Abstract
Background. Sciatica is one of the most frequently reported complaints; it affects quality of life and reduces social and economic efficacy. Clinical studies on the efficacy of acupuncture therapy in sciatica are increasing, while systematic reviews assessing the efficacy of acupuncture therapy are still lacking. Objective. This study aims to assess the effectiveness of acupuncture therapy for sciatica. Methods. Comprehensive searches of 8 databases were conducted up until April 2015. Outcomes included effectiveness (proportion of patients who improved totally or partly in clinical symptoms), pain intensity, and pain threshold. Effect sizes were presented as risk ratio (RR) and mean difference (MD). Pooled effect sizes were calculated by fixed effects or random effects model. Results. A total of 12 studies (involving 1842 participants) were included. Results showed that acupuncture was more effective than conventional Western medicine (CWM) in outcomes effectiveness (RR 1.21, 95% CI: 1.16–1.25), pain intensity (MD −1.25, 95% CI: −1.63 to −0.86), and pain threshold (MD: 1.08, 95% CI: 0.98–1.17). Subgroup and sensitivity analysis found that the results did not change in different treatment method and drug categories substantially. The reported adverse effects were acceptable. Conclusions. Acupuncture may be effective in treating the pain associated with sciatica.
1. Introduction
Sciatica is a syndrome rather than a specific diagnosis [1]. In 90% of cases, sciatica is caused by a herniated disc with nerve-root compression [1]. The prevalence ranges from 1.2% to 43% [2]. A number of risk factors are thought to be associated with first-time incidence of sciatica and influence the development of sciatica; these include smoking, obesity, occupational factors, health status, age, gender, and social class [3, 4]. According to traditional Chinese medicine (TCM), sciatica belongs to the gallbladder meridian of the foot-Shaoyang (GB) and the bladder meridian of the foot-Taiyang (BL), and the Yanglingquan (GB 34) and Huantiao (GB 30) are two key “acupuncture points” (acupoints) for treating sciatica [5].
Acupuncture is widely used in clinical practice in China and in many Western countries [6]; in China, it can be traced back at least 3000 years as part of the healing system based on the principles of TCM. Traditional acupuncturists understand health in terms of a vital force or energy called “qi” which circulates between the organs along channels called meridians [7]. Since sciatica is a channel disorder, acupuncture of points removing channel obstruction and promoting qi and blood circulation is indicated in its treatment [8]. Acupuncture points can be stimulated for about 30 minutes by surface pressure, insertion of a needle with or without manipulation, heating of acupuncture needles through radiant heat or moxibustion, and electrical or laser stimulation [9].
Since the early 1990s, original studies [10–12] have reported the efficacy of acupuncture for the treatment of sciatica. However, the results had been controversial. It is relevant to query whether the effectiveness of acupuncture is evident and knowledge of effective interventions is critical in order to reduce the health and safety risks [13]. Up to now, there is only a systematic review protocol [14] about acupuncture for treating sciatica and no published meta-analysis of the effectiveness of acupuncture compared with medication for sciatica; we carried out a comprehensive and quantitative evaluation analysis to assess its efficacy and safety in the clinical treatment of this condition.
2. Materials and Methods
2.1. Database and Search Strategy
Three Chinese language databases (China National Knowledge Infrastructure (CNKI), Chinese Biomedical Literature Database (CBM), and Wanfang Data) and five English language databases (Cochrane Library, PubMed, Web of Science, Science Direct, and FMRS (Foreign Medical Literature Retrial Service)) were extensively searched until April 30, 2015. Neither the publication status of the search trials nor the basic standard of selecting points for needle insertion was restricted. The search strategy includes the following group terms: English (“acupuncture” OR “electroacupuncture” OR “needle warming therapy” OR “needling methods” OR “fire-needle therapy” OR “acupuncture therapy” OR “acupuncture points” OR “acupuncture analgesia”) AND (“sciatica” OR “sciatic pain” OR “neuralgias, sciatic” OR “sciatic neuralgias” OR “sciatica, bilateral” OR “bilateral sciatica” OR “bilateral sciaticas” OR “neuralgia, sciatic” OR “sciatic neuropathy” OR “sciatic nerve diseases”); Chinese (“zhen jiu” OR “wen zhen” OR “huo zhen liao fa” OR “zhen ci liao fa” OR “zhen jiu zhi liao” OR “zhen jiu xue wei” OR “zhen ci zhen tong” OR “dian zhen”) AND (“zuo gu shen jing tong” OR “zuo gu shen jing bing” OR “zuo gu shen jing yan” OR “zuo gu shen jing ji bing”).
2.2. Inclusion and Exclusion Criteria
Studies that met the following criteria were included in the review: (1) studies published in English or Chinese language; (2) randomized or quasi-randomized clinical trials; (3) participating patients that must have been diagnosed with sciatica or presented with any or all of the following symptoms: radiating pain in the sciatic nerve distribution area, tenderness at the nerve stem, positive Lasegue's sign, Kernig's sign, and Bonnet's sign; (4) any of the manual, warm, electric, or laser types of acupuncture that were used; (5) considering the following comparisons: acupuncture versus conventional Western medicine (CWM); CWM are conservative treatments of Western medicine, including oral drugs (e.g., Prednisone, Ibuprofen, and Nimesulide), external drugs (e.g., Diclofenac Diethylamine gel), and injection (e.g., anisodamine); (6) any of the following outcome measures that were eligible: effectiveness, pain intensity, and pain threshold.
Studies that met the following criteria were excluded: (1) randomized crossover trials, case reports, case series, reviews, qualitative studies, or animal experiments; (2) participants with back pain or low back pain but no symptoms of sciatica; (3) interventions that included a combination of more than one treatment strategy (or mixed treatments); (4) studies comparing interventions grouped under the same treatment strategy (e.g., a comparison between different forms or different acupoints of acupuncture).
2.3. Definitions
The primary outcome analysis for this meta-analysis was effectiveness (the proportion of patients who improved totally or partly in clinical symptoms). The effectiveness was presented by using the following formula: rate (effectiveness) = (N1 + N2 + N3)/N, where N1, N2, and N3 are the number of patients cured, markedly improved, and improved and N is the sample size. Criteria for improvement after treatment are the following: cured: all the symptoms and physical signs referred to above disappeared after the treatment with no relapse found in half a year and the patients could resume work; markedly improved: all the symptoms and physical signs basically disappeared but sometimes might relapse or even be more serious and the patients were able to do light work; improved: the symptoms were relieved with improved limb functions, but the pain always recurred.
Pain intensity and pain threshold were considered as the secondary outcomes. Pain intensity, is got by using a visual analogue scale (VAS) to measure pain on a continuous scale with data converted to a scale of 0–100 mm (0 means no pain, 100 means severe pain, and middle section shows different levels of pain). And the VAS is a common means of measuring individuals' rating of their own health [23]. Pain threshold, a threshold value, is got by using a pain measurement instrument to measure potassium ion. The big difference between the two outcomes is that values of the former are subjective (self-assessment by participants), while the latter ones are objective (tested by detector).
2.4. Data Extraction
Two reviewers (MJ and YS) independently screened the title and abstract of each searched article for eligibility and relevance. Potentially relevant papers were retrieved for further assessment according to the inclusion and exclusion criteria. One reviewer (MJ) extracted the data and another (YS) checked it, and any discrepancy was resolved by discussion. A standardized form was used for data input, consisting of contents such as general information (first author, publication year), patient characteristics, diagnostic criteria, study design, treatment protocol, outcome measurements (effectiveness, pain intensity, and pain threshold), withdrawal, and adverse events. The aforementioned data of N1, N2, N3, and N of effectiveness were also extracted.
The extraction of details of acupuncture treatment and control interventions of studies was on the basis of STRICTA (Standards for Reporting Interventions in Clinical Trials of Acupuncture) reporting guidelines [24] which could improve the completeness and transparency of reporting of interventions in controlled trials of acupuncture. A checklist included acupuncture rationale, details of needling (points used, depth of insertion, response sought, needle stimulation, needle type, and retention time), treatment regimen (number of treatment sessions, frequency), and control interventions.
2.5. Quality Assessment
We analyzed the studies using the Cochrane Handbook, Version 5.1.0. [25]. Quality of the included trials was assessed according to seven domains: random sequence generation (selection bias), allocation concealment (selection bias), binding of participants and personnel (performance bias), binding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias), and other potential sources of bias. Each domain was classified as “yes” (low risk of bias), “no” (high risk of bias), or “unclear” (uncertain risks). This was independently evaluated by two reviewers (MJ and YS). Disagreements were resolved by a third reviewer (XW).
2.6. Data Synthesis and Analysis
We used the Cochrane Collaboration Review Manager software (RevMan 5.3) for statistical analysis. The extracted data were classified into dichotomous and continuous variables. Data were summarized using risk ratio (RR) with 95% confidence intervals (CI) for dichotomous outcome; mean difference (MD) with 95% CI was presented for continuous outcome. Heterogeneity across studies was informally assessed by visually inspecting forest plots and formally estimated by Cochran's Q test in which chi-square distribution is used to make inferences regarding the null hypothesis of homogeneity (P < 0.10 was considered to be representative of statistically significant heterogeneity). We also quantified the effect of heterogeneity using the I 2 statistic, which measures the degree of inconsistency in the studies by calculating what percentage of the total variation across studies is due to heterogeneity rather than by chance. I 2 values of 25, 50, and 75% were nominally assigned as low, moderate, and high estimates, respectively [26]. A fixed effects model was used when there was no significant heterogeneity (I 2 < 50%) of the results of the studies. Otherwise, the random effects model was used (I 2 ≥ 50%). Based on different outcome measures, we would investigate possible causes from clinical perspectives by conducting subgroup and sensitivity analysis. Various subgroup analyses were performed based on types of route of medication (e.g., oral drugs, external drugs, and injection) and drug categories (e.g., Nimesulide, Indomethacin, and Ibuprofen + Prednisone). Sensitivity analysis was performed by removing each study in sequence and recalculating the results, aiming to assess whether one or more studies influenced the overall results. We used funnel plots to examine asymmetry for publication bias, revealing an asymmetrical distribution of studies around the line of identity, indicating the possibility of a small indistinct study bias [27].
3. Results
3.1. Study Selection
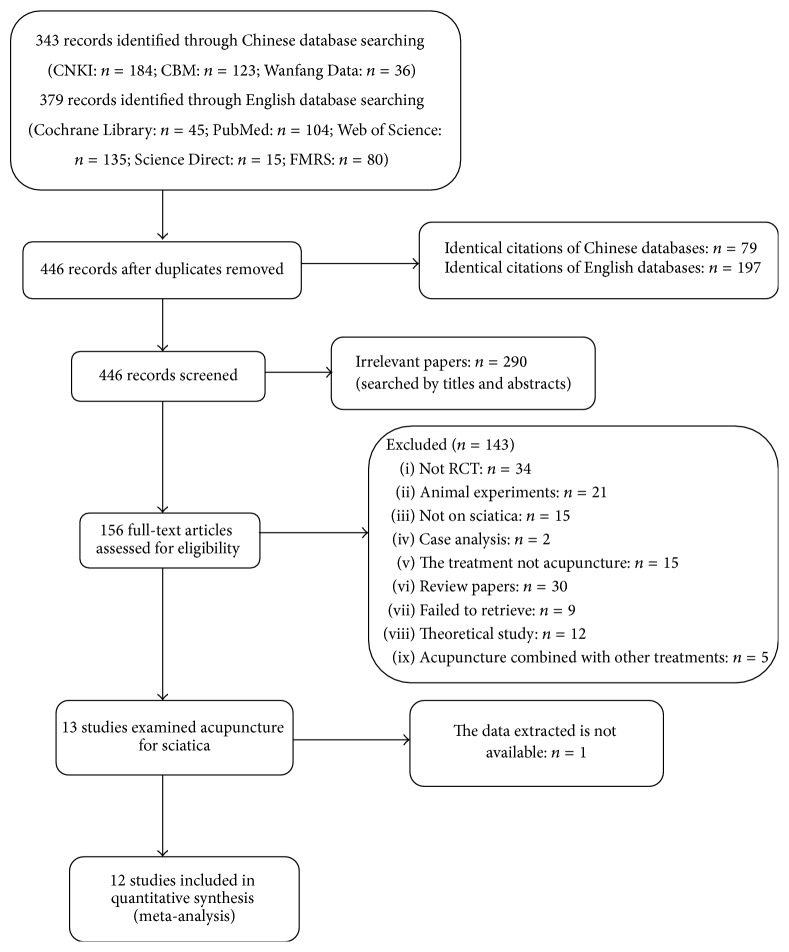
The database search obtained 722 records (343 records from Chinese databases and 379 records from English databases) potentially relevant to the research. Following removal of duplicates, 446 records remained (79 identical citations in Chinese and 197 identical citations in English). A total of 290 trials were excluded following reading of the titles and abstracts, due to lack of relevance. The full text of the remaining 156 articles was read and analyzed in detail, with 12 papers finally included for the systematic review. This screening process is summarized in a flow diagram (Figure 1).
Figure 1.
Flowchart of the trial selection process.
3.2. Study Characteristics and Quality
All of the included trials originated in China, with a total of 1842 participants (901 in treatment groups and 941 in control groups). Of the 12 included studies, 11 demonstrated no significant difference at baseline in gender, age, and other basic information and the remaining study [10] did not report any information about the participants. Two studies [12, 19] have two control groups. Mean age ranged between 18.0 and 77.0 years and disease duration ranged from 4 days to 18 years. Uniformity of inclusion criteria was limited, with five studies [11, 15, 17, 20, 22] mentioning the type of sciatica (one with primary sciatica [15], two with secondary sciatica [17, 20], one with trunk-sciatica [11], and one with root sciatica [22]) and two studies [10, 22] not stating the duration of symptoms. The basic characteristics of the included trials are presented in Table 1. Table 2 presents details of acupuncture treatment and control interventions of studies included in the meta-analysis.
Table 1.
Data summary and characteristics of the 12 studies included in meta-analysis.
| Study ID | Group | Age (year)∗ | Duration (month)∗ | Sample size N (M/F) |
Outcome | Type of sciatica | Diagnostic criteria | Withdrawal/adverse effects |
|---|---|---|---|---|---|---|---|---|
| Zhan and Liang, 1993 [10] | Acupuncture CWM |
NA NA |
NA NA |
420 420 |
Effectiveness | NA | NA | NA/NA |
|
| ||||||||
| Chen et al., 2007 [12] | Acupuncture CWM1 CWM2 |
34.24 ± 5.78 33.36 ± 7.58 35.78 ± 9.65 |
63 ± 43.08 69.36 ± 58.44 56.52 ± 47.52 |
30 (22/8) 30 (21/9) 30 (20/10) |
Effectiveness pain threshold | NA | The clinical diagnostic and curative criteria of diseases (2nd) (1999) | NA/NA |
|
| ||||||||
| Dong et al., 2008 [15] | Acupuncture CWM |
25–64 22–65 |
0.57–252 0.3–216 |
60 (32/28) 60 (34/26) |
Pain intensity | Primary sciatica | 3200 standard diagnoses of diseases in internal medicine | NA/NA |
|
| ||||||||
| Chen, 2010 [16] | Electroacupuncture CWM |
41.72 ± 10.01 42.10 ± 9.87 |
25.29 ± 8.12 24.21 ± 7.98 |
30 (12/18) 30 (11/19) |
Effectiveness pain intensity | NA | Criteria of diagnosis of diseases and syndromes in traditional Chinese medicine (1994) Practical diagnostics and therapeutics of integrated traditional Chinese and Western medicine (1995) |
A/A |
|
| ||||||||
| Zhu et al., 2011 [11] | Electroacupuncture CWM |
18–75 19–76 |
1–60 1.5–66 |
40 (22/18) 40 (21/19) |
Effectiveness | Trunk-sciatica | Physical examination, physical test (straight-leg-raising test), and diagnostic imaging |
NA/NA |
|
| ||||||||
| Zhang, 2012 [17] | Acupuncture CWM |
35 ± 4.5 | 0.3–48 | 145 (89/56) | Effectiveness | Secondary sciatica | Physical examination, physical test (the sciatic nerve traction syndrome), and diagnostic imaging |
NA/A |
|
| ||||||||
| Zhai, 2012 [18] | Acupuncture CWM |
22–71 22–70 |
0.33–12 0.1–12 |
28 (17/11) 28 (16/12) |
Effectiveness | NA | Physical examination, physical test (straight-leg-raising test), and diagnostic imaging |
NA/NA |
|
| ||||||||
| Liu, 2012 [19] | Acupuncture CWM1 CWM2 |
29–35 | 60–108 | 80 (43/37) | Pain threshold | NA | The clinical diagnostic and curative criteria of diseases | NA/A |
|
| ||||||||
| Qiu, 2013 [5] | Acupuncture CWM |
24–68 25–69.5 |
0.4–60 0.5–72 |
87 (52/35) 87 (54/33) |
Effectiveness | NA | Physical examination, physical test (the sciatic nerve traction syndrome), and diagnostic imaging |
NA/NA |
|
| ||||||||
| Huang, 2014 [20] | Acupuncture CWM |
36 ± 4.6 | 10–48 | 76 (50/26) | Effectiveness | Secondary sciatica | Physical examination, physical test (the sciatic nerve traction syndrome), and diagnostic imaging |
NA/NA |
|
| ||||||||
| Wang, 2014 [21] | Electroacupuncture CWM |
53.29 ± 3.17 | 63.84 ± 18.84 | 80 (43/37) | Effectiveness pain threshold | NA | The clinical diagnostic and curative criteria of diseases | NA/NA |
|
| ||||||||
| Ye et al., 2015 [22] | Electroacupuncture CWM |
58.2 ± 9.1 55.5 ± 7.1 |
NA NA |
31 (12/19) 30 (11/19) |
Pain intensity | Root sciatica | Criteria of diagnosis and therapeutic effect of diseases and syndromes in traditional Chinese medicine (1994) Guiding principle of clinical research on new drugs of traditional Chinese medicine (trial) (2002) |
NA/NA |
A: available; M: male; F: female; NA: not available; CWM: conventional Western medicine; RCT: randomized controlled trial.
∗Age and duration were shown in mean ± standard deviation or minimum–maximum.
Table 2.
Details of acupuncture treatment and control interventions of studies included in the meta-analysis.
| Study ID | Acupuncture rationale | Details of needling | Treatment regimen | Control interventions (drug/dosage/frequency) | ||||
|---|---|---|---|---|---|---|---|---|
| Points used | Depth of insertion/response sought | Needle stimulation | Needle type/retention time | No. TS | Frequency | |||
| Zhan and Liang, 1993 [10] | TCM | Shenshu (BL 23), Zhishi (BL 53), Zhibian (BL 54), Huantiao (GB 30), Yanglingquan (GB 34), Xuanzong (GB 39), Qiuxu (GB 40), Taichong (LR 3), and Fengfu (GV 16) | NA/NA | Manual | Number 30 needles (Hua Tuo card)/20 min | 40 | NA | Prednisone, Vit B1, Piroxicam (taken orally)/NA/NA |
|
| ||||||||
| Chen et al., 2007 [12] | TCM | Shenshu (BL 23), Dachangshu (BL 25), Huantiao (GB 30), Weizhong (BL 40), and Kunlun (BL 60) | NA/De qi | Manual | 0.30 × 60–75 mm/5~30 min | 10 | Once a day, 10 times/course, and 3 days' rest after a course | C1: Nimesulide (taken orally)/0.10 g/bid C2: 654-2 injection (i.m.)/2 mg per acupoint/<10 mg/qd 10 times per course, 3 days' rest after a course |
|
| ||||||||
| Dong et al., 2008 [15] | TCM | Huantiao (GB 30) | NA/Gaing of qi | Manual | 0.3 mm × 4-inch unused sterile needles (Ruiqi Er brand)/30 min | 15 | Once a day, 15 times/course | Ibuprofen Sustained Release Capsules (taken orally)/300 mg/bid 15 times per course |
|
| ||||||||
| Chen, 2010 [16] | TCM | Jiaji (L2–4) (EX-B2), Zhibian (BL 54), Huantiao (GB 30), Weizhong (BL 40), Chengshan (BL 57), Xuanzhong (GB 39), Kunlun (BL 60), Yinmen (BL 37), and Ashi point | 2 inches for the points Zhibian and Yanglingquan, 3~4 inches for the point Huantiao; 1.5 inches for the points Yinmen, Weizhong, and Chengshan/muscle twitch | Electrical | 0.30 × 25–40 mm/30 min | 6 | Three times per week, two weeks per course | Ibuprofen (taken orally)/0.2 g/tid; Prednisone (taken orally)/30 mg/tid 7 times per course |
|
| ||||||||
| Zhu et al., 2011 [11] | TCM | Huantiao (GB 30), Juliao (GB 29), Weizhong (BL 40), and Chengshan (BL 57) | NA/Huantiao: Gaing of qi to toes | Electrical | NA/30 min | 6 | Once a day, 6 times/course, and 3 days' rest after a course | Ibuprofen (taken orally)/300 mg/bid; Vit B1 injection (i.m.)/100 mg/qd; Vit B12 injection (i.m.)/0.25 mg/qd 6 times per course, 3 days' rest after a course |
|
| ||||||||
| Zhang, 2012 [17] | TCM | Posterior limb of lower limbs or back pain: Dachangshu (BL 25), Chengshan (BL 57), Huantiao (GB 30), and Weizhong (BL 40); lateral of lower limbs or buttocks pain: Huantiao (GB 30), Xuanzhong (GB 39), Yanglingquan (GB 34), and Fenglong (ST 40); all pain referred to above: Dachangshu (BL 25), Huantiao (GB 30), Zhibian (BL 54), Kunlun (BL 60), and Yanglingquan (GB 34) | NA/De qi | Manual | NA/30 min | 6 | Once a day, six times per week | Ibuprofen (taken orally)/0.6 g/tid; Prednisone/10 mg/tid 7 times per course, 2 days' rest after a course |
|
| ||||||||
| Zhai, 2012 [18] | TCM | Dachangshu (BL 25), Shenshu (BL 23), Huantiao (GB 30), Weizhong (BL 40), and Kunlun (BL 60) | NA/De qi | Manual | 0.30 × 60–75 mm/15~30 min | 10 | Once a day, 10 times/course, and 3 days' rest after a course | Nimesulide (taken orally)/0.10 g/bid 10 times per course, 3 days' rest after a course |
|
| ||||||||
| Liu, 2012 [19] | TCM | Shenshu (BL 23), Dachangshu (BL 25), Huantiao (GB 30), Weizhong (BL 40), and Kunlun (BL 60) | NA/De qi | Manual | 0.30 × 60–75 mm/NA | 10 | Once a day, 10 times/course, and 3 days' rest after a course | C1: Nimesulide (taken orally)/0.10 g/bid C2: 654-2 injection (i.m.)/2 mg per acupoint/<10 mg/qd 10 times per course, 3 days' rest after a course |
|
| ||||||||
| Qiu, 2013 [5] | TCM | Lateral leg or buttocks pain: Xuanzhong (GB 39), Yanglingquan (GB 34), Huantiao (GB 30), and Fenglong (ST 40); back or posterior limb of lower limbs pain: Dachangshu (BL 25), Chengshan (BL 57), Huantiao (GB 30), and Weizhong (BL 40); all pain referred to above: Zhibian (BL 54), Kunlun (BL 60), Yanglingquan (GB 34), Dachangshu (BL 25), and Huantiao (GB 30) | NA/De qi | Manual | Number 26 6-inch long needles/30 min | 10~12 | Once a day, 5~6 times per week, and two weeks per course | Indomethacin (taken orally)/30 mg/bid; Vit B12 (i.m.)/500 u/qd |
|
| ||||||||
| Huang, 2014 [20] | TCM | Lateral of lower limbs or buttocks pain: Yanglingquan (GB 34), Xuanzhong (GB 39), and Fenglong (ST 40); posterior limb of lower limbs or back pain: Chengshan (BL 57), Dachangshu (BL 25), and Huantiao (GB 30); all pain referred to above: Yanglingquan (GB 34), Zhibian (BL 54), Kunlun (BL 60), and Huantiao (GB 30) | NA/NA | Manual | NA/30 min | 6 | Once a day, six times per week | Ibuprofen (taken orally)/0.6 g/tid; Prednisone (taken orally)/10 mg/tid 7 times per course, 2 days' rest after a course |
|
| ||||||||
| Wang, 2014 [21] | TCM | Main points: Zhibian (BL 54), Huantiao (GB 30), Yanglingquan (GB 34), Juliao (GB 29), Kunlun (BL 60), Chengshan (BL 57), and Xuanzhong (GB 39) Optional points: damp-heat syndrome: Yinlingquan (SP 9), Pishu (BL 20); cold-dampness syndrome: Yaoyangguan (GV 3), Shenshu (BL 23); blood stasis syndrome: Weizhong (BL 40), Ciliao (BL 32); deficiency of both qi and blood: Geshu (BL 17), Sanyinjiao (SP 6), and Zusanli (ST 36) |
NA/De qi | Electrical | NA/30 min | 10 | Once a day, 10 times/course, and 5 days' rest after a course | Nimesulide (taken orally)/0.10 g/bid 10 times per course, 3 days' rest after a course |
|
| ||||||||
| Ye et al., 2015 [22] | TCM | Jiaji (L4-5) (EX-B2), Jiaji (L5-S5) (EX-B2), Zhibian (BL 54), and Huantiao (GB 30) | NA/De qi | Electrical | NA/30 min | 6 | Two times per week, for three weeks | Diclofenac Diethylamine gel (external use)/4 g four times per day, three weeks |
C: Control group; NA: not available; TCM: traditional Chinese medicine; No. TS: number of treatment sessions.
i.m.: intramuscular route; qd: once a day; bid: twice a day; tid: three times a day.
For randomization, three studies [12, 16, 22] referred to a random digit table and one study [16] referred to a sealed envelope, with the remainder providing incomplete information. None of the studies were subject blinded or indicated whether the assessors were blinded to treatment allocation. The risk of bias assessment is shown in Figure 2.
Figure 2.
Quality assessment of included studies. (a) Risk of bias graph; (b) risk of bias summary.
3.3. Effectiveness
Pooled analysis of nine studies [5, 10–12, 16–18, 20, 21] with 780 patients in the acupuncture group and 771 in the medication group revealed that acupuncture was significantly more effective than conventional medication (RR: 1.21; 95% CI: 1.16–1.25; P < 0.00001). As there was mild homogeneity in the consistency of the trial results (χ 2 = 12.43; P = 0.13; I 2 = 36%), a fixed effects model was applied (Figure 3). The graphic funnel plot of these nine studies appeared to be slightly asymmetric, suggesting the possibility of publication bias (Figure 4). In the subgroup analysis based on drug categories, subjects were divided into Nimesulide, Ibuprofen + Prednisone, Ibuprofen + Vitamin B1, and Indomethacin. The results did not change (Table 3). Sensitivity analysis was performed to assess the stability of the meta-analysis. When any single study was deleted, the corresponding pooled RR were changed slightly, with the statistically similar results indicating a good stability of the meta-analysis (Table 4).
Figure 3.

Forest of comparisons of total effectiveness between acupuncture group and medication group.
Figure 4.

Funnel plot on effectiveness to evaluate the publication bias of the literatures.
Table 3.
The results of subgroup meta-analysis.
| Subgroup | Eligible studies | Acupuncture group (number) |
Medication group (number) |
RR/MD (95% CI) | P value | Heterogeneity test | Effect model |
|---|---|---|---|---|---|---|---|
| Effectiveness | |||||||
| Drug categories | |||||||
| Nimesulide | 3 | 98 | 98 | 1.28 (1.12, 1.45) | 0.0002 |
P = 0.81, I 2 = 0% |
Fixed |
| Ibuprofen + Prednisone | 3 | 145 | 136 | 1.32 (1.17, 1.49) | <0.00001 |
P = 0.42, I 2 = 0% |
Fixed |
| Ibuprofen + Vitamin B1 | 2 | 450 | 450 | 1.15 (1.11, 1.19) | <0.00001 |
P = 0.59, I 2 = 0% |
Fixed |
| Indomethacin | 1 | 87 | 87 | 1.30 (1.11, 1.52) | 0.001 | — | — |
|
| |||||||
| Pain intensity | |||||||
| Treatment method | |||||||
| Oral | 2 | 90 | 90 | −1.44 (−2.65, −0.24) | 0.02 |
P = 0.07, I 2 = 69% |
Random |
| External | 1 | 31 | 30 | −1.19 (−1.67, −0.71) | <0.00001 | — | — |
| Drug categories | |||||||
| Ibuprofen + Prednisone | 1 | 30 | 30 | −2.10 (−3.15, −1.05) | <0.00001 | — | — |
| Ibuprofen | 1 | 60 | 60 | −0.87 (−1.70, −0.04) | 0.04 | — | — |
| Diclofenac | 1 | 31 | 30 | −1.19 (−1.67, −0.71) | <0.00001 | — | — |
|
| |||||||
| Pain threshold | |||||||
| Treatment method | |||||||
| Oral | 3 | 100 | 100 | 1.18 (1.06, 1.30) | <0.00001 |
P = 0.81, I 2 = 0% |
Fixed |
| Injection | 2 | 60 | 50 | 0.93 (0.79, 1.07) | <0.00001 |
P = 0.81, I 2 = 0% |
Fixed |
| Drug categories | |||||||
| Nimesulide | 3 | 100 | 100 | 1.18 (1.06, 1.30) | <0.00001 |
P = 0.81, I 2 = 0% |
Fixed |
| 654-2 | 2 | 60 | 50 | 0.93 (0.79, 1.07) | <0.00001 |
P = 0.81, I 2 = 0% |
Fixed |
RR: risk ratio; MD: mean difference; 95% CI: 95% confidence interval; 654-2: anisodamine.
Table 4.
The results of the included studies through sensitivity analysis.
| Excluded study | Acupuncture group (number) |
Medication group (number) |
RR/MD (95% CI) | P value | Heterogeneity test | Effect model |
|---|---|---|---|---|---|---|
| Effectiveness | ||||||
| Before excluding | 780 | 771 | 1.21 (1.16, 1.25) | P < 0.00001 | P = 0.13, I 2 = 36% | Fixed |
| Chen, 2007 | 750 | 741 | 1.21 (1.16, 1.25) | P < 0.00001 | P = 0.09, I 2 = 43% | Fixed |
| Chen, 2010 | 750 | 741 | 1.21 (1.16, 1.25) | P < 0.00001 | P = 0.09, I 2 = 44% | Fixed |
| Huang, 2014 | 740 | 735 | 1.20 (1.15, 1.24) | P < 0.00001 | P = 0.24, I 2 = 24% | Fixed |
| Qiu, 2013 | 693 | 684 | 1.20 (1.15, 1.24) | P < 0.00001 | P = 0.19, I 2 = 30% | Fixed |
| Wang, 2014 | 740 | 731 | 1.20 (1.15, 1.25) | P < 0.00001 | P = 0.18, I 2 = 31% | Fixed |
| Zhai, 2012 | 752 | 743 | 1.21 (1.16, 1.25) | P < 0.00001 | P = 0.09, I 2 = 43% | Fixed |
| Zhang, 1993 | 360 | 351 | 1.29 (1.20, 1.39) | P < 0.00001 | P = 0.93, I 2 = 0% | Fixed |
| Zhang, 2012 | 705 | 701 | 1.20 (1.15, 1.24) | P < 0.00001 | P = 0.21, I 2 = 27% | Fixed |
| Zhu, 2011 | 750 | 741 | 1.21 (1.16, 1.25) | P < 0.00001 | P = 0.09, I 2 = 44% | Fixed |
| Pain intensity | ||||||
| Before excluding | 121 | 120 | −1.25 (−1.63, −0.86) | P < 0.00001 | P = 0.18, I 2 = 41% | Fixed |
| Chen, 2010 | 91 | 90 | −1.11 (−1.53, −0.70) | P < 0.00001 | P = 0.51, I 2 = 0% | Fixed |
| Dong, 2008 | 61 | 60 | −1.52 (−2.38, −0.66) | 0.00005 | P = 0.12, I 2 = 58% | Random |
| Ye, 2015 | 90 | 90 | −1.44 (−2.65, −0.24) | 0.02 | P = 0.07, I 2 = 69% | Random |
| Pain threshold | ||||||
| Before excluding | 160 | 150 | 1.08 (0.98, 1.17) | P < 0.00001 | P = 0.13, I 2 = 44% | Fixed |
| Chen, 2007 | 130 | 120 | 1.06 (0.91, 1.22) | P < 0.00001 | P = 0.08, I 2 = 55% | Random |
| Chen_1, 2007 | 130 | 120 | 1.13 (1.02, 1.24) | P < 0.00001 | P = 0.34, I 2 = 11% | Fixed |
| Liu, 2012 | 130 | 120 | 1.06 (0.91, 1.21) | P < 0.00001 | P = 0.09, I 2 = 54% | Random |
| Liu_1, 2012 | 130 | 130 | 1.11 (0.96, 1.25) | P < 0.00001 | P = 0.12, I 2 = 48% | Fixed |
| Wang, 2014 | 120 | 110 | 1.03 (0.91, 1.16) | P < 0.00001 | P = 0.25, I 2 = 27% | Fixed |
RR: risk ratio; MD: mean difference; 95% CI: 95% confidence interval.
3.4. Pain Intensity
Three studies [15, 16, 22] reported pain intensity using a VAS to measure pain. The result revealed that acupuncture group experienced a significantly greater reduction in pain intensity than those who received conventional medication (MD: −1.25; 95% CI: −1.63 to −0.86; P < 0.00001). The result was homogenous (χ 2 = 3.39; P = 0.18; I 2 = 41%) and a fixed effects model was applied (Figure 5). In the subgroup analysis based on treatment method, subjects were divided into oral medication and external medication, and based on drug categories, subjects were divided into Ibuprofen + Prednisone, Ibuprofen, and Diclofenac. The results did not change (Table 3). The results also did not change in sensitivity analysis (Table 4).
Figure 5.
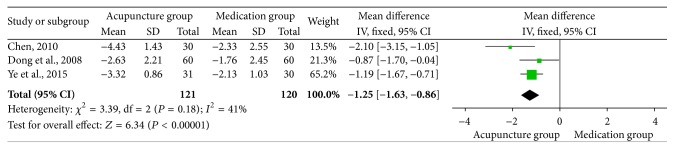
Forest of comparisons of pain intensity: acupuncture versus medication.
3.5. Pain Threshold
Pain threshold data were available in three studies [12, 19, 21] (two studies included two control groups). Meta-analysis revealed that acupuncture increased pain threshold favorably compared with medication (MD: 1.08; 95% CI: 0.98–1.17; P < 0.00001). The result was homogenous (χ 2 = 7.12; P = 0.13; I 2 = 44%) and a fixed effects model was applied (Figure 6). In the subgroup analysis based on treatment method, subjects were divided into oral medication and point-injection medication, and based on drug categories, subjects were divided into Nimesulide and 654-2. Change of the results was not found (Table 3). And similar results were also found in sensitivity analysis (Table 4).
Figure 6.
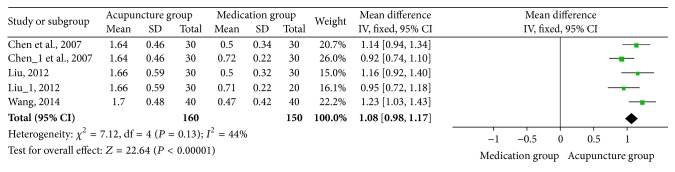
Forest of comparisons of pain threshold: acupuncture versus medication.
3.6. Withdrawal and Adverse Effects
As shown in Table 1, only one trial [16] mentioned withdrawal, reporting no expulsion case. Three trials [16, 17, 19] mentioned adverse effects. Zhang [17] and Liu [19] reported no adverse effects of the acupuncture treatment. In the study of Chen [16], two cases with subcutaneous hemorrhage occurred after needling in the treatment group and the symptom of blood stasis disappeared after three or four days of hot pack.
4. Discussion
Sciatica is one of the most frequently reported complaints affecting quality of life and reducing social and economic efficiency. Most of this cost is not generated by medical treatment but attributable to loss of productivity [28]. In TCM, it is classified into the category of Bi syndrome (Bi Zheng) [29]. Conservative and surgical intervention are two predominant choices for therapy. Conservative treatment for sciatica is primarily aimed at pain reduction, either by analgesics or by reducing pressure on the nerve root, and includes prescription drugs, acupuncture, epidural steroid injections, spinal manipulation, traction therapy, hot packs, and muscle relaxants [30]. Surgical intervention focuses on eliminating the suspected cause of the sciatica, by the removal of part or all of the herniated disc and the alleviation of foraminal stenosis [30].
Acupuncture is an established adjuvant analgesic modality for the treatment of chronic pain, and it is considered a cure for many ailments and disorders [31]. The acupuncture-induced intricate feeling (soreness, numbness, heaviness, and distension) in the deep tissue beneath the acupoint is essential to acupuncture analgesia [32]. Acupuncture is thought to stimulate inhibitory nerve fibers for a short period, reducing transmission of pain signal to the brain [33]. Acupuncture treatment activates endogenous analgesic mechanisms [34], causing secretion of endorphin which is an endogenous opioid [35] and triggering release of adenosine [36], producing a rapidly effective analgesic action on radicular sciatica. Extensive research has shown that acupuncture analgesia may be initiated by stimulation of high-threshold, small-diameter nerves in the muscles [37]. A cohort study found that after electroacupuncture (EA) to the spinal nerve root, the symptoms of patients with radicular sciatica were immediately and markedly reduced [38]. Animal experiments have revealed that acupuncture is a better treatment for regeneration of crushed sciatic nerves than diclofenac sodium [39]. Data exists demonstrating that EA intervention can attenuate pain via regulation of expression of multiple proteins in the hypothalamus [40]. Thus, acupuncture is worthy of wide clinical application.
Following a comprehensive search of eight electronic databases, 12 studies (1842 participants) were included in the review. Analysis of outcomes revealed that acupuncture is more effective than medication for individuals with sciatica for effectiveness (RR 1.21; 95% CI: 1.16–1.25), pain intensity (MD −1.25; 95% CI: −1.63 to −0.86), and pain threshold (MD: 1.08; 95% CI: 0.98–1.17). The pooled results of this meta-analysis indicate that acupuncture is clinically effective, reduces pain intensity, and increases pain threshold in patients with sciatica compared with medication. In the subgroup analysis, the results did not change in different treatment method and drug categories. And in the sensitivity analysis, omitting the study of Zhan and Liang [10] in 1993 or Chen [16] in 2010, the heterogeneity changed from moderate to low. The reasons of the slight change might be that the design of the former one was not restricted (lacking basic data, such as patients characteristics, specific interventions) and the time of performing was too early and the medication routes of the latter were different from others.
Despite an extensive literature search, only a limited number of studies were available, hampering clear and exact conclusions. Most of the randomized controlled trials had low methodological quality with a high risk of bias. All selected trials demonstrated randomization; however, the processes of randomization and allocation concealment were not adequately described and blinding of patients and assessors was seldom mentioned. Only three trials [12, 16, 22] mentioned random sequence generation and only one demonstrated [16] allocation concealment, with none of the trials being blinded. Therefore, selection bias may have existed. For those studies without adequate explanation of quality control measures, it is difficult to rule out the possibility of selective bias, implementation bias, and measurement bias, which may lead to unreliable results. Except for methodological heterogeneity, there existed clinical diversity. (1) Variations of acupuncture: according to TCM, sciatica is caused by invasion of wind-cold or wind-damp, obstruction of channel due to blood stasis or stagnation [8]; based on TCM theory, all acupuncture procedures (e.g., points used, method of stimulation, and number of treatment sessions) need to be performed according to syndrome differentiation and individual differences, so acupuncture modalities are various from study to study and difficult to master and unify. For example, Qiu [5], Huang [20], Zhang [17], and Wang [21] selected acupuncture points based on different parts of pain and types of syndrome. A lack of TCM knowledge can reduce the therapeutic effect to some extent. Therefore, practisers are required to have a deep understanding of sciatica and acupuncture from the aspect of TCM so that clinical techniques could be rigorous [41]. (2) Criterion of CWM: although the CWM were categorized into NSAIDs, steroids, and vitamins, there still existed difference between Piroxicam, Ibuprofen, Nimesulide, and Indomethacin. Additionally, the duration and doses of administered drugs might influence the therapeutic effect to some extent. Above all, the appearance of clinical heterogeneity could be reasonably explained and further solved. Meanwhile, further methodologically robust trials are required. Therefore, although acupuncture may be effective in reducing pain and improving the symptoms compared to medication, the analysis results should be interpreted with caution.
It is evident that further studies of higher quality and with longer-term follow-up are needed for better quality and a more accurate analysis. To clarify the exact effect of acupuncture on patients with sciatica, further well-designed studies are needed. Further study design should take into account the following points: (1) the design should utilize strictly randomized, controlled, double-blind methods with patients selected objectively with standard eligibility; (2) all clinical studies of acupuncture should abide by STRICA; (3) appropriate sample size is required; (4) there is need for long-term follow-up; (5) there is consistency in the inclusion, exclusion, and diagnosis criteria; (6) there is implementation of standardized adverse event monitoring.
For sciatica, there is no gold standard for diagnosis and treatment so that it is difficult to establish effective form of treatment. Acupuncture is used to treat a variety of symptoms, especially pain, and has been demonstrated to be effective, safe, and well tolerated. From our meta-analysis, it is evident that acupuncture could be efficacious in treating the pain associated with sciatica. Although we were unable to draw definite conclusions due to the poor quality of the available trials, this positive result could provide clinicians with an accessible assessment of its therapeutic value and draw attention to acupuncture research.
Acknowledgments
This study was supported by a project funded by the Priority Academic Program Development of Jiangsu Higher Education Institutions (PAPD) and grants from the People Programme (Marie Curie Actions) of the European Union's Seventh Framework Programme FP7/2007–2013/under REA Grant Agreement no. PIR SES-GA-2013-612589.
Conflict of Interests
The authors have declared that no conflict of interests exists.
References
- 1.Valat J.-P., Genevay S., Marty M., Rozenberg S., Koes B. Sciatica. Best Practice and Research: Clinical Rheumatology. 2010;24(2):241–252. doi: 10.1016/j.berh.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 2.Konstantinou K., Dunn K. M. Sciatica: review of epidemiological studies and prevalence estimates. Spine. 2008;33(22):2464–2472. doi: 10.1097/brs.0b013e318183a4a2. [DOI] [PubMed] [Google Scholar]
- 3.Stafford M. A., Peng P., Hill D. A. Sciatica: a review of history, epidemiology, pathogenesis, and the role of epidural steroid injection in management. British Journal of Anaesthesia. 2007;99(4):461–473. doi: 10.1093/bja/aem238. [DOI] [PubMed] [Google Scholar]
- 4.Cook C. E., Taylor J., Wright A., Milosavljevic S., Goode A., Whitford M. Risk factors for first time incidence sciatica: a systematic review. Physiotherapy Research International. 2014;19(2):65–78. doi: 10.1002/pri.1572. [DOI] [PubMed] [Google Scholar]
- 5.Qiu Y. Clinical observation of 87 cases of sciatica treated by acupuncture. Guide of China Medicine. 2013;11(27):490–491. [Google Scholar]
- 6.Zhang Y., Xing J. J., Li J., Zeng B. Y., Liang F. R. International Review of Neurobiology. chapter 1. Vol. 111. Elsevier; 2013. History of acupuncture research; pp. 1–23. [DOI] [PubMed] [Google Scholar]
- 7.Vickers A., Wilson P., Kleijnen J. Acupuncture. Quality and Safety in Health Care. 2002;11(1):92–97. doi: 10.1136/qhc.11.1.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jiang Y. G., Mu J. S., Zhang X. Y., Bai Q. L. Clinical observation on acupuncture treatment of 106 cases of trunk-sciatica. Journal of Traditional Chinese Medicine. 1984;4(3):183–185. [PubMed] [Google Scholar]
- 9.Dorsher P. T. Acupuncture for chronic pain. Techniques in Regional Anesthesia and Pain Management. 2011;15(2):55–63. doi: 10.1053/j.trap.2011.04.002. [DOI] [Google Scholar]
- 10.Zhan W. Z., Liang X. W. Different methods for the treatment of 2100 cases of sciatica. Journal of GanSu College of TCM. 1993;10(2):p. 47. [Google Scholar]
- 11.Zhu J. H., Chen H. Y., Chen J. Y. Treating 30 cases of backbone of sciatica by hip three-needle-based acupuncture. Clinical Journal of Chinese Medicine. 2011;3(5):78–79. [Google Scholar]
- 12.Chen M. R., Wang P., Cheng G., et al. A clinical observation on acupuncture for 30 cases of sciatica. Journal of Traditional Chinese Medicine. 2007;48(3):238–240. [Google Scholar]
- 13.van der Molen H. F., Hoonakker P. L. T., Lehtola M. M., et al. Writing a Cochrane systematic review on preventive interventions to improve safety: the case of the construction industry. Medicina del Lavoro. 2009;100(4):258–267. [PubMed] [Google Scholar]
- 14.Qin Z., Liu X., Yao Q., Zhai Y., Liu Z. Acupuncture for treating sciatica: a systematic review protocol. BMJ Open. 2015;5(4) doi: 10.1136/bmjopen-2014-007498.e007498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dong Q. J., Wu B. H., Zhang Y. M. Observation on the therapeutic effect of searching-needling method of acupuncture for 60 cases of primary sciatica. New Medical Science. 2008;7(4):135–136. [Google Scholar]
- 16.Chen W. K. Clinical study of acupuncture in sciatica patients [M.S. thesis] Guangdong, China: Guangzhou University of Chinese Medicine; 2010. [Google Scholar]
- 17.Zhang Z. Clinical observation of 145 cases of sciatica treated by acupuncture. Chinese Journal of Modern Drug Application. 2012;6(4):124–125. [Google Scholar]
- 18.Zhai L. H. Clinical observation of sciatica treated by acupuncture. Medical Information. 2012;25(2):p. 562. [Google Scholar]
- 19.Liu B. L. Clinical analysis of 80 cases of acupuncture and moxibustion for treatment of sciatica. Guide of China Medicine. 2012;10(24):590–591. [Google Scholar]
- 20.Huang W. D. Clinical observation of 76 cases of sciatica treated by acupuncture. Contemporary Medicine Forum. 2014;12(1):178–179. [Google Scholar]
- 21.Wang C. H. Clinical observation of sciatica treated by acupuncture. Asia-Pacific Traditional Medicine. 2014;10(6):94–95. [Google Scholar]
- 22.Ye X. C., Zhao P., Wang L., et al. Clinical observation on the treatment of root scitica by electro acupuncture at Jiaji point. Information on Traditional Chinese Medicine. 2015;32(1):108–111. [Google Scholar]
- 23.Yang L., Yang Z., Yu H., Song H. Acupuncture therapy is more effective than artificial tears for dry eye syndrome: evidence based on a meta-analysis. Evidence-Based Complementary and Alternative Medicine. 2015;2015:11. doi: 10.1155/2015/143858.143858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Macpherson H., Altman D. G., Hammerschlag R., et al. Revised standards for reporting interventions in clinical trials of acupuncture (STRICTA): extending the consort statement. PLoS Medicine. 2010;7(6) doi: 10.1371/journal.pmed.1000261.e1000261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Higgins J. P. T., Altman D. G., Sterne J. A. C. Assessing risk of bias in included studies. In: Higgins J. P. T., Green S., editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. chapter 8. The Cochrane Collaboration; 2011. http://www.cochrane-handbook.org/ [Google Scholar]
- 26.Higgins J. P. T., Thompson S. G. Quantifying heterogeneity in a meta-analysis. Statistics in Medicine. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 27.Wei R.-L., Teng H.-J., Yin B., et al. A systematic review and meta-analysis of buyang huanwu decoction in animal model of focal cerebral ischemia. Evidence-Based Complementary and Alternative Medicine. 2013;2013:13. doi: 10.1155/2013/138484.138484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Witt C. M., Pach D., Brinkhaus B., et al. Safety of acupuncture: results of a prospective observational study with 229,230 patients and introduction of a medical information and consent form. Forschende Komplementärmedizin. 2009;16(2):91–97. doi: 10.1159/000209315. [DOI] [PubMed] [Google Scholar]
- 29.Wang C. Y., Ma J., Xiao L. Treatment of 50 cases of sciatica by needling zanzhu and fengchi. Journal of Traditional Chinese Medicine. 2003;23(1):51–52. [PubMed] [Google Scholar]
- 30.Koes B. W., Van Tulder M. W., Peul W. C. Diagnosis and treatment of sciatica. British Medical Journal. 2007;334(7607):1313–1317. doi: 10.1136/bmj.39223.428495.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hollisaz M. T. Use of electroacupuncture for treatment of chronic sciatic pain. Internet Journal of Pain, Symptom Control and Palliative Care. 2007;5:p. 7. [Google Scholar]
- 32.Zhao Z.-Q. Neural mechanism underlying acupuncture analgesia. Progress in Neurobiology. 2008;85(4):355–375. doi: 10.1016/j.pneurobio.2008.05.004. [DOI] [PubMed] [Google Scholar]
- 33.Chon T. Y., Lee M. C. Acupuncture. Mayo Clinic Proceedings. 2013;88(10):1141–1146. doi: 10.1016/j.mayocp.2013.06.009. [DOI] [PubMed] [Google Scholar]
- 34.Inoue M., Kitakoji H., Yano T., Ishizaki N., Itoi M., Katsumi Y. Acupuncture treatment for low back pain and lower limb symptoms—the relation between acupuncture or electroacupuncture stimulation and sciatic nerve blood flow. Evidence-Based Complementary and Alternative Medicine. 2008;5(2):133–143. doi: 10.1093/ecam/nem050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cheng K. J. Neuroanatomical basis of acupuncture treatment for some common illnesses. Acupuncture in Medicine. 2009;27(2):61–64. doi: 10.1136/aim.2009.000455. [DOI] [PubMed] [Google Scholar]
- 36.Goldman N., Chen M., Fujita T., et al. Adenosine A1 receptors mediate local anti-nociceptive effects of acupuncture. Nature Neuroscience. 2010;13(7):883–888. doi: 10.1038/nn.2562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kaptchuk T. J. Acupuncture: theory, efficacy, and practice. Annals of Internal Medicine. 2002;136(5):374–383. doi: 10.7326/0003-4819-136-5-200203050-00010. [DOI] [PubMed] [Google Scholar]
- 38.Inoue M., Hojo T., Yano T., Katsumi Y. Electroacupuncture direct to spinal nerves as an alternative to selective spinal nerve block in patients with radicular sciatica—a cohort study. Acupuncture in Medicine. 2005;23(1):27–30. doi: 10.1136/aim.23.1.27. [DOI] [PubMed] [Google Scholar]
- 39.La J.-L., Jalali S., Shami S. A. Morphological studies on crushed sciatic nerve of rabbits with electroacupuncture or diclofenac sodium treatment. American Journal of Chinese Medicine. 2005;33(4):663–669. doi: 10.1142/S0192415X05003259. [DOI] [PubMed] [Google Scholar]
- 40.Gao Y., Chen S., Xu Q., et al. Proteomic analysis of differential proteins related to anti-nociceptive effect of electroacupuncture in the hypothalamus following neuropathic pain in rats. Neurochemical Research. 2013;38(7):1467–1478. doi: 10.1007/s11064-013-1047-7. [DOI] [PubMed] [Google Scholar]
- 41.Lv Z. T., Song W., Wu J., et al. Efficacy of acupuncture in children with nocturnal enuresis: a systematic review and meta-analysis of randomized controlled trials. Evidence-Based Complementary and Alternative Medicine. 2015;2015:12. doi: 10.1155/2015/320701.320701 [DOI] [PMC free article] [PubMed] [Google Scholar]