Abstract
Suicide is a leading cause of death among Korean adolescents. Many suicide attempting adolescents often are discharged against medical advice in the emergency department. The aim of the present study was to determine the risk factors for discharge against medical advice (DAMA) after self-inflicted injury or attempted suicide in the emergency department. We extracted data on adolescents (10-19 yr old) from the national emergency department information system; we used data from 2007 and 2011. A total of 6,394 adolescents visited EDs after self-inflicted injury or attempted suicide. Among these patients, the median age was 17 yr (Interquatile range, 15-18 yr), 83.2% were between 15-19 yr of age, and 63.3% were female. Poisoning was the most common method of attempted suicide, while hanging and fall were the most common methods of fatality. The rate of DAMA from the ED was 22.8%. Independent risk factors for DAMA included female gender (odds ratio [OR], 1.49), older age adolescents (OR, 1.96), residence in a metropolitan/large city area (OR, 1.49), and discharge at night (OR, 1.38). These risk factors should be considered in establishing management and counseling plans for patients discharged against medical advice by community services and EDs.
Graphical Abstract
Keywords: Suicide, Attempted; Adolescent; Emergency Service, Hospital; Risk Factors; Patient Discharge
INTRODUCTION
Suicide is a leading cause of death among Korean adolescents (1). According to the National Evidence-based Healthcare Collaborating Agency, the proportion by suicide among all cause of death increased from 2000 to 2009, from 13.56% to 28.24% between the ages of 15 and 19 yr in Korea (2). Because a previous suicide attempt is a risk factor for a later successful suicide attempt, appropriate management of such patients is extremely important (3,4,5).
Discharge against medical advice (DAMA) is associated with significantly higher risk of morbidity and mortality, hospital readmission, and high economic costs in many mental and medical diseases (6,7,8,9,10). Risk factors for DAMA of adolescents who attempt suicide have not been identified. The objective of the current study was to determine the characteristics of adolescents visiting Korean emergency departments (EDs) because of self-inflicted injury and attempted suicide and the risk factors for discharge against medical advice (DAMA) among these patients.
MATERIALS AND METHODS
Study design and NEDIS database
This was a cross-sectional retrospective study. Data for the period from 2007 to 2011 were extracted from the National Emergency Department Information System (NEDIS), which is managed by the National Emergency Medical Center (NEMC) of Ministry of Health & Welfare. NEDIS has been accumulating data since 2003 from about 130 emergency centers (all regional emergency centers and more than 100 local emergency centers) (11). Data on patients aged 10-19 yr visiting EDs for self-inflicted injuries and attempted suicides were lodged by 99 emergency centers in 2007; this number rose to 106 in 2011.
Variables and analysis for risk factors
NEDIS data include demographic information (age, gender, and region of the medical center visited) and ED treatment information (ED arrival and discharge date and time, method of suicide attempt, emergency care, and results of admission). The methods of self-inflicted injury and attempted suicide were categorized as fall, cutting, drowning, poisoning, hanging, and other methods. Other methods included intentional ingestion of a foreign body, and combined methods such as poisoning and cutting. Patients were categorized according to age into one of two groups: young (10-14 yr old) and older (15-19 yr old) adolescents. Region was categorized as metropolitan/large city or province/rural area. The metropolitan/large city category included seven regions (Seoul, Incheon, Busan, Daegu, Daejeon, Ulsan, and Gwangju) and the province/rural area included six regions (Gyeonggi, Gangwon, Chungcheong, Gyeongsang, Jeolla, and Jeju). Admission and discharge times were described as either day (09:00-16:59) or night (17:00-08:59) to capture variations in the availability of specialists such as psychiatrists. We defined patients who were admitted, transferred to another hospital, or discharged on medical recommendation as a normal disposition group. Excluding deaths and transfers from other facilities, we compared the characteristics of patients discharged against medical advice (DAMA) with those of normal disposition patients by univariate analysis. We also analyzed the risk factors for DAMA in adolescents visiting the ED for self-inflicted injury or attempted suicide.
Statistical analysis
Categorical variables are shown as frequencies (percentages) and continuous variables are shown as medians (±interquartile ranges). Chi-square tests were used for comparisons between the DAMA and normal disposition groups, and Student's t-test was used to compare continuous variables. Multiple logistic regression analysis was used to identify risk factors for DAMA. Statistical analysis employed SPSS software (ver. 20; IBM SPSS Statistics, IBM Corporation, Armonk, NY, USA).
Ethics statement
This study was exempted from review by the institutional review board of the Seoul Metropolitan Government and Seoul National University Boramae Medical Center (approval number: 07-2013-2).
RESULTS
Demographics of adolescents visiting the ED because of self-inflicted injury or attempted suicide
In total, 6,394 individuals aged 10-19 yr who had attempted suicide or who intentionally injured themselves and visited EDs over the 5-yr period were included. ED visits for self-inflicted injuries and attempted suicide accounted for 0.42% of the total 1,520,128 ED visits because of injury between 2007 and 2011 (12). Table 1 shows the demographics of adolescents visiting EDs following self-inflicted injury or attempted suicide grouped by whether the injury or suicide attempt was fatal. Patient median age was 17 yr (15-18 yr), and young adolescents (aged 10-14 yr) constituted 16.8% of the total. Female adolescents constituted 63.3% of all patients and 51.2% of fatalities. The most common method of self-inflicted injury and attempted suicide was poisoning (53.8%), followed by cutting/piercing (31.8%). However, fall and hanging were the most common methods of fatality, totaling 77.1% of all fatalities.
Table 1. Demographics of self-inflicted injury or attempted suicide among adolescents in the emergency department by fatality.
| Variables | All cases | Non-fatal cases | Fatal cases* | P value |
|---|---|---|---|---|
| Patients, No. | 6,394 | 6,228 | 166 | |
| Age, median (IQR), (yr) | 17 (15-18) | 17 (15-18) | 17 (15-18) | 0.978 |
| 10-14, No. (%) | 1,077 (16.8) | 1,040 (16.7) | 37 (22.3) | 0.058 |
| 15-19, No. (%) | 5,317 (83.2) | 5,188 (83.3) | 129 (77.7) | |
| Gender, No. (%) | 0.001 | |||
| Female | 4,049 (63.3) | 3,964 (63.6) | 85 (51.2) | |
| Male | 2,345 (36.7) | 2,264 (36.4) | 81 (48.8) | |
| Methods, No. (%) | < 0.001 | |||
| Poisoning | 3,440 (53.8) | 3,424 (55.0) | 16 (9.6) | |
| Cutting/piercing | 2,031 (31.8) | 2,029 (32.6) | 2 (1.2) | |
| Fall | 332 (5.2) | 254 (4.1) | 78 (47.0) | |
| Hanging | 146 (2.3) | 96 (1.5) | 50 (30.1) | |
| Drowning | 65 (1.0) | 59 (0.9) | 6 (3.6) | |
| Others | 380 (5.9) | 366(5.9) | 14 (8.4) | |
| Transfer from other hospital, No. (%) | 754 (11.8) | 737 (11.8) | 17 (10.2) | 0.820 |
| Use of 119 ambulance, No. (%) | 2,112 (33.0) | 1,999 (32.1) | 113 (68.1) | < 0.001 |
| Disposition in the ED, No. (%) | ||||
| Discharge | 2,735 (42.8) | - | - | |
| DAMA | 1,457 (22.8) | - | - | |
| Admitted | 1,719 (26.9) | - | - | |
| Transfer to other hospital | 317 (4.9) | - | - | |
| Death | 166 (2.6) | - | - |
*Included fatal cases before ED, in the ED and after admission. IQR, interquatile range; DAMA, discharge against medical advice.
Outcomes among adolescent patients visiting EDs following self-inflicted injury or attempted suicide
In total, an average of 42.8% of patients were discharged with medical approval and 26.9% (n=1,719) of these were hospitalized (Table 1). The rate of DAMA was 22.8% (n=1,457). The rate of DAMA, admission/transfer and discharge with medical approval did not significantly differ by year over the five-year period. Among admitted patients, the ICU admission rate was 33.3% and the rate of emergency operation was 5.7%. The rate of transfer to other hospitals was 5.0% (n=317). A total of 166 patients (2.6%) died, of whom 84.9% (n=141) died in the ED or prior to ED arrival. After admission, 15.1% (n=25) patients died in hospital.
Comparisons between normal disposition group and DAMA group
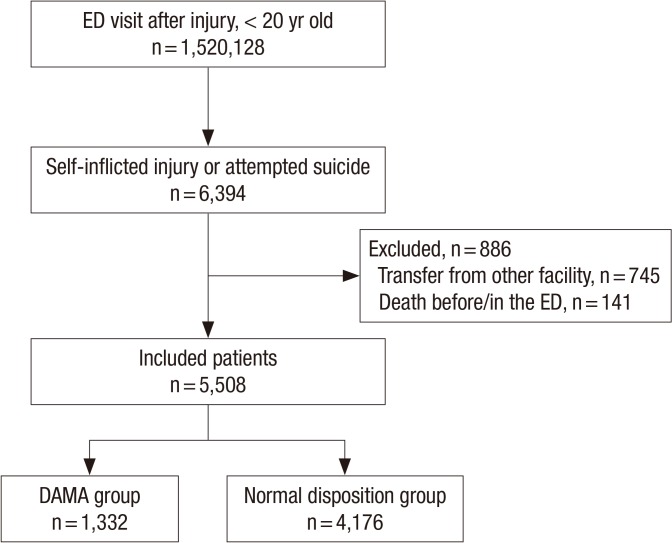
Excluding transfers from other hospitals and patients who died before arrival or in the ED, 5,508 cases were available for comparison (Fig. 1). By definition, normal disposition group was discharged with medical approval (n=2,548) or hospitalized or transferred to another hospital (n=1,628). We compared DAMA patients (n=1,332) to normal disposition group. The rate of DAMA did not differ by year (P=0.707) (Table 2).
Fig. 1. Flow diagram of study population. DAMA, discharge against medical advice.
Table 2. Comparison between normal disposition group and discharge against medical advice group (DAMA).
| Variables | DAMA | Normal disposition group | P value |
|---|---|---|---|
| Patients, No. | 1,332 | 4,176 | |
| Year, No. (%) | 0.707 | ||
| 2007 | 148 (23.5) | 482 (76.5) | |
| 2008 | 221 (23.2) | 730 (76.8) | |
| 2009 | 291 (24.9) | 877 (75.1) | |
| 2010 | 335 (25.3) | 991 (74.7) | |
| 2011 | 337 (23.5) | 1,096 (76.5) | |
| Age, median (IQR), (yr) | 17 (16-18) | 17 (15-18) | < 0.001 |
| 10-14, No. (%) | 147 (11.0) | 759 (18.2) | < 0.001 |
| 15-19, No. (%) | 1,185 (89.0) | 3,417 (81.8) | |
| Gender, Female, No. (%) | 966 (72.5) | 2,542 (60.9) | < 0.001 |
| Method of suicide, No. (%) | < 0.001 | ||
| Poisoning | 871 (65.4) | 2,027 (48.5) | |
| Cutting | 306 (23.0) | 1,635 (39.2) | |
| Fall | 19 (1.4) | 180 (4.3) | |
| Hanging | 27 (2.0) | 53 (1.3) | |
| Drowning | 26 (2.0) | 35 (0.8) | |
| Others | 83 (6.2) | 246 (5.9) | |
| Region of ED, No. (%) | < 0.001 | ||
| Metropolitan/large city | 771 (57.9) | 2,050 (49.1) | |
| Province/rural area | 561 (42.1) | 2,126 (50.9) | |
| Type of emergency center, No. (%) | 0.081 | ||
| Regional emergency center | 184 (13.8) | 660 (15.8) | |
| Local emergency center | 1,148 (86.2) | 3,516 (84.2) | |
| ED visit time, n (%) | 0.964 | ||
| Day (09:00-16:59) | 502 (37.7) | 1,571 (37.6) | |
| Night (17:00-08:59) | 830 (62.3) | 2,605 (62.4) | |
| ED discharge time, No. (%)* | < 0.001 | ||
| Day (09:00-16:59) | 370 (27.8) | 1,390 (33.4) | |
| Night (17:00-08:59) | 961 (72.2) | 2,770 (66.6) |
*Include the patients who were hospitalized or transfer to other hospital. DAMA, discharge against medical advice; IQR, interquatile range; ED, emergency department.
DAMA was more common in older adolescent, female patients than any of the other groups (all P values<0.001). The method of attempted suicide differed by group. Poisoning was significantly more common in DAMA than normal disposition group (P<0.001). Cutting and fall were more common among normal disposition group (P<0.001). Patients with non-DAMA outcomes were more likely to live in rural areas and DAMA was more common in metropolitan areas and large cities. Although the timing of ED visits did not affect outcomes, night discharges were more common in DAMA patients. Type of emergency center did not differ among groups.
Risk factors for DAMA among adolescent patients visiting the ED following self-inflicted injury or attempted suicide
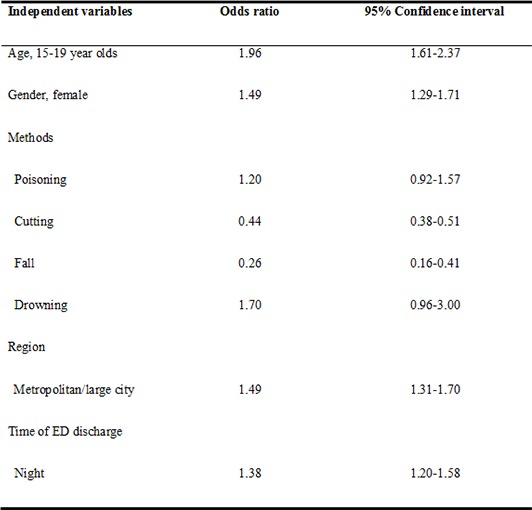
After univariate analysis, multiple logistic regression analysis was performed to identify risk factors for DAMA patients who intentionally injured themselves or attempted suicide. Older age (15-19 yr) (odds ratio [OR], 1.96; 95% confidence interval [CI], 1.61-2.37), female gender (OR, 1.49; 95% CI, 1.29-1.71), injury by cutting (OR, 0.44; 95% CI, 0.38-0.51) or fall (OR, 0.26; 95% CI, 0.16-0.41), residence in a metropolitan area or large city (OR, 1.49; 95% CI, 1.31-1.70) and discharge at night (OR, 1.38; 95% CI, 1.20-1.58) were independent risk factors for DAMA (Table 3).
Table 3. Risk factors of discharge against medical advice among attempted suicide or self-inflicted injuries adolescents.
| Independent variables | Odds ratio | 95% Confidence interval |
|---|---|---|
| Age, 15-19 yr olds | 1.96 | 1.61-2.37 |
| Gender, female | 1.49 | 1.29-1.71 |
| Methods | ||
| Poisoning | 1.20 | 0.92-1.57 |
| Cutting | 0.44 | 0.38-0.51 |
| Fall | 0.26 | 0.16-0.41 |
| Drowning | 1.70 | 0.96-3.00 |
| Region | ||
| Metropolitan/large city | 1.49 | 1.31-1.70 |
| Time of ED discharge | ||
| Night | 1.38 | 1.20-1.58 |
DISCUSSION
This is the first reported study of risk factors for DAMA among adolescent patients who visited EDs because of attempted suicide or self-inflicted injury. We found that about one in four adolescents who attempted suicide was discharged against medical advice. Risk factors for DAMA among these patients included female gender, older age (15-19 yr), residence in a metropolitan area or large city, and ED discharge at night. Our findings indicate that many adolescents with self-inflicted injuries or who had attempted suicide were not managed appropriately in the ED.
Previous estimates of the rates of DAMA of psychiatric patients range from 3% to 51% (13,14). Even though we could not evaluate the outcome or previous history of suicide for DAMA patients in our study, DAMA patients might be at a higher risk of further suicide attempts or poor outcomes. In previous several study, outcomes of patients discharged against medical advice from inpatient psychiatric treatment were characterized by poor outcome in several domains of functioning and more frequent rehospitalizations (14,15). Predictors of DAMA in psychiatric unit were patient factors (young age, single marital status, male gender, comorbid diagnosis of personality or substance use disorders, pessimistic attitudes toward treatment, and history of numerous hospitalizations ending in discharges against medical advice), provider variables (failure to orient patients to hospitalization and failure to establish a supportive provider-patient relationship) and temporal variables (evening and night shifts) (15,16).
Although data on the reasons for DAMA were not available in this study, it seems highly likely that many patients may have refused counseling with a psychiatric physician in the ED and hospitalization to a psychiatric closed ward. In a previous ED-based study in Korea, "conflict with parents" was a major reason for suicide attempt (28.7%) and "conflict with friends" the second-most common reason (13.9%), while psychiatric disease contributed to only 12.5% of attempts in 10-19 yr of age (3). This low prevalence of prior psychiatric diagnoses may contribute to refusal of psychiatric intervention. Also, a psychiatric consultation is not always available in Korean EDs, especially on holidays or at night. The differences in the rates of DAMA and normal discharge by time of day could support one of the reasons for this assumption.
The methods of injury differed between patients DAMA and those admitted or discharged with medical approval. DAMA patients were more likely to have attempted poisoning and less likely to have cut themselves or have jumped than normally discharged patients. Because cutting and fall method could be serious or lethal, the rate of DAMA might be lower among these patients than those who self-injured by other methods. As fall usually causes severe injury, these patients were more likely to have been admitted than discharged.
Suicide is a leading cause of death in Korean adolescents (1). When we consider that only about one-eighth teenagers visit to the hospital after self-inflicted injury, suicide-related behaviors are largely hidden at the community level (5,17,18). Risk factors for suicide in adolescents can be categorized into three classes: sociodemographic, mental health, and individual negative life events and family difficulties (2,4,5,19,20,21,22,23). However, risk factors for suicide and suicidal behavior in Korean adolescents remain to be determined. Although we did not study important variables such as psychiatric diagnoses and socioeconomic status, we used a nationwide database (NEDIS) to monitor trends in self-inflicted injury and suicide attempts among adolescents in the ED. Such an analysis could suggest legal intervention to limit adolescent access to implements commonly used in self-inflicted injury or attempted suicide. About 50% of adolescents in this study poisoned themselves and two thirds of mortality cases involved hanging or fall. In addition to limitation to access of various suicidal methods, preventive strategies should also manage societal influences that could promote suicide. Methods of suicide are known to be affected by mass media coverage of celebrity suicides in Korea (24,25).
According to the studies in the USA and Sweden (intermediate level of suicide rate), ED-based interventions for adolescent patients who have attempted suicide or who have suicidal ideation are especially likely to be effective because the ED experience represents a "teachable moment" (26,27,28). Estimates of the peak hazard of a second suicide attempt are higher than for the first in both genders (29). To prevent further suicide attempts by adolescent DAMA patients, multidisciplinary management and counseling approaches should be developed. As DAMA is especially more likely in metropolitan areas when patients are discharged at night, local governments, hospitals, and community mental health centers in large cities should develop plans to support these patients.
Our study has several potential limitations. First, the NEDIS dataset does not include all emergency centers in Korea. Nevertheless, all regional emergency centers and more than 90% of local emergency centers (annually over 10 million peoples) are registered, and NEDIS represents the most comprehensive national dataset on this topic. Second, because underlying psychiatric diagnoses were not included in the dataset, we could not determine the contribution of background psychiatric status to suicide or attempted suicide. Third, these data did not differentiate attempted suicide from self-inflicted injuries. However, attempted suicide and self-inflicted injuries are both risky behaviors that could precede suicide.
In conclusion, female gender, older age, discharge at night, and treatment in a metropolitan area or large city were the independent risk factors for discharge against medical advice (DAMA) for Korean adolescent who visited ED after attempted suicide or self-inflicted injury. Management and counseling plans for DAMA patients should be established by collaboration between the community and EDs to prevent adolescent suicides in consideration of these risk factors. To decrease suicide attempts, further research is necessary to identify patient motivations for DAMA and follow-up results of these patients.
Footnotes
DISCLOSURE: The authors have no conflicts of interest to discolse.
AUTHOR CONTRIBUTION: Study design: Jung JH, Kwak YH, Kim DK. Sampling and data collection: Jung JH, Kwak YH. Writing: Jung JH, Jung JY, Lee JH. Revision: Kim DK, Jung JY, Lee JH. Approval and submission of final manuscript: All authors.
References
- 1.Statistics Korea. Annual report on the cause of death statistics. Daejeon: Statistics Korea; 2013. [Google Scholar]
- 2.Jeon HJ, Bae J, Woo JM. Recent statistics and risk factors of suicide in children and adolescents. J Korean Med Assoc. 2013;56:93–99. [Google Scholar]
- 3.Lee CA, Choi SC, Jung KY, Cho SH, Lim KY, Pai KS, Cho JP. Characteristics of patients who visit the emergency department with self-inflicted injury. J Korean Med Sci. 2012;27:307–312. doi: 10.3346/jkms.2012.27.3.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. WHO suicide prevention. Geneva: World Health Organization; 2011. [Google Scholar]
- 5.Hawton K, Saunders KE, O'Connor RC. Self-harm and suicide in adolescents. Lancet. 2012;379:2373–2382. doi: 10.1016/S0140-6736(12)60322-5. [DOI] [PubMed] [Google Scholar]
- 6.Baptist AP, Warrier I, Arora R, Ager J, Massanari RM. Hospitalized patients with asthma who leave against medical advice: characteristics, reasons, and outcomes. J Allergy Clin Immunol. 2007;119:924–929. doi: 10.1016/j.jaci.2006.11.695. [DOI] [PubMed] [Google Scholar]
- 7.Fiscella K, Meldrum S, Barnett S. Hospital discharge against advice after myocardial infarction: deaths and readmissions. Am J Med. 2007;120:1047–1053. doi: 10.1016/j.amjmed.2007.08.024. [DOI] [PubMed] [Google Scholar]
- 8.Hwang SW, Li J, Gupta R, Chien V, Martin RE. What happens to patients who leave hospital against medical advice? CMAJ. 2003;168:417–420. [PMC free article] [PubMed] [Google Scholar]
- 9.Anis AH, Sun H, Guh DP, Palepu A, Schechter MT, O'Shaughnessy MV. Leaving hospital against medical advice among HIV-positive patients. CMAJ. 2002;167:633–637. [PMC free article] [PubMed] [Google Scholar]
- 10.Aliyu ZY. Discharge against medical advice: sociodemographic, clinical and financial perspectives. Int J Clin Pract. 2002;56:325–327. [PubMed] [Google Scholar]
- 11.National Emergency Medical Center (KR) 2009 Yearbook of emergency medical statistics. [accessed on 15 May 2015]. Available at http://www.nemc.or.kr/egen/filedown.do?fileName=2009_nemc.pdf.
- 12.National Emergency Medical Center (KR) 2011 Yearbook of emergency medical statistics. [accessed on 15 May 2015]. Available at http://www.nemc.or.kr/egen/filedown.do?fileName=2011_nemc.pdf.
- 13.Shirani F, Jalili M, Asl-E-Soleimani H. Discharge against medical advice from emergency department: results from a tertiary care hospital in Tehran, Iran. Eur J Emerg Med. 2010;17:318–321. doi: 10.1097/MEJ.0b013e3283334ef1. [DOI] [PubMed] [Google Scholar]
- 14.Brook M, Hilty DM, Liu W, Hu R, Frye MA. Discharge against medical advice from inpatient psychiatric treatment: a literature review. Psychiatr Serv. 2006;57:1192–1198. doi: 10.1176/ps.2006.57.8.1192. [DOI] [PubMed] [Google Scholar]
- 15.Pages KP, Russo JE, Wingerson DK, Ries RK, Roy-Byrne PP, Cowley DS. Predictors and outcome of discharge against medical advice from the psychiatric units of a general hospital. Psychiatr Serv. 1998;49:1187–1192. doi: 10.1176/ps.49.9.1187. [DOI] [PubMed] [Google Scholar]
- 16.Gerbasi JB, Simon RI. Patients' rights and psychiatrists' duties: discharging patients against medical advice. Harv Rev Psychiatry. 2003;11:333–343. [PubMed] [Google Scholar]
- 17.Madge N, Hewitt A, Hawton K, de Wilde EJ, Corcoran P, Fekete S, van Heeringen K, De Leo D, Ystgaard M. Deliberate self-harm within an international community sample of young people: comparative findings from the Child & Adolescent Self-harm in Europe (CASE) Study. J Child Psychol Psychiatry. 2008;49:667–677. doi: 10.1111/j.1469-7610.2008.01879.x. [DOI] [PubMed] [Google Scholar]
- 18.Hawton K, Rodham K, Evans E, Weatherall R. Deliberate self harm in adolescents: self report survey in schools in England. BMJ. 2002;325:1207–1211. doi: 10.1136/bmj.325.7374.1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jeon HJ. Depression and suicide. J Korean Med Assoc. 2011;54:370–375. [Google Scholar]
- 20.Bae SB, Woo JM. Suicide prevention strategies from medical perspective. J Korean Med Assoc. 2011;54:386–391. [Google Scholar]
- 21.Jeon HJ, Lee JY, Lee YM, Hong JP, Won SH, Cho SJ, Kim JY, Chang SM, Lee HW, Cho MJ. Unplanned versus planned suicide attempters, precipitants, methods, and an association with mental disorders in a Korea-based community sample. J Affect Disord. 2010;127:274–280. doi: 10.1016/j.jad.2010.05.027. [DOI] [PubMed] [Google Scholar]
- 22.American Academy of Child and Adolescent Psychiatry. Practice parameter for the assessment and treatment of children and adolescents with schizophrenia. American Academy of Child and Adolescent Psychiatry. J Am Acad Child Adolesc Psychiatry. 2001;40:4s–23s. doi: 10.1097/00004583-200107001-00002. [DOI] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention. Suicide prevention: youth suicide. Atlanta: Centers for Disease Control and Prevention; 2012. [Google Scholar]
- 24.Chen YY, Yip PS, Chan CH, Fu KW, Chang SS, Lee WJ, Gunnell D. The impact of a celebrity's suicide on the introduction and establishment of a new method of suicide in South Korea. Arch Suicide Res. 2014;18:221–226. doi: 10.1080/13811118.2013.824840. [DOI] [PubMed] [Google Scholar]
- 25.Suh S, Chang Y, Kim N. Quantitative exponential modelling of copycat suicides: association with mass media effect in South Korea. Epidemiol Psychiatr Sci. 2015;24:150–157. doi: 10.1017/S204579601400002X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Waern M, Sjöström N, Marlow T, Hetta J. Does the Suicide Assessment Scale predict risk of repetition? A prospective study of suicide attempters at a hospital emergency department. Eur Psychiatry. 2010;25:421–426. doi: 10.1016/j.eurpsy.2010.03.014. [DOI] [PubMed] [Google Scholar]
- 27.Currier GW, Fisher SG, Caine ED. Mobile crisis team intervention to enhance linkage of discharged suicidal emergency department patients to outpatient psychiatric services: a randomized controlled trial. Acad Emerg Med. 2010;17:36–43. doi: 10.1111/j.1553-2712.2009.00619.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.King CA, O'Mara RM, Hayward CN, Cunningham RM. Adolescent suicide risk screening in the emergency department. Acad Emerg Med. 2009;16:1234–1241. doi: 10.1111/j.1553-2712.2009.00500.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen CY, Yeh HH, Huang N, Lin YC. Socioeconomic and clinical characteristics associated with repeat suicide attempts among young people. J Adolesc Health. 2014;54:550–557. doi: 10.1016/j.jadohealth.2013.10.008. [DOI] [PubMed] [Google Scholar]