Abstract
Purpose/Objective(s)
To determine trends in radiation oncology malpractice claims and expenses during the last 28 years and compare malpractice claims between radiation oncology and other specialties.
Methods and Materials
We performed a retrospective analysis of closed malpractice claims filed from 1985 to 2012 collected by a nationwide medical liability insurance trade association. We analyzed characteristics and trends among closed claims, indemnity payments (payments to plaintiff), and litigation expenses. We also compared radiation oncology to 21 other medical specialties. Time series dollar amounts were adjusted for inflation (2012 index year).
Results
There were 1,517 closed claims involving radiation oncology, of which 342 (22.5%) were paid. Average and median indemnity payments were $276,792 and $122,500, ranking 5th and 8th among the 22 specialty groups, respectively. Linear regression modeling of time trends showed decreasing total number of claims (β=−1.96 annually, p=0.003), increasing average litigation expenses paid (β=+$1472 annually, p≤0.001), and no significant change in average indemnity payments (β=−$681, p=0.89).
Conclusions
Medical professional liability claims filed against radiation oncologists are not common and have declined in recent years. However, indemnity payments in radiation oncology are large relative to many other specialties. In recent years, the average indemnity payment has been stable, while litigation expenses have increased.
Introduction
The rationale for the medical malpractice liability system is to compensate patients injured due to negligent care and deter providers from practicing negligently1. It is unclear whether this system improves patient safety and quality of care2,3. Certainly, being sued for medical malpractice is a great concern to practicing physicians4. One study from a large liability insurer covering over 40,000 physicians found that 7.4% of all physicians face a malpractice claim in any given year, with 1.6% facing a claim resulting in payment5.
Despite media attention to catastrophic medical errors in radiation oncology6–9, there are very few systematic studies of malpractice claims in the specialty. Elliot et al.10 evaluated 13 cases involving prostate brachytherapy, where claims typically involved an alleged breach of standard of care. Another study reviewing 20 malpractice suits involving a single expert reviewer identified the most common allegations as delays in diagnosis, breach of standard of care, or failure to obtain a second opinion11. Neither of these studies reported the severity of claims or litigation expenses. Studies of malpractice claims filed against oncologists in lung cancer, head and neck cancers, skin cancer, and sarcoma12–17 have neglected implications for radiation oncology. Furthermore, these studies12–17 only describe cases that were formally adjudicated in court, representing only 8% of all filed malpractice claims.18
This study sought to determine trends in radiation oncology malpractice claims and expenses during the last 28 years. We also compared malpractice claims between radiation oncology and other specialties.
Methods and Materials
We performed a retrospective analysis of medical liability claims data from the Physician Insurers Association of America (PIAA) that identified a radiation oncologist as the primary defendant between January 1, 1985, and December 31, 2012. The PIAA is a non-profit trade association representing medical professional liability insurance companies who insure more than two-thirds of private practice physicians in the United States19. The PIAA Data Sharing Project (DSP) is a database containing information on over 278,000 closed medical liability claims from 25 participating companies, representing the largest independent database of medical liability claims with specialty-specific data19.
Primary outcome variables were closed claims, paid claims, percentage of closed claims resulting in indemnity payment to the plaintiff, average indemnity payments, and average litigation expenses for each year of the study period and for the most recent 10 years. A “claim” was defined as any written demand for monetary compensation by a patient or patient’s family stemming from an alleged injury during the patient’s medical care by the insured clinician. A claim was "closed" when there was a resolution by settlement, by court verdict or arbitration, or when a claim was withdrawn, dropped, or dismissed without payment. Indemnity is defined as compensation "for loss or damage that has already occurred, or to guarantee through contractual agreement to repay another party for loss or damage that occurs in the future20." Adjudicatory outcomes included whether the claim resulted in indemnity payment to the plaintiff (“paid claims "), was ended without payment ("no indemnity "), and amount of indemnity payment ("severity"). Litigation expenses ("expenses"), also known as loss adjustment expenses, were also analyzed. These expenses are related to the defense of a liability claim, including expenses paid in the process of administering or adjudicating a claim (such as investigative costs, attorney fees, expert witness fees, court costs, etc.19,21).
First, we evaluated sued physician demographics as compared to the national radiation oncology workforce. Demographic information about the involved radiation oncologist was obtained by PIAA when available and released by the insurer. Because PIAA does not report the number of insured physicians, we used annual workforce data as reported in the American Medical Association (AMA) Physician Masterfile22 to estimate the number of active physicians in each specialty per year in the United States. National workforce data from calendar years 1987, 1990, 1994 and 2002 are not available in the AMA Physician Characteristics and Distribution publication; therefore, linear interpolation to impute the data for the missing years was performed because demographic data were provided in aggregate and variability in physician workforce data for each specialty is expected to be constant (stationary) with time23,24. Demographic comparisons between sued radiation oncologists and the national radiation oncology workforce were performed using Pearson’s chi-squared test for the entire study period as well as for the last 10 years (2003–2012) in order to evaluate recent demographic characteristics.
We then performed a cross-sectional comparison of claims closed during the study period for radiation oncology and 21 other medical specialties. Closed claims, paid claims, and average and median indemnity, and total indemnity were described for each specialty. Median indemnity payments were included when comparing specialties to represent the most common experience in each specialty due to outliers in the data23. We calculated an estimated proportion of active physicians represented in the PIAA DSP by specialty, since the number of active physicians varies considerably by medical specialty. This was done by dividing the number of claims by the cumulative number of active physicians per “physician-year” during the period from AMA workforce data described above, representing the maximum proportion of physicians in each specialty that have a claim in the PIAA DSP. This exploratory analysis was a simple proportion, and not intended as a direct normalization/risk calculation because inherent population differences between the PIAA and AMA datasets preclude the latter.
Finally, we analyzed time trends of closed claims, paid claims, percentage of closed claims that were paid, average indemnity payments, and average litigation expenses for radiation oncology using simple linear regression and log-linear regression. These were reported as trend or annual change (β) and average annual percent change (exp(β) −1)25. We also evaluated claims by associated personnel defined as any associated professional that was named in the claim.
All tests were performed using a=0.05 and 95% confidence intervals. Time series dollar amounts were adjusted for inflation using the Consumer Price Index for All Urban Consumers for All Items with 2012 as the index year26. Statistical analyses were conducted using SPSS software, version 22.0 (IBM Corp., Armonk, NY).
Results
From 1985 to 2012, 1,517 closed claims reported to the PIAA DSP involved radiation oncologists, of which 342 (22.5%) were paid. Table 1 shows demographics of sued radiation oncologists compared with active physicians. Sued radiation oncologists were primarily in solo practice (72.2%), and were more likely to be middle aged (ages 35–54, p<0.001) as compared with national workforce demographic data. The proportion of physicians sued previously was 71.9% and 91.9% of sued physicians were board certified. However these physicians represent only 41.5% and 51.0% of sued physicians because only about 50% of claims reported these data. Sued radiation oncologists were more likely to be male (p<0.001), and international medical graduates (IMGs) (p=0.002). In the last 10 years, there was no difference in the proportion of international medical graduates sued as compared to the national workforce (p=0.41), and a smaller proportion of sued physicians were in solo practice (52% vs. 72% for 1985–2012).
Table 1.
Radiation oncology physician demographics: PIAA sued physicians and the AMA physician workforce, 1985–2012 and 2003–2012
| Radiation Oncologists: 1985–2012 | Radiation Oncologists: 2003–2012 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| PIAA* | AMA† | PIAA* | AMA† | |||||||
| N | % | N | % | p-value†† | N | % | N | % | p-value†† | |
| Age Groups | ||||||||||
| <35 | 121 | 8.0% | 17,659 | 16.8% | <0.001 | 16 | 4.4% | 6,418 | 14.1% | <0.001 |
| 35–44 | 508 | 33.5% | 31,740 | 30.2% | 90 | 24.9% | 11,320 | 24.9% | ||
| 45–54 | 557 | 36.7% | 29,261 | 27.8% | 179 | 49.4% | 13,688 | 30.1% | ||
| 55–64 | 221 | 14.6% | 18,118 | 17.2% | 68 | 18.8% | 9,387 | 20.6% | ||
| ≥65 | 110 | 7.3% | 8,454 | 8.0% | 9 | 2.5% | 4,669 | 10.3% | ||
| Total | 1,517 | 105,226 | 362 | 45,482 | ||||||
| Employment Status | ||||||||||
| Full-Time | 1,284 | 98.3% | -- | -- | -- | 346 | 97.7% | -- | -- | -- |
| Part-Time | 22 | 1.7% | -- | -- | -- | 8 | 2.3% | -- | -- | -- |
| Total | 1,306 | -- | 354 | -- | ||||||
| Gender | ||||||||||
| Male | 1,212 | 92.8% | 81,845 | 77.8% | <0.001 | 315 | 89.0% | 34,218 | 75.2% | <0.001 |
| Full-Time | 1,196 | 98.7% | -- | -- | 309 | 98.1% | -- | -- | ||
| Part-Time | 16 | 1.3% | -- | -- | 6 | 1.9% | -- | -- | ||
| Female | 94 | 7.2% | 23,381 | 22.2% | 39 | 11.0% | 11,264 | 24.8% | ||
| Full-Time | 88 | 93.6% | -- | -- | 37 | 94.9% | -- | -- | ||
| Part-Time | 6 | 6.4% | -- | -- | 2 | 5.1% | -- | -- | ||
| Total | 1,306 | 105,226 | 354 | 45,482 | ||||||
| Board Certification | ||||||||||
| Board Certified | 774 | 91.9% | 82,022 | 77.9% | <0.001 | 225 | 86.9% | 37,032 | 81.4% | 0.02 |
| Not Board Certified | 68 | 8.1% | 23,204 | 22.1% | 34 | 13.1% | 8,450 | 18.6% | ||
| Total | 842 | 105,226 | 259 | 45,482 | ||||||
| Previous Claims Experience | ||||||||||
| Previous Claims Experience | 631 | 71.9% | -- | -- | -- | 52 | 67.5% | -- | -- | -- |
| No Previous Claims Experience | 246 | 28.1% | -- | -- | -- | 25 | 32.5% | -- | -- | -- |
| Total | 877 | -- | 77 | -- | ||||||
| Medical School | ||||||||||
| US Medical Graduate | 1,155 | 76.4% | 83,754 | 79.6% | 0.002 | 292 | 81.6% | 37,835 | 83.2% | 0.41 |
| International Medical Graduate | 357 | 23.6% | 21,472 | 20.4% | 66 | 18.4% | 7,647 | 16.8% | ||
| Total | 1,512 | 105,226 | 358 | 45,482 | ||||||
| Practice Type | ||||||||||
| Group Practice | 302 | 19.9% | -- | -- | -- | 86 | 23.9% | -- | -- | -- |
| Solo Practice | 1,094 | 72.2% | -- | -- | -- | 188 | 52.2% | -- | -- | -- |
| Institution | 119 | 7.9% | -- | -- | -- | 86 | 23.9% | -- | -- | -- |
| Total | 1,515 | -- | 360 | -- | ||||||
Abbreviations: PIAA = Physician Insurers Association of America; AMA=American Medical Association
Represents insured as reported on a per claim basis that released demographic information.
Cumulative active radiation oncology physicians for all years (physician-years) calculated using the annual number of active physicians reported in the AMA masterfile22.
P-value for Pearson’s chi-squared test (α=0.05, 95% CI)
-- not available
Radiation oncology had the fewest number of closed claims (<1%) among all reported specialties during the 28-year period (Table 2). Only 22.5% of closed claims resulted in indemnity payment, ranking radiation oncology 18th of 22 specialties in percentage of closed claims paid. The specialties with the highest percentage of closed claims paid were obstetrics and gynecology, general surgery, and otorhinolaryngology (34.2%, 33.4%, and 33.2%, respectively); gastroenterology ranked last (18.1%).
Table 2.
Characteristics of closed claims and indemnity payments by medical specialty, 1985–2012
| Cumulative Closed Claims | |||||||
|---|---|---|---|---|---|---|---|
| Medical Specialty | Closed Claims* |
Paid Claims† |
% Paid of Closed Claims†† |
Total Indemnity Payment‖ |
Average Indemnity Payment¶ |
Median Indemnity Payment |
Largest Indemnity Payment |
| Anesthesiology | 11,030 | 3,470 | 31.5% | $856,516,675 | $246,835 | $96,774 | $5,048,678 |
| Cardiology | 5,371 | 1,032 | 19.2% | $271,207,784 | $262,798 | $156,250 | $2,000,000 |
| Cardiothoracic Surgery | 7,948 | 1,900 | 23.9% | $457,058,679 | $240,557 | $125,000 | $5,005,000 |
| Dermatology | 3,198 | 906 | 28.3% | $130,900,558 | $144,482 | $35,000 | $3,000,000 |
| Emergency Medicine | 6,887 | 1,864 | 27.1% | $461,440,009 | $247,554 | $120,000 | $2,000,000 |
| Gastroenterology | 3,521 | 661 | 18.8% | $170,353,285 | $257,721 | $119,559 | $4,000,000 |
| General and Family Practice | 30,453 | 9,639 | 31.7% | $1,703,213,764 | $176,700 | $82,246 | $7,239,248 |
| General Surgery | 29,400 | 9,822 | 33.4% | $1,978,471,304 | $201,433 | $99,999 | $3,116,180 |
| Internal Medicine | 37,216 | 9,271 | 24.9% | $2,106,112,462 | $227,172 | $101,400 | $12,000,000 |
| Neurology | 4,474 | 979 | 21.9% | $326,529,544 | $333,534 | $175,000 | $5,000,000 |
| Neurosurgery | 6,443 | 1,814 | 28.2% | $599,483,751 | $330,476 | $183,735 | $5,600,000 |
| Obstetrics and Gynecology | 40,266 | 13,761 | 34.2% | $3,959,561,785 | $286,324 | $149,250 | $13,000,000 |
| Ophthalmology | 7,893 | 2,232 | 28.3% | $429,207,088 | $192,297 | $100,000 | $3,550,000 |
| Orthopedic Surgery | 25,707 | 7,404 | 28.8% | $1,329,643,166 | $179,584 | $90,000 | $3,000,000 |
| Otorhinolaryngology | 4,627 | 1,529 | 33.1% | $336,006,438 | $219,756 | $100,000 | $4,199,329 |
| Pathology | 1,991 | 594 | 29.8% | $158,426,561 | $266,711 | $137,500 | $2,700,000 |
| Pediatrics | 7,825 | 2,180 | 27.9% | $618,020,900 | $283,496 | $126,251 | $5,250,000 |
| Plastic Surgery | 10,174 | 2,697 | 26.5% | $333,545,019 | $123,673 | $50,000 | $2,000,000 |
| Psychiatry | 2,666 | 526 | 19.7% | $84,278,265 | $160,225 | $55,000 | $2,375,000 |
| Radiation Oncology | 1,517 | 342 | 22.5% | $94,662,971 | $276,792 | $122,500 | $2,700,000 |
| Radiology | 16,411 | 4,740 | 28.9% | $1,088,473,008 | $229,636 | $100,000 | $3,364,156 |
| Urologic Surgery | 7,099 | 2,009 | 28.3% | $402,586,508 | $200,391 | $100,000 | $3,200,000 |
| All specialties | 272,117 | 79,372 | 29.2% | $17,895,699,524 | $225,221 | $100,000 | $13,000,000 |
Closed claims are medical liability claims that have been resolved through settlement or verdict or withdrawn, dropped or dismissed without payment.
Paid Claims are medical liability claims that resulted in indemnity payment to the plaintiff as a result of settlement or court adjudication.
Percent paid of closed claims refers to the percentage of all closed claims that were paid to the plaintiff as a result of settlement or court adjudication.
Total indemnity is the sum of all indemnity payments during the period.
Average indemnity is the mean amount of award for paid claims during the period.
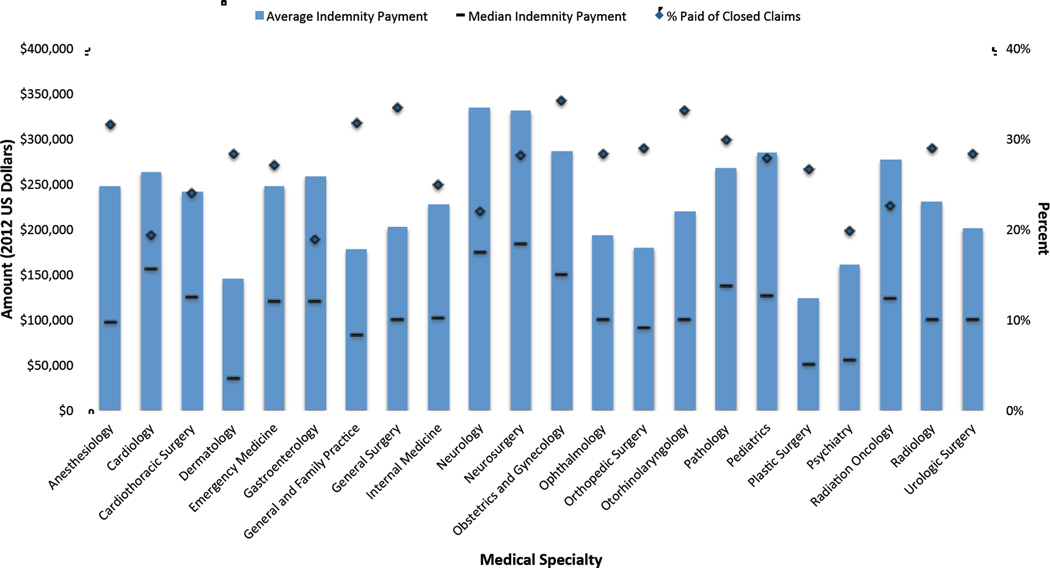
The average indemnity payment per claim for radiation oncology was $276,972, ranking radiation oncology 5th of 22 specialties. The median indemnity payment was lower than the average indemnity payment for all specialties (Figure 1). Total payments for radiation oncology claims ($94,661,971) represented fewer than 1% of total payments for all specialties during the study period ($17,895,699,524). The median indemnity payment for radiation oncology was $122,500, ranking radiation oncology 8th of 22 specialties. The specialties with the highest median indemnity were neurosurgery ($183,735) and neurology ($175,000); dermatology had the lowest median payment of only $35,000.
Figure 1.
Characteristics of closed claims and indemnity payments by medical specialty, 1985–2012
Vertical bars (blue) represent average indemnity payment, with horizontal lines (black) indicating median indemnity for each specialty group during the period. Diamond markers (dark blue) illustrate the percent paid of closed claims--the percentage of all closed claims that were paid to the plaintiff as a result of settlement or court adjudication.
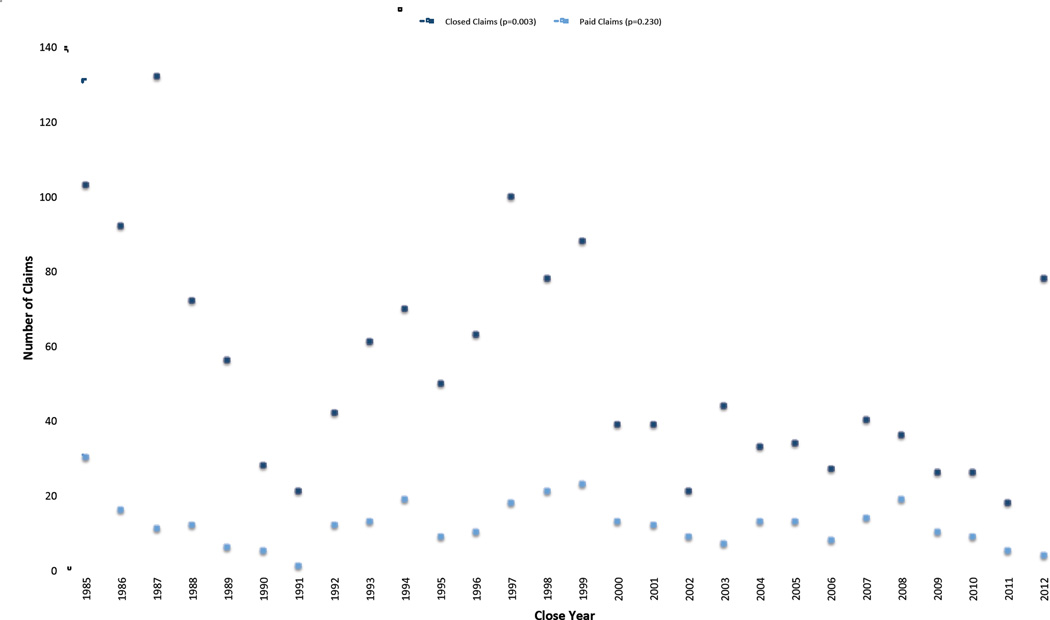
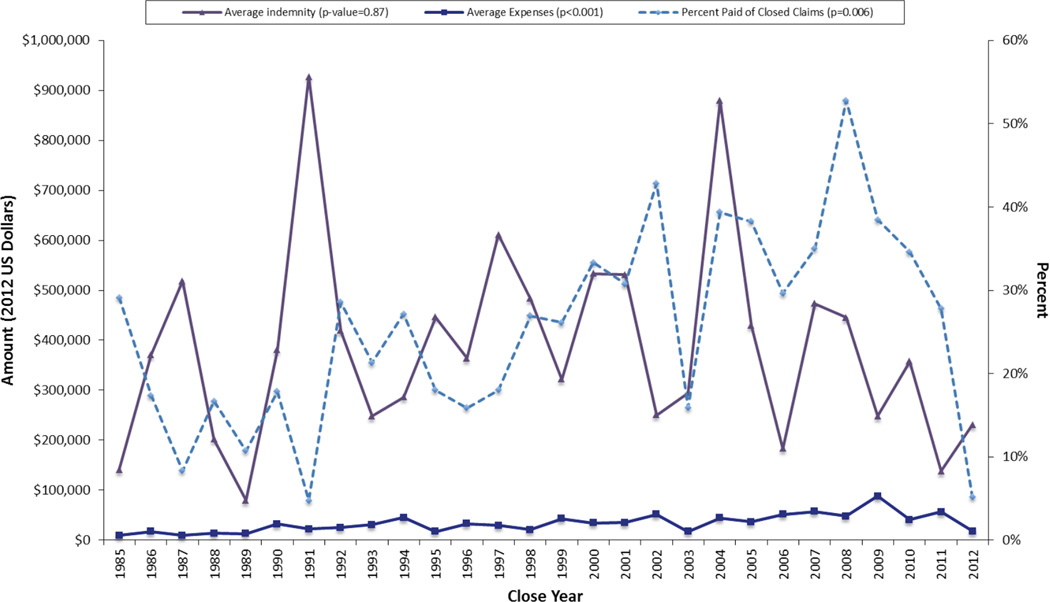
Estimates of the proportion of physicians in each specialty that had closed and paid claims in the PIAA DSP are presented in Table 3. These estimates show that the maximum proportion of the radiation oncology workforce represented in the DSP is 2.4% for closed claims and 0.68% for paid claims. Table 4 shows the trends of radiation oncology closed claims, payments, and expenses over time from 1985 to 2012 and 2003 to 2012. The number of radiation oncology closed claims decreased over time (β= −1.96 claims annually, p=0.003; −3.5% annually, p=0.003), the percent paid of closed claims increased (β =0.73% annually, p=0.006; +2.8% annually, p=0.046), and average expenses paid increased (β =$1472 annually, p≤0.001; +5.0% annually, p<0.001). No significant trend was observed for the average indemnity paid (p=0.89) (Figures 2a and 2b). No significant trend was observed for total indemnity or expenses, or total expenses for paid claims. Over the last 10 years, no significant trends were observed (Table 4).
Table 3.
Comparison of representation of the national physician workforce in the PIAA DSP by medical specialty, 1985–2012
| Closed Claims* | Paid Claims† | ||||
|---|---|---|---|---|---|
| Medical Specialty | Total physicians per year in the US†† (physician-years) |
Closed Claims* | Proportion of physicians with a closed claim in the PIAA DSP‖ |
Paid Claims† | Proportion of physicians with a paid claim in the PIAA DSP‖ |
| Plastic Surgery | 166,911 | 9,312 | 5.58 | 2,456 | 1.47 |
| Cardiothoracic Surgery | 89,818 | 4,962 | 5.52 | 917 | 1.02 |
| Neurosurgery | 139,304 | 5,954 | 4.27 | 1,698 | 1.22 |
| Orthopedic Surgery | 622,728 | 23,786 | 3.82 | 6,949 | 1.12 |
| Obstetrics and Gynecology | 1,083,903 | 37,682 | 3.48 | 13,034 | 1.20 |
| Radiology | 579,689 | 14,770 | 2.55 | 4,299 | 0.74 |
| General Surgery | 1,065,608 | 26,549 | 2.49 | 9,088 | 0.85 |
| Radiation Oncology | 105,226 | 2,531 | 2.41 | 715 | 0.68 |
| Urologic Surgery | 280,809 | 6,166 | 2.20 | 1,806 | 0.64 |
| Otorhinolaryngology | 257,287 | 4,360 | 1.69 | 1,417 | 0.55 |
| Ophthalmology | 489,935 | 7,378 | 1.51 | 2,097 | 0.43 |
| Cardiology | 548,966 | 7,724 | 1.41 | 1,826 | 0.33 |
| General and Family Practice | 2,326,387 | 29,031 | 1.25 | 9,215 | 0.40 |
| Neurology | 341,804 | 4,118 | 1.20 | 906 | 0.27 |
| Dermatology | 260,432 | 2,919 | 1.12 | 847 | 0.33 |
| Anesthesiology | 965,932 | 9,906 | 1.03 | 3,149 | 0.33 |
| Gastroenterology | 285,075 | 2,874 | 1.01 | 548 | 0.19 |
| Internal Medicine | 3,649,954 | 34,993 | 0.96 | 8,754 | 0.24 |
| Emergency Medicine | 635,639 | 4,926 | 0.77 | 1,268 | 0.20 |
| Pediatrics | 1,637,971 | 7,409 | 0.45 | 2,063 | 0.13 |
| Pathology | 500,270 | 1,795 | 0.36 | 519 | 0.10 |
| Psychiatry | 1,072,973 | 2,457 | 0.23 | 496 | 0.05 |
Abbreviations: PIAA = Physician Insurers Association of America; AMA=American Medical Association
Closed claims are medical liability claims that have been resolved through settlement or verdict or withdrawn, dropped or dismissed without payment.
Paid Claims are medical liability claims that resulted in indemnity payment to the plaintiff as a result of settlement or court adjudication.
Calculated using the number of active physicians for each specialty in 2012 obtained from AMA masterfile data22
Proportion of physicians with a closed or paid claim in the PIAA DSP is the number of closed or paid claims over the period divided by the number of physicians over the period in that specialty (physician-years), representing the maximum proportion of physicians in that specialty that have a claim in the DSP during the period.
Table 4.
Trends of radiation oncology closed claims and litigation expenses, 1985–2012 and 2003–2012
| 1985–2012 | 2003–2012 | |||||||
|---|---|---|---|---|---|---|---|---|
| Series | Trend* | Trend p-value |
Average Annual % Change† |
Average Annual % Change p-value |
Trend* | Trend p-value |
Average Annual % Change† |
Average Annual % Change p-value |
| Closed Claims | −1.96 | 0.003 | −3.57% | 0.003 | 0.99 | 0.64 | −0.39% | 0.93 |
| Paid Claims | −0.18 | 0.23 | −0.80% | 0.62 | −0.558 | 0.30 | −7.63% | 0.16 |
| Percent Paid of Closed Claims | 0.73% | 0.006 | 2.77% | 0.046 | −0.01% | 0.56 | −7.23% | 0.36 |
| Total Indemnity†† - All Claims | $4,941 | 0.95 | 0.58% | 0.78 | −$559,626 | 0.17 | −16.86% | 0.11 |
| Average Indemnity†† - All claims | −$681 | 0.89 | 0.22% | 0.87 | −$36,080 | 0.13 | −9.23% | 0.12 |
| Total Expenses‖†† - All Claims | $13,439 | 0.47 | 1.28% | 0.26 | $22,872 | 0.71 | 2.02% | 0.63 |
| Average Expenses‖†† - All Claims | $1,472 | <0.001 | 4.85% | <0.001 | $1,291 | 0.60 | 2.41% | 0.69 |
| Total Expenses‖†† - Paid Claims | $16,421 | 0.18 | 3.08% | 0.11 | −$12,446 | 0.82 | −4.29% | 0.61 |
| Average Expenses‖†† - Paid Claims | $1,742 | 0.008 | 3.88% | 0.001 | $2,308 | 0.50 | 3.34% | 0.48 |
| Total Expenses‖†† - No Indemnity Paid | −$2,982 | 0.78 | −0.18% | 0.88 | $35,319 | 0.16 | 4.29% | 0.24 |
| Average Expenses‖†† - No Indemnity Paid | $1,105 | 0.044 | 4.43% | <0.001 | $1,559 | 0.44 | 3.54% | 0.57 |
Trend over time modeled with linear regression.
Trend over time modeled with log-linear regression25.
Adjusted for inflation, 2012 index year26.
Expenses are litigation expenses related to the defense of a liability claim, including expenses paid in the process of administering or adjudicating a claim.
Figure 2.
a. Radiation oncology closed claims, 1985–2012: closed claims and paid claims
P-value represents significance of change in the number of claims over the time period modeled with linear regression.
b. Radiation oncology closed claims and litigation expenses, 1985–2012: average indemnity*, average expenses*, and percent paid of closed claims
*Adjusted for inflation, 2012 index year26.
P-value represents significance of change over time modeled with linear regression.
During the last 10 years, the two most common associated personnel named in closed claims included physicians (including radiologists, emergency medicine physicians, pathologists, and unspecificed ‘other’ physicians; named 140 times) and therapists (named 7 times). Up to three associated personnel are reported for each record so it is unclear how many individual claims reported associated personnel.
Discussion
The current study is the first comprehensive analysis of nation-wide medical liability claims data for radiation oncology, spanning 28 years. When comparing sued radiation oncologists in the PIAA DSP to the national radiation oncology workforce, we found that a greater proportion of sued physicians were male, and that only 5–6% of sued female physicians reported working part-time which is less than national estimates (17.5%)27. The larger proportion of males working full time may have influenced the gender of sued physicians, however the changing gender demographics of the radiation oncology workforce likely played a larger role; a greater number of claims were closed early in the study period when men represented a greater proportion of the workforce22. Our data show that the proportion of claims attributable to IMGs has decreased consistent with the proportion of IMGs in the radiation oncology workforce also decreasing from 31% in 1985 to 14% in 2012. We also found that the proportion of solo practitioners, compared with other practice types, was high amongst sued physicians. Data from the ACR survey between 1995–2003 shows relatively stable numbers of solo practitioners (8–11%)27,28 and recent NPPES data29 show that 12.5% of 4503 individual radiation oncologists were sole proprietors. Our study found that the proportion of claims attributed to solo practitioners has dropped from 72% overall to 52% for the last 10 years. Radiation oncology practice accreditation though ACR-ASTRO30, requiring peer review documentation, is one possible reason for reduction in claims by introducing increased quality assurance and peer review.
Radiation oncology-related liability claims represent fewer than 1% of all reported closed claims. We expect that this number would be <1% because radiation oncology physician-years during the study period also represent <1% of all physician-years for all specialties. Despite a growing physician workforce and patient population31 over the study period, the number of closed claims has recently declined by approximately 2% per year, and the number of paid claims has also decreased, though this trend was not significant. Our findings are similar, though to a lesser extent, to recent reports on the NPDB showing the number of closed and paid claims dropped 34% and 38%, respectively, in the last 10 years32. Previous authors have also found that payment amounts have not changed significantly in recent years32,33. Indemnity payments in radiation oncology are large relative to many other specialties, though we also found that these payments have been stable over time.
A recent decrease in the volatility of insurance premiums has also been observed34. In addition to other market factors, increased expenses have historically been associated with rising premiums and decreased availability of malpractice insurance35. While we don’t report on insurance premiums, we found that litigation expenses for all radiation oncology closed claims continued to rise on average from 1985 to 2012 for both paid claims and claims with no indemnity, though they have stabilized in the last 10 years. The 2010 final report36 by the Centers for Medicare and Medicaid Services on malpractice relative value units by specialty reflects the relative costs to practitioners of professional liability insurance. This report ranked radiation oncology as having a greater non-surgical risk than 32 of 37 non-surgical specialties. For surgical risk, radiation oncology ranked 15 of 46 specialties. Our data are consistent with CMS estimates that radiation oncology has higher non-surgical risk which may lead to higher payments, but less overall risk due to a lower risk factor associated with surgical procedures, thereby resulting in fewer claims36.
Recent PIAA DSP data on all physician specialties18 showed physicians faced an 8% increase in expenses from 2003 to 2012, and that expenses increased at a rate 2.5 times that of total indemnity payments. For our more recent data regarding total indemnity (2003–2012), data by year are unavailable so we are limited in our ability to comment on trends in indemnity payments without the possible influence of outliers. We also found that other physicians and technicians were the most common associated personnel named in claims. The involvement of associated personnel seems appropriate given the team-based environment in which radiation oncology is practiced, although we cannot comment on what types of claims involved other personnel due to the aggregate nature of the data.
Our study adds to the current literature by providing a large systematic analysis of closed (paid and unpaid) malpractice claims in the United States. Most prior studies of oncology claims have evaluated jury verdicts10,12–15, which are limited to approximately 8% of closed claims18. A prior study about claims in lung cancer patients also using PIAA data does not provide specific information on radiation oncology16. NPDB analyses do not include physician specialty, sufficient data regarding the nature of claims, or information on claims that were not paid21, and represent approximately 30% of all claims filed33,21. Furthermore, PIAA DSP data, while not generalizable given the lack of exposure data, do represent a greater proportion of the physician workforce than studies based on single or small numbers of insurance firms.
Our study has several limitations, many of which are inherent to the source data from the PIAA DSP. The most significant limitation is absence of exposure data. All information in the PIAA DSP database is reported on a per claim basis. They do not report the number of insured physicians in a given year, so it is not possible to directly calculate claims frequency per physician. We used the AMA Masterfile data for active physicians by specialty to understand what percentage of the national workforce was represented as having a closed claim in the PIAA DSP, but these data do not generalize beyond the DSP. Similarly, we compared differences in demographic information among sued radiation oncologists to the national radiation oncology workforce, but again these comparisons are limited in their generalizability beyond the DSP given the selection bias of the data that we are unable to evaluate. A second major limitation is that PIAA member companies have guidelines to ensure that there is consistency and uniformity in data collection and reporting, but there may certainly be errors in such a registry. However, McLean et al.16 analyzed PIAA coding used to aggregate data in the DSP and found only minor differences between the dataset and available case abstracts for malpractice litigation in the setting of lung cancer, suggesting the data for radiation therapy in the present study are likely to be representative of liability claims. Additionally, PIAA DSP aggregation of data without claim-specific or variance measures limit our ability to analyze and draw conclusions from the data presented. Still, the PIAA DSP database is the only national database that provides specialty-specific information on malpractice claims as well as information on closed claims that were not paid.
Our study, while important, demonstrates the need for additional, detailed analyses of the underlying causes of claims in radiation oncology to guide translation of these findings to risk reduction, preventing malpractice claims and improving patient safety37. Malpractice continues to be a significant concern for physicians, policy-makers and patients alike, as the rapidly evolving healthcare environment and ongoing legal battles surrounding malpractice reform add uncertainty to the future. While medical professional liability claims filed against radiation oncologists are not common, and the annual number of closed claims has declined, litigation expenses have increased and indemnity payments in radiation oncology are high relative to many other specialties. This evidence can inform efforts by physicians and national organizations interested in improving patient safety, decreasing costs of care, and minimizing risk.
Summary.
The rationale for the medical malpractice liability system is to compensate patients injured due to negligent care and deter providers from practicing negligently. Limited evidence is available regarding experience with medical malpractice in radiation oncology. In this paper, we review characteristics and national trends in radiation oncology malpractice claims and their associated costs, and compare radiation oncology to other specialties. This study provides evidence that can be used to improve patient safety, minimize risk and influence policymaking relevant to radiation oncology.
Acknowledgments
The authors thank Kwon Miller, Data Analyst, for assistance in obtaining data from the Physician Insurers Association of America.
Sources of support: This project was supported in part by funding from the Joint Center for Radiation Therapy Foundation (JHG; Dana-Farber Cancer Institute, Boston, MA), and by the National Institutes of Health, Grant TL1TR00098 (DM), KL2TR00099 (JHG), and UL1TR000100 (JHG).
Appendix A. Annual characteristics of radiation oncology closed claims, 1985–2012
| Close Year | Closed Claims* |
Paid Claims† |
% Paid of Closed Claims |
Total Indemnity Paid†† |
Average Indemnity Paid†† |
Total Expenses - All Closed Claims††‖ |
Average Expenses - All Closed Claims††‖ |
Total Expenses - Paid Claims††‖ |
Average Expenses - Paid Claims††‖ |
Total Expenses - No Indemnity††‖ |
Average Expenses - No Indemnity††‖ |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1985 | 103 | 30 | 29.1% | $4,216,912 | $140,564 | $942,406 | $9,150 | $334,182 | $11,139 | $608,224 | $8,332 |
| 1986 | 92 | 16 | 17.4% | $5,932,780 | $370,799 | $1,598,860 | $17,379 | $500,081 | $31,255 | $1,098,779 | $14,458 |
| 1987 | 132 | 11 | 8.3% | $5,697,868 | $517,988 | $1,261,349 | $9,556 | $334,407 | $30,401 | $926,942 | $7,661 |
| 1988 | 72 | 12 | 16.7% | $2,415,897 | $201,325 | $983,825 | $13,664 | $251,804 | $20,984 | $732,021 | $12,200 |
| 1989 | 56 | 6 | 10.7% | $476,890 | $79,482 | $715,685 | $12,780 | $193,241 | $32,207 | $522,444 | $10,449 |
| 1990 | 28 | 5 | 17.9% | $1,901,083 | $380,217 | $897,674 | $32,060 | $505,185 | $101,037 | $392,489 | $17,065 |
| 1991 | 21 | 1 | 4.8% | $927,300 | $927,300 | $462,443 | $22,021 | $42,703 | $42,703 | $419,740 | $20,987 |
| 1992 | 42 | 12 | 28.6% | $5,022,453 | $418,538 | $1,050,446 | $25,011 | $491,083 | $40,924 | $559,363 | $18,645 |
| 1993 | 61 | 13 | 21.3% | $3,224,980 | $248,075 | $1,864,954 | $30,573 | $452,226 | $34,787 | $1,412,727 | $29,432 |
| 1994 | 70 | 19 | 27.1% | $5,431,341 | $285,860 | $3,158,611 | $45,123 | $1,941,038 | $102,160 | $1,217,573 | $23,874 |
| 1995 | 50 | 9 | 18.0% | $4,011,456 | $445,717 | $856,659 | $17,133 | $332,584 | $36,954 | $524,074 | $12,782 |
| 1996 | 63 | 10 | 15.9% | $3,642,046 | $364,205 | $2,061,835 | $32,728 | $430,736 | $43,074 | $1,631,099 | $30,775 |
| 1997 | 100 | 18 | 18.0% | $11,007,063 | $611,504 | $2,919,917 | $29,199 | $803,115 | $44,618 | $2,116,802 | $25,815 |
| 1998 | 78 | 21 | 26.9% | $10,152,242 | $483,440 | $1,630,543 | $20,904 | $623,949 | $29,712 | $1,006,594 | $17,660 |
| 1999 | 88 | 23 | 26.1% | $7,395,081 | $321,525 | $3,772,188 | $42,866 | $2,074,997 | $90,217 | $1,697,192 | $26,111 |
| 2000 | 39 | 13 | 33.3% | $6,934,933 | $533,456 | $1,329,486 | $34,089 | $1,013,116 | $77,932 | $316,370 | $12,168 |
| 2001 | 39 | 12 | 30.8% | $6,372,511 | $531,043 | $1,361,719 | $34,916 | $863,144 | $71,929 | $498,575 | $18,466 |
| 2002 | 21 | 9 | 42.9% | $2,250,864 | $250,096 | $1,086,913 | $51,758 | $470,959 | $52,329 | $615,955 | $51,330 |
| 2003 | 44 | 7 | 15.9% | $2,061,267 | $294,467 | $758,090 | $17,229 | $274,817 | $39,260 | $483,273 | $13,061 |
| 2004 | 33 | 13 | 39.4% | $11,431,328 | $879,333 | $1,460,579 | $44,260 | $804,026 | $61,848 | $656,553 | $32,828 |
| 2005 | 34 | 13 | 38.2% | $5,576,519 | $428,963 | $1,240,191 | $36,476 | $588,580 | $45,275 | $651,611 | $31,029 |
| 2006 | 27 | 8 | 29.6% | $1,466,463 | $183,308 | $1,399,207 | $51,822 | $569,972 | $71,246 | $829,235 | $43,644 |
| 2007 | 40 | 14 | 35.0% | $6,625,672 | $473,262 | $2,282,798 | $57,070 | $1,493,022 | $106,644 | $789,776 | $30,376 |
| 2008 | 36 | 19 | 52.8% | $8,465,816 | $445,569 | $1,731,377 | $48,094 | $1,259,247 | $66,276 | $472,130 | $27,772 |
| 2009 | 26 | 10 | 38.5% | $2,482,618 | $248,262 | $2,291,271 | $88,126 | $1,303,909 | $130,391 | $987,362 | $61,710 |
| 2010 | 26 | 9 | 34.6% | $3,219,021 | $357,669 | $1,065,315 | $40,974 | $621,599 | $69,067 | $443,716 | $26,101 |
| 2011 | 18 | 5 | 27.8% | $689,175 | $137,835 | $1,018,205 | $56,567 | $193,370 | $38,674 | $824,834 | $63,449 |
| 2012 | 78 | 4 | 5.1% | $923,000 | $230,750 | $1,382,555 | $17,725 | $284,577 | $71,144 | $1,097,978 | $14,838 |
| Cumulative | 1,517 | 342 | 22.5% | $129,954,578 | $379,984 | $42,585,100 | $28,072 | $19,051,669 | $55,707 | $23,533,432 | $20,028 |
Closed claims are medical liability claims that have been resolved through settlement or verdict or withdrawn, dropped or dismissed without payment.
Paid Claims are medical liability claims that resulted in indemnity payment to the plaintiff as a result of settlement or court adjudication.
Adjusted for inflation, 2012 index year26.
Expenses are litigation expenses related to the defense of a liability claim, including expenses paid in the process of administering or adjudicating a claim.
Appendix B. Claims by Associated Personnel, 2003–2012
| 2003–2012 | |||||
|---|---|---|---|---|---|
| Associated Personnel* | Closed Claims† |
Paid Claims†† |
% Paid of Closed Claims |
Total Indemnity‖ |
Average Indemnity‖ |
| Other Physician | 117 | 11 | 9.4% | $4,744,999 | $431,364 |
| Radiologist | 20 | 3 | 15.0% | $1,607,500 | $535,833 |
| Other Person or Personnel | 3 | 0 | 0.0% | $0 | $0 |
| Technician | 7 | 3 | 42.9% | $355,000 | $118,333 |
| Consultant | 3 | 1 | 33.3% | $360,000 | $360,000 |
| Emergency Medicine Physician | 3 | 1 | 33.3% | $360,000 | $360,000 |
| Nurse | 2 | 0 | 0.0% | $0 | $0 |
| Pathologist | 2 | 0 | 0.0% | $0 | $0 |
| Other Therapist | 2 | 0 | 0.0% | $0 | $0 |
| Physician's Assistant | 2 | 0 | 0.0% | $0 | $0 |
| Other Office Personnel | 1 | 0 | 0.0% | $0 | $0 |
| Physical Therapist | 1 | 1 | 100.0% | $38,000 | $38,000 |
| Nurse Anesthetist | 1 | 0 | 0.0% | $0 | $0 |
| Nurse Practitioner | 1 | 1 | 100.0% | $80,000 | $80,000 |
| Manufacturer of Drug or Equipment | 1 | 0 | 0.0% | $0 | $0 |
| Associated Personnel Total: | 166 | 21 | 12.7% | $7,545,499 | $359,309 |
Any associated professional that was named in the claim. Up to three associated personnel can be reported for each record.
Closed claims are medical liability claims that have been resolved through settlement or verdict or withdrawn, dropped or dismissed without payment.
Paid Claims are medical liability claims that resulted in indemnity payment to the plaintiff as a result of settlement or court adjudication.
Adjusted for inflation, 2012 index year26.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest: none
Disclaimers: The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the Dana-Farber Cancer Institute.
References
- 1.Kessler DP. Evaluating the medical malpractice system and options for reform. J Econ Perspect. 2011;25(2):93–110. doi: 10.1257/jep.25.2.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kachalia A, Gandhi TK, Puopolo AL, et al. Missed and delayed diagnoses in the emergency department: a study of closed malpractice claims from 4 liability insurers. Ann Emerg Med. 2007;49(2):196–205. doi: 10.1016/j.annemergmed.2006.06.035. [DOI] [PubMed] [Google Scholar]
- 3.Studdert DM, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. New Engl J Med. 2006;354(19):2024–2033. doi: 10.1056/NEJMsa054479. [DOI] [PubMed] [Google Scholar]
- 4.Carrier ER, Reschovsky JD, Katz DA, Mello MM. High physician concern about malpractice risk predicts more aggressive diagnostic testing in office-based practice. Health Aff (Millwood) 2013;32(8):1383–1391. doi: 10.1377/hlthaff.2013.0233. [DOI] [PubMed] [Google Scholar]
- 5.Jena AB, Seabury S, Lakdawalla D, Chandra A. Malpractice risk according to physician specialty. New Engl J Med. 2011;365(7):629–636. doi: 10.1056/NEJMsa1012370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bogdanich W. At hearing on radiation, calls for better oversight. The New York Times. 2010:12. [Google Scholar]
- 7.Bogdanich W. At VA hospital, a rogue cancer unit. The New York Times. 2009:20. [Google Scholar]
- 8.Bogdanich W. Radiation offers new cures, and ways to do harm. The New York Times. 2010:23. [Google Scholar]
- 9.Bogdanich W. As technology surges, radiation safeguards lag. The New York Times. 2010:15. [Google Scholar]
- 10.Elliott K, Wallner K, Merrick G, Herstein P. Medical malpractice of prostate brachytherapy. Brachytherapy. 2004;3(4):231–236. doi: 10.1016/j.brachy.2004.07.003. [DOI] [PubMed] [Google Scholar]
- 11.Halperin EC. Insurance and malpractice disputes in radiation oncology. Am J Clin Oncol. 2009;32(4):432–435. doi: 10.1097/COC.0b013e318187dd82. [DOI] [PubMed] [Google Scholar]
- 12.Epstein JB, Kish RV, Hallajian L, Sciubba J. Head and neck, oral, and oropharyngeal cancer: a review of medicolegal cases. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014 doi: 10.1016/j.oooo.2014.10.002. [DOI] [PubMed] [Google Scholar]
- 13.Lydiatt DD. Medical malpractice and cancer of the skin. Am J Surg. 2004;187(6):688–694. doi: 10.1016/j.amjsurg.2003.10.018. [DOI] [PubMed] [Google Scholar]
- 14.Lydiatt DD. Medical malpractice and the thyroid gland. Head Neck. 2003;25(6):429–431. doi: 10.1002/hed.10254. [DOI] [PubMed] [Google Scholar]
- 15.Lydiatt DD. Medical malpractice and cancer of the larynx. Laryngoscope. 2002;112(3):445–448. doi: 10.1097/00005537-200203000-00007. [DOI] [PubMed] [Google Scholar]
- 16.McLean TR. Why do physicians who treat lung cancer get sued? Chest. 2004;126(5):1672–1679. doi: 10.1378/chest.126.5.1672. [DOI] [PubMed] [Google Scholar]
- 17.Mesko NW, Mesko JL, Gaffney LM, Halpern JL, Schwartz HS, Holt GE. Medical malpractice and sarcoma care—A thirty-three year review of case resolutions, inciting factors, and at risk physician specialties surrounding a rare diagnosis. J Surg Oncol. 2014;110(8):919–929. doi: 10.1002/jso.23770. [DOI] [PubMed] [Google Scholar]
- 18.Guardado JR. Professional Liability Insurance Indemnity Payments, Expenses, Claim Disposition, and Policy Limits 2003–2012. American Medical Association. 2013 [Google Scholar]
- 19.Physician Insurers Association of America. [Accessed June 30, 2014];About PIAA. 2014 https://www.piaa.us/wcm/About_PIAA/wcm/_About/Todays_PIAA.aspx?hkey=7b39bd4c-64db-4fdb-ac69-501bcc453bfc.
- 20.Cornell University Law School, Legal Information Institute. [Accessed April 17, 2015];Wex Legal Encyclopedia. 2015 https://www.law.cornell.edu/wex/indemnify.
- 21.Smarr L. A comparative assessment of the PIAA Data Sharing Project and the National Practitioner Databank: Policy, purpose, and application. Law and Contemp Probs. 1997;60(1):59–79. [Google Scholar]
- 22.Physician Characteristics and Distribution in the United States. Survey & Data Resources. American Medical Association; 1986–2013. [Google Scholar]
- 23.Wooldridge J. Introductory econometrics: A modern approach. 5th Edition ed. Mason, OH: South-Western; 2012. [Google Scholar]
- 24.Yaffee RA, McGee M. Introduction to time series analysis and forecasting : with applications in SAS and SPSS. San Diego: Academic Press; 2000. [Google Scholar]
- 25.Clegg LX, Hankey BF, Tiwari R, Feuer EJ, Edwards BK. Estimating average annual per cent change in trend analysis. Stat Med. 2009;28(29):3670–3682. doi: 10.1002/sim.3733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.US Department of Labor, Bureau of Labor Statistics. [Accessed June 30, 2014];Consumer Price Index-All Urban Consumers for All Items. 2012 http://www.bls.gov/cpi.
- 27.Lewis RS, Sunshine JH. Radiation oncologists in the United States. Int J Radiat Oncol Biol Phys. 2007;69(2):518–527. doi: 10.1016/j.ijrobp.2007.02.053. [DOI] [PubMed] [Google Scholar]
- 28.Cypel Y, Sunshine JH, Schepps B. Radiation oncologists in 2000: demographic, professional, and practice characteristics. Int J Radiat Oncol Biol Phys. 2002;53(3):720–728. doi: 10.1016/s0360-3016(02)02758-x. [DOI] [PubMed] [Google Scholar]
- 29.Centers for Medicare and Medicaid Services. [Accessed April 15, 2015];National Plan and Provider Enumeration System (NPPES) 2013 Apr; 2013; www.cms.gov/Regulations-and-Guidance/HIPAA-Administrative-Simplification/NationalProvIdentStand/Downloads/Data_Dissemination_File-Readme.pdf.
- 30.American College of Radiology (ACR) Radiation Oncology practice accreditation program requirements. 2015. [Accessed April 1, 2015]. [Google Scholar]
- 31.American Society of Clinical Oncology. [Accessed June 30, 2014];Key trends in tracking supply of and demand for oncologists. 2013 https://www.asco.org/sites/default/files/workforce_information_system_12.17.12.pdf.
- 32.Paik MBB, Hyman DA. The receding tide of medical malpractice litigation: Part 1 -- national trends. J Emperic Legal Stud. 2013;10(4):612–638. [Google Scholar]
- 33.Mello MM, Chandra A, Gawande AA, Studdert DM. National costs of the medical liability system. Health Aff (Millwood) 2010;29(9):1569–1577. doi: 10.1377/hlthaff.2009.0807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mello MM, Studdert DM, Kachalia A. The medical liability climate and prospects for reform. JAMA. 2014;312(20):2146–2155. doi: 10.1001/jama.2014.10705. [DOI] [PubMed] [Google Scholar]
- 35.Mello MM. Understanding medical malpractice insurance: A primer. The Robert Wood Johnson Foundation. Research Synthesis Report No. 8. 2006 Jan; [PubMed] [Google Scholar]
- 36.Revisions to payment policies under the physicians fee schedule and Part B for CY 2010. Centers for Medicare and Medicaid Services; CMS-1413-FC2009. [Google Scholar]
- 37.Medical Malpractice: Implications of Rising Premiums on Access to Health Care. Washington (DC): United States, General Accounting Office (GAO); 2003. [Google Scholar]