Abstract
Objectives: We reviewed our series of patients who underwent open abdominal aortic aneurysm (AAA) repair and constructed a prediction model for postoperative delirium.
Methods: 397 patients who underwent open AAA repair at our institution between April 2005 and June 2013 were retrospectively reviewed. Postoperative delirium was diagnosed from the patients’ medical records according to the Diagnostic and Statistical Manual of Mental Disorders 4th Edition (DSM-IV) criteria. Mental alterations resulting from postoperative cerebrovascular events or preexisting mental disorders were excluded. Parameters with significant differences on univariate analysis were subjected to a logistic regression analysis.
Results: There were 46 patients (11.5%) diagnosed with postoperative delirium. The following parameters were significant in the univariate analysis: age, history of stroke, hyperlipidemia, forced expiratory volume in 1 s (FEV1), percent vital capacity (%VC), and blood urea nitrogen (BUN) level. A logistic regression analysis revealed that an age ≥70 years (odds ratio [95% confidence interval], 3.342 [1.437–7.774]), blood loss ≥1517 mL (2.707 [1.359–5.391]), and the absence of hyperlipidemia (2.154 [1.060–4.374]) were significant risk factors.
Conclusions: Older patients with substantial intraoperative blood loss require highly vigilant postoperative care. Further studies are necessary to elucidate the relationship between cholesterol and delirium.
Keywords: delirium, abdominal aortic aneurysm, open repair
Introduction
Delirium is one of the most common complications after major surgery. It is defined in the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders 4th Edition (DSM-IV) as a disturbance of consciousness and cognition that develops over a short period of time (often within hours or days) and fluctuates over time.1)
Due to its sudden onset, postoperative delirium requires unscheduled medical resources such as extra nursing workloads, psychiatric consultations, measures for patients’ safety, and longer hospital stays. Moreover, it can also result in higher complication rates. Therefore, predicting and preventing postoperative delirium could improve morbidity and reduce the use of medical resources.2,3)
The overall incidence of postoperative delirium following a variety of surgical procedures has been reported to range from 0 to 73.5%.4) Among the various types of surgery, open abdominal aortic aneurysm (AAA) repair is recognized as a particularly high-risk procedure. Marcantonio et al. reported that abdominal aortic surgery was an independent strong predictor of delirium among 1341 patients who underwent major non-cardiac surgery (odds ratio (OR) 8.3).5,6) That study was one of the largest studies to identify predictive factors for postoperative delirium. However, their patient population was heterogeneous and had undergone a variety of non-cardiac surgeries. In their study, orthopedic surgery predominated (43%), and only 55 patients (4%) had undergone aortic aneurysm repair. This limited number of patients suggested that the prediction model generated in the study might be of limited use for AAA patients.
Studies with patient populations limited to vascular cases are rare; we found only two prospective studies that exclusively enrolled vascular surgery patients, who are expected to be older and may have more cardiovascular risk factors than general surgery or orthopedic surgery patients. Sasajima et al. reported that the incidence of postoperative delirium was 29% among 110 patients with chronic lower limb ischemia.7) Additionally, Böhner et al. reported that the incidence of postoperative delirium was 39% among 153 patients undergoing various types of vascular surgery.8) Although these studies were well designed, they included vascular diseases other than AAA.
We retrospectively reviewed our own series of open AAA repair patients and constructed a risk prediction model for postoperative delirium based on pre- and intraoperative factors. To our knowledge, this is the largest study cohort to date that is limited to open AAA repair.
Materials and Methods
Study population
Between April 2005 and June 2013, 769 patients underwent open AAA repair at the Department of Vascular Surgery, Nagoya University Hospital. Elective open repair was performed in 408 patients. Cases of thoracoabdominal aortic aneurysm or simultaneous endovascular repair for thoracic aortic aneurysm were excluded. The remaining 397 patients were enrolled in this study.
All of the patients gave their informed consent, and the Institutional Review Board of the Nagoya University Graduate School of Medicine approved this study.
Surgical procedures
Open AAA repair was performed under general anesthesia. In most cases, epidural anesthesia was also used. A transperitoneal approach using a midline incision was applied in all cases. After systemic heparinization, clamps were placed distally over the iliac arteries. Proximal clamps were placed either inferior or superior to the renal arteries depending on the anatomy of the aneurismal neck. Straight or bifurcated knitted Dacron grafts were selected and anastomosed for in situ repair. The abdomen was closed following retroperitoneal repair. The Cell Saver System (Haemonetics Corporation, Braintree, MA, USA) was used intraoperatively in all cases. The need for intraoperative blood transfusion was determined by the attending anesthesiologist.
Patients spent their first postoperative days in the intensive care unit (ICU) or on our general ward depending on the availability of ICU beds and their need for intensive care. Patients without any need for intensive care went to the general ward on the 2nd postoperative day and were started on oral intake. Physical therapy for early ambulation was initiated in the general ward. In successful courses, a postoperative computed tomography (CT) was performed on the 6th postoperative day. The patients were discharged from the hospital on the 7th postoperative day.
Data collection
The patients’ medical records and nursing charts were retrospectively reviewed to collect the preoperative and intraoperative parameters as potential predictors of postoperative delirium. Their postoperative courses were also evaluated. If the patient had postoperative mental alterations, the case was retrospectively assessed to determine whether it was due to delirium according to DSM-IV criteria.1) Other syndromes such as anxiety, depression, and dementia were ruled out. In most cases, psychiatrists (and neurologists when necessary) had been consulted for definitive diagnosis during the patients’ hospitalization. Brain imaging studies such as CT and magnetic resonance imaging were used to exclude stroke in suspected cases.
Delirium diagnosed on the day of surgery (postoperative day zero) or after the sixth postoperative day was excluded because the condition could have been due to etiologies other than surgical intervention.9) This study aimed to estimate the impact of pre- and postoperative factors. Therefore, delirium in patients who were dependent on ventilator support for more than 24 h after their surgery were also excluded to eliminate the effects of prolonged intubation and the accompanying sedatives that are usually administered postoperatively.
Data analysis
Continuous data with normal distributions were expressed as the means ± standard deviation (SD). Medians and interquartile ranges (IQRs) were used for other continuous data. The distribution of the data was assessed using the Shapiro-Wilk test.
Student’s t-test or the Mann-Whitney U-test was used for univariate analysis of continuous parameters. The chi-squared test or Fisher’s exact test was used for univariate analysis of categorical parameters.
A P <.05 was considered significant for all analyses. All of the statistical analyses were performed using IBM Statistics Statistical Package for Social Science (SPSS) version 21 (IBM Corporation, Arkmont, NY, USA).
The pre- and intraoperative variables collected through retrospective medical chart review were subjected to univariate analysis. Only the variables that showed significant differences on univariate analysis were included in the subsequent multivariate analysis. For the multivariate analysis, the independent association of each risk factor with postoperative delirium was determined using a stepwise logistic regression. In the logistic regression, certain continuous parameters were dichotomized at cut-off points; for age, greater than 70 years; and for blood loss, above 1517 mL. Age greater than 70 was chosen to provide data comparable with other studies. The median value was used as the blood loss cut-off.
The number of blood transfusions and lowest postoperative hematocrit were highly collinear with intraoperative blood loss. Therefore, these variables were not included in the analysis.5)
Results
Of the 397 patients, 338 (85.1%) were male. The median age was 72 years old (range, 50–86; IQR, 66–76). The median postoperative hospital stay was 12 days (range, 7–168; IQR, 10–16).
Incidence of delirium
In this study cohort, 48 patients had postoperative mental status alterations. One patient had been intubated and received sedatives in the ICU until the 5th postoperative day. Another patient was diagnosed by psychiatrists as suffering from senile dementia. These cases were excluded from the delirium group. Intoxication due to intravenous lidocaine might have caused delirium in another patient, and the patient recovered immediately after discontinuation of the lidocaine. This patient was included in the delirium group in accordance with DSM-IV criteria. Consequently, 46 patients (11.5%) were included in the postoperative delirium group. The median time of onset of delirium was the second postoperative day (IQR, 2–3). In our series, the length of the postoperative hospital stay was not significantly different between delirious and non-delirious patients (median [IQR], 13.5 [11–16] vs. 12.0 [10–16]; P = .112).
Preoperative data
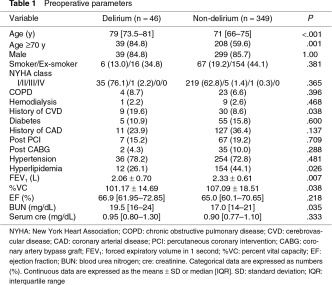
Preoperative variables for the delirious (n = 46) and non-delirious (n = 349) groups and the results of the univariate analysis are shown in Table 1.
The delirium group was significantly older (P <.001) and had a more frequent history of cerebrovascular disease, including stroke and transient ischemic attack (P = .038). Conversely, hyperlipidemia was more common in the non-delirium group (P = .026). Delirious patients had decreased pulmonary function with reduced vital capacities and forced expiratory volumes in one second (P = .038 and .007, respectively). The blood urea nitrogen (BUN) level was higher in delirious patients (P = .035). However, there was no significant contribution to postoperative delirium by hemodialysis.
Intraoperative data
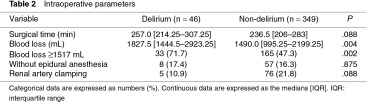
The intraoperative variables for both groups and the results of the univariate analysis are shown in Table 2. The duration of the surgical procedure was not significantly different between the groups. However, a significantly larger amount of blood was lost intraoperatively in the delirium group (P = .004). No significant correlation between delirium and epidural anesthesia was observed in the univariate analysis.
Prediction model for postoperative delirium
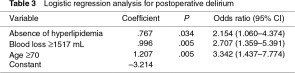
The significant variables between the delirium and non-delirium groups identified by the univariate analysis were subjected to a stepwise logistic regression analysis in which the presence of postoperative delirium was the dependent variable. The prediction model constructed is shown in Table 3. Age ≥70 years old, the absence of hyperlipidemia, and blood loss ≥1517 mL were identified as significant risk factors.
The result of the chi-squared test for this model was significant (P <.001). The Hosmer-Lemeshow test revealed an excellent fit for this model (P = .995), which yielded a satisfactory predictive value of 88.1%.
Discussion
In our prediction model, age ≥70 years old was a significant predictor of postoperative delirium with an odds ratio (OR) of 3.342 (95% confidence interval (CI); 1.437–7.774) (Table 3). Advanced age has been generally reported to be a risk factor for delirium in previous studies.2–8) Age ≥70 years old, the cut-off point used in this study, was reported as an independent risk factor both in Marcantonio’s study involving various non-cardiac surgeries (OR [95% CI], 2.8 [1.6–4.4]) and in Sasajima’s series involving bypass surgery for chronic ischemia (14.1 [2.7–72.0]).5–7)
Following the introduction of endovascular aneurysm repair (EVAR) in Japan in 2007, patients over 75 years of age became candidates for treatment with EVAR instead of open surgery at our institution. However, in the present study population, neither patient age nor the rate of postoperative delirium was significantly different after 2007 (P = .095 and .458, respectively). This result occurred because we were conservative in introducing EVAR. We expect an in-progress study to demonstrate that delirium has become less common in vascular wards since the introduction of EVAR. To date in our EVAR series, postoperative mental alterations have only been observed in 1.6% of 430 older patients (median age [IQR]; 78 [74–82]).
Intraoperative blood loss ≥1517 mL was also identified as a risk factor in the logistic regression analysis. Intraoperative anemia (low hemoglobin and hematocrit) were reported as independent risk factors in the study by Marcantonio et al.5) In other studies analyzing intraoperative factors for various types of surgery, electrolyte disturbances and colloid infusion requirements have also been found to be predictors of delirium. These parameters are likely surrogate indicators of surgical stress. In the present study, intraoperative blood loss was adopted as a representative stress indicator, and no other intraoperative parameters were included in the analysis due to the difficulty of collecting the data retrospectively.
Another significant risk factor in our prediction model was the absence of hyperlipidemia, which had an OR of 2.154. This was a very interesting and unexpected finding that, to the best of our knowledge, has only appeared in one other study. Böhner et al. also identified the absence of hyperlipidemia as a significant parameter in their prediction for postoperative delirium with an OR of 5.51.8)
It is somewhat difficult to explain the mechanism underlying the association between hyperlipidemia and postoperative delirium. One speculation is that this finding might have resulted from the pleiotropic effects of statins, which are cholesterol-lowering agents. In a prospective study including 1059 patients after cardiac surgery, the administration of statins had a protective effect and reduced the odds of delirium by 46%.10) However, in our series, the univariate analysis of preoperative statin use showed no significant difference between delirious and non-delirious patients (P = .074; data not shown). Another study also showed no association between the use of statins and delirium.11) Thus, further studies are necessary to elucidate the relationship between cholesterol levels and delirium.
In our series, 11.5% of patients who underwent elective open AAA repair were diagnosed with postoperative delirium. This result was comparable to the 9% incidence in the study by Marcantonio et al. However, non-vascular patients predominated in their series.5,6) In previous studies limited to vascular patients, postoperative delirium has been more common. Sasajima et al. reported that the incidence of postoperative delirium was 29% among 110 patients with chronic lower limb ischemia.7) Böhner et al. reported that the incidence of postoperative delirium was 39% among 153 patients undergoing various types of vascular surgery.8) Compared with these studies, our incidence was remarkably low. There are several possible reasons for this variance apart from differences in patients’ backgrounds. First, the diagnostic methods used in each of the studies might have varied. The studies of Marcantonio and Sasajima adopted the Confusion Assessment Method (CAM), which was established to enable non-psychiatric clinicians to detect delirium with an excellent sensitivity and specificity based on DSM-III-R.12) In Böhner’s study, the delirium had to be diagnosed by psychiatrists, and the Delirium Rating Scale (DRS) score13) was used in addition to DSM-IV criteria.
Second, the study design varied between the studies. The present study was a retrospective study, while the others were prospective studies. Active behavior such as agitation, compulsive nurse-calling, spontaneous removal of lines, and nocturnal wandering are typical in delirious patients and often exasperate clinical staff. In addition to this hyperactive state, delirium can also include a hypoactive (quiet) state. In the present study, it is possible that only the patients with obvious symptoms drawing the attention of the medical staff were recognized, and cases of hypoactive delirium might have been overlooked. In such cases, the description of the patients’ mental status in the medical records may be poor, resulting in underestimation of the number of delirium patients due to the retrospective nature of the present study.14,15) To avoid this result in the future a prospective protocol to evaluate patients at least once a day should be designed.
The present study had some other limitations. For example, preoperative cognitive function was not routinely assessed. The preoperative effects of alcohol, psychotropic agents, mental illnesses, and anesthetic drugs were not evaluated. The patients’ preoperative physical function, which has previously been reported as a predictor of delirium,5) was excluded from the analyses. These parameters were eliminated because of incomplete and inconsistent data sets. In one patient, the postoperative intoxication of lidocaine, rather than surgical interventions, was possibly a major cause of his delirium. However, we consciously included him in the study population to avoid a bias of arbitrary patient selections.
In conclusion, advanced age was a risk factor for delirium after open AAA repair, which was consistent with results for other types of surgery. Our results suggested that older patients with substantial intraoperative blood loss require highly vigilant postoperative care. Further studies are necessary to elucidate the relationship between cholesterol levels and delirium.
Disclosure Statements
None to declare.
Funding
No financial support from outside.
References
- American PsychiatricAssociation Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, text revision. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Inouye SK, Bogardus ST, Charpentier PA, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med 1999; 340: 669-76. [DOI] [PubMed] [Google Scholar]
- Koster S, Oosterveld FG, Hensens AG, et al. Delirium after cardiac surgery and predictive validity of a risk checklist. Ann Thorac Surg 2008; 86: 1883-7. [DOI] [PubMed] [Google Scholar]
- Dyer CB, Ashton CM, Teasdale TA. Postoperative delirium. A review of 80 primary data-collection studies. Arch Intern Med 1995; 155: 461-5. [DOI] [PubMed] [Google Scholar]
- Marcantonio ER, Goldman L, Orav EJ, et al. The association of intraoperative factors with the development of postoperative delirium. Am J Med 1998; 105: 380-4. [DOI] [PubMed] [Google Scholar]
- Marcantonio ER, Goldman L, Mangione CM, et al. A clinical prediction rule for delirium after elective noncardiac surgery. JAMA 1994; 271: 134-9. [PubMed] [Google Scholar]
- Sasajima Y, Sasajima T, Uchida H, et al. Postoperative delirium in patients with chronic lower limb ischaemia: what are the specific markers. Eur J Vasc Endovasc Surg 2000; 20: 132-7. [DOI] [PubMed] [Google Scholar]
- Böhner H, Hummel TC, Habel U, et al. Predicting delirium after vascular surgery: a model based on pre- and intraoperative data. Ann Surg 2003; 238: 149-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazmierski J, Kowman M, Banach M, et al. Incidence and predictors of delirium after cardiac surgery: Results from The IPDACS Study. J Psychosom Res 2010; 69: 179-85. [DOI] [PubMed] [Google Scholar]
- Katznelson R, Djaiani GN, Borger MA, et al. Preoperative use of statins is associated with reduced early delirium rates after cardiac surgery. Anesthesiology 2009; 110: 67-73. [DOI] [PubMed] [Google Scholar]
- Mariscalco G, Cottini M, Zanobini M, et al. Preoperative statin therapy is not associated with a decrease in the incidence of delirium after cardiac operations. Ann Thorac Surg 2012; 93: 1439-47. [DOI] [PubMed] [Google Scholar]
- Inouye SK, van Dyck CH, Alessi CA, et al. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med 1990; 113: 941-8. [DOI] [PubMed] [Google Scholar]
- Trzepacz PT, Baker RW, Greenhouse J. A symptom rating scale for delirium. Psychiatry Res 1988; 23: 89-97. [DOI] [PubMed] [Google Scholar]
- Gustafson Y, Brännström B, Norberg A, et al. Underdiagnosis and poor documentation of acute confusional states in elderly hip fracture patients. J Am Geriatr Soc 1991; 39: 760-5. [DOI] [PubMed] [Google Scholar]
- Johnson JC, Kerse NM, Gottlieb G, et al. Prospective versus retrospective methods of identifying patients with delirium. J Am Geriatr Soc 1992; 40: 316-9. [DOI] [PubMed] [Google Scholar]