Abstract
Objectives:
The aim of the current study was to examine the longitudinal relationship between bedtimes and body mass index (BMI) from adolescence to adulthood in a nationally representative sample.
Design:
Three waves of data from the National Longitudinal Study of Adolescent Health were used to assess the bedtimes and BMI of 3,342 adolescents between 1994 and 2009. Hypotheses were tested with hierarchical linear models using a two-level, random intercept and slopes model.
Results:
Later average bedtime during the workweek, in hours, from adolescence to adulthood was associated with an increase in BMI over time (b = 0.035 kg/m2 per min later bedtime per 6 years; standard error = 0.016; t = 2.12, degrees of freedom = 3,238, P < 0.05). These results remained significant after controlling for demographic characteristics and baseline BMI. Although sleep duration, screen time, and exercise frequency did not attenuate the relationship between workday bedtime and BMI over time, fast-food consumption was recognized as a significant partial mediator of the relationship between bedtimes and BMI longitudinally.
Conclusions:
The results highlight bedtimes as a potential target for weight management during adolescence and during the transition to adulthood.
Citation:
Asarnow LD, McGlinchey E, Harvey AG. Evidence for a possible link between bedtime and change in body mass index. SLEEP 2015;38(10):1523–1527.
Keywords: bedtime, BMI, longitudinal, obesity, sleep
INTRODUCTION
The World Health Organization has identified obesity as a global epidemic1 with rates of obesity, poor diet, and inadequate exercise rapidly rising in children, adolescents, and adults.2–4 Obesity is a multisystem disease with potentially devastating consequences for physical5–10 and emotional health11–14 across the lifespan.
In adolescence, circadian timing is of critical importance. Approximately 40% of teens select later bedtimes, a pattern of behavior often referred to as an evening circadian preference or eveningness.15–17 With the onset and progression of puberty, evening preference adolescents exhibit a delayed sleep schedule, whereby they increase activity later in the day and both go to sleep and get up later.18 Indeed, Price et al.19 reported that 60% of 11th and 12th graders who were surveyed reported that they “enjoyed staying up late.”
An eveningness circadian pattern has been linked to risk for obesity in a handful of studies. Gonnissen et al.20 reported that, in a sample of 13 adults who were experimentally induced into either phase advanced or phase delayed circadian misalignment, eating and sleeping at unusual times of day resulted in a disturbed glucose and insulin metabolism. A study by Spaeth et al.,21 in a large sample of adults, provides direct experimental evidence that delaying bedtimes for 5 nights (and thereby reducing sleep duration) results in significant weight gain within a single week. Moreover, in a sample of 52 adults, Baron et al.22 showed that individuals with later bedtimes tended to consume meals later in the day than those with earlier bedtimes. Compared to those with earlier bedtimes, individuals with later bedtimes ate fewer fruits and vegetables and consumed an average of 248 more calories, most of which were consumed at dinner or after 20:00. Fleig and Randler23 found that later sleep timing in adolescents on non-school days was associated with greater “fast food” consumption. In a large sample of Australian adolescents, those with late bedtimes were 1.47 times more likely to be overweight or obese than those with early bedtimes and more than twice as likely to be obese.24 Moreover, later bedtimes are associated with more screen time,25 which is associated with obesity26 and increased daytime sleepiness, which is associated with decreased physical activity.27 The cross-sectional and experimental data indicate that bedtime is important to consider when identifying risks for obesity.
Regular insufficient sleep and excessive daytime sleepiness is another serious epidemic among adolescents. In several studies with large samples of adolescents, researchers reported that between 45% and 80% of adolescents experience insufficient sleep on school nights.28,16
Although the evidence is inconsistent, there is growing literature indicating a relationship between risk for obesity and both insufficient sleep in adults and children and too much sleep in adults. In a meta-analysis, Cappuccio et al.29 concluded that cross-sectional studies from around the world show a consistent increased risk of obesity amongst children who are sleep deprived, and also a 60% to 80% increase in the odds of being sleep deprived for obese children. Other researchers have found that the relationship between sleep and risk for obesity in adults holds to a curvilinear relationship, where both too much sleep and too little sleep is associated with adverse impacts on metabolic health.30,31 Thus, sleep is a plausible partial mediator of the association between bedtime and weight gain.32
To the best of our knowledge, there have been no longitudinal observational studies examining the relationship between bedtime and change in body mass index (BMI). We endeavored to explore whether later bedtimes would be associated with an increase in BMI from adolescence to adulthood and whether the relationship would be partially mediated by sleep duration, fast-food consumption, screen time, and exercise frequency in a longitudinal nationally representative data set.
METHODS
Sample
The National Longitudinal Study of Adolescent Health (Add Health) is a longitudinal study in the United States that contains data on the health and behavior of adolescents who were in grades 7 to 12 in the first two waves of the study and 18 to 32 years of age in the third and fourth waves. Surveys were administered at home and in school to adolescents and their parents at wave I from September 1994 to April 1995. There were three follow-up interviews: wave II in April-August 1996, wave III in July 2001–April 2002, and wave IV in January 2008–February 2009. The current study only included data from participants in waves II through IV of data collection. A stratified random sampling of US high schools was included (79% of targeted schools agreed to participate). The collection of data followed informed consent procedures approved by the institutional review board at the University of North Carolina, Chapel Hill. The clustered sampling design was school based. Several eligible high schools were selected and stratified by region, urbanicity, school type, ethnic mix, and size, which resulted in a final sample of 132 discrete schools. The current analysis used the public-use data from the Add Health dataset. The public-use dataset consists of one half of the core sample that completed an in-home interview and includes an overs-ample of African-American adolescents with a parent with a college degree.
Measures
Sleep/circadian variables were determined via self-report measures at all three waves. In wave II, all participants were in school. Therefore, workday bedtime in wave II was defined by response to the question “During the school year, what time do you usually go to bed on week nights?” In waves III and IV, workday bedtime was defined by response to the question “On days when you go to work, school, or similar activities, what time do you usually go to bed?” Workday bedtime was a continuous variable; standard clock times were converted into variables representing the number of hours and minutes from noon, such that larger numbers indicate later bedtimes. For example, individuals going to bed at 01:30 have a bedtime of 13.5 and individuals going to bed at 23:30 have a bedtime of 11.5.
Sleep duration was investigated as a potential partial mediator. Rise times were not available at wave II; therefore, wave II workday estimated total sleep time (TST) was defined by response to the question “How many hours of sleep do you usually get?” In waves III and IV workday TST was calculated based on the workday bedtime and rise time reported at each wave. Workday TST was a continuous variable, formatted in hours with additional minutes as fractions of hours.
Investigators measured height and weight at each wave, from which BMI was calculated. BMI in adolescents and children is typically converted to a z-score because body fat percentage changes as a child develops and in growing children BMI also varies by sex. Therefore, BMI in children and adolescents is not age and sex adjusted and thereby does not accurately reflect norms unless converted to a z-score. However, in the current study, we are interested in change in an individuals' BMI over time, and the age-adjusted norms are less relevant. Moreover, in the current study age and sex have been included as covariates to account for age-related differences in BMI. Some previous studies that examined individual changes in BMI across this developmental period also did not use age-adjusted BMI values.33–35
Fast-food consumption, television viewing, and exercise were included as potential partial mediators. Fast-food consumption is a continuous variable, defined by the number of times the adolescent endorsed having consumed fast food in the past week. Fast-food consumption was collected at all three waves. Screen time per week is a continuous variable collected at each wave of data collection and was determined by response to the question “How many hours a week do you watch television?” Exercise frequency at wave II is a continuous variable and was defined by response to the question “During the past week, how many times did you exercise, such as jogging, walking, doing karate, jumping rope, doing gymnastics or dancing?” Questions assessing exercise frequency were inconsistent across waves, posing a methodological challenge in assessing exercise frequency across waves. Therefore, exercise frequency was based only on data from wave II in the current study.
Demographic characteristics controlled for included age (continuous; collected at all three waves), race/ethnicity (African American, Hispanic, Asian/Pacific Islander, Native American, or white), and welfare status (one parent receiving public assistance or no parent receiving public assistance).
A proxy for puberty was obtained via self-reported menarche for girls and levels of voice change for boys. Previous research has shown that voice change is a good indicator of puberty for boys.36–38 For voice change, boys were asked, “Is your voice lower now than it was when you were in grade school?” We combined some responses to create three categories for boys' voice change (none, a little/somewhat, a lot/a whole lot of change). For menarche, girls were asked the following yes/ no question: “Have you ever had a menstrual period (menstruated)?” Pubertal status data were only collected at wave II.
Statistical Analyses
We tested whether later bedtimes would be associated with an increase in BMI from adolescence to adulthood with hierarchical linear models (HLM) using a two-level, random intercept and slopes model. The HLM analyses were completed using maximum likelihood estimation with STATA 12 software (StatCorp, College Station, TX, 2011), utilizing methods for cluster design survey data. All measures were centered at the individual mean. Preliminary analyses determined that there was a linear trend in the repeated measures for BMI (intraclass correlation coefficient [ICC] = 0.75; χ2 = 0; degrees of freedom [df] = 3,238; P < 0.001) and workday bedtime (ICC 0.36; χ2 = 0; df = 3,238; P < 0.001).
Longitudinal mediation analyses were conducted to explore whether sleep duration, fast-food consumption, screen time, and exercise frequency acted as partial mediators of the relationship between bedtimes and BMI. The first multivariate model (model 1) included age, wave II BMI, race/ethnicity pubertal status, welfare status, and biological sex. The theorized mediating variables of sleep duration, fast-food consumption, screen time, and exercise frequency were progressively added in subsequent models (models 2, 3, 4, and 5) to test whether these variables acted as mediators of the relationship between bedtime and BMI. We considered an attenuation of 10% in the beta between bedtimes and BMI after including TST as a covariate to be consistent with mediation on an a priori basis.
RESULTS
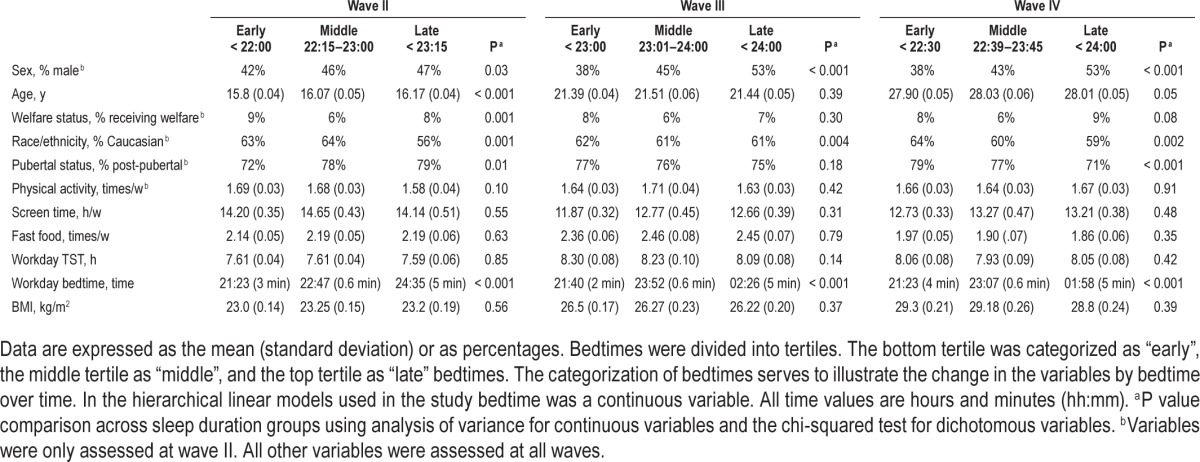
A total of 3,342 participants comprised the sample for the current study. Table 1 displays analyses on the relationship between weekday bedtime, covariates, and potential mediators across waves.
Table 1.
Predictor, covariate, and potential mediator variables by workday bedtime across waves.
Results for the tests of whether later bedtimes were associated with an increase in BMI from adolescence to adulthood are shown in Table 2. Later average workday bedtime (b = 0.048; standard error [SE] = 0.017; t = 2.80, df = 3,238, P < 0.05) was associated with an increase in BMI controlling for age, wave II BMI, pubertal status, welfare status, and sex. In addition, even after controlling for covariates and potential mediators (sleep duration, fast food consumption, exercise frequency, and screen time) later average workday bedtime was associated with an increase in BMI (b = 0.035; SE = 0.016; t = 2.12, df = 3,238, P < 0.05).
Table 2.
Hierarchical linear models assessing the relationship between bedtime and body mass index and models assessing the contribution of potential mediators.
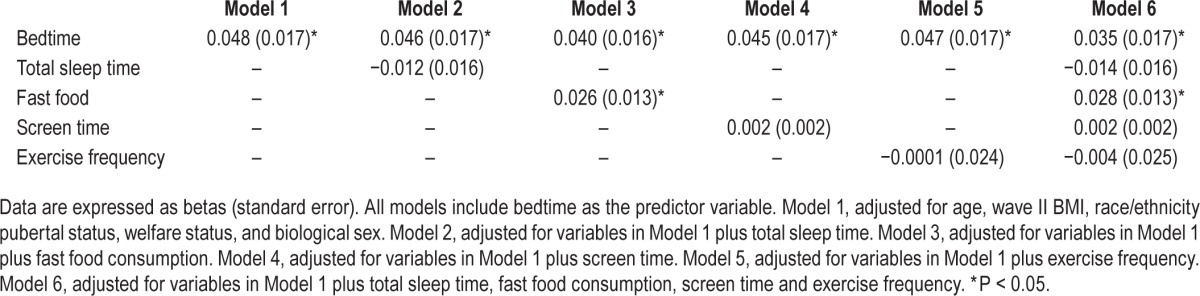
Results for the tests to evaluate sleep duration, fast-food consumption, exercise frequency, and screen time as potential mediators in the relationship between bedtimes and BMI longitudinally are displayed in Table 2. The relationship between bedtime and BMI was not appreciably attenuated with the inclusion of sleep duration, exercise frequency, and screen time in subsequent models 2, 4, and 5, indicating that these variables did not act as mediators of the relationship between bedtime and BMI. However, the relationship between bedtime and BMI was appreciably attenuated with the inclusion of fast-food consumption (model 3).
No significant interactions were found between age and sleep duration and age and bedtime during the workweek (all Ps > 0.28).
DISCUSSION
To the best of our knowledge, this is the first study to investigate the longitudinal relationship between bedtimes and BMI in any age group in an observational study. Our results indicate that later average bedtime during the workweek from adolescence to adulthood was associated with an increase in BMI over time in a nationally representative sample of more than 3,000 participants. Going to bed during the workweek each additional hour later is associated with an increase of 2.1 BMI kg/m2 (calculated by multiplying the beta (0.035) from the fully adjusted model by 60 min/h). Indeed, a chronic pattern of late sleep timing (over a period of 13–15 years) has been previously demonstrated to contribute to metabolic disturbance,20 which in turn may contribute to the physiologic processes underlying the steeper increase in BMI observed in this study.
Our results were not consistent with sleep duration, screen time, or exercise acting as partial mediators of the relationship between bedtimes and BMI longitudinally. Although surprising that these factors were not significant mediators, this finding supports the importance of considering bedtime in future research regarding the relationship between sleep and BMI. Conversely, fast-food consumption was a significant partial mediator of the relationship between bedtimes and BMI longitudinally. The effect of later bedtimes upon dietary habits therefore represents a potential target for future research and intervention.
The results of the current study should be interpreted within the confines of several limitations. First, “gold standard” measures for sleep and circadian rhythms such as sleep diary, actigraphy,39 and forced desynchrony protocols40 were not used. However, the Add Health questions used as proxies are often used as an index of TST and bedtime preference.41,42 Second, all of the sleep data included in this study are based on self-report. Although adolescents appear to be largely accurate and reliable on self-report measures,43 it can be difficult to accurately estimate one's sleep duration, bedtime, and wake times. For example, participants may have been influenced by biases such as most recent night or most salient night sleep44 and adolescents may have incorporated their weekend bedtimes and total sleep times into their assessment of what is “usual.” Although impractical in large epidemiological studies, future research in smaller samples should endeavor to use the “gold standard” tools to improve the contribution to knowledge.45 Third, measurements of waist circumference would have been valuable. Unfortunately, waist circumference measurements were not available at all three waves. Although BMI is a ratiometric measurement that accounts for variation in height over weight,46 it cannot distinguish between lean muscle and abdominal fat. Fourth, Add Health questions assessing exercise frequency were inconsistent across waves and therefore exercise frequency across waves was not available. Instead, exercise frequency at wave II was included as a covariate. Future research should investigate how exercise frequency over time may contribute to the relationship between bedtime and BMI. Last, loss to follow-up (n = 52) was related to baseline levels of BMI in the current study (t = 3.62, P = 0). The reasons for this pattern of findings are unknown. No other variables were related to loss to follow-up.
In conclusion, to our knowledge, this is the first study to investigate the relationship between bedtime and BMI longitudinally in an observational study. Later average bedtime during the workweek in the years from adolescence to adulthood was associated with an increase in BMI across that period. These results remained significant even after controlling for sleep duration, baseline BMI, demographic characteristics, screen time, exercise frequency, and fast-food consumption. Our results highlight adolescent bedtimes as a potential target for weight management concurrently and in the transition to adulthood.
DISCLOSURE STATEMENT
This project was supported by a National Science Foundation Graduate Research Fellowship DGE 1106400 awarded to Dr. Asarnow, a National Institute of Mental Health Grant T32MH016434 awarded to Dr.McGlinchey, and grant 1R01HD071065-01A1 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development awarded to Dr. Harvey. This research uses data from Add Health, a program project designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris, and funded by a grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 17 other agencies. Special acknowledgment is due Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. Persons interested in obtaining data files from Add Health should contact Add Health, Carolina Population Center, 123 W. Franklin Street, Chapel Hill, NC 27516-2524 (addhealth@unc.edu). No direct support was received from grant P01-HD31921 for this analysis.
This research uses data from the AHAA study, which was funded by a grant (R01 HD040428-02, Chandra Muller, PI) from the National Institute of Child Health and Human Development, and a grant (REC-0126167, Chandra Muller, PI, and Pedro Reyes, Co-PI) from the National Science Foundation. This research was also supported by grant, 5 R24 HD042849, Population Research Center, awarded to the Population Research Center at The University of Texas at Austin by the Eunice Kennedy Shriver National Institute of Health and Child Development. Opinions reflect those of the authors and do not necessarily reflect those of the granting agencies.
The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.World Health Organization. World health statistics 2006. Geneva, Switzerland: WHO Press; 2006. [Google Scholar]
- 2.Ebbeling CB, Pawlak DB, Ludwig DS. Childhood obesity: public-health crisis, common sense cure. Lancet. 2002;360:473–82. doi: 10.1016/S0140-6736(02)09678-2. [DOI] [PubMed] [Google Scholar]
- 3.Wang Y, Lobstein T. Worldwide trends in childhood overweight and obesity. IJPO. 2006;1:11–25. doi: 10.1080/17477160600586747. [DOI] [PubMed] [Google Scholar]
- 4.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA. 2006;295:1549–55. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 5.Calamaro CJ, Mason TB, Ratcliffe SJ. Adolescents living the 24/7 lifestyle: effects of caffeine and technology on sleep duration and daytime functioning. Pediatrics. 2009;123:e1005–10. doi: 10.1542/peds.2008-3641. [DOI] [PubMed] [Google Scholar]
- 6.Ford ES, Galuska DA, Gillespie C, Will JC, Giles WH, Dietz WH. C-reactive protein and body mass index in children: findings from the Third National Health and Nutrition Examination Survey, 1988-1994. J Pediatr. 2001;138:486–92. doi: 10.1067/mpd.2001.112898. [DOI] [PubMed] [Google Scholar]
- 7.Ludwig DS, Ebbeling CB. Type 2 diabetes mellitus in children: primary care and public health considerations. JAMA. 2001;286:1427–30. doi: 10.1001/jama.286.12.1427. [DOI] [PubMed] [Google Scholar]
- 8.Redline S, Tishler PV, Schluchter M, Aylor J, Clark K, Graham G. Risk factors for sleep-disordered breathing in children. Associations with obesity, race, and respiratory problems. Am J Resp Crit Care. 1999;159:1527–32. doi: 10.1164/ajrccm.159.5.9809079. [DOI] [PubMed] [Google Scholar]
- 9.Figueroa-Munoz JI, Chinn S, Rona RJ. Association between obesity and asthma in 4-11 year old children in the UK. Thorax. 2001;56:133–7. doi: 10.1136/thorax.56.2.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gunnell DJ, Frankel SJ, Nanchahal K, Peters TJ, Davey Smith G. Childhood obesity and adult cardiovascular mortality: a 57-y follow-up study based on the Boyd Orr cohort. Am J Clin Nutr. 1998;67:1111–8. doi: 10.1093/ajcn/67.6.1111. [DOI] [PubMed] [Google Scholar]
- 11.Hill AJ, Silver EK. Fat, friendless and unhealthy: 9-year old children's perception of body shape stereotypes. Int J Obesity. 1995;19:423–30. [PubMed] [Google Scholar]
- 12.Sjoberg RL, Nilsson KW, Leppert J. Obesity, shame, and depression in school-aged children: a population-based study. Pediatrics. 2005;116:e389–92. doi: 10.1542/peds.2005-0170. [DOI] [PubMed] [Google Scholar]
- 13.Stunkard AJ, Faith MS, Allison KC. Depression and obesity. Biol Psychiatry. 2003;54:330–7. doi: 10.1016/s0006-3223(03)00608-5. [DOI] [PubMed] [Google Scholar]
- 14.Roberts RE, Deleger S, Strawbridge WJ, Kaplan GA. Prospective association between obesity and depression: evidence from the Alameda County Study. Int J Obesity. 2003;27:514–21. doi: 10.1038/sj.ijo.0802204. [DOI] [PubMed] [Google Scholar]
- 15.Roenneberg T, Kuehnle T, Pramstaller PP, et al. A marker for the end of adolescence. Curr Biol. 2004;14:R1038–9. doi: 10.1016/j.cub.2004.11.039. [DOI] [PubMed] [Google Scholar]
- 16.Tonetti L, Fabbri M, Natale V. Sex difference in sleep-time preference and sleep need: a cross-sectional survey among Italian pre-adolescents, adolescents, and adults. Chronobiol Int. 2008;25:745–59. doi: 10.1080/07420520802394191. [DOI] [PubMed] [Google Scholar]
- 17.Carskadon MA, Acebo C, Richardson GS, Tate BA, Seifer R. An approach to studying circadian rhythms of adolescent humans. J Biol Rhythm. 1997;12:278–89. doi: 10.1177/074873049701200309. [DOI] [PubMed] [Google Scholar]
- 18.Carskadon MA, Vieira C, Acebo C. Association between puberty and delayed phase preference. Sleep. 1993;16:258–62. doi: 10.1093/sleep/16.3.258. [DOI] [PubMed] [Google Scholar]
- 19.Price VA, Coates TJ, Thoresen CE, Grinstead OA. Prevalence and correlates of poor sleep among adolescents. Arch Pediatr Adolesc Med. 1978;132:583–6. doi: 10.1001/archpedi.1978.02120310047009. [DOI] [PubMed] [Google Scholar]
- 20.Gonnissen HK, Rutters F, Mazuy C, Martens EA, Adam TC, Westerterp-Plantenga MS. Effect of a phase advance and phase delay of the 24-h cycle on energy metabolism, appetite, and related hormones. Am J Clin Nutr. 2012;96:689–97. doi: 10.3945/ajcn.112.037192. [DOI] [PubMed] [Google Scholar]
- 21.Spaeth AM, Dinges DF, Goel N. Effects of experimental sleep restriction on weight gain, caloric intake, and meal timing in healthy adults. Sleep. 2013;36:981–90. doi: 10.5665/sleep.2792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baron KG, Reid KJ, Kern AS, Zee PC. Role of sleep timing in caloric intake and BMI. Obesity. 2011;19:1374–81. doi: 10.1038/oby.2011.100. [DOI] [PubMed] [Google Scholar]
- 23.Fleig D, Randler C. Association between chronotype and diet in adolescents based on food logs. Eating Behav. 2009;10:115–8. doi: 10.1016/j.eatbeh.2009.03.002. [DOI] [PubMed] [Google Scholar]
- 24.Olds TS, Maher CA, Matricciani L. Sleep duration or bedtime? Exploring the relationship between sleep habits and weight status and activity patterns. Sleep. 2011;34:1299–307. doi: 10.5665/SLEEP.1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Giannotti F, Cortesi F, Sebastiani T, Vagnoni C. Sleeping habits in Italian children and adolescents. Sleep Biol Rhythm. 2005;3:15–21. [Google Scholar]
- 26.Gortmaker SL, Must A, Sobol AM, Peterson K, Colditz GA, Dietz WH. Television viewing as a cause of increasing obesity among children in the United States, 1986-1990. Arch Pediatr Adolesc Med. 1996;150:356. doi: 10.1001/archpedi.1996.02170290022003. [DOI] [PubMed] [Google Scholar]
- 27.Whitney CW, Enright PL, Newman AB, Bonekat W, Foley D, Quan SF. Correlates of daytime sleepiness in 4578 elderly persons: the Cardiovascular Health Study. Sleep. 1998;21:27–36. doi: 10.1093/sleep/21.1.27. [DOI] [PubMed] [Google Scholar]
- 28.National Sleep Foundation. 2006 Sleep in America Poll. Washington DC: National Sleep Foundation; 2006. Available at: http://sleepfoundation.org/sites/default/files/2006_summary_of_findings.pdf. [Google Scholar]
- 29.Cappuccio FP, Taggart FM, Kandala NB, et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31:619–26. doi: 10.1093/sleep/31.5.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chaput JP, Leblanc C, Perusse L, Despres JP, Bouchard C, Tremblay A. Risk factors for adult overweight and obesity in the Quebec Family Study: have we been barking up the wrong tree? Obesity. 2009;17:1964–70. doi: 10.1038/oby.2009.116. [DOI] [PubMed] [Google Scholar]
- 31.Gangwisch JE, Heymsfield SB, Boden-Albala B, et al. Sleep duration as a risk factor for diabetes incidence in a large US sample. Sleep. 2007;30:1667–73. doi: 10.1093/sleep/30.12.1667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Marshall NS, Glozier N, Grunstein RR. Is sleep duration related to obesity? A critical review of the epidemiological evidence. Sleep Med Rev. 2008;12:289–98. doi: 10.1016/j.smrv.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 33.Gordon-Larsen P, Adair LS, Nelson MC, Popkin BM. Five-year obesity incidence in the transition period between adolescence and adulthood: the National Longitudinal Study of Adolescent Health. Am J Clin Nutr. 2004;80:569–75. doi: 10.1093/ajcn/80.3.569. [DOI] [PubMed] [Google Scholar]
- 34.Berkey CS, Rockett HR, Gillman MW, Field AE, Colditz GA. Longitudinal study of skipping breakfast and weight change in adolescents. IJPO. 2003;27:1258–66. doi: 10.1038/sj.ijo.0802402. [DOI] [PubMed] [Google Scholar]
- 35.Hancox RJ, Milne BJ, Poulton R. Association between child and adolescent television viewing and adult health: a longitudinal birth cohort study. Lancet. 2004;364:257–62. doi: 10.1016/S0140-6736(04)16675-0. [DOI] [PubMed] [Google Scholar]
- 36.Benjet C, Hernández-Guzmán L. A short-term longitudinal study of pubertal change, gender, and psychological well-being of Mexican early adolescents. J Youth Adolescence. 2002;31:429–42. [PubMed] [Google Scholar]
- 37.Cota-Robles S, Neiss M, Rowe DC. The role of puberty in violent and nonviolent delinquency among Anglo American, Mexican American, and African American boys. J Adolesc Res. 2002;17:364–76. [Google Scholar]
- 38.Ge X, Conger RD, Elder GH., Jr Pubertal transition, stressful life events, and the emergence of gender differences in adolescent depressive symptoms. Dev Psychol. 2001;37:404–17. doi: 10.1037//0012-1649.37.3.404. [DOI] [PubMed] [Google Scholar]
- 39.Sadeh A, Alster J, Urbach D, Lavie P. Actigraphically based automatic bedtime sleep-wake scoring: validity and clinical applications. J Ambul Mon. 1989;2:209–16. [Google Scholar]
- 40.Dijk D-J, Czeisler CA. Contribution of the circadian pacemaker and the sleep homeostat to sleep propensity, sleep structure, electroencephalographic slow waves, and sleep spindle activity in humans. J Neurosci. 1995;15:3526–38. doi: 10.1523/JNEUROSCI.15-05-03526.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Asarnow LD, McGlinchey E, Harvey AG. The effects of bedtime and sleep duration on academic and emotional outcomes in a nationally representative sample of adolescents. J Adolesc Health. 2014;54:350–6. doi: 10.1016/j.jadohealth.2013.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Crowley SJ, Acebo C, Carskadon MA. Sleep, circadian rhythms, and delayed phase in adolescence. Sleep Med. 2007;8:602–12. doi: 10.1016/j.sleep.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 43.Winters KC, Stinchfield RD, Henly GA, Schwartz RH. Validity of adolescent self-report of alcohol and other drug involvement. Int J Addict. 1990;25:1379–95. doi: 10.3109/10826089009068469. [DOI] [PubMed] [Google Scholar]
- 44.Schacter DL. The seven sins of memory: how the mind forgets and remembers. New York, NY: Houghton Mifflin Harcourt; 2002. [Google Scholar]
- 45.Buysse DJ, Ancoli-Israel S, Edinger JD, Lichstein KL, Morin CM. Recommendations for a standard research assessment of insomnia. Sleep. 2006;29:1155–73. doi: 10.1093/sleep/29.9.1155. [DOI] [PubMed] [Google Scholar]
- 46.Tirosh A, Shai I, Afek A, et al. Adolescent BMI trajectory and risk of diabetes versus coronary disease. N Engl J Med. 2011;364:1315–25. doi: 10.1056/NEJMoa1006992. [DOI] [PMC free article] [PubMed] [Google Scholar]


