Abstract
Setting: While some studies have reported the prevalence of dental caries in sub-Saharan Africa, little is known about care-seeking behavior or how dental caries are managed, particularly at rural district hospitals.
Objective: To describe the management of patients seeking care for dental caries at Butaro District Hospital (BDH) in rural Rwanda.
Design: This cross-sectional descriptive study was conducted in BDH, in northern Rwanda. A sample of 287 patient encounters for dental caries between January and December 2013 was randomly selected and stratified by age group (⩽5 years, 6–21 years and >21 years). We estimated the treatment received with 95% confidence intervals in each age group, and differences between age groups were assessed using Fisher's exact test.
Results: Nearly all patients (97.6%) underwent tooth extraction, and this did not vary significantly by age group (P = 0.558). In addition to dental caries, most patients also had chronic pulpitis (74.9%).
Conclusion: Caries prevention and care should be prioritized through a developed community program on oral health. We recommend introducing advanced training, equipment and materials for dental caries management other than tooth extraction, and increasing the number of qualified dentists.
Keywords: dental care, tooth extraction, pulpitis, cellulitis, Africa
Abstract
Contexte : Si certaines études rapportent des taux de prévalence des caries dentaires en Afrique sub-saharienne, on sait peu de choses sur le comportement en termes de recherche de soins ni de prise en charge des caries, surtout dans les hôpitaux de district ruraux.
Objectif : Décrire la prise en charge des patients sollicitant des soins pour caries dentaires à l'Hôpital de District de Butaro (BDH) en zone rurale du Rwanda.
Schéma : Cette étude descriptive transversale a été réalisée au BDH, au nord du Rwanda. Un échantillon de 287 consultations de patients pour caries dentaires entre janvier et décembre 2013 a été sélectionné de façon aléatoire et stratifié sur l'âge (⩽5 ans, 6–21 ans et >21 ans). Nous avons estimé le traitement reçu avec des intervalles de confiance de 95% dans chaque tranche d'âge et les différences entre les groupes d'âge ont été évaluées grâce au test exact de Fisher.
Résultats : Presque tous les patients (97,6%) ont eu une extraction de la dent cariée et cela n'a pas varié de façon significative en fonction du groupe d'âge (P = 0,558). En plus des caries, la majorité des patients avait également une pulpite chronique (74,9%).
Conclusion : La prévention des caries et les soins conservateurs devraient être une priorité grâce à un programme de santé orale communautaire. Nous recommandons l'introduction d'une formation avancée, d'équipement et de matériels de prise en charge des caries dentaires autres que l'extraction des dents et l'augmentation du nombre de dentistes qualifiés.
Abstract
Marco de referencia: Algunos estudios han notificado la prevalencia de caries dental en África subsahariana, pero se conoce poco sobre el comportamiento de búsqueda de atención o el tratamiento de la caries dental, sobre todo en los hospitales distritales de las zonas rurales.
Objetivo: Describir el tratamiento de los pacientes que buscan atención por caries dental en el Hospital Distrital de Butaro, en una zona rural de Rwanda.
Métodos: El presente estudio transversal se llevó a cabo en el Hospital Distrital de Butaro en el norte de Rwanda. Se escogió una muestra aleatoria de 287 citas de pacientes que acudían por caries dental de enero a diciembre del 2013 y se estratificó por grupos de edad (⩽5 años, 6 a 21 años y >21 años). Se evaluaron las proporciones del tipo de tratamiento recibido con un intervalo de confianza del 95% en cada grupo etario y las diferencias entre los grupos se analizaron con una prueba exacta de Fisher.
Resultados: En casi todos los pacientes se practicó la extracción (97,6%) y no se observaron diferencias significativas en los grupos de edad (P = 0,558). Además de la caries, la mayoría de pacientes presentaba pulpitis crónica (74,9%).
Conclusión: Es preciso priorizar la prevención y el tratamiento de la caries mediante un programa comunitario de salud bucodental. Se recomienda introducir una capacitación avanzada, suministrar equipos y materiales de tratamiento de la caries dental diferente de la extracción y aumentar la cantidad de odontólogos calificados.
In 2013, 3.9 billon people had oral health conditions worldwide, and of the 291 diseases and conditions assessed in the 2010 Global Burden of Disease study, untreated dental caries was the most prevalent condition.1 Although the prevalence of dental caries in low-income countries has been low compared to high-income countries, the prevalence rates are now increasing.2 Recent studies on dental caries prevalence in sub-Saharan Africa are limited, with most focusing on specific subpopulations. In these studies, the dental caries prevalence in children and adolescents ranged from 10% to as high as 60%,3–7 while in the only recent study on dental caries in adults, the estimated prevalence in Uganda was 57.3%.8 The prevention and care of dental caries is often neglected in sub-Saharan Africa, and the World Health Organization (WHO) Africa Region Office has recommended more commitment at the country level in this domain.9
While some studies have reported the prevalence of dental caries in sub-Saharan Africa, little is known about care-seeking behavior or how dental caries are managed, particularly at rural district hospitals. In 2013, the leading cause of all out-patient visits in hospitals in Rwanda was tooth and gum diseases, accounting for 26% of all out-patient consultations.10 Of 8990 new out-patient visits in 2012 at Butaro District Hospital (BDH) in northern Rwanda, tooth and gum diseases were the principal reason for presenting, with 1917 cases (Rwanda Health Management Information System [HMIS] database report). More than 80% of these patients were diagnosed with dental caries.
This study aimed to examine how patients seeking care for dental caries at BDH are managed. The study is expected to improve awareness and management of dental caries cases in Rwanda and highlight gaps in dental care in the Africa region.
METHODS
Study design
This cross-sectional descriptive study was conducted in BDH, the district hospital of Burera District in the Northern Province of Rwanda, which covers a catchment area of 336852 individuals and 17 health centers (HCs).
Setting
The Rwanda Ministry of Health manages BDH with support from Partners In Health (PIH)/Rwanda, a US-based non-governmental organization. When seeking care for dental issues, patients are required to first visit the HC for their geographic area. Because there are no qualified dental practitioners at the HCs, patients with dental problems are then referred to the district hospital for management. Patients referred to BDH present to the out-patient consultation room and from there are referred to the Dental Department, which is open Monday to Friday from 7 am to 5 pm. Patient data from these visits are recorded on paper patient charts in the Dental Department.
At the time of the study, BDH had one qualified dental technician with the minimum government-regulated required dental equipment, including a dental chair and chair accessories such as low- and high-speed hand pieces, a dental curing light and a compressor. In addition to the basic medical instruments, the BDH Dental Department had a periodontal curette, dental forceps, detractors, curved dental root elevator, dental elevator right, dental mirrors, picette, dental syringes, dental probe, cement spatula, mouth gag molt and dental stool, which are used in the management of oral diseases including dental caries (source: BDH inventory report).
Study population and sample
The study population included a sample of patients presenting with a diagnosis of dental caries at BDH between 1 January and 31 December 2013, in three age strata: children aged ⩽5 years, adolescents/young adults aged 6–21 years and adults aged >21 years. Individuals with oral problems other than dental caries were excluded, except for those with other dental diseases in addition to dental caries.
A sample of 96 encounters per stratum was needed to estimate the proportion of patients receiving different types of treatment with 95% confidence intervals (CI) with a ± 10% level of precision. To account for missing data (estimated at 10%), we increased the sample size to 107 individuals for each age group. In the oldest and middle age groups, we aimed to randomly sample 107 individuals using segmented sampling. In the youngest age group (⩽5 years), all 73 patients who presented in 2013 were included in the study.
Data collection and analysis
Data was extracted from the BDH dental register and the patient dental care file, which contain routinely collected patient data, into a paper form. A separate file linking patient and study identifiers was kept for data validation/cleaning and was destroyed at the end of data validation. For patients' sociodemographic characteristics, we included the following variables: sex, whether referred from health center, occupation, district of origin and health insurance. For patients' clinical characteristics, we included other diagnosis and type of clinical management (use of pain killer, antibiotics, tooth cleaning, tooth filling, tooth extraction, anesthesia, oral hygiene advice and referral for further care). We estimated the proportion, with 95%CI, of patients with different types of clinical management and used Fisher's exact test to compare the management of dental caries by age group. Stata v12 (StataCorp LP, College Station, TX, USA) was used for data analysis.
Ethics
Confidentiality was assured during data collection, analysis and dissemination. Data were de-identified and stored securely in a password-protected spreadsheet. Study staff received training on patient confidentiality and signed a confidentiality agreement. The study received technical review and approval from the PIH/Rwanda Research Committee and the National Health Research Committee, and ethics approval from the Rwanda National Ethics Committee.
RESULTS
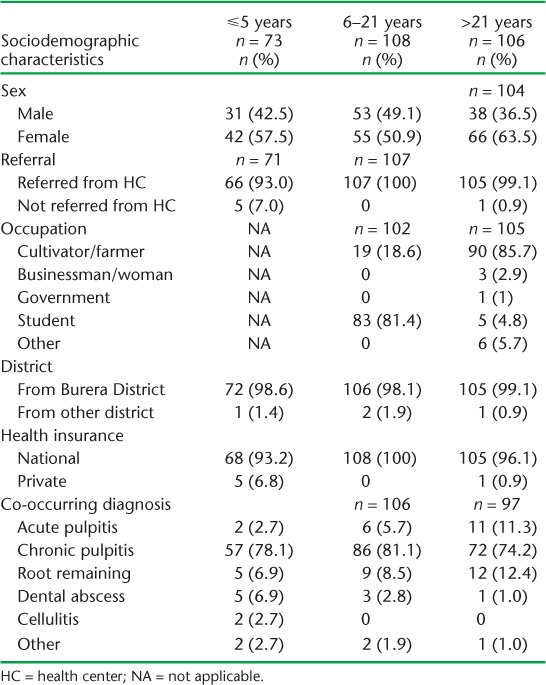
In the study, 73 encounters were included for children aged ⩽5 years, 108 encounters for patients aged 6–21 years and 106 encounters for those aged >21 years. In all age groups, females were more common (57.5% in the ⩽5 years age group, 50.9% in the 6–21 years age group and 63.5% in the >21 years age group) (Table 1). Most individuals (96.9%) were referred from HCs and were from Burera District (98.6%). In the 6–21 years age group, 81.4% were students, and in the oldest age group, 85.7% were farmers. All of the individuals sampled had health insurance; 97.9% had national community health insurance provided through the government. The most common co-occurring diagnosis with dental caries was chronic pulpitis (74.9%).
TABLE 1.
Sociodemographic characteristics and diagnosis of a sample of dental caries patients seen at Butaro District Hospital in 2013
Tooth extraction, pain killers and antibiotics were most commonly used for clinical management across the three age groups (Table 2). Overall, the majority of the patients (97.6%, n = 280) underwent tooth extraction, and 78.4% (n = 225) of these received anesthesia during tooth extraction. Across all the age groups, 89.6% (n = 257) received painkillers, and 98% of these (n = 252) had a tooth extracted. For the 271 patients who received antibiotics, 98.2% (n = 266) had a tooth extracted. There was no significant difference in the use of pain killers, antibiotics and tooth extraction across the three age groups (P = 0.082, P = 0.064 and P = 0.558, respectively). However, there was a significant difference in the use of anesthesia during tooth extraction across the age groups (P < 0.001), with most patients in the youngest (97.3%) and oldest (96.2%) age groups receiving anesthesia versus only 48.2% of the patients in the middle group. Tooth cleaning, tooth filling, oral hygiene advice and referral for further care were uncommon across all the age groups, with less than 2% of patients in each age group receiving this type of care.
TABLE 2.
Clinical management of patients seen with dental caries at Butaro District Hospital
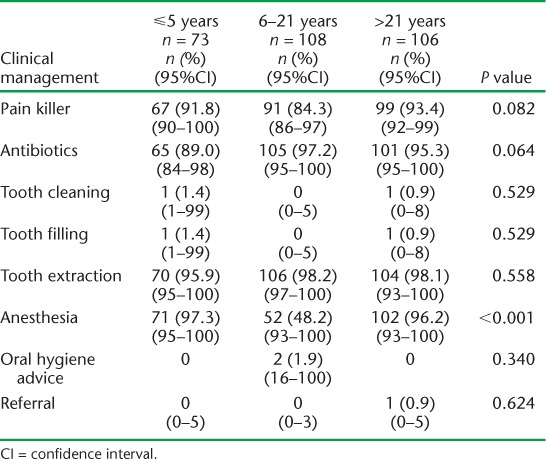
Further analysis of the relationship between co-occurring diagnosis and the three most common forms of clinical management showed that for patients co-diagnosed with chronic pulpitis, 79% received painkillers, 80% received antibiotics and 78.1% underwent tooth extraction. There was no significant difference in the use of painkillers and tooth extraction by co-occurring diagnosis (P = 0.327 and P = 0.171). However, there was a significant difference in the use of antibiotics (P = 0.005), with 96.7% use among those with chronic pulpitis, 89.5% for those with acute pulpitis, 88.5% among those with root remaining, 66.7% for dental abscess and 100% for cellulitis.
DISCUSSION
In our study, we found that more than 90% of patients with dental caries presenting at BDH underwent tooth extraction. This is consistent with the findings of a WHO report that notes that the rate of tooth extraction is considerably higher in low-income countries than in high-income nations.2 The pain and discomfort of dental caries and consequent tooth extraction places a financial burden on the family, leads to embarrassment due to changes in appearance, affects the individual's choice of foods and ability to eat, and impacts the general quality of life of individuals.11
The high rates of tooth extraction reflect two potential challenges in the health system. The first possibility is that patients are presenting late with severe dental disease, as supported by the fact that many individuals in our study also had chronic pulpitis. This may reflect a community-level lack of awareness about dental illnesses and the possibility of preventing dental diseases with proper oral hygiene. While health insurance coverage is high in Rwanda (93.4% of the population in Burera District were insured in October 2012),12 the fact that all the study patients had insurance may indicate that the uninsured are either not seeking care or that they are seeking care from practitioners outside the health system. The second health system challenge is the limited number of treatment options and dental technicians at the district hospital. Only one dental technician serves the entire district, working with limited dental equipment. Although 78 of the targeted 80 places for dental technicians were filled in Rwandan district hospitals in 2009, by 2011 there were only 66.13 The limited availability of treatment options necessitates advocacy for prevention as an immediate response to reduce the incidence of advanced dental illnesses.
The Rwandan Ministry of Health initiated the introduction of the country's first Bachelor of Dental Surgery program in 2012 through the Human Resources for Health program.14 This degree program, which is currently in development, aims to address the shortage of dental health providers and strengthen training for dental practitioners.15 Dental technicians currently receive the basic training needed to perform filling and tooth cleaning; while these skills could be used in some cases to avoid tooth extraction, they are not commonly practiced, mainly due to the lack of appropriate materials and equipment at the hospital. The advanced training through the Bachelor of Dental Surgery program therefore needs to be complemented by the availability of the necessary equipment at the district hospitals.
Although we cannot directly estimate the prevalence of dental caries with the available data, based on out-patient presentations we suspect that the magnitude of dental caries in Burera District and rural Rwanda as a whole is substantial. The most common presentations at BDH and in all Rwandan district hospitals are for quite advanced dental diseases (such as chronic pulpitis), suggesting that the greater population suffering from mild dental illness is likely high. Population-based studies in sub-Saharan Africa have estimated the prevalence of caries in adults and children to be as high as 40–60%,6–8 and we suspect a similar burden in the general Rwandan population.
To our knowledge, this is the first study describing how dental caries are managed in rural hospitals in sub-Saharan Africa. However, there are several limitations that should be considered in the interpretation of the results. Although the study is limited to one rural hospital, we believe it is representative of the management of the dental caries burden in other rural hospitals in Rwanda due to comparable data from the national health information system.
This study does not include details of the clinical management or outcomes of the dental caries cases who presented at health centers (the first place to seek care in Rwanda) but were not referred to the hospital, and this should be explored in future research. Finally, at the hospital, there were no detailed data on the type or severity of dental caries or other diagnoses (such as chronic pulpitis), and we could not comment on the appropriateness of the use of tooth extraction. We recommend that patients' dental files be modified to better assess the type and appropriateness of patient care in district hospitals.
CONCLUSION
With dental caries being the number one presentation at BDH and with more than 95% of these patients undergoing tooth extraction, caries prevention and alternative treatment options should be prioritized. Affordable fluoridated toothpastes have been reported as an effective means for caries prevention,16 and should be made available in rural Rwanda. Prevention measures should also be taken through a developed community program on oral health.
We also recommend a focused plan for improving dental health care in Rwanda, building on the Bachelor of Dental Surgery program that has recently been introduced. Dental health should be included in the next national Health Sector Strategic Plan and more advanced equipment, materials and training for dental caries management options, in addition to tooth extraction, should be introduced. In addition, increasing the number of dental technicians working in the public sector may improve access to care, and all health personnel should be trained in the WHO's Basic Package of Oral Care.16 While there are limited studies in this domain, we suspect that many sub-Saharan African countries are facing similar challenges and that dental care should be prioritized within national health systems. Future studies should estimate the burden and identify factors associated with dental caries in the general population in sub-Saharan Africa and assess interventions to prevent and better manage dental caries in rural settings.
Acknowledgments
The authors acknowledge Partners In Health (PIH)/Inshuti Mu Buzima (IMB) and the IMB Innovation Grants for the support of this work. This study was developed under the PIH/IMB Intermediate Operational Research Training Program, developed and facilitated by BHG and CLA. The authors are also grateful to the management of Butaro District Hospital for their support of this project.
Footnotes
CM and BU are both first authors.
Conflicts of interest: none declared.
References
- 1.Marcenes W, Kassebaum N J, Bernabé E et al. Global burden of oral conditions in 1990–2010: a systematic analysis. J Dent Res. 2013;92:592–597. doi: 10.1177/0022034513490168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Petersen P E, Bourgeois D, Ogawa H et al. The global burden of oral diseases and risks to oral health. Bull World Health Organ. 2005;85:661–669. [PMC free article] [PubMed] [Google Scholar]
- 3.Umesi-Koleso D C, Ayanbadejo P O, Oremosu O A. Dental caries trend among adolescents in Lagos, South-West Nigeria. West Afr J Med. 2007;26:201–205. doi: 10.4314/wajm.v26i3.28309. [DOI] [PubMed] [Google Scholar]
- 4.Gathecha G, Makokha A, Wanzala P et al. Dental caries and oral health practices among 12 year old children in Nairobi West and Mathira West Districts, Kenya. Pan Afr Med J. 2012;12:1–7. [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 5.Adeniyi A A, Agbaje O, Onigbinde O et al. Prevalence and pattern of dental caries among a sample of Nigerian public primary school children. Oral Health Prev Dent. 2012;10:267–274. [PubMed] [Google Scholar]
- 6.Mafuvadze B T, Mahachi L, Mafuvadze B. Dental caries and oral health practice among 12 year old school children from low socio-economic status background in Zimbabwe. Pan Afr Med J. 2013;14:1–6. doi: 10.11604/pamj.2013.14.164.2399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fakuda H, Ogada C N, Kihara E et al. Oral health status among 12-year-old children in a rural Kenyan community. J Dent Oral Health. 2014;1:1–5. [Google Scholar]
- 8.Rwenyonyi C M, Muwazi L M, Buwembo W. Assessment of factors associated with dental caries in rural communities in Rakai District, Uganda. Clin Oral Invest. 2011;15:75–80. doi: 10.1007/s00784-009-0363-4. [DOI] [PubMed] [Google Scholar]
- 9.Ndiaye C T. Oral health in the Africa region: progress and perspectives of the regional strategy. Afr J Oral Health. 2005;2:2–9. [Google Scholar]
- 10.Rwanda Ministry of Health. Rwanda Annual Health Statistics Booklet 2013. Kigali, Rwanda: Rwanda Ministry of Health; 2014. http://www.moh.gov.rw/fileadmin/templates/policies/Rwanda_Annual_Health_Statistics_Booklet_2013_signed.pdf Accessed June 2015. [Google Scholar]
- 11.Sischo L, Broder H L. Oral health-related quality of life: what, why, how, and future implications. J Dent Res. 2011;90:1264–1270. doi: 10.1177/0022034511399918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rwanda Ministry of Health. Annual Report: Community Based Health Insurance October 2012. Kigali, Rwanda: Rwanda Ministry of Health; 2012. http://www.moh.gov.rw/fileadmin/templates/Docs/CBHI-Annual-Report-2011-2012f-3__1_.pdf Accessed June 2015. [Google Scholar]
- 13.Rwanda Ministry of Health. Health Sector Strategic Plan 2012–2018. Kigali, Rwanda: Rwanda Ministry of Health; 2012. http://www.moh.gov.rw/fileadmin/templates/Docs/HSSP_III_FINAL_VERSION.pdf Accessed June 2015. [Google Scholar]
- 14.Binagwaho A, Kyamanywa P, Farmer P et al. The Human Resources for Health Program in Rwanda – A New Partnership. N Engl J Med. 2013;369:2054–2059. doi: 10.1056/NEJMsr1302176. [DOI] [PubMed] [Google Scholar]
- 15.Seymour B, Muhumuza I, Mumena C et al. Including oral health training in a health system strengthening program in Rwanda. Global Health Action. 2013;6:1–6. doi: 10.3402/gha.v6i0.20109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Petersen P E. Improvement of oral health in Africa in the 21st century—the role of the WHO Global Oral Health Programme. Developing Dentistry. 2004;5:9–20. [Google Scholar]


