Abstract
Objective
Although South Asian populations have among the highest burden of type 2 diabetes in the world, their diabetes management remains poor. We systematically reviewed studies on South Asian patient’s perspectives on the barriers and facilitators to diabetes management.
Methods
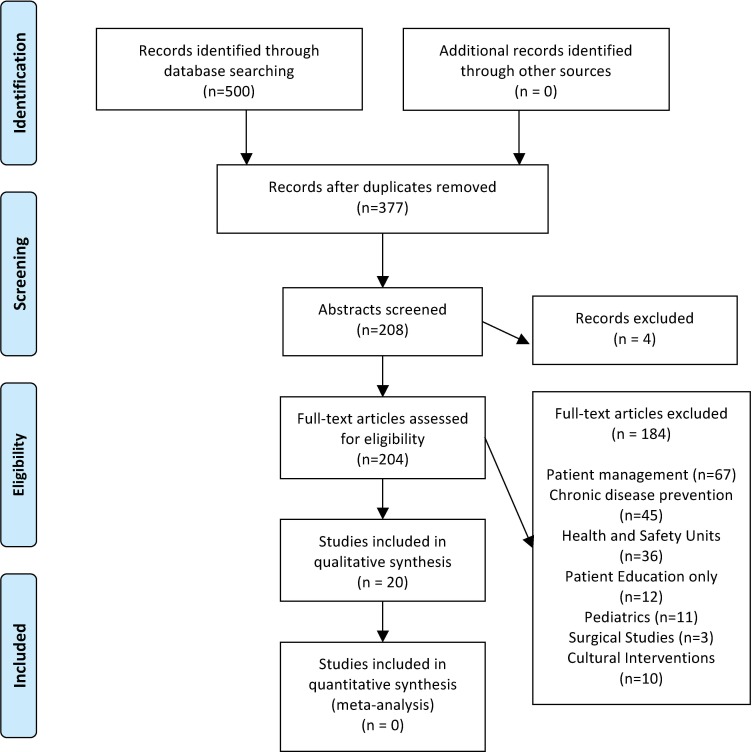
We conducted a literature search using OVID, CINHAL and EMBASE (January, 1990 –February, 2014) evaluating the core components of diabetes management: interactions with health care providers, diet, exercise, and medication adherence. South Asian patients were self-reported as Indian, Pakistani, Malaysian-Indian or Bangladeshi origin. From 208 abstracts reviewed, 20 studies were included (19 qualitative including mixed methods studies, 1 questionnaire). Barriers and facilitators were extracted and combined using qualitative synthesis.
Results
All studies included barriers and few facilitators were identified. Language and communication discordance with the healthcare provider was a significant barrier to receiving and understanding diabetes education. There was inconsistent willingness to partake in self-management with preference for following their physician’s guidance. Barriers to adopting a diabetic diet were lack of specific details on South Asian tailored diabetic diet; social responsibilities to continue with a traditional diet, and misconceptions on the components of the diabetic diet. For exercise, South Asian patients were concerned with lack of gender specific exercise facilities and fear of injury or worsening health with exercise. Patients reported a lack of understanding about diabetes medication management, preference for folk and phytotherapy, and concerns about the long-term safety of diabetes medications. Facilitators included trust in care providers, use of culturally appropriate exercise and dietary advice and increasing family involvement. Overall themes for the barriers included lack of knowledge and misperceptions as well as lack of cultural adaptation to diabetes management.
Conclusion
Diabetes programs that focus on improving communication, addressing prevailing misconceptions, and culture specific strategies may be useful for improving diabetes management for South Asians.
Introduction
South Asians represent approximately one-fifth of the global population and have a disproportionately higher incidence of type-2 diabetes mellitus. Diabetes occurs at 50% higher rates in South Asian patients compared to the general population [1]. Diabetes develops 5 to 10 years earlier and is one of the principle causes of premature heart attack and death in this population [1, 2]. Multiple randomized controlled trials identified pharmacological and non-pharmacological strategies to substantially reduce the risk of diabetes related complications and premature mortality. These effective strategies for chronic diabetes management are incorporated into diabetes guidelines and include: ongoing diabetes monitoring by a health care provider, adherence to a diabetic diet, exercise and medical therapy [3].
Despite clear evidence that diabetes management (dietary changes, regular exercise, and adherence to appropriate medications) leads to a 53–63% reduction in complications and a 46% reduction in mortality [4,5], diabetes management and control remain poor in South Asian patients. South Asians are less likely to exercise or follow a healthy diet compared to the general population [6]. Among South Asian patients with diabetes prescribed oral hypoglycemic agents, ACE inhibitor and statin therapy, only 40–45% were adherent to these medications [7]. North American studies identified that the majority (55%) of South Asian patients were above recommended A1C targets (target A1C ≤7%, the standard measure for the average level of blood sugar over the past 2–3 months), 36% were above blood pressure targets and 58% were above lipid level targets for diabetes [8]. South Asian patients were 24% less likely to achieve these critical targets than White patients [9] and had 60–113% higher A1C levels compared with the general population [10–12]. According to the International Diabetes Federation (IDF), the global health expenditure of diabetes including diabetes management and costs attributed to complications was $376 billion (USD) in 2010. This cost is expected to exceed $490 billion (USD) by 2030. Understanding patient level barriers and facilitators perceived or experienced underlying poor diabetes management is essential to inform the development of effective diabetes education and management programs to reduce risk of diabetes-related complications.
To help clarify the factors influencing diabetes management, we conducted a systematic review of qualitative and mixed methods studies investigating patient’s views, attitudes or beliefs on barriers and facilitators in the core components of diabetes management: interactions with health care workers, diet, exercise and medication adherence in South Asian patients with type 2 diabetes.
Methods
Data Sources and Searches
We conducted a literature search investigating patient reported barriers and facilitators in South Asian patients with type 2 diabetes. With a medical librarian, we conducted a search using OVID, CINHAL and EMBASE from January 1, 1990 to February 1, 2014. We also hand searched review articles on barriers and facilitators. We used the following medical subject headings and free text terms: India AND Diabetes Mellitus, Type-2 AND Management.mp, India AND Diabetes Mellitus, Type 2 AND Manage$.mp, India AND Diabetes Mellitus, Type 2 AND Intervention.mp, Pakistan AND Diabetes Mellitus, Type 2 AND Management.mp, Pakistan AND Diabetes Mellitus, Type 2 AND Manage$.mp, Pakistan AND Diabetes Mellitus, Type 2 AND Intervention.mp, Bangladesh AND Diabetes Mellitus, Type 2 AND Management.mp, Bangladesh AND Diabetes Mellitus, Type 2 AND Manage$.mp, and Bangladesh AND Diabetes Mellitus, Type 2 AND Intervention.mp.
Study Selection
We included qualitative studies that used either interviews or focus groups to examine barriers and facilitators to type-2 diabetes management as well as mixed methods quantitative studies that included surveys and interviews. South Asian patients were defined as of self-reported Indian, Pakistani, Malaysian-Indian or Bangladeshi origin. Studies with pediatric populations, type-1 diabetes, gestational diabetes, were excluded. Studies involving views from only health care workers and studies published before 1990 were also excluded. There was no language restriction. There were 500 records identified through the database searches, and 377 records after the duplicates were removed. Finally, there were 208 abstracts and full text articles assessed for eligibility. From 208 abstracts or full text articles reviewed, 20 studies were included in this review (19 qualitative or mixed methods with a qualitative component). Excluded studies consisted of 67 patient management studies, 45 chronic disease prevention studies, 36 studies using health and safety units, 32 studies of health care workers, 10 studies evaluating culturally tailored interventions, 12 based on patient education only, 11 pediatric, and 3 surgical studies.
Study Quality Assessment and Data Extraction
We assessed the quality and risk of bias of qualitative studies using CASP (Critical Appraisal Skills Program) [13], NICE-SCIE (National Institute for Health and Clinical Excellence-Social Care Institute of Excellence) criteria [14] as well as the NIH quality assessment tool for observational and cross-sectional studies [15]. The quality appraisal criteria for qualitative studies included: study purpose, design, type of reasoning involved, thinking of theoretical perspective of the researcher, saturation sampling, constant comparison, inductive/collaborated findings, decision trail developed and rules of analysis reported, process of transforming data into themes/codes, and reported triangulation (Table 1).
Table 1. Summary of Studies by Country.
| Country (Number of Studies) | Ethnicity | Sample Size | Female (%) | Age | Duration of Diabetes | Average Age |
|---|---|---|---|---|---|---|
| India (5) | Indian Malaysian | 1215 | 38.3 | 20–80 | 6.5 >10 5.95+4.42 | 46.5 |
| England (8) | BangladeshPakistani White Kashmiri Afro-Caribbean | 533 | 39.9 | 21–81 | 2–15 | 52.9 |
| Scotland (3) | BangladeshiIndian Pakistani | 123 | 65 | 30–71 | 0–16 | 47 |
| Norway (2) | Pakistani | 41 | 73 | 38–7 | 0.5–15 | 52 |
| USA (2) | BangladeshiIndian | 77 | 48.5 | 54–60 | >18 | 57 |
Data were collected by two reviewers in duplicate (TS, NK) on patient’s views, beliefs, understanding, attitudes and experiences on barriers and facilitators within diabetes management categories: healthcare worker interactions, exercise, diet, and medication adherence. We did not include other components of diabetes care including ophthalmology visits, foot care, and monitoring as there were insufficient data for these topics in the primary studies.
Data Synthesis and Analysis
We constructed evidence tables of the barriers and facilitators organized by diabetes management component. Study findings were also stratified among those studies where the participants lived in Western countries, and those living in South Asian countries.
For the data synthesis, we drew from Schutz’s first, second and third order qualitative synthesis framework for meta-ethnography [16]. A meta-ethnographic analysis is interpretive rather than purely aggregative. We first reviewed the direct quotations of participant’s views or beliefs presented in each study (first-order constructs) and the primary study author’s interpretations of the data (second-order constructs). Two authors (TS, NK) coded the first and second order constructs independently. There was a substantial amount of consistency between the coders and any conflicts were resolved by using an iterative process and discussion to reach consensus. We then determined the themes across the first and second order constructs to develop third order constructs. Two reviewers (TS, NK) met to analyze and discuss the first-and second-order constructs, resulting in continuous development and refinement of third-order constructs. These constructs were interpreted and organized into overall diabetes management barriers [17].
Results
Primary Study Characteristics
There were a total of 20 studies (n = 1980 participants) collected based upon the search terms from the online databases (Fig 1). Studies included participants originating from Bangladesh (n = 6), Pakistan (n = 7), and India (n = 9) (Table 2). As per to Table 1, studies were conducted in England (n = 8), Scotland (n = 3), Norway (n = 2), US (n = 2), and India (n = 5). The majority of the studies were qualitative studies [18–35], one cross sectional survey [36] and one mixed methods study [37]. Most qualitative studies used in-depth interviews and considered the ethnography (What is the culture of a group of people?) or phenomenology (What is it like to have a certain experience?) of the ethnic minority populations. The majority of participants were women and ages ranged between 20–80 years. Few studies included information on the participant’s religion.
Fig 1. Participant Flow Diagram.
From: Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and MetaAnalyses: The PRISMA Statement. PLoS Med 6(6): e1000097. doi:10.1371/journal.pmed1000097
Table 2. Study Characteristics.
| Author, year | Country | Setting | Participant Ethnicity | Typology | Sample Size | Women (%) | Age Range, years | Diabetes Duration, years | Average Age, years |
|---|---|---|---|---|---|---|---|---|---|
| Rhode 2003 [18] | England | 1 Hospital, 2 Diabetes Clinics, GP or Practice Nurse | Bangladeshi | Semi-structured, focused interviews | 55 | 67 | 21–81 | 2–15 | 51 |
| Rhode 2003 [19] | England | Central Diabetes Register | Bangladeshi | In-depth interviews | 12 | 67 | 43–75 | Mean 6 Bangladeshi; 9 Others | 59 |
| Chacko 2003 [20] | India | 3 Hospitals with diabetes treatment facilities | Malaysian | Patient observations, in-depth interviews | 50 | 52 | 42–75 | N/A | 58.5 |
| Meeto 2005 [21] | England | Diabetes Clinic | Pakistani, Caucasian | Semi-structured interviews | 49 | 68 Asian 58W | 20–80 | >1 | 50 |
| Naeem 2003 [22] | England | Diabetes Clinic | Kashmiri | Interview | 106 | 0 | >40–60+ | N/A | 50 |
| Kellehar1994 [23] | England | Health Centre | Bangladeshi | Interview | 40 | 37.5 | Vary | N/A | |
| Stone 2005 [24] | England | GP Clinics | Indian, Caucasian | Semi-structured interviews | 20 (15 SA, 5 W) | 55 (60 SA, 40 W) | 33–80 | 8.7 (SA), 11.4 (W) | 56.5 |
| Fagerli 2007 [25] | Norway | GP, Local Hospitals, group education program on diabetes | Pakistani | Semi-structured Interviews | 26 (15 diabetes) | 73 | 38–66 | 0–1+ | 52 |
| Lawton2006 [26] | Scotland | GP, Local Community | Pakistani, Indian | Interview | 23 Pakistani, 9 Indian | 52 Pakistani 56 Indian | 30–71 | 0–16+ | 50.5 |
| Fagerli 2005 [27] | Norway | GP, Local Hospital | Pakistani | Semi-structured interviews | 15 | 73 | 38–66 | 0.5–15 | 52 |
| Lawton 2005 [28] | Scotland | Primary care, Community sources | Pakistani, Indian | In-depth Interviews | 32 (9 Indian, 23 Pakistani) | 53 | 30–71 | 0–16+ | 50.5 |
| Greenhalgh 1998 [29] | England | Primary Care | Bangladeshi, 10, 9 Caucasian, 2 Afro-Caribbean | Narratives, semi-structured interviews, focus groups, and pile sorting exercises | 50 | 34 | 21–80 | N/A | 50.5 |
| Venkatesh 2013 [30] | US | Asian Indian organizations, stores, restaurants, relevant organizations | Indian | In-depth audiotaped interviews | 30 | 47 | 54–60 | >18 | 57 |
| Venkataraman 2011 [31] | India | Hospital | Indian | Focus groups, semi-structured interviews | 507 | 55.4 | Mean: 54 | Mean: 6.5 | 54 |
| Jepson 2012 [32] | Scotland | Natural Groups (exercise, mother & baby, prayer) | Bangladeshi, Indian, Pakistani | Focus groups, In-depth interviews | 59 | 56% | Middle-age | N/A | 40 |
| Islam 2012 [33] | US | Community Events | Bangladeshi | Focus groups | 47 | 50 | N/A | N/A | |
| Wilson 2010 [34] | India | GP & cardiologist offices | Indian | Formal & informal interviewsPatient observations | 200 | N/A | N/A | N/A | |
| Mendenhall 2012 [35] | India | Enrolled in cardio-metabolic Risk Reduction in South Asia Study | Indian | Interview | 59 | 49% | Over 20 | >10 (41%) | 20 |
| Patel 2012 [36] | India | Diabetes Centre | Indian | Questionnaire | 399 | 35% | Mean: 53 | 5.95+4.42 | 53 |
| Hawthorne 1999 [37] | England | Diabetes Center and GP run diabetic mini-clinics | Pakistani | Semi-structured interview & Questionnaire | 201 | 53% | Mean: 53 | Mean Women 5; men 7.8 | 53 |
GP refers to General Practitioner. W refers to White. SA refers to South Asian.
Quality of Primary Studies
For the qualitative and mixed methods studies, few studies reported information on whether sampling was done to saturation or the decision trail process (Table 3). For the single cross sectional survey, the quality was rated as good by the NIH scale.
Table 3. Study Quality.
| Strategy Identified | Number of Studies | Reference |
|---|---|---|
| Study Purpose | 7 | 19, 21, 25, 28–30, 33 |
| Ethnography | 7 | 19, 25, 28–30, 32, 33 |
| Phenomenology | 7 | 19, 21,25, 28–30, 33 |
| Grounded Theory | 1 | 20 |
| Participatory Action Research | 3 | 25, 28, 30 |
| Types of Reasoning Involved | 2 | 21,25 |
| Theoretical Perspective Included | 0 | |
| Sampling done to Saturation | 1 | 25 |
| Constant Comparison | 1 | 25 |
| Inductive and Collaborating findings | 6 | 19, 25, 28–30,33 |
| Decision Trail developed and rules of analysis reported | 3 | 19, 30, 33 |
| Adequate data transformation process into themes/codes | 7 | 19, 21,25, 28–30, 33 |
| Triangulation Reported | 6 | 19, 21, 24, 28–30 |
Barriers and Facilitators to Diabetes Management
The first and second order constructs for the barriers and facilitators for health care system interactions, physical activity, diet, and medication adherence are presented below and summarized in Table 4.
Table 4. Patient Perceptions of Barriers and Facilitators in Diabetes Management.
| Diabetes Management | Barrier | Facilitator | Reference |
|---|---|---|---|
| Health Care Worker Interaction | Patient autonomy | Bicultural, bilingual interpreters | 18,19, 21, 25–27, 36, 37 |
| Lack of time with HCW | Family support | ||
| Lack of empathy, reassurance by HCW | HCW trusted authority figures | ||
| Difficulty disclosing issues around management and non-compliance | |||
| Engaging in Physical Activity | Misconceptions of physical activity (harmful) | Needed to be enjoyable, social and culturally specific | 21, 22, 26, 27, 29, 31–34 |
| Lack of motivation, fatalism | Gender specific facilities | ||
| Culturally inappropriate facilities | |||
| Adopting a Diabetic Diet | Little specific information on dietary changes | Family Support | 20,21,23–25,27,29–31,33,34,37 |
| Misconceptions on what is a healthy diet | Specific information on traditional diet (portion, cooking method) | ||
| Cultural events and socializing was a deterrent to dietary adherence | |||
| Diabetes Medication Taking | Lack of understanding of role of medications and medication taking behaviors | 18–20,23,27,28,33 | |
| Concern for long term safety of medications | |||
| Preference for phytotherapy and folk remedies |
HCW refers to health care worker.
Patient interactions with the healthcare system
Eight studies reported patient views on interactions with health care workers. Most participants trusted their healthcare provider [18,25–27,36]. Despite this trust, participants also reported that language and communication discordance was a significant barrier in receiving information and understanding information on diabetes management [18,19,25–27,29]. Translation services were only intermittently provided and there was a reluctance to use interpreters from the participants’ own community [18]. Patients did not want to burden family members to act as translators [18,24], although some identified they preferred family members to act as translators as it would serve to reinforce the doctor’s advice when the patient was at home. South Asian patients considered the physician as the authoritative source of diabetes knowledge and management [18,25–27, 36] as “physicians were the best people to control glucose” [21]. There were mixed reporting of willingness and confidence to partake in self-management [25,26]. Some South Asian participants did not prefer self-management or autonomy and viewed self-efficacy negatively as they appreciated an authoritative approach [25,26]. Physician’s advice was viewed as superseding advice from others (e.g. family members, dieticians, nurses). In one study [36], 77% of patients reported their preferred source of advice was their family physician, whereas 4% preferred advice from dieticians and 1% from families or friends. Patients also found it challenging to disclose to physicians if they failed to comply with physician recommendations [25]. Although South Asian participants generally appreciated and relied on physicians to provide diabetes advice, they noted a lack of time with physicians and lack of empathy and reassurance from the physicians as a significant barrier to diabetes management [18,25]. Health care workers were seen as sometimes not being able to understand the patient’s economic, social and cultural factors that influenced the patient’s ability to manage their diabetes [21]. Patients also reported transportation difficulties, childcare and lack of available persons to accompany them to appointments as barriers to seeking physician care [2]. Patients in Western countries found that allied healthcare workers were better able to understand their needs and concerns since they had more time available instead of the limited time with the physician [18]. Patients in India found it easier to access their family physician versus dieticians, and were highly likely to follow a suggested diet plan [36].
Engaging in physical activity
There were 9 studies that included perceived barriers and facilitators to increased physical activity. The most common barriers included lack of motivation, lack of knowledge, and misconceptions on physical activity. Some South Asian participants held fatalistic beliefs around their ability to prevent diabetes complications [21,26,29,37]. In one study, exercise was thought to have little cultural meaning especially in the context of health and fitness [29]. Moreover, exercise was considered as potentially exacerbating illness or weakness [29, 34] and especially the elderly, should ‘just rest’. Some patients perceived that shortness of breath with increased levels of exercise was a sign of illness, therefore the patients often stopped engaging in physical activity [29]. There was anxiety surrounding safety and security for women when exercising outside of the home in addition to a lack of confidence to attend exercise classes [22,25,29–32]. There was also low understanding of health awareness and particularly, how to incorporate physical activity into their regular lifestyle. Some participants reported a difference in body image perception where a larger body size was considered more prosperous and healthy in this population. Other barriers to physical activity include cold weather, cost of exercise programs, fear of injury with exercise, and transportation difficulties [27,32]. Another significant barrier to physical activity was competing demands and lack of culturally appropriate exercise options [32]. Participants reported that motivators for exercise were to make exercise more enjoyable and role modeling from their own community. A social and cultural focus was also needed to improve their levels of exercise. Participants suggested bhangra dance, sex specific exercise classes and walking groups with friends as enjoyable and culturally appropriate physical activities [31–33].
Adopting a diabetic diet
Twelve studies included patient views on adopting a diabetic diet. Modifying the South Asian diet was most often considered difficult in diabetes management by South Asians given the central role of diet in South Asian culture [24]. Food played a key role in maintaining relationships with others and there was considerable social pressure to eat especially during social events [23,24]. Advice to avoid some traditional food items and devaluing the South Asian diet by health care workers as harmful was thought to act as an impediment to adopting dietary advice [27]. The most common barriers to adopting a healthy diabetic diet were lack of awareness on the components and quantities of that diet, general misconceptions on diet, and competing cultural expectations. The South Asian traditional diet typically has high levels of saturated fats, mainly from ghee, milk and yoghurt. Many patients reported not having enough specific details on what types of food to consider that would still be culturally appropriate [23,25,27,34,37]. Participants did not know how to respond to high glucose levels in their diet [37]. Participants believed they should avoid ‘strong foods’, including white sugar, lamb, beef, ghee, solid fat, and spices; and increase consumption of ‘weak foods’ such as boiled rice and cereals to improve their glycemic control [29]. South Asians, especially women, relied on traditional foods and used their traditional diet as a means of treatment for diabetes [20,21,33]. Examples of phytotherapy included using ‘karela’ (bitter gourd), okra, and grapefruits for glycemic control [21]. However, participants reported that healthcare providers were uninformed on whether or not the individuals were eating traditional foods with the purpose of improving hyperglycemia in addition to the prescribed medication [21]. Men and women did appear to have similar knowledge of food values [21, 29]. Both men and women found it challenging to adhere to their diabetic diet during social visits, weddings and extended travel to South Asian countries [21,24,33]. Some participants stated that families were an important source of support as well for maintaining the diabetic diet at home [31,33] whereas others felt family members were occasionally too strict in enforcing a diabetic diet or that not having family or social obligations led to having to eat less [30].
Medication taking behavior
Eight studies examined patients’ views on the barriers medication taking or medication adherence and none of the studies included facilitators. There was a lack of understanding that diabetes was a chronic condition that required ongoing and escalating medication therapy [18]. In a study of Bangladeshi patients, there was little impetus to take medicines to reduce diabetes-related mortality given South Asian’s tendency to have fatalistic views [23]. There was reluctance to initiate diabetes medications as South Asian patients felt this signaled their diabetes had deteriorated and they would be identified as “sick” [28]. One participant said; “If you start taking them, you become a patient.” [28] Although participants acknowledged the importance of taking diabetes medications, some participants stated that they deliberately and routinely reduced the amounts of medications. They believed these medications worked instantly and when patients felt they did not need them, or when they ate less, they did not need to be taken. Some participants reduced or missed dosages to avoid short-term side effects or when travelling overseas [27,28]. There was also a general concern that taking diabetes medications long term would be harmful [28]. There was considerable preference and usage of ayurvedic and phytotherapy as these treatments were believed to be effective but considerably safer than western medication [19, 20, 33]. South Asians were also reluctant to disclose to their healthcare worker if they were missing or reducing their diabetes medications [28].
Differences in barriers and facilitators in South Asians living in western countries and India
In comparing findings in studies conducted in Western countries and India, most barriers were consistent across countries. Preference for traditional therapies, perceptions that exercise depletes energy, and a priority to keep families well fed were similar among South Asians living in the West and India. Both groups considered the physician as the main source of information, physicians as an authority and described poor self-efficacy in diabetes self-management. However, patients living in India reported that they only sought care when they felt they had a problem and avoided routine diabetes care because of high costs. South Asians living in the West viewed lay sources of knowledge as a major influence on their behavior, difficulties with transportation, access to health care, and perceived diabetes care (physician visits etc.) as being a burden on their family. Barriers reported only among South Asians living in the West additionally included cold climate, language barriers and that advice was not considered culturally appropriate or specific enough to operationalize. Some South Asians living in the West also felt that their diabetes was better controlled when they would return to their native country.
Overarching Themes
Two overarching themes emerged from review of patient’s reported barriers from the primary studies: 1) lack of knowledge and prevailing misconceptions, and 2) lack of culturally specific management to effective diabetes management.
Lack of knowledge and misconceptions
Lack of knowledge was a theme pervasive across all aspects of diabetes management. Lack of specific and concrete culturally appropriate information was considered a significant barrier to diabetes knowledge. Language barriers and also preferences for information and direction from physicians were limiting factors for receiving knowledge. Receiving knowledge through families as translators had some noted limitations. Media, specifically television and newspapers were considered helpful sources of knowledge for women working inside the home [19].
Along with lack of knowledge, there were misconceptions within diabetes management as well as each component of diabetes management. Preventative care was not well understood as patients had a passive or fatalistic view towards their prognosis. Several common misconceptions included that exercise led to deteriorating health, understanding on what foods were appropriate for a diabetic diet, and medication taking behaviors.
Lack of culturally specific chronic care modifications
Throughout the components of diabetes care, there was a reported need for understanding of the South Asian culture and its impact on diabetes management. Dietary advice needed to be centered on concrete examples of South Asian traditional foods and ingredients. The role of western medications in addition to folk remedies also needed to be discussed. Sex specific facilities for exercise or safe environments for exercise were viewed as important especially for women [26]. Many of these barriers were more prevalent among South Asians living in Western countries.
Discussion
Our literature review revealed multiple experienced or perceived barriers and few facilitators to diabetes management in South Asian populations. The barriers and facilitators were generally similar among South Asian patients with diabetes living in Western countries and in South Asian countries, however with a few differences. The key themes across many aspects of diabetes management included lack of knowledge, prevailing misconceptions, and lack of culturally specific management as barriers to effective diabetes management. There were few studies that identified facilitators to management, but culturally appropriate strategies and family support was identified across various components of diabetes management.
Similar to South Asian participants in this review, limited knowledge of diabetes and language discordance between patient and provider are barriers to diabetes self-management in the general population, and in other non-English speaking ethnic groups [38]. Misperceptions of diabetes management are also common among ethnic groups. Some Hispanic Americans reported misconceptions that insulin therapy was harmful [39], held fatalistic beliefs, used folk healers and alternative treatments for diabetes management [40]. Culture also played a role in willingness to adhere to diabetes management. Family needs are considered paramount and adhering to a treatment regimen that takes time or resources away from family responsibilities is considered self-indulgent to Latino patients. In Chinese culture, the freedom to enjoy food is an essential component in one's quality of life [41].
The barriers identified for diabetes were also similar for other chronic diseases among South Asians. In a qualitative study of 91 participants of the Khush Dil program originating from Pakistan, Bangladesh and India living in Edinburgh, participants reported competing priorities, social pressures to not change their diet and stress as barriers to adopting a heart healthy diet and physical activity [42]. Barriers reported among South Asians to attend cardiac rehabilitation programs or cardiac prevention programs included lack of transportation, a sense of fatalism, the harmful effects of exercise, and language barriers [43]. Facilitators included family support, and spoken content rather than written literature [43]. There are few studies evaluating the effectiveness of addressing these barriers and facilitators for chronic disease management in South Asians. In a qualitative precede-proceed study in Canada to improve cardiac rehabilitation attendance by addressing barriers in South Asians, investigators stressed the importance of physician endorsement of the program given the strong emphasis that South Asians place on the physician as the major authoritative source of knowledge and expertise, making programs more accessible (provided transportation, accessible hours), family and community support that leverages the collectivism within the South Asian culture, caring staff and ongoing support from physicians. These factors were considered by the South Asian patients to account for their improved adherence and participation in cardiac rehabilitation programs [44].
Challenges In Developing Culturally Tailored Diabetes Management
Culturally tailored diabetes education programs have been shown to improve diabetes targets such as A1c compared to programs that were not culturally tailored in Hispanic and African-American patients [45]. Although diabetes education and other health interventions targeted to South Asian patients rely on bicultural and bilingual delivery of health information, from this review, the lack of knowledge and understanding suggests deeper cultural adaptations, aimed at addressing the groups’ cultural beliefs, knowledge and understanding are also needed [46]. Although diabetes education programs in western countries are heavily grounded in patient centeredness and empowerment, some South Asian patients may not actively follow these ideals, since they rely on tradition and authority [25, 26]. There is still low motivation for patients to become partners with healthcare providers to address diabetes management in part due to beliefs in fatalism. Health programs that include deeper cultural adaptations, addressing the cultural beliefs and culture based understanding of disease including poor understanding of the natural course and chronicity of disease and beliefs in fatalism may begin to help improve disease management. The importance of empathy, care, cultural sensitivity and clarity of advice from health care workers may also improve diabetes management in this group.
Changing diet in the South Asian community is likely difficult given the deep cultural significance of food and the important social role of diet in maintaining social relationships and tradition. Barriers to diet can be addressed through increasing the individual’s knowledge and awareness of what traditional foods are appropriate with additional specific details on portion size and cooking methods. A potential facilitator in dietary change was increasing family support and creating family level changes in the household diet. However, family involvement in diabetes prevention and weight loss studies in South Asian patients have not shown any benefit compared to care without family involvement [47].
A major component in achieving glycemic control in diabetes is through physical activity. Knowledge translation strategies would need to address culturally- based concerns including dispelling fears of injury or safety and overcoming the predominant view that elderly people should ‘just rest’. As regular exercise is not a significant part of South Asian culture, improving participation using peer or community role models, and readily available exercise facilities in local areas with a high South Asian population might mitigate reluctance to incorporate physical exercise into daily routines. These facilities would need to leverage gaining social networks and have a culturally appropriate social element (e.g. dance for some South Asian groups) which was considered a high priority for South Asian patients. Some of the other barriers to physical activity include the structural landmark of the facilities and activity sessions, such as gender specific especially women-only facilities. This type of implementation may help to address the lack of confidence to attend exercise class as especially reported by Muslim women.
Patients of South Asian descent in both western countries and South Asian countries appear to use both biomedicine and aryuvedic medicine in addition to self-therapy [20]. Although the use of both types of medications varies depending on the duration of diabetes, many of the patients hope to delay their dependence of bio medicinal drugs by using natural therapies such as herbs, and homeopathy [20]. Many of these patients find aryuvedic and plant therapy to be safer due to fewer perceived side effects [20]. Improving medication adherence in South Asian patients would also have to address fundamental misconceptions that diabetes medications need to be taken regularly to extract the maximum benefit and that diabetes is a chronic condition that often requires lifelong medications to prevent complications. Addressing concerns of long-term side effects against long-term benefits would also need to be discussed. Working with patients to incorporate both phytotherapy and western medications may be a culturally appropriate strategy to enhance adherence.
Although many barriers and facilitators were consistent among South Asians living in India and the West such as knowledge deficits and misperception, not surprisingly, the lack of cultural adaptation were reported by South Asians living in Western countries. These findings suggest that some interventions that focus on knowledge deficits and misperceptions may be translatable across countries, but appropriate cultural adaptation is still required in the West.
Limitations
There were several limitations in this study. There was a lack of information on facilitators for medication compliance, and lack of comparisons between ethnic groups. We were unable to stratify the results by sub-groups (e.g. elderly vs. younger) as these groups may have differing beliefs. Finally, although this review included 1980 participant views, the reported barriers and facilitators may not be representative within subgroups of the South Asian population with diabetes.
Conclusion
Our review, demonstrated several recurring themes of lack of knowledge, prevailing misconceptions and lack of culturally tailored diabetes management as key barriers to diabetes management from South Asian patient’s view. Culturally appropriate programs that focus on improving communication; discussing common misperceptions in the South Asian community on diabetes management and leveraging cultural beliefs and family as a resource may help to improve diabetes control.
Data Availability
As this is a systematic review, we have referenced all included papers and barriers, and facilitators may be found in these references.
Funding Statement
NAK was supported by a Michael Smith Foundation for Health Research Career Scientist Award, and KKS was supported by an Alberta Innovates-Health Solutions Health Scholar Award.
References
- 1. Khan NA, Wang H, Anand S, Jin Y, Campbell NR, Pilote L, et al. Ethnicity and sex affect diabetes incidence and outcomes. Diabetes Care. 2011;34(1):96–101. 10.2337/dc10-0865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Forouhi NG, Sattar N, Tillin T, McKeigue PM, Chaturvedi N. Do known risk factors explain the higher coronary heart disease mortality in South Asian compared with European men? Prospective follow-up of the Southall and Brent studies, UK. Diabetologia. 2006;49(11):2580–2588. [DOI] [PubMed] [Google Scholar]
- 3. Handelsman Y, Mechanick JI, Blonde L, Grunberger G, Bloomgarden ZT, Bray GA, et al. AACE Task Force for Developing Diabetes Comprehensive Care Plan. American Association of Clinical Endocrinologists Medical Guidelines for Clinical Practice for developing a diabetes mellitus comprehensive care plan. Endocr Pract. 2011;17 Suppl 2:1–53. [DOI] [PubMed] [Google Scholar]
- 4. Gaede P, Vedel P, Parving HH, Pedersen O. Intensified multifactorial intervention in patients with type 2 diabetes mellitus and microalbuminuria: the Steno type 2 randomised study. Lancet. 1999; 20;353(9153):617–22. [DOI] [PubMed] [Google Scholar]
- 5. Macisaac RJ, Jerums G. Intensive glucose control and cardiovascular outcomes in type 2 diabetes. Heart Lung Circ. 2011;20(10):647–54. 10.1016/j.hlc.2010.07.013 [DOI] [PubMed] [Google Scholar]
- 6. Liu R, So L, Mohan S, Khan N, King K, Quan H. Cardiovascular Risk Factors in Canadian Ethnic Populations: results from national surveys. Open Medicine. 2010;4(3):e143–53. [PMC free article] [PubMed] [Google Scholar]
- 7. Chong E, Wang H, King-Shier KM, Quan H, Rabi DM, Khan NA. Prescribing patterns and adherence to medication among South-Asian, Chinese and white people with Type 2 diabetes mellitus: a population-based cohort study. Diabet Med. 2014. August 11 10.1111/dme.12559 [DOI] [PubMed] [Google Scholar]
- 8. Shah BR, Cauch-Dudek K, Anand SS, Austin PC, Manuel DG, Hux JE. Absence of disparities in the quality of primary diabetes care for South Asians and Chinese in an urban Canadian setting. Diabetes Care. 2012;35(4):794–6. 10.2337/dc11-1845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gray J, Millett C, Saxena S, Netuveli G, Khunti K, Majeed A. Ethnicity and quality of diabetes care in a health system with universal coverage: population-based cross-sectional survey in primary care. J Gen Intern Med. 2007;22(9):1317–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mukhopadhyay B. Diabetes and cardiac disease in South Asians. Br J Diabetes Vasc Dis. 2005;5:253–9. [Google Scholar]
- 11. Mukhopadhyay B, Forouhi NG, Fisher BM, Kesson CM, Sattar N. A comparison of glycaemic and metabolic control over time among South Asian and European patients with type 2 diabetes: results from follow-up in a routine diabetes clinic. Diabet Med. 2006;23:94–8. [DOI] [PubMed] [Google Scholar]
- 12. Millett C, Netuveli G, Saxena S, Majeed A. Impact of pay for performance on ethnic disparities in intermediate outcomes for diabetes: a longitudinal study. Diabetes Care 2009;32:404–409. 10.2337/dc08-0912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. CASP. Qualitative research: appraisal tool. 10 questions to help you make sense of qualitative research. In. Oxford: Public Health Resource Unit; 2006. p. 1–4. Available: www.phru.nhs.uk/Doc_Links/Qualitative_Appraisal_Tool.pdf. [Google Scholar]
- 14. Rutter D, Francis J. Social Care Institute for Excellence. SCIE systematic research reviews: guidelines. December 2013. Available: http://www.scie.org.uk/publications/researchresources/rr01.pdf. [Google Scholar]
- 15. National Heart Lung and Blood Institute. NIH quality assessment tool for observational and cross-sectional studies. 2014. Available: http://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools/cohort.htm. [Google Scholar]
- 16. Schutz A. On Phenomenology and Social Relations: Selected Writings. Chicago, Ill: University of Chicago Press; 1970. [Google Scholar]
- 17. Campbell R, Pound P, Pope C, Britten N, Pill R, Morgan M et al. Evaluating meta-ethnography: a synthesis of qualitative research on lay experiences of diabetes and diabetes care. Soc Sci Med. 2003;56:671–84. [DOI] [PubMed] [Google Scholar]
- 18. Rhodes P, Nocon A. A problem of communication? Diabetes care among Bangladeshi people in Bradford. Health and Social Care in the Community. 2003;11(1):45–54. [DOI] [PubMed] [Google Scholar]
- 19. Rhodes P, Nocon A, Wright J. Access to Diabetes Services: The Experiences of Bangladeshi People in Bradford, UK. Ethnicity & Health. 2003;8(3):171–188. [DOI] [PubMed] [Google Scholar]
- 20. Chacko E. Culture and therapy: complementary strategies for the treatment of type-2 diabetes in an urban setting in Kerala, India. Social Science & Medicine. 2003;56:1087–1098. [DOI] [PubMed] [Google Scholar]
- 21. Meetoo D, Meetoo L. Explanatory models of diabetes among Asian and Caucasian participants. British Journal of Nursing. 2005;14(3):154–159. [DOI] [PubMed] [Google Scholar]
- 22. Naeem A. The role of culture and religion in the management of diabetes: a study of Kashmiri men in Leeds. The Journal of the Royal Society of Health Promotion. 2003;123:110–116. [DOI] [PubMed] [Google Scholar]
- 23. Kellehar D, Islam S. The problem of integration: Asian people and diabetes. Journal of the Royal Society of Medicine. 1994;87:414–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Stone M, Pound E, Pancholi A, Farooqi A, Khunti K. Empowering patients with diabetes: a qualitative primary care study focusing on South Asians in Leicester, UK. Family Practice. 2005;22(647–652). [DOI] [PubMed] [Google Scholar]
- 25. Fagerli RA, Lien M, Wandel M. Health worker style and trustworthiness as perceived by Paskistani-born persons with type 2 diabetes in Oslo, Norway. Health: An Interdisciplinary Journal for the Social Study of Health, Illness, and Medicine. 2007;11(1):109–129. [DOI] [PubMed] [Google Scholar]
- 26. Lawton J, Ahmad N, Hanna L, Douglas M, Hallowell N. Diabetes service provision: a qualitative study of the experiences and views of Pakistani and Indian patients with Type 2 diabetes. Diabetic Medicine. 2006;23:1003–1007. [DOI] [PubMed] [Google Scholar]
- 27. Fagerli RA, Lien ME, Wandel M. Experience of dietary advice among Pakistani-born persons with type 2 diabetes in Oslo. Appetite. 2005;45:295–304. [DOI] [PubMed] [Google Scholar]
- 28. Lawton J, Ahmad N, Hallowell N, Hanna L, Douglas M. Perceptions and experiences of taking oral hypoglycaemic agents among people of Pakistani and Indian origin: qualitative study. British Medical Journal. 2005;330 IS 7502 SP 1247(7502):1247–1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Greenhalgh T, Helman C, Chowdhury A. Health beliefs and folk models of diabetes in British Bangladeshis: a qualitative study. British Medical Journal. 1998;316:978–983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Venkatesh S, Weatherspoon L, Kaplowitz S, Song W. Acculturation and Glycemic Control of Asian Indian Adults with Type 2 Diabetes. Journal of Community Health. 2013;38:78–85. 10.1007/s10900-012-9584-6 [DOI] [PubMed] [Google Scholar]
- 31. Venkataraman K, Kannan A, Kalra O, Gambhir J, Sharma A, Sundaram K, et al. Diabetes Self-Efficacy Strongly Influences Actual Control of Diabetes in Patients Attending a Tertiary Hospital in India. Journal of Community Health. 2012;37:653–662. 10.1007/s10900-011-9496-x [DOI] [PubMed] [Google Scholar]
- 32. Jepson R, Harris FM, Bowes A, Robertson R, Avan G, Sheikh A. Physical Activity in South Asians: An In-Depth Qualitative Study to Explore Motivations and Facilitators. PLoS ONE. 2012;7(10):e45333–10. 10.1371/journal.pone.0045333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Islam N, Tandon D, Mukherji R, Tanner M, Ghosh K, Alam G, et al. Understanding the Barriers to and Facilitators of Diabetes Control and Prevention in the New York City Bangladeshi Community: A Mixed-Methods Approach. Research and Practice. 2012;102(3):486–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Wilson C. 'Eating, eating is always there': food, consumerism and cardiovascular disease. Some evidence from Kerala, south India. Anthropology & Medicine. 2010;17(3):261–275. [DOI] [PubMed] [Google Scholar]
- 35. Mendenhall E, Shivashankar R, Tandon N, Ali M, Narayan V, Prabhakaran D. Stress and diabetes in socioeconomic context: A qualitative study of urban Indians. Social Science & Medicine. 2012;75:2522–2529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Patel M, Patel I, Patel Y, Rathi S. Factors Associated with Consumption of Diabetic Diet among Type 2 Diabetic Subjects from Ahmedabad, Western India. Journal of Health, Population and Nutrition. 2012;30(4):447–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Hawthorne K, Tomlinson S. Pakistani moslems with Type 2 diabetes mellitus: effect of sex, literacy skills, known diabetic complications and place of care on diabetic knowledge, reported self-monitoring management and glycaemic control Diabetic Medicine. 1999; 16(7):1464–5491. [DOI] [PubMed] [Google Scholar]
- 38. Nam S, Chesla C, Stotts NA, Kroon L, Janson SL. Barriers to diabetes management: patient and provider factors. Diabetes Res Clin Pract. 2011;93(1):1–9. 10.1016/j.diabres.2011.02.002 [DOI] [PubMed] [Google Scholar]
- 39. Lipton RB, Losey LM, Giachello A, Mendez J, Girotti MH. Attitudes and issues in treating Latino patients with type 2 diabetes: views of healthcare providers. Diabetes Educ. 1998; 24: 67–71. [DOI] [PubMed] [Google Scholar]
- 40. Caban A, Walker EA. A systematic review of research on culturally relevant issues for Hispanic with diabetes. Diabetes Educ. 2006; 32:584–595. [DOI] [PubMed] [Google Scholar]
- 41. Yao G, Chung CW, Yu CF, Wang JD. Development and verification of validity and reliability of the WHOQOL-BREF Taiwan version. J Formos Med Assoc. 2002; 101: 342–351. [PubMed] [Google Scholar]
- 42. Netto G, McCloughan L, Bhatnagar A. Effective heart disease prevention: lessons from a qualitative study of user perspectives in Bangladeshi, Indian and Pakistani communities. Public Health. 2007;121(3):177–86. [DOI] [PubMed] [Google Scholar]
- 43. Cross-Bardell L, George T, Bhoday M, Tuomainen H, Qureshi N, Kai J. Perspectives on enhancing physical activity and diet for health promotion among at-risk urban UK South Asian communities: a qualitative study. BMJ Open. 2015;5(2):e007317 10.1136/bmjopen-2014-007317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Banerjee AT, Grace SL, Thomas SG, Faulkner G. Cultural factors facilitating cardiac rehabilitation participation among Canadian South Asians: a qualitative study. Heart Lung. 2010;39(6):494–503. 10.1016/j.hrtlng.2009.10.021 [DOI] [PubMed] [Google Scholar]
- 45. Liu JJ. Davidson E, Bhopal RS, White M Johnson MRD, Netto G, et al. Adapting health promotion interventions to meet the needs of ethnic minority groups: mixed-methods evidence synthesis. Health Technology Assessment. 2012; 16 (44). 10.3310/hta16440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Resnicow K, Baranowski T, Ahluwalia JS, Braithwaite RL. Cultural sensitivity in public health: defined and demystified. Ethn Dis 1999;9:10–21. [PubMed] [Google Scholar]
- 47. Admiraal WM, Vlaar EM, Nierkens V, Holleman F, Middelkoop BJ, Stronks K, et al. Intensive lifestyle intervention in general practice to prevent type 2 diabetes among 18 to 60-year-old South Asians: 1-year effects on the weight status and metabolic profile of participants in a randomized controlled trial. PLoS One. 2013;8(7):e68605 10.1371/journal.pone.0068605 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
As this is a systematic review, we have referenced all included papers and barriers, and facilitators may be found in these references.