Abstract
Importance
Thickening of the center of the retina, diabetic macular edema, is the most common cause of vision loss from diabetes. Treatment of diabetic macular edema has improved dramatically over the past few years. As such, prompt diagnosis and referral of patients with these complications has become more critical. Nonetheless, awareness and care of diabetic macular edema in the U.S. population is uncharacterized.
Objective
To characterize eye care and awareness of eye disease among persons with diabetic macular edema in the general U.S. population.
Design, Setting, and Participants
Cross-sectional analysis of data from participants in the 2005 to 2008 National Health and Nutrition Examination Survey aged 40 years or older with diabetes mellitus and fundus photographs.
Main Outcomes and Measures
Among those with diabetic macular edema: (1) awareness that diabetes has affected one's eyes; (2) report on last time one saw a diabetes specialist; (3) report on last time one had an eye exam with pupil dilation; and (4) prevalence of vision impairment.
Results
In 2010, 55.3% (95%confidence interval [CI], 37.6%-73.0%) of U.S. adults aged 40 years and older with diabetic macular edema reported they had not been told by a doctor that diabetes had affected their eyes or that they had retinopathy, 46.7% (95% CI, 27.5%-66.0%) reported they had not been to a diabetes nurse educator, dietician or nutritionist for their diabetes in the last year, and 39.3% (95% CI, 23.8%-54.8%) reported they did not receive an eye exam with dilation of the pupils in the last year. Among persons with diabetic macular edema, 28.7% (95% CI, 12.7%-44.7%) were visually impaired (visual acuity worse than 20/40 in the eye with diabetic macular edema) based on presenting visual acuity and 16.0% (95% CI, 2.5%-29.4%) based on best-corrected visual acuity.
Conclusions and Relevance
Many individuals with diabetes in the United States are not getting care that can avoid vision impairment and blindness. Strategies to increase awareness are warranted, especially given the recent availability of improved therapies for diabetic macular edema.
Diabetic retinopathy is the most common cause of new cases of blindness in working-age Americans,1 usually from proliferative diabetic retinopathy or diabetic macular edema. It is also the most common cause of less severe levels of vision impairment in this age group,2-4 most often from diabetic macular edema.5 Since diabetic macular edema can lead to substantial vision loss if left untreated for a year or more,6,7 health care providers need to be sure that individuals with diabetes are aware that diabetes can affect their eyes, especially those with diabetic macular edema. According to the American Diabetes Association8 and the American Academy of Ophthalmology,6 an eye exam with pupil dilation is needed at least annually to identify the presence of diabetic retinopathy—including diabetic macular edema—even in the absence of vision loss.
Treatment of diabetic macular edema has improved dramatically over the past few years. Recent government-sponsored and industry-sponsored trials9-14 have shown that injections of anti-vascular endothelial growth factor drugs, sometimes in combination with laser photocoagulation, safely provide superior vision outcomes compared with the previous standard of care of laser photocoagulation alone in eyes with diabetic macular edema causing vision impairment. For example, the National Institutes of Health-funded Diabetic Retinopathy Clinical Research Network reported in 2012 that ranibizumab with prompt or deferred laser photocoagulation in eyes with diabetic macular edema causing vision loss resulted in approximately 50% of treated eyes gaining substantial vision and less than 5% losing substantial vision through at least 3 years of follow-up compared with laser alone.9 However, prompt diagnosis and referral of patients with these complications is critical to initiate treatment before substantial vision loss has occurred. Despite these recent advances, awareness and care of diabetic macular edema in the U.S. population, to our knowledge, is uncharacterized. This study was undertaken to characterize the prevalence of eye care, awareness of eye disease, and vision impairment among persons with diabetic macular edema in the general U.S. population.
Methods
Study Population
The National Health and Nutrition Examination Survey (NHANES) is a series of cross-sectional surveys conducted by the National Center for Health Statistics, a part of the Centers for Disease Control and Preventions15. Participants are selected from the non-institutionalized civilian population in the United States using a stratified multistage probability sampling design. This study analyzed data from 2005 to 2008 NHANES cycles during which retinal photographs were obtained among participants aged 40 years or older. Persons were excluded from the retinal imaging exam for blindness, eye infections, or eye patches on both eyes.16 The present analysis includes persons who completed a mobile examination visit (n = 6797), with complete retinal imaging data (n = 5351), and who had self-reported diabetes mellitus (defined below; n = 798). The NHANES protocol was approved by a human subjects review board and written informed consent was obtained from all participants17.
Assessment of Diabetes and Diabetic Retinopathy
Persons were classified as having diagnosed diabetes if they answered yes to the question: “Have you ever been told by a doctor or health professional that you have diabetes or sugar diabetes?” Diagnosis of diabetic retinopathy, including diabetic macular edema, was based on grading of fundus photographs by masked graders at the University of Wisconsin Ocular Epidemiologic Reading Center, Madison, WI, using a single non-mydriatic image of the optic nerve and macula in each eye from a Canon CR6-45NM ophthalmic digital imaging system and Canon EOS 10D digital camera.
Assessment of Eye Care and Visual Acuity
Persons who reported a diagnosis of diabetes were asked the following questions during the interview: 1) “Have you been told by a doctor that diabetes has affected your eyes or that you had retinopathy?” 2) “When was the last time you saw a diabetes nurse educator, or dietitian or nutritionist for your diabetes?” and 3) “When was the last time you had an eye exam in which the pupils were dilated?” For the question regarding a visit to a diabetes specialist, the response options “13-24 months”, “greater than 2 years” and “never” were aggregated together in this analysis to improve the precision of the estimate for a combined group “>1 year or never”. Likewise, this aggregation was done for question 3 (the last time the individual had an eye exam in which the pupils were dilated). In addition, presenting and best-corrected visual acuity of eyes diagnosed with diabetic retinopathy and diabetic macular edema were determined. Presenting visual acuity was measured using the Nidek Auto Lensmeter ModelLM-990A allowing for individuals to use any necessary usual correction, which could include eyeglasses, contacts, or both. For eyes with usual correction of 20/30 or worse, best-corrected visual acuity was determined following refraction of these eyes using the Nidek Auto Refractor Model ARK-760. For eyes with usual correction better than 20/30, the usual correction was considered the best-corrected visual acuity. If both eyes had diabetic retinopathy and diabetic macular edema, the visual acuity of the worse-seeing eye was used in the analysis.
Statistical analysis
All analyses were performed incorporating the sampling weights to account for the complex NHANES sampling design. The standard errors for all estimates were obtained using the Taylor series (linearization) method following recommended procedures.18 Any estimate with an associated relative standard error greater than 30% of the estimate may be unreliable and should be interpreted with caution.19 Statistical analyses were conducted using SAS version 9.2 (SAS Institute, Cary, North Carolina).
Results
Characteristics of the population aged 40 years or older with diabetes are summarized in the TABLE. Among 798 persons with self-reported diabetes in the analytic sample, 238 had diabetic retinopathy without diabetic macular edema and 48 had diabetic macular edema. Persons with diabetic macular edema had higher glycated hemoglobin A1c and longer duration of diabetes compared with persons with diabetes without macular edema. Among those with diabetes and diabetic macular edema, only 44.7% (95% confidence interval [CI], 27.0%-62.4%) reported being told by a doctor that diabetes had affected their eyes or that they had retinopathy (FIGURE 1) compared with 26.1% (95% CI, 19.8%-32.3%) and 15.3% (95% CI, 12.3%-18.3%), respectively, with diabetic retinopathy but no macular edema or diabetes with no retinopathy. Only 49.2% (95% CI, 29.4%-69.0%) with diabetic macular edema reported seeing a diabetes nurse educator, or dietician or nutritionist for their diabetes within the past year compared with 33.5% (95% CI, 23.8%-43.3%) and 30.5% (95% CI, 26.1%-34.9%), respectively, with diabetic retinopathy but no macular edema or diabetes with no retinopathy. In contrast, 46.7% (95% CI, 27.5%-66.0%) with diabetic macular edema reported seeing such a person more than a year ago or never (FIGURE 2) compared with 64.7% (95% CI, 55.5%-74.0%) and 69.5% (95% CI, 65.1%-73.9%), respectively, with diabetic retinopathy but no macular edema or diabetes with no retinopathy. Furthermore, only 59.7% (95% CI, 43.5%-75.9%) of persons with diabetic macular edema reported having had an eye exam in which the pupils were dilated within the past year (FIGURE 3) compared with 67.5% (95% CI, 59.6%-75.4%) and 61.8% (95% CI, 54.7%-68.9%), respectively, with diabetic retinopathy but no macular edema or diabetes with no retinopathy. Among persons with diabetic macular edema, the presenting visual acuity of the eye with disease was 20/40 or better in 69.4% (95% CI, 52.9%-86.0%) compared with 76.6% (95%CI, 71.4%-81.8%) and 75.1 (95% CI, 70.8%-79.4%), respectively, with diabetic retinopathy but no macular edema or diabetes with no retinopathy, while the best-corrected visual acuity was 20/40 or better in 81.4% (95% CI, 66.6%-96.1%) compared with 87.3% (95%CI 83.2%- 91.5%) and 88.0% (95%CI, 84.5%- 91.5%), respectively, with diabetic retinopathy but no macular edema or diabetes with no retinopathy; (FIGURE 4 displays percentage of persons with DME with presenting or best-corrected visual acuity worse than 20/40).
Table 1.
Demographics and clinical characteristics of U.S. adults aged ≥40 years with self-reported diabetes stratified by diabetic retinopathy (DR) and diabetic macular edema (DME) status.
| Characteristicsa | Diabetes without DR or DME (Unweighted n=512) | DR without DME (Unweighted n=238) | DME (Unweighted n=48) | |||
|---|---|---|---|---|---|---|
| Unweighted frequency | Weightedb mean or % (95% CI) | Unweighted frequency | Weightedb mean or % (95% CI) | Unweighted frequency | Weightedb mean or % (95% CI) | |
| Age at screening, y | 512 | 60.1 (58.9-61.4) | 238 | 61.7 (59.8-63.5) | 48 | 62.8 (59.5-66.0) |
| Race/ethnicity,c % | ||||||
| Non-Hispanic White | 216 | 66.3 (57.0-75.6) | 91 | 64.8 (55.4-74.3) | 10 | 44.1 (23.8-64.3) |
| Hispanic | 143 | 12.7 (8.0-17.3) | 62 | 13.4 (8.4-18.3) | 15 | 16.7 (4.1-29.3) |
| Non-Hispanic Black | 138 | 14.7 (9.0-20.4) | 80 | 20.0 (14.0-26.0) | 23 | 39.3 (20.4-58.1) |
| Education level, % | ||||||
| Less than college education | 332 | 57.2 (48.9-65.4) | 158 | 56.0 (48.0-64.0) | 31 | 68.6 (52.4-84.9) |
| Any college | 180 | 42.8 (34.6-51.1) | 80 | 44.0 (36.0-52.0) | 17 | 31.4 (15.1-47.6) |
| Sex, % | ||||||
| Women | 276 | 56.8 (50.3-63.3) | 104 | 44.3 (36.3-52.2) | 24 | 51.0 (32.7-69.4) |
| Men | 236 | 43.2 (36.7-49.8) | 134 | 55.8 (47.8-63.7) | 24 | 49.0 (30.6-67.3) |
| BMI, kg/m2 | 502 | 32.7 (32.1-33.4) | 237 | 31.9 (30.8-33.0) | 48 | 33.6 (30.4-36.9) |
| Hypertension | ||||||
| Yes, % | 381 | 72.9 (67.5-78.4) | 184 | 68.4 (59.6-77.2) | 41 | 89.9 (79.4-100.0) |
| No, % | 131 | 27.1 (21.6-32.5) | 54 | 31.6 (22.8-40.4) | 7 | 10.1e (0-20.6) |
| History of CVDd | ||||||
| Yes, % | 138 | 27.7 (23.0-32.4) | 72 | 28.1 (21.6-34.5) | 13 | 22.0 (11.4-32.6) |
| No, % | 374 | 72.3 (67.6-77.0) | 166 | 71.9 (65.5-78.4) | 35 | 78.0 (67.4-88.6) |
| HbA1C, % | 491 | 6.8 (6.6-6.9) | 226 | 7.8 (7.5-8.1) | 44 | 8.1 (7.7-8.4) |
| Duration of diabetes, y | ||||||
| <10 y | 381 | 76.6 (73.2-80.1) | 87 | 36.4 (26.5-46.2) | 10 | 18.5e (6.7-30.3) |
| ≥10 y | 128 | 22.7 (19.2-26.1) | 151 | 63.6 (53.8-73.5) | 38 | 81.5 (69.7-93.3) |
Abbreviations: BMI, body mass index; CI, confidence interval; CVD, cardiovascular disease; DME, diabetic macular edema; DR, diabetic retinopathy; HbA1c, glycosylated hemoglobin A1c; WF, weighted frequency,
Data are weighted means (95% CI) or proportions (95% CI).
Weighted estimate accounts for multistage sampling design, oversampling, and survey nonresponse.
The “Other” race category was excluded because there were no DME cases in this group.
Based on self-report of congestive heart failure, coronary heart disease, angina pectoris, or heart attack.
Standard error is >30% of the estimate; estimate may be unreliable.
Figure 1.
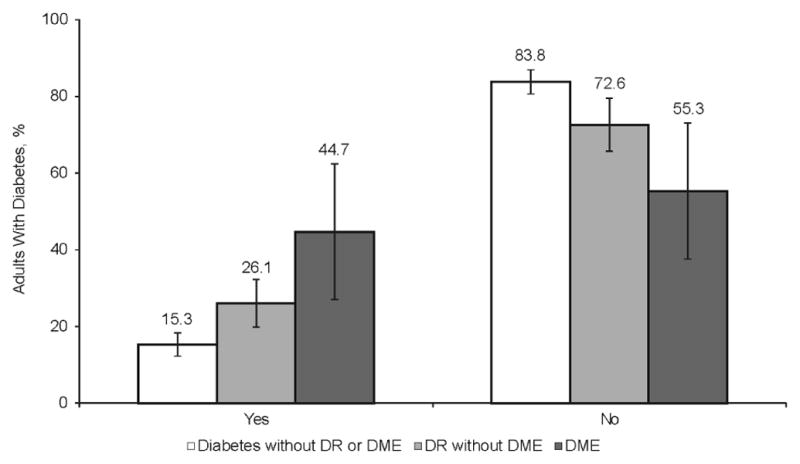
Awareness of eye diseases among U.S. adults aged ≥40 years with self-reported diabetes. Participants were asked “Have you been told by a doctor that diabetes has affected your eyes or that you had retinopathy?” Unknown category not reported. Error bars represent 95% confidence intervals. DME, diabetic macular edema; DR, diabetic retinopathy.
Figure 2.
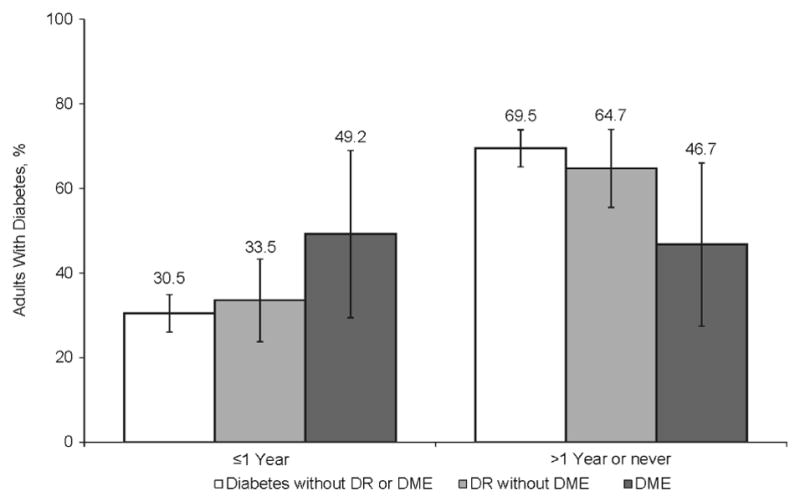
Self-reported last visit to a diabetes specialist among U.S. adults aged ≥40 years with diabetes. Participants were asked “When was the last time you saw a diabetes nurse educator, or dietitian or nutritionist for your diabetes?” The total for each cohort equals 100%. If not, the difference represents subject who responded as “don't know” to this question (not shown). Error bars represent 95% confidence intervals. DME, diabetic macular edema; DR, diabetic retinopathy.
Figure 3.
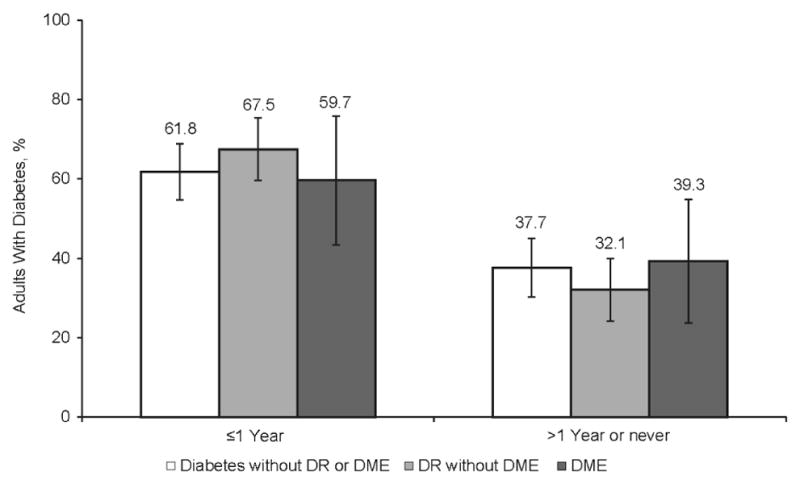
Self-reported last pupil dilation exam among U.S. adults ≥40 years with diabetes. Participants were asked “When was the last time you had an eye exam in which the pupils were dilated?” The total for each cohort equals 100%. If not, the difference represents subject who responded as “don't know” to this question (not shown). Error bars represent 95% confidence intervals. DME, diabetic macular edema; DR, diabetic retinopathy.
Figure 4.
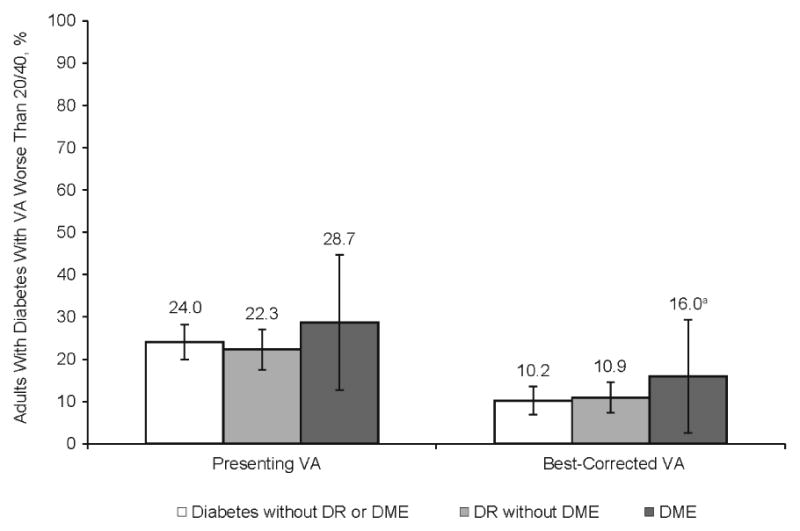
Percentage of U.S. adults aged ≥40 years with diabetes, diabetes and diabetic retinopathy (DR) without diabetic macular edema (DME), or diabetes with DME, with presenting or best-corrected visual acuity (VA) worse than 20/40. Unknown category not reported. Error bars represent 95% confidence intervals. aStandard error is >30% of the estimate; estimate may be unreliable.
Comment
Diabetic macular edema is a major cause of vision impairment among U.S. adults aged 40 years and older with diabetes.1,20,21 A recent report suggests that approximately 745,000 persons with diabetes in the U.S. population have swelling of the center of the retina or diabetic macular edema.22 Treatment of diabetic macular edema has improved dramatically over the past few years, so that prompt diagnosis and referral of patients with these complications has become more critical. Since, to our knowledge, the awareness and care of diabetic macular edema in the U.S. population is uncharacterized, this study aimed to characterize eye care and awareness of eye disease among persons with diabetic macular edema in the general U.S. population. Our results suggest that many individuals with diabetic macular edema report not receiving prompt diabetes-related or eye-related care, even though many of these individuals are at risk of substantial vision loss which could be lessened or eliminated with appropriate care. Furthermore, many people aged 40 years and older in the United States have diabetic macular edema with best-corrected visual acuity of 20/40 or better when they may not be seeking vision correction services, including many who are unaware that diabetes has affected their eyes. This study indicates that, even though diabetic macular edema is a major cause of vision impairment among people with diabetes, many individuals with diabetic macular edema report not receiving diabetes-related or eye-related care for at least 1 year.
Limitations of this study include the relatively small number of NHANES participants with diabetic macular edema, fundus photographs were not stereoscopic pairs, and optical coherence tomography measurements were not available to determine the proportion of cases with central macular thickening among those in whom diabetic macular edema was or was not suggested by retinal photographs. Furthermore, the answers to the eye care questions were based on self-report (as opposed to actual recorded utilization), precluding the ability to eliminate recall bias. The possibility of under-reporting cannot be excluded, nor can its magnitude, if present, be determined. However, with respect to pupil dilation, self-reported use within the last year was comparable to the National Committee for Quality Assurance indicators report,23 suggesting that the self-reported data, at least for that parameter, is likely not affected substantially by recall bias. Also, persons who are severely ill may be less likely to participate in NHANES. While the NHANES design should account for this differential nonresponse by health status, it remains possible that severely ill people are under-represented in this dataset.
In summary, our results suggest that despite recent successes in the ability to treat vision loss from diabetes, one of the most frequent and most feared complications of the disease, hundreds of thousands of people in the United States report they are not getting care which can avoid vision impairment and blindness. These findings from the NHANES, which present nationally representative estimates of the burden of diabetic eye disease and awareness of having the condition in the general U.S. population, emphasize the need to strengthen our efforts in educating patients with diabetes on the eye complications of the disease. These efforts include getting patients to health care providers including diabetes nurse educators, dieticians, nutritionists, primary care physicians, or endocrinologists for treatment of their diabetes; getting appropriate eye exams to detect and treat diabetic retinopathy, including diabetic macular edema; and identifying strategies which might result in greater awareness and appropriate eye care 24 to reduce the magnitude of vision impairment and blindness from this common complication of diabetes mellitus.
Acknowledgments
Study concept and design: Bressler, Varma, Doan, Danese, Dolan, Colman, Turpcu.
Acquisition of data: Doan, Danese, Bower, Selvin, Turpcu.
Analysis and interpretation of data: Bressler, Varma, Doan, Gleeson, Danese, Bower, Selvin, Dolan, Fine, Colman, Turpcu.
Drafting of the manuscript: Bressler, Varma, Doan, Bower, Selvin, Dolan.
Critical revision of the manuscript for important intellectual content: Bressler, Varma, Doan, Gleeson, Danese, Bower, Selvin, Dolan, Fine, Colman, Turpcu.
Statistical analysis: Bower, Selvin, Doan, Gleeson.
Obtained funding: Bressler, Doan, Colman.
Administrative, technical, or material support: Bressler, Dolan, Fine, Colman.
Funding/Support: This study was supported by a grant from Genentech, Inc./Roche to The Johns Hopkins University through the Office of Research Administration of the Johns Hopkins University School of Medicine. Support for third-party editorial assistance by Rebecca Jarvis, PhD, CMPP, of Envision Scientific Solutions, was provided by Genentech, Inc. This effort does not meet authorship criteria per ICJME guidelines including no involvement in study design, analysis, drafting, or critically revising the manuscript.
Footnotes
Meeting presentations: Portions of these data were presented at the 2012 Retina Society Annual Meeting, Washington, DC (September 28, 2012) and the 2013 Macula Society Annual Meeting, Dana Point, CA (March 1, 2013) and the 2012 American Academy of Optometry Annual Meeting, Phoenix, AZ (October 24, 2012).
Author Contributions: Drs. Bressler, Bower, and Selvin had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Role of the Sponsor: Genentech, Inc./Roche employees participated in the design of the study and in the revision of the manuscript, but The Johns Hopkins University School of Public Health investigators independently replicated and verified all analyses.
Independent Statistical Analysis: An independent statistical analysis, used for all data provided in the manuscript, was conducted by the Johns Hopkins University Bloomberg School of Public Health faculty (Drs. Bower and Selvin). Additional statistical analysis was performed by Outcomes Insights, Inc. (Q.V. Dolan, M. Gleeson). Genentech, Inc./Roche employees did not participate in the statistical analysis but did have access to the data prior to the completion of data analysis.
Conflict of Interest Disclosures: N. Bressler is principal investigator of grants at The Johns Hopkins University sponsored by the following entities (not including the National Institutes of Health): Bausch & Lomb Incorporated; ForSight Labs, LLC; Genentech, Inc.; Genzyme Corporation; Lumenis Inc.; Notal Vision; Novartis Pharma AG; Optovue, Inc.; Regeneron Pharmaceuticals, Inc. R. Varma is a consultant for Allergan, Aquesys, Genentech, Merck, and Replenish and has received research funding from Genentech, and Replenish. Q. Doan, M. Gleeson, and M. Danese are employees of Outcomes Insights, Inc. and paid consultants for Genentech. J. Bower and E. Selvin are co-investigators of Dr Bressler's grant at The Johns Hopkins University sponsored by Genentech. C. Dolan is a paid consultant for Genentech. A. Turpcu, J. Fine, and S. Colman are employees of Genentech.
Contributor Information
Neil Bressler, Email: nmboffice@jhmi.edu.
Rohit Varma, Email: rvarma@uic.edu.
Quan V. Doan, Email: quan@outins.com.
Michelle Gleeson, Email: michelle@outins.com.
Mark Danese, Email: mark@outins.com.
Julie K. Bower, Email: jbower@jhsph.edu.
Elizabeth Selvin, Email: lselvin@jhsph.edu.
Chantal Dolan, Email: chantal.dolan@gmail.com.
Jennifer Fine, Email: fine.jennifer@gene.com.
Shoshana Colman, Email: shoshanc@gene.com.
Adam Turpcu, Email: adamht@gene.com.
References
- 1.Centers for Disease Control and Prevention. National diabetes fact sheet. [Accessed April 30, 2013];2011 http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf.
- 2.Roy MS, Klein R, O'Colmain BJ, Klein BE, Moss SE, Kempen JH. The prevalence of diabetic retinopathy among adult type 1 diabetic persons in the United States. Arch Ophthalmol. 2004;122(4):546–551. doi: 10.1001/archopht.122.4.546. [DOI] [PubMed] [Google Scholar]
- 3.Congdon N, O'Colmain B, Klaver CC, et al. Eye Diseases Prevalence Research Group. Causes and prevalence of visual impairment among adults in the United States. Arch Ophthalmol. 2004;122(4):477–485. doi: 10.1001/archopht.122.4.477. [DOI] [PubMed] [Google Scholar]
- 4.Prevent Blindness America. Vision problems in the U.S.: prevalence of adult visioni Impairment and age-related eye disease in America [2008] [Accessed April 30, 2013]; http://www.preventblindness.net/site/DocServer/VPUS_2008_update.pdf.
- 5.Klein R, Lee KE, Gangnon RE, Klein BE. The 25-year incidence of visual impairment in type 1 diabetes mellitus the wisconsin epidemiologic study of diabetic retinopathy. Ophthalmology. 2010;117(1):63–70. doi: 10.1016/j.ophtha.2009.06.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American Academy of Ophthalmology Retina/Vitreous Panel. Preferred Practice Pattern® Guidelines: diabetic retinopathy. San Francisco, CA: American Academy of Ophthalmology; 2008. [Accessed April 30, 2013]. www.aao.org/ppp. [Google Scholar]
- 7.Ferris FL. How effective are treatments for diabetic retinopathy? JAMA. 1993;269(10):1290–1291. [PubMed] [Google Scholar]
- 8.American Diabetes Association. Standards of medical care in diabetes–2013. Diabetes Care. 2013;36(suppl 1):S11–S66. doi: 10.2337/dc13-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Elman MJ, Qin H, Aiello LP, et al. Diabetic Retinopathy Clinical Research Network. Intravitreal ranibizumab for diabetic macular edema with prompt versus deferred laser treatment: three-year randomized trial results. Ophthalmology. 2012;119(11):2312–2318. doi: 10.1016/j.ophtha.2012.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rajendram R, Fraser-Bell S, Kaines A, et al. A 2-year prospective randomized controlled trial of intravitreal bevacizumab or laser therapy (BOLT) in the management of diabetic macular edema: 24-month data: report 3. Arch Ophthalmol. 2012;130(8):972–979. doi: 10.1001/archophthalmol.2012.393. [DOI] [PubMed] [Google Scholar]
- 11.Nguyen QD, Brown DM, Marcus DM, et al. RISE and RIDE Research Group. Ranibizumab for diabetic macular edema: results from 2 phase III randomized trials: RISE and RIDE. Ophthalmology. 2012;119(4):789–801. doi: 10.1016/j.ophtha.2011.12.039. [DOI] [PubMed] [Google Scholar]
- 12.Mitchell P, Bandello F, Schmidt-Erfurth U, et al. RESTORE study group. The RESTORE study: ranibizumab monotherapy or combined with laser versus laser monotherapy for diabetic macular edema. Ophthalmology. 2011;118(4):615–625. doi: 10.1016/j.ophtha.2011.01.031. [DOI] [PubMed] [Google Scholar]
- 13.Do DV, Nguyen QD, Boyer D, et al. DA VINCI Study Group. One-year outcomes of the DA VINCI Study of VEGF Trap-Eye in eyes with diabetic macular edema. Ophthalmology. 2012;119(8):1658–1665. doi: 10.1016/j.ophtha.2012.02.010. [DOI] [PubMed] [Google Scholar]
- 14.Ohji M, Ishibashi T REVEAL study group. Efficacy and safety of ranibizumab 0.5 mg as monotherapy or adjunctive to laser versus laser monotherapy In Asian patients with visual impairment due to diabetic macular edema: 12-month results of the REVEAL study. Presented at: the Association for Research in Vision and Ophthalmology Annual Meeting; May 6-9, 2012; Fort Lauderdale FL. [Google Scholar]
- 15.Centers for Disease Control and Prevention. About the National Health and Nutrition Examination Survey. [Accessed April 30, 2013]; http://www.cdc.gov/nchs/nhanes/about_nhanes.htm. Updated April 2, 2013.
- 16.Center for Disease Control and Prevention. National Health and Nutrition Examination Survey (NHANES): ophthalmology procedures manual. [Accessed April 30, 2013]; http://www.cdc.gov/nchs/data/nhanes/nhanes_05_06/OP.pdf. Updated September 2005.
- 17.Centers for Disease Control and Prevention. Plan and operation of the Third National Health and Nutrition Examination Survey, 1988-94. Vial Health Stat 1. 1994;(32):1–407. [Google Scholar]
- 18.National Center for Health Statistics and the Centers for Disease Control and Prevention. ANALYTIC AND REPORTING GUIDELINES: The National Health and Nutrition Examination Survey (NHANES) http://www.cdc.gov/nchs/data/nhanes/nhanes_03_04/nhanes_analytic_guidelines_dec_2005.pdf. Accessed March 25, 2013.
- 19.Centers for Disease Control and Prevention. NHANES 1999–2000 addendum to the NHANES III Analytic Guidelines. [Accessed April 30, 2013]; http://www.cdc.gov/nchs/data/nhanes/guidelines1.pdf.
- 20.Moss SE, Klein R, Klein BE. Ten-year incidence of visual loss in a diabetic population. Ophthalmology. 1994;101(6):1061–1070. doi: 10.1016/s0161-6420(94)31217-6. [DOI] [PubMed] [Google Scholar]
- 21.Klein R, Klein BE. Diabetes in America. 2nd. Bethesda, MD: National Diabetes Data Group of the National Institute of Diabetes and Digestive and Kidney Diseases National Institutes of Health; 1995. Chapter 14: vision disorders in diabetes; pp. 293–338. http://diabetes.niddk.nih.gov/dm/pubs/america/pdf/chapter14.pdf. [Google Scholar]
- 22.Varma R, Bressler NM, Doan Q, et al. African Americans at highest risk of diabetic macular edema compared with non-Hispanic whites and Hispanics: the prevalence of and risks for diabetic macular edema from the National Health and Nutrition Examination Survey. Presented at: the American Academy of Ophthalmology 2012 Annual Meeting; Nov 10-13, 2012; Chicago, IL. [Google Scholar]
- 23.National Committee for Quality Assurance. Continuous improvement and the expansion of quality measurement: the state of health care quality 2011. Washingtonn, DC: National Committee for Quality Assurance; 2011. [Accessed April 30, 2013]. http://www.ncqa.org/Portals/0/SOHC-web1.pdf. [Google Scholar]
- 24.Diabetic Retinopathy Clinical Research Network (DRCRnet) Effect of diabetes education during retinal ophthalmology visits on diabetes control. [Accessed April 30, 2013]; http://drcrnet.jaeb.org/Studies.aspx?RecID=197.


