Abstract
Introduction
Kidney diseases are a growing worldwide problem and one of the major public health threats. We analyzed the spectrum of kidney diseases seen over a five-year period in the nephrology in-patient unit of the Yaounde general hospital.
Methods
This was a retrospective analysis of 225 medical records of patients admitted from January 2005 to December 2009 in the unit with a discharge diagnosis of kidney and urinary tract diseases. The first hospitalization was considered for patients admitted several times for the same disease. Socio-demographic and clinical patient data were recorded.
Results
The patients mean age was 44.8±16 years with 135 (60%) males and 211 (93.8%) emergency admissions. All 139 (61.8%) patients with chronic kidney disease (CKD) had chronic renal failure. Acute kidney injury (AKI) (28%), nephrotic syndrome (7.6%), renal colic (1.3%) and acute pyelonephritis (1.3%) were other patterns observed. Chronic glomerulonephritis (25.9%), hypertension (22.3%) and diabetes (20.1%) were the main etiological factors of CKD. All AKI patients were in stage RIFLE-F. AKI was secondary to parenchymal (58.7%), functional (25.4%) and obstructive (15.9%) etiologies. Black water fever (36.4%), sepsis (22.7%), drugs (18.2%), eclampsia (13.6%) and herbal concoctions (9.1%) were the etiologies of acute tubular necrosis while enterocolitis (56.2%), heart failure (31.3%) and digestive hemorrhage (12.5%) were the etiologies of functional AKI.
Conclusion
The clinical pattern of renal diseases is dominated by advanced CKD and AKI secondary to preventable causes. This study suggests a need for an array of actions including sensitization, continuous medical education and strengthening of the health system.
Keywords: Kidney diseases, clinical pattern, Cameroon, Sub-Saharan Africa
Introduction
Kidney diseases are a growing worldwide problem and constitute one of the major public health threats [1]. Whether acute or chronic, the progressive increase in prevalence is related to modifications in life style, an increase in life span, medical progress and nephrotoxin abuse [2]. Chronic kidney disease (CKD) is the leading kidney disease which causes end-stage renal disease (ESRD) and cardiovascular deaths. In developed countries, CKD is related to the high prevalence of diabetes and hypertension [3] while renal hypoperfusion, sepsis and nephrotoxin constitute the main etiologies of acute kidney injury (AKI) [4–7]. However, sub-Saharan African (SSA) countries face the dual burden of non-communicable and transmissible diseases which may predispose to an increase in prevalence and a modified spectrum of kidney diseases [8]. Despite epidemiological transition in this setting, CKD remains the leading kidney disease, affecting predominantly young male adults, in their economically productive years, with chronic glomerulonephritis, hypertension and diabetes as the main etiological factors [9–16] while AKI is mainly secondary to diarrhea, obstetric complications, toxins and infections [17, 18]. Few countries in SSA have nephrologists and where available, nephrology units are under-equipped and understaffed; hence, patients with kidney diseases are generally managed in general internal medicine wards [11]. In Cameroon at the time of conducting this study, only five nephrologists, working in the two main cities of Douala and Yaounde provided care for an estimated population of 20 million inhabitants [19]. Consequently, both community and hospital-based data on the types of kidney disease in the country are lacking. This study was designed to analyze the spectrum of kidney diseases seen over a five-year period in the main nephrology in-patient unit of the country in order to assess the disease burden and to design preventive measures.
Methods
Study setting
This was a retrospective analysis of medical records of patients admitted from January 2005 to December 2009 in the nephrology-cardiology-psychiatry unit of the Yaoundé General Hospital (YGH); the main tertiary hospital in the Cameroon capital city. This unit of 25 beds is part of the internal medicine department and constitutes the main national referral nephrology unit. The staff comprised three nephrologists taking care of patients mainly from the center region and neighborhood but also from other parts of the country. This study received administrative authorization from the YGH and was approved by the Ethic Committee of the Faculty of Medicine and Biomedical Sciences (FMSB) of Yaoundé 1 University, Cameroon.
Data collection
During the study period, we used the in-patient register of the unit to identify all patients with a discharge diagnosis of diseases of the kidney and urinary tract. This list was then used to retrieve the individual medical records from the hospital archives department. We considered only the first hospitalization for patients admitted several times for the same disease. For those with several diagnoses, each diagnosis was counted separately. We excluded files with missing data and patients hospitalized for hemodialysis-related complications. Patient information recorded included age, gender, type of admission (emergency, elective), kidney and urinary tract disorder, comorbidities, type and etiological factors of AKI, as well as stage and etiological factors of CKD.
Definitions
Acute kidney disease (AKD) referred to any kidney disease of less than three months duration including AKI. AKI was defined as sudden loss of kidney function with recovering within three months. AKI was then classified into functional, parenchymal and obstructive. The RIFLE classification was used to stage AKI severity [20]. CKD referred to any kidney disease of more than three months duration including chronic renal failure which corresponds to persistent glomerular filtration rate (GFR) [21]. Nephrotic syndrome was defined by the association of proteinuria >3.5g/24 hours, hypoalbuminemia < 3.0g/dl and edema. Chronic glomerulonephritis referred to a chronic renal failure in patient of younger age (< 45 years) with hypertension, proteinuria, haematuria and small size kidney on ultrasonography. Hypertension was defined as a systolic blood pressure (SBP) ≥140 mmHg and/or a diastolic blood pressure (DBP) ≥90 mmHg or use of blood pressure lowering medications. Diabetes mellitus was defined as fasting capillary glucose? 126 mg/dl or use of glucose control agents. All diagnoses were made by a nephrologist.
Statistical analysis
Statistical analysis were performed using the SPSS® 9 software for Windows (SPSS, Chicago, IL, USA). We have reported results as mean (standard deviation) and count (percentages).
Results
General profile of the study population
During the study period, 358 patients were hospitalized for kidney and urinary tract disorder among which 256 (71.5%) fulfilled the study criteria. Only 225 (87.9%) files were available for analysis divided into 139 (61.8%) CKD and 86 (38.2%) AKD. As presented in Table 1, the patients’ age ranged from 13 to 84 years with a mean of 44.8±16 years, 135 (60%) were males and 211 (93.8%) were emergency admissions. Hypertension was the main comorbidity recorded in 142 (63.1%) patients whereas 26 (11.6%) patients had HIV infection.
Table 1.
Characteristics overall and by diagnostic categories
| Characteristics | Overall n (%) | CRF n (%) | AKI n (%) | NS n (%) | RC n (%) | AP n (%) |
|---|---|---|---|---|---|---|
| n | 225 (100) | 139 (61.8) | 63 (28.0) | 17 (7.6) | 3 (1.3) | 3 (1.3) |
| Male sex | 135 (60.0) | 85 (61.2) | 37 (58.7) | 10 (58.8) | 2 (66.7) | 1 (33.3) |
| Emergency admission | 211 (93.8) | 139 (100) | 63 (100) | 3 (17.6) | 3 (100) | 3 (100) |
| Diabetes | 56 (24.9) | 49 (32.2) | 5 (7.9) | 1 (5.9) | 0 (0.0) | 1 (33.3) |
| Hypertension | 142 (63.1) | 113 (81.3) | 24 (38.1) | 2 (11.8) | 2 (66.7) | 1 (33.3) |
| Smoking | 36 (16.0) | 21 (15.1) | 14 (22.2) | 1 (5.9) | 0 (0.0) | 0 (0.0) |
| HIV infection | 26 (11.6) | 14 (10.1) | 10 (15.9) | 1 (5.9) | 0 (0.0) | 1 (33.3) |
CRF – Chronic renal failure; AKI – Acute kidney injury; NS – Nephrotic syndrome; RC – Renal colic; AP – Acute pyelonephritis
Stage and etiological factors of CKD
All CKD patients had chronic renal failure. According to KDOQI classification, 4 (2.9%), 19 (13.7%) and 116 (83.4%) patients were respectively classified in stage 3, 4 and 5. Chronic glomerulonephritis (25.9%), hypertension (22.3%) and diabetes (20.1%) were the main etiological factors of CKD as presented in Figure 1.
Figure 1.
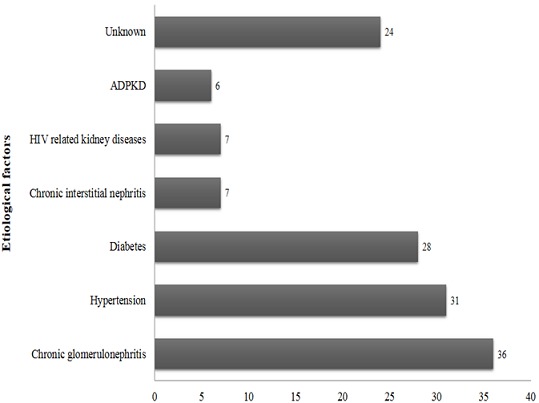
Type and frequency of etiological factors of chronic renal failure
Type and etiological factors of AKI
All AKI patients were in RIFLE-F; with the suspected mechanism of injury being parenchymal, functional and obstructive in 37 (58.7%), 16 (25.4%) and 10 (15.9%) patients respectively. As presented in Figure 2, acute tubular necrosis (ATN) was the main suspected lesion in parenchymal AKI. Black water fever (n=8, 36.4%), sepsis (n=5, 22.7%), drugs (n=4, 18.2%), eclampsia (n=3, 13.6%) and herbal concoctions (n=2, 9.1%) were the etiologies of ATN. Acute interstitial nephritis was drug-induced (n=4, 57.1%), infectious (n=2, 28.6%) and due to lymphoma (n=1, 14.3%). Malignant nephroangiosclerosis (N=2, 50%) and ANCA-vasculitis (n=2, 50%) were the causes of vascular AKI whereas acute glomerulonephritis was exclusively post-infectious. Enterocolitis (n=9, 56.2%), heart failure (n=5, 31.3%) and digestive hemorrhage (n=2, 12.5%) were the etiologies of functional AKI meanwhile obstructive AKI was secondary to prostatic hypertrophy (n=6, 60%), nephrolithiasis (n=2, 20%) and cervical cancer (n=2, 20%).
Figure 2.
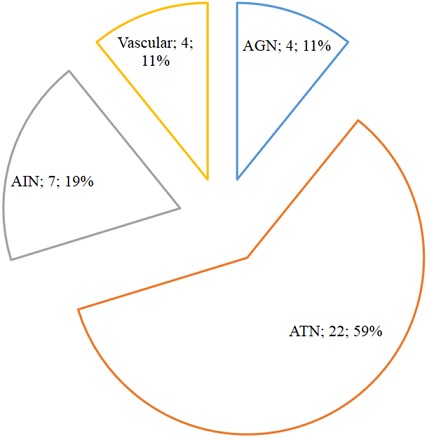
Etiological factors of acute kidney injury
Etiology of nephrotic syndrome
Among 17 patients with kidney biopsy for nephrotic syndrome, 10 (58.8%) cases were identified as primary including focal and segmental glomerulosclerosis (n=8, 80%) and minimal change disease (n=2, 20%) lesions on kidney biopsy. The remaining cases were identified secondary to systemic lupus erythematosus (n=2, 28.6%), HIV-associated nephropathy (n=2, 28.6%), hepatitis B virus (n=1, 14.3%), filariasis (n=1, 14.3%) and non-steroidal anti-inflammatory drugs (n=1, 14.3%).
Discussion
In a context marked by a scarcity of kidney specialists and units dedicated to renal care, we found that the clinical spectrum of diseases of the kidney and urinary tract observed in an in-patient medical ward were diverse and included CKD, AKI, nephrotic syndrome, renal colic and acute pyelonephritis. They affect mostly young males who frequently are admitted as emergency. This study revealed that kidney diseases dominated by CRF affect young individuals in their economically productive years and who are usually diagnosed late already in end stage as previously reported in similar settings; thus contrasting with the advanced age of patients in developed countries [3, 9–16]. The socio-cultural and economic factors favoring males in this setting could explain this gender bias in addition to being a risk factor for kidney disease [10–13, 16]. Chronic kidney disease was the main presentation accounting for nearly two-thirds of renal admissions with etiological factors similar to earlier reports [9, 10, 12–16]. The high prevalence of CKD reported in this setting could be related to the epidemiological transition with the increased prevalence of diabetes and hypertension coupled with unresolved transmissible diseases dominated by HIV/AIDS [8, 10]. In the present study, over half of the patients with HIV infection had CRF. We had previously reported a significant decrease in renal function as well as a high frequency of urine abnormalities in treatment-naïve HIV infected patients in this setting [22]. More than 8 in 10 patients with CKD were in ESRD, most often in a state of uremia requiring emergency renal replacement therapy; which probably reflects the late referral previously reported in this SSA setting [10, 16]. This could be explained by the under-resourced health systems and highlight the need for community-based awareness campaigns and continuous medical education for care-providers on the prevention and control of risk factors for CKD.
Acute kidney injury was the second most frequent presentation of kidney disease in our setting with unsurprisingly all patients in RIFLE-F. AKI was mainly from renal parenchymal disease dominated by acute tubular necrosis with etiologies similar to previous reports in developing countries [17, 18]. The high frequency of acute tubular necrosis likely reflects the longstanding evolution and inadequate management of functional AKI in other health facilities before transfer to our unit; the unique specialized unit with renal replacement therapy facilities in the city during the study period. As reported in other SSA settings, we found that malaria and its related disorders, pregnancy related complications and nephrotoxic drugs were the main etiologies of AKI implying more sensitization of populations on AKI prevention and health care-providers on early diagnostic and referral for better management. However, this etiological profile of AKI is quite different from developed countries where it usually occurs following cardiovascular procedures and sepsis in elderly persons [4–7]. The small number of patients with the nephrotic syndrome in this study reflects the local practice whereby only nephrotic patients with life-threatening complications are admitted to hospital. However, apart from diabetes, the potential secondary causes of nephrotic syndrome observed were dominated by endemic infections similar to those reported in SSA [23]. The absence of hypertension, as an entity in the disease spectrum observed in this study, results from the fact that in Cameroon, hypertension is managed by cardiologists except when it occurs in association with renal diseases. This study has some limitations. We excluded some patients due to incomplete files pointing out the weakness of archives service in our setting. The etiological diagnosis of renal disorders was mainly clinical due to the unavailability and unaffordability of renal histology as well as the late presentation of patients with CKD which reduces the sensitivity and specificity of renal histology. Moreover, most patients are self-funded, such that only patients who can pay for their care are admitted into hospital thus constituting a selection bias. Nevertheless, our study provides an overview of the spectrum of kidney diseases in our setting since it was conducted in the main national referral nephrology unit.
Conclusion
This study revealed that patients admitted in a specialized nephrology unit for kidney and urinary tract diseases in Cameroon are mainly young adults in their economically productive years. The clinical pattern of disease is dominated by advanced CKD and AKI secondary to preventable causes. This study suggests a need for an array of actions including sensitization, continuous medical education and strengthening of the health system to improve the management of patients with kidney disease, and the implementation of a national program to prevent and control risk factors for kidney diseases.
Competing interests
The authors declare no competing interests.
Authors’ contributions
GA and FFK conceived the study, supervised data collection, analyzed data and drafted the manuscript; FEE performed data collection and critically revised the manuscript; APM, HF and MPH critically revised the manuscript. All authors read and approved the final manuscript.
References
- 1.Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, Abraham J, Adair T, Aggarwal R, Ahn SY, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Kidney Day. World kidney day: FAQS; Available from: http://www.worldkidneyday.org/faqs (accessed date: 15th August 2014) [Google Scholar]
- 3.USRDS. the United States Renal Data System. Am J Kidney Dis. 2003;42(6 Suppl 5):1–230. [PubMed] [Google Scholar]
- 4.Abuelo JG. Normotensive ischemic acute renal failure. N Engl J Med. 2007;357(8):797–805. doi: 10.1056/NEJMra064398. [DOI] [PubMed] [Google Scholar]
- 5.Thadhani R, Pascual M, Bonventre JV. Acute renal failure. N Engl J Med. 1996;334(22):1448–1460. doi: 10.1056/NEJM199605303342207. [DOI] [PubMed] [Google Scholar]
- 6.Nash K, Hafeez A, Hou S. Hospital-acquired renal insufficiency. Am J Kidney Dis. 2002;39(5):930–936. doi: 10.1053/ajkd.2002.32766. [DOI] [PubMed] [Google Scholar]
- 7.Liano F, Pascual J. Epidemiology of acute renal failure: a prospective, multicenter, community-based study: Madrid Acute Renal Failure Study Group. Kidney Int. 1996;50(3):811–818. doi: 10.1038/ki.1996.380. [DOI] [PubMed] [Google Scholar]
- 8.Marshall SJ. Developing countries face double burden of disease. Bull World Health Organ. 2004;82(7):556. [PMC free article] [PubMed] [Google Scholar]
- 9.Diouf B, Ka EF, Niang A, Diouf ML, Mbengue M, Diop TM. Etiologies of chronic renal insufficiency in a adult internal medicine service in Dakar. Dakar Med. 2000;45(1):62–65. [PubMed] [Google Scholar]
- 10.Arogundade FA, Sanusi AA, Hassan MO, Akinsola A. The pattern, clinical characteristics and outcome of ESRD in Ile-Ife, Nigeria: is there a change in trend? Afr Health Sci. 2011;11(4):594–601. [PMC free article] [PubMed] [Google Scholar]
- 11.Bamgboye EL. End-stage renal disease in sub-Saharan Africa. Ethn Dis. 2006;16(2 Suppl 2):S2–5-9. [PubMed] [Google Scholar]
- 12.van Rensburg BW, van Staden AM, Rossouw GJ, Joubert G. The profile of adult nephrology patients admitted to the Renal Unit of the Universitas Tertiary Hospital in Bloemfontein, South Africa from 1997 to 2006. Nephrol Dial Transplant. 2010;25(3):820–824. doi: 10.1093/ndt/gfp535. [DOI] [PubMed] [Google Scholar]
- 13.Diallo AD, Niamkey E, Beda Yao B. Chronic renal insufficiency in Cote d'Ivoire: study of 800 hospital cases. Bull Soc Pathol Exot. 1997;90(5):346–348. [PubMed] [Google Scholar]
- 14.Bah AO, Kaba ML, Diallo MB, Kake A, Balde MC, Keita K, Dore H, Toure YI. Renal diseases--morbidity and mortality in Nephrology Service, National Hospital Donka. Mali Med. 2006;21(4):42–46. [PubMed] [Google Scholar]
- 15.Alebiosu CO, Ayodele OO, Abbas A, Olutoyin AI. Chronic renal failure at the Olabisi Onabanjo University Teaching Hospital, Sagamu, Nigeria. Afr Health Sci. 2006;6(3):132–138. doi: 10.5555/afhs.2006.6.3.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Halle MP, Kengne AP, Ashuntantang G. Referral of patients with kidney impairment for specialist care in a developing country of sub-Saharan Africa. Ren Fail. 2009;31(5):341–348. doi: 10.1080/08860220902882014. [DOI] [PubMed] [Google Scholar]
- 17.El Hadji FK, Diouf B, Niang A, Ndiaye MF, Diop TM. Acute renal failure in adults in dakar. Saudi J Kidney Dis Transpl. 1999;10(4):513–514. [PubMed] [Google Scholar]
- 18.Anandh U, Renuka S, Somiah S, Vincent L. Acute renal failure in the tropics: emerging trends from a tertiary care hospital in South India. Clin Nephrol. 2003;59(5):341–344. doi: 10.5414/cnp59341. [DOI] [PubMed] [Google Scholar]
- 19.Kaze FF, Kengne AP, Choukem SP, Dzudie A, Halle MP, Dehayem MY, Ashuntantang G. Dialysis in Cameroon. Am J Kidney Dis. 2008;51(6):1072–1074. doi: 10.1053/j.ajkd.2008.02.366. [DOI] [PubMed] [Google Scholar]
- 20.Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P. Acute renal failure - definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004;8(4):R204–212. doi: 10.1186/cc2872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification, kidney Disease Outcome Quality Initiative. Am J Kidney Dis. 2002;39(S):1–246. [PubMed] [Google Scholar]
- 22.Folefack Kaze F, Kengne AP, Pefura Yone EW, NdamFemben NS, Ashuntantang G. Renal function, urinalysis abnormalities and correlates among HIV-infected Cameroonians naive to antiretroviral therapy. Saudi J Kidney Dis Transpl. 2013;24(6):1291–1297. doi: 10.4103/1319-2442.121280. [DOI] [PubMed] [Google Scholar]
- 23.Diallo AD, Nochy D, Niamkey E, Yao Beda B. Etiologic aspects of nephrotic syndrome in Black African adults in a hospital setting in Abidjan. Bull Soc Pathol Exot. 1997;90(5):342–345. [PubMed] [Google Scholar]


