Abstract
Despite recent advances in understanding of the pathobiology and targeted treatments of pulmonary arterial hypertension (PAH), epidemiologic data from large populations have been limited to western countries. The aim of the Korean Registry of Pulmonary Arterial Hypertension (KORPAH) was to examine the epidemiology and prognosis of Korean patients with PAH. KORPAH was designed as a nationwide, multicenter, prospective data collection using an internet webserver from September 2008 to December 2011. A total of 625 patients were enrolled. The patients' mean age was 47.6 ± 15.7 yr, and 503 (80.5%) were women. The diagnostic methods included right heart catheterization (n = 249, 39.8%) and Doppler echocardiography (n = 376, 60.2%). The etiologies, in order of frequency, were connective tissue disease (CTD), congenital heart disease, and idiopathic PAH (IPAH) (49.8%, 25.4%, and 23.2%, respectively). Patients with WHO functional class III or IV at diagnosis were 43.4%. In total, 380 (60.8%) patients received a single PAH-specific treatment at the time of enrollment, but only 72 (18.9%) patients received combination therapy. Incident cases during the registry represented 297 patients; therefore, the incidence rate of PAH was 1.9 patients/yr/million people. The 1st-, 2nd-, and 3rd-yr estimated survival rates were 90.8%, 87.8%, and 84.4%, respectively. Although Korean PAH patients exhibited similar age, gender, and survival rate compared with western registries, they showed relatively more CTD-PAH in the etiology and also systemic lupus erythematosus among CTD-PAH. The data suggest that earlier diagnosis and more specialized therapies should be needed to improve the survival of PAH patients.
Graphical Abstract
Keywords: Hypertension, Pulmonary; Pulmonary Arterial Hypertension; Prognosis; Korean
INTRODUCTION
Pulmonary arterial hypertension (PAH) is characterized by remodeling of the small pulmonary arteries leading to a progressive increase in pulmonary vascular resistance (PVR), right ventricular failure and death (1,2,3,4). The diagnosis and management of PAH has undergone significant change since the National Institutes of Health (NIH) conducted the first registry of primary pulmonary hypertension in the early 1980s (5,6). According to the last update at the 5th World Symposium on Pulmonary Hypertension, PAH, or group 1 pulmonary hypertension (PH), includes idiopathic PH, inherited PH, and PH associated with other conditions or diseases, such as connective tissue disease, congenital heart disease, portal hypertension, HIV infection, and exposure to toxins and drugs (7). Even with increased physician awareness and the relatively recent therapeutic developments, PAH remains an incurable and eventually fatal disease.
From 2006 to 2007, the Registry to EValuate Early And Long-term PAH disease management (REVEAL) study in the United States provided us with important basic data on the epidemiology, clinical characteristics, and prognosis of PAH (8,9,10). However, it is not known whether the results of these studies can be extended to different races, such as East Asian. The Korean Registry of Pulmonary Arterial Hypertension (KORPAH) was initiated to obtain additional insight into the incidence, prevalence, epidemiology, therapeutic modalities and survival data of Korean patients with PAH.
MATERIALS AND METHODS
Patients
This registry was designed as a multicenter, prospective data collection center using a common internet webserver. In January 2008, a task force team was formulated from 4 academic societies in Korea (The Korean Academy of Tuberculosis and Respiratory Diseases, The Korean Society of Cardiology, Korean College of Rheumatology, and The Korean Pediatric Heart Society) to create a common diagnostic protocol and webserver for the registry. Thirty-five university hospitals and tertiary hospitals in South Korea participated in this registry. When a patient with suspected pulmonary hypertension (PH) presented to the hospital, a series of investigations was performed to confirm the diagnosis, determine the World Health Organization (WHO) group, and evaluate the functional and hemodynamic impairment. According to the update guidelines (7), PAH or Group 1 PH was defined as a mean pulmonary artery pressure (PAP) >25 mmHg and a mean pulmonary capillary wedge pressure (PCWP) <15 mmHg by right heart catheterization (RHC). When RHC could not be performed, Doppler echocardiography was used to confirm the diagnosis. The diagnostic criteria by Doppler echocardiography were as follows: pulmonary artery systolic pressure (PASP) >40 mmHg calculated using a maximal systolic velocity (Vmax) of tricuspid regurgitation (TR) jet; mean PAP >25 mmHg calculated based on the acceleration time of the pulse Doppler spectral wave (PW) on the right ventricular outflow track (RVOT); and normal LV systolic and diastolic function and normal left arterial (LA) volume.
When the patients were confirmed to have PAH, a specific etiology of PAH was also determined by well-established algorithms (7). Patients with Group 2 PH (PH owing to left heart diseases), Group 3 PH (PH owing to lung diseases), Group 4 PH (PH owing to chronic pulmonary thromboembolism), and Group 5 PH (PH with unclear multifactorial mechanisms), as well as those who refused to be included, were excluded from the registry.
Data collection
When a patient was diagnosed and agreed to be included in the study, all of the patient data were input by individual investigators into the webserver (http://www.korpah.or.kr). The following baseline demographics were collected: age at diagnosis, gender, specific etiology of PAH, past medical history, date of confirmation, blood pressure, WHO functional class, electrocardiography, chest radiography, laboratory examinations (including serum brain natriuretic peptide [BNP, pg/mL) or N-terminal proBNP [NT-proBNP, pg/mL]), pulmonary function test results (including diffusion capacity for carbon monoxide [DLCO]), 6-min walking distance (6MWD, meters), comorbid conditions and treatment modalities. RHC parameters were also collected, including mean pulmonary artery pressure (mPAP, mmHg), mean pulmonary capillary wedge pressure (mPCWP, mmHg), mean right arterial pressure (mRAP, mmHg), pulmonary vascular resistance index (PVRI, Wood U*m2), cardiac index (CI, L/min*m2), and mixed venous oxygen saturation (SvO2, %).
Doppler echocardiographic indices such as peak tricuspid regurgitation velocity (TR Vmax, m/sec) of the tricuspid annulus, time velocity integral (TVI, cm) and acceleration time (msec) of the pulse wave spectral wave signal of the right ventricular outflow track were measured. From these Doppler data, pulmonary artery systolic pressure (PASP, mmHg), mean pulmonary artery pressure (mPAP, mmHg) and pulmonary vascular resistance (PVR, WU) were derived. Inferior vena cava (IVC) diameter with/without respiratory variation, pericardial effusion and tricuspid annular plane systolic excursion (TAPSE, mm) were also recorded. Follow-up clinical data and Doppler echocardiographic data were regularly recorded in every 6-12 months. When a clinical event (death or re-hospitalization) occurred, the date and cause of the event were updated on the webserver.
Statistical analysis
To describe the baseline characteristics and co-morbid conditions of all the KORPAH patients and incident PAH cases, we used frequency (proportion) for categorical variables and means ± standard deviations for continuous variables. The denominator for proportion was based on the number of patients with complete data. To compare baseline characteristics according to subgroups of PAH (idiopathic pulmonary arterial hypertension [IPAH] or acquired pulmonary arterial hypertension [APAH]) and WHO functional classes (less than class II or more than class III) in the KORPAH patients, we used the independent t-test or Wilcoxon rank sum test for continuous variables and the chi-square test for categorical variables. In the KORPAH patients diagnosed by RHC, diagnostic RHC parameters such as mPAP, PCWP, mRAP, PVRI, and SvO2 were compared between IPAH and APAH patients using the independent t-test. Survival rates from enrollment among newly diagnosed PAH patients were calculated using the life-table method. We conducted log-rank tests to compare survival rates according to PAH subgroups (IPAH, congenital heart disease [CHD], and connective tissue disease [CTD]). To assess the factors associated with mortality among newly diagnosed PAH patients, hazard ratios and 95% confidence intervals were calculated using the Cox's proportional hazard model. Univariate analysis was conducted, and the multivariate Cox's proportional hazard model was used to adjust for confounding variables. We used SAS 9.3.1 (SAS Institute, Cary, NC, USA) for all statistical analyses, and P values less than 0.05 were considered significant.
Ethics statements
The protocol of the KORPAH was reviewed and approved by the institutional review board of each participating hospital (hospital of corresponding author: KC13RIMI0384). The need for informed consent was exempted by the board. Audit processes were performed by an independent investigator to validate the diagnosis of PAH and the precision of the data.
RESULTS
Demographics and baseline characteristics of all patients
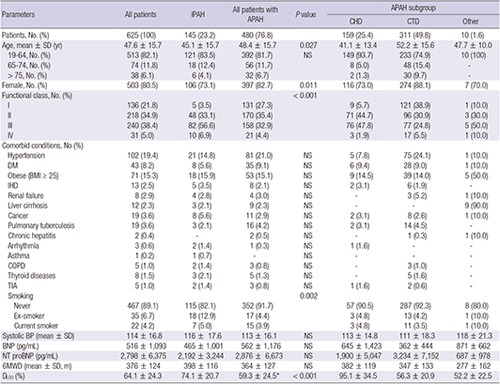
From September 2008 to December 2011, a total of 625 consecutive patients with WHO group 1 PH or PAH were enrolled in the registry. In total, 249 (39.8%) patients met the study entry criteria of RHC, and 376 (60.2%) patients met those of Echo. The baseline characteristics and comorbid conditions of all patients and their respective percentages according to the specific etiologies are summarized in Table 1. Of all 625 patients, the mean age at enrollment was 47.6±15.7 yr. In total, 112 patients (17.9%) were older than 65 yr, and there were 503 female patients (80.5%). The most common etiology of PAH was CTD (n=311, 49.8%), followed by CHD (n=159, 25.4%) and IPAH (n=145, 23.2%). Approximately 19.4% of patients had essential hypertension, 8.2% had diabetes, 15.3% were obese and only 4.2% were current smokers. WHO functional classes II, III, and IV corresponded to 218 (34.9%), 240 (38.4%), and 31 patients (5.0%), respectively. Systolic blood pressure, BNP or NT-proBNP, and 6-min walking distances were not significantly different between the IPAH and APAH patients. However, DLCO was significantly lower in APAH patients (P=0.001). Table 2 presents the characteristics according to the WHO functional class at enrollment. IPAH patients exhibited a more severe functional class than other subtypes, whereas CTD patients exhibited a less severe functional class (P<0.001). There were significant differences in 6MWD or NT-proBNP between functional classes I/II and III/IV (P<0.001). Functional class III or IV patients were more frequently treated by PAH-specific single or combination treatments. Conversely, functional class I or II patients were more frequently treated by conventional drugs such as diuretics and warfarin.
Table 1. Baseline characteristics and comorbid conditions of KORPAH patients.
| Parameters | All patients | IPAH | All patients with APAH | P value | APAH subgroup | ||
|---|---|---|---|---|---|---|---|
| CHD | CTD | Other | |||||
| Patients, No. (%) | 625 (100) | 145 (23.2) | 480 (76.8) | 159 (25.4) | 311 (49.8) | 10 (1.6) | |
| Age, mean ± SD (yr) | 47.6 ± 15.7 | 45.1 ± 15.7 | 48.4 ± 15.7 | 0.027 | 41.1 ± 13.4 | 52.2 ± 15.6 | 47.7 ± 10.0 |
| 19-64, No. (%) | 513 (82.1) | 121 (83.5) | 392 (81.7) | NS | 149 (93.7) | 233 (74.9) | 10 (100) |
| 65-74, No. (%) | 74 (11.8) | 18 (12.4) | 56 (11.7) | 8 (5.0) | 48 (15.4) | - | |
| > 75, No. (%) | 38 (6.1) | 6 (4.1) | 32 (6.7) | 2 (1.3) | 30 (9.7) | - | |
| Female, No. (%) | 503 (80.5) | 106 (73.1) | 397 (82.7) | 0.011 | 116 (73.0) | 274 (88.1) | 7 (70.0) |
| Functional class, No. (%) | < 0.001 | ||||||
| I | 136 (21.8) | 5 (3.5) | 131 (27.3) | 9 (5.7) | 121 (38.9) | 1 (10.0) | |
| II | 218 (34.9) | 48 (33.1) | 170 (35.4) | 71 (44.7) | 96 (30.9) | 3 (30.0) | |
| III | 240 (38.4) | 82 (56.6) | 158 (32.9) | 76 (47.8) | 77 (24.8) | 5 (50.0) | |
| IV | 31 (5.0) | 10 (6.9) | 21 (4.4) | 3 (1.9) | 17 (5.5) | 1 (10.0) | |
| Comorbid conditions, No (%) | |||||||
| Hypertension | 102 (19.4) | 21 (14.8) | 81 (21.0) | NS | 5 (7.8) | 75 (24.1) | 1 (10.0) |
| DM | 43 (8.2) | 8 (5.6) | 35 (9.1) | NS | 6 (9.4) | 28 (9.0) | 1 (10.0) |
| Obese (BMI ≥ 25) | 71 (15.3) | 18 (15.9) | 53 (15.1) | NS | 9 (14.5) | 39 (14.0) | 5 (50.0) |
| IHD | 13 (2.5) | 5 (3.5) | 8 (2.1) | NS | 2 (3.1) | 6 (1.9) | - |
| Renal failure | 8 (2.9) | 4 (2.8) | 4 (3.0) | NS | - | 3 (5.2) | 1 (10.0) |
| Liver cirrhosis | 12 (2.3) | 3 (2.1) | 9 (2.3) | NS | - | - | 9 (90.0) |
| Cancer | 19 (3.6) | 8 (5.6) | 11 (2.9) | NS | 2 (3.1) | 8 (2.6) | 1 (10.0) |
| Pulmonary tuberculosis | 19 (3.6) | 3 (2.1) | 16 (4.2) | NS | 2 (3.1) | 14 (4.5) | - |
| Chronic hepatitis | 2 (0.4) | - | 2 (0.5) | NS | - | 1 (0.3) | 1 (10.0) |
| Arrhythmia | 3 (0.6) | 2 (1.4) | 1 (0.3) | NS | 1 (1.6) | - | - |
| Asthma | 1 (0.2) | 1 (0.7) | - | NS | - | - | - |
| COPD | 5 (1.0) | 2 (1.4) | 3 (0.8) | NS | - | 3 (1.0) | - |
| Thyroid diseases | 8 (1.5) | 3 (2.1) | 5 (1.3) | NS | - | 5 (1.6) | - |
| TIA | 5 (1.0) | 2 (1.4) | 3 (0.8) | NS | 1 (1.6) | 2 (0.6) | - |
| Smoking | 0.002 | ||||||
| Never | 467 (89.1) | 115 (82.1) | 352 (91.7) | 57 (90.5) | 287 (92.3) | 8 (80.0) | |
| Ex-smoker | 35 (6.7) | 18 (12.9) | 17 (4.4) | 3 (4.8) | 13 (4.2) | 1 (10.0) | |
| Current smoker | 22 (4.2) | 7 (5.0) | 15 (3.9) | 3 (4.8) | 11 (3.5) | 1 (10.0) | |
| Systolic BP (mean ± SD) | 114 ± 16.8 | 116 ± 17.6 | 113 ± 16.1 | NS | 113 ± 14.8 | 111 ± 18.3 | 118 ± 21.3 |
| BNP (pg/mL) | 516 ± 1,093 | 465 ± 1,001 | 562 ± 1,176 | NS | 645 ± 1,423 | 362 ± 444 | 871 ± 662 |
| NT proBNP (pg/mL) | 2,798 ± 6,375 | 2,192 ± 3,244 | 2,876 ± 6,673 | NS | 1,900 ± 5,047 | 3,234 ± 7,152 | 687 ± 978 |
| 6MWD (mean ± SD, m) | 376 ± 124 | 398 ± 116 | 364 ± 127 | NS | 382 ± 119 | 347 ± 133 | 277 ± 162 |
| DLCO (%) | 64.1 ± 24.3 | 74.1 ± 20.7 | 59.3 ± 24.5* | < 0.001 | 95.1 ± 34.5 | 56.3 ± 20.9 | 52.2 ± 22.5 |
P values for 6 MWD, SBP, BNP, NT proBNP, and DLCO were obtained from the independent t-test or Wilcoxon rank sum test to compare the means between functional classes I/II and III/IV. P values for categorical data were obtained from chi-square test or Fisher's exact test. NS: P>0.05. APAH, acquired pulmonary arterial hypertension; IPAH, idiopathic pulmonary arterial hypertension; CHD, congenital heart disease; CTD, connective tissue disease; DM, diabetes mellitus; IHD, ischemic heart disease; COPD, chronic obstructive lung disease; TIA, transient ischemic attack; BP, blood pressure; BNP, serum brain natriuretic peptide; NT-proBNP, serum N-terminal proBNP; 6MWD, 6-minute walking distance; DLCO, diffusion capacity for carbon monoxide.
Table 2. Comparisons according to WHO functional classes in KORPAH patients.
| Parameters | Class I, II (n = 354, 56.6%) | Class III, IV (n = 271, 43.4%) | P value |
|---|---|---|---|
| Age (yr) | NS | ||
| < 40 | 116 | 95 | |
| 40-49 | 83 | 69 | |
| 50-59 | 70 | 49 | |
| ≥ 60 | 85 | 58 | |
| Sex | NS | ||
| Male | 71 | 51 | |
| Female | 283 | 220 | |
| Department | < 0.001 | ||
| Cardiology | 60 | 72 | |
| Pulmonology | 51 | 91 | |
| Rheumatology | 199 | 54 | |
| Pediatrics | 44 | 54 | |
| Subtype | < 0.001 | ||
| IPAH | 53 | 92 | |
| CHD | 80 | 79 | |
| CTD | 217 | 94 | |
| Other | 4 | 6 | |
| Time at diagnosis | NS | ||
| Before 2005. 8 | 78 | 65 | |
| After 2005. 8 | 276 | 206 | |
| Diagnosis method | 0.002 | ||
| RHC | 122 | 127 | |
| Echo | 232 | 144 | |
| Treatment | < 0.001 | ||
| No | 58 | 25 | |
| Conventional | 122 | 45 | |
| Single | 146 | 162 | |
| Bosentan | 58 | 97 | |
| Sildenafil | 29 | 16 | |
| Iloprost | 9 | 13 | |
| Beraprost | 50 | 36 | |
| Combination | 28 | 44 | |
| 6MWD (m) | < 0.001 | ||
| < 379 | 26 | 66 | |
| 380-439 | 20 | 24 | |
| ≥ 440 | 42 | 25 | |
| BNP (pg/mL) | NS | ||
| < 174 | 26 | 33 | |
| ≥ 174 | 20 | 32 | |
| NT proBNP (pg/mL) | < 0.001 | ||
| < 797 | 104 | 40 | |
| ≥ 797 | 53 | 66 |
P values for BNP and NT proBNP were obtained from the Wilcoxon rank sum test to compare the means between functional classes I/II and III/IV. NS: P>0.05. Echo, Doppler echocardiography; RHC, right heart catheterization; 6MWD, 6 minutes Walking distances.
Of 625 patients, only 249 patients were diagnosed by RHC. As shown in Table 3, of these 249 patients, 34.9%, 43.0%, and 20.9% had IPAH, CHD, and CTD, respectively. These proportions were quite different than those of all patients (23.2%, 25.4%, and 49.8%, respectively). The comparisons of RHC parameters for the 249 patients are presented in Table 3. There were no significant differences in any parameters between patients with IPAH and those with APAH.
Table 3. Comparison of RHC parameters between IPAH and APAHs.
| Parameters | All patients | IPAH | All patients with APAH | P value | APAH subgroup | ||
|---|---|---|---|---|---|---|---|
| CHD | CTD | Other | |||||
| Patients, No. (%) | 249 | 87 (34.9) | 162 (65.1) | 107 (43) | 52 (20.9) | 3 (1.2) | |
| RHC parameters | |||||||
| mPAP (mmHg) | 55.3 ± 17.3 | 57.7 ± 18.2 | 54.0 ± 16.7 | NS | 58.5 ± 16.1 | 44.4 ± 13.8 | 47.0 ± 17.0 |
| mPCWP (mmHg) | 8.18 ± 3.47 | 8.68 ± 3.18 | 7.66 ± 3.70 | NS | 6.97 ± 3.64 | 8.67 ± 3.34 | 9.33 ± 6.03 |
| mRAP (mmHg) | 8.92 ± 5.64 | 9.74 ± 6.75 | 8.51 ± 5.00 | NS | 7.80 ± 4.07 | 12.9 ± 8.10 | 10.0 ± 4.24 |
| PVRI (Wood units·m2) | 9.28 ± 5.84 | 8.40 ± 4.97 | 10.1 ± 6.55 | NS | 10.2 ± 7.18 | 9.41 ± 4.04 | 14.4 ± 17.4 |
| CI (L/min·m2) | 2.44 ± 0.77 | 2.43 ± 0.68 | 2.46 ± 0.92 | NS | 2.99 ± 1.03 | 2.17 ± 0.62 | 2.12 ± 1.33 |
| SvO2 (%) | 51.6 ± 21.0 | 52.4 ± 16.3 | 51.0 ± 24.4 | NS | 57.5 ± 28.9 | 45.1 ± 12.7 | 34.0 ± 8.72 |
NS: P>0.05. APAH, acquired pulmonary arterial hypertension; IPAH, idiopathic pulmonary arterial hypertension; CHD, congenital heart disease; CTD, connective tissue disease; RHC, right heart catheterization; mPAP, mean pulmonary artery pressure; mPCWP, mean pulmonary capillary wedge pressure; mRAP, mean right arterial pressure; PVRI, pulmonary vascular resistance index; CI, cardiac index; SvO2, mixed venous oxygen saturation.
Characteristics of the incident cases
Of all patients, 328 patients were enrolled at the beginning of registry (prevalent cases), and 297 patients were enrolled during the study (incident cases). The specific etiology of PAH and the baseline characteristics of the 297 incident cases are presented in Table 4. Of these 297 patients, CTD was the most common etiology (57.6%), followed by CHD (26.9%) and IPAH (12.5%). The mean age and the frequency of women among these patients were similar to those of all patients. Systolic blood pressure, BNP or NT-proBNP, 6MWD and DLCO were not significantly different between IPAH and APAH in the incident cases (Table 4). According to the Korean Statistical Information Service in the year of 2010, the population was 47,990,761. Therefore, the incidence rate of PAH was 1.9 patients/yr/million people. At enrollment, 123 of 297 (41.0%) patients were functional class III, and 19 (6.0%) were functional class IV. IPAH patients exhibited more severe functional classes than did other subtypes (Table 4). Among the 297 patients, only 106 patients were diagnosed by RHC. The comparisons of the RHC parameters in the 106 patients are presented in Table 5. Among the incident cases diagnosed by RHC, CHD and CTD comprised 49.1% and 30.2%, respectively (Table 5). There were no significant differences in any of the RHC parameters between patients with IPAH and APAH. Table 6 presents the PAH-specific medications in all patients (n=625) and incidence patients (n=297) in the KORPAH. Among the 297 incidence patients, 182 (61.3%) patients were treated by PAH-specific medical therapies. Of those, 154 (84.6%) patients received single medications; 93 were on bosentan, 23 were on beraprost, 21 were on sildenafil, and 17 were on inhaled iloprost. Twenty-eight (15.4%) patients received combination therapy.
Table 4. Baseline characteristics of incident cases in KORPAH.
| Parameters | All patients | IPAH | All patients with APAH | P value | APAH subgroup | ||
|---|---|---|---|---|---|---|---|
| CHD | CTD | Other | |||||
| Patients, No. (%) | 297 (100) | 37 (12.5) | 260 (87.5) | 80 (26.9) | 171 (57.6) | 9 (3.0) | |
| Age, mean ± SD (yr) | 50.0 ± 16.6 | 47.0 ± 16.6 | 50.5 ± 16.6 | NS | 43.2 ± 13.7 | 54.1 ± 17.0 | 46.3 ± 9.6 |
| Female, No. (%) | 233 (78) | 27 (73) | 206 (79) | NS | 54 (68) | 146 (85) | 6 (67) |
| Functional class, No. (%) | 0.002 | ||||||
| I | 58 (20) | 1 (3) | 57 (22) | 3 (4) | 53 (31) | 1 (11) | |
| II | 97 (33) | 8 (22) | 89 (34) | 33 (41) | 54 (32) | 2 (22) | |
| III | 123 (41) | 25 (68) | 98 (38) | 43 (54) | 50 (29) | 5 (56) | |
| IV | 19 (6) | 3 (8) | 16 (6) | 1 (1) | 14 (8) | 1 (11) | |
| Systolic BP (mean ± SD) | 114 ± 16.5 | 113 ± 16.2 | 115 ± 16.7 | NS | 115 ± 16.0 | 112 ± 17.5 | 115 ± 20.8 |
| BNP (pg/mL) | 721 ± 1,619 | 749 ± 1,652 | 705 ± 1,632 | NS | 922 ± 2,117 | 305 ± 385 | 871 ± 662 |
| NT proBNP (pg/mL) | 3,173 ± 6,960 | 2,508 ± 3,890 | 3,247 ± 7,276 | NS | 2,203 ± 5,589 | 3,762 ± 7,878 | 787 ± 1,059 |
| 6MWD (mean ± SD, m) | 363 ± 116 | 353 ± 124 | 365 ± 115 | NS | 378 ± 109 | 358 ± 114 | 237 ± 173 |
| DLCO (%) | 62.0 ± 26.3 | 70.6 ± 24.8 | 60.3 ± 26.4 | NS | 93.1 ± 33.9 | 56.7 ± 22.7 | 52.2 ± 22.5 |
P values for 6MWD, SBP, BNP, NT proBNP, and DLCO were obtained from the independent t-test to compare the means between patients diagnosed with IPAH and all patients with APAH. P values for categorical data were obtained from chi-square test or Fisher's exact test. NS: P>0.05. APAH, acquired pulmonary arterial hypertension; IPAH, idiopathic pulmonary arterial hypertension; CHD, congenital heart disease; CTD, connective tissue disease; BP, blood pressure; BNP, serum brain natriuretic peptide; NT-proBNP, serum N-terminal proBNP; 6MWD, 6-minute walking distance; DLCO, diffusion capacity for carbon monoxide.
Table 5. Comparisons of RHC parameters between IPAH and APAH in the incident cases of KORPAH.
| Parameters | All patients | IPAH | All patients with APAH | P value | APAH subgroup | ||
|---|---|---|---|---|---|---|---|
| CHD | CTD | Other | |||||
| Patients, No. (%) | 106 | 19 (17.9) | 87 (82.1) | 52 (49.1) | 32 (30.2) | 3 (2.8) | |
| RHC parameters | |||||||
| mPAP (mmHg) | 51.9 ± 16.3 | 47.8 ± 11.3 | 52.8 ± 17.2 | 0.249 | 56.5 ± 17.3 | 46.5 ± 15.5 | 47.0 ± 17.0 |
| mPCWP (mmHg) | 7.36 ± 3.53 | 6.63 ± 3.12 | 7.68 ± 3.70 | 0.346 | 6.67 ± 3.10 | 9.30 ± 3.80 | 9.33 ± 6.03 |
| mRAP (mmHg) | 8.19 ± 4.18 | 6.57 ± 4.38 | 8.71 ± 4.02 | 0.096 | 8.66 ± 4.13 | 8.60 ± 3.97 | 10.0 ± 4.24 |
| PVRI (Wood units·m2) | 10.2 ± 6.38 | 8.91 ± 4.62 | 10.7 ± 7.03 | 0.652 | 10.6 ± 7.32 | 10.0 ± 4.56 | 14.4 ± 17.4 |
| CI (L/min·m2) | 2.35 ± 0.79 | 2.20 ± 0.44 | 2.44 ± 0.93 | 0.673 | 2.79 ± 1.00 | 2.19 ± 0.71 | 2.12 ± 1.33 |
| SvO2 (%) | 51.4 ± 22.0 | 51.0 ± 15.3 | 51.5 ± 25.3 | 0.628 | 57.5 ± 28.9 | 45.4 ± 15.5 | 34.0 ± 8.72 |
APAH, acquired pulmonary arterial hypertension; IPAH, idiopathic pulmonary arterial hypertension; CHD, congenital heart disease; CTD, connective tissue disease; RHC, right heart catheterization; mPAP, mean pulmonary artery pressure; mPCWP, mean pulmonary capillary wedge pressure; mRAP, mean right arterial pressure; PVRI, pulmonary vascular resistance index; CI, cardiac index; SvO2, mixed venous oxygen saturation.
Table 6. PAH-specific medications of KORPAH in all patients and incident patients.
| Medications | Treatments in all patients (n = 625) | Treatments in incidence cases (n = 297) |
|---|---|---|
| No. (%) of patients receiving PAH-specific medications in all treatments | 380 (60.8) | 182 (61.3) |
| No. (%) of medications in all PAH-specific treatments | ||
| Single bosentan | 155 (40.9) | 93 (51.1) |
| Single sildenafil | 45 (11.8) | 21 (11.6) |
| Single inhaled iloprost | 22 (5.8) | 17 (9.3) |
| Single beraprost | 86 (22.6) | 23 (12.6) |
| Combinations of above single medications | 72 (18.9) | 28 (15.4) |
Prognosis of incident cases
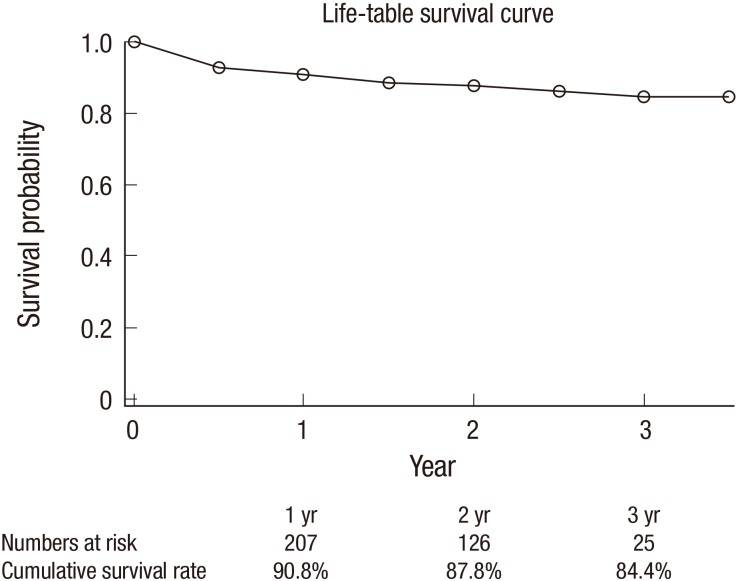
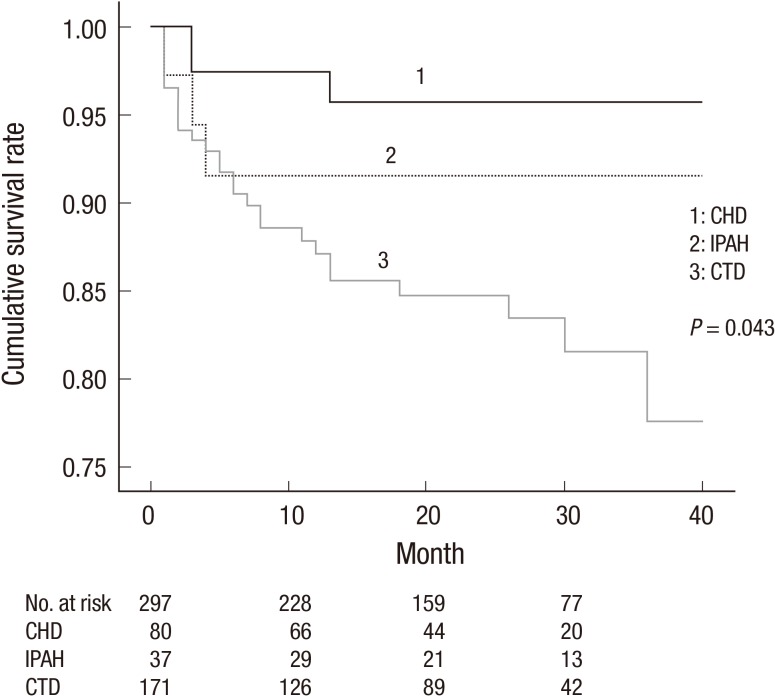
Of all 297 incidence cases, there were 35 cases of mortality during the mean 1.7 yr of follow-up. The estimated mortality rate was 7/100 person-years. The cumulative survival curve of incident cases is presented in Fig. 1. The 1st-, 2nd-, and 3rd-year estimated survival rates were 90.8%, 87.8%, and 84.4%, respectively. Fig. 2 presents the comparison of prognosis according to the etiologies of PAH. PAH with CTD corresponded to the highest mortality (18.8%), followed by IPAH (8.1%) and CHD (3.9%) (P=0.043).
Fig. 1. Cumulative survival curve of the incident cases in the KORPAH (n = 297). The first-, second- and third-year estimated survival rates were 90.8%, 87.8%, and 84.4%, respectively.
Fig. 2. Comparison of survival according to the etiologies of PAH of the incident cases in the KORPAH (n = 297). This figure presents a comparison of prognoses according to the etiologies of PAH. PAH with CTD corresponded to the highest mortality (18.8%), followed by idiopathic PAH (IPAH) (8.1%) and PAH with congenital heart disease CHD (3.9%) (P = 0.043). CHD, congenital heart disease; CTD, connective tissue disease.
DISCUSSION
The present study is the first report of the clinical characteristics and epidemiology of Korean PAH patients as well as the first PAH nationwide registry data in Asian counties. The important findings of the KORPAH were as follows: 1) the most common etiology of PAH was CTD, followed by CHD and IPAH in incidence cases as well as in all patients; 2) middle-aged females were the most common subgroup of patients (80.5%); 3) approximately 43.4% of patients had WHO class III or IV disease at diagnosis; 4) patients concurrently had essential hypertension (19.4%); diabetes (8.2%) and obesity (15.3%); 5) the incidence rate of PAH was 1.9 patients/yr/million people; 6) the estimated mortality rate was 7/100 person-years, and CTD-associated PAH (CTD-PAH) exhibited the worst prognosis (18.8%); 7) the incidence of systemic lupus erythematosus (SLE) (35.3%) was comparable to that of systemic sclerosis (SSc) (28.3%) in CTD-PAH; 8) the 1st-, 2nd-, and 3rd-yr estimated survival rates were 90.8%, 87.8%, and 84.4%, respectively.
Previous large national observational registries have provided information on current PAH epidemiology, increasing awareness about the disease (6,8,9,10,11). However, most of the current data come from Western countries, and the few reports from PAH registries from Asian countries are limited to single referral center registries or registries from a single country (12,13). One previous report from a Chinese registry included only IPAH and familial PAH patients who had not taken PAH-targeted drugs and were much younger than those included in western registries (12). The demographics of the KORPAH registry participants were similar to those of western registry participants (Table 7). The observed mean age (47.6 yr old) and female proportion of patients (80.5%) in the KORPAH more closely resembled those observed in the REVEAL registry (50.1 yr old and 79.5%, respectively) than those in the Chinese registry (35.9 yr old and 70.8%, respectively). The KORPAH and other contemporary registries, including the REVEAL registry, indicate a similar shift in the age demographic to an older age at diagnosis and a greater female predominance since the time of the NIH registry (5,6,8,9,10,11,12,13,14,15,16).
Table 7. Comparisons of demographic, clinical and hemodynamic characteristics in world registries of PAH.
| Parameters | REVEAL 2010 | French 2006 | Spain 2012 | China 2011 | Korea 2011 |
|---|---|---|---|---|---|
| Cases (No) | 2,525 | 674 | 866 | 956 | 625 |
| Mean age (yr) | 50 ± 14 | 50 ± 15 | 45 ± 17 | 36 ± 13 | 48±16 |
| Female (%) | 80 | 65 | 71 | 70 | 80.5 |
| WHO III/IV (%) | 56 | 75 | 69 | 54 | 48.7 |
| 6MWD (m) | 366 ± 126 | 329 ± 112 | 382 ± 117 | 353 ± 127 | 372 ± 123 |
| mPAP (mmHg) | 51 ± 14 | 55 ± 15 | 54 ± 16 | 63 ± 15 | 66 ± 22 |
| PVRI (Wood U*m2) | 21 ± 13 | 21 ± 10 | NA | 25 ± 14 | 10 ± 6 |
6MWD, 6-minute walking distance; mPAP, mean pulmonary artery pressure; PVRI, pulmonary vascular resistance index.
Recently, the Registry of Pulmonary Hypertension Associated with Rheumatic Disease (REOPARD), a nationwide, multicenter, observational Korean registry, reported that Korean CTD-PAH patents exhibit some differences with respect to underlying diseases, functional status and treatment compared with western country registries (17,18). However, this survey included only CTD-PAH diagnosed by rheumatologists and exhibited some limitations (17). Therefore, the KORPAH may be an important and valuable registry because it explores the epidemiological and clinical characteristics of Korean PAH patients for the first time.
Compared with previous registries, the most striking difference and limitation in the KORPAH was the performance rate of RHC. Among 625 patients, only 249 patients were diagnosed by RHC. RHC was performed in 60% of IPAH patients, 67% of CHD-PAH patients and 17% of CTD-PAH patients. Another difference between the KORPAH and other studies was the higher proportion of CTD-PAH patients (49.8%) relative to other registries. In the French and REVEAL registries, approximately half of the patients exhibited idiopathic disease, whereas the other half exhibited APAH (8,9,10,11).
Meta-analyses reveal that patients with CTD-PAH exhibit more severe symptoms and worse prognoses compared with other etiologies of PAH (18,19). Although CTD-PAH patients in the KORPAH exhibited the worst prognoses, there were some differences relative to other registries. With respect to functional class, CTD-PAH in the KORPAH corresponded to a remarkably higher proportion of WHO functional class I and II (63%) patients than did IPAH in the KORPAH, which differed significantly from the results of other registries (12%-28%). This discrepancy may be partly due to the diagnostic tool used in this study. Most CTD-PAH patients in the KORPAH were diagnosed only with Doppler echocardiography and clinical histories, suggesting that many rheumatology doctors may have included PAH patients without confirmation of RHC (17). This fact may have contributed to the relatively higher proportion of CTD-PAH patients, an overestimation of mPAP, and a higher proportion of patients with less severe disease in the KORPAH.
In previous studies, patients with CTD-PAH exhibited worse DLCO, had higher BNP levels, and performed more poorly on the 6MWD test compared with patients with PAH due to other causes (18,19). However, in this study, these parameters did not differ significantly between CTD-PAH patients and IPAH patients. With respect to the survival rate, worse prognostic factors failed to exhibit significant differences between patients with CTD-PAH and IPAH, and CTD-PAH patients exhibited the worst 1-yr survival rate (81.2%). However, this result was better than those reported from other large registries. The 1- and 3-yr survival rates were 78% and 47% in SSc-PAH patients, respectively, and 78% and 74% in SLE-PAH patients, respectively, in a UK registry (15); the one-year survival rate of CTD-PAH was 86% in the REVEAL registry (8,9,10). A recent cohort study from China (12) indicated that the 1- and 3-yr survival rates of CTD-PAH patients are 85.4% and 53.6%, respectively. The superior survival outcomes of our registry may be the result of employing patients with less severe disease or attributed to ethnic differences.
Finally, with respect to the subgroups of CTD-PAH, the most common underlying diseases associated with CTD-PAH in previous studies were reported to be systemic sclerosis, followed by SLE and mixed connective tissue disease; most of these studies were conducted in western countries (18,19). In contrast, the frequency of SLE as the underlying CTD was higher than that of systemic sclerosis in our study (35.3% vs. 28.3%). This pattern was also noted in other studies conducted in Japan (20), China (13), and the Philippines (21). This discrepancy of underlying diseases may also result from differences in environment and ethnicity.
With respect to hemodynamic data from RHC in the KORPAH, CTD-PAH patients exhibited no significant differences in important parameters such as mPAP, PCWP, or RVSP relative to IPAH patients. Furthermore, the mPAP values of the IPAH patients who underwent RHC in the KORPAH were similar to the values in the IPAH patients in the REVEAL and French registries but were slightly lower than a single center cohort of IPAH patients in Korea (57.7 mmHg, 52.1 mmHg, 55 mmHg, and 61 mmHg, respectively) (8,9,10,11,22).
Approximately 43% of patients in the KORPAH had WHO class III or IV disease at diagnosis which was quite similar to a previously reported single center cohort in Korea (40%) (23), suggesting that PAH continues to be detected at an advanced stage of the disease. In addition to the under-utilization of RHC for the confirmation of PAH, the KORPAH reveals that PAH-targeted drugs are under-prescribed (approximately 61%). Only 380 (60.8%) patients received a single PAH-specific treatment at the time of enrollment, and only 72 (18.9%) patients received combination therapy. The reasons for this late detection and under-treatment might be due to insufficient awareness of the disease in Korea. Thus, continued efforts to increase awareness among the public and clinicians should be warranted for the early detection and optimal management of PAH patients.
The KORPAH was a national observational and voluntary registry that was created by 4 Korean academic societies. Therefore, the web design of the registry and its tone varied among participating academic societies, and the completeness of data entered into the registry varied. However, we nonetheless believe that a nationwide, multicenter registry is necessary for a rare disease like PAH. McLaughlin and Suissa (24) described the importance and limitations of nationwide registries as follows: "To further our comprehension of rare diseases, we often turn to registries constructed as multicenter cohorts of patients who have the disease with longitudinal follow-up. Despite the inherent limitations of their observational and uncontrolled nature, which also represent strengths, these cohorts are useful to describe and compare patient characteristics, practice patterns, and outcomes." To maintain the quality and precision of the KORPAH data, multiple audit processes should be undertaken by an independent investigator.
In conclusion, we report the clinical data of all 625 patients and 297 incidence patients with PAH in Korea in this article. Compared with western registries, Korean PAH patients exhibited similar age, gender and survival rate. However, in the etiology, KORPAH and Chinese registry show more CTD-PAH and SLE among them than western registries, which may be related to ethnic difference. Also, as showed in other world registries, the results of KORPAH suggest that earlier standardized diagnosis and more specialized medical therapies should be needed to improve the survival of PAH patients in Korea. Finally, observations from the KORPAH should generate hypotheses that will prompt future subsequent studies.
ACKNOWLEDGMENTS
We deeply appreciate The Korean Vascular Research Working Group, The Korean Society of Cardiology; The Pulmonary Vascular Study Group, The Korean Academy of Tuberculosis and Respiratory Diseases; Korean College of Rheumatology; The Korean Pediatric Heart Society for their support of this registry. We particularly appreciate Yeon Do Choi, Hoon Cho, Chi Hyun Chang and Sun Bok Kang for their administrative support and auditing.
Footnotes
Funding: This study was funded by Handok, Inc. (Seoul, Korea) and Actelion Pharmaceuticals (Allschwil, Switzerland).
DISCLOSURE: The authors have no conflicts of interest to disclose. The sponsors have not involved any of the research procedures or writing.
AUTHOR CONTRIBUTION: Conception and design of this study: all authors. Interpretation of results and drafting the manuscript: Chung WJ, Park YB, Jeon CH, Jung JW and Jung HO. Analysis and interpretation of data: Ko KP, Chung WJ, and Jung HO. Critical revision and final submission of manuscript: Chung WJ and Jung HO. Manuscript approval: all authors.
KORPAH INVESTIGATORS: KORPAH investigators were as follows: Hae Ok Jung, Seoul St. Mary's Hospital, The Catholic University of Korea, Seoul; Wook-Jin Chung, Gachon University Gil Medical Center, Incheon; Yong Bum Park, Hallym University Medical Center, Seoul; Chan Hong Jeon, Soonchunhyang University Hospital, Bucheon; Jo-Won Jung, Severance Hospital, Yonsei University, Seoul; Kwang-Phil Ko, Gachon University College of Medicine, Incheon; Sung Jae Choi, Korea University Ansan Hospital, Ansan; Hye-Sun Seo, SoonChunHyang University Hospital, Bucheon; Jaeseung Lee, Asan Medical Center, Seoul; Sung-A Chang, Samsung Medical Center, Seoul; Sang Do Lee, Asan Medical Center, Seoul; Sang-Min Lee, Seoul National University Hospital, Seoul; Ki-Jo Kim, Yeouido St. Mary's Hospital, The Catholic University of Korea, Seoul; Kwi-Young Kang, Incheon St. Mary's Hospital, The Catholic University of Korea, Incheon; Choong-Won Lee, Wallace Memorial Baptist center, Busan; Mie-Jin Lim, Inha University Hospital, Incheon; Yong-Beom Park, Severance Hospital, Yonsei University, Seoul; Won Park, Inha University Hospital, Incheon; Sung Hwan Park, Seoul St. Mary's Hospital, The Catholic University of Korea, Seoul; Jae-Bum Jun, Hanyang University Medical Center, Seoul; Hojoong Kim, Samsung Medical Center, Seoul; Byung-Su Yoo, Wonju Severance Christian Hospital, Wonju; Young Ho Lee, Korea University Anam Hospital, Seoul; Sang-Youn Jung, Severance Hospital, Yonsei University, Seoul; Kichul Shin, Seoul National University Hospital, Seoul; Sung Ji Lee, Chonnam National University Hospital, Gwangju; Hyo-Jin Choi, Gachon University Gil Medical Center, Incheon; Hyun-A Kim, Ajou University Hospital, Suwon; Chang-Hee Suh, Ajou University Hospital, Suwon; Jong-Dae Ji, Korea University Anam Hospital, Seoul; Eun-Mi Koh, Samsung Medical Center, Seoul; Hoon-Suk Cha, Samsung Medical Center, Seoul; Kwang-Hoon Lee, Severance Hospital, Yonsei University, Seoul; Yonggil Kim, Asan Medical Center, Seoul; Shin Seok Lee, Chonnam National University Hospital, Gwangju; Seong-Su Nah, Soonchunhyang University Hospital, Cheonan; Seong-Ryul Kwon, Inha University Hospital, Incheon; Bo-Young Yoon, Inje University Ilsan Paik Hospital, Goyang; Eun-Young Lee, Seoul National University Hospital, Seoul; Hyun-Sook Kim, Chosun University Hospital, Gwangju; Ki-Won Moon, Seoul National University Hospital, Seoul; Yong Wook Park, Chonnam National University Hospital, Gwangju; Jin Ho Shin, Hanyang University Medical Center, Seoul; Joong-Kyong Ahn, Samsung Medical Center, Seoul; Dae Hyun Yoo, Hanyang University Medical Center, Seoul; Jaejoon, Lee, Samsung Medical Center, Seoul; Seong-Ho Kim, Sejong General Hospital, Bucheon; Gi-Beom Kim, Seoul National University Hospital, Seoul; I-Seok Kang, Samsung Medical Center, Seoul; Jae-Young Choi, Severance Hospital, Yonsei University, Seoul; Seong-Mi Park, Korea University Anam Hospital, Seoul; Se Joong Rim, Gangnam Severance Hospital, Yonsei University, Seoul; Sang Jea Lee, Wonkwang University School of Medicine&Hospital, Iksan; Young Hwue Kim, Asan Medical Center, Seoul; Deok-Young Choi, Gachon University Gil Medical Center, Incheon; Kye Hun Kim, Chonnam National University Hospital, Gwangju; Kyung-Im Cho, Maryknoll medical center, Busan; Se-Whan Lee, Soonchunhyang University Hospital, Cheonan; Hyoung-Doo Lee, Pusan National University Yangsan Hospital, Yangsan; Woo-Shik Kim, Kyung Hee University Medical Center, Seoul; Won Ho Kim, Chonbuk National University Hospital, Jeonju; Il-Suk Sohn, Kyung Hee University Hospital at Gandong, Seoul; Geu-Ru Hong, Yeungnam University Medical Center, Daegu; Nam Su Kim, Hanyang University Medical Center, Seoul; Yeo Hyang Kim, Keimyung University Dongsan Medical Center, Daegu; Yong-Jin Kim, Seoul National University Hospital, Seoul; Dae Gyun Park, Hallym University Medical Center, Seoul; Kwang Je Lee, Chung-Ang University, College of Medicine, Seoul; Suk-koo Choi, Inje University Seoul Paik Hospital, Seoul; Mi Young Han, Kyung Hee University Medical Center, Seoul; Myung Chul Hyun, Kyungpook National University Hospital, Daegu; Kyung-Soon Hong, Hallym University Chuncheon Sacred Heart Hospital, Chuncheon; In-Jae Oh, Chonnam National University Hospital, Gwangju; Byoung Whui Choi, Chung-Ang University, College of Medicine, Seoul; Myung-Goo Lee, Hallym University Chuncheon Sacred Heart Hospital, Chuncheon; Ji-Hyun Lee, Bundang CHA Hospital, Seongnam; and Moo Suk Park, Severance Hospital, Yonsei University, Seoul.
References
- 1.McGoon M, Gutterman D, Steen V, Barst R, McCrory DC, Fortin TA, Loyd JE American College of Chest Physicians. Screening, early detection, and diagnosis of pulmonary arterial hypertension: ACCP evidence-based clinical practice guidelines. Chest. 2004;126:14s–34s. doi: 10.1378/chest.126.1_suppl.14S. [DOI] [PubMed] [Google Scholar]
- 2.Simonneau G, Galiè N, Rubin LJ, Langleben D, Seeger W, Domenighetti G, Gibbs S, Lebrec D, Speich R, Beghetti M, et al. Clinical classification of pulmonary hypertension. J Am Coll Cardiol. 2004;43:5s–12s. doi: 10.1016/j.jacc.2004.02.037. [DOI] [PubMed] [Google Scholar]
- 3.Rubin LJ, Badesch DB. Evaluation and management of the patient with pulmonary arterial hypertension. Ann Intern Med. 2005;143:282–292. doi: 10.7326/0003-4819-143-4-200508160-00009. [DOI] [PubMed] [Google Scholar]
- 4.McLaughlin VV, Presberg KW, Doyle RL, Abman SH, McCrory DC, Fortin T, Ahearn G American College of Chest Physicians. Prognosis of pulmonary arterial hypertension: ACCP evidence-based clinical practice guidelines. Chest. 2004;126:78s–92s. doi: 10.1378/chest.126.1_suppl.78S. [DOI] [PubMed] [Google Scholar]
- 5.Rich S, Dantzker DR, Ayres SM, Bergofsky EH, Brundage BH, Detre KM, Fishman AP, Goldring RM, Groves BM, Koerner SK, et al. Primary pulmonary hypertension. A national prospective study. Ann Intern Med. 1987;107:216–223. doi: 10.7326/0003-4819-107-2-216. [DOI] [PubMed] [Google Scholar]
- 6.D'Alonzo GE, Barst RJ, Ayres SM, Bergofsky EH, Brundage BH, Detre KM, Fishman AP, Goldring RM, Groves BM, Kernis JT, et al. Survival in patients with primary pulmonary hypertension. Results from a national prospective registry. Ann Intern Med. 1991;115:343–349. doi: 10.7326/0003-4819-115-5-343. [DOI] [PubMed] [Google Scholar]
- 7.Hoeper MM, Bogaard HJ, Condliffe R, Frantz R, Khanna D, Kurzyna M, Langleben D, Manes A, Satoh T, Torres F, et al. Definitions and diagnosis of pulmonary hypertension. J Am Coll Cardiol. 2013;62:D42–D50. doi: 10.1016/j.jacc.2013.10.032. [DOI] [PubMed] [Google Scholar]
- 8.Badesch DB, Raskob GE, Elliott CG, Krichman AM, Farber HW, Frost AE, Barst RJ, Benza RL, Liou TG, Turner M, et al. Pulmonary arterial hypertension: baseline characteristics from the REVEAL Registry. Chest. 2010;137:376–387. doi: 10.1378/chest.09-1140. [DOI] [PubMed] [Google Scholar]
- 9.Frost AE, Badesch DB, Barst RJ, Benza RL, Elliott CG, Farber HW, Krichman A, Liou TG, Raskob GE, Wason P, et al. The changing picture of patients with pulmonary arterial hypertension in the United States: how REVEAL differs from historic and non-US Contemporary Registries. Chest. 2011;139:128–137. doi: 10.1378/chest.10-0075. [DOI] [PubMed] [Google Scholar]
- 10.McGoon MD, Miller DP. REVEAL: a contemporary US pulmonary arterial hypertension registry. Eur Respir Rev. 2012;21:8–18. doi: 10.1183/09059180.00008211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Humbert M, Sitbon O, Chaouat A, Bertocchi M, Habib G, Gressin V, Yaici A, Weitzenblum E, Cordier JF, Chabot F, et al. Pulmonary arterial hypertension in France: results from a national registry. Am J Respir Crit Care Med. 2006;173:1023–1030. doi: 10.1164/rccm.200510-1668OC. [DOI] [PubMed] [Google Scholar]
- 12.Jing ZC, Xu XQ, Han ZY, Wu Y, Deng KW, Wang H, Wang ZW, Cheng XS, Xu B, Hu SS, et al. Registry and survival study in chinese patients with idiopathic and familial pulmonary arterial hypertension. Chest. 2007;132:373–379. doi: 10.1378/chest.06-2913. [DOI] [PubMed] [Google Scholar]
- 13.Zhang R, Dai LZ, Xie WP, Yu ZX, Wu BX, Pan L, Yuan P, Jiang X, He J, Humbert M, et al. Survival of Chinese patients with pulmonary arterial hypertension in the modern treatment era. Chest. 2011;140:301–309. doi: 10.1378/chest.10-2327. [DOI] [PubMed] [Google Scholar]
- 14.Escribano-Subias P, Blanco I, López-Meseguer M, Lopez-Guarch CJ, Roman A, Morales P, Castillo-Palma MJ, Segovia J, Gómez-Sanchez MA, Barberà JA, et al. REHAP investigators. Survival in pulmonary hypertension in Spain: insights from the Spanish registry. Eur Respir J. 2012;40:596–603. doi: 10.1183/09031936.00101211. [DOI] [PubMed] [Google Scholar]
- 15.Ling Y, Johnson MK, Kiely DG, Condliffe R, Elliot CA, Gibbs JS, Howard LS, Pepke-Zaba J, Sheares KK, Corris PA, et al. Changing demographics, epidemiology, and survival of incident pulmonary arterial hypertension: results from the pulmonary hypertension registry of the United Kingdom and Ireland. Am J Respir Crit Care Med. 2012;186:790–796. doi: 10.1164/rccm.201203-0383OC. [DOI] [PubMed] [Google Scholar]
- 16.McGoon MD, Benza RL, Escribano-Subias P, Jiang X, Miller DP, Peacock AJ, Pepke-Zaba J, Pulido T, Rich S, Rosenkranz S, et al. Pulmonary arterial hypertension: epidemiology and registries. J Am Coll Cardiol. 2013;62:D51–D59. doi: 10.1016/j.jacc.2013.10.023. [DOI] [PubMed] [Google Scholar]
- 17.Jeon CH, Chai JY, Seo YI, Jun JB, Koh EM, Lee SK Pulmonary Hypertension Study Group of Korean College of Rheumatology. Pulmonary hypertension associated with rheumatic diseases: baseline characteristics from the Korean registry. Int J Rheum Dis. 2012;15:e80–e89. doi: 10.1111/j.1756-185X.2012.01815.x. [DOI] [PubMed] [Google Scholar]
- 18.Chung L, Liu J, Parsons L, Hassoun PM, McGoon M, Badesch DB, Miller DP, Nicolls MR, Zamanian RT. Characterization of connective tissue disease-associated pulmonary arterial hypertension from REVEAL: identifying systemic sclerosis as a unique phenotype. Chest. 2010;138:1383–1394. doi: 10.1378/chest.10-0260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang X, Mardekian J, Sanders KN, Mychaskiw MA, Thomas J., 3rd Prevalence of pulmonary arterial hypertension in patients with connective tissue diseases: a systematic review of the literature. Clin Rheumatol. 2013;32:1519–1531. doi: 10.1007/s10067-013-2307-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shirai Y, Yasuoka H, Okano Y, Takeuchi T, Satoh T, Kuwana M. Clinical characteristics and survival of Japanese patients with connective tissue disease and pulmonary arterial hypertension: a single-centre cohort. Rheumatology (Oxford) 2012;51:1846–1854. doi: 10.1093/rheumatology/kes140. [DOI] [PubMed] [Google Scholar]
- 21.Santos Estrella PV, Lin YC, Navarra SV. Pulmonary arterial hypertension among Filipino patients with connective tissue diseases. Mod Rheumatol. 2007;17:224–227. doi: 10.1007/s10165-007-0569-8. [DOI] [PubMed] [Google Scholar]
- 22.Ahn JH, Kang BJ. Clinical characteristics and survival of Korean idiopathic pulmonary arterial hypertension patients based on vasoreactivity. J Korean Med Sci. 2014;29:1665–1671. doi: 10.3346/jkms.2014.29.12.1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Park YM, Chung WJ, Choi DY, Baek HJ, Jung SH, Choi IS, Shin EK. Functional class and targeted therapy are related to the survival in patients with pulmonary arterial hypertension. Yonsei Med J. 2014;55:1526–1532. doi: 10.3349/ymj.2014.55.6.1526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McLaughlin VV, Suissa S. Prognosis of pulmonary arterial hypertension: the power of clinical registries of rare diseases. Circulation. 2010;122:106–108. doi: 10.1161/CIRCULATIONAHA.110.963983. [DOI] [PubMed] [Google Scholar]