Abstract
Purpose
To study the feasibility of engineering conjunctival epithelial cell sheets on a temperature-responsive culture dish for ocular surface reconstruction.
Methods
Rabbit conjunctival epithelial cells (rCjECs) were cultured in DMEM/F-12 (1:1) medium. The morphology and phenotype of the rCjECs were confirmed with phalloidin staining, periodic acid–Schiff (PAS) staining, and immunocytochemistry. The rCjECs cultured on a temperature-responsive culture dish for 10 days produced confluent conjunctival epithelial cell sheets. Then, the phenotype, structure, and function of the conjunctival epithelial cell sheets were examined.
Results
The conjunctival epithelial cells were compact, uniform, and cobblestone shape. All cultured conjunctival epithelial cells were harvested as intact cell sheets by reducing the culture temperature to 20 °C. Conjunctival epithelial cells were stratified in four to five cell layers similar to the conjunctival epithelium. CCK-8 analysis, 5-bromo-2’-deoxyuridine (BrdU) staining, and the live and dead viability assay confirmed that viable proliferation cells were retained in the cell sheets. Immunohistochemistry for CK4, CK19, and MUC5AC showed the cell sheets still maintained characteristics of the conjunctival epithelium.
Conclusions
A temperature-responsive culture dish enables fabrication of viable conjunctival epithelial cell sheets with goblet cells and proliferative cells. Conjunctival epithelial cell sheets will be promising for reconstruction of the conjunctival epithelium.
Introduction
The ocular surface is a complex biologic continuum, covered by at least two types of epithelia: corneal and conjunctival. The conjunctival epithelium, a stratified nonkeratinizing epithelium (two to ten cell layers), covers the anterior scleral surface and the posterior surface of the eyelids, plays a critical role in maintaining the health of the ocular surface, and has the capacity to spontaneously reepithelialize upon slight injury [1,2]. However, this reepithelialization is usually accompanied by wound contracture and even culminates in corneal blindness, especially in serious ocular surface disorders, including Stevens-Johnson syndrome, ocular cicatricial pemphigoid, and thermal and chemical burns [3]. Therefore, the reconstruction of the conjunctival epithelium should be a priority condition for successful restoration of the ocular surface. Currently, different types of substitutes have been developed and studied for reconstruction of the ocular surface, including allografts and autografts from a healthy conjunctiva and oral mucous membrane [4], human amniotic membrane (AM) [4], and synthetic materials based on fibroin [5], collagen [6,7], etc. However, these materials are limited for numerous reasons. For example, autografts are restricted due to the shortage of healthy autologous tissue, and the application of allografts inevitably leads to the risk of allogenic rejection. Furthermore, the inflammatory reactions of synthetic matrices remain a problem. In recent years, cell sheet engineering using a temperature-responsive culture dish has been used in tissue engineering [8]. The surface of a temperature-responsive culture dish is covalently immobilized with a temperature-responsive polymer, poly (N-isopropylacrylamide; PIPAAm), which is hydrophobic at 37 °C, facilitating cell adhesion and proliferation. When the temperature decreases to the low critical solution temperature (LCST) of 32 °C, the polymer becomes hydrophilic, and a hydration layer is formed between the surface and the cells. Therefore, all confluent adhesion cells seeded on a temperature-responsive culture dish can be automatically separated from the dish surface by reducing the temperature, without using trypsin digestion. The cell sheets contain extracellular matrix (ECM), ion channels, growth factor receptors, and connexins [9,10]. Previously, cell sheet technology with a temperature-responsive culture dish has been successfully applied to various tissues, including the corneal epithelium [11], the esophageal mucosa [12], and the heart [13]. In this study, we employed a temperature-responsive culture dish to culture conjunctival epithelial cell sheets.
First, rabbit conjunctival epithelial cells (rCjECs) were cultured and identified, and then the rCjECs were seeded on a temperature-responsive culture dish. Cell morphology, phenotype, and proliferation, the viability of the conjunctival epithelial cell sheets, and the degree of stratification were examined.
Methods
Isolation and culture of rabbit conjunctival epithelial cells
All experimental procedures adhered to the guidelines of the Chinese Animal Administration and the Association for Research in Vision and Ophthalmology Statement for the use of animals in ophthalmic and vision research. The rCjECs were isolated and cultured as previously described [14]. Briefly, the conjunctiva originating from the palpebral and fornix regions of New Zealand white rabbits was carefully dissected. The entire sheet of conjunctival epithelial tissue was separated from the attaching Tenon’s tissue. The sheet was rinsed three times with PBS (1X; 130 mM NaCl, 3 mM KCl, 10 mM Na2HPO4, 2 mM KH2PO4, pH 7.4) containing 100 U/ml penicillin and then was incubated with Dispase II (2.4 units/ml; Sigma-Aldrich, St. Louis, MO) at 4 °C for 16 h. The detached epithelial layer was then scattered into single cells with 0.05% trypsin/EDTA for 10 min at 37 °C. The cells were then seeded on a cell culture dish (with I collagen coating, Millipore Corporation, Billerica, MA) in Dulbecco’s modified Eagle’s medium/Ham’s nutrient mixture F12 (1:1 DMEM/F12, Invitrogen, Carlsbad, CA) supplemented with 10% fetal bovine serum (FBS; HyClone Laboratories, Inc., Logan, UT), 5 μg/ml insulin, 5 μg/mL transferrin, 5 ng/ml selenium, 1% penicillin/streptomycin, 10 ng/ml human epidermal growth factor (hEGF; R&D Systems, Minneapolis, MN) and 100 ng/ml nerve growth factor (NGF; R&D Systems). After 2 days of culture, the non-adherent cells were removed by washing with PBS. When the adherent cells reached approximately 80% to 90% confluence, the cells were rendered single cells by trypsin/EDTA and subcultured for additional experiments.
Cell morphology and phenotype
The morphology of the rCjECs was viewed with phalloidin staining [15]. The subcultured cells were cultured on glass coverslips. When the cells reached 70% to 80% confluence, they were fixed with 4% paraformaldehyde (PFA; Sigma-Aldrich), permeabilized with 0.5% Triton X-100 (Sigma-Aldrich), and stained with Alexa Fluor 546 phalloidin (Life Technologies, Carlsbad, CA) for 30 min. The nuclei were counterstained with 4',6-diamidino-2-phenylindole dihydrochloride (DAPI, Life Technologies) for 30 min.
Periodic acid–Schiff (PAS) staining was performed for the detection and distribution of the mucosubstances [16]. When the subcultured cells cultured on glass coverslips reached 70% to 80% confluence, they were fixed with 4% PFA, and then the cells were stained using a PAS staining kit (Sigma-Aldrich) according to the manufacturer’s manual.
For the identification of the cell phenotype, immunocytochemistry staining was performed as described previously [17]. The subcultured cells were seeded onto glass coverslips, fixed with 4% PFA for 15 min, and permeabilized with 0.3% Triton X-100 in PBS. After blocking with 10% normal goat serum (Invitrogen), the cells were incubated with primary antibodies overnight at 4 °C: rabbit polyclonal anti-CK19 (1:200, Abcam, Cambridge, MA), mouse monoclonal anti-CK4 (1:200, Sigma-Aldrich), and mouse monoclonal anti-MUC5AC (1:200, Abcam). Subsequently, the samples were subjected to a fluorescent-labeled secondary antibodies (Alexa Fluor 546 goat anti-mouse/rabbit, BD Biosciences, San Jose, CA) for 1 h. The nuclei were counterstained with DAPI (Invitrogen, Molecular Probes, Eugene, OR). Negative control samples were processed in parallel but without a primary antibody. An Olympus BX51 (Tokyo, Japan) fluorescent microscope was used to capture the images.
Preparation of the temperature-responsive culture dish
A temperature-responsive culture dish was purchased from CellSeed (Tokyo, Japan). The 35-mm cell culture dish was first exposed to ultraviolet (UV) light for 30 min to disinfect the surface. A temperature-responsive polymer, PIPAAm, was grafted to the surfaces of the cell culture dish. For cell culture use, these surfaces were washed twice with PBS.
Preparation of the cell sheets
The subcultured cells were plated at a density of 1.0×107 cells/dish and cultured on the surface of a 35-mm temperature-responsive culture dish. After culture for 4 days, the cells reached confluence. The same number of cells was then seeded on the confluent cells and cultured for 6 days. The culture medium was removed, and a hydrophilically modified polyvinylidene fluoride (PVDF) membrane was placed over the cell sheet. Fresh medium was added to prevent dryness. The cell sheet was harvested from the culture dish by reducing the culture temperature to 20 °C for 30 min.
Cell proliferation and viability
To investigate cell proliferation, Cell Counting Kit-8 (CCK-8; Dojindo, Japan) assay and 5-bromo-2’-deoxyuridine (BrdU) staining were performed. Briefly, the conjunctival epithelial cell sheets were dissociated with trypsin-EDTA, and then the cells were seeded on 24-well plates at a density of 2×104 cell/well. After 1, 3, and 5 days of cell culture, the cells were washed with PBS and incubated with 10% of CCK-8 containing DMEM/F12. After incubation for 3 h, 200 μl DMEM/F12 containing CCK-8 was transferred to 96-well plates. The absorbance of each well was measured at 450 nm with a microplate reader (ELX800, BioTek, Winooski, VT) At least six samples were measured at each time point [18]. A BrdU label retention assay was also performed. Briefly, the conjunctival epithelial cell sheets were dissociated with trypsin-EDTA, and then the cells were seeded on glass coverslips at a density of 2×106 cell/well. After the cells were attached on the glass coverslips, they were then incubated with fresh DMEM/F12 medium containing with 10 μM BrdU (Sigma-Aldrich) for 4 h at 37 °C in a humidified 5% CO2 atmosphere. After fixation with 4% PFA, the samples were incubated with 2 N HCl at 37 °C for 1 h to denature the DNA, neutralized in 0.1 M borate buffer, permeabilized with 0.3% Triton X-100 in PBS, and blocked with normal goat serum. After overnight incubation at 4 °C with a rabbit anti-BrdU polyclonal antibody (1:200, Santa Cruz Biotechnology, Santa Cruz, CA), the cells were incubated with a fluorescent-labeled secondary antibody (Alexa Fluor 488 goat anti-rabbit, BD) for 1 h at room temperature in the dark. The nuclei were counterstained with DAPI (Invitrogen). The cells were imaged using an Olympus BX51 fluorescent microscope [19].
A Live/Dead® Viability/Cytotoxicity Kit (Life Technologies, Carlsbad, CA) was used to investigate cell viability in the conjunctival epithelial cell sheets. The staining was based on the differential permeability of live and dead cells. When the cells cultured on temperature-responsive culture dish reached confluence, the live cells were stained with green fluorescent calcein-acetoxymethyl ester (CAM), a cytoplasm stain, and dead cells were stained with red fluorescent ethidium homodimer-2 (EthD-2). A fluorescent microscope (Olympus BX51) was used to analyze the images of the cell staining patterns [20]. The number of live and dead cells (green and red fluorescence, respectively) was counted in three different areas.
Identification of goblet cells, histology, and immunostaining
After being cultured for 10 days, conjunctival epithelial cell sheets were harvested from the surface of the temperature-responsive culture dish by decreasing the culture temperature to 20 °C. Conjunctival epithelial cell sheets were embedded in Tissue-Tek optimum cutting temperature (OCT) compound (Sakura Seiki, Tokyo, Japan) and processed into 6 μm frozen sections on cryofilm. The samples were then stained with a PAS staining kit (Sigma-Aldrich) according to the manufacturer’s manual. Hematoxylin and eosin (H&E) staining was used to assess the degree of stratification of the conjunctival epithelial cells [21]. Briefly, the sections were fixed with 4% PFA at room temperature for 5 min, washed three times with distilled-deionized water (DDW), and then stained with H&E. Specific cell marker expression was visualized in the immunostaining experiments. Primary antibodies of CK4, CK19, and MUC5AC were used to stain the frozen sections of the conjunctival epithelial cell sheets. The biotin-conjugated secondary antibodies (4 mg/ml; Vector Laboratories, Burlingame, CA) were used to visualize the specific marker. Briefly, after fixation with 4% PFA for 30 min, the sections were blocked for 1 h in a blocking solution (PBS containing 10% (v/v) normal goat serum (Invitrogen), 0.3% Triton X-100 (Sigma-Aldrich), and 0.1% NaN3 (Sigma-Aldrich)) at room temperature for 1 h. After washing, the primary antibodies (CK4, CK19, and MUC5AC) at a dilution of 1:200 were incubated at 4 °C overnight. The next day, after extensive washing, the secondary antibody was incubated for 2 h at room temperature. Primary antibodies were not added in the negative control group. Positive control samples (native rabbit conjunctival tissue) were processed in parallel. The images were observed with a microscope (Olympus BX51).
Reverse transcription and qPCR
Total RNA was extracted from the conjunctival epithelial cell sheets using the RNeasy Mini Kit (Qiagen, Valencia, CA). The concentration and purity of the total RNA were determined spectrophotometrically at OD260 nm and OD280 nm. Quantitative-PCR (qPCR) analyses were performed with A260/A280 ratios between 1.9 and 2.1. cDNA was synthesized using a PrimeScriptTM RT reagent kit (TaKaRa, Dalian, China). qPCR was performed in a 20-μl solution containing a 10 μl reaction mixture, 1 μl cDNA, 2 μl primers (Table 1), and 7 μl ddH2O. The reaction was conducted using a 7500 Real-Time PCR Detection System (Applied Biosystems, Irvine, CA) and activated at 95 °C for 10 min and 40 cycles of amplification (15 s at 95 °C and 1 min at 60 °C). Each sample was tested in triplicate [22]. The Pfaffl method was used to analyze the relative gene expression [23]. Glyceraldehyde 3-phosphate dehydrogenase (GAPDH, endogenous control) was selected to normalize the gene expression.
Table 1. Primers used in qPCR studies.
| Genes | Accession number | Forward (5′-3′) | Reverse (5′-3′) | Annealing Temperature(°C) | Product size (base pairs) | |
|---|---|---|---|---|---|---|
| CK4 |
XM_008256495.1 |
CAACCTGAAGACCACCAAGA |
CAGAGTCTGGCACTGCTTT |
60 |
100 |
|
| MUC5AC |
XM_008253634.1 |
TGATGACCAACCAGGTCATTT |
GGGATGGTCACGTACATCTTG |
60 |
106 |
|
| GAPDH | NM_001082253 | GGTCGGAGTGAACGGATTT | TGTAGTGGAGGTCAATGAATGG | 60 | 113 | |
Statistical analyses
The experimental results were expressed as the mean ± the standard derivation (SD). All experiments were performed in triplicate unless otherwise specified. Statistical analyses were performed using a two-sample equal variance Student t test, and a p value of less than 0.05 was considered to be statistically significant.
Results
Morphology and phenotype of cultured rabbit conjunctival epithelial cells
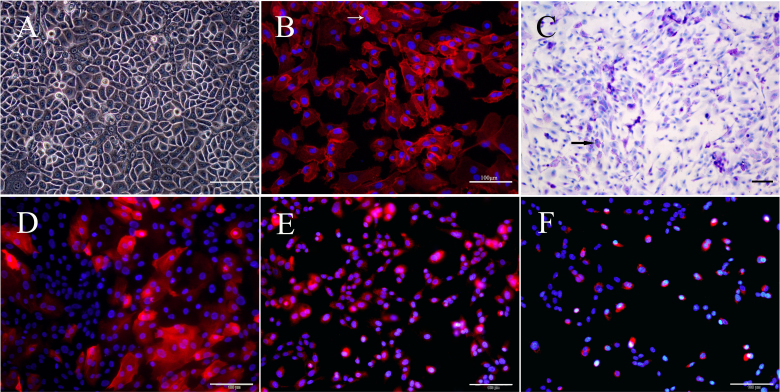
The confluent rCjECs appeared to be compact, uniform, tightly joined, and the typical cobblestone shape (Figure 1A). As observed in the phalloidin staining (Figure 1B), the majority of the cultured cells appeared to be non-goblet epithelial cells with a small squamous morphology; a few cells contained vesicles in the cytoplasm and had the typical shape of goblet cells. PAS staining showed that a few cells were strongly stained, indicating the presence of mucin-secreting goblet cells (Figure 1C).
Figure 1.
Morphology and characterization of rCjECs. Light microscopy showed the morphology of the rabbit conjunctival epithelial cells (rCjECs). A: Cells appear to be compact, uniform, and the typical cobblestone shape. Phalloidin staining for visualization of rCjEC morphology. Goblet cells contain secretory vesicles in the cytoplasm (the arrowhead indicates goblet cells). B: Mucins were detected with periodic acid–Schiff (PAS) staining (goblet cells are indicated by the arrowhead). C: Immunocytochemistry was performed to observe conjunctival epithelial-specific markers. D: CK4 for non-goblet cells. E: CK19 for non-goblet cells. F: MUC5AC for goblet cells. Nuclei were counterstained with 4',6-diamidino-2-phenylindole dihydrochloride (DAPI). Scale bars: 100 μm.
Immunofluorescence staining of CK4, CK19, and MUC5AC was used to identify the rCjECs. As shown in Figure 1D–F, the specific markers of these conjunctival epithelial cells were expressed in cultured cells, and the positive rate for MUC5AC-positive cells was approximately 21.5% ±1.65%. The results indicated that these cultured cells were conjunctival epithelial cells containing goblet cells.
Assessment of conjunctival epithelial cell sheets
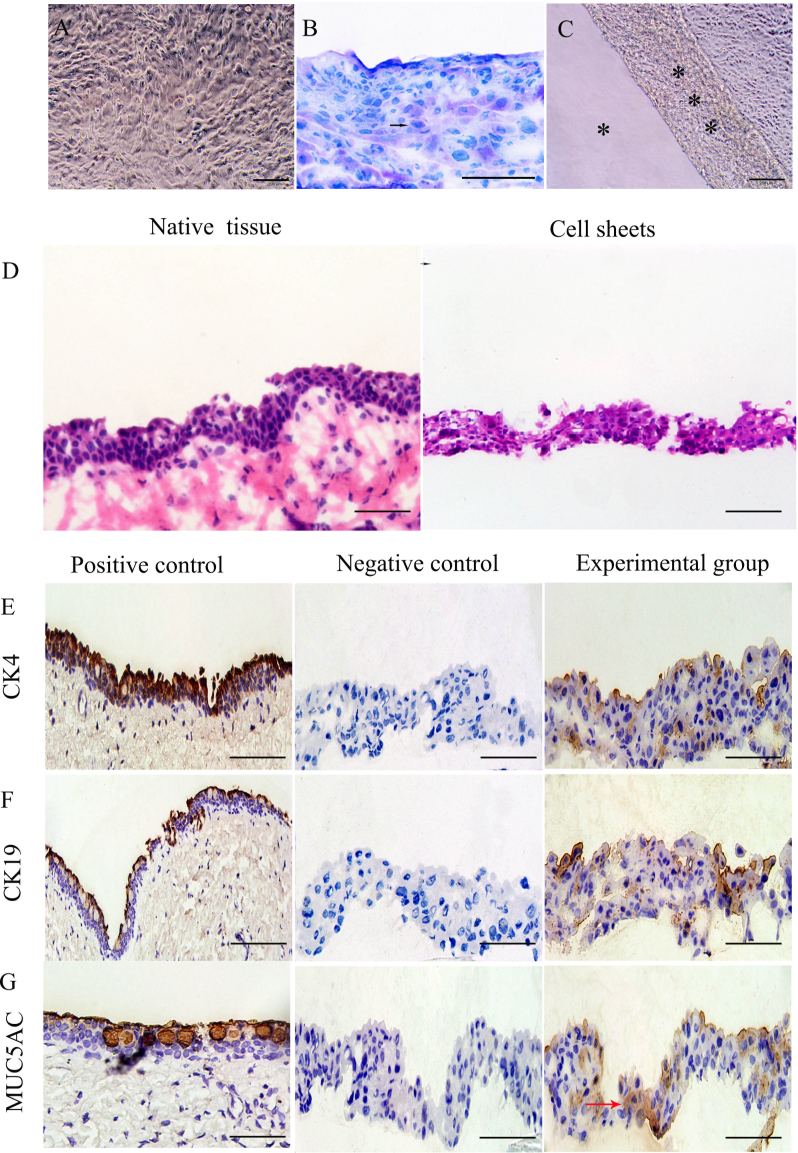
After the rCjECs were seeded and cultured on a temperature-responsive culture dish for 4 days, the attached cells reached confluence, and the morphology of the conjunctival epithelial cells remained (Figure 2A). As shown in Figure 2B, strong PAS staining was found in a few cells, indicating the presence of conjunctival goblet cells. The cell sheets were harvested as a contiguous cell sheet by reducing the temperature to 20 °C without using a digestive enzymatic treatment (Figure 2C). H&E staining showed that the conjunctival epithelial cell sheets displayed a coherent, stratified structure, which was approximately four to five cell layers similar to the native conjunctival epithelium (Figure 2D).
Figure 2.
Evaluation of conjunctival epithelial cell sheets fabricated with a temperature-responsive culture dish. A: Phase contrast microscopy showed that after culture for 4 days, the rabbit conjunctival epithelial cells (rCjECs) reached confluence. PAS staining in conjunctival epithelial cell sheets. The positive cells indicate the presence of goblet cells (arrowhead indicated goblet cells). B: Harvest of a conjunctival epithelial cell sheet. *** represents the cell sheets, * represents the culture surface (C). D: Hematoxylin and eosin (H&E) staining in conjunctival epithelial cell sheets. The result showed 4 to 5 cell layers. E, F: Immunohistochemical analysis of the cell sheets. CK4, CK19 staining for non-goblet cells. G: MUC5ac staining for goblet cells. Nuclei were counterstained with 4',6-diamidino-2-phenylindole dihydrochloride (DAPI). Scale bars: 200 μm in A, B, C, D; 100 μm in E, F, G.
To further study the cell sheets, immunohistochemistry was performed. As revealed in the immunostaining results (Figure 2E–G), the staining of CK4 and CK19, conjunctival putative specific cytokeratin, showed that numerous CK4-positive and CK19-positive cells were located on the conjunctival epithelial cell sheets. Examination of the MUC5AC staining showed that the goblet cells that occurred singly or in clusters were surrounded by conjunctival epithelial cells.
Proliferation and viability of conjunctival epithelial cells
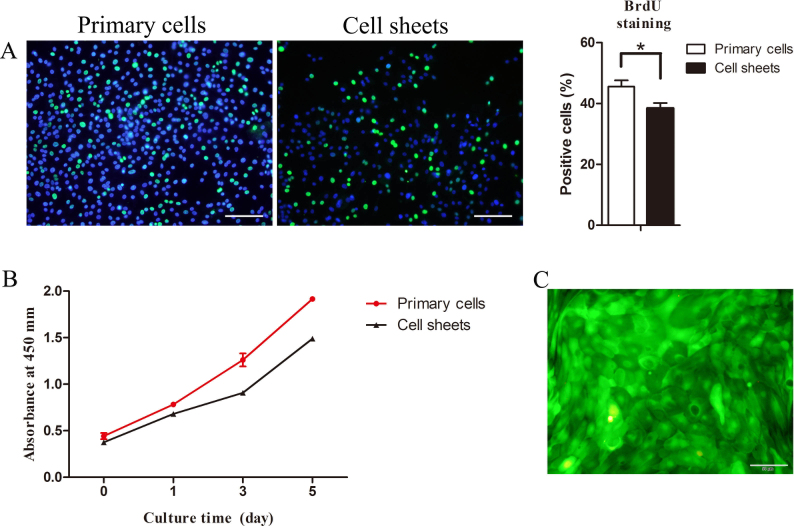
BrdU staining was performed to reflect the cell proliferation. As shown in Figure 3A, the immunofluorescence analysis of BrdU was positive in part of the cells, and the proliferation rate was approximately 38.4±1.75%, indicating the cell sheets cultured on the temperature-responsive culture dish maintained proliferative ability. CCK-8 analysis was performed to observe the proliferation of the cells. Figure 3B shows that the cells proliferated well, and the number of the cells increased with the duration of the culture, indicating that the cell sheets retained proliferative cells, similar to what was observed for the BrdU staining.
Figure 3.
Proliferation and viability of conjunctival epithelial cell sheets. 5-bromo-2´-deoxyuridine (BrdU) staining was performed to detected cell proliferation in the cell sheets, and the nuclei were stained with 4',6-diamidino-2-phenylindole dihydrochloride (DAPI: blue). A: The results show that the BrdU-positive cells (green) indicate the presence of the proliferative cells. The proliferation of the cells in conjunctival epithelial cell sheets was measured with a CCK-8 kit. B: The results show that rabbit conjunctival epithelial cells (rCjECs) proliferated well and the number of rCjECs increased with culture time, indicating that the cells in the cell sheets maintain proliferative cell properties. C: Live and dead staining in the conjunctival epithelial cell sheets. The results show that few dead cells can be seen. Scale bars: 100 μm in A, 50 μm in C.
Live and dead staining was used to evaluate the toxicity of the temperature-responsive culture dish. The results of the live and dead staining showed a low percentage of dead cells in the conjunctival epithelial cell sheets (Figure 3C).
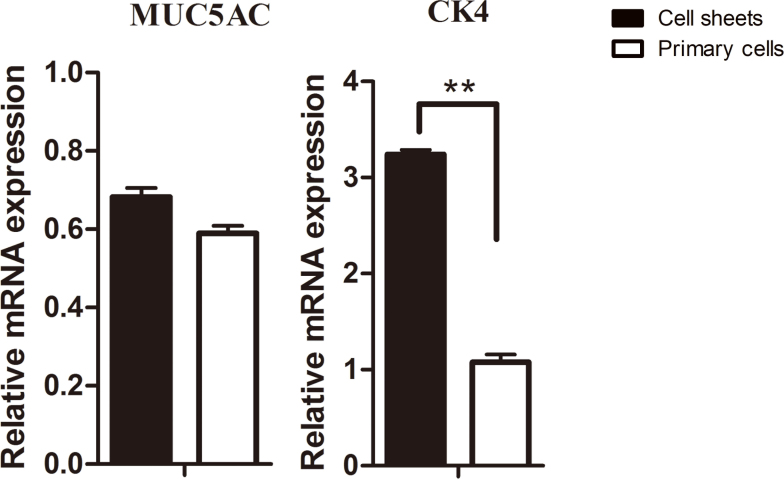
Gene expression
The putative specific gene expression levels of the rCjECs were examined with qPCR. With the extension of the culture time, the expression of CK4 mRNA was apparently increased in the conjunctival epithelial cell sheets, and the expression of MUC5AC mRNA, which was of the most interest to us, was not notably decreased (Figure 4). The results demonstrated that CK4 and MUC5AC mRNA were stably expressed in the conjunctival epithelial cell sheets, indicating that the temperature-responsive culture dish did not have a negative effect on the proliferation and differentiation of conjunctival cells, especially goblet cells.
Figure 4.
Gene expression. The expression of functional correlation genes was tested. The quantitative PCR (qPCR) results show that with the extension of the culture time, the expression of MUC5AC mRNA was not significantly decreased, and CK4 expression exhibits apparent increases in the conjunctival epithelial cell sheets. ** p≤0.01.
Discussion
In this study, we demonstrated the potential of a temperature-responsive culture dish for constructing multilayered conjunctival epithelium-like tissue, which could maintain the function of the normal conjunctival epithelium. The surface of the temperature-responsive culture dish did not have an adverse effect on cell viability, adhesion, and proliferation based on the results of the CCK-8 assay, BrdU staining, and live and dead staining. The temperature-responsive culture dish was chosen for the reconstruction of the conjunctival epithelium based on several considerations. First, cultured cells can be completely detached as intact cell sheets by reducing the culture temperature without typical proteolytic enzymes treatments. Cell damage is reduced, and ECM is retained, which greatly improved cell utilization and the biologic activity of the seeded cells [8,24]. Second, previous studies have demonstrated that cell sheet technology has been successfully used with various types of cells: corneal epithelial cells, oral mucosal epithelial cells, stem cells, and pluripotent stem-derived cells [11,25]. Third, traditional technology is limited for numerous reasons. For example, human AM is the most widely accepted substitute, but goblet cells cultured on AM do not regenerate [14,26]. Therefore, a temperature-responsive culture dish was used in this study.
Mucins play a critical role in the protection of the ocular surface, including lubrication and clearance of allergens and pathogens. MUC5AC is secreted mainly by goblet cells of the conjunctiva. Therefore, the number and secretory level of goblet cells are key hallmarks of the conjunctival epithelium’s function [27-29]. Previously, studies demonstrated that conjunctival epithelial cells cultured and subcultured in vitro are difficult to differentiate to goblet cells [15,30]. However, in the present study, the temperature-responsive culture dish supported the growth and phenotypic development of rCjECs, including goblet cells, as shown by gene expression, PAS staining, and immunohistochemistry. Cell differentiation largely depends on the surrounding environment, such as the ECM, and the temperature-responsive culture dish could make ECM cell layers more similar to normal tissue than that made by traditional technology [8,31]. Therefore, PIPAAm could support the growth and phenotypic development of goblet cells.
The live and dead staining showed that few dead cells could be seen on the temperature-responsive culture dish. This seems to be the natural mortality rate. CCK-8 assay and BrdU staining reflected indirectly that the cell sheets maintained a proliferative ability. This results indicate that a temperature-responsive culture dish is safe and nontoxic and does not have an adverse effect on cell proliferation and viability.
Numerous localizations have been suggested for the conjunctival epithelial stem and progenitor cells and goblet cells. Recently, several studies demonstrated that conjunctival epithelial stem and progenitor cells may preferentially reside in the palpebral and fornix conjunctiva by immunostaining with BrdU and several proposed stem and progenitor cell markers (△Np63α, ABCG2, and p63) [20,32,33]. Thus, in the current study, conjunctival tissue originating from the palpebral and fornix regions was cultured.
Previously, studies demonstrated that the temperature-responsive culture dish allows cultured cells to be harvested as a contiguous cell sheet. Furthermore, it was commonly accepted that the function of multilayered sheet cultured in vitro was higher than that of a monolayer sheet [10,34]. In this study, immunohistochemistry showed that CK4- and CK19-positive cells were located at the cell sheets, and MUC5AC-positive cells were surrounded by stratified epithelial cells. H&E staining showed that the conjunctival epithelial cell sheets formed a three-dimensional (3D) structure and became a thick conjunctival epithelium-like tissue, which was stratified in four to five cell layers, similar to the native conjunctival epithelium. Taken together, the temperature-responsive culture dish can be used for culturing conjunctival epithelium-like tissue.
In summary, we have demonstrated that a temperature-responsive culture dish can be used for culturing viable, well-differentiated, multilayered conjunctival epithelial cell sheets that contain goblet cells and proliferative cells, and the epithelial cell sheets can be harvested as an intact sheet by reducing the culture temperature. Additional studies are necessary to assess whether conjunctival epithelial cell sheets can be effectively applied to conjunctival epithelial defects in animal models in vivo.
ACKNOWLEDGMENTS
This work was supported by the National High Technology Research and Development Program (863 Program; 2015AA020311), National Natural Science Foundation of China (81370992), Shanghai Municipal Commission of Health and Family Planning Found (20144Y0221), and Shanghai Young Doctor Training Programme.
References
- 1.Hodges RRDA. Dartt. Tear film mucins: front line defenders of the ocular surface; comparison with airway and gastrointestinal tract mucins. Exp Eye Res. 2013;117:62–78. doi: 10.1016/j.exer.2013.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mason SL, Stewart RM, Kearns VR. R L WilliamsC M Sheridan. Ocular epithelial transplantation: current uses and future potential. Regen Med. 2011;6:767–82. doi: 10.2217/rme.11.94. [DOI] [PubMed] [Google Scholar]
- 3.Tanioka H, Kawasaki S, Yamasaki K, Ang LP, Koizumi N, Nakamura T, Yokoi N, Komuro A. T InatomiS Kinoshita. Establishment of a cultivated human conjunctival epithelium as an alternative tissue source for autologous corneal epithelial transplantation. Invest Ophthalmol Vis Sci. 2006;47:3820–7. doi: 10.1167/iovs.06-0293. [DOI] [PubMed] [Google Scholar]
- 4.Selvam S. P B ThomasS C Yiu. Tissue engineering: current and future approaches to ocular surface reconstruction. Ocul Surf. 2006;4:120–36. doi: 10.1016/s1542-0124(12)70039-3. [DOI] [PubMed] [Google Scholar]
- 5.Rama P, Bonini S, Lambiase A, Golisano O, Paterna P. M De LucaG Pellegrini. Autologous fibrin-cultured limbal stem cells permanently restore the corneal surface of patients with total limbal stem cell deficiency. Transplantation. 2001;72:1478–85. doi: 10.1097/00007890-200111150-00002. [DOI] [PubMed] [Google Scholar]
- 6.Hsu WC, Spilker MH. I V YannasP A Rubin. Inhibition of conjunctival scarring and contraction by a porous collagen-glycosaminoglycan implant. Invest Ophthalmol Vis Sci. 2000;41:2404–11. [PubMed] [Google Scholar]
- 7.Takezawa T, Ozaki K, Nitani A. C TakabayashiT Shimo-Oka. Collagen vitrigel: a novel scaffold that can facilitate a three-dimensional culture for reconstructing organoids. Cell Transplant. 2004;13:463–73. doi: 10.3727/000000004783983882. [DOI] [PubMed] [Google Scholar]
- 8.Chen T, Wang Y. L BuN Li. Construction of functional tissue-engineered bone using cell sheet technology in a canine model. Exp Ther Med. 2014;7:958–62. doi: 10.3892/etm.2014.1514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yan H. Tsujii. Thermo-responsive poly(N-isopropylacrylamide) gel containing polymeric surfactant poly(2-(methacryloyloxyl)decylphosphate): correlation between rapid collapsing characters and micelles of polymeric surfactant. J Oleo Sci. 2008;57:401–5. doi: 10.5650/jos.57.401. [DOI] [PubMed] [Google Scholar]
- 10.Takagi S, Shimizu T, Kuramoto G, Ishitani K, Matsui H. M YamatoT Okano. Reconstruction of functional endometrium-like tissue in vitro and in vivo using cell sheet engineering. Biochem Biophys Res Commun. 2014;446:335–40. doi: 10.1016/j.bbrc.2014.02.107. [DOI] [PubMed] [Google Scholar]
- 11.Hayashida Y, Nishida K, Yamato M, Watanabe K, Maeda N, Watanabe H, Kikuchi A. T OkanoY Tano. Ocular surface reconstruction using autologous rabbit oral mucosal epithelial sheets fabricated ex vivo on a temperature-responsive culture surface. Invest Ophthalmol Vis Sci. 2005;46:1632–9. doi: 10.1167/iovs.04-0813. [DOI] [PubMed] [Google Scholar]
- 12.Ohki T, Yamato M, Ota M, Takagi R, Murakami D, Kondo M, Sasaki R, Namiki H, Okano T, Yamamoto M. Prevention of esophageal stricture after endoscopic submucosal dissection using tissue-engineered cell sheets. Gastroenterology. 2012;143:582–8. doi: 10.1053/j.gastro.2012.04.050. [DOI] [PubMed] [Google Scholar]
- 13.Sawa Y, Miyagawa S, Sakaguchi T, Fujita T, Matsuyama A, Saito A. T ShimizuT Okano. Tissue engineered myoblast sheets improved cardiac function sufficiently to discontinue LVAS in a patient with DCM: report of a case. Surg Today. 2012;42:181–4. doi: 10.1007/s00595-011-0106-4. [DOI] [PubMed] [Google Scholar]
- 14.Meller D. V DabulS C Tseng. Expansion of conjunctival epithelial progenitor cells on amniotic membrane. Exp Eye Res. 2002;74:537–45. doi: 10.1006/exer.2001.1163. [DOI] [PubMed] [Google Scholar]
- 15.Zhou H, Lu Q, Guo Q, Chae J, Fan X. J H ElisseeffM P Grant. Vitrified collagen-based conjunctival equivalent for ocular surface reconstruction. Biomaterials. 2014;35:7398–406. doi: 10.1016/j.biomaterials.2014.05.024. [DOI] [PubMed] [Google Scholar]
- 16.Tian L, Qu M, Wang Y, Duan H, Di G. L XieQ Zhou. Inductive differentiation of conjunctival goblet cells by gamma-secretase inhibitor and construction of recombinant conjunctival epithelium. Exp Eye Res. 2014;123:37–42. doi: 10.1016/j.exer.2014.04.001. [DOI] [PubMed] [Google Scholar]
- 17.Hu Y, Ji J, Xia J, Zhao P, Fan X, Wang Z, Zhou X. M LuoP Gu. An in vitro comparison study: the effects of fetal bovine serum concentration on retinal progenitor cell multipotentiality. Neurosci Lett. 2013;534:90–5. doi: 10.1016/j.neulet.2012.11.006. [DOI] [PubMed] [Google Scholar]
- 18.He X, Fu W, Feng B, Wang H, Liu Z, Yin M. W WangJ Zheng. Electrospun collagen-poly(L-lactic acid-co-epsilon-caprolactone) membranes for cartilage tissue engineering. Regen Med. 2013;8:425–36. doi: 10.2217/rme.13.29. [DOI] [PubMed] [Google Scholar]
- 19.Ni N, Zhang D, Xie Q, Chen J, Wang Z, Deng Y, Wen X, Zhu M, Ji J, Fan X. M LuoP Gu. Effects of let-7b and TLX on the proliferation and differentiation of retinal progenitor cells in vitro. Sci Rep. 2014;4:6671. doi: 10.1038/srep06671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Eidet JR, Utheim OA, Raeder S, Dartt DA, Lyberg T, Carreras E, Huynh TT, Messelt EB, Louch WE. B RoaldT P Utheim. Effects of serum-free storage on morphology, phenotype, and viability of ex vivo cultured human conjunctival epithelium. Exp Eye Res. 2012;94:109–16. doi: 10.1016/j.exer.2011.11.015. [DOI] [PubMed] [Google Scholar]
- 21.Nakajima R, Kobayashi T, Kikuchi T, Kitano Y, Watanabe H, Mizutani M, Nozaki T, Senda N, Saitoh K, Takagi R, Yamato M. T OkanoS Takeda. Fabrication of transplantable corneal epithelial and oral mucosal epithelial cell sheets using a novel temperature-responsive closed culture device. J Tissue Eng Regen Med. 2015 doi: 10.1002/term.1728. [DOI] [PubMed] [Google Scholar]
- 22.Zhao P, Deng Y, Gu P, Wang Y, Zhou H, Hu Y. P ChenX Fan. Insulin-like growth factor 1 promotes the proliferation and adipogenesis of orbital adipose-derived stromal cells in thyroid-associated ophthalmopathy. Exp Eye Res. 2013;107:65–73. doi: 10.1016/j.exer.2012.11.014. [DOI] [PubMed] [Google Scholar]
- 23.Pfaffl MW. A new mathematical model for relative quantification in real-time RT-PCR. Nucleic Acids Res. 2001;29:e45. doi: 10.1093/nar/29.9.e45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shimizu T, Yamato M. A KikuchiT Okano. Cell sheet engineering for myocardial tissue reconstruction. Biomaterials. 2003;24:2309–16. doi: 10.1016/s0142-9612(03)00110-8. [DOI] [PubMed] [Google Scholar]
- 25.Nishida K, Yamato M, Hayashida Y, Watanabe K, Maeda N, Watanabe H, Yamamoto K, Nagai S, Kikuchi A. Y TanoT Okano. Functional bioengineered corneal epithelial sheet grafts from corneal stem cells expanded ex vivo on a temperature-responsive cell culture surface. Transplantation. 2004;77:379–85. doi: 10.1097/01.TP.0000110320.45678.30. [DOI] [PubMed] [Google Scholar]
- 26.Meller D. Tseng. Conjunctival epithelial cell differentiation on amniotic membrane. Invest Ophthalmol Vis Sci. 1999;40:878–86. [PubMed] [Google Scholar]
- 27.Mantelli F. Argueso. Functions of ocular surface mucins in health and disease. Curr Opin Allergy Clin Immunol. 2008;8:477–83. doi: 10.1097/ACI.0b013e32830e6b04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chung SH, Lee JH, Yoon JH. H K LeeK Y Seo. Multi-layered culture of primary human conjunctival epithelial cells producing MUC5AC. Exp Eye Res. 2007;85:226–33. doi: 10.1016/j.exer.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 29.Li W, Sun X, Wang Z. R LiL Li. The effect of nerve growth factor on differentiation of corneal limbal epithelial cells to conjunctival goblet cells in vitro. Mol Vis. 2010;16:2739–44. [PMC free article] [PubMed] [Google Scholar]
- 30.Ray Jui-Fang Tsai Scheffer C. G. TsengJ-K Chen. <Conjunctival epithelial cells in culture-growth and globlet cell differentiation.pdf>. Prog Retin Eye Res. 1997;16:227–41. [Google Scholar]
- 31.Elisseeff J, Ferran A, Hwang S. S VargheseZ Zhang. The role of biomaterials in stem cell differentiation: applications in the musculoskeletal system. Stem Cells Dev. 2006;15:295–303. doi: 10.1089/scd.2006.15.295. [DOI] [PubMed] [Google Scholar]
- 32.Sapkota K, Franco S. P SampaioM Lira. Goblet cell density association with tear function and ocular surface physiology. Cont Lens Anterior Eye. 2015 doi: 10.1016/j.clae.2015.01.016. [DOI] [PubMed] [Google Scholar]
- 33.Su L, Cui H, Xu C, Xie X. Q ChenX Gao. Putative rabbit conjunctival epithelial stem/progenitor cells preferentially reside in palpebral conjunctiva. Curr Eye Res. 2011;36:797–803. doi: 10.3109/02713683.2011.593727. [DOI] [PubMed] [Google Scholar]
- 34.Geng W, Ma D, Yan X, Liu L, Cui J, Xie X. H LiF Chen. Engineering tubular bone using mesenchymal stem cell sheets and coral particles. Biochem Biophys Res Commun. 2013;433:595–601. doi: 10.1016/j.bbrc.2013.03.034. [DOI] [PubMed] [Google Scholar]