SUMMARY
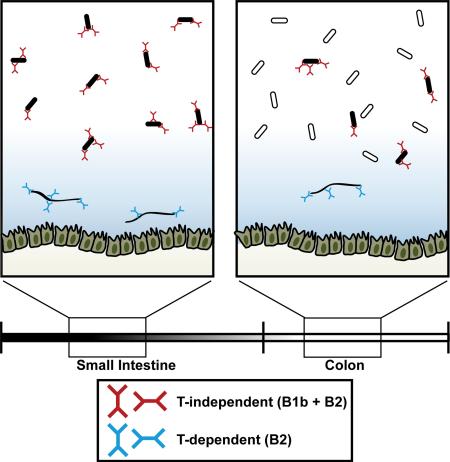
Immunoglobulin A (IgA) is prominently secreted at mucosal surfaces and coats a fraction of the intestinal microbiota. However, the commensal bacteria bound by IgA are poorly characterized and the type of humoral immunity they elicit remains elusive. We used bacterial flow cytometry coupled with 16S rRNA gene sequencing (IgA-Seq) in murine models of immunodeficiency to identify IgA-bound bacteria and elucidate mechanisms of commensal IgA targeting. We found that residence in the small intestine, rather than bacterial identity, dictated induction of specific IgA. Most commensals elicited strong T-independent (TI) responses that originated from the orphan B1b lineage and from B2 cells, but excluded natural antibacterial B1a specificities. Atypical commensals including segmented filamentous bacteria and Mucispirillum evaded TI responses but elicited T-dependent IgA. These data demonstrate exquisite targeting of distinct commensal bacteria by multiple layers of humoral immunity and reveal a specialized function of the B1b lineage in TI mucosal IgA responses.
Graphical Abstract
INTRODUCTION
Host-commensal symbiosis is mediated at mucosal surfaces by secreted host-derived factors including mucus, antimicrobial peptides, and immunoglobulin A (IgA) (Pabst, 2012). Mammals invest significant resources into IgA production: more than 80% of all human plasma cells secrete IgA and reside in the intestinal lamina propria. IgA can mediate protective immunity to enteric pathogens including viruses, bacteria, and toxins (Pabst, 2012). However, IgA also contributes to intestinal homeostasis. Mice and humans with defective IgA secretion show increased susceptibility to inflammatory bowel disease, celiac disease, and allergy (Cunningham-Rundles, 2001; Moon et al., 2015). IgA may regulate commensal community composition, gene expression, and motility, which in turn influence host epithelial physiology and innate immunity (Cullender et al., 2013; Fagarasan et al., 2002; Kawamoto et al., 2014; Peterson et al., 2007). Notably, IgA coating of commensal bacteria can be detected by flow cytometric and microscopic analysis of fecal samples from healthy mice and humans (Kau et al., 2015; Kroese et al., 1996; Palm et al., 2014; Tsuruta et al., 2010; Tsuruta et al., 2009; van der Waaij et al., 1996). However, the commensal bacteria bound by IgA are poorly characterized and the mechanisms by which they induce specific IgA are unclear.
Mucosal IgA+ plasma cells can be generated by both T-dependent (TD) and T-independent (TI) mechanisms. However, the relative contributions of each pathway remain unclear. TD responses are typically directed against protein antigens and occur in gut-associated lymphoid tissues including Peyer's patches (PPs) and mesenteric lymph nodes (mLNs), where germinal centers (GCs) are constitutively active. TD responses require signals from CD4+ T follicular helper (Tfh) cells that direct the selection and differentiation of high affinity GC B cells into long-lived plasma cells. In contrast, TI responses may occur both in organized lymphoid tissues and in non-lymphoid tissues (Tezuka et al., 2011; Tsuji et al., 2008). In both TD and TI pathways, factors in the intestinal microenvironment such as transforming growth factor β (TGF-β), interleukin 10 (IL-10), and retinoic acid direct class switch recombination to the IgA isotype (Pabst, 2012). TI IgA responses may produce primarily ‘natural,’ polyreactive specificities with low affinity for commensal bacteria (Kubinak et al., 2015; Pabst, 2012; Slack et al., 2012; Stephens and Round, 2014), but have been demonstrated against a limited number of commensal model antigens (Macpherson et al., 2000). Thus, although protective immune responses to many enteric pathogens are TD (Pabst, 2012), it is unclear whether IgA coating of commensal bacteria is more dependent on TD or TI responses.
While TI antigens can stimulate circulating follicular B2 B cells, they can also activate innate B1 B cells that reside primarily in the peritoneal cavity (Baumgarth, 2011). In contrast, TD responses are thought to predominantly involve B2 B cells. Both B1 and B2 B cells can differentiate into intestinal IgA+ plasma cells, although the relative contributions of these lineages remain controversial (Kroese et al., 1989; Macpherson et al., 2000; Thurnheer et al., 2003). Two subsets of B1 B cells, B1a and B1b, are present in the peritoneal cavity. Although limited data suggest differential capacity of B1a and B1b to undergo IgA class switch recombination (Roy et al., 2013), it is not known whether both subsets coat commensal bacteria in vivo. Peritoneal B1a secrete ‘natural’ antibodies that react with conserved microbial antigens and have been hypothesized to contribute to control of the microbiota (Kroese et al., 1989; Pabst, 2012). In contrast, very little is known about the role of B1b except that they can generate protective TI responses against Borrelia hermsii and Salmonella typhimurium outer membrane proteins and Streptococcus pneumoniae capsular polysaccharides after systemic infection (Alugupalli et al., 2004; Gil-Cruz et al., 2009; Haas et al., 2005).
To characterize the commensal bacterial targets of IgA, we utilized bacterial flow cytometry coupled with 16S rRNA gene sequencing (IgA-Seq) (Kau et al., 2015; Kawamoto et al., 2014; Palm et al., 2014). We found that IgA coated many but not all commensals in the homeostatic state and that dramatic differences were associated with bacterial localization along the gastrointestinal tract. Using murine genetic models of immunodeficiency, we found that most IgA-bound taxa were specifically targeted by TI IgA. We further demonstrated that natural antibacterial B1a specificities did not contribute to IgA coating. In contrast, innate B1b - a phenotypically related but poorly understood, “orphan” lineage - and adaptive B2 B cells each contributed diverse commensal-reactive specificities. Finally, we identified an atypical subset of commensals that evaded TI responses but elicited TD IgA. Together, these data indicate that multiple layers of humoral immunity are elicited by distinct commensal bacteria in the small intestine and reveal a novel specialization for the B1b lineage in mucosal TI responses.
RESULTS
Distinct regulation of IgA synthesis in the small intestine and colon of mice and humans
To study the commensal bacteria targeted by IgA under homeostatic conditions, we established a flow cytometric assay to visualize IgA-bound (IgA+) bacteria in murine feces. We found that approximately 20% of bacteria were IgA+ in the feces of wild-type (WT) C57BL/6 mice and verified that this staining was specific and absent from Rag2−/−γ−/−c and Aicda−/− feces (Figure 1A), as reported previously (Kau et al., 2015; Kawamoto et al., 2014; Kroese et al., 1996; Palm et al., 2014; Tsuruta et al., 2010; Tsuruta et al., 2009; van der Waaij et al., 1996). While the frequency of IgA+ bacteria in the colon was relatively constant, we found substantial differences along the gastrointestinal tract. IgA coated a significantly greater fraction of bacteria in the small intestine than the colon (40-80% IgA+ vs 10-30% IgA+; Figure 1B), as reported previously (Kroese et al., 1996; Tsuruta et al., 2009). This correlated with significantly higher titers of luminal free IgA in the small intestine (Figure 1B) and 10-15 fold more IgA+ plasma cells in the small intestinal lamina propria relative to the colonic lamina propria (Figure 1B). Similar trends were apparent in WT BALB/c and C3H mice (data not shown). We also observed a higher frequency of IgA+ bacteria in small intestinal aspirates of healthy humans relative to colonic aspirates (Figure 1C). These data suggest that IgA responses against commensal bacteria are most prominent in the small intestine.
Figure 1. IgA responses predominantly target commensal bacteria of the small intestine.
(A) Representative staining of C57BL/6 feces and negative controls showing staining in the presence of excess purified IgA and of Rag2−/− Il2rg−/− mice lacking B cells or Aicda−/− mice lacking IgA. All bacterial flow cytometry plots were gated FSC+SSC+SYTO BC+DAPI−. (B) Representative staining and quantification of IgA+ bacteria measured by flow cytometry (n=12) or free IgA measured by ELISA (n=19) or absolute numbers of IgA+ plasma cells. Data compiled from five independent experiments. (C) Staining and quantification of IgA+ bacteria in ileal or colonic aspirates from healthy humans. Lines connect samples from the same patient (n=6). (D) Representative pre- and post-MACS purity analysis of IgA+ and IgA− fractions. (E) Average relative abundance of taxa in indicated fractions as assessed by 16S sequencing. Duodenal and colonic samples were taken from the same mice, n=3. (F) Log10 relative abundance of each taxa in the IgA+ divided by relative abundance in IgA− from panel (E). (G) Quantification of average % of colonic IgA+ or IgA− taxa found at >1% relative abundance in the duodenum (black) or found at <1% relative abundance in the duodenum (white) in panel (E). See also Figure S1.
IgA predominantly targets commensal bacteria of the small intestine
To identify commensal bacteria targeted by IgA, we fractionated samples into highly pure IgA+ and IgA− fractions by stringent magnetic purification with an autoMACS separator (Figure 1D), and classified bacteria present in each fraction by IgA-Seq. We found that colonic bacteria markedly segregated into IgA+ and IgA− taxa (Figure 1E, F), as recently reported (Kau et al., 2015; Palm et al., 2014). Numerous taxa were heavily enriched in the colonic IgA+ fraction, suggesting specific targeting by IgA (Figure 1F). Conversely, numerous colonic taxa were not targeted by IgA and were instead enriched in the IgA− fraction (Figure 1E, F). These trends were also apparent in human colonic samples (Figure S1). In stark contrast to the colon, duodenal bacteria did not segregate into IgA+ and IgA− taxa (Figure 1E, F). Instead, most duodenal taxa were found equally represented in both fractions. These data, as well as the high frequency of IgA+ bacteria in the duodenum (Figure 1B), suggest that most duodenal commensals elicit specific IgA whereas many colonic commensals do not.
We reasoned that segregation of colonic bacteria into IgA+ and IgA− taxa could be explained if 1) Most bacteria indigenous to the colon were not targeted by IgA; and 2) Colonic IgA+ bacteria also reside in the small intestine. In support of this, we found that the colonic IgA+ fraction closely resembled the duodenal community whereas the colonic IgA− fraction was mostly composed of taxa indigenous to the colon (Figure 1E). In total, more than 90% of colonic IgA+ bacteria were present at >1% relative abundance in the duodenum (Figure 1G). A member of Bacteroidetes, S24-7, was the only taxon found appreciably in the colonic IgA− fraction and at >1% relative abundance in the duodenum, but this taxon was also found enriched in the IgA+ fraction in both locations (Figure 1E-G). Thus, nearly all colonic IgA+ taxa were also abundant in the small intestine whereas most IgA− taxa were abundant only in the colon.
To assess whether colonic IgA+ bacteria could establish residence in the small intestine, we colonized germ free mice with either IgA+ or IgA− colonic fractions and analyzed small intestinal and colonic communities 28 days later. Consistent with origins in the small intestine, colonic IgA+ bacteria stably colonized the jejunum of germ free mice and gave rise to a community that closely resembled the input community (Figure 2A). In contrast, the colonic community of these mice did not resemble the input community, likely representing outgrowth of minor contaminants in the input fraction (Figure 1D). Beta diversity-based analysis of bacterial communities further verified that small intestinal communities of recipient mice were more similar to the IgA+ input than colonic communities (Figure 2B). Mice colonized with a colonic IgA− inoculum showed an opposite pattern: IgA− bacteria stably colonized the colon and gave rise to a colonic community that resembled the IgA− inoculum (Figure 2A). In contrast, the small intestinal communities of these mice did not resemble the inoculum. Beta diversity-based analysis verified that colonic communities were more similar to the IgA− inoculum than small intestinal communities (Figure 2B). These data support the hypothesis that colonic IgA+ bacteria also reside in the small intestine whereas colonic IgA− bacteria are indigenous to the colon.
Figure 2. Colonic IgA+ and IgA− bacteria differentially colonize the small intestine or colon.
(A) Average relative abundance of indicated taxa in the jejunum or colon of germ free mice colonized with IgA+ colonic bacteria (n=4) or mice colonized with IgA− colonic bacteria (n=3). Input fractions used to colonize recipient germ-free mice were from WT B6 mice. Recipients of IgA+ or IgA− inocula were housed in separate gnotobiotic isolators and mice were analyzed 28 days after colonization. (B) Beta diversity analysis comparing intestinal microbial communities of mice colonized with IgA+ colonic bacteria or IgA− colonic bacteria indicate similarity between samples shown in (A). Branch length is scaled to the weighted UniFrac distance.
In summary, we conclude that IgA predominantly targets small intestinal commensals and that most small intestinal bacteria elicit specific IgA. In contrast, bacteria found primarily in the colon are not major targets of IgA.
T-independent and T-dependent IgAs coat distinct commensal bacteria
Commensal-specific IgAs have been posited to be largely TD (Kubinak et al., 2015; Palm et al., 2014; Stephens and Round, 2014). However, the specificity of TD IgA remains poorly understood and it is not clear whether GC reactions target all IgA+ commensals or only a subset. Although mucosal GCs depend in part on signals from the microbiota (Casola et al., 2004; Kubinak et al., 2015), we detected GC B cells, Tfh cells, and IgA in germ-free mice, suggesting that non-microbial antigens such as dietary antigens may also stimulate TD responses (data not shown). Seminal work by Macpherson and colleagues demonstrated that TI IgA could react with model antigens expressed by E. coli or with lysates from the model culturable commensal Enterobacter cloacae (Macpherson et al., 2000). However, it is unclear whether most commensal bacteria elicit TI responses in vivo and the commensals targeted by TI specificities have not been characterized.
To determine whether TI IgA is sufficient to coat commensal bacteria, we examined IgA responses in Tcrb−/−d−/− mice and Tcrb+/−d+/− littermate controls. Tcrb−/−d−/− mice lack all αβ and γδ T cells and thus cannot mount TD antibody responses (Macpherson et al., 2000). Tcrb−/−d−/− mice did not form GCs in mLNs and PPs but had normal numbers of B220+ IgA+ class-switched B cells (Figure 3A, B), as previously reported (Casola et al., 2004; Tezuka et al., 2011). Despite this, small intestinal and colonic lamina propria B220−IgA+ plasma cells were reduced 10-fold in Tcrb−/−d−/− mice (Figure 3C), consistent with previous reports (Macpherson et al., 2000). Tcrb−/−d−/−IgA+ small intestinal plasma cells displayed a mixed surface IgAhi and IgAlo phenotype while WT cells were largely IgAlow; colonic IgA+ plasma cells were IgAhi in both Tcrb−/−d−/− mice and controls (Figure 3C). Surprisingly, we observed substantial commensal IgA coating in Tcrb−/−d−/− mice (Figure 3D). Indeed, IgA+ bacteria were found at identical frequencies to co-housed littermate controls and no appreciable differences in IgA staining intensity were apparent (Figure 3D). These observations suggest that TI IgA may account for most commensal bacterial coating.
Figure 3. T-independent and T-dependent IgAs coat distinct commensal bacteria.
(A) Representative staining and absolute numbers of indicated populations in the mLN, (B) PP, or (C) small intestinal and colonic lamina propria of Tcrb−/−d−/− mice or Tcrb+/−d+/− littermate controls. CD95 by Gl7 plots were gated CD19+. B220 by IgA plots were gated Tcrb−CD3− in the mLN and PP and Lin− (CD3, Tcrb, CD4, CD11c, NK1.1, F4/80) in the intestinal lamina propria. Data compiled from three independent experiments. (D) Representative staining and quantification of IgA+ bacteria in Tcrb−/−d−/− mice (n=8) and littermate controls (n=9). Data compiled from four independent experiments. (E) (Left panel) Free IgA in Tcrb−/−d−/− mice (n=8) and littermate controls (n=9) or (Right panels) Endogenous IgA coating in the ileum or colon of co-housed B6 and Rag1−/− mice and staining of Rag1−/− bacteria with B6 free IgA, as indicated. (F) Relative enrichment of taxa in the colonic IgA+ fraction of controls (black) or knockouts (white). n=6 each genotype, representative of two independent experiments. See also Figure S2.
While commensal-specific IgA appeared largely intact in Tcrb−/−d−/− mice, free IgA was significantly reduced (Figure 3E) (Macpherson et al., 2000). As this compartment was dramatically affected by the loss of T cells, we considered that it may contain TD specificities against non-microbial antigens and therefore assessed whether free IgA could bind commensal bacteria. We cohoused WT C57BL/6 mice with Rag1−/− mice for three weeks, which equilibrated microbial communities (Figure S2A). We then isolated ileal or colonic free IgA from WT mice and used it to stain Rag1−/− ileal or colonic bacteria, respectively. While some free IgA reacted with Rag1−/− bacteria, this staining was faint and insufficient to restore IgA coating to WT frequencies, even at high staining concentrations >100 μg/mL (Figure 3E). Thus, commensal-reactive specificities appear to be dilute in the free IgA and this compartment may contain primarily TD specificities against other luminal antigens.
To identify commensal bacteria targeted by TI IgA, we performed IgA-Seq on colonic and jejunal samples from Tcrb−/−d−/− mice and co-housed littermate controls. Co-housed Tcrb−/−d−/−mice and Tcrb+/−d+/− littermates displayed largely overlapping small intestinal and colonic microbial communities (Figure S2B). Most IgA+ bacteria found in controls were equally enriched in the IgA+ fraction of Tcrb−/−d−/− mice (Figure 3F, S2C). This trend was apparent in both the colon and jejunum (Figure 3F, S2C). These data suggest that most IgA+ bacteria induce robust TI responses.
We identified two taxa, segmented filamentous bacteria (SFB) and Mucispirillum, that were absent from the IgA+ fraction of Tcrb−/−d−/− mice but enriched in the IgA+ fraction of Tcrb+/−d+/− littermate controls (Figure 3F, S2B). This pattern was observed in both colonic and jejunual samples (Figure 3F, S2B). Thus, TD specificities appear necessary for IgA coating of these taxa. Notably, both SFB and Mucispirillum interact closely with the intestinal epithelium in the terminal ileum (Lecuyer et al., 2014; Robertson et al., 2005). We hypothesize that SFB andMucispirillum may possess atypical cell wall structures that poorly stimulate TI responses and may therefore come into close contact with the mucosa, allowing sampling by antigen-presenting cells and priming of TD IgA responses.
Together, these data suggest that TD and TI responses may coat non-overlapping commensal bacterial taxa. While most IgA+ bacteria induce strong TI responses, atypical commensals such as SFB and Mucispirillum exclusively elicit TD responses.
Germinal centers and somatic hypermutation are dispensable for commensal coating
We found prominent TI IgA coating in Tcrb−/−d−/− mice, but it was possible that these mice had defects related to the absence of T cells but unrelated to TD IgA. Therefore, we sought to validate these observations by examining bacterial coating in two additional models.
We first examined IgA responses in CD4-Cre Bcl-6fl/fl (Bcl-6ΔT) mice, in which conditional deletion of the transcription factor BCL-6 in T cells prevents Tfh differentiation and GC formation (Hollister et al., 2013). Bcl-6ΔT mice lacked GCs and Tfh but had normal numbers of B220+IgA+ B cells in mLNs and PPs (Figure 4A). Bcl-6ΔT small intestinal IgA+ plasma cell numbers were reduced three-fold compared to controls (Figure 4A). Similar to Tcrb−/−d−/− mice, bacterial IgA coating in Bcl-6ΔT mice was identical to controls and no differences in staining intensity were apparent (Figure 4B).
Figure 4. Germinal centers and somatic hypermutation are dispensable for commensal coating.
(A) Absolute numbers of indicated populations in the mLN, PP, or small intestinal lamina propria of CD4-Cre Bcl-6 flfl mice or littermate controls. Data compiled from three independent experiments. (B) IgA bacterial coating, compiled from two independent experiments. (C) Fold enrichment of indicated taxa in colonic IgA+ fraction of Bcl-6ΔT mice or co-housed littermate controls. n=3 each genotype, representative of two independent experiments. (D) Absolute numbers of indicated populations in the mLN, PP, or small intestinal lamina propria of Aicda−/− mice or Aicda+/− littermate controls. Data compiled from two independent experiments. (E) IgM bacterial coating (Aicda−/− mice) or IgA bacterial coating (Aicda+/−) mice. Data compiled from two independent experiments. (F) Fold enrichment of indicated taxa in colonic IgM+ fraction of Aicda−/− mice or IgA+ fraction of Aicda+/− mice. n=5 each genotype. See also Figures S3 and S4.
IgA-Seq revealed that all IgA+ commensal bacteria induced potent GC-independent IgA responses (Figure 4C) and that IgA+ bacteria in littermate controls were equally enriched in the IgA+ fraction of co-housed Bcl-6ΔT mice. We found that SFB and Mucispirillum were IgA+ in Bcl-6ΔT mice, suggesting that coating these bacteria is TD but GC-independent. These data support the conclusion that IgA+ commensal bacteria prominently induce TI responses.
As a second approach, we examined bacterial coating in mice lacking activation-induced cytidine deaminase (AID; encoded by Aicda). AID is required for somatic hypermutation (SHM) and class-switch recombination and thus Aicda−/− mice produce unmutated antibodies of the IgM isotype (Fagarasan et al., 2002). We observed Tfh and GCs in Aicda−/− mice (Figure 4D), and Aicda−/− mice had B220−IgM+ but not B220−IgA+ plasma cells in their small intestinal lamina propria (Figure 4D), as reported previously (Fagarasan et al., 2002). As expected, we found no IgA+ bacteria in Aicda−/− mice (Figure 1A). Instead, we readily detected IgM+ bacteria in Aicda−/− mice but not in Aicda+/− or Rag1−/− controls (Figure S3A). The frequency of IgM+ bacteria in Aicda−/− mice was identical to the frequency of IgA+ bacteria in Aicda+/− littermate controls (Figure 4E).
To identify bacteria coated in the absence of SHM, we performed IgM-Seq on Aicda−/− mice and IgA-Seq on co-housed Aicda+/− littermate controls (Figure S3B). IgM+ bacteria in Aicda−/− mice were identical to IgA+ bacteria in controls and all taxa were equally enriched in the IgM+ fraction of Aicda−/− mice and the IgA+ fraction of controls (Figure 4F). SFB and Mucispirillum were both strongly IgM+ in Aicda−/− mice, further suggesting that coating of these taxa is TD but independent of SHM.
Together, these data indicate that GCs and SHM are dispensable for IgA coating of commensal bacteria and support the hypothesis that commensal-specific IgA is primarily TI.
Exaggerated coating of S24-7 in a model of Tfh hyper-sufficiency
As a complementary approach, we analyzed IgA coating in a model of Tfh hyper-sufficiency. Our laboratory recently identified the E3 ubiquitin ligase Cullin-3 (CUL3) as a co-repressor that complexes with BCL-6 and limits Tfh differentiation (Mathew et al., 2014). Conditional deletion of CUL3 in T cells (CD4-Cre Cul3flfl; Cul3ΔT) results in mLN hyperplasia driven by spontaneous, cell-intrinsic, antigen-specific expansion of Tfh and T follicular regulatory (Tfr) cells in the absence of observable pathology (Mathew et al., 2014). This expansion drove a 10-15-fold increase in mLN GC B cells and B220+IgA+ B cells (Figure S4A) and a corresponding increase in B220−IgA+ plasma cells in the proximal small intestinal lamina propria (Figure S4B). Cul3ΔT mice had an increased frequency of IgA+ bacteria compared to co-housed littermate controls (Figure S4C). Increased IgA coating was clearly driven by exaggerated TD responses against a single taxon, S24-7 (Figure S4D). Cul3ΔT mice also showed a notable absence of Mycoplasmataceae, which were abundant in littermate controls (Figure S4D). S24-7 did not require T cells for IgA targeting, as its relative enrichment in the IgA+ fraction was not altered in Tcrb−/−d−/− mice (Figure 3F, S2B). These data suggest that S24-7 can induce TD responses but, unlike SFB and Mucispirillum, does not require TD specificities to become IgA+.
Commensal-specific IgA+ plasma cells differentiate from B1b and B2 B cell precursors
IgA+ plasma cells can derive from both B1 and B2 B cell precursors, although the relative contributions of these lineages remain controversial (Kroese et al., 1989; Macpherson et al., 2000; Thurnheer et al., 2003). Limited evidence based on mixed bone marrow-peritoneal cell chimeric mice suggest that many IgA+ plasma cells in Tcrb−/−d−/− mice may be of B1 origin (Macpherson et al., 2000). However, it is unclear whether both B1 and B2 B cells give rise to commensal-specific IgA and whether these lineages contribute differentially to IgA coating of certain commensal taxa.
Analysis of B1 B cells is complicated by a lack of genetic tools, such as fate-mapping models, to study these cells in vivo. Moreover, genetic alterations that disrupt B1 lineage development involve BCR signaling-related molecules that also disrupt the activation and function of B2 B cells (Baumgarth, 2011). Therefore, to assess whether B1 or B2 B cells were sufficient to generate commensal-specific IgA, we reconstituted immunodeficient Rag1−/− mice with exclusively B1 or B2 B cells by transferring pure sorted populations. We initially established groups of Rag1−/− recipients reconstituted by: 1) Intraperitoneal (i.p.) transfer of B1 B cells; 2) i.p. B1 B cells + splenic CD4+ and CD8+ T cells (B1+T); 3) Intravenous (i.v.) transfer of B2 B cells; and 4) i.v. B2 B cells + splenic CD4+ and CD8+ T cells (B2+T). We readily detected IgA+ plasma cells and bacterial IgA coating in mice reconstituted with either B1 or B2 B cells (Figure 5A-C). Addition of T cells did not affect B1 differentiation into IgA+ plasma cells but did induce free IgA, albeit at low titers (Figure 5A-C). In contrast, T cells markedly increased the number of B2 B cell-derived IgA+ plasma cells and supported generation of high titers of free IgA (Figure 5A-C). Thus, TI B1 B cells and TI and TD B2 B cells can coat commensal bacteria while free IgA is predominantly derived from TD B2 B cells.
Figure 5. Commensal-specific IgA+ plasma cells differentiate from B1b and B2 B cell precursors.
(A)Representative staining and (B) absolute numbers of small intestinal or colonic IgA+ plasma cells recovered from Rag1−/− mice that received the indicated sorted populations. B1 populations were transferred i.p. (500,000 B1, 1,000,000 CD4/CD8 T cells, or 250,000 B1a or B1b) and B2 populations were transferred i.v. (1,000,000 B2, 1,000,000 CD4/CD8 T cells). Mice were analyzed 5 weeks after transfer. Data compiled from six independent experiments and two separate sorts for each transferred population. (C) IgA bacterial coating or free IgA in indicated recipient mice. (D) Immunoglobulin heavy chain repertoire sequencing of indicated populations. Tree plots are shown - each shape indicates a unique IgH CDR3 and size is scaled to relative clonal abundance. (E) Frequency of VH11 gene segments within the populations shown in (D) or number of sequences containing the indicated canonical B1a CDR3's. See also Figure S5.
We next assessed the ability of peritoneal B1a and B1b subsets to differentiate into IgA+ plasma cells by i.p. transfer of sorted B1a or B1b into Rag1−/− recipients. While B1b B cells gave rise to a substantial population of IgA+ plasma cells and coated commensal bacteria, B1a B cells did not differentiate into IgA+ plasma cells (Figure 5A-C). We verified that both B1a and B1b B cells stably reconstituted the peritoneal cavity of recipient mice (Figure S5). To further assess whether B1a B cells contribute to the IgA+ plasma cell pool, we performed immunoglobulin repertoire sequencing of peritoneal B1a and B1b B cells, splenic B2 B cells, WT IgA+ plasma cells, and Tcrb−/−d−/− IgA+ plasma cells. The B1a B cell repertoire is enriched in canonical rearrangements of the VH11 gene family that encode specificities toward conserved microbial antigens such as phosphorylcholine (Baumgarth, 2011). Indeed, we found that the B1a repertoire was partially restricted and that approximately 8% of sequences were of the VH11 gene family (Figure 5D, E). The B1a repertoire also contained prominent clonal populations with conserved CDR3 sequences representing the VH11, VH1-55, and VH1-9 gene families (Figure 5D, E). In contrast, VH11 gene segments made up a negligible fraction of the repertoires of splenic B2, peritoneal B1b, WT IgA+ plasma cells, or Tcrb−/−d−/− IgA+ plasma cells and canonical B1a CDR3s were completely absent (Figure 5D, E). The peritoneal B1b repertoire was broad and of comparable diversity to that of splenic B2 B cells with little evidence of clonal expansion or conserved immunoglobulin rearrangements. Together, these data suggest that B1a B cells do not contribute to the IgA+ plasma cell repertoire or IgA coating of commensals. We conclude that commensal-specific IgA is derived from B1b and B2 B cell precursor populations, although the precise contributions of each subset remain unclear due to limitations in cell transfer studies and a lack of genetic tools to dissect these responses in intact mice.
TI B1b and B2 B cells coat diverse and overlapping commensal bacterial taxa
To identify commensal bacteria bound by B1b or B2-derived IgA, we performed IgA-Seq on colonic samples from Rag1−/− mice reconstituted with B1 or B2 B cells. This analysis revealed that TI B1b and B2 B cells were each sufficient to coat a diverse array of commensal bacteria (Figure 6). B1b and B2 coated overlapping bacterial taxa and there were no apparent differences in efficacy of coating certain taxa by either subset (Figure 6). This is consistent with the observation that both B1b and B2 B cells possess broad and diverse immunoglobulin repertoires (Figure 5D). Addition of T cells did not alter the taxa targeted by B1b or B2 B cells, further supporting the conclusion that most commensal bacteria primarily induce TI IgA (Figure 6).
Figure 6. B1b and B2 B cells coat diverse and overlapping commensal bacterial taxa.

Fold enrichment of indicated taxa in colonic IgA+ fractions of Rag1−/− mice reconstituted with sorted B cell populations, as described in Figure 5. n=3 each group of mice, compiled from two independent experiments.
TI antibodies bind specifically to commensal bacteria
TI IgA responses may give rise to polyreactive specificities (Mestecky, 2005; Pabst, 2012). Further, IgA may interact with bacteria nonspecifically via the IgA fragment crystallizable (Fc) region or secretory component (Mathias and Corthesy, 2011). We generated recombinant monoclonal antibodies from single Tcrb−/−d−/− small intestinal IgA+ plasma cells and engineered them to express the human IgG1 Fc instead of mouse IgA Fc. Five out of five antibodies recognized Rag1−/− small intestinal or colonic commensal bacteria (Figure 7). Each antibody bound to a discrete bacterial subset and their mixture stained an even greater fraction of bacteria, revealing distinct specificities. Recognition was specific, as none of the antibodies reacted with the colonic commensal Bacteroides fragilis (Figure 7).
Figure 7. TI antibodies bind specifically to commensal bacteria.

Staining of total small intestinal or colonic bacteria from Rag1−/− mice or pure cultures of Bacteroides fragilis with indicated recombinant monoclonal antibodies derived from single Tcrb−/−d−/− small intestinal IgA+ plasma cells and engineered to express human IgG1 Fc instead of mouse IgA Fc Staining was performed using supernatants from transduced HEK293T cells expressing indicated antibody constructs. Untransfected supernatant was used as a negative control. Data representative of two independent experiments.
DISCUSSION
The commensal bacteria targeted by IgA have remained enigmatic. Recent studies suggest that IgA targets particularly immunogenic or invasive bacteria (Kau et al., 2015; Palm et al., 2014). In contrast, we found that anatomical location was the primary factor that determined whether a particular taxon elicited an IgA response. Under homeostatic conditions, most small intestinal bacteria were IgA+ and induced specific IgA. Although a fraction of colonic bacteria were IgA+, colonic IgA+ taxa were also abundant in the small intestine and homed to the small intestine upon transfer into germ free mice. It is possible that colonic IgA+ bacteria represent small intestinal contaminants rather than indigenous colonic flora, and distinct physiological properties may contribute to the differential ability of colonic IgA+ and IgA− commensals to colonize the small intestine and colon. However, it seems unlikely that small intestinal bacteria are more immunogenic than colonic bacteria. Instead, this anatomical regulation is likely due to extensive priming of commensal-specific IgA+ plasma cells in secondary lymphoid tissues accompanying the small intestine. PPs and isolated lymphoid follicles are predominantly associated with the small intestine and possess a specialized epithelium that allows sampling of luminal antigens (Tsuji et al., 2008). Our data suggest that these tissues prime IgA against nearly all bacteria present in the small intestinal lumen.
Previous work has suggested that TI IgA responses generate low affinity antibodies that react poorly with commensal bacteria (Fagarasan et al., 2002; Kubinak et al., 2015; Pabst, 2012; Slack et al., 2012; Stephens and Round, 2014). Further, recent studies of dysbiotic mice suggested that many commensals may elicit TD responses (Palm et al., 2014). In contrast, we found strong commensal Ig coating in mice lacking T cells, GCs, or SHM. These data indicate that most commensals elicit strong TI responses and that TI IgA is completely sufficient to coat most commensal bacteria at frequencies and staining intensities found in WT mice. This conclusion was also strongly supported by our finding that five out of five antibodies generated from Tcrb−/−d−/− small intestinal IgA+ plasma cells recognized commensal bacteria. Although we did not directly measure their affinity, these TI antibodies were clearly sufficient to brightly stain commensal bacteria. TI responses generate short-lived plasma cells, and active turnover of commensal-specific plasma cells may facilitate rapid, dynamic IgA responses upon exposure to novel commensal antigens. TI responses may also prevent pathological activation of commensal-specific T cells by sequestering bacteria away from antigen-presenting cells in the intestinal epithelium.
TI responses may promote the generation of polyreactive specificities (Mestecky, 2005; Pabst, 2012), and IgA may bind nonspecifically to bacteria via the Fc region or secretory component (Mathias and Corthesy, 2011). However, by generating recombinant monoclonal antibodies from single Tcrb−/−d−/− IgA+ plasma cells engineered to express the human IgG1 Fc region instead of mouse IgA Fc, we demonstrated Fab-dependent binding to discrete subsets of commensal bacteria but not to cultured B. fragilis. Ongoing work in our laboratory is focused on characterizing the commensal bacteria and specific antigens recognized by these antibodies.
B1a cells constitute the most abundant peritoneal B cell lineage and have been extensively investigated and shown to produce natural IgM antibodies with antimicrobial and self reactivities. However, the minor “sister” B1b lineage has remained largely elusive and has only been reported to participate in humoral responses against B. hermsii, S. typhimurium, and S. pneumoniae (Alugupalli et al., 2004; Gil-Cruz et al., 2009; Haas et al., 2005). Our results extend these early reports and reveal a specialization of the B1b lineage in TI IgA responses against intestinal commensal bacteria. Future work should address the development of B1b cells and the sites at which they encounter intestinal antigens and undergo class-switch recombination in vivo.
Previous work has suggested that TI B1a B cells may give rise to ‘natural’ IgA in the form of intestinal free IgA, which resembles ‘natural’ low-affinity IgM found in circulation in the absence of immunization (Baumgarth, 2011; Mestecky, 2005; Pabst, 2012; Slack et al., 2012). However, we found that the IgA+ plasma cell immunoglobulin repertoire did not include canonical ‘natural’ B1a specificities and that B1a B cells did not differentiate into IgA+ plasma cells, consistent with a previous study (Roy et al., 2013). IgA plasma cells contributing to the free IgA compartment appeared to be predominantly derived from TD B2 B cells. Thus, although many potential antigens may stimulate free IgA, this compartment does not represent ‘natural’ IgA and appeared largely specific for non-microbial antigens.
Interestingly, SFB and Mucispirillum evaded TI IgA and instead elicited TD specificities to become IgA coated. Yet, IgA coating of these taxa was independent of GCs and SHM and thus these organisms may induce IgA by atypical mechanisms that are dependent on T cells or T cell-derived factors. SFB is known to be particularly immunogenic and can induce formation of GCs and tertiary lymphoid structures as well as effector T cell differentiation (Lecuyer et al., 2014). SFB also induces large quantities of free IgA that is not SFB-specific (Lecuyer et al., 2014). In contrast to SFB, the immunogenicity of Mucispirillum remains uncharacterized. Ongoing work in our laboratory is focused on culturing and characterizing the properties of this organism. Notably, SFB and Mucispirillum both closely associate with the intestinal epithelium in the terminal ileum (Lecuyer et al., 2014; Robertson et al., 2005). Thus, these organisms may inhabit similar niches and possess atypical immunogenic properties, allowing them to evade TI responses and come into close contact with the mucosa where they can be sampled by antigen-presenting cells and elicit TD responses.
We consistently observed that most small intestinal commensal bacteria were IgA+, however we found no instances in which 100% were IgA+. As small intestinal IgA− bacteria appeared taxonomically similar to IgA+ bacteria, a fraction of bacteria may escape coating. This may result from phase variation of surface capsular polysaccharide antigens (Peterson et al., 2007). Alternatively, commensal-specific IgA may be limiting or may be actively degraded by bacterial IgA proteases (Moon et al., 2015). Understanding the specificity of individual IgA antibodies will shed light on this important issue.
We found that ~20% of colonic bacteria were typically IgA+, similar to reports by Kroese et al. (1996) and Tsuruta et al. (2009), but higher than the ~8% reported by Palm et al. (2014). These differences may be technical, as we used a polyclonal anti-IgA antibody whereas Palm et al. (2014) used a monoclonal antibody. Palm et al. (2014) also described a population of IgAhi bacteria that was enriched in commensals with pathogenic properties and largely targeted by TD IgA. This observation may be limited to a dysbiotic flora, as we did not observe an IgAhi population in healthy mouse microbiota.
In summary, our data reveal the prominent role of the enigmatic B1b lineage in control of the microbiota, and suggest a model whereby multiple layers of humoral immunity contribute to homeostatic IgA coating of microbiota in the small intestine. Most commensals induce TI responses from B1b and B2 B cells and these responses sequester bacteria away from the intestinal epithelium, preventing T cell activation. However, atypical commensals including SFB and Mucispirillum evade TI responses and penetrate the mucus layer, where they interact with antigen presenting cells and prime T cell responses. Humoral regulation of commensal bacteria may have represented a substantial evolutionary force promoting the diversification and maintenance of peripheral B cell lineages, including the elusive B1b lineage. While these data clarify the homeostatic regulation of commensal-specific IgA, a further understanding of the antigens targeted by IgA may shed light on the regulation of IgA responses and allow opportunities for therapeutic intervention in microbiota-associated pathologies such as inflammatory bowel disease, obesity, diabetes, and celiac disease.
EXPERIMENTAL PROCEDURES
Mice
8-12 week old knockout mice were compared to co-housed littermate controls and maintained under strict SPF conditions. Germ-free C57BL/6 mice were housed at the University of Chicago gnotobiotic facility and experimental groups were housed in separate gnotobiotic isolators. See also Supplemental Experimental Procedures.
Antibodies and Flow Cytometry
Conjugated antibodies purchased from commercial vendors were used to stain samples prior to analysis on a LSRII flow cytometer (Becton Dickinson), sorting on a FACSAria (Becton Dickinson), or separation with an autoMACS (Miltenyi). Data were analyzed using FlowJo (TreeStar). See also Supplemental Experimental Procedures.
Analysis of IgA+ bacteria, IgM+bacteria and free IgA
Homogenized intestinal contents were resuspended at 0.1 mg/μL in PBS with protease inhibitors (Sigma), homogenized, and centrifuged at 400g to remove large debris. Supernatant was filtered through a sterile 70 μm strainer and centrifuged at 8000g to pellet bacteria. This supernatant was collected and assayed for free Ig by ELISA. The bacterial pellet was resuspended in PBS 0.25% BSA with SYTO BC (Life Technologies) and 5% goat serum and then stained with biotinylated goat anti-mouse IgA, goat anti-human IgA, or goat anti-mouse IgM (Southern Biotech). After washing, bacteria were stained with streptavidin-APC (BioLegend). Bacteria were washed and resuspended in PBS 0.25% BSA with DAPI (Life Technologies) prior to flow cytometry using a low FSC and SSC threshold to allow bacterial detection. See also Supplemental Experimental Procedures.
Human Samples
Human study was approved by the Institutional Review Board at the University of Chicago. Healthy subjects undergoing routine colonoscopy were recruited at their procedure and informed consent was obtained from all subjects. See also Supplemental Experimental Procedures.
16S rRNA Gene Sequencing and Microbial Community Analysis
Bacterial DNA was extracted and16S rRNA gene amplicons were generated and sequenced on an Illumina MiSeq. Sequence data was processed and analyzed using QIIME (Caporaso et al., 2010) and Primer-6 (Primer-E Ltd). Sequence data is publicly available through MG-RAST (Meyer et al., 2008) under project 14533. See also Supplemental Experimental Procedures.
Rag1−/− Cell Transfers
Indicated populations were sorted on a FACSAria cell sorter (Becton Dickinson) and post-sort samples were verified for purity. Combinations of 500,000 peritoneal B1, 250,000 B1a, 250,000 B1b, and 1,000,000 splenic T cells were injected intraperitoneally into Rag1−/− mice. Combinations of 1,000,000 splenic B2 and 1,000,000 splenic T cells were injected intravenously. Recipients were analyzed 5 weeks after transfer. See also Supplemental Experimental Procedures.
Immunoglobulin Repertoire Analysis
RNA was extracted from sorted samples using an RNeasy kit (Qiagen) and sent on dry ice to iRepertoire, Inc. for cDNA synthesis, PCR amplification, and sequencing on an Illumina MiSeq. See also Supplemental Experimental Procedures.
Monoclonal Antibody Generation
Recombinant monoclonal antibodies were generated from sorted single IgA+ plasma cells and expressed as chimeric human IgG1 constructs. Culture supernatants from transfected 293T cell cultures were sterile filtered and used for staining of intestinal bacteria at 2 μg/mL. See also Supplemental Experimental Procedures.
Statistical Analysis
Unpaired or paired student's t test was performed with Prism (Graph Pad). *p<0.05, **p<0.01, ***p<0.001.
Supplementary Material
ACKNOWLEDGMENTS
We thank the University of Chicago Flow Cytometry Core for assistance with cell sorting, S. Owens and S. Greenwald in the Next Generation Sequencing Core at Argonne National Laboratory for assistance with amplicon sequencing, and B. Casterline for providing B. fragilis cultures. J.J.B and B.D.M. were supported by an NIH Medical Scientist Training Program grant T32GM007281 and M.M. by FWF Austrian Science Fund grant J3418-B19. This work was supported by NIH grants R01AI038339, R01AI108643, R01GM106173, and R01HL118092 to A.B., NIH grant 1R21AI099825 to A.L.D., NIH grants to R01DK067180 and R01DK098435 to B.J., and support to D.A.A. from the University of Chicago DDRCC, NIDDK P30DK42086.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
AUTHOR CONTRIBUTIONS
J.J.B. designed research, performed experiments, and analyzed data. T.M.F. analyzed 16S rRNA sequencing data. J.C.K. performed bacterial DNA extractions and generated 16S rRNA amplicon libraries. D.G.S. obtained patient samples. M.M., B.D.M., and I.E.I. assisted with experiments shown in Figure 2. A.L.D. contributed reagents. P.C.W. contributed methods, reagents and advice in generating monoclonal antibodies from single plasma cells. B.J., D.A.A., and A.B. designed and supervised research. J.J.B. and A.B. wrote the paper. All authors reviewed and approved the final manuscript.
SUPPLEMENTAL INFORMATION
Supplemental Information includes five figures and Supplemental Experimental Procedures.
REFERENCES
- Alugupalli KR, Leong JM, Woodland RT, Muramatsu M, Honjo T, Gerstein RM. B1b lymphocytes confer T cell-independent long-lasting immunity. Immunity. 2004;21:379–390. doi: 10.1016/j.immuni.2004.06.019. [DOI] [PubMed] [Google Scholar]
- Baumgarth N. The double life of a B-1 cell: self-reactivity selects for protective effector functions. Nature Reviews Immunology. 2011;11:34–46. doi: 10.1038/nri2901. [DOI] [PubMed] [Google Scholar]
- Caporaso JG, Kuczynski J, Stombaugh J, Bittinger K, Bushman FD, Costello EK, Fierer N, Pena AG, Goodrich JK, Gordon JI, et al. QIIME allows analysis of high-throughput community sequencing data. Nat Methods. 2010;7:335–336. doi: 10.1038/nmeth.f.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casola S, Otipoby KL, Alimzhanov M, Humme S, Uyttersprot N, Kutok JL, Carroll MC, Rajewsky K. B cell receptor signal strength determines B cell fate. Nature Immunology. 2004;5:317–327. doi: 10.1038/ni1036. [DOI] [PubMed] [Google Scholar]
- Cullender TC, Chassaing B, Janzon A, Kumar K, Muller CE, Werner JJ, Angenent LT, Bell ME, Hay AG, Peterson DA, et al. Innate and adaptive immunity interact to quench microbiome flagellar motility in the gut. Cell Host & Microbe. 2013;14:571–581. doi: 10.1016/j.chom.2013.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham-Rundles C. Physiology of IgA and IgA deficiency. Journal of Clinical Immunology. 2001;21:303–309. doi: 10.1023/a:1012241117984. [DOI] [PubMed] [Google Scholar]
- Fagarasan S, Muramatsu M, Suzuki K, Nagaoka H, Hiai H, Honjo T. Critical roles of activation-induced cytidine deaminase in the homeostasis of gut flora. Science. 2002;298:1424–1427. doi: 10.1126/science.1077336. [DOI] [PubMed] [Google Scholar]
- Gil-Cruz C, Bobat S, Marshall JL, Kingsley RA, Ross EA, Henderson IR, Leyton DL, Coughlan RE, Khan M, Jensen KT, et al. The porin OmpD from nontyphoidal Salmonella is a key target for a protective B1b cell antibody response. Proceedings of the National Academy of Sciences of the United States of America. 2009;106:9803–9808. doi: 10.1073/pnas.0812431106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haas KM, Poe JC, Steeber DA, Tedder TF. B-1a and B-1b cells exhibit distinct developmental requirements and have unique functional roles in innate and adaptive immunity to S. pneumoniae. Immunity. 2005;23:7–18. doi: 10.1016/j.immuni.2005.04.011. [DOI] [PubMed] [Google Scholar]
- Hollister K, Kusam S, Wu H, Clegg N, Mondal A, Sawant DV, Dent AL. Insights into the role of Bcl6 in follicular Th cells using a new conditional mutant mouse model. Journal of Immunology. 2013;191:3705–3711. doi: 10.4049/jimmunol.1300378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kau AL, Planer JD, Liu J, Rao S, Yatsunenko T, Trehan I, Manary MJ, Liu TC, Stappenbeck TS, Maleta KM, et al. Functional characterization of IgA-targeted bacterial taxa from undernourished Malawian children that produce diet-dependent enteropathy. Science Translational Medicine. 2015;7:276ra224. doi: 10.1126/scitranslmed.aaa4877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawamoto S, Maruya M, Kato LM, Suda W, Atarashi K, Doi Y, Tsutsui Y, Qin H, Honda K, Okada T, et al. Foxp3(+) T cells regulate immunoglobulin a selection and facilitate diversification of bacterial species responsible for immune homeostasis. Immunity. 2014;41:152–165. doi: 10.1016/j.immuni.2014.05.016. [DOI] [PubMed] [Google Scholar]
- Kroese FG, Butcher EC, Stall AM, Lalor PA, Adams S, Herzenberg LA. Many of the IgA producing plasma cells in murine gut are derived from self-replenishing precursors in the peritoneal cavity. International Immunology. 1989;1:75–84. doi: 10.1093/intimm/1.1.75. [DOI] [PubMed] [Google Scholar]
- Kroese FG, de Waard R, Bos NA. B-1 cells and their reactivity with the murine intestinal microflora. Seminars in Immunology. 1996;8:11–18. doi: 10.1006/smim.1996.0003. [DOI] [PubMed] [Google Scholar]
- Kubinak JL, Petersen C, Stephens WZ, Soto R, Bake E, O'Connell RM, Round JL. MyD88 Signaling in T Cells Directs IgA-Mediated Control of the Microbiota to Promote Health. Cell Host & Microbe. 2015;17:153–163. doi: 10.1016/j.chom.2014.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lecuyer E, Rakotobe S, Lengline-Garnier H, Lebreton C, Picard M, Juste C, Fritzen R, Eberl G, McCoy KD, Macpherson AJ, et al. Segmented filamentous bacterium uses secondary and tertiary lymphoid tissues to induce gut IgA and specific T helper 17 cell responses. Immunity. 2014;40:608–620. doi: 10.1016/j.immuni.2014.03.009. [DOI] [PubMed] [Google Scholar]
- Macpherson AJ, Gatto D, Sainsbury E, Harriman GR, Hengartner H, Zinkernagel RM. A primitive T cell-independent mechanism of intestinal mucosal IgA responses to commensal bacteria. Science. 2000;288:2222–2226. doi: 10.1126/science.288.5474.2222. [DOI] [PubMed] [Google Scholar]
- Mathew R, Mao AP, Chiang AH, Bertozzi-Villa C, Bunker JJ, Scanlon ST, McDonald BD, Constantinides MG, Hollister K, Singer JD, et al. A negative feedback loop mediated by the Bcl6-cullin 3 complex limits Tfh cell differentiation. The Journal of Experimental Medicine. 2014;211:1137–1151. doi: 10.1084/jem.20132267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathias A, Corthesy B. Recognition of gram-positive intestinal bacteria by hybridoma- and colostrum-derived secretory immunoglobulin A is mediated by carbohydrates. The Journal of Biological Chemistry. 2011;286:17239–17247. doi: 10.1074/jbc.M110.209015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mestecky J. Mucosal Immunology. 3rd edn Elsevier Academic Press; Amsterdam ; Boston: 2005. [Google Scholar]
- Meyer F, Paarmann D, D'Souza M, Olson R, Glass EM, Kubal M, Paczian T, Rodriguez A, Stevens R, Wilke A, et al. The metagenomics RAST server - a public resource for the automatic phylogenetic and functional analysis of metagenomes. BMC Bioinformatics. 2008;9:386. doi: 10.1186/1471-2105-9-386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moon C, Baldridge MT, Wallace MA, Burnham CA, Virgin HW, Stappenbeck TS. Vertically transmitted faecal IgA levels determine extra-chromosomal phenotypic variation. Nature. 2015;521:90–93. doi: 10.1038/nature14139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pabst O. New concepts in the generation and functions of IgA. Nature Reviews. Immunology. 2012;12:821–832. doi: 10.1038/nri3322. [DOI] [PubMed] [Google Scholar]
- Palm NW, de Zoete MR, Cullen TW, Barry NA, Stefanowski J, Hao L, Degnan PH, Hu J, Peter I, Zhang W, et al. Immunoglobulin A coating identifies colitogenic bacteria in inflammatory bowel disease. Cell. 2014;158:1000–1010. doi: 10.1016/j.cell.2014.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson DA, McNulty NP, Guruge JL, Gordon JI. IgA response to symbiotic bacteria as a mediator of gut homeostasis. Cell Host & Microbe. 2007;2:328–339. doi: 10.1016/j.chom.2007.09.013. [DOI] [PubMed] [Google Scholar]
- Robertson BR, O'Rourke JL, Neilan BA, Vandamme P, On SL, Fox JG, Lee A. Mucispirillum schaedleri gen. nov., sp. nov., a spiral-shaped bacterium colonizing the mucus layer of the gastrointestinal tract of laboratory rodents. International Journal of Systematic and Evolutionary Microbiology. 2005;55:1199–1204. doi: 10.1099/ijs.0.63472-0. [DOI] [PubMed] [Google Scholar]
- Roy B, Brennecke AM, Agarwal S, Krey M, Duber S, Weiss S. An intrinsic propensity of murine peritoneal B1b cells to switch to IgA in presence of TGF-beta and retinoic acid. PloS ONE. 2013;8:e82121. doi: 10.1371/journal.pone.0082121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slack E, Balmer ML, Fritz JH, Hapfelmeier S. Functional flexibility of intestinal IgA - broadening the fine line. Frontiers in Immunology. 2012;3:100. doi: 10.3389/fimmu.2012.00100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephens WZ, Round JL. IgA targets the troublemakers. Cell Host & Microbe. 2014;16:265–267. doi: 10.1016/j.chom.2014.08.012. [DOI] [PubMed] [Google Scholar]
- Tezuka H, Abe Y, Asano J, Sato T, Liu J, Iwata M, Ohteki T. Prominent role for plasmacytoid dendritic cells in mucosal T cell-independent IgA induction. Immunity. 2011;34:247–257. doi: 10.1016/j.immuni.2011.02.002. [DOI] [PubMed] [Google Scholar]
- Thurnheer MC, Zuercher AW, Cebra JJ, Bos NA. B1 cells contribute to serum IgM, but not to intestinal IgA, production in gnotobiotic Ig allotype chimeric mice. Journal of Immunology. 2003;170:4564–4571. doi: 10.4049/jimmunol.170.9.4564. [DOI] [PubMed] [Google Scholar]
- Tsuji M, Suzuki K, Kitamura H, Maruya M, Kinoshita K, Ivanov II, Itoh K, Littman DR, Fagarasan S. Requirement for lymphoid tissue-inducer cells in isolated follicle formation and T cell-independent immunoglobulin A generation in the gut. Immunity. 2008;29:261–271. doi: 10.1016/j.immuni.2008.05.014. [DOI] [PubMed] [Google Scholar]
- Tsuruta T, Inoue R, Iwanaga T, Hara H, Yajima T. Development of a method for the identification of S-IgA-coated bacterial composition in mouse and human feces. Bioscience, Biotechnology, and Biochemistry. 2010;74:968–973. doi: 10.1271/bbb.90801. [DOI] [PubMed] [Google Scholar]
- Tsuruta T, Inoue R, Nojima I, Tsukahara T, Hara H, Yajima T. The amount of secreted IgA may not determine the secretory IgA coating ratio of gastrointestinal bacteria. FEMS Immunology and Medical Microbiology. 2009;56:185–189. doi: 10.1111/j.1574-695X.2009.00568.x. [DOI] [PubMed] [Google Scholar]
- van der Waaij LA, Limburg PC, Mesander G, van der Waaij D. In vivo IgA coating of anaerobic bacteria in human faeces. Gut. 1996;38:348–354. doi: 10.1136/gut.38.3.348. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.