Abstract
Setting: Pimpri Chinchwad Municipal Corporation area, Pune, India.
Objective: To assess the proportion of private practitioners (PPs) who notified tuberculosis (TB) patients during February–April 2013 and their contribution to the overall number notified, and to determine their perceived challenges in reporting TB cases.
Design: Mixed-method study including an analysis of notification data, followed by in-depth interviews with PPs. Interviews were transcribed and inductive content analysis was performed to derive themes.
Results: Of 831 PPs, 533 (64%) participated in case notification; of these 87 (16%) notified at least one TB case during the study period. In all, 138 TB cases were notified by PPs, accounting for 20% of the total TB cases notified. Emerging themes among perceived challenges and barriers were lack of complete knowledge about TB notification, fear of a breach of patient confidentiality, lack of a simplified operational mechanism of notification, and lack of trust and coordination with the government health system.
Conclusion: About two thirds of PPs participated in case notification and contributed significantly to the overall TB cases notified. India's national TB programme should focus on training PPs and targeted media communication campaigns, and establish alternative mechanisms for notification, such as the internet and mobile telephones, to overcome perceived barriers.
Keywords: tuberculosis, notification, private practitioners, challenges, India
Abstract
Cadre : Zone de la Corporation Municipale de Chinchwad, Pune, Inde.
Objectif : Evaluer la proportion de praticiens privés (PP) qui ont déclaré des patients ayant la tuberculose (TB) entre février et avril 2013 et leur contribution au total de cas déclarés, et déterminer les défis perçus en matière de déclaration des cas de TB.
Schéma : Etude reposant sur plusieurs méthodes, notamment une analyse des données de déclaration suivie d'entretiens approfondis avec des PP. Ces entretiens ont été transcrits et leur contenu a été analysé pour en dériver des thèmes.
Résultats : Sur 831 PP, 533 (64%) ont participé à la notification, et parmi eux 87 (16%) ont déclaré au moins un cas de TB pendant la période d'étude. Au total, 138 cas de TB ont été déclarés par les PP, ce qui constitue 20% du total de cas de TB notifiés. Les thèmes qui ont émergé parmi les défis et contraintes perçus ont été la connaissance incomplète du système de notification de la TB, la peur d'enfreindre la confidentialité des patients, l'absence de système opérationnel simplifié de déclaration et le manque de confiance envers le système de santé gouvernemental et le manque de coordination avec ce dernier.
Conclusion : Près de deux tiers des PP ont participé à la notification et ont apporté une contribution significative à l'ensemble des cas de TB déclarés. Le programme national TB devrait se concentrer sur la formation des PP, sur des campagnes de communication ciblées auprès des media et sur la mise en place de mécanismes alternatifs de notification (par exemple, par internet et par téléphone portable) pour vaincre les obstacles perçus.
Abstract
Marco de referencia: La región de la Corporación Municipal de Pimpri Chinchwad de Pune, en la India.
Objetivo: Evaluar la proporción de médicos del sector privado (PP) que notificaban pacientes con diagnóstico de tuberculosis (TB) durante el período del febrero a abril del 2013 y su contribución al número global de casos notificados, y determinar las dificultades que encontraron los profesionales con respecto a la notificación de casos.
Método: La presente investigación adoptó un diseño de métodos mixtos, que incluyó el análisis de los datos de notificación seguido de entrevistas exhaustivas a los PP. Las entrevistas se transcribieron y se llevó a cabo un análisis de contenido de tipo inductivo con el fin de derivar los temas.
Resultados: De los 831 PP, 533 participaban en la notificación (64%) y de ellos 87 notificaron como mínimo un caso de TB durante el período del estudio (16%). En total, los PP notificaron 138 casos de TB, que correspondieron al 20% de todos los casos notificados. Los temas que surgieron sobre las dificultades y las barreras a la notificación fueron la falta de un conocimiento completo sobre la notificación de la TB, el temor a infringir la confidencialidad del paciente, la carencia de un mecanismo operativo simplificado de notificación y la falta de confianza y coordinación con el sistema de salud gubernamental.
Conclusión: Cerca de dos tercios de los PP participaban en la notificación y su contribución fue considerable con respecto a la totalidad de casos de TB notificados. El programa nacional contra la TB debe centrar su interés en la formación de los PP, llevar a cabo campañas dirigidas en los medios de comunicación y establecer mecanismos alternos de notificación (por ejemplo, en internet o por conducto de los teléfonos móviles), con el fin de superar las barreras percibidas en el estudio.
In India, between 34% and 57% of tuberculosis (TB) cases are diagnosed and managed outside the public sector, often inappropriately.1–4 Studies on anti-tuberculosis drug sales in India estimate that the number of cases treated in the private sector alone exceeds estimated overall TB incidence.5 Studies from Mumbai and elsewhere have shown poor diagnosis and treatment practices among practitioners in the private health sector that contribute to acquired drug resistance.6–10 To reduce TB transmission and prevent the emergence of virtually incurable forms of drug-resistant TB, TB management in the private sector must be aligned with the international standards of TB care.6–10 The involvement of the private sector in India's Revised National TB Control Programme (RNTCP) is therefore crucial.1,4
In India, the RNTCP uses a standard recording and reporting system for TB patients.11 As TB was not a nationally notifiable disease in India until May 2012, there was no routine system to capture information on the number of TB cases managed in the private health sector. Since then, the Government of India has declared TB a nationally notifiable disease and has issued an executive order mandating that all health care providers in the country notify local government health authorities of TB cases managed by them (Figure).12 Mandatory TB notification will help better patient management by enabling the RNTCP to conduct contact screening, provide the option of free drugs under the RNTCP and monitor treatment outcomes and TB treatment regimens among private providers through reported data. These are essential steps for achieving universal access to quality-assured diagnosis and treatment for all TB patients. Complete and accurate data obtained from mandatory TB notification requirements will also help the RNTCP estimate the TB burden with greater accuracy and periodically evaluate the impact of TB control efforts. While anecdotal evidence suggests that the compliance of private practitioners (PPs) in adhering to national policy has been suboptimal, there has to date been no systematic assessment of the challenges involved.
FIGURE.
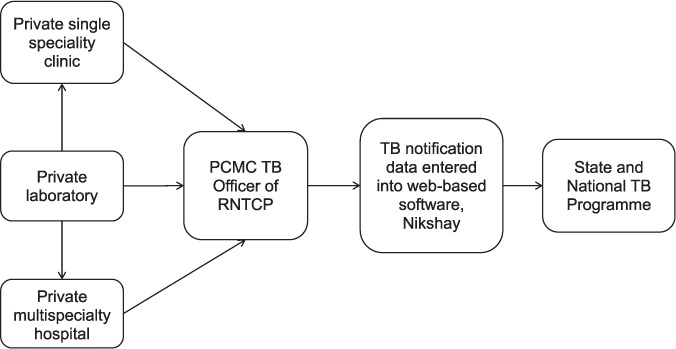
Flow chart of private provider and laboratory TB notifications, PCMC, Pune, India. PCMC = Pimpri Chinchwad Municipal Corporation; TB = tuberculosis; RNTCP = Revised National TB Control Programme.
We conducted this operational research study in the Pimpri Chinchwad Municipal Corporation (PCMC) area, Pune, India. The specific objectives were to determine, for the period February–April 2013, 1) the proportion of PPs who participated in the notification system, 2) the contribution of PPs to the overall number of TB cases notified to the RNTCP in PCMC, and 3) the perceived challenges and barriers faced by PPs in notifying TB cases.
METHODS
Setting
Pimpri-Chinchwad, an industrial city in the Pune Metropolitan Region in the state of Maharashtra, India (population 1.8 million; area 171 km2), is governed by the Pimpri-Chinchwad Municipal Corporation (PCMC), an urban local self-government body. As a municipal corporation, the PCMC has been designated an RNTCP district implementing unit. In 2012, the PCMC's annual TB case notification rate was 117 per 100 000 population. TB control programme services in the district are available through a decentralised network of primary, secondary and tertiary government health care facilities, with an estimated 115 doctors in a total of 31 health care facilities. The government facilities provide general health services, including diagnosis and treatment for TB, according to RNTCP guidelines.11 The RNTCP employs TB health visitors (TB HVs) (one per 0.1 million urban population), whose responsibilities include meeting and creating awareness among PPs about case notification and collecting case notification data.
Study design
In this mixed-methods study, we analysed TB notification data and interviewed PPs. The purpose of utilising both quantitative and qualitative approaches was to gain a more comprehensive understanding of the notification process by PPs. This design has been previously categorised as an ‘expansion’ mixed methodology.13 While the quantitative data inform the extent of PP notification, the qualitative data explore the challenges involved in implementation. Because our interest was the direct exploration of the phenomenon of PP notification, our approach to the interviews was based on a qualitative descriptive framework.14
Private practitioners
We defined PPs as those with a qualification in one of the systems of medicine officially recognised in India (allopathy, Ayurveda, Unani, naturopathy, Siddha and homeopathy) who provide health care services for a fee outside the public sector. In the PCMC, there are approximately 400 PPs who practise allopathic medicine and 500 PPs who practise other systems of medicine. These PPs independently diagnose and treat TB patients for profit. From the authors' previous experiences, TB patients seeking care from PPs were likely to consult with specialist physicians for the treatment of TB complications, including meningitis, pleural effusions and drug resistance.
Tuberculosis notification
Following the declaration of TB as a nationally notifiable disease, we attempted to enlist all PPs in the PCMC for TB case notification. PPs were identified from a list of private hospitals registered with the Municipal Corporation and by local canvasing for other non-listed PPs by RNTCP staff. The PPs received information on TB notification procedures (i.e., case notification and collecting case notification data) from the TB HVs. Information on the process of TB case notification by PPs was also advertised in local newspapers and shared at meetings of professional bodies attended by PPs such as the Indian Medical Association. PPs were expected to send TB notifications in hard copy by post/courier/person to the nodal officer for TB notification.
Study participants and study period
All enlisted PPs practising in the PCMC during the period February–April 2013 were eligible to participate in the study. The in-depth interviews with PPs are described below.
Notification data
PPs were visited once a month, from February to April 2013, to collect information on patients diagnosed with TB or receiving anti-tuberculosis treatment from standardised paper-based registers. This information was collected in structured TB notification forms and maintained in an electronic database. The electronic records were reviewed to assess the number of PPs who notified cases and the number of TB cases notified. To determine the relative contribution of PPs to overall TB notifications, we also extracted information on TB cases notified to the RNTCP in the PCMC during the same period from standard TB registers that did not include PP notifications.
Qualitative interviews
In this mixed-methods study, following our analysis of PP notification data, we conducted qualitative interviews from May to June 2013. After obtaining informed consent, we conducted in-depth interviews with the PPs to assess their perceptions of the challenges in notifying TB cases. In our analysis of notification data, PPs were selected to ensure geographic representation within the PCMC as well as representation of those who notified TB cases and those who did not.
We purposively selected PPs to cover allopathic private practitioners for interviews, particularly specialists. This focus was due to the overall lower participation in TB notification by allopathic providers and the greater likelihood of patients with TB being referred to allopathic providers, particularly specialists in chest medicine, general medicine and paediatrics.
Interviews were conducted in the vernacular (Marathi), English or both, as applicable. A semi-structured interview format was used as a guide for interviews after pilot-testing. The interviews were recorded and transcribed verbatim. Validation of transcription accuracy and completeness was ascertained by review by at least two study team members. The information collected was de-identified to ensure anonymity. Authors RY (male, doctor, MD) and KK (male, doctor, MD), who conducted the interviews with the PPs, live and work in the same communities as the PPs and speak the regional dialect as well as English, and had established relationships with the PPs prior to the interviews. PPs were also informed that that they could stop at any time during the interviews. Once saturation of responses to interview questions was achieved, the interviews were considered completed.
We conducted a focus group discussion (FGD) with all TB HVs (n = 11) who participated in PP enrolment and case notification data collection to assess the challenges they faced when enlisting PPs and collecting notification data, and their suggestions for improvement. These FGDs also served to verify the validity of the PPs' responses.
Data analysis
Quantitative data extracted from TB notification data were used to calculate the proportions of PPs who participated. Participation in TB notification was defined as having submitted a monthly TB notification report during the study period, including a nil report when they did not have a patient with TB. The number of TB cases notified by PPs was divided by the total number of TB cases notified to the RNTCP during the study period to calculate the proportion contributed by PPs. The total number of TB cases notified was the sum of TB cases notified by PPs and those reported by traditional means via aggregated data from all TB registers.
We used inductive analysis for the qualitative data obtained from provider responses (i.e., categories of analysis were not imposed a priori on the data, but were defined through the analysis). Interview transcripts were reviewed line by line and coded to classify major themes representing the perceptions of PPs about the barriers and challenges they faced when notifying TB cases. Data collection and content analysis were performed simultaneously and were iterative. This guided us during the study in selecting PPs and in framing questions for subsequent interviews. The analysis of transcribed data was first performed by the first author and then independently analysed by the second author to ensure descriptive validity and consistency. There was no significant difference between the themes derived from these analyses. Complete, de-identified representative statements were included in the results to illustrate the main themes. COREQ (Consolidated Criteria for Reporting Qualitative Studies) guidelines were used for reporting on the study.15
Ethics considerations
Participation in interviews was entirely voluntary, and written informed consent was provided by all those interviewed. Ethics approval was obtained from the Ethics Advisory Group of the International Union Against Tuberculosis and Lung Disease, Paris, France, and the institutional ethics committee of the National TB Institute, Bangalore, India. Administrative approval to conduct the study was obtained from the State Health Society (TB Control), Maharashtra State, India.
RESULTS
Tuberculosis notification
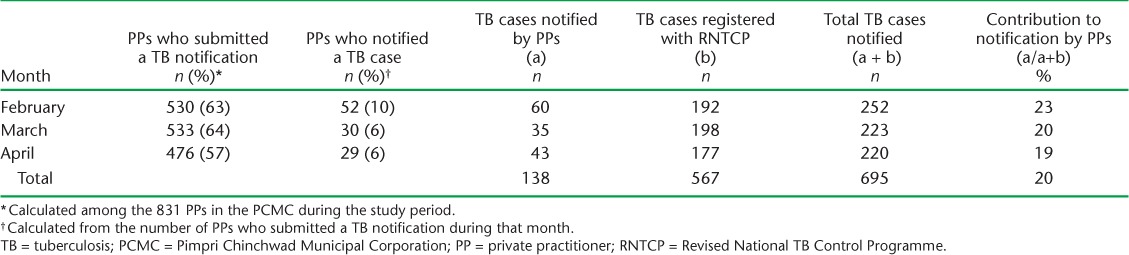
Of 831 PPs in the PCMC during the study period, 533 (64%) participated in notification, 87 (16%) of whom notified a total of 138 TB cases during the study period (Table 1). The number of TB cases notified by PPs represents 20% of all TB cases notified to the RNTCP (Table 1), which includes both PP notifications from the study as well as all cases recorded in registers maintained by public providers. Among the PPs participating in notification, 148 (28%) were qualified in allopathic medicine, and the remainder in other systems of medicine. Among the 138 TB cases notified during the study period, 77 (56%) were notified by allopathic PPs.
TABLE 1.
Private practitioners participating in TB case notification and their contribution overall in PCMC, Pune, India, February–April 2013
Private practitioner interviews
The 24 PPs interviewed comprised general physicians (n = 5), specialist physicians (n = 12), pathologists (n = 4), radiologists (n = 1) and those practising non-allopathic systems of medicine (n = 2). The 12 specialist physicians included chest physicians (n = 4), general practitioners (n = 6) and paediatricians (n = 2). Among the 24 PPs interviewed, 10 notified patients and 14 did not. Saturation in PP responses during the interviews was achieved.
The main perceived challenges and barriers to notifying TB cases by PPs were grouped into four thematic areas that emerged: 1) lack of complete knowledge about TB notification, 2) breach of confidentiality of TB patients and stigma related to TB, 3) lack of a simplified mechanism for notification, and 4) lack of trust and coordination with the government health system. The challenges faced by the PPs are described thematically in Table 2.
TABLE 2.
Perceived barriers and challenges to adopting the system of TB case notification by PPs in Pimpri Chinchwad Municipal Corporation, Pune, India, February–April 2013
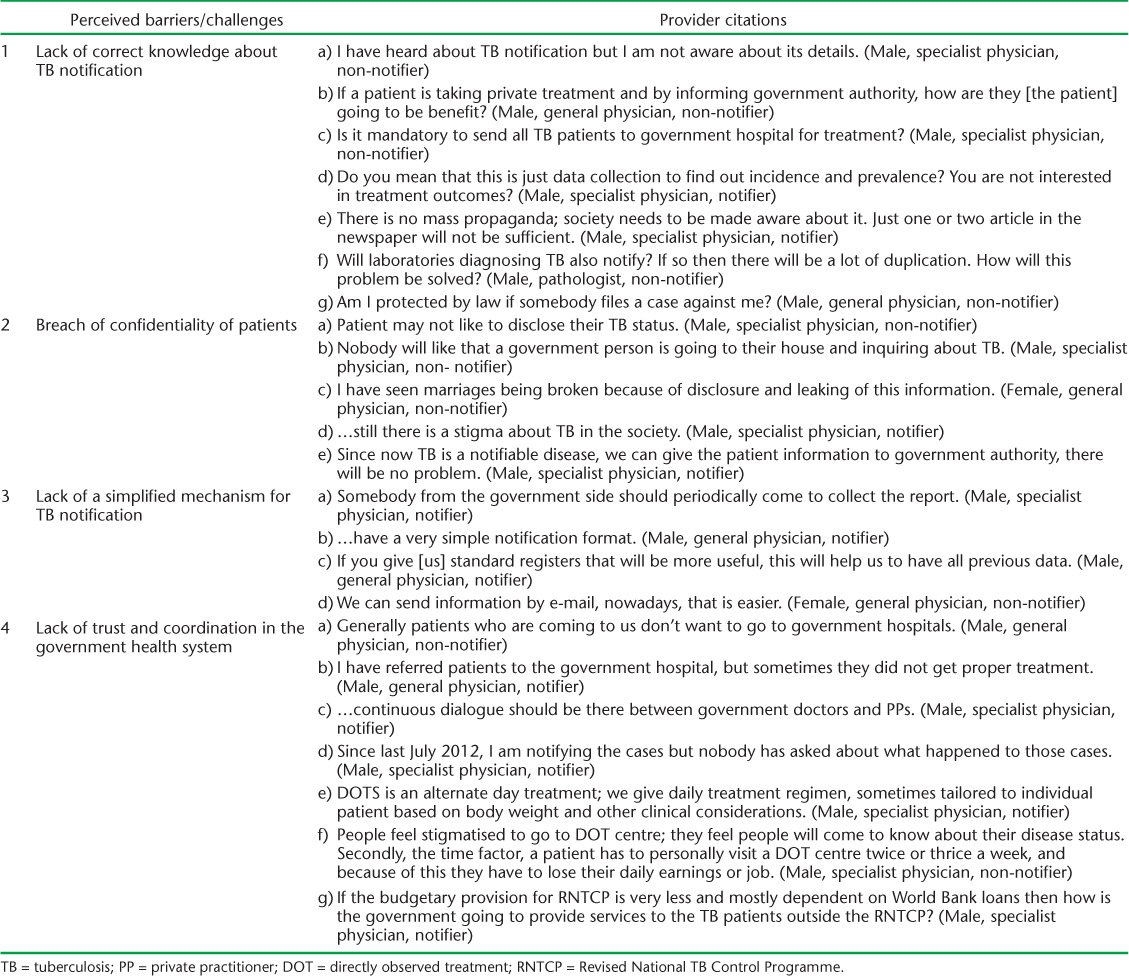
Lack of correct knowledge about tuberculosis notification
The majority of the PPs interviewed had heard of TB notification. During the interviews, however, it was observed that they did not fully understand the rationale, potential patient benefits and details of TB notification. They raised many queries. Some of them perceived notification to mean the mandatory referral of TB patients to government hospitals for treatment. Because of this misconception, some PPs referred all TB cases and did not notify them. Some misunderstood, and assuming that only pulmonary TB cases needed to be notified, did not notify extra-pulmonary TB cases. Some PPs questioned the need for notification and were not clear about the potential patient benefits (Table 2, 1a–d).
Many PPs reported a lack of general awareness among the general public about TB notification, which made it difficult for them to adhere to the government order. To address this problem, they suggested that there should be a more intensified communication campaign (Table 2, 1e). A few practitioners expressed fears about whether they were legally protected when sharing patient information with government authorities (Table 2, 1g). Some also questioned a possible duplication of data if patients were notified by both PPs and laboratories (Table 2, 1f). One PP believed that TB notification meant that the RNTCP was itself responsible for the patient management of all notified cases but had an inadequate budget to do so for cases diagnosed outside the public health services (Table 2, 4g).
Breach of patient confidentiality
PPs noted that, according to the TB notification guidelines, public health staff generally visit patient homes to initiate public health measures. Such visits, however, could lead to loss of patient confidentiality (Table 2, 2a), a concern expressed by the majority of the PPs. Many of them stated that TB patients would dislike it if personnel from the government health system visited their homes, particularly without consent (Table 2, 2b). PPs feared that if they notified, they would be questioned by their patients, which would ultimately lead to a loss of trust and the rapport that they had built over the years with patients and their families (Table 2, 2c). This loss would be particularly damaging given the stigma about TB that was still prevalent in their communities (Table 2, 2c). A few PPs felt reassured, however, about the legal support that the government order provides and said that they would be able to overcome the stigma through patient education (Table 2, 2e).
Lack of a simplified mechanism for tuberculosis notification
Most PPs said that it would be difficult for them to submit the notification report in person, and would prefer regular visits by government staff to their clinics to collect the reports (Table 2, 3a). They also expressed concern that providing detailed information about patients in a standardised format would be too time-consuming (Table 2, 3b). Others said that maintaining patient records would not be a major problem and that standardised registers should be provided (Table 2, 3c). Some suggested that they could send information by e-mail. A few PPs also preferred to submit the information by phone or by SMS, where such a mechanism existed (Table 2, 3d).
Lack of trust in and coordination with the government health system
Issues regarding patient mistrust of the government health system were expressed by PPs. Several practitioners noted that their patients were generally unwilling to attend government hospitals (Table 2, 4a). Some reported that although they did refer patients to government hospitals, patients sometimes did not receive proper anti-tuberculosis treatment (Table 2, 4b). Others also said that patients found it inconvenient to visit DOT (directly observed treatment) centres one to three times a week; patients could lose their daily wages or jobs due to visits to collect their drugs (Table 2, 4f). Because of these issues, PPs also mistrusted the government health system.
PPs noted that the lack of trust between PPs and their patients and the government influences TB notification efforts as well as government initiatives to improve the quality of TB care in general. To establish stronger relationships, PPs expressed the need for strong coordination and regular dialogue between government doctors and PPs (Table 2, 4c and 4d). They believed that this would help to strengthen not only the notification system but also TB management. One TB management issue that emerged during interviews was the conflict between the PPs' preference for daily TB treatment regimens vs. the intermittent treatment regimens used by the RNTCP (Table 2, 4e).
Focus group discussion with tuberculosis health visitors
The TB HVs said that they had no difficulty gathering information from general practitioners and PPs practising alternative systems of medicine, but that they had to wait for long periods for specialist PPs and multispeciality hospitals to respond:
Sometimes, we have to wait for long time with busy PPs; we have to visit multiple times to a multi-specialty hospital to get the data from every individual PP as there is no centralised recording system.
…In my area, there are about 70 doctors of different specialities. To visit all of them every month I have to spend about 7 to 10 days, which is affecting my other RNTCP duties. We have to wait for long time to meet the doctor sometimes.
TB HVs also felt incompetent to answer the questions from specialists about TB notification. They said that ascertaining the exact number of PPs practising in a particular area was a challenge, as many specialist PPs practise at more than one hospital and in different locations. All said that PPs had not been provided with registers and that they maintained data either in an ad hoc format or in their personal registers, while some did not maintain any written records. They expressed concern about PPs who did not maintain records and who could not provide details on all the TB cases they managed.
DISCUSSION
Nearly two thirds of the PPs interviewed participated in the TB notification system, and a total of 138 TB cases were notified over the 3-month study period, accounting for 20% of all TB notifications in the PCMC, a substantial proportion. We observed that PPs practising non-allopathic systems of medicine were more likely to participate in the notification of TB cases. According to RNTCP staff, non-allopathic PPs were more easily accessible when collecting notification reports and had shorter collection times than allopathic PPs.
Recognising and responding to these barriers is important, given that TB has been declared nationally notifiable by the Government of India and given the substantial role played by PPs in treating TB patients in India. Our findings are indicative of an urgent need to educate PPs systematically about TB notification and to improve the TB notification system, as has also been recommended by Philip et al.16 In our study, issues regarding ethics, confidentiality and the notification process itself emerged from PP interviews. These areas could all be addressed by training PPs in TB notification by RNTCP staff. Mass communication campaigns directed toward the general population were suggested as a way to raise awareness about TB, as recommended by Nagaraja et al.17 This may be accomplished by using print and electronic media, famous celebrities as brand ambassadors, continuing medical education courses or mass public advertisements. Many of the PPs felt that government media initiatives needed to be implemented more rigorously.
Some PPs were also apprehensive about the legal aspects of notification. These apprehensions may be alleviated by educating them about the Medical Council of India (MCI) ethics guidelines relating to notification. According to the 2002 MCI code of Ethics, Rules and Regulations (Chapter 7, points 7.7 and 7.14), registered medical practitioners need to give accurate information about cases with notifiable diseases to government authorities, for which they may disclose patient details to the government.18 Many PPs expressed concern about patient confidentiality and needed reassurance that confidentiality would be maintained. Of particular concern were home visits by government staff to patient homes without prior notification. Alternative processes using other modes of communication, such as mobile phones, to contact patients could be explored to address these privacy concerns.
Simplified TB case reporting formats may also help facilitate the notification process among PPs. Other possible alternatives to paper-based notifications raised by PPs, such as notification by e-mail, calls to a toll-free number and SMS, should be explored by the RNTCP. These options may save time spent by health workers in collecting notification data.
The debate between PPs and the RNTCP regarding intermittent and daily regimens has been ongoing for decades. The World Health Organization recommends daily treatment regimens because they lead to fewer treatment relapses and better outcomes than intermittent treatment regimens.19 Many PPs also preferred daily treatment regimens to intermittent regimens because of the increased likelihood of favourable treatment outcomes. As DOT is not possible in private practice, patients tend to self-administer treatment, and in self-administration the adverse consequence of missing a dose is much higher with intermittent regimens than with daily regimens. This was expressed as one of the barriers to TB notification. Several of the PPs felt that if the RNTCP could provide daily regimens, they would be willing to refer their patients to the government health system for treatment.
Full PP participation, including the submission of regular notification reports, is necessary to accurately determine the TB burden in the community. Ensuring that community-level data are complete and accurate is critical for the appropriate planning of TB control activities and evaluating their impact. As local data are aggregated to form regional and national estimates, greater completeness and accuracy of local data would also reduce the need to estimate the national burden of disease and enable more targeted planning of services at local and national levels.
Limitations of the study
Data on the total number of PPs enumerated in the study area may not be accurate, as many PPs practised at multiple facilities. We may therefore have overestimated the proportion of PPs participating in the notification system. Moreover, as only 64% of PPs submitted any notification report (including nil reports), we may have underestimated the number of TB cases managed by them and their contribution to the overall notification of TB cases. The potential impact on the total number of TB cases in our study would likely be higher if PP notification was complete.
Although 72% of the PPs participating in notification were non-allopathic, only 2 of the 21 in-depth interviews were conducted with non-allopathic PPs. Although saturation was achieved and responses by non-allopathic PPs were similar to those of allopathic PPs, additional themes might have emerged if additional non-allopathic PPs had been interviewed. Our analyses also did not find meaningful differences in themes between notifiers and non-notifiers. This may have been due to the compressed time frame of the study, and differences may have been less pronounced than they would have been over a longer period; TB notification was a rare event for the PPs.
The sampling of providers for interviews was to emphasise allopathic physicians and was not intended to be representative of the 831 PPs in the PCMC. This limitation should be taken into consideration when interpreting our findings. As the interviews were conducted by a person who did not have any administrative jurisdiction over PPs, PPs did not hesitate to speak the truth. We therefore do not believe that the study was subject to the Hawthorne effect.
CONCLUSION
About two thirds of the PPs included in the study participated in TB notification and in making a significant contribution to the overall number of notified cases. However, we noted a number of challenges, mainly related to a lack of correct knowledge about notification among PPs and their fears about breach of patient confidentiality, both of which need to be addressed urgently. We recommend that the RNTCP focus on a targeted media campaign and establish alternative notification mechanisms, such as internet and mobile telephones, to overcome perceived barriers and improve the efficiency of the notification process. We plan to conduct a follow-up study to monitor changes.
Acknowledgments
The study was conducted as a part of the TB Operations Research Training Project aimed to build operational research capacity of the Government of India's Revised National TB Control Programme (RNTCP). This training project was conceived and implemented jointly by the Central TB Division, Directorate General of Health Services, Ministry of Health and Family Welfare, Government of India (New Delhi), the National TB Institute, Directorate General of Health Services, Ministry of Health and Family Welfare, Government of India (Bangalore), the World Health Organization (WHO) (India Country Office, New Delhi), the International Union Against Tuberculosis and Lung Disease (The Union) South-East Asia Regional Office (New Delhi, India) and the Division of TB Elimination, Centers for Disease Control and Prevention (CDC) (Atlanta, GA, USA). The authors acknowledge the support of all the above. The authors also thank all study participants and RNTCP staff of the Pimpri Chinchwad Municipal Corporation, Pune, especially all TB health visitors and data entry operators. The findings and conclusions in this article are those of the authors and do not necessarily represent the views of the WHO, The Union or the CDC.
Funding support was provided in part by The Union from the Global Fund Round 9 India TB Project funds and the remaining part by WHO India from United States Agency for International Development (Washington DC, USA) funds. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Conflicts of interest: none declared.
References
- 1.Satyanarayana S, Nair S A, Chadha S S et al. From where are tuberculosis patients accessing treatment in India? Results from a cross-sectional community based survey of 30 districts. PLOS ONE. 2011;6:e24160. doi: 10.1371/journal.pone.0024160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Uplekar M W, Rangan S. Private doctors and tuberculosis control in India. Tubercle Lung Dis. 1993;74:332–337. doi: 10.1016/0962-8479(93)90108-A. [DOI] [PubMed] [Google Scholar]
- 3.Uplekar M, Juvekar S, Morankar S, Rangan S, Nunn P. Tuberculosis patients and practitioners in private clinics in India. Int J Tuberc Lung Dis. 1998;2:324–329. [PubMed] [Google Scholar]
- 4.Hazarika I. Role of private sector in providing tuberculosis care: evidence from a population-based survey in India. J Glob Infect Dis. 2011;3:19–24. doi: 10.4103/0974-777X.77291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wells W A, Ge C F, Patel N, Oh T, Gardiner E, Kimerling M E. Size and usage patterns of private TB drug markets in the high-burden countries. PLOS ONE. 2011;6:e18964. doi: 10.1371/journal.pone.0018964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Uplekar M W, Shepard D S. Treatment of tuberculosis by private general practitioners in India. Tubercle. 1991;72:284–290. doi: 10.1016/0041-3879(91)90055-w. [DOI] [PubMed] [Google Scholar]
- 7.Uplekar M, Pathania V, Raviglione M. Private practitioners and public health: weak links in tuberculosis control. Lancet. 2001;358:912–916. doi: 10.1016/S0140-6736(01)06076-7. [DOI] [PubMed] [Google Scholar]
- 8.Udwadia Z F, Pinto L M, Uplekar M W. Tuberculosis management by private practitioners in Mumbai, India: has anything changed in two decades? PLOS ONE. 2010;5:e12023. doi: 10.1371/journal.pone.0012023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bhargava A, Pinto L, Pai M. Mismanagement of tuberculosis in India: causes, consequences, and the way forward. Hypothesis. 2011;9:1–13. [Google Scholar]
- 10.Sharma V. Management of tuberculosis—the need to enforce proper treatment guidelines among private practitioners in India. Online J Heal Allied Sci. 2012;10:1–2. [Google Scholar]
- 11.Central TB Division, Directorate General Health Services, Ministry of Health and Family Welfare, Government of India. Technical and operational guidelines for tuberculosis control. New Delhi, India: Government of India; 2005. http://tbcindia.nic.in/pdfs/Technical%20&%20Operational%20guidelines%20for%20TB%20Control.pdf Accessed August 2015. [Google Scholar]
- 12.Central TB Division, Directorate General Health Services, Ministry of Health and Family Welfare, Government of India. Tuberculosis India 2013: annual report of the Revised National Tuberculosis Control Programme. New Delhi, India: Government of India; 2013. http://tbcindia.nic.in/Pdfs/TB%20INDIA%202013.pdf Accessed August 2015. [Google Scholar]
- 13.Greene J C, Caracelli V J, Graham W F. Toward a conceptual framework for mixed-method evaluation designs. Educ Eval Policy Anal. 1989;11:255–274. [Google Scholar]
- 14.Sandelowski M. Whatever happened to qualitative description? Res Nurs Health. 2000;23:334–340. doi: 10.1002/1098-240x(200008)23:4<334::aid-nur9>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 15.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349–357. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 16.Philip S, Isaakidis P, Sagili K D, Meharunnisa A, Mrithyunjayan S, Kumar A M V. They know, they agree, but they don't do: the paradox of tuberculosis case notification by private practitioners in Alappuzha District, Kerala, India. PLOS ONE. 2015;10:e0123286. doi: 10.1371/journal.pone.0123286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nagaraja S B, Achanta S, Kumar A M V, Satyanarayana S. Extending tuberculosis notification to the private sector in India: programmatic challenges? Int J Tuberc Lung Dis. 2014;18:1353–1356. doi: 10.5588/ijtld.13.0836. [DOI] [PubMed] [Google Scholar]
- 18.Medical Council of India. Code of Ethics Regulations. New Delhi, India: MCI; 2002. http://www.mciindia.org/RulesandRegulations/CodeofMedicalEthicsRegulations2002.aspx Accessed August 2015. [Google Scholar]
- 19.World Health Organization. Treatment of tuberculosis: guidelines. 4th ed. Geneva, Switzerland: WHO; 2010. WHO/HTM/TB/2009.420. [PubMed] [Google Scholar]


