Abstract
Purpose
The aim of this project was to develop a biomechanically based quantification of the Balance Error Scoring System (BESS) using data derived from the accelerometer and gyroscope of a mobile tablet device.
Methods
Thirty-two healthy youth and adults completed the BESS while an iPad was positioned at the sacrum. Data from the iPad data was compared to position data gathered from a 3D motion capture system. Peak-to-peak (P2P), normalized path length (NPL), and root mean squared (RMS) were calculated for each system and compared. Additionally, a 95% ellipsoid volume, iBESS volume, was calculated using center of mass (COM) movements in the anterior-posterior (AP), mediolateral (ML), and trunk rotation planes of movement to provide a comprehensive, 3-dimensional metric of postural stability.
Results
Across all kinematic outcomes, data from the iPad were significantly correlated with the same outcomes derived from the motion capture system (Rho range: 0.37- 0.94, p<0.05). The iBESS volume metric was able to detect a difference in postural stability across stance and surface, showing a significant increase in volume in increasingly difficult conditions, while traditional error scoring was not as sensitive to these factors.
Conclusions
The kinematic data provided by the iPad is of sufficient quality relative to motion capture data to accurately quantify postural stability in healthy young adults. The iBESS volume provides a more sensitive measure of postural stability than error scoring alone, particularly in conditions 1 and 4, which often suffer from floor effects, and condition 5, which can experience ceiling effects. The iBESS metric is ideally suited for clinical and in the field applications in which characterizing postural stability is of interest.
Keywords: postural stability, accelerometer, gyroscope, concussion, iBess, BESS
Introduction
The annual reported incidence of sport-related concussions has been estimated between 1.6 to 3.8 million (10). Concussion results in multi-system impairments, typically transitory, most often including declines in cognitive and motor performance, postural stability and vestibular function (11, 15). Based on the consensus statement from the 4th International Conference on Concussion, optimal management of concussion necessarily consists of an interdisciplinary team including certified athletic trainers, physicians, physical therapists and other medical professionals (11). A fundamental challenge that limits the effectiveness of interdisciplinary care teams with diverse training is the lack of systematic and consensus based assessments of neurologic function. A solution to this challenge is to develop objective and quantitative outcomes of the neurological domain of interest. Recently, the National Athletic Trainers’ Association (NATA) position statement regarding the management of sport concussion recommended that objective assessment of balance be included as a fundamental component in the management of concussion as postural stability provides a window into motor control processes and how concussion may impact these processes (2). While clinical balance assessments have become the standard of care due to convenience and feasibility in the field, their ability to provide an objective and reliable measure of postural control and stability has been questioned (4, 7). Biomechanical measures of postural stability, including computerized dynamic posturography (CDP), force platforms and 3D motion capture systems are more sensitive in detecting subtle deficits in postural stability not captured with subjective clinical assessments of balance and postural stability (5, 6, 14). While traditional, laboratory-based biomechanical approaches to measuring postural stability are accurate and objective, these approaches have not been broadly implemented in clinical settings. The time and financial costs of testing, large space requirements, expensive specialized equipment, lack of portability and potential to disrupt clinical workflow serve as major barriers to adoption. The development and integration of an accurate method of quantifying postural stability that is portable while simultaneously being affordable and conducive to integration in the field and clinical environments addresses a fundamental need in the management of concussion: the objective quantification of postural stability across the concussion spectrum (from injury to return to play) that can be shared across providers.
The primary clinical balance test developed specifically for concussion assessment and most often used clinically and described in the literature is the Balance Error Scoring System (BESS) (3, 8, 16, 17). The BESS is an inexpensive and portable technique designed to estimate postural stability (8, 16, 17) and has been adopted as the clinical standard of care for balance assessment in concussion (11, 17). Its three stances on firm ground have been incorporated into the Sport Concussion Assessment Tool 3 (SCAT3) to provide an assessment of the motor domain of neurologic function (11). The BESS manipulates somatosensory and visual afferent inputs by requiring participants to maintain postural stability with feet together, on one leg, and with feet in tandem for 20-second trials with eyes closed on both firm and foam surfaces. Postural stability is assessed by a test administrator who observes the athlete/patient perform each condition and counts errors committed. Any of the following would be counted as an error: 1) lifting hands off iliac crests; 2) opening eyes; 3) a step, stumble, or fall; 4) moving the hip into greater than 30 degrees of flexion or abduction; 5) lifting the forefoot or heel; and, 6) remaining out of correct testing position for more than five seconds (8, 17). Each type of error is scored equally and error scores for each of the six conditions, with a maximum of 10 per condition, are summed to provide a total BESS score (range 0-60) where higher error scores suggest greater postural instability (8, 17).
Validation of the BESS as a measure of postural stability was originally performed by comparing error scores with postural sway metrics measured by force platforms (17). Original data indicated modest to moderately high correlation coefficients comparing error scores and target sway measures for five of the six conditions (the exception being double-leg stance on firm surface) (17). While intraclass correlation coefficient (ICC) values measuring inter-rater reliability were originally reported as moderately high, a recent study by Finnoff and colleagues reported a substantially lower inter-rater reliability ICC of 0.57 for the total BESS score, with individual conditions ranging from 0.44 – 0.83 (7). Relationships involving double-leg stance on firm surface could not be determined as no errors were observed for this condition (7). Their results indicated that only one condition (single limb stance on firm surface) had inter-rater reliability ICC above 0.75, leading the authors to conclude “the remaining stance positions and the total BESS score appear to be invalid postural stability measures.” (7) Additionally, Finnoff and colleagues reported intra-rater reliability ICC of 0.74 for the total BESS score (0.50 – 0.88 for individual conditions), further highlighting the inconsistencies in scoring test performance (7). Collectively, these data provide rationale for the development of an objective and quantitative balance metric whose outcomes are determined using biomechanics, which will facilitate consistent evaluation of motor control function across providers.
Recently, Brown and colleagues used seven inertial measurement units (IMU's) on healthy participants performing the BESS in an effort to overcome the subjectivity of the BESS scoring system (4). Interestingly, their primary outcome was the relationship between subjective BESS error scoring and IMU data (linear acceleration and angular velocity) from each landmark, and their aim was to determine an algorithm with the fewest number of sensors that accurately predicted BESS scores. The algorithm they chose had high correlation with mean total BESS error scores and used only linear acceleration data from the IMU affixed at the forehead and no data from the IMU's affixed to other body segments. Further analysis revealed that the algorithm fit accurately with error scores only under the foam conditions, not for the subset of firm conditions. While the study by Brown and colleagues provided insight into the relationship between kinematic outcomes and BESS errors, it did not provide a true measure of postural stability, hence departing from the original approach used in the development of the BESS (17); rather, a measure was developed related to error scoring, a subjective metric whose reliability and validity has been questioned (7). The error scoring method employs a subjective approach to quantify discreet losses of balance or the frequency that balance strategies are used in the maintenance of postural stability over the course of the 20-second trial. Conversely, objective biomechanical measures of postural stability track the kinematics and kinetics of human movement during balance. Given that balance has been considered an “unbiased indicator of concussion severity” (4), it is sensible to use technology to gather kinematic data and utilize biomechanical approaches to processing these data to provide an unbiased indicator of postural stability. Characterizing actual postural stability, rather than fitting kinematic data to a subjective total error score across multiple conditions has greater utility in understanding the precise effects of concussion on postural stability and its recovery over time. An objective measure of postural stability in conditions that evaluate somatosensory and visual afferent inputs that is free of subjective scoring would provide clinical value in the form of reduced variability of assessment for concussion management teams that typically consists of multiple providers from various disciplines.
Recently, we demonstrated that a prevalent consumer electronics tablet, the Apple iPad (Apple, Inc. Cupertino, CA, USA), provided kinematic data of sufficient precision and quality to accurately characterize postural stability during performance of the NeuroCom Sensory Organization Test (SOT, Natus Medical, Inc. Clackamas, OR, USA) (1). Bland-Altman analysis demonstrated that Equilibrium Scores (ES) calculated using accelerometer and gyroscope data from the iPad were nearly identical to the NeuroCom ES (1). We also demonstrated that anterior-posterior (AP) center of gravity (COG) sway calculated with iPad sensor data was similar to the NeuroCom's COG measurement for all trials, with a mean difference of -0.010 degree of COG sway.
In addition to characterizing postural stability using anterior-posterior (AP) movement, the accelerometer and gyroscope within the tablet also collect medial-lateral (ML), and trunk-rotation movements (TR). Using data from all three planes of movement, we have recently shown correlation between inertial sensors within the iPad and three-dimensional (3D) motion analysis in a cohort of healthy older adults (12). While participants completed six balance tasks of varying difficulty, four summative metrics were computed using data from the iPad and motion capture: 1) Peak-to-peak (P2P) which measures displacement amplitude, 2) normalized path length (NPL), 3) root mean square distance (RMS) which measures magnitude of center of mass (CoM) displacement, and 4) ellipsoid volume, a metric containing the center of points of sway in 3D with 95% probability. The summative metrics computed using data from the iPad correlated significantly with motion capture computations for all six balance tasks. Furthermore, five of the six balance tasks (all but double limb support with eyes open on firm ground) demonstrated significance in discriminating the postural stability of individuals with Parkinson's disease from healthy age-matched controls (13).
The aim of this project was to address a fundamental gap in the assessment of postural stability in athletes: objectively quantify postural stability during performance of the BESS using technology that is scalable in terms of portability and affordability. Our approach was to first validate the accuracy of the iPad by comparing summative metrics of postural stability across the iPad and motion capture systems. Next, data from the iPad were used to develop an objective measure of postural stability for each of the six BESS conditions: a 3D 95% ellipsoid volume termed the iBESS volume.
Methods
Participants
Thirty-two neurologically healthy high school and college-aged students (14 male; 18 female; mean age = 20.9 years) participated in this study at the Cleveland Clinic Biomechanics Laboratory. All participants met the following criteria: 1) age 18-25 years; 2) no history of concussion in the previous six months; 3) no known neurological disorder or no known musculoskeletal injury, condition or surgery that would affect their balance; and, 4) no knee or ankle injury in the previous six months. All participants completed the informed consent process that was approved by the Cleveland Clinic Institutional Review Board.
Testing Procedure
Participants completed all six conditions of the Balance Error Scoring System (BESS): 1) double leg stance on firm surface; 2) single leg stance on firm surface; 3) tandem stance on firm surface; 4) double leg stance on foam surface; 5) single leg stance on foam surface and 6) tandem stance on foam surface. Per BESS instructions, participants wore socks for all trials, and were instructed to stand as still as possible for 20 seconds with eyes closed and hands resting on their iliac crests (17). Standardized instructions for completing the BESS were read aloud to each participant and the administrator demonstrated each task before testing (17). The same trained and experienced test administrator monitored the participant and scored each stance according to the standardized BESS scoring instructions previously published (17) and described above. All BESS trials were videotaped for verification of error scoring by a group of trained personnel.
Quantitative Data Collection
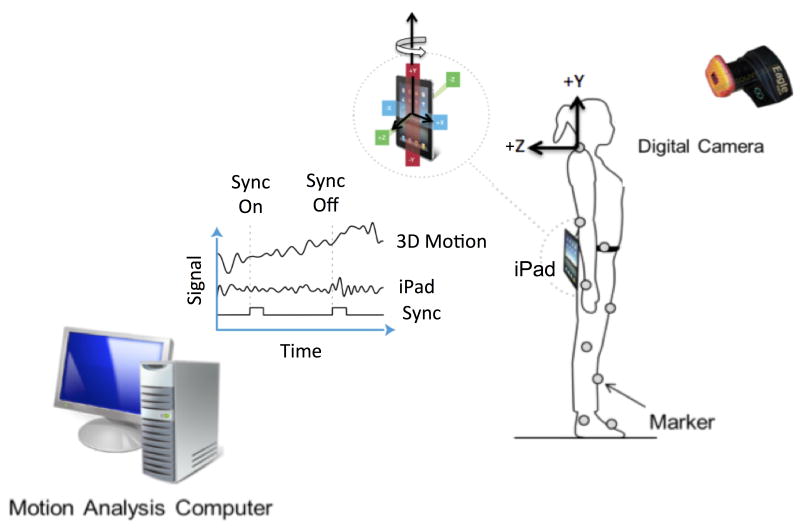
Figure 1 illustrates the experimental set-up with the iPad and biomechanical data collection model. Participants wore loose clothing, t-shirts and shorts, and completed each BESS condition with an iPad positioned securely at the sacral-level, the approximate center of mass (CoM) during upright stance, using a belt with customized housing for the iPad. In addition, 25 retro-reflective markers were placed at bony landmarks that were consistent with the Helen Hayes marker-set (9, 12). The motion capture system sampled the 3D position data of each reflective marker at 100 Hz using 8 infrared Eagle digital cameras and Cortex Software (Motion Analysis Corporation Eagle System; Santa Rosa, CA). The iPad tablet collected linear and angular acceleration from the embedded accelerometer (ST Micro LIS331DLH) and gyroscope (ST Micro L3G4200D). Complete specifications of the accelerometer and gyroscope are provided in our previous work (1, 12). In summary, measurements were made in three dimensions, with linear acceleration measured along each of the iPad's three major axes and rotation-rate measured about each of those axes (Figure 1). Acceleration measurements were recorded independent of gravitational effects and reflect only accelerations imparted on the device by the user's movement. Gyroscope and accelerometer data were sampled at 100 Hz using an in-house balance module from the Cleveland Clinic Concussion (C3) Application which was written in Objective-C, a general purpose programming language used in Apple's iOS operating system. Data collected with the iPad and motion capture system were synchronized by using an Arduino Pro Mini 3.3v coupled with a light-emitting diode which was used to produce a synchronization signal. Upon initiation of iPad data collection, an output signal from the tablet's audio headphone jack triggered the light-emitting diode light to illuminate. The light was recognized by the motion analysis system indicating that the tablet had begun collecting data. The raw data were stored locally on each device and were extracted for data analysis following test completion.
Figure 1.
Illustration of experimental set-up.
Data Analysis
The linear and angular accelerations of the CoM movements during the six BESS conditions were used for all outcome metrics in this study. Specifically, the linear acceleration of the CoM in the anterior-posterior (along Z axis in Figure 1) and medial-lateral (along X axis in Figure 1) directions, in addition to the angular acceleration of the trunk rotation about the vertical axis (Y axis in Figure 1) were included. For the 3D motion capture system, the XYZ location of the CoM segments was computed for each body segment and then the position of whole body CoM was determined using the mass of each body segment and the location of the CoM for each segment (Motion Analysis Software; Santa Rosa, CA). In addition, trunk rotational movements (rotation about Y axis) were calculated using the motion of the shoulder and pelvic markers (Goods and Suntray method using Othrotrack, Motion Analysis Corporation Eagle System; Santa Rosa, CA). Custom scripts in Matlab® (Mathworks, Natick, Massachusetts) were then used to first filter the CoM position and angular data with a 4th order, low pass Butterworth filter with cut-off frequency of 4 Hz, and then calculate the second order derivative of the positional and angular data with respect to time to yield linear (ML and AP) acceleration of CoM and angular acceleration of the Trunk (TR). In regards to the iPad, the raw data from the gyroscope and accelerometer were filtered using the same filter as the 3D motion capture data via custom scripts in Matlab®. The first derivative of the angular rotation of the device (gyroscope) about the vertical axis with respect to time was calculated to obtain a measurement of trunk rotational acceleration (along the Y axis, Figure 1). The linear acceleration of the CoM in the ML (accelerometer data along X axis Figure 1) and AP (accelerometer data along Z axis of Figure 1) directions were also used for analysis.
Summative metrics of the ML and AP CoM accelerations and TR acceleration were computed using data from the iPad and motion capture and included: 1) Peak-to-peak (P2P) which measures displacement amplitude, 2) normalized path length (NPL) which measures the average difference between sequential values, and 3) root mean square distance (RMS) which measures magnitude of CoM displacement. The mathematical equations for these metrics have been described previously (19).
3-D Measure of Balance: 95% volume of ellipse (iBESS volume)
The acceleration of the CoM in AP and ML and the trunk rotational (TR) acceleration from the iPad's gyroscope and accelerometer were used to establish a comprehensive postural stability measure, termed iBESS volume. Specifically, for each trial, these data were used to construct an ellipsoid volume that, with 95% probability, contained the center of the 3D acceleration data. iBESS volumes were calculated for each ellipsoid using 95% volume = 4πabc/3, where a, b, and c were the three axes of the ellipsoid and correspond to the ML, AP and TR directions.
Statistical Analysis
Spearman's rank-order correlation analyses were used to assess the relationship between the summative metrics from the iPad and 3-D motion capture system due to non-normal distributions in both data sets. Kolmogorov-Smirnov tests were used to test for normal distributions of the data sets. A three-factor mixed effect ANOVA was performed on both iBESS volumes and error scores data to determine the random effects of different participants, fixed effects of the three different stances, and fixed effects of the two surfaces. Tukey post-hoc multiple comparison analyses were performed to determine pair-wise differences between the stances and surfaces. Significant differences between the data sets were assumed when p<0.05 for all statistical tests. Values presented are group average ± pooled standard deviation values.
Results
Agreement between 3-D Motion Capture and iPad
The CoM acceleration measurements from the iPad and the motion capture systems were similar across the six BESS conditions (Table 1). Correlation analyses indicated, in general, that the P2P, NPL, and RMS metrics across the three directions (AP, ML, and TR) were significantly correlated between the motion capture system and iPad metrics. The lowest correlations were found in Conditions 1 and 4, the double leg stance conditions on firm and foam surfaces (respectively). The highest correlations were in Conditions 2 and 5, single leg support conditions on foam and firm surfaces (respectively).
Table 1. The CoM acceleration measurements from the iPad and the motion capture systems were similar across conditions.
| Condition 1 | Condition 2 | Condition 3 | Condition 4 | Condition 5 | Condition 6 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Rho | P value | Rho | P value | Rho | P value | Rho | P value | Rho | P value | Rho | P value | ||
| AP | NPL | 0.34 | 0.068 | 0.73 | 0.0001 | 0.87 | 0.0001 | 0.58 | 0.0011 | 0.89 | 0.0001 | 0.72 | 0.0001 |
| P2P | 0.50 | 0.0057 | 0.80 | 0.0001 | 0.77 | 0.0001 | 0.67 | 0.0001 | 0.74 | 0.0001 | 0.66 | 0.0002 | |
| RMS | 0.66 | 0.0001 | 0.77 | 0.0001 | 0.85 | 0.0001 | 0.70 | 0.0001 | 0.92 | 0.0001 | 0.72 | 0.0001 | |
| ML | NPL | 0.43 | 0.0182 | 0.65 | 0.0001 | 0.70 | 0.0001 | 0.43 | 0.0195 | 0.87 | 0.0001 | 0.79 | 0.0001 |
| P2P | 0.41 | 0.0238 | 0.83 | 0.0001 | 0.86 | 0.0001 | 0.44 | 0.0178 | 0.90 | 0.0001 | 0.72 | 0.0001 | |
| RMS | 0.64 | 0.0002 | 0.81 | 0.0001 | 0.80 | 0.0001 | 0.59 | 0.001 | 0.93 | 0.0001 | 0.81 | 0.0001 | |
| TR | NPL | 0.37 | 0.0472 | 0.73 | 0.0001 | 0.71 | 0.0001 | 0.51 | 0.0054 | 0.77 | 0.0001 | 0.76 | 0.0001 |
| P2P | 0.14 | 0.4463 | 0.89 | 0.0001 | 0.60 | 0.0009 | 0.56 | 0.002 | 0.78 | 0.0001 | 0.86 | 0.0001 | |
| RMS | 0.49 | 0.0063 | 0.84 | 0.0001 | 0.73 | 0.0001 | 0.58 | 0.0012 | 0.87 | 0.0001 | 0.84 | 0.0001 | |
| iBess Volume | 0.68 | 0.0001 | 0.94 | 0.0001 | 0.87 | 0.0001 | 0.72 | 0.0001 | 0.94 | 0.0001 | 0.91 | 0.0001 | |
Characterizing BESS Postural Stability
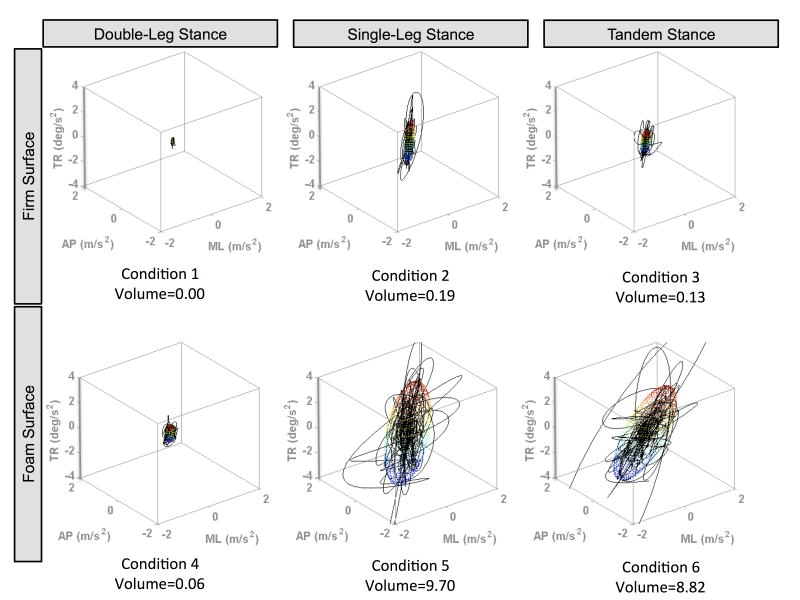
Figure 2 illustrates the iBESS volumes, combining medial-lateral, anterior-posterior, and trunk rotation acceleration from the iPad for one representative participant across the six conditions. Figure 2 indicates an increase in movement acceleration, resulting in an increase in iBESS volumes as the task becomes more challenging by altering the stance from double support to single and tandem stances (Condition 1vs 2&3 and 4 vs 5&6) and changing the support surface from firm to foam (Conditions 1-3 versus 4-6).
Figure 2.
Representative graphs from a single subject to show the three-dimensional traces combining linear and angular acceleration using the tablet's built-in accelerometer and gyroscope during all six BESS conditions. 95% ellipsoid volumes, iBESS volumes, are shown as an ellipse, illustrating the amount of movement increasing and thus increasing postural instability as the balance task becomes more difficult.
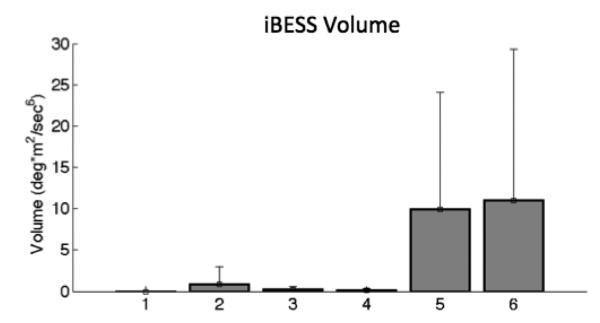
Increased variability as a function of the difficulty of the condition was present as the iBESS volume metric tended to increase across conditions. Figure 3 illustrates that the mean iBESS volume for the firm conditions and double-leg stance on foam were relatively small (range= 0.0-0.9 deg*m2/sec6; Conditions 1-4). Not surprisingly, the largest average iBESS volumes were found in the most challenging conditions: single-leg (condition 5) and tandem (condition 6) stances on foam: 9.9 and 11.0 deg*m2/sec6, respectively. In addition, the largest variability across the sample (assessed through standard deviation) was observed in these same two conditions; 14.2 and 18.3 deg*m2/sec6 respectively.
Figure 3.
Mean values of 95% iPad Ellipsoid Volumes (deg*m2/sec6 ) from iPad sensors showing greater postural instability measured by 95% volumes as the balance tasks increase in difficulty across the six BESS conditions. Error bars representing +/- 1 standard deviation.
Correlation analysis between BESS errors and the iBESS volume metrics were compared across all 6 BESS conditions. In conditions 2, 3 and 6 there was a significant correlation between the iBESS volume from the iPad and error score for that condition (see Table 2). Of note, no errors were committed in BESS Condition 1; therefore no correlation analysis could be performed with 3D volumes.
Table 2. In conditions 2, 3, and 6 there was a significant correlation between the iBESS Volume from the iPad and error score for that condition.
| Condition | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| Rho | NA | 0.51 | 0.54 | 0.27 | -0.17 | 0.55 |
| P Value | NA | p<0.001 | p<0.001 | 0.16 | 0.36 | p<0.01 |
| Bess Error Mean (STD) Median [Min-Max Range] | 0 (0) 0 [0-0] |
1.5 (1.7) 1 [0-6] |
0.3 (0.5) 0 [0-1] |
0.04 (0.19) 0 [0-1] |
5.3 (1.61) 5 [2-10] |
2.5 (0.95) 3 [0 4] |
| iBESS Volume (STD) | 0.00 (0.00) | 0.9 (2.09) | 0.20 (0.37) | 0.12 (0.15) | 9.9 (14.21) | 11.00 (18.33) |
Mean iBESS volume values across the six conditions were evaluated to determine if changes in stance or support surfaces produced a significant change in 95% volume measures (Table 3). In all seven comparisons, the iBESS volume was able to detect a significant difference between the stance conditions (double leg compared to tandem or single leg support) and between the support surfaces (firm compared to foam). Specifically, in all seven of the comparisons in Table 3 between stance and surface changes, the iBESS volume showed a significant increase in value as the tasks became more challenging (Table 2). The BESS error metric was not as sensitive to changes in the support surface as the iBESS volume metric. The BESS error metric was able to detect a significant change in 6/7 comparisons but failed to detect a change in support surface during the double leg stance trials (Trial 1 versus Trial 4).
Table 3. Mean iBESS volume values across the six conditions were evaluated to determine if changes in stance or support surfaces produced a significant change in 95% volume measures.
| iBESS Volume | BESS Error | ||
|---|---|---|---|
|
Difference in Stance |
Condition 1 vs Condition 2 |
p<0.001 | p<0.001 |
|
Condition 1 vs Condition 3 |
p<0.001 | p=0.002 | |
|
Conditon 4 vs Condition 5 |
p<0.001 | p<0.001 | |
|
Conditon 4 vs Condition 6 |
p<0.001 | p<0.001 | |
|
Difference in Surface |
Condition 1 vs Condition 4 |
p<0.001 | p=0.3255 |
|
Condition 2 vs Condition 5 |
p<0.001 | p<0.001 | |
|
Condtion 3 vs Condition 6 |
p<0.001 | p<0.001 |
Discussion
The BESS is a portable clinical balance assessment that is recognized as the standard for the evaluation of postural stability following a concussion (17). The conditions of the BESS tax the physiologic domains associated with postural stability, however the lack of an objective and quantitative scoring system limits its utility in the interdisciplinary management of athletes with concussion, including its use in return to play decision-making. The primary results of this project indicate: 1) the kinematic data provided by the iPad are of sufficient quality relative to motion capture data to accurately calculate a measure of postural stability in healthy young adults and 2) the development of an objective measure of postural stability, the iBess volume, provides a more sensitive measure of BESS performance than errors alone.
Using AP, ML and TR movement data from the iPad to create the iBESS volume provides an objective biomechanical measure of postural stability that is conducive to characterize a clinical test such as the BESS. A clinically relevant and valuable component of the iBESS volume is its ability to quantify and visually demonstrate directional sway (A-P, M-L, or T-R) during the 20-second balance task. The value of tracking changes in postural stability in each of these directions was highlighted in a recent study in 29 collegiate athletes who, after sustaining a head injury, performed at baseline on the Sensory Organization Test 3-4 days following concussion. However, approximate entropy values measured in A-P and M-L time series remained abnormal relative to baseline values well after SOT scores returned to baseline(5, 6). Thus, the ability for the iBESS volume to quantify postural sway in the AP, ML, and TR planes of movement may provide diagnostic value, and may improve the sensitivity of detecting residual deficits in postural control in injured athletes. While the BESS was not initially conceived to distinguish among the three domains of postural stability (visual, somatosensory, and vestibular) or to capture movement in specific planes of movement, it demonstrates clinical utility by minimizing or eliminating one or more of these afferent influences during performance of the six balance tasks. In quantifying postural sway in each of three planes of movements during a given task, the iBESS volume metric may provide diagnostic value for clinicians in the detection of injury and certainly in the tracking and rehabilitation of balance impairments post-injury. For example, a symmetrical increase in sway may demonstrate increased latency in the afferent system's recognition of postural sway changes or a delay in the efferent response to perturbations. Conversely, asymmetrical changes, in which there is significant bias toward one direction of movement over the other, may indicate a unilateral vestibular hypofunction or unilateral impairment in the motor control mechanisms (either afferent input or efferent response) responsible for balance maintenance. Importantly, this biomechanical assessment of postural stability provides an objective metric to evaluate motor control as recommended by the NATA position statement on the management of concussion in sport (2). This objective metric can serve as a method to evaluate injured athletes’ motor control, helping to inform the clinical team in return to play decisions and facilitate clinical hand-offs between the interdisciplinary team of providers. Additionally, these detailed metrics may inform rehabilitation strategies utilized by clinicians. Studies are currently underway in injured and diseased populations that may provide a greater understanding of the clinical interpretation and implications of iBESS volume metric.
Importantly, contrary to the design of the objective BESS study by Brown and colleagues (4), our objective was not to demonstrate correlation with the error scoring method, as the two metrics measure different aspects of postural stability. The iBess volume metric quantifies CoM movements that occur in the AP, ML and TR planes, while the error counting method measures discrete losses of balance (step, stumble, or fall; remaining out of position) or the strategies one uses to maintain balance (opening eyes; taking hands off hips; lifting forefoot or heels; hip flexion/abduction >30 degrees) within a 20 second trial. The biomechanical approach of the iBESS volume overcomes the shortcomings associated with the subjective scoring method employed by the BESS, while the algorithm developed for the oBESS strived to validate the error scoring method. The best oBESS algorithm that accurately predicted mean total BESS errors was computed from data from a single IMU attached at the forehead, and matched only the subset of error scores for foam conditions, and not the subset for firm ground conditions. This finding that the algorithm did not predict errors for both firm and foam stances further verifies that fitting a biomechanical metric to a clinical, non-biomechanical variable of postural stability (error scores) may be considered an inferior approach. Furthermore, using the forehead as the only landmark by which to measure postural stability is not a typical landmark used in biomechanical studies of postural stability (19), as measuring the body's center of gravity or center of mass (at the sacrum) are critical to the accurate biomechanical assessment of balance. The iBESS volume metric employs a more sophisticated biomechanical approach, enabling the quantification of postural sway in the AP, ML and TR planes of movement, allowing for the detection of subtle changes in postural stability that do not result in significant losses of balance and are therefore not captured by error scoring or potentially, the oBESS.
A potential limitation of the BESS scoring system is its floor and ceiling effects. In this study, the iBESS volume metric does not show the same vulnerability. As indicated in Table 3, the iBESS volume showed greater sensitivity in detecting changes in postural stability in conditions 1 and 4, where the error scoring method suffered from floor effects. In BESS conditions 1 and 4, participants are asked to maintain the most stable stance with both feet together on firm ground and a foam surface, respectively, lending to subtle balance adjustments. These subtle adjustments are typically managed with ankle strategies too small in magnitude to result in an “error” yet detectable by the inertial sensors of the iPad. Therefore, while errors as calculated using the BESS scoring method are infrequent in these stances (firm: 0; foam: 0.04 +/- 0.19), the iBESS volume metric, computed using gyroscopic and accelerometry data captured by the iPad, demonstrated significant differences between these two conditions. Furthermore, when considering that double limb stance on firm ground is one of only three stances included in the SCAT3, the sensitivity of the BESS and its use on the sideline may be substantially improved by utilizing a biomechanical approach to measuring postural sway. Conversely, a ceiling effect has been reported during BESS condition 5 (single limb stance on foam) (18) with healthy individuals scoring the maximum number of errors (10) during the 20-second trial. A range of 0-13 errors was originally reported in this condition prior to the truncation of scores at the 10 error cap (17). A maximum error score in a given condition threatens the sensitivity of the measure, as it is then unable to distinguish between healthy and injured individuals. The iBESS volume metric has a continuous scale and therefore does not show this limitation. Collectively, these results increase the sensitivity of a well-designed and accepted clinical test of postural assessment, allowing for finer differentiation among subjects and providing discriminatory value in the two conditions that previously suffered from floor effects (BESS-1 and BESS-4) and in condition 5 that suffered from a ceiling effect using the traditional BESS scoring method.
While our aim was not to demonstrate correlation with error scores, a relationship between errors and the iBESS metric was anticipated, and therefore, evaluated. As shown in Table 2, error scores correlated with iBESS scores for BESS conditions 2, 3, and 6 (single limb firm, tandem firm, and tandem foam). Participants were uniformly instructed to “try to maintain stability” yet two clear behavioral tendencies were observed, particularly with the two single-limb stances. Individuals either repeatedly responded to smaller perturbations by toe-tapping, or touching their foot to the ground, resulting in several “errors” to prevent a more significant loss of balance (a pseudo-feed-forward motor control strategy), while others attempted to maintain the testing position at all costs, resulting in fewer errors, but more significant losses of balance (a pseudo-feedback strategy). These strategies became evident in the iBESS volume metric, as the former strategy resulted in more errors but a smaller volume of postural sway, while the latter resulted in fewer errors, but increased postural sway. These behavioral responses provide insightful data into an individual's postural stability “fingerprint”, which can be quantified by the iBESS volume metric, but are lost with the error scoring method of the BESS. Additional data investigating the test-retest reliability of this metric and performance under injured conditions will provide greater insight into this concept of an individual's postural stability “fingerprint” or detailed characterization of balance maintenance strategies.
We acknowledge limitations to this project. All participants were healthy young adults. Investigation into the sensitivity and specificity of the test in injured or concussed individuals is currently underway. Although comparing an individual's post-injury data to his/her baseline is clinically optimal, gender- and age-based normative data are typically used in the absence of a baseline assessment. These normative data are currently being established in a larger cohort of children and young adults. It could be conceived that this technology would be used on the sideline or locker room as part of the clinical evaluation related to concussion. Under these conditions, in which the athlete may have protective padding or footwear (including ice skates), data in the present study did not account for these ecological characteristics and the precise influence of padding or footwear would certainly impact postural stability. The technology developed would provide an accurate measure of that performance, however, the algorithm does not yet correct for these external factors. Current studies are underway to determine the efficacy of developing an “environmental correction” factor to accommodate these types of changes. Our initial aim was to first validate our approach in the biomechanical assessment of postural stability using a consumer electronic device, which we have demonstrated in the current study. This project relied upon the hardware of a consumer electronics device; clearly device hardware has the potential to change in future iterations of these devices. While changes are certainly possible, considering the processing speed and precision of OEM sensor packages tends to improve over time, we believe precision of measuring motor control processes with these systems will only become better. The techniques used to calculate the iBESS volume can be applied to these potentially more precise sensor data in the future with minimal effort. We believe the ability to rapidly deal with these changes in improved sensor quality coupled with an objective approach to balance assessment makes this a feasible approach to the clinical evaluation of postural stability across the spectrum of concussion providers.
The calculation of the iBESS volume metric using gyroscopic and accelerometer data captured by the iPad can add significant value and integrity to the current error scoring system used by the multiple clinicians utilizing the BESS in concussion management. Postural stability measures during BESS conditions 1 and 4, which previously held little to no clinical value due to floor effect, now have quantifiable values associated with them using the biomechanical approach and the resultant iBESS volume metric. Particularly during the administration of the BESS as part of the SCAT3 when only the three firm ground conditions are tested, value is added by quantifying postural sway during double limb stance when the traditional error scoring method often suffered from a floor effect in yielding no errors. Furthermore, the iBESS volume graphical illustrations provide directional data with respect to A-P, M-L, and T-R postural sway over the entire 20-second trial. These data can provide a specific “fingerprint” of the individual's behavioral tendencies and balance reactions during quiet stance and in perturbed conditions, and can potentially inform rehabilitation approaches. In summary, the iBESS overcomes limitations associated with the error scoring method of the BESS by providing an objective metric of postural stability, thus providing a proxy of motor control as recommended by the NATA, using a portable, affordable consumer electronic platform.
Acknowledgments
The authors wish to acknowledge Scott Campbell and Daniel Kana for their contributions in data collection.
Funding: This project was supported by NIH 1R01NS073717-01 to JLA.
Footnotes
Conflict of Interest: The authors have no conflicts of interest to disclose related to this study. The results of the present study do not constitute endorsement by the American College of Sports Medicine (ACSM).
References
- 1.Alberts JL, Hirsch J, Koop MM, et al. Quantification of postural stability using accelerometer and gyroscopic measures. Journal of athletic training. 2014 doi: 10.4085/1062-6050-50.2.01. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Broglio SP, Cantu RC, Gioia GA, et al. National Athletic Trainers' Association position statement: management of sport concussion. Journal of athletic training. 2014;49(2):245–65. doi: 10.4085/1062-6050-49.1.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Broglio SP, Zhu W, Sopiarz K, Park Y. Generalizability theory analysis of balance error scoring system reliability in healthy young adults. J Athl Training. 2009;44(5):497–205. doi: 10.4085/1062-6050-44.5.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brown HJ, Siegmund GP, Guskiewicz KM, Van Den Doel K, Cretu E, Blouin JS. Development and validation of an objective balance error scoring system. Medicine and science in sports and exercise. 2014;46(8):1610–6. doi: 10.1249/MSS.0000000000000263. [DOI] [PubMed] [Google Scholar]
- 5.Cavanaugh JT, Guskiewicz KM, Giuliani C, Marshall S, Mercer V, Stergiou N. Detecting altered postural control after cerebral concussion in athletes with normal postural stability. Br J Sports Med. 2005;39(11):805–11. doi: 10.1136/bjsm.2004.015909. Epub 2005/10/26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cavanaugh JT, Guskiewicz KM, Giuliani C, Marshall S, Mercer VS, Stergiou N. Recovery of postural control after cerebral concussion: new insights using approximate entropy. Journal of athletic training. 2006;41(3):305–13. [PMC free article] [PubMed] [Google Scholar]
- 7.Finnoff JT, Peterson VJ, Hollman JH, Smith J. Intrarater and interrater reliability of the Balance Error Scoring System (BESS) Pm R. 2009;1(1):50–4. doi: 10.1016/j.pmrj.2008.06.002. Epub 2009/07/25. [DOI] [PubMed] [Google Scholar]
- 8.Guskiewicz KM, Ross SE, Marshall SW. Postural Stability and Neuropsychological Deficits After Concussion in Collegiate Athletes. J Athl Train. 2001;36(3):263–73. Epub 2003/08/26. [PMC free article] [PubMed] [Google Scholar]
- 9.Kadaba MP, Ramakrishnan HK, Wootten ME. Measurement of lower extremity kinematics during level walking. Journal of orthopaedic research : official publication of the Orthopaedic Research Society. 1990;8(3):383–92. doi: 10.1002/jor.1100080310. [DOI] [PubMed] [Google Scholar]
- 10.Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain injury: a brief overview. The Journal of head trauma rehabilitation. 2006;21(5):375–8. doi: 10.1097/00001199-200609000-00001. [DOI] [PubMed] [Google Scholar]
- 11.McCrory P, Meeuwisse WH, Aubry M, et al. Br J Sports Med; Consensus statement on concussion in sport: the 4th International Conference on Concussion in Sport held in Zurich; November 2012; 2013. pp. 250–8. Epub 2013/03/13. [DOI] [PubMed] [Google Scholar]
- 12.Ozinga SJ, Alberts JL. Quantification of postural stability in older adults using mobile technology. Exp Brain Res. 2014 doi: 10.1007/s00221-014-4069-8. [DOI] [PubMed] [Google Scholar]
- 13.Ozinga SJ, Machado A, Rosenfeldt A, Alberts J. Society for Neuroscience. Walter E. Washington Convention Center; Washington, DC: Nov 15-19, 2014. Quantification of postural stability in patients with Parkinson's disease using mobile technology. [Google Scholar]
- 14.Powers KC, Kalmar JM, Cinelli ME. Recovery of static stability following a concussion. Gait Posture. 2014;39(1):611–4. doi: 10.1016/j.gaitpost.2013.05.026. [DOI] [PubMed] [Google Scholar]
- 15.Putukian M. The acute symptoms of sport-related concussion: diagnosis and on-field management. Clin Sports Med. 2011;30(1):49–61. viii. doi: 10.1016/j.csm.2010.09.005. Epub 2010/11/16. [DOI] [PubMed] [Google Scholar]
- 16.Riemann BL, Guskiewicz K. Effects of mild head injury on postural stability as measured through clinical balance testing. J Athl Training. 2000;35(1):19–25. [PMC free article] [PubMed] [Google Scholar]
- 17.Reimann BL, Guskiewicz K, Shields EW. Relationship between clinical and forceplate measures of postural stability. J Sports Rehabil. 1999;8:71–82. [Google Scholar]
- 18.Valovich McLeod TC, Barr WB, McCrea M, Guskiewicz KM. Psychometric and Measurement Properties of Concussion Assessment Tools in Youth Sports. J Athl Training. 2006;41(4):399–408. [PMC free article] [PubMed] [Google Scholar]
- 19.Whitney SL, Roche JL, Marchetti GF, et al. A comparison of accelerometry and center of pressure measures during computerized dynamic posturography: a measure of balance. Gait Posture. 2011;33(4):594–9. doi: 10.1016/j.gaitpost.2011.01.015. Epub 2011/02/22. [DOI] [PMC free article] [PubMed] [Google Scholar]