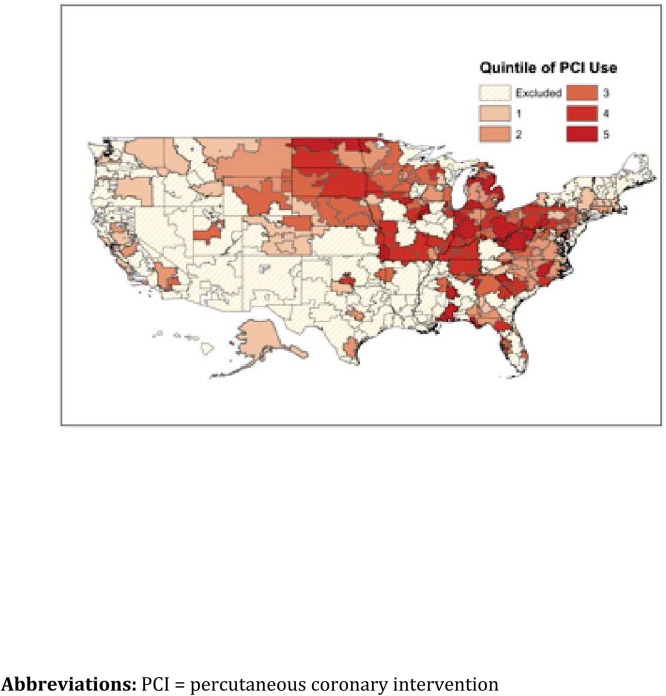
The extent of geographic variation in PCI rates for HRRs included in the analysis is depicted in Fig 2and for the entire country in S1 Fig. The mean PCI rate per 1000 progressing from Quintile 1 to Quintile 5 is 4.6, 6.0, 6.9, 8, and 10.8, respectively (Table 1)
Fig 2. Geographic distribution of HRRs categorized by quintiles of PCI utilization and included in analysis.
Shown are the HRRs divided by quintile of PCI utilization and the HRRs that were excluded from the analysis.
Table 1. Mean PCI rates within each quintile of utilization (per 1000).
| Quintile | # of HRRs | Mean % Capture | Mean PCI Rate (SD) |
|---|---|---|---|
| 1 | 37 | 98.6% | 4.6 (.61) |
| 2 | 40 | 96.7% | 6.0 (.31) |
| 3 | 37 | 96.9% | 6.9 (.27) |
| 4 | 30 | 95.1% | 8.0 (.42) |
| 5 | 34 | 97% | 10.8 (2.0) |
Abbreviations: HRR = hospital referral regions; PCI = percutaneous coronary intervention
PCI Distribution and Patient Characteristics
The average age of the total cohort was 64.5 years and 67.1% were male. 28.6% of the population were current smokers or had smoked within the past year and over 80% of the population had either hypertension or dyslipidemia, or both. Diabetes was present in 35.6% of the cohort. Of all the PCIs, 14.09% were for ST-elevation myocardial infarction (STEMI), 44.93% for non-STEMI or unstable angina, and 41% were for stable CAD, with 9.27% of the cohort being asymptomatic at the time of intervention. Tables 2 and 3summarizes the patient demographic and clinical characteristics stratified by quintile of PCI rate. In Quintile 1, of the 55,727 PCIs performed, 72.3% were for ACS compared to Quintile 5 where 69.3% of the 80,010 PCIs were for ACS (proportion of patients who underwent PCI for ACS in quintiles 2,3, and 4 are 70.6%, 71.5%, and 69%, respectively).
Table 2. Baseline demographic characteristics of all patients stratified by quintile of PCI rate.
| Variable | Total #,% | Quintile 1 #,% | Quintile 2 #,% | Quintile 3 #,% | Quintile 4 #,% | Quintile 5 #,% |
|---|---|---|---|---|---|---|
| Total | 380981, 100 | 55727, 100 | 72942, 100 | 88886, 100 | 83416, 100 | 80010, 100 |
| Age Mean (SD) | 64.5, 12.2 | 64.5, 12.1 | 64.4, 12.2 | 64.8, 12.3 | 64.4, 12.2 | 64.5, 12.1 |
| Male | 255693, 67.1 | 39051, 70.1 | 49703, 68.1 | 59823, 67.3 | 55316, 66.3 | 51800, 64.7 |
| White Race | 341206, 89.6 | 49172, 88.2 | 63615, 87.2 | 79543, 89.5 | 76658, 91.9 | 72218, 90.3 |
| Private Insurance | 244820, 64.3 | 36012, 64.6 | 47037, 64.5 | 58442, 65.8 | 52345, 62.8 | 50984, 63.7 |
| Public Insurance | 217889, 57.2 | 30120, 54.1 | 41152, 56.4 | 49675, 55.9 | 47988, 57.5 | 48954, 61.2 |
| Non-US Insurance | 137, 0.04 | 20, 0.04 | 24, 0.03 | 59, 0.07 | 19, 0.02 | 15, 0.02 |
| No Insurance | 23817, 6.3 | 3070, 5.5 | 4934, 6.8 | 5734, 6.5 | 5350, 6.4 | 4729, 5.9 |
Table 3. Baseline clinical characteristics of all patients stratified by quintile of PCI rate.
| Variable | Total #,% | Quintile 1 #,% | Quintile 2 #,% | Quintile 3 #,% | Quintile 4 #,% | Quintile 5 #,% | |
|---|---|---|---|---|---|---|---|
| Total | 380981, 100 | 55727, 100 | 72942, 100 | 88886, 100 | 83416, 100 | 80010, 100 | |
| Current / Recent Smoker (w/in 1 year) | 108719, 28.6 | 14256, 25.6 | 20816, 28.6 | 24227, 27.3 | 25349, 30.4 | 24071, 30.1 | |
| Hypertension | 311080, 81.7 | 44082, 79.1 | 58911, 80.8 | 72158, 81.2 | 68230, 81.9 | 67699, 84.7 | |
| Dyslipidemia | 307237, 80.7 | 44379, 79.7 | 58068, 79.7 | 72534, 81.7 | 67152, 80.6 | 65104, 81.5 | |
| Family History of Premature CAD | 97210, 25.5 | 12745, 22.9 | 19586, 26.9 | 21481, 24.2 | 24056, 28.9 | 19342, 24.2 | |
| Prior MI | 116895, 30.7 | 15811, 28.4 | 21963, 30.1 | 27247, 30.7 | 25708, 30.8 | 26166, 32.7 | |
| Prior Heart Failure | 44787, 11.8 | 5221, 9.4 | 8337, 11.4 | 10097, 11.4 | 10239, 12.3 | 10893, 13.6 | |
| Prior Valve Surgery / Procedure | 5457, 1.4 | 745, 1.3 | 1057, 1.45 | 1373, 1.6 | 1178, 1.4 | 1104, 1.4 | |
| Prior PCI | 154064, 40.5 | 19835, 35.6 | 28157, 38.6 | 34980, 39.4 | 34911, 41.9 | 36181, 45.2 | |
| Prior CABG | 70942, 18.6 | 8540, 15.3 | 13109, 18.0 | 16230, 18.3 | 16855, 20.2 | 16208, 20.3 | |
| Currently on Dialysis | 8298, 2.2 | 1221, 2.2 | 1783, 2.5 | 1816, 2.0 | 1663, 2.0 | 1815, 2.3 | |
| Cerebrovascular Disease | 47072, 12.4 | 5811, 10.4 | 8740, 12.0 | 10920, 12.3 | 10508, 12.6 | 11093, 13.9 | |
| Peripheral Arterial Disease | 48300, 12.7 | 5892, 10.6 | 8827, 12.1 | 11156, 12.6 | 10713, 12.9 | 11712, 14.6 | |
| Chronic Lung Disease | 60486, 15.9 | 7140, 12.8 | 10219, 14.0 | 13067, 14.7 | 14174, 17.0 | 15886, 19.9 | |
| Diabetes Mellitus | 135509, 35.6 | 18218. 32.7 | 25760, 35.3 | 30758, 34.6 | 29993, 36.0 | 30780, 38.5 | |
| PCI Indication | |||||||
| Immediate PCI for STEMI | 53677, 14.1 | 9329, 16.7 | 11110, 15.2 | 13073, 14.7 | 10926, 13.1 | 9239, 11.6 | |
| PCI for STEMI (Unstable, >12 hrs from symptom onset) | 3217, 0.8 | 649, 1.2 | 572, 0.8 | 777, 0.9 | 641, 0.8 | 578, 0.7 | |
| PCI for STEMI (Stable, > 12 hrs from symptom onset) | 2210, 0.6 | 362, 0.7 | 431, 0.6 | 525, 0.6 | 439, 0.5 | 453, 0.6 | |
| PCI for STEMI (Stable after successful full-dose thrombolysis) | 1696, 0.5 | 348, 0.6 | 343, 0.5 | 359, 0.4 | 366, 0.4 | 280, 0.4 | |
| Rescue PCI for STEMI (after failed full-dose lytics) | 2047, 0.5 | 382, 0.7 | 446, 0.6 | 445, 0.5 | 434, 0.5 | 340, 0.4 | |
| PCI for high risk Non-STEMI or unstable angina | 171123, 44.9 | 24442, 43.9 | 32936, 45.2 | 41591, 46.8 | 37576, 45.1 | 34578, 43.2 | |
| Staged PCI | 24509, 6.4 | 2585, 4.6 | 4132, 5.7 | 5094, 5.7 | 6668, 8.0 | 6030, 7.5 | |
| Other | 122358, 32.1 | 17616, 31.6 | 22933, 31.5 | 26988, 30.4 | 26338, 31.6 | 28483, 35.6 | |
| CAD Presentation | |||||||
| No symptom, no angina | 35325, 9.3 | 4642, 8.3 | 6374, 8.7 | 8195, 9.2 | 8536, 10.2 | 7578, 9.5 | |
| Symptom unlikely to be ischemic | 11931, 3.1 | 1489, 2.7 | 2199, 3.0 | 2935, 3.3 | 2750, 3.3 | 2558, 3.2 | |
| Stable angina | 65030, 17.1 | 9297, 16.7 | 12858, 17.6 | 14204, 16.0 | 14302, 17.2 | 14369, 18.0 | |
| Unstable angina | 138774, 36.4 | 17834, 32.0 | 25413, 34.8 | 32028, 36.0 | 31507, 37.8 | 31992, 40.0 | |
| Non-STEMI | 68816, 18.1 | 11681, 21.0 | 13521, 18.5 | 16736, 18.8 | 13877, 16.6 | 13001, 16.3 | |
| ST-Elevation MI (STEMI) or equivalent | 61036, 16 | 10774, 19.3 | 12572, 17.2 | 14776, 16.6 | 12426, 14.9 | 10488, 13.1 | |
| Coronary Artery Stenoses | |||||||
| 0 | 21969, 6.4 | 2610, 5.1 | 3694, 5.6 | 5073, 6.4 | 4633, 6.1 | 5959, 8.4 | |
| 1 | 178870, 51.9 | 28113, 54.4 | 34661, 52.4 | 41736, 52.4 | 39093, 51.6 | 35267, 49.6 | |
| 2 | 90822, 26.4 | 13711, 26.5 | 17617, 26.6 | 20920, 26.3 | 19947, 26.3 | 18627, 26.2 | |
| 3 | 52732, 15.3 | 7293, 14.1 | 10169, 15.4 | 11857, 14.9 | 12135, 16.0 | 11278, 15.9 | |
| Presence of Proximal LAD Stenosis | 97810, 28.2 | 14842, 28.3 | 18955, 28.7 | 22789, 28.3 | 20942, 27.6 | 20282, 28.3 |
Abbreviations: CABG = coronary artery bypass grafting; CAD = coronary artery disease; LAD = left anterior descending; MI = myocardial infarction; PCI = percutaneous coronary intervention; STEMI = ST elevation myocardial infarction
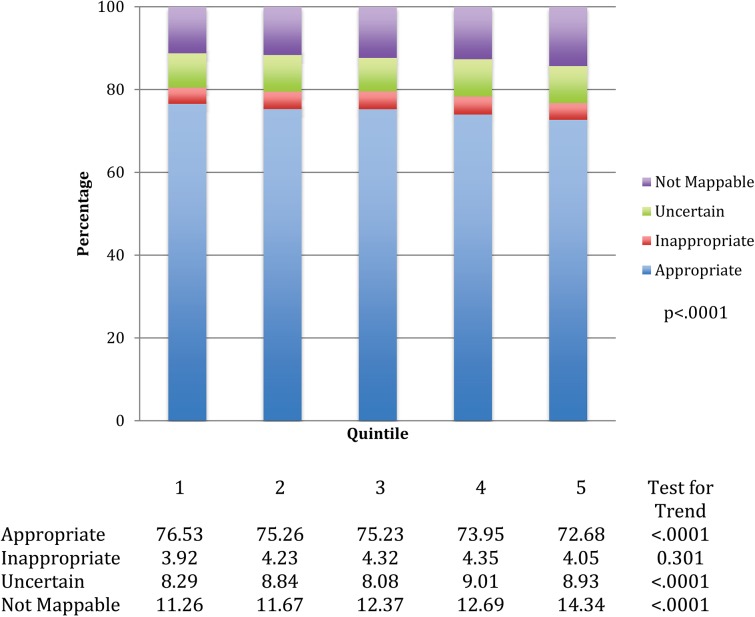
Appropriateness of PCI
The rates for appropriate, inappropriate, uncertain, and not mappable for all PCIs in each quintile are displayed in Fig 3. Lower utilization areas had a higher rate of appropriate PCIs (Quintile 1, 76.5%, Quintile 5, 72.7%) while there is an increase in rates of unmappable PCIs in higher utilization regions (Quintile 1, 11.3%, Quintile 5, 14.3%). There was a smaller variation seen in the rates of inappropriate PCI (from 3.92% in the lowest volume quintile vs. 4.19% in the higher quintiles).
Fig 3. Distribution of PCI appropriateness across HRR quintiles for all PCIs.
Shown is the application of the appropriate use criteria to quintiles of PCI utilization for all PCIs.
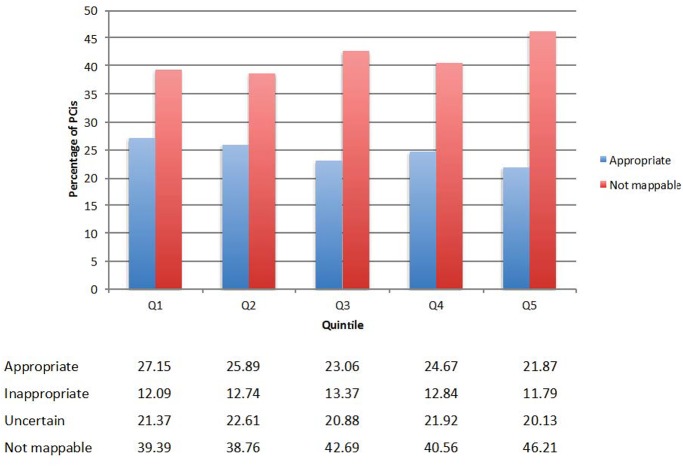
When stratified by clinical status, the rates of appropriate PCIs for acute indications was high (range 95.14%- 96.05%) across all the quintiles. However, the rates of appropriate PCIs for non-acute indications for each quintile varied across these regions and decreased from Quintile 1 to Quintile 5. Importantly, the rates of unmappable PCIs increased substantially from Quintile 1 to Quintile 5, with smaller variation in the rates of inappropriate PCI. With progressing from Quintile 1 to Quintile 5, the rates of appropriate PCI decreased from 27.15% to 21.87% while the ranges of inappropriate PCI were 11.79% to 12.74% and uncertain PCI were 20.13% to 22.61%, however the rates of unmappable PCI increased from 39.39% in Quintile 1 to 46.21% in Quintile 5 (Fig 4). A significant difference exists across the quintiles (p < .0001) for the entire cohort as well as among sub group of patients undergoing acute and non acute PCI. There was no difference in risk-adjusted mortality across quintiles of PCI utilization (Table 4).
Fig 4. Appropriateness use criteria classification of non- acute PCI across HRR quintiles of PCI utilization.
Shown is the application of appropriate use criteria to quintiles of PCI utilization for non-acute PCIs.
Table 4. In-hospital mortality rates by quintile of PCI rate.
| Quintile 1 | Quintile 2 | Quintile 3 | Quintile 4 | Quintile 5 | ||
|---|---|---|---|---|---|---|
| All PCIs | ||||||
| Adjusted mortality rate | 1.35 | 1.34 | 1.28 | 1.32 | 1.38 | |
| Acute PCIs | ||||||
| Adjusted mortality rate | 1.81 | 1.81 | 1.73 | 1.79 | 1.87 | |
| Non-acute PCIs | ||||||
| Adjusted mortality rate | 0.25 | 0.22 | 0.21 | 0.21 | 0.24 |
Abbreviations: PCI = percutaneous coronary intervention
Sensitivity Analysis
When we restricted the analysis to HRRs with 100% penetrance of the CathPCI Registry, there remained consistent variation in the proportion of acute and non-acute PCIs across utilization areas with lower utilization areas performing a higher percentage of acute cases. In Quintile 1, 73.27% of cases were for an acute indication compared to Quintile 5 where 66.76% of the PCIs were for ACS. (S2 Fig) The appropriateness of the cases progressively decreased from Quintile 1 to Quintile 5, due primarily to the greater use of PCI in ACS cases in the lower utilization regions. (S3–S5 Figs)
Discussion
In this large, national registry, we evaluated the association between geographic variation in PCI rates and the appropriateness of these procedures using contemporary Appropriate Use Criteria. We observed differences among quintiles of PCI utilization as there was a decreasing percentage of appropriate use of PCIs and an increasing percentage of not mappable PCIs with increasing PCI utilization rates. As PCI utilization increases, the percentage of total case volume comprised of non-acute cases also increases, where the appropriateness of intervention is often lower and the rates of cases that are not mappable are higher compared to acute cases. Importantly, despite variation in the level of appropriateness, there was no clear influence on mortality.
Leape et al. examined geographic variation in rates of coronary angiography and its correlation with appropriateness in 1990. [14] The authors utilized data from 23 counties in one state and found that overall rate of coronary angiography (per 10,000 Medicare beneficiaries) varied from 13 to 158 and inappropriate use varied from 8 to 75%. The data suggested a positive correlation with use rate and inappropriateness. Furthermore, inappropriate use accounted for a 28% variance in rates. However, when the authors excluded one county, the amount of variance attributable to inappropriate use dropped and the correlation became insignificant. This led the authors to conclude that inappropriate use occurs in both low and high utilization areas and the objective should not merely be a reduction in the number of procedures performed, but elimination of those performed inappropriately in high or low utilization areas.
It is in this background and the findings of the current study, that the unmappable cases fall under greater scrutiny. Although a large proportion of unmappable cases make it difficult to precisely determine appropriateness, it is possible that some of the unmappable cases are discretionary and PCI may be able to be avoided. Unmappable PCIs include non-ACS presentations when a stress test was not performed or the results were not available. Recent data from Abdallah and colleagues suggests that patients who undergo elective PCI without a stress test do not have more severe symptoms or angiographic disease as compared with those undergoing PCI following stress tests. [15] This indirectly suggests that a proportion of the unmappable PCIs are likely inappropriate and that a substantial number of such PCIs in the high utilization areas could potentially be avoided.
This large variation in unmappable PCIs may provide a valuable target for quality improvement. Since there is little clinical downside to delaying PCI in the setting of stable CAD, ensuring appropriate risk stratification to better clarify the potential benefits of PCI seems reasonable. This process has been facilitated by the ready availability of online and downloadable applications supported by ACC and SCAI and is already a part of clinical work flow at many institutions across the country. [16]
Despite variation in the ratio of acute / non-acute cases across quintiles of PCI utilization and the decreasing rate of appropriate PCIs in higher utilization areas, rates of mortality were largely unaffected. Given that variations in appropriateness were mainly influenced by non-acute cases, this finding is not surprising since the non-acute patients are generally healthier and post PCI mortality or complications in this population are exceedingly uncommon. Our findings mirror prior work demonstrating that the proportion of inappropriate cases for a hospital is not related to outcomes such as mortality. [17]
Study Limitations
The findings of this paper must be taken into context with the study’s limitations. Not all hospitals that perform PCIs within the United States participate in the CathPCI Registry. Additionally, the CathPCI Registry is a self-reported database and all cases do not undergo an audit. Furthermore, HRRs were excluded from the analysis given lack of penetrance of the CathPCI Registry within that HRR thereby excluding approximately 200,000 PCIs from analysis. This geographic-level analysis is also unable to tell us about individual patients and the appropriateness of their PCI. Some procedures that are considered inappropriate may indeed be appropriate when considering unique clinical features about the patient. Furthermore, the preferences of treatment choice by the patient were not assessed. Finally, the large proportion of unmappable cases highlighted not only reflects difficulty in applying the AUC to PCIs, but also to incomplete data sets. Of course, it is striking that there is a strong correlation between the number of unmappable PCIs and geographic variation in PCI use.
Conclusions
Geographic regions that have low PCI rates have a higher proportion of PCIs performed for appropriate indications per AUC. Areas of high PCI utilization appear to perform more elective PCI and many of these procedures could not be mapped by the AUC. Our study findings support the need to explore the utility of routine application of AUC classification prior to elective PCI as a strategy to optimize utilization of PCI.
Partners and Sponsors
CathPCI Registry is an initiative of the American College of Cardiology Foundation and The Society for Cardiovascular Angiography and Interventions.
Supporting Information
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Abbreviations
- PCI
percutaneous coronary intervention
- NCDR
National Cardiovascular Disease Registry
- AUC
appropriate use criteria
- ACS
acute coronary syndrome
- HRR
hospital referral region
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors have no support or funding to report.
References
- 1. Matlock DD, Groeneveld PW, Sidney S, Shetterly S, Goodrich G, Glenn K, et al. Geographic variation in cardiovascular procedure use among Medicare fee-for-service vs Medicare Advantage beneficiaries. JAMA 2013;310:155–162. 10.1001/jama.2013.7837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Journal of the American College of Cardiology 2011;58:e44–122. 10.1016/j.jacc.2011.08.007 [DOI] [PubMed] [Google Scholar]
- 3. Patel MR, Dehmer GJ, Hirshfeld JW, Smith PK, Spertus JA. ACCF/SCAI/STS/AATS/AHA/ASNC 2009 Appropriateness Criteria for Coronary Revascularization: a report by the American College of Cardiology Foundation Appropriateness Criteria Task Force, Society for Cardiovascular Angiography and Interventions, Society of Thoracic Surgeons, American Association for Thoracic Surgery, American Heart Association, and the American Society of Nuclear Cardiology Endorsed by the American Society of Echocardiography, the Heart Failure Society of America, and the Society of Cardiovascular Computed Tomography. Journal of the American College of Cardiology 2009;53:530–553. 10.1016/j.jacc.2008.10.005 [DOI] [PubMed] [Google Scholar]
- 4. Chan PS, Patel MR, Klein LW, Krone RJ, Dehmer GJ, Kennedy K, et al. Appropriateness of percutaneous coronary intervention. JAMA 2011;306:53–61. 10.1001/jama.2011.916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hannan EL, Cozzens K, Samadashvili Z, Walford G, Jacobs AK, Holmes DR, et al. Appropriateness of coronary revascularization for patients without acute coronary syndromes. Journal of the American College of Cardiology 2012;59:1870–1876. 10.1016/j.jacc.2012.01.050 [DOI] [PubMed] [Google Scholar]
- 6. Bradley SM, Maynard C, Bryson CL. Appropriateness of percutaneous coronary interventions in Washington State. Circ Cardiovasc Qual Outcomes 2012;5:445–453. 10.1161/CIRCOUTCOMES.111.964320 [DOI] [PubMed] [Google Scholar]
- 7. Ko DT, Guo H, Wijeysundera HC, Natarajan MK, Nagpal AD, Feindel CM, et al. Assessing the association of appropriateness of coronary revascularization and clinical outcomes for patients with stable coronary artery disease. Journal of the American College of Cardiology 2012;60:1876–1884. 10.1016/j.jacc.2012.06.056 [DOI] [PubMed] [Google Scholar]
- 8. Brindis RG, Fitzgerald S, Anderson HV, Shaw RE, Weintraub WS, Williams JF. The American College of Cardiology-National Cardiovascular Data Registry (ACC-NCDR): building a national clinical data repository. Journal of the American College of Cardiology 2001;37:2240–2245. [DOI] [PubMed] [Google Scholar]
- 9. Weintraub WS, McKay CR, Riner RN, Ellis SG, Frommer PL, Carmichael DB, et al. The American College of Cardiology National Database: progress and challenges. American College of Cardiology Database Committee. Journal of the American College of Cardiology 1997;29:459–465. [DOI] [PubMed] [Google Scholar]
- 10. Hendel RC, Patel MR, Allen JM, Min JK, Shaw LJ, Wolk MJ, et al. Appropriate use of cardiovascular technology: 2013 ACCF appropriate use criteria methodology update: a report of the American College of Cardiology Foundation appropriate use criteria task force. Journal of the American College of Cardiology 2013;61:1305–1317. 10.1016/j.jacc.2013.01.025 [DOI] [PubMed] [Google Scholar]
- 11. Wennberg DE BJ, Birkmeyer NJO. The Dartmouth Atlas of Cardiovascular Care Chicago: AHA Press; 1999. [Google Scholar]
- 12. Patel MR, Dehmer GJ, Hirshfeld JW, Smith PK, Spertus JA. ACCF/SCAI/STS/AATS/AHA/ASNC/HFSA/SCCT 2012 Appropriate use criteria for coronary revascularization focused update: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, Society for Cardiovascular Angiography and Interventions, Society of Thoracic Surgeons, American Association for Thoracic Surgery, American Heart Association, American Society of Nuclear Cardiology, and the Society of Cardiovascular Computed Tomography. Journal of the American College of Cardiology 2012;59:857–881. 10.1016/j.jacc.2011.12.001 [DOI] [PubMed] [Google Scholar]
- 13. Peterson ED, Dai D, DeLong ER, Brennan JM, Singh M, Rao SV, et al. Contemporary mortality risk prediction for percutaneous coronary intervention: results from 588,398 procedures in the National Cardiovascular Data Registry. Journal of the American College of Cardiology 2010;55:1923–1932. 10.1016/j.jacc.2010.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Leape LL, Park RE, Solomon DH, Chassin MR, Kosecoff J, Brook RH. Does inappropriate use explain small-area variations in the use of health care services? JAMA: the journal of the American Medical Association 1990;263:669–672. [PubMed] [Google Scholar]
- 15. Abdallah MS, Spertus JA, Nallamothu BK, Kennedy KF, Arnold SV, Chan PS. Symptoms and angiographic findings of patients undergoing elective coronary angiography without prior stress testing. The American journal of cardiology 2014;114:348–354. 10.1016/j.amjcard.2014.04.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.SCAI-QIT Appropriate Use Criteria App for Diagnostic Catheterization and Coronary Revascularization. Available: http://scaiaucapp.org/8/31/15.
- 17. Bradley SM, Chan PS, Spertus JA, Kennedy KF, Douglas PS, Patel MR, et al. Hospital percutaneous coronary intervention appropriateness and in-hospital procedural outcomes: insights from the NCDR. Circ Cardiovasc Qual Outcomes 2012;5:290–297. 10.1161/CIRCOUTCOMES.112.966044 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.