Abstract
T follicular helper cells (TFH) are critical for the development and maintenance of germinal centers (GC) and humoral immune responses. During chronic HIV/SIV infection TFH accumulate, possibly as a result of antigen persistence. The HIV/SIV-associated TFH expansion may also reflect lack of regulation by suppressive follicular regulatory CD4+ T-cells (TFR). TFR are natural regulatory T-cells (TREG) that migrate into the follicle and, similarly to TFH, up-regulate CXCR5, Bcl-6, and PD1. Here we identified TFR as CD4+CD25+FoxP3+CXCR5+PD1hiBcl-6+ within lymph nodes of rhesus macaques (RM) and confirmed their localization within the GC by immunohistochemistry. RNA sequencing showed that TFR exhibit a distinct transcriptional profile with shared features of both TFH and TREG, including intermediate expression of FoxP3, Bcl-6, PRDM1, IL-10, and IL-21. In healthy, SIV-uninfected RM, we observed a negative correlation between frequencies of TFR and both TFH and GC B-cells as well as levels of CD4+ T-cell proliferation. Following SIV infection, the TFR/TFH ratio was reduced with no change in the frequency of TREG or TFR within the total CD4+ T-cell pool. Finally, we examined whether higher levels of direct virus infection of TFR were responsible for their relative depletion post-SIV infection. We found that TFH, TFR and TREG sorted from SIV- infected RM harbor comparable levels of cell-associated viral DNA. Our data suggests that TFR may contribute to the regulation and proliferation of TFH and GC B-cells in vivo and that a decreased TFR/TFH ratio in chronic SIV infection may lead to unchecked expansion of both TFH and GC B-cells.
Introduction
Several key findings over the past few years have energized efforts towards the development of an effective HIV vaccine, including the discovery and characterization of a number of broadly neutralizing antibodies (bnAbs) that develop in a subset of HIV-infected individuals. However, the mechanisms involved in shaping antibody responses to immunization with HIV antigens or natural HIV infection, including the generation of bnAbs remain incompletely understood (1). Importantly, HIV-Env-specific bnAbs develop at relatively late stages of HIV infection, and show peculiar genetic and molecular features, including a high level of divergence from germ line predecessors, which indicates that they are the products of extensive somatic hyper-mutation within germinal centers (GCs), as well as the presence of unusually long CDR3 regions (2). Perplexingly, there appear to be no direct or predictable routes to the development of these bnAbs from the germ line predecessors, and it remains unclear whether this process is driven by antigenic mutations and/or escape as opposed to specific intrinsic aspects of the B-cell or T-helper cell response (3). A better understanding of the mechanisms responsible for the development of bnAbs is crucial to harness this type of immunity for HIV prevention and therapy in humans.
T follicular helper cells (TFH) are critical for the development and maintenance of GCs and competition for survival signals from TFH via molecules such as CD40L and IL-21 is thought to be a key mechanism of selection of high affinity B-cells (4). The regulation of TFH frequency, and by extension the regulation of their impact on GC B-cell development and function, is vital to the quality of the humoral immune response (5). While the presence of too few TFH may lead to abortive GC formation and defective B-cell responses, an over-expansion was found to be associated with the prevalence of autoantibodies (6, 7). It is possible that an expansion of TFH also lowers the selection pressure on GC B-cells and leads to the emergence of low-affinity B-cells (8).
Several studies have shown that TFH accumulate during the chronic stages of HIV/SIV infection. This accumulation occurs even though these cells support high levels of viral replication and represent an important component of the persistent virus reservoir under anti-retroviral therapy (9). The chronic expansion of TFH in the case of HIV/SIV infection with persistent virus replication may be a direct result of antigenic persistence. As expected, HIV/SIV-associated expansion of TFH is associated with dysregulation of B-cell responses with ineffective memory cell formation and hyper-gammaglobulinemia (10),(11). Whether and to what extent this TFH expansion is also related to a deficit in the physiologic regulation of specific TFH immune response within the lymph nodes remains unknown. However, this possibility would be consistent with the well-known observation that the chronic phase of pathogenic HIV/SIV infections is associated with a state of generalized immune activation that is resistant to the normal mechanisms of immune regulation.
Under normal circumstances, regulation of TFH function is mediated at least in part by a recently described subset of CD4+ T-cells termed T follicular regulatory (TFR) cells. TFR are thought to develop from natural regulatory T-cells (TREG) that express lineage-associated markers such as FoxP3, CD25, as well as low levels of CD127. These TFR migrate into the follicles and GCs of lymph nodes by virtue of their expression of CXCR5 (and down-modulation of CCR7) and, similarly to TFH, express high levels of Bcl-6 and PD1 (12) (13). Of note, the role of TFR in the immuno-pathogenesis of HIV/SIV infections is currently unknown, both in terms of ability to negatively regulate HIV-specific B-cell responses (including, potentially, the production of bnAbs) and to suppress local virus-induced immune activation. Indeed, none of the previous reports on TFH dynamics in the context of SIV or HIV infection have distinguished between cells that either do or do not co-express TREG-associated markers. Thus the TFR subset within the broader CXCR5+Bcl-6+PD1+ is not fully characterized in the setting of HIV/SIV infection.
In this study, we described and characterized phenotypically, histologically, and genomically a TFR population that is found within the GCs of rhesus macaques (RM) and express markers associated with both TFH and TREG cells. The hypothesis that TFR play a suppressive role in vivo is supported by the observation that their frequency is inversely correlated with both the levels of TFH and GC B-cells and the percentage of proliferating CD4+ T-cells. In the setting of SIV infection, we found that TFR show a slow in vivo proliferative response after the initial infection and exhibit only a small increase in their frequency within the total CD4+ T-cell pool during the chronic phase. In conjunction with the large expansion of TFH observed following SIV infection, this phenomenon leads to a significantly decreased TFR/TFH ratio in the lymph nodes of chronically SIV-infected RM. These data may suggest that, during SIV infection, a lack of TFR expansion may allow for a progressive accumulation of TFH cells in the lymph nodes of chronically infected RM, thus indirectly contributing to the aberrant immune activation that characterizes this pathogenic infection.
Materials and Methods
Animals
The study involved a total of 40 Indian origin female rhesus macaques (RM) divided as follows: (i) Ten healthy, unvaccinated and SIV-uninfected RM; (ii) Ten healthy, SIV-immunized but SIV-uninfected RM; (iii) Eleven unvaccinated SIV-infected animals; and (iv) Nine vaccinated and SIV-infected RM. Animals were vaccinated with a SIVmac239 Gag-, Pol-, and Env-expressing DNA vaccine with inactivating mutations in proteases, half of which also co-expressed GM-CSF. These were followed by two boosts of a SIVmac239 Gag-, Pol-, and Env-expressing MVA vaccine as described previously (14). All infections were a result of SIVsmE660 intra-vaginal challenge at 2.06×104 TCID50 grown in RM peripheral blood mononuclear cells (PBMC). Lymph node biopsies were collected for measurement of a number of immunological parameters at day -35 prior to infection and days 14 and 168 after infection (i.e., acute and chronic phase, respectively). Spleen and lymph nodes were collected at necropsies performed at six months post infection. All animals were housed at Yerkes National Primate Center at Emory University and were cared for in accordance with National Institute of Health guidelines and following protocols approved by the Institutional Animal Care and Use Committee.
Tissue processing
Lymphocytes were isolated from freshly obtained lymph node and spleens by passing homogenized tissue through a 70-μm cell strainer and lysing blood cells with ACK Lysis buffer. Tissue collection was performed as previously described (15). Cells to be later used for sorting were cryopreserved at −80 degrees C in FBS media containing 10% DMSO.
Immunophenotyping and flow cytometry
Multi-color flow cytometric analysis was performed on mononuclear cells isolated from blood and lymph nodes according to standard procedures using monoclonal antibodies directed against RM markers and human markers that also cross-react with the same markers in RM. For optimum staining of intra-cellular markers, permeabilization of cells using the eBioscience FoxP3-permeabalization buffer was performed as recommended by the manufacturers. Pre-determined optimal concentrations of the following antibodies and reagents were used: CD3-Alexa700 (clone SP34-2), CD4-Allophycocyanin-Cy7 (clone OKT-4), Bcl-6-PeTexasRed (clone K112-91), Ki67- FITC (clone B56), CCR5-PE (clone 3A9), CTLA4- BV421 (clone BNI3) from BD, CXCR5-PerCP eFlour 710 (clone MU5BEE), PD1-PeCy7 (clone J105), CD127-PeCy5 (clone eBio-RDR5) from eBioscience and CD20-BV650 or PE-CF594 (clone 2H7), CD25-BV711 (clone BC96), Helios-FITC (clone 22F6) and FoxP3-Allophycocyanin (clone 150D) from Biolegend, and Live/Dead Fixable Aqua from Invitrogen. Flow cytometric data were acquired using LSRII flow cytometer using BD’s FACS DiVA software. Acquired data were analyzed using Flow Jo version9.3.2 following the gating strategy described in Figure1. Further analyses were performed using PRISM (GraphPad) and Excel (Microsoft Office 2011) software.
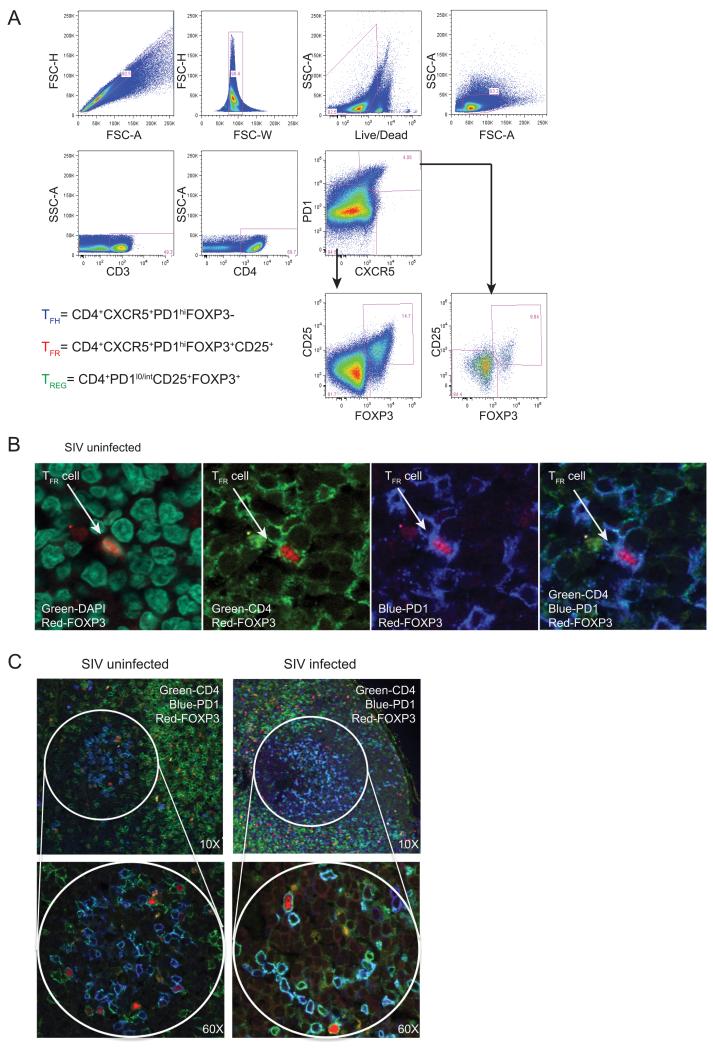
Figure 1. TFR can be defined by flow cytometry and identified by confocal microscopy within the germinal centers of RM.
(A) Representative flow cytometry plot of lymphocytes from lymph nodes of untreated uninfected RM showing the gating strategy used to define TFR, TFH and TREG cell populations. (B) Representative confocal microscope image showing a single TFR within the lymph node of an uninfected RM. The first image shows staining for DAPI (green) and FoxP3 (red). The second image shows the same section with CD4 (green) and FoxP3 (red), the third PD1 (blue) and FoxP3 (red) and the last image CD4 (green), PD1 (blue) and FoxP3 (red). (C) Representative images of lymph node biopsies from SIV uninfected and acutely infected RM showing cells stained with CD4 (green), FoxP3 (red) and PD1 (blue) within the GC regions.
Cell Sorting
Cryopreserved cells were thawed in a 37 degree C water bath and rested overnight for 8-10 hours and then stained for sorting. Splenocytes from 5 SIV-uninfected and vaccinated RM as well as 9 unvaccinated SIV-infected animals were used for sorting of TFH, TFR, and TREG. Cell populations were sorted using FACS Aria II flow cytometer. Cells were first gated based on light scatter followed by positive gating on cells negative for Live/Dead Fixable Aqua and positive for CD3 and CD4. After collecting bulk CD4+ cells the following three populations were collected: TFR (CXCR5+PD1hiCD127−CD25+), TFH (CXCR5+PD1hiCD127+/−CD25−) and TREG (CXCR5+/−PD1lo/intCD127−CD25+).
Immunohistochemistry and Confocal Microscopy
Immunohistochemstry was performed on 5-μm tissue sections mounted on glass-slides, which were deparaffinized and rehydrated with double-distilled H2O. Antigen retrieval was performed in 1xDako Target Retrieval Solution (pH 6.0) in a pressure cooker heating slides to 122 degrees C for 30s. Slides were then rinsed in ddH2O and incubated for 10 minutes using Dako Protein block. Slides were then incubated with rabbit anti-(1:200), mouse anti-FoxP3 (1:100) and goat anti-PD1 (1:500) for 1 hour at room temperature. Next, slides were washed in TBS with 0.05% Tween-20. Slides were then incubated for an hour in the dark with secondary antibody cocktail containing donkey anti-rabbit Alexa 488 (1:500), donkey anti-mouse Alexa-594 (1:500) and donkey anti-goat Alexa 647 (1:500). After washing in TBS with 0.05% Tween-20, Prolong Gold with DAPI was applied to all the slides. Confocal microscope images were obtained using Olympus FV10i® Confocal Microscope with CellSens® 1.9 Digital Imaging software.
Quantitative PCR for SIV gag DNA
Cell-associated viral DNA was measured in sorted cell populations from RM lymph nodes by RT-PCR as previously described(16-18).
RNA-Seq Library Preparation
Total RNA was prepared using the QIAGEN RNEasy Micro Kit. Libraries were generated using the CLONTECH SMARTer HV kit, barcoding and sequencing primers were added using NexteraXT DNA kit. Libraries were validated by microelectrophoresis, quantified, pooled and clustered on Illumina TruSeq v3 flowcell. Clustered flowcell was sequenced on an Illumina HiSeq 1000 in 100-base single-read reactions.
RNA-Seq Data Analysis
RNA-Seq data were submitted to the GEO repository at the National Center for Biotechnology Information (NCBI). RNA-Seq data were aligned to a provisional assembly of Indian Macaca mulatta (MaSuRCA rhesus assembly v.7_20130927) using STAR version 2.3.0e (19) (20). Transcripts were annotated using the provisional UNMC annotation v7.6. Transcript assembly, abundance estimates, and differential expression analysis was performed using Cufflinks v2.1.1 and Cuffdiff (21). All samples had read counts > 12000000 and unique mapping percentages in the range of 63 – 76 %; no samples were excluded from the analysis for technical issues. Differentially expressed genes were defined by pair-wise comparison of each phenotype. Differential gene lists were uploaded to Ingenuity Pathway Analysis software (v1.0 Ingenuity Systems, http://www.ingenuity.com/) and pathways with significant enrichment by Fisher’s Exact test and the Benjamini-Hochberg multiple testing correction. Heat maps and other visualization were generated using Partek Genomics Suite v6.6. RNA-seq data is publically available at the GEO repositories (accession number: GSE69756, URL: http://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE69756).
RT-PCR validation of RNA sequencing data
Total RNA was prepared using the QIAGEN RNEasy Micro Kit from sorted TFR, TFH and TREG cells. RNA quantity was measured using Nanodrop analysis and reverse transcribed as previously described for RNA sequencing. Finally, 0.1 μl of cDNA was used for real time SYBR green PCR analysis using an ABI 7900 HT Real-time PCR instrument (Applied Biosystems). Primer sequences for PCR were GAPDH: Fwd5′-GCACCACCAACTGCTTAGCAC-3′, Rev 5′- TCTTCTGGGTGGCAGTGATG-3′. IL2RA: Fwd5′- GGCTTCATTTTCCCACGGT-3′, Rev 5′- GCAGCTGGCGGACCAA-3′. IL6R: Fwd5′- TTCGGCCGGACTGTTCTG-3′, Rev 5′- GCACCCCATCTCCGACG-3′. SLAMF6: Fwd5′- TGG AAC ATC TCT TGC CTT CAT AG-3′, Rev 5′- GTT GCT GAG TTT CAG GGA GTA G-3′. SAP/SH2D1A: Fwd5′- CTC TGC AGT ATC CAG TTG AGA AG-3′, Rev 5′- GGC TTT CAG GCA GAC ATC A-3′. XIAP: Fwd 5′- GAG GAA CCC TGC CAT GTA TAG-3′, Rev 5′- GTG TAG TAG AGT CCA GCA CTT G-3′; PRDM1: Fwd 5′- TGT GGT ATT GTC GGG ACT TTG-3′, Rev 5′- GCT TGA GAT TGC TCT GTG TTT G-3′; CCL20: Fwd 5′- GCA ACT TTG ACT GCT GTC TTC-3′, Rev 5′- CAG CAT TGA TGT CAC AGG TTT C-3′; PD1: Fwd 5′- TCCTTGGCCACTGGTGTTC-3′, Rev 5′- CTTCTCCTGAGGGAAGGAGC-3′; IL10: Fwd 5′- AAGACCCTCAGGCTGAGGCT-3′, Rev 5′- TCCACGGCCTTGCTCTTG-3′; IL21: Fwd 5′- TGTGAATGACTTGGACCCTGAA-3′, Rev 5′AAACAGGAAATAGCTGACCACTCA-3′. Relative RNA transcript levels were calculated normalized to primer efficiency and housekeeping gene RNA (GAPDH).
Statistical Analyses
Except for RNA sequencing data, all statistical analyses were conducted using GraphPad Prism 5.0. Comparisons of mean fluorescence intensity between cell populations in uninfected RM were made using Wilcoxon signed rank tests (Fig 2). Man-Whitney U tests were used to compare frequencies of populations in uninfected, acutely infected and chronically infected RM (Figure 4, 5). Spearman rank correlation tests were used to analyze all correlations (Figure 6). All p values less than 0.05 were defined as significant.
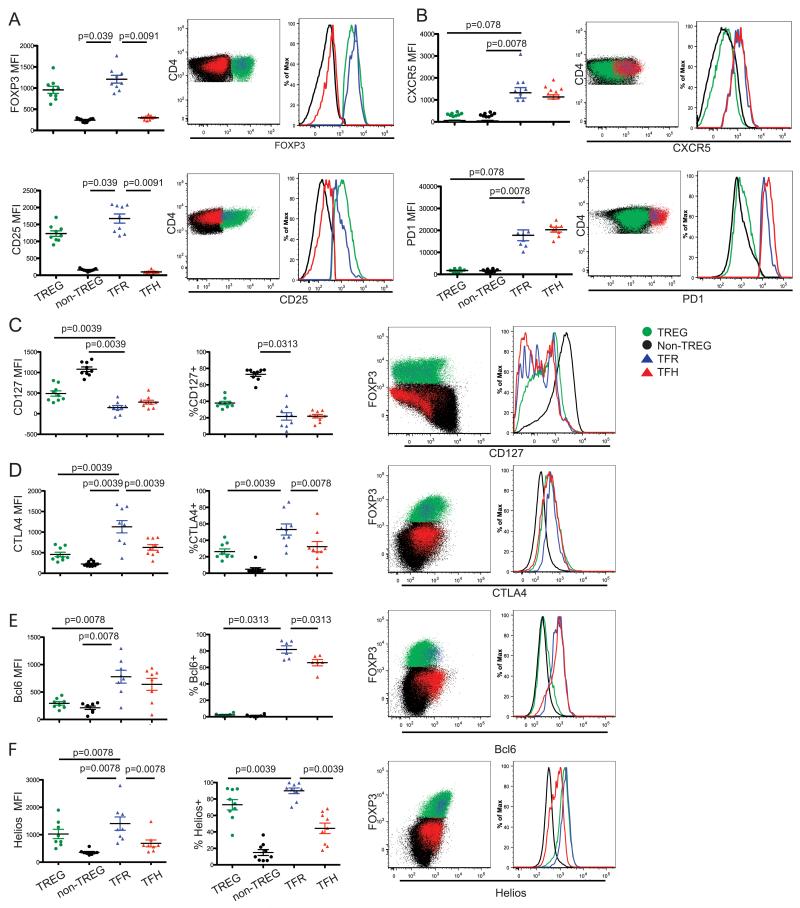
Figure 2. TFR share immunophenotypical features of both TFH and TREG populations.
Mean fluorescence intensity, percent positive, representative flow cytometry plots and histograms (Panels A, B, C, D, E, F) for expression of various immunophenotypical markers (i.e., FoxP3, CD25, CXCR5, PD-1, CD127, CTLA4, Bcl-6 and Helios) among TREG, non- TREG, TFR and TFH populations from LN of healthy, unvaccinated and uninfected RM. Non-TREG here are defined as all CD4+CD25−FoxP3− T-cells. Significance was determined by Wilcoxon signed rank tests.
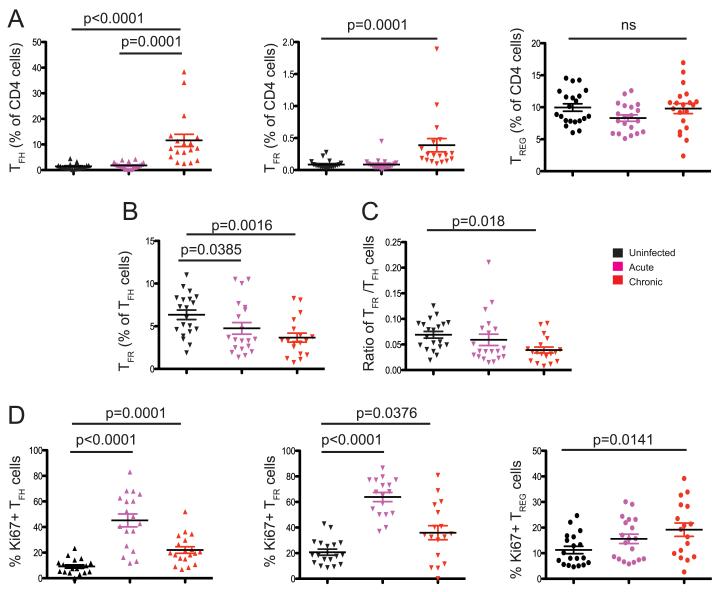
Figure 4. Kinetics of TFR, TFH and TREG after SIV infection.
(A) Frequency of TFH, TFR and TREG as percentage of the total CD4+ T-cell population within lymph nodes of uninfected, acutely (week 2) SIV-infected and chronically (week 24) SIV-infected RM. (B) Frequency of TFR as a percent of TFH within the lymph nodes of the same animals. (C) Ratio of frequencies of TFR to the frequency of TFH (both calculated as a percent of the total CD4+ T-cell population). (D) Percent of proliferating, Ki67+, TFH, TFR and TREG within the lymph nodes of uninfected, acutely SIV-infected and chronically SIV-infected RM. Statistical analyses were performed using Mann-Whitney U tests.
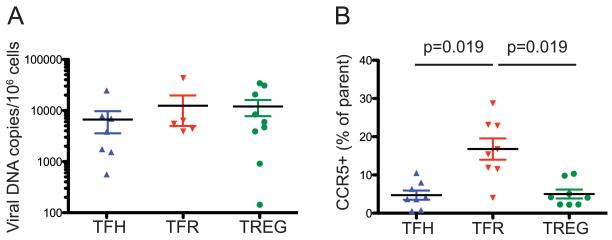
Figure 5. Comparable levels of SIV infection in TFH, TFR and TREG isolated from the spleen of chronically SIV-infected RM.
(A) Viral DNA copies per million sorted TFH, TFR and TREG from spleens of unvaccinated chronically SIV-infected RM. (B) Percent of CCR5-expressing cells among TFH, TFR and TREG in unvaccinated SIV-infected RM. Statistical analyses were performed using Mann-Whitney U tests.
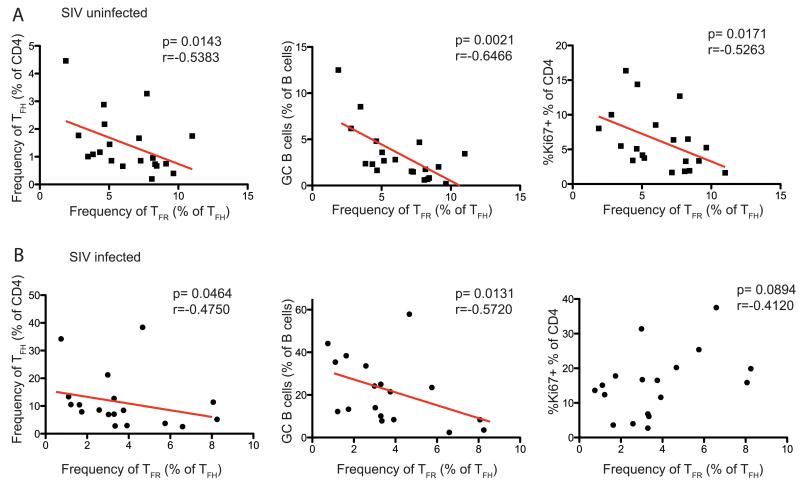
Figure 6. TFR frequencies negatively correlate with TFH and GC B-cell frequencies in the lymph nodes of RM.
Correlations between the frequencies of TFR (calculated as frequency of TFH) and the frequencies of TFH calculated as percent of total CD4+ T-cells (left) and GC B-cells calculated as percent of total B-cells (center) and proliferating (i.e., Ki67+) CD4+ T-cells (right) within the lymph nodes of SIV-uninfected (A) and chronically SIV-infected (B) RM. Statistical analyses were performed using Spearman rank correlation tests.
Results
TFR are distinct from TFH and TREG and can be found within lymph node GCs in RM
Recent studies of GC TFH have defined these cells based on their surface expression of the chemokine receptor CXCR5 and very high levels of the co-inhibitory receptor PD1 (10). However, a fraction of these canonically defined TFH also express the lineage-specific TREG marker FoxP3 and have been therefore defined as TFR as proposed in (22-24). Here we identified CD4+ TFR by flow cytometry by their co-expression of CXCR5, PD1, FoxP3 and CD25 within lymph nodes of uninfected RM. The gating strategy used to define TFH, TFR, and TREG throughout this study is shown in Figure 1A. Of note, the gating strategy for TREG cells includes both CXCR5+ and CXCR5− cells. To confirm the presence of TFR within GCs we conducted an immuno-histochemistry (IHC) analysis. As shown in Figure 1B, single cells with nuclear expression for FoxP3 and surface expression of and PD1 were identified with GCs of uninfected RM. These TFR can also be readily identified within GCs of SIV-infected RM (Fig 1C). Interestingly, several bonafide TREG, identified by their expression of FoxP3 and but not PD1, are visible in the T-cell zone just outside the GC (Fig 1C). Presumably, some of these TREG migrate into the GC and up-regulate TFH-like markers along their differentiation pathway to TFR. Figure 1C also shows that, as expected, non-FoxP3 expressing “true” TFH are also seen within GCs of the same animals.
TFR express markers of both TFH and TREG differentiation
We next performed a comprehensive examination of the TFR phenotype in healthy, SIV-uninfected RM. As shown in Figure 2, our analysis of relative mean fluorescence intensities (MFI) for TFR markers confirmed that TFR express FoxP3 and CD25 at comparable levels to TREG (Figure 2A) and both CXCR5 and PD1 at comparable levels to TFH (Figure 2B). We next examined in TFR the expression patterns of a series of markers (i.e., CD127, CTLA4, Bcl-6, and Helios) that have been linked to either TFH or TREG phenotype and function (1, 25). CD127, the IL-7 receptor α-chain, is expressed at low levels on TREG in humans (26), (27) (28). As expected, we find that TFR express CD127 at lower levels than the bulk of CD4+ T-cells, and similar or even lower levels than those observed in TREG and TFH (Figure 2C). CTLA4 is a key negative T-cell regulator that is constitutively expressed on TREG and, upon ligation, induces down-modulation of cytokine production and inhibition of cell-cycle progression (25). Consistent with previous reports in murine models (12), we observed that TFR express CTLA4 at a higher frequency and MFI than both TREG and TFH cell populations (Figure 2D), consistent with a putative role of TFR as negative regulators of GC responses. Helios is a transcription factor expressed in thymus-derived natural TREG cells (29). As shown in Figure 2F, TFR express Helios at levels that are even higher than those observed in TREG in terms of both frequency of positive cells and MFI, thus suggesting that TFR originate from natural TREG in RM as well as in mice.
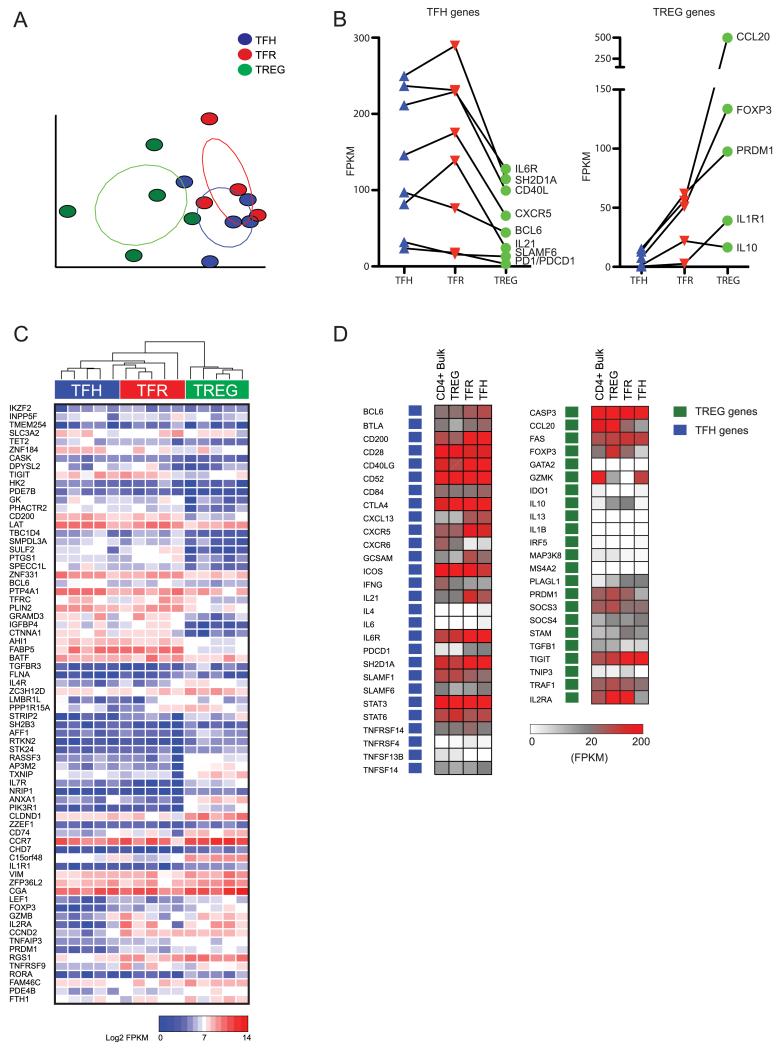
Transcriptome analysis of TFR reveals a distinct but overlapping transcriptional profile compared to TFH and TREG
To further define the functional features of TFR in RM, we next examined the transcriptional profiles of TFH, TFR and TREG using RNA-Seq by Illumina technology. Splenocytes from five healthy, SIV-uninfected and unvaccinated RM were sorted into “bulk” CD3+CD4+ T-cells, TREG, TFH and TFR based on the following phenotypic markers: TFR (CXCR5+PD1hiCD127−CD25+), TFH (CXCR5+PD1hiCD127+/−CD25−) and TREG (CXCR5+/−PD1lo/intCD127−CD25+). In mice, TFR are derived from thymic TREG precursors and acquire homing markers that allow them to traffic to GCs, while maintaining a transcriptome and suppressive function that most closely resembles TREG (12, 13). To examine the transcriptional profile of TFR relative to TREG and TFH in healthy, SIV-uninfected RM, we first performed principal component analysis (PCA) on a subset of the most highly expressed transcripts detected in TFH, TREG and TFR (Figure 3A). The transcriptomes of each subset were clearly distinct and grouped by subset, with TREG displaying the highest degree of intra-subset variability, and TFH and TFR subsets being more tightly distributed. We next compared the expression of several canonical TFH and TREG transcripts between the three subsets. As shown in Figure 3B-D, TFH- and TREG-related genes showed expression patterns that behaved as predicted with genes such as IL-10 expressed in TFR and TREG but absent in TFH. Importantly, RNA sequencing data confirmed that TFR share expression of TREG signature transcripts such as FoxP3, GZMB, PRDM1 and IL2RA (Figure 3A). However, we found that several other TREG-specific transcripts were expressed at lower levels in TFR than in TREG, including TRAF6, CD74, CCL20 and IL1R1. Similar to previous studies in mice, TFR also showed elevated expression of the prototypical TFH genes CXCR5, PD1/PDCD1, BCL-6, CXCL13, and ICOS. In fact, TFR demonstrated a peculiarly high expression of the TFH and TREG-specific genes Bcl-6 and FoxP3, respectively. Interestingly, for several genes (SH2D1A/SAP, IL-21, CXCR5, IL-10) gene expression was higher in TFR than either TREG or TFH, thus suggesting that the CD25+CXR5+PD1hi phenotype may represent a more transcriptionally active population than classical TREG or TFH. This latter set of RNA-sequencing data provides strong evidence that TFR are indeed a distinct cell subset and that the somewhat hybrid transcriptional profile of TFR is not simply due to the sample being a mixture of TREG and TFH. Of note, elevated expression of IL-10 in TFR compared to TREG has been previously reported in murine studies (13).
Figure 3. RNA expression patterns confirm that TFR share TFH and TREG like phenotype.
(A) Principal components analysis of RNA transcripts from five healthy, SIV-uninfected RM. Each circle represents the transcriptome of a sorted population of TFH (blue), TREG (green), or TFR (red) from a single animal. (B) Expression in FPKM of select TFH and TREG genes in sorted populations from uninfected RM. (C) Heat map of log 2 transformed gene expression of transcripts in FPKM. Transcripts represent TFH and TREG signature genes. The TFH gene signature was defined as transcripts that were significantly differentially expressed in sorted TFH compared to bulk CD4+ T-cells. TREG gene signature was defined as genes that were significantly differentially expressed in sorted TREG compared to bulk CD4+ T-cells. (D) Expression pattern of key TFH and TREG genes in sorted bulk CD4+ T-cell, TFH, TFR and TREG populations.
To then compare the profile of gene expression between TFR with TREG and TFH subsets without using any a priori information, we defined TFH and TREG expression signatures by statistically contrasting RNA-sequencing data from TFH and TREG with bulk CD4+ T-cells. After exclusion of transcripts that had zero expression in any of the populations, a total of 88 genes made up the combined TFH and TREG signature of which 12 genes were TREG related. Many, but not all, canonical TREG and TFH genes were also identified as significantly upregulated compared to bulk CD4+ T-cells. The lack of statistical significance for some prototypical transcripts is likely due to the presence TREG and TFH subsets within the bulk CD4+ population used as a comparator sample. Nevertheless, we found that TFR cells show similar levels of expression of TFH signature genes such as Bcl-6, TIGIT, CD200, LAT and BATF (Figure 3C). TFR cells also express mRNA for key TFH-related genes that are important for B-cell help, including IL-21, SH2D1A, CD40L and CD84. One notable difference between our data in RM and previously published mouse studies is that we observed high expression of IL-21 in TFR, suggesting that these cells have acquired some specific genomic and functional features in primates. As shown in Supplementary Figure 2A-C, the expression patterns of IL-21, SH2D1A, SLAMF6, PD1, IL6R, CCL20, IL2RA, IL10, PRDM1, and XIAP were confirmed by RT-PCR quantification. In addiction, levels of protein expression of IL-21 by TFR , TFH, and TREG were also measured by flow cytometry and further confirmed the pattern observed by RNA sequencing and RT-PCR (Supplementary Figure 2D).
SIV infection is associated with a decrease in the TFR/TFH ratio
The dynamics of TFR in the setting of HIV or SIV infection have not been previously investigated, and in fact all published studies of TFH dynamics during HIV/SIV infection used a definition of these cells that included TFR as well. To study the kinetics of TFR, TFH, and TREG following SIV infection of RM we measured the frequency of these cells within the lymph nodes prior to infection, 2 weeks post infection and 6 months post infection with SIVsmE660. The RM included in these kinetics analyses included both unvaccinated as well as animals that were challenged following immunization with a SIVmac239 Gag-, Pol-, and Env-expressing DNA vaccine (with or without GM-CSF) followed by two boosts of a SIV239 Gag-, Pol-, and Env-expressing MVA vaccine. As previously reported, we found a significant increase (p<0.0001) in frequency of TFH at 24 weeks post infection (Figure 4A). Interestingly, the frequency of TFR measured as percent of total CD4+ T-cells also showed a significant (p=0.0001) increase during chronic SIV infection (Figure 4A). However, when the frequency of TFR is measured as percentage of total TFH, we found that the TFR decrease significantly at both the acute (p=0.0385) and chronic (p=0.0016) stages of SIV infection (Figure 4B). Accordingly, the overall ratio of TFR to TFH cells also decreased significantly (p=0.0018) at the week 24 post-infection time point as compared to baseline (Figure 4C). The increase of both TFH and TFR as a percent of CD4+ T-cells after infection is likely the result of proliferation driven by antigen-persistence as well as virus-mediated depletion of other CD4+ T-cell subsets. However, the relative decrease in the frequency of TFR when measured as percentage of TFH suggests that the low frequency of these regulatory cells might contribute to the expansion and accumulation of TFH in chronically SIV-infected RM. Of note, we found no significant changes in TREG frequencies after SIV infection within the lymph nodes. To better define the kinetics of TFH and TFR during SIV infection we next measured the level of cell proliferation using the well-established marker Ki67. We observed that TFH show a significant increase in proliferating cells during the acute (p<0.0001) phase and chronic (p=0.0001) phase of infection (Figure 4D). TFR have a similar pattern of proliferation, with a significant increase in proliferating cells during the acute (p<0.0001) phase and chronic (p=0.0376) phase of infection (Figure 4D). In contrast, the level of Ki67 expression in TREG remains relatively low throughout our analysis with a small significant increase (p=0.0141) during the chronic phase of infection (Figure 4D).
Similar levels of SIV infection of TFR as compared to TFH and TREG despite higher CCR5 expression
Several studies have shown that, during HIV and SIV infection, TFH are highly infected with the virus despite their relative increase within the total CD4+ T-cell pool (9). While the actual in vivo lifespan of TFH, either infected or uninfected, remains unknown in the setting of HIV/SIV infection, the presence of a notable fraction of these cells expressing the proliferation marker Ki67 suggests that their number could be maintained through continual replenishing from precursors located outside the GC. To measure the level of direct SIV infection of TFR, TFH, and TREG we sorted these subpopulations from the lymph nodes of a subset of our studied animals and quantified the levels of total cell-associated SIV-DNA by RT-PCR. This analysis revealed that TFH, TFR and TREG derived from chronically SIV-infected RM all harbor comparably high levels of cell-associated viral DNA (Figure 5A). Interestingly, the levels of SIV infection were similarly high between TFR and TFH even though the surface expression levels of the main SIV co-receptor CCR5 were significantly higher in TFR as compared to TFH (Figure 5B).
The frequency of TFR is negatively correlated with the number and proliferation of both TFH and GC B-cells
To further examine the relationship between TFR and TFH and GC B-cells we next performed a set of correlation analyses in the RM included in this study, both SIV-infected and uninfected. We first observed that, in healthy uninfected RM, the frequency of TFR (as fraction of the total TFH pool) is negatively correlated with the percentages of TFH (as fraction of total CD4+ T-cells) and GC B-cells (as fraction of total B-cells) (Figure 6A). In addition, we found that, in the same animals, the frequency of TFR (as fraction of TFH) is negatively correlated with the level of CD4+ T-cell proliferation as measured by Ki67 expression (Figure 6A).
We next performed the same correlation analyses in our cohort of SIV-infected RM. The SIV-infected RM included in these regression analyses included both unvaccinated as well as animals that were challenged following immunization with a SIVmac239 Gag-, Pol-, and Env-expressing DNA vaccine (with or without GM-CSF) followed by two boosts of a SIV239 Gag-, Pol-, and Env-expressing MVA vaccine. In the SIV- infected RM, similar to what was observed in uninfected animals, the frequency of TFR (as fraction of TFH) is negatively correlated with the percentages of both TFH and GC B-cells (Figure 6B). However, the negative correlation between frequency of TFR (as fraction of TFH) and the level of CD4+ T-cell proliferation as measured by Ki67 expression is not seen in SIV-infected RM (Figure 6B). The negative correlation between TFR cells (as a frequency of TFH cells) and both TFH and GC B-cell frequencies is consistent with the hypothesis that TFR cells play a role in regulating TFH and GC responses under normal circumstances and in the setting of chronic SIV infection.
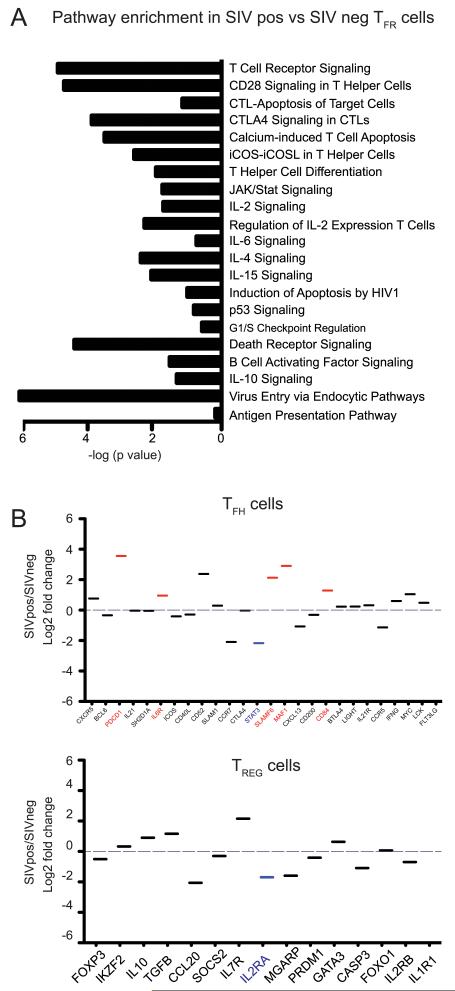
Comparative analysis of the TFR transcriptome in SIV-infected and uninfected RM
To further define the effect of SIV infection on TFR, we next compared the transcription profiles of TFR that were isolated from unvaccinated chronically SIV-infected and uninfected RM (Fig. 7). We performed RNA-Seq analysis and transcripts that were significantly differentially expressed in TFR sorted from SIV infected vs. uninfected RM were analyzed by Ingenuity Pathway Analysis. Unsurprisingly, a large proportion of genes induced during SIV infection in TFR (CD3G, FOS, CD4, ZAP70, PIK3CD, STAT3) were components of T-cell proliferation, activation of T-cell effector function, and co-stimulatory activation (data not shown). The enhanced T-cell activation was consistent with our observation that TFR cells express higher levels of the proliferation marker Ki67 compared to TREG (Figure 4D). We also observed that several genes implicated in pathways regulating apoptosis or cell cycle control were perturbed in SIV-infected RMs. Of particular interest was the observation that the pro-apoptotic gene FASLG was >100-fold induced, while the anti-apoptotic regulator XIAP was significantly down-regulated. This latter finding was again validated by RT-PCR (Supplementary Figure 2B). Thus, while we observed a significant increase of the proliferation marker Ki67 in TFR after SIV infection (Figure 4D), a pro-apoptotic shift of gene expression may explain why only a modest increase in TFR frequency was observed (Figure 4A).
Figure 7. RNA expression within TFR cells in uninfected and infected RM.
(A) Enrichment of gene pathways in TFR derived from the lymph nodes of unvaccinated SIV infected RM as compared to TFR from SIV-uninfected animals as determined by Ingenuity Pathway Analysis. (B) Log 2 fold change of expression of TFH and TREG related gene transcripts in TFR sorted from unvaccinated SIV-infected RM and SIV-uninfected RM. Significantly upregulated genes are in red and significantly down-regulated genes are in blue.
TFH require IL-6 signaling and STAT3 expression for differentiation and, once mature, produce several factors that support B-cell activation. Conversely, IL-2 receptor signaling drives STAT5 to activate Blimp1/PRDM1, which ultimately blocks TFH differentiation (30). However, TFR express both Blimp/PRDM1 and Bcl-6. Here we find that both IL-6 and IL-2 signaling genes are enriched in TFR after SIV infection. However, several of these genes, such as MAPK1, are common to different cytokine signaling pathways, thus making it difficult to establish if SIV infection causes a shift in the TFR/TFH differentiation pressure. Interestingly, downstream signaling for IL-10, a regulatory cytokine produced by both TFR and TREG, is also enriched in TFR post infection. Additionally, ICOS-ICOSL signaling was also enriched in TFR post infection. These data suggest that TFR may be engaged in similar TFH-like cell-surface receptor-ligand interactions with B-cells. In addition to genes that were identified with differential expression without any a priori knowledge, we also examined genes with known function in TFR and TREG. After infection, TFR cells show a significant increase in the expression of PD1, IL6R, SLAMF6 and CD84, i.e., all markers associated with TFH differentiation and function (Figure 7B). We also found a significant decrease in STAT3 and IL2RA in TFR after SIV infection and a non-significant decrease in Bcl-6 expression. Finally, as expected, we also observed several other changes in expression patterns of the TFH and TFR signature gene sets as we had previously determined (Supplementary Figure 1). Overall, these data indicate a complex remodeling of gene expression in TFR following SIV infection of RM.
Discussion
TFH cells are critical to the development of the humoral response to infections, and their role in the setting of HIV and SIV infection (and vaccination) is the subject of intense investigation. However, some aspects of the complex TFH response to HIV/SIV infection remain poorly understood, including (i) their role in promoting the development of broadly neutralizing HIV/SIV-specific antibodies, and (ii) their role in the immunopathogenesis of the infection. In particular, the mechanisms by which TFH accumulate during the chronic stage of infection despite high levels of direct virus infection are unclear. Importantly, a series of recent studies have shown that TFH include a subset of cells that are derived from thymic TREG precursors, express the classical TREG markers (i.e., FoxP3 and CD25 as well as low levels of CD127), and acquire TFH markers (i.e., PD1, CXCR5, and Bcl-6) while migrating into the GC of lymph nodes, where they are thought to act as regulators of the host humoral immune response. To the best of our knowledge this study-- together with the independently generated set of data that are included in the accompanying manuscript by the group of Dr. Franchini and Dr. Vaccari -- represents the first description of the main features of TFR in a non-human primate species. In this work we also investigated the dynamics of this cell subset during SIV infection of rhesus macaque (RM).
The main findings of the current study are the following: (i) TFR show distinct yet overlapping phenotype as compared to TFH and TREG based on a combination of flow cytometric, histological, and transcriptional analyses; (ii) in healthy, SIV-uninfected RM, the frequencies of TFR are negatively correlated with the levels of both TFH and GC B-cells; (iii) following SIV infection, the TFR/TFH ratio is reduced; and (iv) TFR sorted from SIV-infected RM harbor comparable levels of cell-associated viral DNA as compared to TFH and TREG. Collectively, these data indicate that while TFR closely resemble TFH in several biological aspects, they are also clearly distinguishable from this cell subset in terms of both their immunophenotype and transcriptional profile. It is therefore important that, in future studies of TFH, a distinction be made between TFR and true, “non-TFR” TFH to fully take into account the complexity of the different CD4+ T-cell subsets that are present in the GC of lymph nodes.
The observation that TFR express proteins typically expressed by TFH, such as CD40L, as well as proteins typically expressed by TREG, like IL-10 and CTLA4, is consistent with studies in mice showing that TFR are thymic-derived T regulatory (nTREG) cells that migrate into the follicle and, in a manner similar to TFH, up-regulate CXCR5, Bcl-6 and PD1 in a B-cell dependent manner (24). The production of IL-21 by TFR cells is an intriguing new finding and suggests that TFR play a more complex role in RMs than has been described in mice. In addition, PCA suggests that the transcriptional profile of TFR tend to be more similar to TFH than TREG. Further studies are required to fully investigate the functional role played by TFR in RMs and, specifically, in the context of SIV infection. The finding that over 90% of TFR express Helios as measured by flow cytometry is also consistent with the nTREG origin of these cells. Importantly, these immunophenotypic and RNA sequencing data were complemented by histological analyses showing that TFR are found within GCs of both uninfected and infected RM. While CD4+FoxP3+ TREG were found in abundance outside the GC, CD4+PD1+TFH and CD4+PD1+FoxP3+TFR were both only seen within the GC. The hypothesis that TFR play an immune regulatory role in vivo is supported by the observation that their frequency is inversely correlated with both the levels of TFH and GC B-cells. These data are consistent with mouse studies indicating that (i) TFR suppress TFH in vitro and prevent the outgrowth of non-antigen specific B-cells (13), and that (ii) TFR may inhibit antibody production without an effect on T-cell activation, thus indicating an ability to directly regulate B-cells(31).
In the setting of in vivo SIV infection, we found that TFR exhibited only a small increase in their frequency within the total CD4+ T-cell pool. In conjunction with the large expansion of TFH that is consistently observed following SIV infection, the minor expansion of TFR leads to a significantly decreased TFR/TFH ratio in the lymph nodes of chronically SIV-infected RM. We confirmed this trend in the ratio of TFR/TFH cells after SIV infection by quantifying the number of TFH and TFR cells by immunohistochemistry (Supplementary Table 1). While the current set of results does not allow us to determine whether and to what extent the kinetics of TFH and TFR during SIV infection are mechanistically linked, it is conceivable that the limited TFR expansion facilitates progressive accumulation of TFH in chronically SIV-infected RM, thus indirectly contributing to the aberrant immune activation that characterizes this pathogenic infection. On the other hand, it is also possible that the strong proliferation of TFH and associated increase in PD1 expression following SIV infection hampers the development or differentiation of TFR as suggested (31).
Comparison of the transcriptional profiles of TFR cells pre and post-SIV infection showed a significant up-regulation of transcripts typically expressed by activated TREG including FOSB, FABP5, USP2 and USP13 (data not shown) (32), thus suggesting that TFR may be involved in the generalized immune activation associated with pathogenic SIV infection. Interestingly, we also observed a down regulation of several TFH and TREG signature genes as established by our own algorithm. This somewhat unexpected observation indicates that SIV infection has a complex effect on the in vivo phenotype and function of TFR. A better understanding of the overall contribution of TFR to the immunopathogenesis of AIDS, in terms of causing either the virus-associated B-cell dysfunction or the changes in the lymph node architecture and function, will require further in vitro and in vivo investigation of the suppressive effect by these TFR on the function of either TFH or GC B-cells.
While CD4+ T-cells are the main target for HIV and SIV infection, substantial difference exist between various CD4+ T-cell subsets in terms of their relative levels of direct virus infection in vivo (33-35). In this study we tested the possibility that the decrease in the TFR/TFH ratio observed during SIV infection of RM was associated with higher level of virus infection in TFR as compared to TFH. However, our comparative analysis of the cell-associated viral burdens in sorted TFR, TFH, and TREG revealed similar levels of SIV-DNA in the three CD4+ T-cell subsets, even though TFR exhibited higher levels of the SIV co-receptor CCR5 as compared to the other two subsets.
In summary, the presented data provide the first comprehensive description of TFR in healthy, uninfected RM, as well as the first examination of the kinetics of these cells in the setting of pathogenic SIV infection. These results support the hypothesis that these cells play an important immune regulatory role in vivo, and that a relative decline of the TFR/TFH ratio may be involved in establishing a state of chronic immune activation in the B-cell areas of lymph nodes during pathogenic HIV and SIV infection.
Supplementary Material
Acknowledgements
We would like to thank Dr. Barbara Cervasi and Dr. Kiran Gill at the Flow Cytometry Core at Emory Vaccine Center and Dr. Prachi Sharma and Dr. Deepa Kodandera at the Molecular Pathology Core Lab. We would also like to thank the animal care and veterinary staff at the Yerkes National Primate Research Center.
This work was supported by National Institutes of Health Grant U19 AI096187, RR000165/OD011132 to the Yerkes National Primate Research Center and P30 AI050409 to the Emory Center for AIDS Research.
References
- 1.Pissani F, Streeck H. Emerging concepts on T follicular helper cell dynamics in HIV infection. Trends in immunology. 2014;35:278–286. doi: 10.1016/j.it.2014.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Corti D, Lanzavecchia A. Broadly neutralizing antiviral antibodies. Annual review of immunology. 2013;31:705–742. doi: 10.1146/annurev-immunol-032712-095916. [DOI] [PubMed] [Google Scholar]
- 3.Murphy MK, Yue L, Pan R, Boliar S, Sethi A, Tian J, Pfafferot K, Karita E, Allen SA, Cormier E, Goepfert PA, Borrow P, Robinson JE, Gnanakaran S, Hunter E, Kong XP, Derdeyn CA. Viral escape from neutralizing antibodies in early subtype A HIV-1 infection drives an increase in autologous neutralization breadth. PLoS pathogens. 2013;9:e1003173. doi: 10.1371/journal.ppat.1003173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Crotty S. Follicular helper CD4 T cells (TFH) Annual review of immunology. 2011;29:621–663. doi: 10.1146/annurev-immunol-031210-101400. [DOI] [PubMed] [Google Scholar]
- 5.Pratama A, Vinuesa CG. Control of TFH cell numbers: why and how? Immunology and cell biology. 2014;92:40–48. doi: 10.1038/icb.2013.69. [DOI] [PubMed] [Google Scholar]
- 6.Yang X, Yang J, Chu Y, Xue Y, Xuan D, Zheng S, Zou H. T follicular helper cells and regulatory B cells dynamics in systemic lupus erythematosus. PloS one. 2014;9:e88441. doi: 10.1371/journal.pone.0088441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ma CS, Deenick EK. Human T follicular helper (Tfh) cells and disease. Immunology and cell biology. 2014;92:64–71. doi: 10.1038/icb.2013.55. [DOI] [PubMed] [Google Scholar]
- 8.Vinuesa CG. HIV and T follicular helper cells: a dangerous relationship. The Journal of clinical investigation. 2012;122:3059–3062. doi: 10.1172/JCI65175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Perreau M, Savoye AL, De Crignis E, Corpataux JM, Cubas R, Haddad EK, De Leval L, Graziosi C, Pantaleo G. Follicular helper T cells serve as the major CD4 T cell compartment for HIV-1 infection, replication, and production. The Journal of experimental medicine. 2013;210:143–156. doi: 10.1084/jem.20121932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lindqvist M, van Lunzen J, Soghoian DZ, Kuhl BD, Ranasinghe S, Kranias G, Flanders MD, Cutler S, Yudanin N, Muller MI, Davis I, Farber D, Hartjen P, Haag F, Alter G, Schulze zur Wiesch J, Streeck H. Expansion of HIV-specific T follicular helper cells in chronic HIV infection. The Journal of clinical investigation. 2012;122:3271–3280. doi: 10.1172/JCI64314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Petrovas C, Koup RA. T follicular helper cells and HIV/SIV-specific antibody responses. Current opinion in HIV and AIDS. 2014;9:235–241. doi: 10.1097/COH.0000000000000053. [DOI] [PubMed] [Google Scholar]
- 12.Chung Y, Tanaka S, Chu F, Nurieva RI, Martinez GJ, Rawal S, Wang YH, Lim H, Reynolds JM, Zhou XH, Fan HM, Liu ZM, Neelapu SS, Dong C. Follicular regulatory T cells expressing Foxp3 and Bcl-6 suppress germinal center reactions. Nature medicine. 2011;17:983–988. doi: 10.1038/nm.2426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Linterman MA, Pierson W, Lee SK, Kallies A, Kawamoto S, Rayner TF, Srivastava M, Divekar DP, Beaton L, Hogan JJ, Fagarasan S, Liston A, Smith KG, Vinuesa CG. Foxp3+ follicular regulatory T cells control the germinal center response. Nature medicine. 2011;17:975–982. doi: 10.1038/nm.2425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lai L, Kwa S, Kozlowski PA, Montefiori DC, Ferrari G, Johnson WE, Hirsch V, Villinger F, Chennareddi L, Earl PL, Moss B, Amara RR, Robinson HL. Prevention of infection by a granulocyte-macrophage colony-stimulating factor co-expressing DNA/modified vaccinia Ankara simian immunodeficiency virus vaccine. The Journal of infectious diseases. 2011;204:164–173. doi: 10.1093/infdis/jir199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ortiz AM, Klatt NR, Li B, Yi Y, Tabb B, Hao XP, Sternberg L, Lawson B, Carnathan PM, Cramer EM, Engram JC, Little DM, Ryzhova E, Gonzalez-Scarano F, Paiardini M, Ansari AA, Ratcliffe S, Else JG, Brenchley JM, Collman RG, Estes JD, Derdeyn CA, Silvestri G. Depletion of CD4(+) T cells abrogates post-peak decline of viremia in SIV-infected rhesus macaques. The Journal of clinical investigation. 2011;121:4433–4445. doi: 10.1172/JCI46023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cartwright EK, McGary CS, Cervasi B, Micci L, Lawson B, Elliott ST, Collman RG, Bosinger SE, Paiardini M, Vanderford TH, Chahroudi A, Silvestri G. Divergent CD4+ T memory stem cell dynamics in pathogenic and nonpathogenic simian immunodeficiency virus infections. Journal of immunology. 2014;192:4666–4673. doi: 10.4049/jimmunol.1303193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vanderford TH, Slichter C, Rogers KA, Lawson BO, Obaede R, Else J, Villinger F, Bosinger SE, Silvestri G. Treatment of SIV-infected sooty mangabeys with a type-I IFN agonist results in decreased virus replication without inducing hyperimmune activation. Blood. 2012;119:5750–5757. doi: 10.1182/blood-2012-02-411496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Klatt NR, Shudo E, Ortiz AM, Engram JC, Paiardini M, Lawson B, Miller MD, Else J, Pandrea I, Estes JD, Apetrei C, Schmitz JE, Ribeiro RM, Perelson AS, Silvestri G. CD8+ lymphocytes control viral replication in SIVmac239-infected rhesus macaques without decreasing the lifespan of productively infected cells. PLoS pathogens. 2010;6:e1000747. doi: 10.1371/journal.ppat.1000747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sandler NG, Bosinger SE, Estes JD, Zhu RT, Tharp GK, Boritz E, Levin D, Wijeyesinghe S, Makamdop KN, del Prete GQ, Hill BJ, Timmer JK, Reiss E, Yarden G, Darko S, Contijoch E, Todd JP, Silvestri G, Nason M, Norgren RB, Jr., Keele BF, Rao S, Langer JA, Lifson JD, Schreiber G, Douek DC. Type I interferon responses in rhesus macaques prevent SIV infection and slow disease progression. Nature. 2014;511:601–605. doi: 10.1038/nature13554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dobin A, Davis CA, Schlesinger F, Drenkow J, Zaleski C, Jha S, Batut P, Chaisson M, Gingeras TR. STAR: ultrafast universal RNA-seq aligner. Bioinformatics. 2013;29:15–21. doi: 10.1093/bioinformatics/bts635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Trapnell C, Hendrickson DG, Sauvageau M, Goff L, Rinn JL, Pachter L. Differential analysis of gene regulation at transcript resolution with RNA-seq. Nature biotechnology. 2013;31:46–53. doi: 10.1038/nbt.2450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vinuesa CG, Cyster JG. How T cells earn the follicular rite of passage. Immunity. 2011;35:671–680. doi: 10.1016/j.immuni.2011.11.001. [DOI] [PubMed] [Google Scholar]
- 23.Alexander CM, Tygrett LT, Boyden AW, Wolniak KL, Legge KL, Waldschmidt TJ. T regulatory cells participate in the control of germinal centre reactions. Immunology. 2011;133:452–468. doi: 10.1111/j.1365-2567.2011.03456.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wollenberg I, Agua-Doce A, Hernandez A, Almeida C, Oliveira VG, Faro J, Graca L. Regulation of the germinal center reaction by Foxp3+ follicular regulatory T cells. Journal of immunology. 2011;187:4553–4560. doi: 10.4049/jimmunol.1101328. [DOI] [PubMed] [Google Scholar]
- 25.Wing JB, Sakaguchi S. Foxp3(+) T(reg) cells in humoral immunity. International immunology. 2014;26:61–69. doi: 10.1093/intimm/dxt060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liu W, Putnam AL, Xu-Yu Z, Szot GL, Lee MR, Zhu S, Gottlieb PA, Kapranov P, Gingeras TR, Fazekas de St Groth B, Clayberger C, Soper DM, Ziegler SF, Bluestone JA. CD127 expression inversely correlates with FoxP3 and suppressive function of human CD4+ T reg cells. The Journal of experimental medicine. 2006;203:1701–1711. doi: 10.1084/jem.20060772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Seddiki N, Santner-Nanan B, Martinson J, Zaunders J, Sasson S, Landay A, Solomon M, Selby W, Alexander SI, Nanan R, Kelleher A, Fazekas de St Groth B. Expression of interleukin (IL)-2 and IL-7 receptors discriminates between human regulatory and activated T cells. The Journal of experimental medicine. 2006;203:1693–1700. doi: 10.1084/jem.20060468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dunham RM, Cervasi B, Brenchley JM, Albrecht H, Weintrob A, Sumpter B, Engram J, Gordon S, Klatt NR, Frank I, Sodora DL, Douek DC, Paiardini M, Silvestri G. CD127 and CD25 expression defines CD4+ T cell subsets that are differentially depleted during HIV infection. Journal of immunology. 2008;180:5582–5592. doi: 10.4049/jimmunol.180.8.5582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Getnet D, Grosso JF, Goldberg MV, Harris TJ, Yen HR, Bruno TC, Durham NM, Hipkiss EL, Pyle KJ, Wada S, Pan F, Pardoll DM, Drake CG. A role for the transcription factor Helios in human CD4(+)CD25(+) regulatory T cells. Molecular immunology. 2010;47:1595–1600. doi: 10.1016/j.molimm.2010.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ray JP, Marshall HD, Laidlaw BJ, Staron MM, Kaech SM, Craft J. Transcription factor STAT3 and type I interferons are corepressive insulators for differentiation of follicular helper and T helper 1 cells. Immunity. 2014;40:367–377. doi: 10.1016/j.immuni.2014.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sage PT, Francisco LM, Carman CV, Sharpe AH. The receptor PD-1 controls follicular regulatory T cells in the lymph nodes and blood. Nature immunology. 2013;14:152–161. doi: 10.1038/ni.2496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Birzele F, Fauti T, Stahl H, Lenter MC, Simon E, Knebel D, Weith A, Hildebrandt T, Mennerich D. Next-generation insights into regulatory T cells: expression profiling and FoxP3 occupancy in Human. Nucleic acids research. 2011;39:7946–7960. doi: 10.1093/nar/gkr444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moreno-Fernandez ME, Zapata W, Blackard JT, Franchini G, Chougnet CA. Human regulatory T cells are targets for human immunodeficiency Virus (HIV) infection, and their susceptibility differs depending on the HIV type 1 strain. Journal of virology. 2009;83:12925–12933. doi: 10.1128/JVI.01352-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brenchley JM, Hill BJ, Ambrozak DR, Price DA, Guenaga FJ, Casazza JP, Kuruppu J, Yazdani J, Migueles SA, Connors M, Roederer M, Douek DC, Koup RA. T-cell subsets that harbor human immunodeficiency virus (HIV) in vivo: implications for HIV pathogenesis. Journal of virology. 2004;78:1160–1168. doi: 10.1128/JVI.78.3.1160-1168.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brenchley JM, Vinton C, Tabb B, Hao XP, Connick E, Paiardini M, Lifson JD, Silvestri G, Estes JD. Differential infection patterns of CD4+ T cells and lymphoid tissue viral burden distinguish progressive and nonprogressive lentiviral infections. Blood. 2012;120:4172–4181. doi: 10.1182/blood-2012-06-437608. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.