Abstract
Screening is important for early detection of colorectal cancer. Our aim was to determine whether a simple anticipated regret (AR) intervention could increase uptake of colorectal cancer screening. A randomised controlled trial of a simple, questionnaire-based AR intervention, delivered alongside existing pre-notification letters, was conducted. A total of 60,000 adults aged 50–74 years from the Scottish National Screening programme were randomised into the following groups: (1) no questionnaire (control), (2) Health Locus of Control questionnaire (HLOC) or (3) HLOC plus AR questionnaire. The primary outcome was return of the guaiac faecal occult blood test (FOBT). The secondary outcomes included intention to return test kit and perceived disgust (ICK). A total of 59,366 people were analysed as allocated (intention-to-treat (ITT)); no overall differences were seen between the treatment groups on FOBT uptake (control: 57.3%, HLOC: 56.9%, AR: 57.4%). In total, 13,645 (34.2%) individuals returned the questionnaires. Analysis of the secondary questionnaire measures showed that AR indirectly affected FOBT uptake via intention, whilst ICK directly affected FOBT uptake over and above intention. The effect of AR on FOBT uptake was also moderated by intention strength: for less-than-strong intenders only, uptake was 4.2% higher in the AR (84.6%) versus the HLOC group (80.4%) (95% CI for difference (2.0, 6.5)). The findings show that psychological concepts including AR and perceived disgust (ICK) are important factors in determining FOBT uptake. However, the AR intervention had no simple effect in the ITT analysis. It can be concluded that, in those with low intentions, exposure to AR may be required to increase FOBT uptake. The current controlled trials are presented at the website www.controlled-trials.com (number: ISRCTN74986452).
Keywords: Colorectal cancer, Screening, Anticipated regret, Faecal occult blood test, Disgust
Highlights
-
•
Colorectal cancer is a major cause of deaths worldwide; hence, screening is important for early detection.
-
•
Anticipated regret (AR) can lead to a significant increase in screening uptake.
-
•
A simple, questionnaire-based AR RCT intervention was tested on 60,000 participants.
-
•
No overall effect of the AR intervention on uptake was observed in the ITT analysis.
-
•
AR strengthened intentions and increased uptake in those with low intentions.
1. Introduction
Colorectal cancer is the second leading cause of death from cancer in many Western countries including the UK (SIGN, 2011). Screening is important for early detection, which in turn is associated with reduced mortality (Jørgensen et al., 2002). Therefore, many countries have introduced national programmes of colorectal cancer screening. In Scotland, all adults aged 50–74 years are invited, every 2 years, to complete a guaiac faecal occult blood test (FOBT) by collecting their own faecal samples and returning the test kit by post for testing. A recent matched cohort study found that this national programme has reduced the overall colorectal cancer mortality by 10%, and by 27% amongst those who returned a completed test kit (Libby et al., 2012).
Despite the clear benefits of screening, uptake is often suboptimal, with overall participation rarely exceeding 60% (von Euler-Chelpin et al., 2010). In Scotland, from November 2011 to October 2013, the participation rates ranged from 42% for men living in the most deprived areas to 68% for the least deprived women (ISD, 2014), indicating a common marked social gradient in participation. This social gradient is of particular concern, as poorer survival following a diagnosis of colorectal cancer is also associated with lower socio-economic status (von Euler-Chelpin et al., 2010). Thus, the potential benefit of FOBT screening, in terms of early detection and better survival, will depend on the level of uptake, therefore increasing this is a priority particularly amongst lower socio-economic groups.
A large (n = 60,000), randomised controlled trial (RCT) was conducted to investigate the efficacy of a simple pre-notification letter (with and without an explanatory booklet) within the Scottish national colorectal cancer screening programme. The results showed significantly higher uptake with both the pre-notification letter (59.0%) and the letter plus booklet (58.5%), than with the usual invitation without prior notification (53.9%) (Libby et al., 2011). Importantly, the increases were observed for men and women of all age groups and all deprivation categories, including the groups with the highest and lowest levels of uptake, that is, the least deprived women (letter 69.9%, usual invitation 66.6%) and the most deprived men (42.6% and 36.1%). This indicates that simple postal interventions can be effective in increasing FOBT uptake across all socio-economic groups. As a result of these findings, the pre-notification letter has become standard practice in the Scottish screening programme. However, many fail to reap the benefits of screening, for example, around 45% of people who are posted FOBT kits still do not complete and return them.
Health behaviours, such as screening participation, are considered to be shaped by the following two distinct systems: (1) a reflective, rational, goal-oriented system driven by values and intentions, requiring cognitive capacity and (2) an automatic, affective system, requiring little or no cognitive engagement, guided by immediate feelings and emotions (Strack and Deutsch, 2004). The emotion of ‘anticipated regret’ (AR) has been recently tested in health behaviour change interventions. Regret is a negative cognitive-based emotion experienced when an individual believes that the present situation could have been better had he or she acted differently. It is also possible to anticipate regret, and thus decide to take action to avoid actually experiencing this unpleasant emotion. AR may be particularly relevant to cancer screening, where a lack of screening may result in a poorer outcome if subsequently diagnosed (e.g., a more advanced and perhaps untreatable cancer). Abraham and Sheeran (2003) demonstrated that AR adds significantly to the prediction of intentions and exercise behaviour over and above the traditional attitudinal components of the theory of planned behaviour (TPB) (Ajzen, 1991). Further, the additional effect of AR has been observed across a range of health behaviours including those that may be considered protective (e.g., condom use and physical activity), risky (e.g., smoking and unhealthy diet) and/or preventive (e.g., dental check-ups and self-examination) (Conner et al., 2015; Sandberg and Conner, 2008; Sheeran et al., 2014). Essentially, AR strengthens behavioural intentions and drives people to action, because failing to act is associated with aversive emotions. AR has previously been tested in cervical cancer screening: Sandberg and Conner (2009) randomised women who were due to be invited for a screening into the following groups: (1) a control group, (2) a group sent a TPB questionnaire and (3) a group sent a TPB questionnaire plus two AR questions: ‘If I did not attend for a cervical smear in the next few weeks I would feel regret’ and ‘If I did not attend for a cervical smear in the next few weeks, I would later wish I had’. The overall screening attendance was 21%, 26% and 26%, respectively (i.e., simply sending out a questionnaire appeared to increase attendance by 5%). The attendance rates of those who completed and returned the questionnaire (i.e., those who were definitely exposed to the intervention) were 44% (TPB) and 65% (TPB plus AR). Compared with the 21% uptake in the control group, this represents a remarkable effect for so simple an intervention. In the context of colorectal cancer screening, Ferrer et al. (2012) tested the effect of loss- versus gain-framed messages and, consistent with previous research, found that loss-framed messages (i.e., where people are asked to consider the negative outcomes of not attending screening) were more effective in increasing intentions to screen. The authors speculated that AR and worry may be triggered in response to such loss-framed messages.
Another psychological barrier to participating in FOBT screening is the emotion of disgust (the ‘ICK’ factor: Morgan et al., 2008; O'Carroll et al., 2011). In a recent systematic review, Reynolds et al. (2012) concluded that anticipated disgust was a contributory factor in avoiding colorectal cancer screening. Reynolds et al. (2014) also demonstrated experimentally that trait disgust moderated the influence of state disgust on anticipated avoidance, specifically delaying seeking help for bowel symptoms. Another recent study of >6000 participants found that two major perceived barriers to colorectal cancer screening were commonly reported: ‘I do not want to handle my stool’ and ‘I do not want to keep my stools on a card in my house’ (Jones et al., 2010). Patients have also expressed discomfort or shame on posting their faecal samples in the mail (Chapple et al., 2008; Palmer et al., 2014). Other psychological factors possibly affecting participation in cancer screening are perceived benefit of screening and beliefs about control over one's health (Health Locus of Control (HLOC)) (Wallston et al., 1978), that is, the extent to which people believe their health and health outcomes are determined primarily by (a) themselves (internal), (b) chance/fate and (c) powerful others (e.g., doctors). It is hypothesised that individuals who believe their health is largely predetermined by fate (i.e., high chance) would be significantly less likely to participate in colorectal cancer screening.
For many years, it has been noted that health-related intentions, behaviour and/or related cognitions may change as a result of being measured, but the exact magnitude and mechanism of this effect is unclear. This has been called the mere-measurement effect (Sherman, 1980; Morwitz and Fitzsimons, 2004) or, more recently, the question–behaviour effect or QBE. In a recent review of this area, Rodrigues et al. (2015) stated: ‘Investigation of the QBE on health-related behaviors is important for research as well as for evidence-based practice in health care (French and Sutton, 2010). The positive implications of the QBE on behavior for health care practice is that many forms of measurement, such as self-report questionnaires, are inexpensive and could be distributed widely. If their completion is found to lead to desirable changes in behavior, then distributing questionnaires could potentially be a viable and cost-effective public health intervention’. Accordingly, the primary aim of the present study was to test the feasibility of a simple AR questionnaire-based manipulation, sent along with the standard FOBT pre-notification letter, to increase uptake of FOBT screening in Scotland across all socio-economic groups. In order to test the effect of AR, or a non-specific QBE, on any change in behaviour, participants were randomised into one of the following three treatment arms: (1) no questionnaire (control), (2) control (HLOC) questionnaire and (3) HLOC + AR questionnaire (AR). The additional aims were to evaluate any effects of demographic factors on uptake (i.e., age, gender and socio-economic status), and to examine the effect of psychological factors (AR, ICK, HLOC and perceived benefit) on FOBT uptake via a mediating and/or moderating effect on intentions.
2. Methods
The present study was a single-centre trial based at the Scottish Bowel Screening Centre in Dundee. Full details of methods for this RCT are reported in the protocol paper (O'Carroll et al., 2013) and at the website www.controlled-trials.com (number: ISRCTN74986452).
2.1. Participants
Based on the method described by Libby et al. (2011), a large, nationally representative sample of the general Scottish population were sent questionnaires via post. All of the participants were adults aged 50–74 years, who were participants in the screening programme, and due to be invited for screening within the study recruitment period (April to June 2013). As this was a questionnaire-based survey, the ethnicity of participants was not known. As seeking informed consent in the control arm was not feasible, doing so from those returning questionnaires would have confounded the results. Therefore, written informed consent was not sought from participants. This study was approved by the UK National Health Service (NHS) IRAS (Tayside NHS Board, East of Scotland Research Ethics Committee; REC ref. no. 12/ES/0092). All remaining procedures were carried out in accordance with the Helsinki declaration (1975, revised 2000). All patients currently included in the Scottish Bowel Screening Programme were eligible for this study, and there were no exclusion criteria for participation.
2.2. Measures
2.2.1. FOBT uptake
The primary outcome variable was return of an FOBT test kit to the central laboratory at the Scottish Bowel Screening Centre, within 6 months of the kit being posted (FOBT uptake). Data were supplied by the NHS Information Services Division from the screening database, and these were anonymously linked via a unique identifier with the questionnaire data. This data file also included anonymised demographic data (i.e., age, gender, Scottish Index of Multiple Deprivation (SIMD)), plus FOBT uptake history for previous invitation rounds, that is, the total number of previous rounds for which each participant had returned a kit, and the total number of previous rounds for which they had failed to return a kit. All available data on kits returned up to the time of data extraction were included, as any uptake in this period was consequent to the study pre-notification letter/questionnaire. Kits returned completely unused were designated as not having achieved FOBT uptake, whereas all other returned kits denoted FOBT uptake, as the behaviour of interest was simply returning a kit. We were not interested in whether there was a valid test result.
2.2.2. Secondary outcomes
All secondary outcomes on the two questionnaires were measured using simple one-to seven-point Likert-type scales from ‘strongly disagree’ to ‘strongly agree’. The 18-item Health Locus of Control (HLOC) (Wallston et al., 1978) is a well-used and validated measure that assesses beliefs about influences on health outcomes via three subscales (‘internal’ (HLOC I), ‘chance’ (HLOC C) and ‘powerful others’ (HLOC O)). This questionnaire showed good reliability in the current study (Cronbach's α: HLOC I = 0.71, HLOC C = 0.73, HLOC O = 0.74). Perceived disgust (ICK) and perceived benefit of FOBT screening were measured using modified versions of the ICK factor (four items, α = 0.87; e.g., ‘The idea of completing my test kit is somewhat disgusting’) and perceived benefit scales (two items, α = 0.52; e.g., ‘I am likely to benefit if I complete and return my test kit’), as reported by O'Carroll et al. (2011). Two items measured intention to return the FOBT kit (‘I will definitely complete and return my test kit’ and ‘I strongly intend to complete and return my test kit’) (α = 0.70). AR was measured by two items placed as the first question of the survey (‘If I did not complete and return my test kit, I would later feel regret’) and immediately preceding the final intention question (‘If I did not complete and return my test kit, I would later wish I had’), as described by Sandberg and Conner (2009) (α = 0.64). Placing AR items before intention has shown greater effects on behaviour (Abraham and Sheeran, 2003). Both questionnaires had identical items except for the two AR questions; these were replaced by two filler questions (regarding general awareness of the bowel screening programme) on the HLOC questionnaire in order to control for questionnaire length. The physical design of the questionnaire was based on the recommendations of a Cochrane review (Edwards et al., 2009) to increase response rate in this type of study (e.g., coloured ink, stamped (not franked) self-addressed return envelope and university sponsorship).
2.3. Procedure
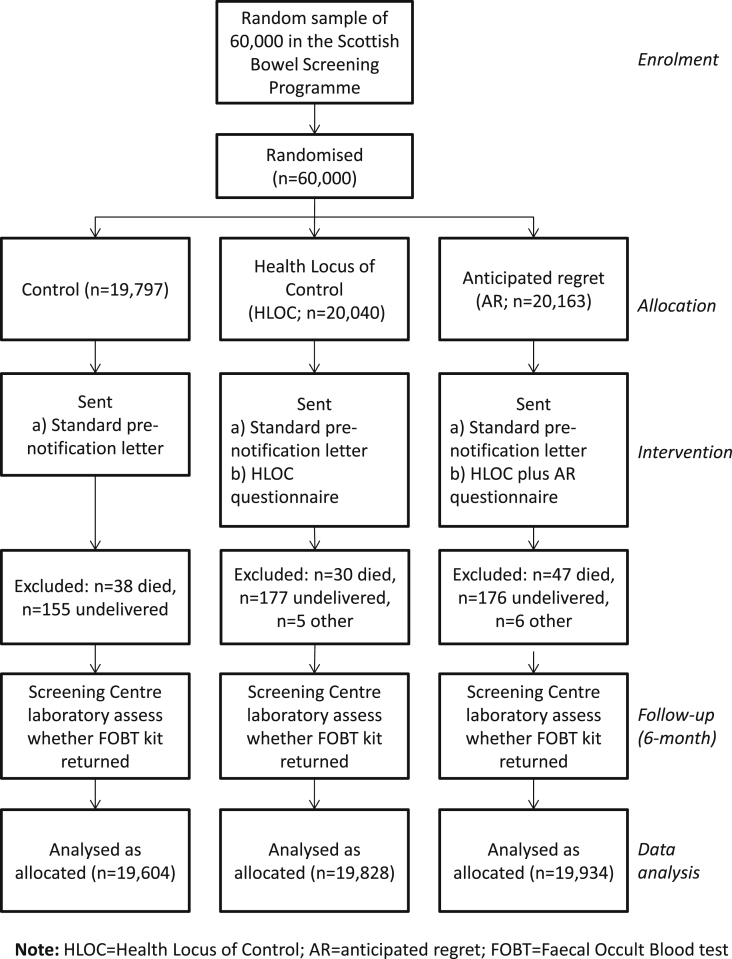
This study comprised a simple three-arm RCT: (1) no-questionnaire control group (2) HLOC questionnaire control group and (3) AR questionnaire group. The CONSORT diagram is shown in Fig. 1. Currently all participants in the Scottish Bowel Screening programme are sent a standard pre-notification letter 2 weeks before being sent a FOBT by post, which they are required to complete at home and then return to the laboratory at the bowel screening centre for analysis. For this study, the questionnaires were included along with the pre-notification letter.
Fig. 1.
CONSORT diagram.
2.3.1. Control
The control-arm participants were sent the standard pre-notification letter, according to current practice; thus, they are considered ‘treatment as usual’.
2.3.2. HLOC intervention
The HLOC group was sent the pre-notification letter plus a questionnaire comprising the HLOC scale, the ICK and perceived benefit items, and two items indicating intention to return their kit (e.g., ‘I will definitely complete and return my test kit’).
2.3.3. AR intervention
The AR group was sent the pre-notification letter and the same HLOC/ICK/perceived benefit/intentions questionnaire as the HLOC group plus the two additional AR questions; thus, the AR manipulation was tested after measuring the other secondary outcomes.
2.4. Randomisation
The participants were sampled and randomised via a computer by the external IT company that manages the Scottish Bowel Screening Centre IT database, which governs the national FOBT screening programme and identifies when individuals are invited to participate. Simple randomisation was used to allocate individuals to the control, HLOC or AR groups in a 1:1:1 ratio. The process of generating and mailing the pre-notification letters is fully automated, currently handled by a not-for-profit, mail-handling company. A data file containing contact details for the pre-notification letters is sent to the mail-handling company on a daily basis, and the questionnaires were added to the letters at the time of mailing. Therefore, the researchers were blinded to the allocation of the intervention to individuals. The following two additional variables were generated for the study participants: (a) a field representing the treatment arm and (b) a unique identifier printed on each pre-notification letter/questionnaire, which was used to record-link the data with each individual's subsequent FOBT return.
2.5. Statistical analysis
All analyses were carried out in SPSS version 19: χ2 was used to test the basic differences between treatment groups and logistic regression was used to assess the predictors of FOBT uptake in the intention-to-treat (ITT) analysis (where all participants were analysed as allocated (randomised) to treatment group). To examine the relationships between variables prior to the mediation and moderation analysis, first-order correlations for the secondary outcome measures and FOBT uptake were determined for those returning questionnaires. Spearman's rho (ρ) was used to assess first-order correlations as the secondary outcome variables were not normally distributed.
Bootstrapping procedures (based on 5000 samples) were used to estimate the confidence intervals (CIs) for indirect effects through the proposed mediators (Hayes, 2013). This method was chosen as it makes no assumptions about the distribution of indirect effects (Preacher and Hayes, 2004). The mediator variables were standardised before analysis to allow comparison of effect sizes. Significant mediator (indirect) effects were found when CIs excluded zero.
The moderator effects were examined via hierarchical regression incorporating interaction terms using bootstrapping analyses. Moderator variables were mean-centred before analysis as this renders hypotheses tests and regression coefficients more meaningful and interpretable (Hayes, 2013, p. 298). The mediators and moderators were analysed with the PROCESS computational tool developed by Hayes (2013) for use within SPSS.
Our extremely large sample size indicated that we could not rely on significant p-values, as ‘in very large samples, p-values go quickly to zero, and solely relying on p-values can lead the researcher to claim support for results of no practical significance’ (Min et al., 2013, p. 1). Effect sizes (including odds ratios, correlation coefficients and point estimates for bootstrapping analyses) and 95% CIs are therefore reported for all analyses, as these provide a range for the magnitude of the observed effect.
2.6. Power calculations
Following Libby et al. (2011), in a sample of 60,000 subjects, with 20,000 randomised to each of the three treatment groups, an increase in FOBT uptake of between 3% and 5% can be detected in all social deprivation groups with 80% power at the 5% level.
3. Results
3.1. Participants
60,000 participants were randomised to the control (n = 19,797), HLOC (n = 20,040) and AR (n = 20,163) treatment arms (Fig. 1). A number (n = 13) of questionnaires were not sent as the addresses were not in Scotland (and hence not eligible for screening). A further 621 participants were excluded from the analysis for various reasons such as not receiving the pre-notification letter (n = 115 died, n = 104 transferred out (of Scotland), n = 391 undelivered (e.g., ‘returned to sender’)), refusing/being unable to give consent (n = 7) (as indicated by a spouse or carer either telephoning on behalf of the participant or making a note on a blank returned questionnaire), or withdrawing from the screening programme (n = 4). There were no differences in exclusions by treatment group. Supplementary Table S1 shows the demographic data for the included participants by treatment group; no differences were observed between groups indicating successful randomisation.
3.2. Analysis as allocated (ITT)
Supplementary Table S2 shows the FOBT uptake by treatment group, age, gender, SIMD quintiles and history of returning kits for the ITT analysis (n = 59,366). Overall, 57.2% of the participants returned their FOBT kits at a mean of 27.7 days (standard deviation (SD) 24.3, Mdn = 19 days, range 1–276 days) after it was sent. No differences were observed between the three treatment groups, either overall (i.e., control: 57.3%, HLOC: 56.9%, AR: 57.4%) or by gender, age band, SIMD quintile or history of returning kits (see Electronic Supplementary Table S2), indicating that the intervention did not have any simple overall effect on FOBT uptake in the ITT analysis.
3.3. Logistic regression
Table 1 shows both the unadjusted and adjusted effects of the logistic regression analysis of the demographic variables, treatment group and history of returning kits on FOBT uptake for the ITT analysis (n = 59,366). The treatment group showed no effect. As expected, older age, lower deprivation (SIMD quintile) and female gender were all predictive of higher FOBT uptake. The strongest predictors of FOBT uptake were a greater number of previous kit returns and fewer previous failures to return a kit.
Table 1.
Logistic regression of FOBT uptake by treatment group unadjusted and adjusted for demographics and history of returning kits.
| Unadjusted odds ratio (95% CI) | aAdjusted odds ratio (95% CI) | |
|---|---|---|
| Treatment group: | ||
| Control | – | – |
| HLOC | 0.98 (0.94, 1.02) | 0.97 (0.91, 1.01) |
| AR | 1.00 (0.97, 1.05) | 1.00 (0.95, 1.06) |
| Gender: | ||
| Male | – | – |
| Female | 1.24 (1.20, 1.28) | 1.03 (0.98, 1.07) |
| Age: | ||
| 50–54 years | – | – |
| 55–59 years | 1.33 (1.27, 1.39) | 1.14 (1.06, 1.23) |
| 60–65 years | 1.62 (1.54, 1.71) | 1.34 (1.23, 1.45) |
| 66–69 years | 1.95 (1.85, 2.04) | 1.41 (1.31, 1.53) |
| 70–74 years | 1.68 (1.59, 1.77) | 0.99 (0.91, 1.07) |
| SIMD quintile: | ||
| 1 (Most deprived) | – | – |
| 2 | 1.36 (1.29, 1.44) | 1.21 (1.12, 1.30) |
| 3 | 1.68 (1.59, 1.77) | 1.36 (1.27, 1.46) |
| 4 | 2.09 (1.98, 2.20) | 1.57 (1.46, 1.69) |
| 5 (Least deprived) | 2.30 (2.18, 2.43) | 1.66 (1.55, 1.80) |
| No. of previous kits returned | 7.97 (7.72, 8.22) | 4.15 (3.97, 4.33) |
| No. of previous failures to return kit | 0.16 (0.16, 0.17) | 0.35 (0.33, 0.36) |
Adjusted for all other variables in the regression. Treatment group in both analyses and gender and 70–74 age band in the adjusted analysis are not considered significant (i.e., CI includes the value 1.0). FOBT = faecal occult blood test; AR = anticipated regret; HLOC = Health Locus of Control; SIMD = Scottish Index of Multiple Deprivation.
3.4. Questionnaire returns
Overall, 13,677 (34.4%) people returned questionnaires between May 2013 and February 2014. This represents a good response rate for a large-scale survey without reminders (c.f. Edwards et al., 2009). The questionnaires were returned at a mean of 18.9 days (SD 22.3, median = 11 days, range 2–280 days) after the questionnaire was sent. Time taken to return the questionnaire did not differ by treatment group, nor was it related to FOBT uptake; the difference between the time of FOBT uptake and time of questionnaire return was also not related to FOBT uptake. Slightly more participants in the HLOC group returned questionnaires (n = 6968, 35.1%) compared with the AR group (n = 6709, 33.7%; difference = 1.4%; 95% CI (0.5%, 2.4%)). Questionnaire return was related to older age, female gender, higher SIMD quintile, higher previous kit returns and lower previous failures to return a kit (see Electronic Supplementary Table S3).
3.4.1. Missing data
A small number (n = 32, 0.2%) of returned questionnaires were completely blank, thus were excluded from the analysis involving the questionnaire data (they are included in the ITT analysis). Therefore, 13,645 questionnaires were included in the secondary analyses of questionnaire data. Some questionnaires were incomplete; the amount of data missing for each individual item ranged from 0.3% to 1.6%. All secondary outcome measures (i.e., AR, intention, ICK, HLOC and perceived benefit) were calculated as means of available items. Multiple imputation was used to estimate means for all secondary outcome measures where fewer than 50% of items had been completed (n = 189 means, across n = 137 (0.1%) of returned questionnaires). Multiple imputation is the current preferred method of handling missing data in clinical trials (Graham, 2009). The data were imputed via the multiple imputation routine (fully conditional model) in SPSS with age, gender, SIMD quintile, previous kits returned, previous failures to return kit and the remaining secondary outcome measures as predictor variables. Single iteration was performed as the amount of missing data was very small. Imputed means were constrained to within 1–7.
3.4.2. FOBT uptake by treatment group
For those returning questionnaires (n = 13,645), FOBT uptake was extremely high (n = 12,393, 90.8%) but only 1% higher in the AR (n = 6113, 91.3%) than in the HLOC group (n = 6280, 90.3%) (mean difference 1.0%, odds ratio AR vs. HLOC = 1.13, 95% CI (1.01, 1.27)), indicating a possible QBE for both groups. However, it seems unlikely that merely returning a questionnaire could result in such a marked increase in FOBT uptake compared with the whole sample (n = 33,969, 57.2%); rather, it is somewhat likely that both FOBT uptake and questionnaire return were related to the same demographic (i.e., older age, less deprivation and female gender) and kit return history variables (i.e., more previous returns and fewer previous failures to return) (see Electronic Supplementary Tables S1 and S2).
3.4.3. Influence of secondary outcome measures on FOBT uptake
Table 2 shows the mean scores (columns 2–6) and first-order correlations (columns 7–13) of the outcome measures for those returning questionnaires. Higher AR showed a marked correlation with stronger intention (ρ = 0.62) and higher perceived benefit of screening (ρ = 0.57), and small associations with lower disgust (ICK) (ρ = −0.21) and higher internal health beliefs (HLOC Internal) (ρ = 0.19). Intention also showed a marked correlation with higher perceived benefit (ρ = 0.54) and a small association with lower ICK (ρ = −0.24). Higher perceived benefit was also related to lower ICK (ρ = −0.21) and higher HLOC Internal (ρ = 0.25). Health beliefs relating to chance (HLOC Chance) showed only a very small association with ICK (ρ = 0.17), and not intention, contrary to predictions. Intention was most associated with FOBT uptake (ρ = 0.37), followed by AR (ρ = 0.30), ICK (ρ = −0.28) and perceived benefit (ρ = 0.21). FOBT uptake was not found to be associated with any of the HLOC variables.
Table 2.
Mean (SD) by treatment group and first-order correlations of outcome measures.
| AR |
HLOC |
All |
M difference (95% CI) | Spearman's ρ |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
n |
6692 |
6953 |
13,645 |
6692 |
13,645 |
||||||
| M (SD) | M (SD) | M (SD) | AR | INT | ICK | PB | HI | HC | HO | ||
| AR | 6.19 (1.01) | – | – | ||||||||
| Intention (INT) | 6.62 (0.71) | 6.68 (0.72) | 6.65 (0.72) | 0.06 (0.04, 0.09) | 0.62 | ||||||
| ICK | 3.08 (1.47) | 3.06 (1.51) | 3.07 (1.49) | −0.02 (−0.07, 0.03) | −0.21 | −0.24 | |||||
| Perceived benefit (PB) | 6.47 (0.69) | 6.53 (0.69) | 6.50 (0.69) | 0.06 (0.04, 0.08) | 0.57 | 0.54 | −0.21 | ||||
| HLOC Internal (HI) | 4.91 (0.87) | 4.94 (0.86) | 4.93 (0.87) | 0.04 (0.01, 0.06) | 0.19 | 0.14 | −0.08 | 0.25 | |||
| HLOC Chance (HC) | 3.43 (1.07) | 3.41 (1.09) | 3.42 (1.08) | −0.02 (−0.06, 0.02) | −0.03 | −0.08 | 0.17 | −0.06 | −0.04 | ||
| HLOC Others (HO) | 3.91 (1.14) | 3.88 (1.17) | 3.89 (1.15) | −0.02 (−0.06, 0.02) | 0.14 | 0.01 | 0.02 | 0.16 | 0.24 | 0.34 | |
| aFOBT uptake | – | – | – | – | 0.30 | 0.37 | −0.28 | 0.21 | 0.00 | −0.07 | −0.02 |
Rank biserial correlation coefficient: 0.20 is considered the smallest effect for ‘practical significance’, 0.50 a moderate effect and 0.80 a large effect, according to recent studies (Ferguson, 2009); AR = anticipated regret; ICK = perceived disgust; HLOC = Health Locus of Control; FOBT = faecal occult blood test.
3.4.3.1. Mediator effects
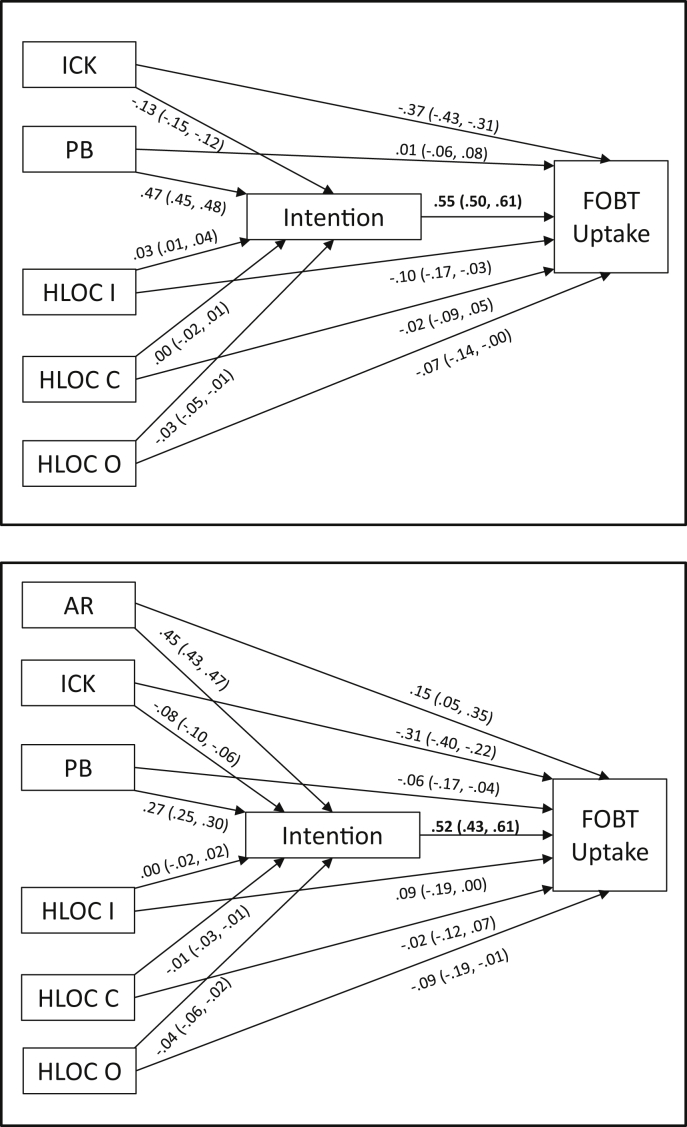
Table 3 shows the indirect effects of the secondary outcome measures via intention on FOBT uptake. The regression coefficients for the ‘a’ (effect of secondary outcome on intention), ‘b’ (effect of intention on FOBT uptake) and ‘c'’ (direct effect of secondary outcome on FOBT uptake) paths for all of those returning questionnaires and those in the AR group are shown in Fig. 2. Logistic regression was used in the bootstrapping analysis as FOBT uptake is a dichotomous variable.
Table 3.
Direct and indirect (via intention) effects of the secondary outcome variables on FOBT uptake.
| Direct effect | Indirect effects |
|||||
|---|---|---|---|---|---|---|
| Point estimate | Product of coefficients |
95% CI |
||||
| SE | Z | Lower | Upper | |||
| HLOC and AR groups (n = 13,645) | ||||||
| ICK | −0.37 | −0.07 | 0.01 | −13.27 | −0.09 | −0.06 |
| Perceived benefit | 0.01 | 0.26 | 0.02 | 18.97 | 0.23 | 0.29 |
| HLOC Internal | −0.10 | 0.01 | 0.00 | 3.22 | 0.005 | 0.02 |
| HLOC Chance | −0.02 | 0.00 | 0.00 | −0.42 | −0.01 | 0.01 |
| HLOC Others | −0.07 | −0.02 | 0.01 | −3.37 | −0.03 | −0.01 |
| AR group only (n = 6692) | ||||||
| AR | 0.15 | 0.23 | 0.02 | 10.91 | 0.19 | 0.28 |
| ICK | −0.31 | −0.04 | 0.01 | −6.85 | −0.06 | −0.03 |
| PB | −0.06 | 0.14 | 0.02 | 10.28 | 0.11 | 0.18 |
| HLOC Internal | 0.09 | 0.00 | 0.01 | 0.22 | −0.01 | 0.01 |
| HLOC Chance | −0.02 | −0.01 | 0.01 | −1.02 | −0.02 | 0.01 |
| HLOC Others | −0.09 | −0.02 | 0.01 | −3.68 | −0.03 | −0.01 |
Note: Based on 5000 bootstrapping samples; 95% CI = lower and upper level of the bias-corrected confidence intervals for α = 0.05: intervals are significant if they do not contain zero (Preacher and Hayes, 2004). Direct effects (including 95% CIs) are also shown in Fig. 2. FOBT = faecal occult blood test; AR = anticipated regret; ICK = perceived disgust; HLOC = Health Locus of Control.
Fig. 2.
Direct and indirect effects of secondary outcome variables via intentions on FOBT uptake: for both questionnaire groups (top: N = 13,645) and AR group only (bottom: N = 6692).
For both questionnaire-treated groups (HLOC and AR), the bootstrap analyses indicated a mediation effect for perceived benefit (point estimate 0.26, 95% CI (0.23, 0.29)), as well as a small effect for the ICK factor, and negligible effects for HLOC Internal and HLOC Others, but no effect for HLOC Chance (Table 3). The results indicate that the effect of perceived benefit on FOBT uptake could be explained chiefly by its association with intention (Fig. 2). The direct effect of intention on FOBT was very high (point estimate 0.55, 95% CI (0.50, 0.61)), and the secondary outcome measures predicted 26% of the variance in intention (r = 0.51, R2 = 0.26).
For the AR group only (i.e., including AR in the mediator analysis), the results of the bootstrap analyses indicate that there was an indirect effect for AR (point estimate 0.23, 95% CI (0.19, 0.28)). The effect of perceived benefit was smaller than that found for the whole sample (i.e., when AR was not entered into the analysis), indicating that perceived benefit also shared variance with AR. There were a small indirect effect of ICK and a negligible effect of HLOC others, but no effects for the remaining HLOC subscales (Table 3). The secondary outcome measures predicted 42% of the variance in intention (r = 0.65, R2 = 0.42), and the direct effect of intention on FOBT remained high (point estimate 0.52, 95% CI (0.43, 0.61)). In both analyses, the direct effects of ICK were much greater than any indirect effect via intentions, suggesting that ICK had a separate effect on FOBT uptake over and above the intention to return kit.
3.4.3.2. Moderator effect of AR and intention
The intention to return the FOBT kit was extremely high in those who returned questionnaires (mean = 6.5, SD = 0.7, median = 7) with marked ceiling effects (67.3% had a maximum score of 7). As determining the effect of the intervention on FOBT uptake was important in those uncertain of returning their kit, differences by treatment group for those with strong (i.e., mean > 6.5) versus less-than-strong intentions (mean ≤ 6.5) to return their kit were evaluated. This cut-off was chosen as the median score for intention equalled 7 (representing ‘strongly agree’ on both intention items).
For those with less-than-strong intentions, 4.2% more participants in the AR group returned their FOBT kit than in the HLOC group (84.6% (N = 2093/2473) vs. 80.4% (N = 1594/1982), odds ratio 1.34, 95% CI (1.15, 1.57)), whilst the difference in those with strong intentions was only 1% (AR: 95.3% (N = 4020/4219) vs. HLOC: 94.3% (N = 4686/4971), odds ratio 1.23, 95% CI (1.02, 1.48)). This indicated that any effect of the AR intervention on FOBT uptake may have been moderated by intention strength. The greatest effect sizes (i.e., difference in FOBT uptake between AR and HLOC groups) for those with less-than-strong intentions were observed in SIMD quintiles 1 (i.e., most deprived) (less-than-strong intentions: AR: 81.6% vs. HLOC: 74.0%, odds ratio 1.55, 95% CI (1.03, 2.34); strong intentions: 92.5% vs. 89.4%, odds ratio 1.46, 95% CI (0.94, 2.27)), 2 (less-than-strong intentions: 83.5% vs. 77.8%, odds ratio 1.45, 95% CI (1.001, 2.09); strong intentions: 94.5% vs. 94.4%, odds ratio 1.01, 95% CI (0.64, 1.58)) and 5 (i.e., least deprived) (less-than-strong intentions: 87.9% vs. 81.9%, odds ratio 1.60, 95% CI (1.14, 2.26); strong intentions: 96.6% vs. 95.6%, odds ratio 1.33, 95% CI (0.86, 2.04)).
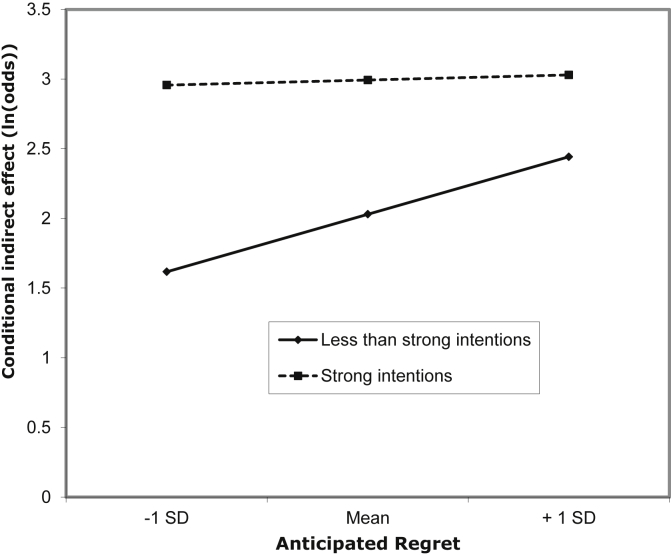
As intention has already been shown to mediate the AR–FOBT uptake association, a moderated mediation model was used to examine the interaction effect of AR with intention strength (i.e., strong vs. less-than-strong intentions) on FOBT uptake (Preacher et al., 2007). We examined intention strength as a moderator of AR, rather than the reverse, as this was consistent with the observed mediation effects of AR and intention; however, as moderation analysis is symmetrical, AR can also be considered as a moderator of intention. The moderation was tested via two bootstrapping analyses. First, AR predicted intention strength (β = 1.45, 95% CI (1.31, 1.60)). Subsequently, FOBT uptake was predicted by intention strength (β = 0.96, 95% CI (0.76, 1.17)), AR (β = 0.18, 95% CI (0.05, 0.30)) and the interaction of AR with intention strength (β = −0.38, 95% CI (−0.58, −0.17)) (see Electronic Supplementary Figure S1). This confirms that the effect of AR on FOBT uptake was moderated by intention strength. This association and the negative coefficient of the interaction term are consistent with the assumption that AR strengthened the association between intention and behaviour (FOBT uptake) for those with less-than-strong intentions. Table 4 shows the bootstrapped indirect effects on less-than-strong and strong intentions, and Fig. 3 shows the estimates of the indirect effects plotted for different values of AR. Each one-SD increase (i.e., 1.01) in the value of AR resulted in an approximately 50% increase in the odds of FOBT uptake for participants with less-than-strong intentions to return their kit, but no increase was observed for those with strong intentions, thus supporting a moderated mediation model.
Table 4.
Bootstrapped indirect effects of AR via intention strength on FOBT uptake.
| Intentions | Point estimate | SE | Z | 95% CI for point estimate |
aOdds ratio (95% CI) | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Less than strong | 0.41 | 0.04 | 9.34 | 0.33 | 0.50 | 1.51 (1.39, 1.65) |
| Strong | 0.04 | 0.09 | 0.39 | −0.15 | 0.22 | 1.04 (0.86, 1.25) |
Note: Based on 5000 bootstrapping samples; 95% CI = lower and upper level of the bias-corrected confidence interval for α = 0.05.
The estimated increase in odds of FOBT uptake for each one-standard deviation increase in AR score, evaluated at lower and high intention. AR = anticipated regret; FOBT = faecal occult blood test.
Fig. 3.
Indirect effect of anticipated regret (AR) on faecal occult blood test (FOBT) uptake at levels of intention strength evaluated at one SD below AR mean, AR mean and 1 SD above AR mean.
4. Discussion
A recent systematic review of the QBE (Rodrigues et al., 2015) made the following three recommendations: (1) QBE trials should be pre-registered, (2) publication bias should be avoided by publishing negative trial findings and (3) intervention procedures should be clearly described. The authors believe this study fulfils all three criteria. Contrary to expectations, no overall effect was observed on FOBT uptake of randomisation to treatment group. FOBT uptake in the current study was 1.1% higher than that observed in the two-year period from November 2011 to October 2013 for the whole of Scotland (57.2% vs. 56.1%) (ISD, 2014). However, the national figures only include kits resulting in a valid test result (negative or positive), whereas the figures in the present study are based on any kit returned (other than blank kits), including incorrectly completed (and therefore not testable) kits. Thus, the present study did not result in any notable increase over the national figures.
A QBE of both questionnaires could not be ruled out, as a very high FOBT uptake was seen in those returning questionnaires. However, those returning questionnaires were very motivated (had strong intentions) to return their FOBT kit; thus, it highly possible that a third factor (e.g., the personality trait conscientiousness) may have resulted in both questionnaire and kit return. No overall QBE of the AR was observed compared with the HLOC questionnaire, which is consistent with two questionnaire-based studies examining the effect of AR in addition to behavioural intention in blood donors (Godin et al., 2010, 2014). Godin et al. (2014) proposed that the lack of an additional effect of AR over the QBE on intention could be partly due to a low response rate and/or having no control over how carefully participants had read the questionnaire items, indicating that many participants may not have been fully exposed to the intervention. In the present study, AR was found to have an effect on those reporting less-than-strong intentions, indicating that anticipated future regret after not taking part in screening may have been more important than psychological measures in changing the behaviour of participants who were definitely exposed to the intervention. Importantly, this effect was observed across all socio-economic groups, but it was most impressive (7.6% difference) in the lowest SIMD quintile.
The strongest predictors of FOBT uptake were higher number of previous kits returned and fewer previous failures to return kit. Importantly, both higher self-reported AR and lower perceived disgust (ICK) had direct positive effects on FOBT uptake. The direct effect of AR on FOBT uptake was small; its main effect was to increase the participants' intention to return their kits, which in turn increased FOBT uptake. By contrast, ICK had a moderate effect on FOBT uptake over and above any effect of intention, supporting previous evidence that disgust may be a major barrier to colorectal cancer screening (Reynolds et al., 2012). Perceived benefit only influenced FOBT uptake via its effect on intention. Contrary to expectation, none of the HLOC belief subscales were related to FOBT uptake in this sample. However, the HLOC Chance scores in the present study were relatively low compared with other representative samples (e.g., Wardle and Steptoe, 2003). This result suggests that this group of participants returning questionnaires, who seemed predisposed to take part in healthy behaviours (i.e., had strong intentions to participate in screening), may not have been influenced by beliefs that chance is a major determinant of health outcomes.
For those definitely exposed to the intervention (i.e., returned a questionnaire), FOBT uptake was very high (90.8%), which reflects the strong intentions reported by this group. Therefore, those expressing less-than-strong intentions to return their kit were of interest. Amongst this subgroup, uptake was 4.2% higher in the AR versus the HLOC treatment arm. A 7.6% higher uptake was observed for the most deprived quintile, indicating that the AR intervention may have changed the behaviour of the chiefly targeted participants, that is, those from lower socio-economic groups who were uncertain of completing and returning their kit. The intention strength-moderated effect of the AR measure on FOBT uptake could result from the ceiling effect of intentions, as those with strong intentions were highly likely to return their kit. Nonetheless, the finding that AR increased FOBT uptake in those with less-than-strong intentions is important. Further, the observed increase in uptake in the AR group for those with less-than-strong intentions was similar to that achieved across the whole sample in participants who received a pre-notification letter, 2 weeks before the FOBT kit was sent by post (Libby et al., 2011). A 5% increase in FOBT uptake is estimated to translate into approximately 11 additional cancers diagnosed per 100,000 of the target population (Libby et al., 2012); thus, the observed increase of 4.2% is likely to be clinically important, providing it could be more widely achieved.
Despite using very similar methods to Sandberg and Conner (2009), the marked AR effect reported for cervical cancer screening could not be replicated, suggesting that the intervention did not generalise. Although Sandberg and Conner (2009) also observed much higher uptake of cervical screening amongst those who returned questionnaire than controls, a simple AR questionnaire conferred a distinct advantage over a TPB questionnaire in their research. Our findings highlight the limitations in translating existing approaches to different screening contexts. Thus, it is important to understand the underlying mechanisms of interventions. Participants may have very different perceptions of illness and treatment in relation to cervical versus colorectal cancer screening, which may attenuate any impact of AR on colorectal cancer screening, thus possibly explaining the differential findings (Lo et al., 2013). The ordering of AR items may have also affected the outcome; although AR was placed immediately before intention items according to previous guidance (Abraham and Sheeran, 2003), one of the AR–intention pairs formed the last two items on the questionnaire. Sandberg and Conner (2011) found that placing all AR items at the beginning was more effective in increasing behaviour than when they were mixed throughout the questionnaire. In addition, the current questionnaire contained a second affective measure, that is, ICK, which was completed in both the HLOC and AR groups. Whilst tapping affective factors may promote behaviour, adding additional affective items (e.g., AR to ICK) may not confer any additional advantage. The strengths of the current study include the large sample size, indicating the generalisability of the results, and the use of an objective outcome measure of behaviour. The study's limitations include a lack of data on ethnicity, as they were not recorded in the screening database, and the questionnaires did not collect any personal information. In addition, people choosing to return a questionnaire were also very likely to return their kit, indicating that data on the secondary outcome measures for those not participating in screening were limited. The findings are consistent with the assumption that completing a questionnaire was a prerequisite for behaviour change; up to 66% of participants in the present study may not have been exposed to the AR intervention (i.e., they may have disposed of the questionnaire without reading it), which is a significant limitation. Godin et al. (2010, p. 642) also observed that completion, and not just receipt, of a questionnaire may be necessary for QBEs to be detected. It is important to note that, although many chose not to complete the questionnaire, return of questionnaires did not appear to have any detrimental effect on kit return. However, as the HLOC variables did not show marked correlation with FOBT uptake, a shorter questionnaire omitting these variables may have been more acceptable and therefore more effective in achieving exposure to the AR intervention.
5. Conclusions
The findings show that psychological concepts including AR and perceived disgust (ICK) are important factors that determine FOBT uptake. However, the AR intervention did not have any simple effect on the ITT analysis, indicating that exposure to the intervention was not sufficiently achieved by merely posting a simple questionnaire. Nonetheless, AR was effective in strengthening participants' intention to return a FOBT kit in those with less-than-strong intentions who had definite exposure to the intervention (i.e., completed a questionnaire). Therefore, AR manipulations could be effective in increasing FOBT uptake, providing a wider population could be successfully exposed. Other methods of delivering the AR intervention may be worth examining, for example, a shorter questionnaire or inclusion in the text of information leaflets and/or the pre-notification letter itself. As the history or returning kits was the strongest predictor of FOBT uptake, targeting interventions at first-time participants, before they have established a pattern of non-participation, may result in the greatest long-term gains.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
This project was funded by a grant from the Scottish Government, Department of Health, Chief Scientist Office, grant reference number CZH/4/763.
Footnotes
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.socscimed.2015.07.026.
Contributor Information
Ronan E. O'Carroll, Email: reo1@stir.ac.uk.
Julie A. Chambers, Email: jac2@stir.ac.uk.
Linda Brownlee, Email: linda.brownlee@nhs.net.
Gillian Libby, Email: g.libby@dundee.ac.uk.
Robert J.C. Steele, Email: r.j.c.steele@dundee.ac.uk.
Appendix A. Supplementary data
The following are the supplementary data related to this article:
Electronic Supplementary Table S1. Demographics by treatment group (N = 59,366).
Electronic Supplementary Table S2. FOBT uptake by treatment group, age band, gender and SIMD quintile (N = 59,366).
Electronic Supplementary Table S3. Questionnaire return rates by age, gender and SIMD quintile (N = 39,762).
Electronic Supplementary Fig. S1. Results of regression analyses for moderated mediation.
References
- Abraham C., Sheeran P. Acting on intentions: the role of anticipated regret. Br. J. Soc. Psychol. 2003;42:495–511. doi: 10.1348/014466603322595248. [DOI] [PubMed] [Google Scholar]
- Ajzen I. The theory of planned behaviour. Organ. Behav. Hum. Decis. Process. 1991;50:179–211. [Google Scholar]
- Chapple A., Ziebland S., Hewitson P., McPherson A. What affects the uptake of screening for bowel cancer using a faecal occult blood test (FOBT): a qualitative study. Soc. Sci. Med. 2008;66:2425–2435. doi: 10.1016/j.socscimed.2008.02.009. [DOI] [PubMed] [Google Scholar]
- Conner M., McEachan R., Taylor N., O'Hara J., Lawton R. Role of affective attitudes and anticipated affective reactions in predicting health behaviors. Health Psychol. 2015;34:642–652. doi: 10.1037/hea0000143. [DOI] [PubMed] [Google Scholar]
- Edwards P.J., Roberts I.G., Clarke M.J., DiGuiseppi C., Wentz R., Kwan I., Cooper R., Felix L., Pratap S. Methods to increase response rates to postal questionnaires. Cochrane Database Syst. Rev. 2009;(2) doi: 10.1002/14651858.MR000008.pub3. [DOI] [PubMed] [Google Scholar]
- Ferguson C.J. An effect size primer: a guide for clinicians and researchers. Prof. Psychol. Res. Pract. 2009;40:532–538. [Google Scholar]
- Ferrer R.A., Klein W.M., Zajac L.E., Land S.R., Ling B.S. An affective booster moderates the effect of gain-and loss-framed messages on behavioral intentions for colorectal cancer screening. J. Behav. Med. 2012;35:452–461. doi: 10.1007/s10865-011-9371-3. [DOI] [PubMed] [Google Scholar]
- French D.P., Sutton S. Reactivity of measurement in health psychology: how much of a problem is it? What can be done about it? Br. J. Health Psychol. 2010;15:453–468. doi: 10.1348/135910710X492341. [DOI] [PubMed] [Google Scholar]
- Godin G., Germain M., Conner M., Delage G., Sheeran P. Promoting the return of lapsed blood donors: a seven-arm randomised controlled trial of the question-behaviour effect. Health Psychol. 2014;33:646–655. doi: 10.1037/a0033505. [DOI] [PubMed] [Google Scholar]
- Godin G., Sheeran P., Conner M., Delage G., Germain M., Bélanger-Gravel A., Naccache H. Which survey questions change behaviour? Randomized controlled trial of mere measurement interventions. Health Psychol. 2010;29:636–644. doi: 10.1037/a0021131. [DOI] [PubMed] [Google Scholar]
- Graham J. Missing data analysis: making it work in the real world. Annu. Rev. Psychol. 2009;60:549–576. doi: 10.1146/annurev.psych.58.110405.085530. [DOI] [PubMed] [Google Scholar]
- Hayes A.F. Guilford Press; NY: 2013. Introduction to Mediation, Moderation and Conditional Process Analysis: a Regression-based Approach. [Google Scholar]
- ISD (Information Services Division), NHS Scotland . 2014. Scottish Bowel Screening Programme Key Performance Indicators Report: Invitations between 1 November 2011 and 31 October 2013.www.isdscotland.org/Health-topics/Cancer/Bowel-Screening on 11.2.2015 Downloaded from: [Google Scholar]
- Jones R.M., Woolf S.H., Cunningham T.D., Johnson R.E., Krist A.H., Rothemich S.F., Vernon S.W. The relative importance of patient-reported barriers to colorectal cancer screening. Am. J. Prev. Med. 2010;38:499–507. doi: 10.1016/j.amepre.2010.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jørgensen O.D., Kronborg O., Fenger C. A randomised study of screening for colorectal cancer using faecal occult blood testing: results after 13 years and 7 biennial screening rounds. Gut. 2002;50:29–32. doi: 10.1136/gut.50.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Libby G., Bray J., Champion J., Brownlee L.A., Birrell J., Gorman D.R., Crighton E.M., Fraser C.G., Steele R.J. Pre-notification increases uptake of colorectal cancer screening in all demographic groups: a randomized controlled trial. J. Med. Screen. 2011;8:24–29. doi: 10.1258/jms.2011.011002. [DOI] [PubMed] [Google Scholar]
- Libby G., Brewster D., McClements P.L., Carey F.A., Black R.J., Birrell J., Fraser C.G., Steele R.J. The impact of population-based faecal occult blood test screening on colorectal cancer mortality: a matched cohort study. Br. J. Cancer. 2012;107:255–259. doi: 10.1038/bjc.2012.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo S.H., Waller J., Wardle J., von Wagner C. Comparing barriers to colorectal cancer screening with barriers to breast and cervical screening: a population-based survey of screening-age women in Great Britain. J. Med. Screen. 2013;20:73–79. doi: 10.1177/0969141313492508. [DOI] [PubMed] [Google Scholar]
- Min M., Lucas H.C., Jr., Shmuel G. Too big to fail: large samples and the P-Value problem. Inf. Syst. Res. 2013;24:906–917. [Google Scholar]
- Morgan S.E., Stephenson M.T., Harrison T.R., Afifi W.A., Long S.D. Facts versus ‘feelings’: how rational is the decision to become an organ donor? J. Health Psychol. 2008;13:644–658. doi: 10.1177/1359105308090936. [DOI] [PubMed] [Google Scholar]
- Morwitz V.G., Fitzsimons G.J. The mere-measurement effect: why does measuring intentions change actual behaviour? J. Consum. Psychol. 2004;14:64–73. [Google Scholar]
- O'Carroll R.E., Foster C., McGeechan G., Sandford K., Ferguson E. The “ick” factor, anticipated regret, and willingness to become an organ donor. Health Psychol. 2011;30:236–245. doi: 10.1037/a0022379. [DOI] [PubMed] [Google Scholar]
- O'Carroll R.E., Steele R., Brownlee L., Libby G., Chambers J.A. Anticipated regret to increase uptake of colorectal cancer screening in Scotland (ARTICS): study protocol for a randomised controlled trial. BMC Public Health. 2013;13:849. doi: 10.1186/1471-2458-13-849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmer C.K., Thomas M.C., von Wagner C., Rain R. Reasons for non-uptake and subsequent participation in the NHS Bowel Cancer Screening Programme: a qualitative study. Br. J. Cancer. 2014;110:1705–1711. doi: 10.1038/bjc.2014.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher K.J., Hayes A.F. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav. Res. Methods Instrum. Comput. 2004;36:717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Preacher K.J., Rucker D.D., Hayes A.F. Assessing moderated mediation hypotheses: theory, methods, and prescriptions. Multivar. Behav. Res. 2007;42:185–227. doi: 10.1080/00273170701341316. [DOI] [PubMed] [Google Scholar]
- Reynolds L.M., Consedine N.S., Pizarro D.A., Bissett I.P. Disgust and behavioral avoidance in colorectal cancer screening and treatment: a systematic review and research agenda. Cancer Nurs. 2012;32:122–130. doi: 10.1097/NCC.0b013e31826a4b1b. [DOI] [PubMed] [Google Scholar]
- Reynolds L.M., McCambridge S.A., Bissett I.P., Consedine N.S. Trait and state disgust: an experimental investigation of disgust and avoidance in colorectal cancer decision scenarios. Health Psychol. 2014;33:1495–1506. doi: 10.1037/hea0000023. [DOI] [PubMed] [Google Scholar]
- Rodrigues A.M., O'Brien N., French D.P., Glidewell L., Sniehotta F.F. The question–behavior effect: genuine effect or spurious phenomenon? A systematic review of randomized controlled trials with meta-analyses. Health Psychol. 2015;34:61–78. doi: 10.1037/hea0000104. [DOI] [PubMed] [Google Scholar]
- Sandberg T., Conner M. Anticipated regret as an additional predictor in the theory of planned behaviour: a meta-analysis. Br. J. Soc. Psychol. 2008;47:589–606. doi: 10.1348/014466607X258704. [DOI] [PubMed] [Google Scholar]
- Sandberg T., Conner M. A mere measurement effect for anticipated regret: impacts on cervical screening attendance. Br. J. Soc. Psychol. 2009;48:221–236. doi: 10.1348/014466608X347001. [DOI] [PubMed] [Google Scholar]
- Sandberg T., Conner M. Using self-generated validity to promote exercise behaviour. Br. J. Soc. Psychol. 2011;50:769–783. doi: 10.1111/j.2044-8309.2010.02004.x. [DOI] [PubMed] [Google Scholar]
- Sheeran P., Harris P.R., Epton T. Does heightening risk appraisals change people's intentions and behavior? A meta-analysis of experimental studies. Psychol. Bull. 2014;140:511–543. doi: 10.1037/a0033065. [DOI] [PubMed] [Google Scholar]
- Sherman S.J. On the self-erasing nature of errors of prediction. J. Pers. Soc. Psychol. 1980;39:211–221. [Google Scholar]
- SIGN (Scottish Intercollegiate Guidelines Network) SIGN; Edinburgh: 2011. Guideline No. 126: Diagnosis and Management of Colorectal Cancer. [Google Scholar]
- Strack F., Deutsch R. Reflective and impulsive determinants of social behavior. Pers. Soc. Psychol. Rev. 2004;8:220–247. doi: 10.1207/s15327957pspr0803_1. [DOI] [PubMed] [Google Scholar]
- von Euler-Chelpin M., Brasso K., Lynge E. Determinants of participation in colorectal cancer screening with faecal occult blood testing. J. Public Health. 2010;32:395–405. doi: 10.1093/pubmed/fdp115. [DOI] [PubMed] [Google Scholar]
- Wallston K.A., Wallston B.S., DeVellis R. Development of the Multidimensional Health Locus of Control (MHLC) scales. Health Educ. Monogr. 1978;6:160–170. doi: 10.1177/109019817800600107. [DOI] [PubMed] [Google Scholar]
- Wardle J., Steptoe A. Socioeconomic differences in attitudes and beliefs about healthy lifestyles. J. Epidemiol. Community Health. 2003;57:440–443. doi: 10.1136/jech.57.6.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.