The authors observed a high unplanned readmission rate among their population of patients with cancer.
Abstract
Purpose:
Hospital readmissions are considered by the Centers for Medicare and Medicaid as a metric for quality of health care delivery. Robust data on the readmission profile of patients with cancer are currently insufficient to determine whether this measure is applicable to cancer hospitals as well. To address this knowledge gap, we estimated the unplanned readmission rate and identified factors influencing unplanned readmissions in a hospitalist service at a comprehensive cancer center.
Methods:
We retrospectively analyzed unplanned 30-day readmission of patients discharged from the General Internal Medicine Hospitalist Service at a comprehensive cancer center between April 1, 2012, and September 30, 2012. Multiple independent variables were studied using univariable and multivariable logistic regression models, with generalized estimating equations to identify risk factors associated with readmissions.
Results:
We observed a readmission rate of 22.6% in our cohort. The median time to unplanned readmission was 10 days. Unplanned readmission was more likely in patients with metastatic cancer and those with three or more comorbidities. Patients discharged to hospice were less likely to be readmitted (all P values < .01).
Conclusion:
We observed a high unplanned readmission rate among our population of patients with cancer. The risk factors identified appear to be related to severity of illness and open up opportunities for improving coordination with primary care physicians, oncologists, and other specialists to manage comorbidities, or perhaps transition appropriate patients to palliative care. Our findings will be instrumental for developing targeted interventions to help reduce readmissions at our hospital. Our data also provide direction for appropriate application of readmission quality measures in cancer hospitals.
Introduction
In the past few years, hospital readmission has been brought to the forefront as a measure of quality of care. Unplanned readmissions are viewed by some as an indicator of poor hospital care, a reflection of breakdown in the care transition process, or even a missed opportunity to better coordinate care.1 Many still question the validity of readmission as a quality metric and argue that this concept may be misguided, that readmissions may in fact be a “rescue” and appropriate care for patients suffering complications: a necessary evil.2 Though their validity may be debatable, what is certain is that readmissions are common and have known cost implications. In 2009, it was found that 20% of 12 million Medicare beneficiaries were readmitted within 30 days of a hospital discharge.3 This translated into an estimated cost of approximately $17 billion for unplanned readmissions in 2004 alone. To address this issue, the Hospital Readmissions Reduction Program (HRRP) was implemented by Congress in 2010 as part of the Patient Protection and Affordable Care Act.4 HRRP calls for reduced payment reimbursements to hospitals with high readmission rates. The impact of HRRP is unclear, but more than half of hospitals in the United States are currently estimated to be at risk of incurring penalties.5
Prospective Payment System–exempt cancer hospitals such as The University of Texas MD Anderson Cancer Center are currently excluded from HRRP because cancer hospitals care for a unique patient population whose readmission profiles may not be comparable to those of other hospitals. In a study by Singh et al,6 it was shown that a large part of the variation in readmission risk among hospitals is, in fact, attributable to patient characteristics. This suggests that readmission risk indices should be adjusted according to a hospital's case mix. The authors also suggested that accountability may not solely be the responsibility of the discharging hospital. Evidently, more data are needed to determine whether readmission measures are applicable to cancer hospitals, which often care for patients who have more advanced or more complex diseases. At present, there is no standardized definition of an avoidable readmission in the context of the cancer population. Readmission patterns among patients with cancer and in cancer hospitals are poorly understood. This should be studied further and described in order to elucidate the reasons for readmissions and identify risk factors for readmission. Moreover, quality data need to be benchmarked in this population in anticipation of future requirements by the Centers for Medicare and Medicaid Services (CMS).7
To this end, we sought to estimate the unplanned readmission rate among patients discharged from the General Internal Medicine Hospitalist Service at The University of Texas MD Anderson Cancer Center, and identify risk factors for unplanned readmission in this patient population. These baseline data will also improve understanding of our population of patients with cancer, and can inform future plans to reduce readmissions on our hospitalist service. This project was approved by the quality improvement assessment board at MD Anderson.
Methods
Using a retrospective cohort study design, we identified all patients who were discharged from the General Internal Medicine Hospitalist Service between April 1, 2012, and September 30, 2012. The hospitalist service at MD Anderson admits adult patients with solid tumors who are actively receiving cancer treatment and in need of acute inpatient care, cancer survivors who have no evidence of disease, patients with a suspected or unconfirmed diagnosis of cancer, patients who had cancer-directed surgery more than 30 days previously, and patients who do not have cancer but have medical issues or who have an existing relationship with MD Anderson. Patients whose treatment plans consist of radiotherapy alone could potentially be admitted to the hospitalist service as well. For purposes of this study, we excluded patients with nonmalignant and in situ disease only and those who died during the first hospitalization.
We used the University HealthSystem Consortium (UHC) Clinical Data Base/Resource Manager to obtain patient-level data relating to each patient's hospital encounter. UHC is a national alliance of 120 academic medical centers, including MD Anderson.8 The UHC clinical database is a source of clinical, administrative, financial, and operations data submitted regularly by all member institutions to an electronic repository. The data are available in de-identified and aggregate form for comparative analyses between member institutions. De-identified patient-level data may be obtained; however, many specific variables are available only to the home institution for patient-level case analysis. For this study, we used patient-level data from UHC for our hospital and augmented this with tumor information (ie, cancer type and stage) from our institutional database. Approval for data use and publication of results for this project was obtained from UHC.
The outcome of interest was 30-day unplanned readmission. We defined this as a nonelective admission that occurred within 30 days of a hospitalist discharge. We excluded readmissions that were mainly for chemotherapy, radiotherapy, and rehabilitation services because these admissions are almost always planned.9–11 Patients who died during the index hospitalization were excluded from the analysis.12 The unit of analysis was a discharge encounter. A readmission could also serve as an index hospitalization for a subsequent discharge encounter. To determine the unplanned readmission rate, we divided the total number of unplanned readmissions after a hospitalist discharge by the total number of discharge encounters from the hospitalist service within the specified time frame. We collected information about the following independent variables to determine their association with unplanned readmission: age, sex, race, residency (ie, inside or outside of the United States), type of insurance, type of cancer, stage of disease, comorbidities, discharge disposition, discharge day of the week, length of stay, and number of days spent in the intensive care unit during the index hospitalization. To identify patient comorbidities, we searched the database for hospital encounters within 1 year before the first date of our observation period for codes pertaining to comorbidities, as defined by the Agency for Healthcare Research and Quality. Twenty-six noncancer Elixhauser comorbidities were identified from the database for each patient, and the number of unique comorbidities identified for each patient was summed and recorded.13
Descriptive statistics were used to summarize continuous and categorical variables. Univariable and multivariable logistic regression models using generalized estimating equations were used to fit the unplanned readmission data to take into account intrapatient correlation and determine the effect of each of the covariates. In the model building process, a regression model was obtained by first including an initial set of candidate predictor variables with a P value of ≤ .10 in the univariable analysis. A stepwise backward elimination was then performed using P < .05 as the significance cutoff level of the Wald χ2 for an effect to stay in the model. All tests were two-sided. P values < .05 were considered statistically significant. All analyses were conducted using SAS software (version 9.2; SAS Institute, Cary, NC).
Results
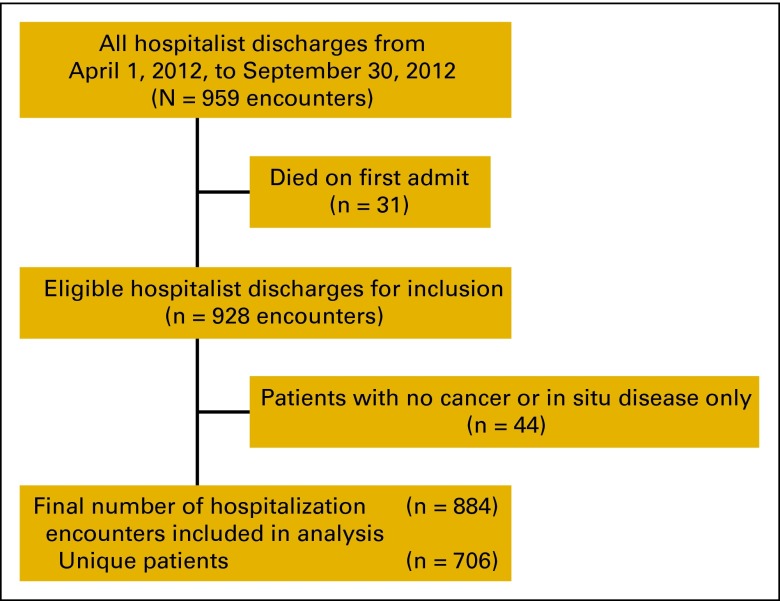
We identified a total of 959 discharge encounters in the General Internal Medicine Hospitalist Service at MD Anderson between April 1, 2012, and September 30, 2012. We excluded 31 encounters from patients who died during the index hospitalization. Forty-four patients who had no cancer or who had in situ disease only were also excluded, for a final cohort of 706 unique patients with 884 discharge encounters (Figure A1).
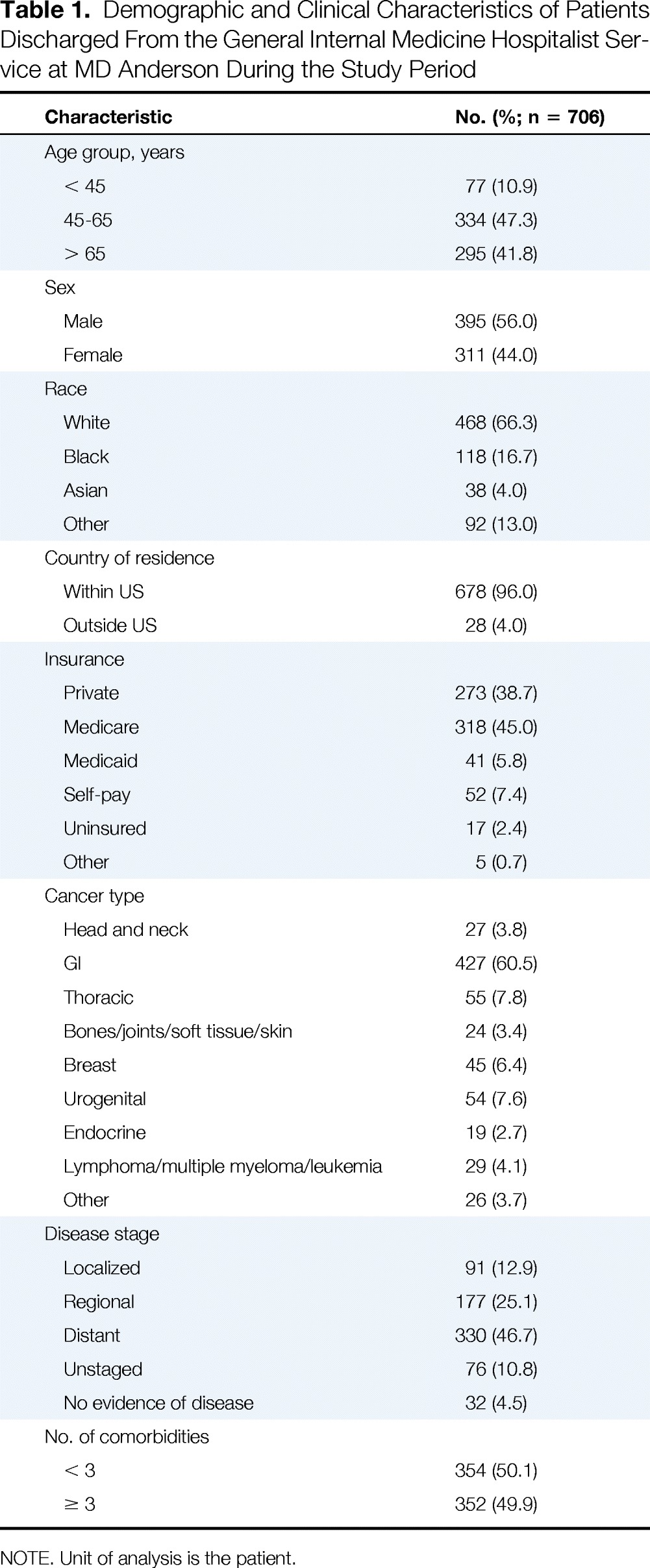
Table 1 shows the demographic and clinical characteristics of our final cohort. Briefly, 66.3% of patients were white, 41.8% were age 65 years or older, 47.3% were between the ages of 45 and 65 years, 60.5% had GI cancer, 46.7% had distant or metastatic disease, and 49.9% had three or more comorbidities.
Table 1.
Demographic and Clinical Characteristics of Patients Discharged From the General Internal Medicine Hospitalist Service at MD Anderson During the Study Period
| Characteristic | No. (%; n = 706) |
|---|---|
| Age group, years | |
| < 45 | 77 (10.9) |
| 45-65 | 334 (47.3) |
| > 65 | 295 (41.8) |
| Sex | |
| Male | 395 (56.0) |
| Female | 311 (44.0) |
| Race | |
| White | 468 (66.3) |
| Black | 118 (16.7) |
| Asian | 38 (4.0) |
| Other | 92 (13.0) |
| Country of residence | |
| Within US | 678 (96.0) |
| Outside US | 28 (4.0) |
| Insurance | |
| Private | 273 (38.7) |
| Medicare | 318 (45.0) |
| Medicaid | 41 (5.8) |
| Self-pay | 52 (7.4) |
| Uninsured | 17 (2.4) |
| Other | 5 (0.7) |
| Cancer type | |
| Head and neck | 27 (3.8) |
| GI | 427 (60.5) |
| Thoracic | 55 (7.8) |
| Bones/joints/soft tissue/skin | 24 (3.4) |
| Breast | 45 (6.4) |
| Urogenital | 54 (7.6) |
| Endocrine | 19 (2.7) |
| Lymphoma/multiple myeloma/leukemia | 29 (4.1) |
| Other | 26 (3.7) |
| Disease stage | |
| Localized | 91 (12.9) |
| Regional | 177 (25.1) |
| Distant | 330 (46.7) |
| Unstaged | 76 (10.8) |
| No evidence of disease | 32 (4.5) |
| No. of comorbidities | |
| < 3 | 354 (50.1) |
| ≥ 3 | 352 (49.9) |
NOTE. Unit of analysis is the patient.
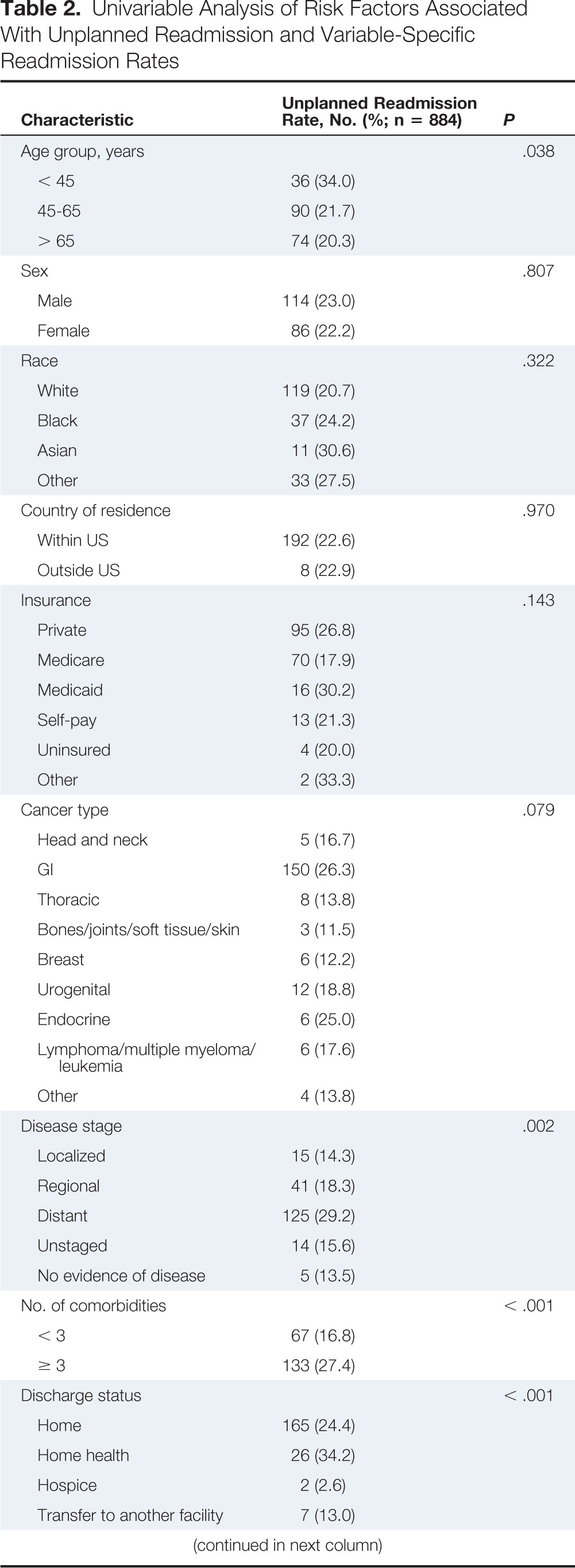
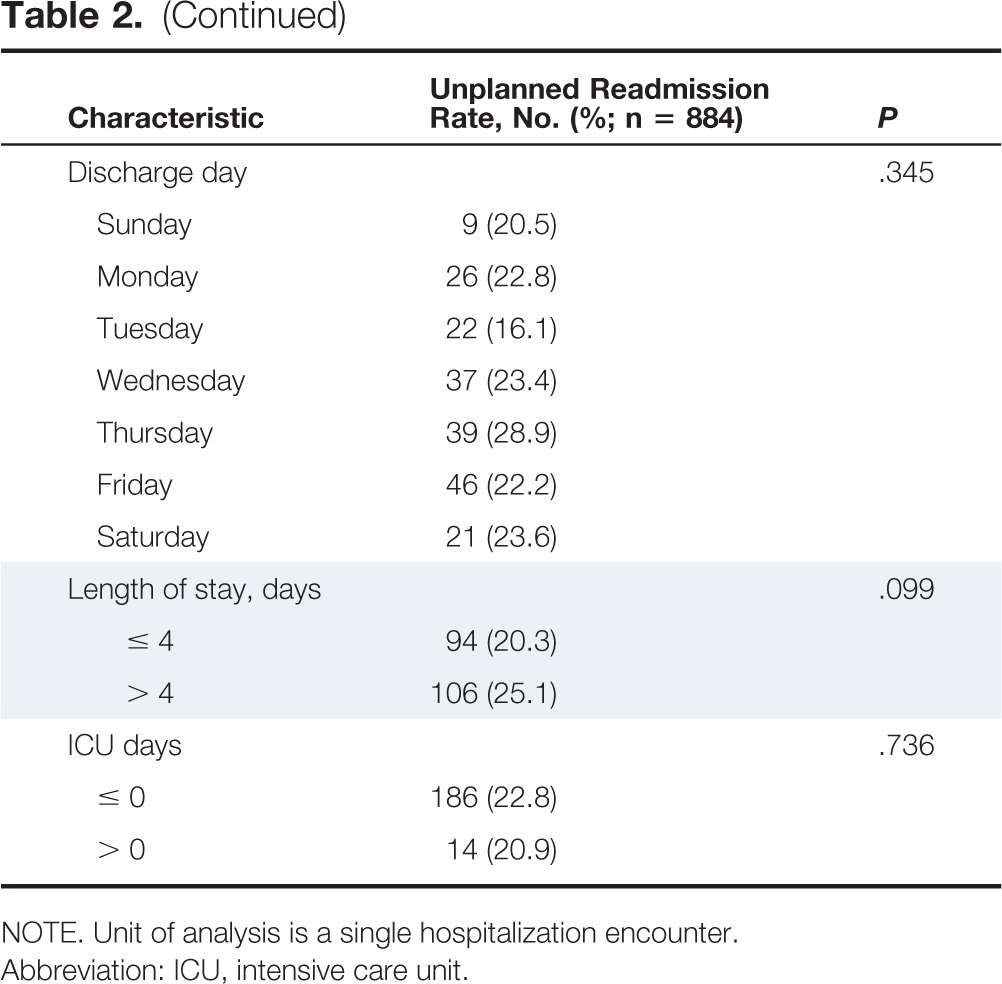
We identified 200 unplanned readmission encounters out of 884 hospitalist discharges, for an estimated unplanned readmission rate of 22.6% on our General Internal Medicine Hospitalist Service. Table 2 shows unplanned readmission rates for each of the subgroups defined in Table 1. The median time to unplanned readmission was 10 days for the entire cohort. Excluding diagnoses for the primary cancer, the most common principal diagnoses recorded for unplanned readmissions were for metastatic disease (eg, malignant ascites, peritoneal carcinomatosis, malignant pleural effusion; n = 23; 12.7%); intestinal obstruction without hernia and pneumonia (n = 10; 5.5%); GI hemorrhage (n = 9; 5.0%); septicemia, biliary tract disease, acute renal failure, complications of device, and urinary tract infection (n = 8 for each; 4.4%); and complications of surgical procedure or medical care (n = 6; 3.3%).
Table 2.
Univariable Analysis of Risk Factors Associated With Unplanned Readmission and Variable-Specific Readmission Rates
| Characteristic | Unplanned Readmission Rate, No. (%; n = 884) | P |
|---|---|---|
| Age group, years | .038 | |
| < 45 | 36 (34.0) | |
| 45-65 | 90 (21.7) | |
| > 65 | 74 (20.3) | |
| Sex | .807 | |
| Male | 114 (23.0) | |
| Female | 86 (22.2) | |
| Race | .322 | |
| White | 119 (20.7) | |
| Black | 37 (24.2) | |
| Asian | 11 (30.6) | |
| Other | 33 (27.5) | |
| Country of residence | .970 | |
| Within US | 192 (22.6) | |
| Outside US | 8 (22.9) | |
| Insurance | .143 | |
| Private | 95 (26.8) | |
| Medicare | 70 (17.9) | |
| Medicaid | 16 (30.2) | |
| Self-pay | 13 (21.3) | |
| Uninsured | 4 (20.0) | |
| Other | 2 (33.3) | |
| Cancer type | .079 | |
| Head and neck | 5 (16.7) | |
| GI | 150 (26.3) | |
| Thoracic | 8 (13.8) | |
| Bones/joints/soft tissue/skin | 3 (11.5) | |
| Breast | 6 (12.2) | |
| Urogenital | 12 (18.8) | |
| Endocrine | 6 (25.0) | |
| Lymphoma/multiple myeloma/leukemia | 6 (17.6) | |
| Other | 4 (13.8) | |
| Disease stage | .002 | |
| Localized | 15 (14.3) | |
| Regional | 41 (18.3) | |
| Distant | 125 (29.2) | |
| Unstaged | 14 (15.6) | |
| No evidence of disease | 5 (13.5) | |
| No. of comorbidities | < .001 | |
| < 3 | 67 (16.8) | |
| ≥ 3 | 133 (27.4) | |
| Discharge status | < .001 | |
| Home | 165 (24.4) | |
| Home health | 26 (34.2) | |
| Hospice | 2 (2.6) | |
| Transfer to another facility | 7 (13.0) | |
| Discharge day | .345 | |
| Sunday | 9 (20.5) | |
| Monday | 26 (22.8) | |
| Tuesday | 22 (16.1) | |
| Wednesday | 37 (23.4) | |
| Thursday | 39 (28.9) | |
| Friday | 46 (22.2) | |
| Saturday | 21 (23.6) | |
| Length of stay, days | .099 | |
| ≤ 4 | 94 (20.3) | |
| > 4 | 106 (25.1) | |
| ICU days | .736 | |
| ≤ 0 | 186 (22.8) | |
| > 0 | 14 (20.9) |
NOTE. Unit of analysis is a single hospitalization encounter.
Abbreviation: ICU, intensive care unit.
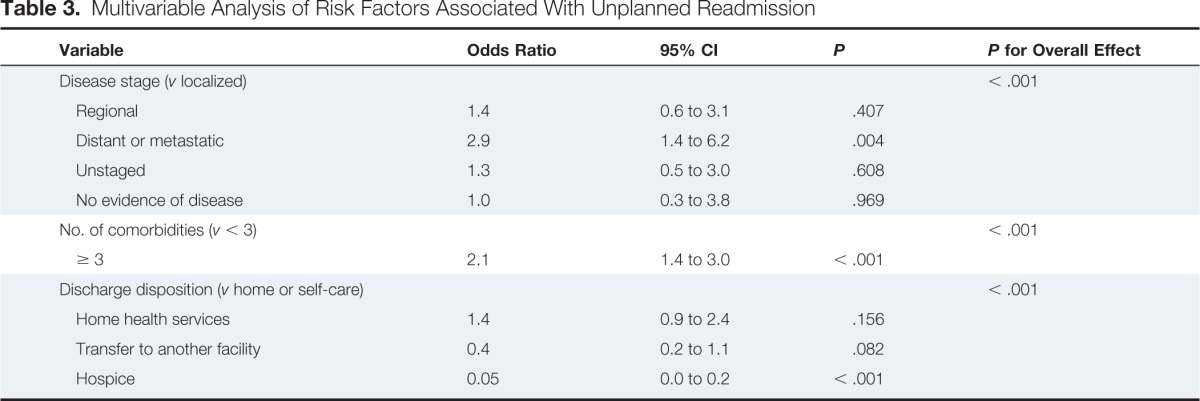
Multivariable analysis showed that compared to those with localized disease, those with distant or metastatic disease were more likely to have unplanned readmission (odds ratio [OR] = 2.9; 95% CI, 1.4 to 6.2); compared to those with fewer than three comorbidities, patients with three or more comorbidities were associated with a significantly increased likelihood of unplanned readmission (OR = 2.1; 95% CI, 1.4 to 3.0); and compared to those who were discharged to self-care, patients who were discharged to hospice were significantly less likely to be readmitted within 30 days of discharge (OR = 0.05; 95% CI, 0.0 to 0.2; Table 3).
Table 3.
Multivariable Analysis of Risk Factors Associated With Unplanned Readmission
| Variable | Odds Ratio | 95% CI | P | P for Overall Effect |
|---|---|---|---|---|
| Disease stage (v localized) | < .001 | |||
| Regional | 1.4 | 0.6 to 3.1 | .407 | |
| Distant or metastatic | 2.9 | 1.4 to 6.2 | .004 | |
| Unstaged | 1.3 | 0.5 to 3.0 | .608 | |
| No evidence of disease | 1.0 | 0.3 to 3.8 | .969 | |
| No. of comorbidities (v < 3) | < .001 | |||
| ≥ 3 | 2.1 | 1.4 to 3.0 | < .001 | |
| Discharge disposition (v home or self-care) | < .001 | |||
| Home health services | 1.4 | 0.9 to 2.4 | .156 | |
| Transfer to another facility | 0.4 | 0.2 to 1.1 | .082 | |
| Hospice | 0.05 | 0.0 to 0.2 | < .001 |
Discussion
We found an unplanned readmission rate of 22.6% in our cohort of patients discharged from the General Internal Medicine Hospitalist Service at MD Anderson. In a similar study by Saunders et al14 that was performed at a comprehensive cancer hospital, the readmission rate was 11%. The study involved both surgical and medical patients with CMS as the primary payer, and the outcome studied was related readmissions only. This difference in cohort and outcome definition likely explains the discrepancy in rates observed between our two studies. Another academic hospital found readmission rates across different cancer patients ranging from 4.0% (genitourinary) to 19.3% (GI).2 However, that study considered only related readmissions in their outcome definition, and again, this may account for the difference in our findings. Brooks et al15 observed a readmission rate of 27% among patients with GI cancer discharged from a cancer institute. This is in fact similar to the readmission rate observed among our patients with GI cancer (Table 2). One pan-Canadian study that examined readmission rates among patients with cancer after medical visits reported a readmission rate of 19.6%.10 Although closer to our estimate, this study included hospitalizations at any acute care facility, and not cancer hospitals alone. The authors did note a lower readmission rate after surgical visits (9.3%), which may justify examining readmission rates after surgical and medical visits separately.
Our descriptive analysis showed that half of our admitted patients had three or more comorbidities, and nearly half had metastatic disease. Both of these factors were associated with unplanned readmission in our cohort. This suggests a patient population that may be more complex than most general hospitals and supports the importance of adjusting risk indices by patient case mix and severity of illness.
Fifty percent of patients who experienced unplanned readmission in our cohort were readmitted within 10 days of discharge. A study on readmissions after colon cancer surgery showed similar findings, with a median time to readmission of 9 days.16 Saunders et al14 reported a median time to readmission of 8.5 days in their cancer hospital. In another study, patients who underwent surgery for hepato-pancreato-biliary malignancies were found to have a mean time to readmission of 11.3 days.11 Readmissions after medical visits and surgical visits may vary. Nevertheless, the 10-day window described in our study suggests that more than half of unplanned cancer readmissions could potentially be affected, if interventions are implemented in the first 10 days after discharge.
In our study, some of the most common reasons for unplanned readmission appeared to be cancer-related. Sixty percent of the patients in our cohort had GI cancer, and some of our findings may have been driven by this population characteristic. However, some diagnoses that led to unplanned readmission in our cohort, such as urinary tract infection and complications of treatment, may be considered amenable to outpatient management. According to the Agency for Healthcare Research and Quality, some of these hospitalizations are potentially preventable, if high-quality preventive care and primary care are practiced.17 Although this supports initiatives to strengthen coordination of care among health care providers in general, these potentially preventable conditions may not be as straightforward in patients with cancer as in the general population as a result of their immunocompromised status. More studies are needed to examine the reasons for readmission of patients with cancer in comprehensive cancer centers, to better define which ones are preventable, and to appropriately apply standardized readmission measures to this population.
An important component of understanding readmission patterns is identification of risk factors for readmission, as was performed in our study. This allows for risk stratification of patients as they are admitted in the inpatient setting. This could be useful for resource allocation and identification of special populations that can be targeted for specific interventions to help reduce readmissions. Having multimorbidity, for example, was identified as a significant predictor for readmission in our study. This is not surprising, as comorbidity is actually one of the most consistent predictors of readmission in both cancer and noncancer populations.10,16,18,19 This emphasizes the need for strong chronic disease management especially in the outpatient setting, as well as the need to ensure that patients have a primary care provider who will be able to follow and manage other medical issues after discharge. Although different studies have observed variable outcomes in terms of the impact of outpatient follow-up and primary care access on readmission rates, patient-centered coordinated care is high-value and high-quality care and should be the best practice.20 Interventions that focus on this and its effectiveness in the cancer population could be a focus of future studies.
In a 2011 study of a cohort of general medical patients at a single academic medical center, both metastatic and nonmetastatic cancers were associated with readmission.21 In a study by Rocque et al22 done in an academic inpatient oncology service, unplanned hospitalizations in patients with metastatic disease was a marker for poor survival. The authors believed these encounters represent opportunities to transition appropriate patients to end-of-life care. Forty-seven percent of our population, in fact, had metastatic disease at time of presentation to our hospital. Although the proportion is less than that observed in other studies investigating cancer hospitalizations, adjusted multivariable analysis identifies this as a risk factor significantly associated with unplanned readmission nonetheless. This raises the question of whether a proportion of our patients were eligible for end-of-life care. A strong partnership and continued discussion with primary oncologists are necessary to make this determination.
We also found that patients discharged to home hospice or inpatient hospice were less likely to be readmitted. This was not surprising, and it is likely that hospice is an appropriate disposition for many patients with cancer who are symptomatic as a result of progressive or widely metastatic disease. Future investigations can focus on identifying patients who fall into this category and assessing whether or not patients who are appropriate for transition to palliative care contribute to high readmission rates on our service.
To the best of our knowledge, no previously published work has described unplanned readmission patterns in a general internal medicine hospitalist service at a comprehensive cancer center. If readmission measures are to be applied to these kinds of hospitals, more work is needed to understand the factors that contribute to overall unplanned readmission rates. We have reported readmission rate data for our particular service, but these data may be quite different from the hospital-wide, all-cause unplanned readmission rates and patterns for the entire cancer center, which admits surgical patients as well. Patients admitted under the leukemia, lymphoma, and phase I service at the cancer center also were not included in our cohort. This limits the generalizability of our findings to centers with the same patient mix as is generally seen by the General Internal Medicine Hospitalist Service at MD Anderson. Moreover, we were unable to capture readmissions to other hospitals, and thus our unplanned readmission rate may actually be an underestimate. Another limitation of our study is the inability to include socioeconomic status in our model as a result of database limitations. We did investigate insurance status as a possible predictor of readmission. Medicaid eligibility has been used by other authors as an indicator of poverty, although one can argue that there may be better proxy indicators.6
In conclusion, we have described the unplanned readmission rate and factors contributing to unplanned readmission in a population of medical patients admitted to a hospitalist service at a comprehensive cancer center. The risk factors for unplanned readmission that we identified can allow us to risk stratify our patients and develop interventions tailored to our specific population. Equally important, our baseline data can help inform current efforts at developing risk-adjustment models and benchmark indices for readmissions that are specific to cancer centers. Regardless of the validity of readmissions as a quality measure applied to this particular population (ie, patients admitted to comprehensive cancer centers), initiatives to reduce readmissions are always of interest because they encourage good clinical practice and enhance patient care.
Acknowledgment
Supported by the National Institutes of Health Cancer Center Support Grant, No. CA016672. Data presented in part at the Annual Meeting of the Society of Hospital Medicine, Las Vegas, NV, March 24, 2014; at the International Forum on Quality and Safety in Health Care, Paris, France, April 8-11, 2014; and at the American Society of Clinical Oncology Quality Care Symposium, San Diego, CA, October 17-18, 2014.
The information contained in this article was based on the Clinical Data Base provided by the University HealthSystem Consortium. The data presented herein are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health or the University HealthSystem Consortium. We thank Karl Jonsson and the Section of Hospital Medicine, Department of General Internal Medicine at The University of Texas MD Anderson Cancer Center for their assistance in data collection and technical support, and Erica Goodoff for help in editing this article.
Appendix
Figure A1.
Cohort selection algorithm.
Authors' Disclosures of Potential Conflicts of Interest
Disclosures provided by the authors are available with this article at jop.ascopubs.org.
Author Contributions
Conception and design: Joanna-Grace M. Manzano, Sahitya Gadiraju, Adarsh Hiremath, Jeff Farroni, Josiah Halm
Administrative support: Joanna-Grace M. Manzano
Collection and assembly of data: Joanna-Grace M. Manzano, Sahitya Gadiraju, Adarsh Hiremath, Jeff Farroni, Josiah Halm
Data analysis and interpretation: Joanna-Grace M. Manzano, Sahitya Gadiraju, Adarsh Hiremath, Heather Yan Lin, Josiah Halm
Manuscript writing: All authors
Final approval of manuscript: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Unplanned 30-Day Readmissions in a General Internal Medicine Hospitalist Service at a Comprehensive Cancer Center
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or jop.ascopubs.org/site//misc/ifc.xhtml.
Joanna-Grace M. Manzano
No relationship to disclose
Sahitya Gadiraju
No relationship to disclose
Adarsh Hiremath
No relationship to disclose
Heather Yan Lin
No relationship to disclose
Jeff Farroni
No relationship to disclose
Josiah Halm
Consulting or Advisory Role: Otsuka
References
- 1.Medicare Payment Advisory Commission. Report to the Congress: Promoting Greater Efficiency in Medicare. Washington, DC: Medicare Payment Advisory Commission; 2007. pp. 103–120. [Google Scholar]
- 2.Brown EG, Burgess D, Li CS, et al. Hospital readmissions: Necessary evil or preventable target for quality improvement. Ann Surg. 2014;260:583–589. doi: 10.1097/SLA.0000000000000923. discussion 589-591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 4.Medicare Payment Advisory Commission. Report to the Congress: Medicare and the Health Care Delivery System. Washington, DC: Medicare Payment Advisory Commission; 2013. pp. 91–114. [Google Scholar]
- 5.Kocher RP, Adashi EY. Hospital readmissions and the Affordable Care Act: Paying for coordinated quality care. JAMA. 2011;306:1794–1795. doi: 10.1001/jama.2011.1561. [DOI] [PubMed] [Google Scholar]
- 6.Singh S, Lin YL, Kuo YF, et al. Variation in the risk of readmission among hospitals: The relative contribution of patient, hospital and inpatient provider characteristics. J Gen Intern Med. 2013;29:572–578. doi: 10.1007/s11606-013-2723-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Comprehensive Cancer Center Consortium for Quality Improvement. Activities. www.c4qi.net/
- 8.University HealthSystem Consortium. About UHC. https://www.uhc.edu/12443.htm.
- 9.Halfon P, Eggli Y, van Melle G, et al. Measuring potentially avoidable hospital readmissions. J Clin Epidemiol. 2002;55:573–587. doi: 10.1016/s0895-4356(01)00521-2. [DOI] [PubMed] [Google Scholar]
- 10.Ji H, Abushomar H, Chen X, et al. All-cause readmission to acute care for cancer patients. Healthc Q. 2012;15:14–16. doi: 10.12927/hcq.2013.23044. [DOI] [PubMed] [Google Scholar]
- 11.Schneider EB, Hyder O, Wolfgang CL, et al. Patient readmission and mortality after surgery for hepato-pancreato-biliary malignancies. J Am Coll Surg. 2012;215:607–615. doi: 10.1016/j.jamcollsurg.2012.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Horwitz LI, Grady JN, Dorsey KB, et al. New Haven, CT: Yale New Haven Health Services Corporation/Center for Outcomes Research and Evaluation; 2014. 2014 Measures Updates and Specifications Report: Hospital-Wide All-Cause Unplanned Readmission. [Google Scholar]
- 13.Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Saunders ND, Nichols SD, Antiporda MA, et al. Examination of unplanned 30-day readmissions to a comprehensive cancer hospital. J Oncol Pract. 2015;11:e177–e181. doi: 10.1200/JOP.2014.001546. [DOI] [PubMed] [Google Scholar]
- 15.Brooks GA, Abrams TA, Meyerhardt JA, et al. Identification of potentially avoidable hospitalizations in patients with GI cancer. J Clin Oncol. 2014;32:496–503. doi: 10.1200/JCO.2013.52.4330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Greenblatt DY, Weber SM, O'Connor ES, et al. Readmission after colectomy for cancer predicts one-year mortality. Ann Surg. 2010;251:659–669. doi: 10.1097/SLA.0b013e3181d3d27c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kruzikas DT, Jiang HJ, Remus D, et al. Rockville, MD: Agency for Healthcare Research and Quality; 2004. Preventable Hospitalizations: A Window Into Primary and Preventive Care 2000. [Google Scholar]
- 18.Marcantonio ER, McKean S, Goldfinger M, et al. Factors associated with unplanned hospital readmission among patients 65 years of age and older in a Medicare managed care plan. Am J Med. 1999;107:13–17. doi: 10.1016/s0002-9343(99)00159-x. [DOI] [PubMed] [Google Scholar]
- 19.Silverstein MD, Qin H, Mercer SQ, et al. Risk factors for 30-day hospital readmission in patients ≥ 65 years of age. Proc (Bayl Univ Med Cent) 2008;21:363–372. doi: 10.1080/08998280.2008.11928429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Agency for Healthcare Research and Quality. Care Coordination Measures Atlas Update: Chapter 1: Background. Rockville, MD: Agency for Healthcare Research and Quality; 2014. [Google Scholar]
- 21.Allaudeen N, Vidyarthi A, Maselli J, et al. Redefining readmission risk factors for general medicine patients. J Hosp Med. 2011;6:54–60. doi: 10.1002/jhm.805. [DOI] [PubMed] [Google Scholar]
- 22.Rocque GB, Barnett AE, Illig LC, et al. Inpatient hospitalization of oncology patients: Are we missing an opportunity for end-of-life care? J Oncol Pract. 2013;9:51–54. doi: 10.1200/JOP.2012.000698. [DOI] [PMC free article] [PubMed] [Google Scholar]