Abstract
Background
There is a lack of recent studies examining recording of influenza-like illness (ILI) in primary care in the UK over time and according to population characteristics. Our aim was to determine time trends and socio-demographic patterns of ILI recorded consultations in primary care.
Methods
We used The Health Improvement Network (THIN) UK primary care database and extracted data on all ILI consultations between 1995 and 2013. We estimated ILI recorded consultation rates per 100,000 person-weeks (pw) by age, gender, deprivation and winter season. Negative binomial regression models were used to examine time trends and the effect of socio-demographic characteristics. Trends in ILI recorded consultations were compared to trends in consultations with less specific symptoms (cough or fever) recorded.
Results
The study involved 7,682,908 individuals in 542 general practices. The ILI consultation rate decreased from 32.5/100,000 pw (95% confidence interval (CI) 32.1, 32.9) in 1995–98 to 15.5/100,000 pw (95% CI 15.4, 15.7) by 2010–13. The decrease occurred prior to 2002/3, and rates have remained largely stable since then. Declines were evident in all age groups. In comparison, cough or fever consultation rates increased from 169.4/100,000 pw (95% CI 168.6, 170.3) in 1995–98 to 237.7/100,000 pw (95% CI 237.2, 238.2) in 2010–13. ILI consultation rates were highest among individuals aged 15–44 years, higher in women than men, and in individuals from deprived areas.
Conclusion
There is substantial variation in ILI recorded consultations over time and by population socio-demographic characteristics, most likely reflecting changing recording behaviour by GPs. These results highlight the difficulties in using coded information from electronic primary care records to measure the severity of influenza epidemics across time and assess the relative burden of ILI in different population subgroups.
Introduction
The influenza virus is a common cause of respiratory tract infections. Antigenic shift of the virus may lead to pandemics,[1] the most recent caused by influenza A/H1N1 in 2009.[2] Although the majority of infections are mild and self-limiting, influenza can cause severe complications leading to hospital admission or death.[3, 4] Nationally representative influenza surveillance systems are required by governments to implement timely prevention efforts to mitigate the effects of seasonal and pandemic influenza.
In the United Kingdom (UK) and many other countries, a cornerstone of clinical influenza surveillance is monitoring of patient consultations in primary care.[5, 6] These surveillance systems are based on extracts from primary care electronic records where a relevant diagnosis has been made. However, influenza is difficult to diagnose clinically, and only a small minority of suspected cases undergo confirmatory diagnostic tests in a primary care setting. Instead, general practitioners (GPs, primary care physicians) make decisions regarding diagnosis and management during a short consultation, based solely on presenting symptoms. Primary care surveillance is therefore based on a clinical diagnosis of influenza-like illness (ILI), rather than influenza itself. The symptoms included in the clinical definition of ILI include sudden onset of fever (above 38.5°C) and cough.[7, 8] However, ILI symptoms can be caused by a number of other viruses, including adenovirus, rhinovirus and human metapneumovirus.[9, 10] Conversely, persons with influenza may not receive a diagnosis of ILI when they consult primary care. A recent community study demonstrated that only 8% of a small sample of symptomatic individuals with confirmed influenza who consulted their GP had ILI recorded in their primary care record.[11]
Coding of ILI in primary care records may be driven by the incidence of influenza and other respiratory viruses, or unrelated factors. Such factors include clinician preference or recommendations regarding treatment, which may change over time, such as during pandemics.[12] ILI recording rates in primary care are also likely to be determined by demographic characteristics. For example, ILI consultation rates have been found to consistently vary by age group, with the highest consultation rates in young children compared to adults,[13, 14] and in women compared to men.[15] Studies of ILI recording in UK primary care are now dated.[15–17]. Our objectives were to determine long-term trends in recording of ILI in UK primary care, examine more recent recording patterns according to population socio-demographic characteristics, and variation in recording at GP practice level. We aimed to inform interpretation of data from surveillance systems for ILI based on electronic primary care records.
Methods
Data source
Around 98% of the UK population is registered with a GP.[18] The Health Improvement Network (THIN) is a database containing longitudinal primary care records from around 6% of the UK population, registered with GP practices that use VISION patient management software and have agreed to contribute data to THIN.[19] THIN contains data on prescriptions and diagnoses, together with additional demographic information. The registered THIN population is broadly representative of UK demography, and general practices contributing data to THIN are representative of UK general practices in terms of prescribing and consultation frequency.[20, 21]
Diagnoses and symptoms are entered in primary care electronic records using Read codes [22] by the GP, usually during patient consultations. Read codes are a coding system used to record clinical summary information. Two systematic reviews [23, 24] found that a high proportion of diagnoses recorded as Read codes in electronic medical records were confirmed using internal validation, or external validation using GP questionnaires or paper medical records. Prescriptions are entered using drug codes that map onto chapters of the British National Formulary.[25]
Severe outcomes of influenza are more common in persons of low socio-economic status,[26, 27] and consultations rates for lower respiratory tract infections are higher among individuals living in deprived areas.[28] We therefore examined the effect of socio-economic deprivation on ILI consultations, using quintiles of Townsend scores. The Townsend score is a small area based measure of multiple deprivation based on data from the 2001 Census. It takes into account property and car ownership, overcrowding and unemployment in the resident population of a small area consisting of approximately 150 households. In THIN, the Townsend score is linked to a patient through their postcode of residence by the data providers; however the actual postcodes and lower level geographies are not made available to researchers due to concerns regarding anonymity.
Study population and period
We included all individuals registered in a contributing THIN practice from birth up to 99 years inclusive, who were registered for at least seven days at any point during the study period, 2nd October 1995 to 19th May 2013. Patient electronic records were included from the date at which practices met quality criteria regarding data entry.[29, 30] We examined consultations occurring in the winter seasons 1995/1996 to 2012/2013, where a winter season is defined as Monday week 40 (beginning of October) in year x to Sunday in week 20 (middle of May) in year x+1.[31]
Definition of influenza-like illness (ILI)
We used established methods based on word searches of the Read code dictionary,[32] to create a code list for ILI (S1 Table), including codes for influenza-like illness, influenza and positive swab results for influenza. These codes were chosen as they indicate clinicians’ willingness to record a specific diagnosis of ILI or influenza infection (even if only suspected). We also included prescriptions of neuraminidase inhibitors (NIs, oseltamivir or zanamivir) as indicators of ILI.
We compared trends in recording of specific ILI codes to trends in recording of cough or fever (S1 Table), as an indicator of recording of non-specific symptoms of respiratory tract infections. We chose fever or cough as these two symptoms are recommended for community influenza surveillance by the World Health Organisation,[8] although only a minority of cough or fever episodes would be expected to be caused by influenza.[11] Since it is rare for GPs to record two different diagnoses during a consultation, we did not examine recording of cough or fever during the same consultation. We included only the first ILI record per person within each season as infection with two different influenza strains during a season is rare,[33] and only a small minority (around 1%) of persons consulting with ILI consulted twice or more during a season. Likewise, we only included the first cough or fever consultation per person per season in order to carry out similar comparisons over time between specific and non-specific diagnoses.
Statistical methods
Time trends in ILI recorded consultations, 1995–2013
We calculated consultation rates for ILI and cough or fever symptoms per 100,000 person-weeks with 95% confidence intervals (CI), according to gender, age group (coded into standard groups for influenza, [34, 35] see S2 Table), quintiles of Townsend score and winter season. We validated the ILI consultation rate in THIN in 2010 against the ILI consultation rate from a separate primary care surveillance scheme in England, run by the Royal College of General Practitioners (RCGP).[36]
We calculated the percentage change in ILI and cough or fever consultation rates between the first three seasons (1995/96, 1996/97 and 1997/98) and the last three seasons (2010/11, 2011/12 and 2012/13) of the study period.
Details of model fitting are fully described in S1 text. Briefly, we fitted negative binomial regression models with number of ILI consultations in a winter season as the outcome variable, ordered winter season (eg. 1995/96 = 1, 1996/97 = 2) as the predictor variable (using restricted cubic splines) and person-time at risk as the offset. We varied the number of internal knots of the splines from one to five to obtain the best fit to the data. The knots were placed at equally spaced percentiles of the distribution of ordered winter season, as suggested by Harrell.[37] Age group, gender, Townsend quintile and a pandemic season indicator were added as covariates. Interaction terms between ordered winter season: age group, and the pandemic indicator: age group were included to examine whether time trends were significantly different according to age group. We used minimisation of Akaike’s Information Criterion (AIC) to determine whether the inclusion of a particular variable significantly improved the fit of the model.
Recent recoding of ILI according to socio-demographic characteristics, 2010–2013
To examine recent ILI recording according to socio-demographic variables, we fitted negative binomial regression models with number of ILI recorded consultations as the outcome variable, age group, gender, winter season, Townsend quintile and a gender: age group interaction term as predictor variables and person-time at risk as the offset, to data from the last three seasons of the study period. The AIC was used to determine whether a particular variable significantly improved the fit of the model. We calculated the proportion of the registered population at the start of each season who had at least one consultation for ILI during that season, by age group, gender and Townsend quintile, with 95% confidence intervals.
Practice-level variation in ILI recorded consultations, 2010–2013
We predicted the number of consultations with an ILI recorded by practice, based on the model with age, gender, winter season and Townsend quintile, and divided the observed by the predicted number of ILI consultations to calculate standardised consultation ratios (SCRs). We used funnel plots,[38] with 95% overdispersion-adjusted control limits to compare the SCRs against an SCR of 1, which would be expected if observed and expected consultation rates were equal.
All statistical analyses were carried out using Stata version 13.[39]
Ethics
All data were anonymised. THIN data collection has been approved by the South East NHS Multicentre Research Ethics Committee. The analyses for this study were approved by the Scientific Review Committee of the data providers (CSD Medical Research, now IMS Health), study reference number SRC 14–004.
Results
The study included 7,682,908 individuals from 542 general practices, who had 287,320 first episodes of ILI during the 18 winter seasons in the study period. S2 Table shows the distribution of socio-demographic variables in the study population. The overall ILI consultation rate during winter seasons was 17.1/100,000 person-weeks (pw; 95% CI 17.0, 17.1 per 100,000 pw). In 2010, the overall rate of ILI was 12.2/100,000 pw in THIN and 11.8/100,000 pw in the RCGP network.
Time trends in ILI recorded consultations, 1995–2013
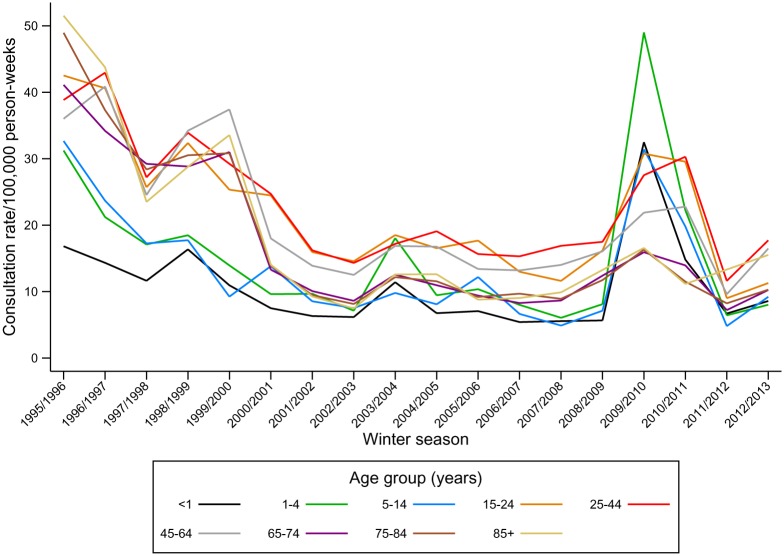
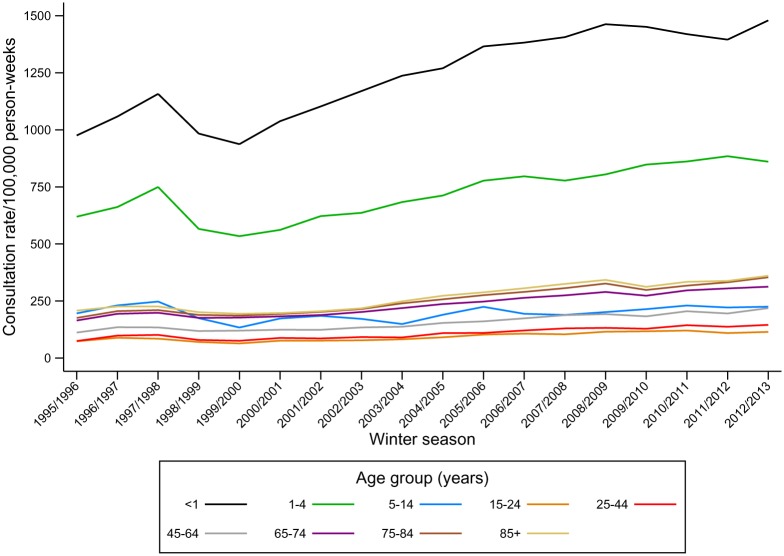
ILI consultation rates decreased by 52% during the study period (Fig 1); from 32.5/100,000 pw in the first three seasons, 1995/96, 1996/97 and 1997/98, (95% CI 32.1, 32.9) to 15.5/100,000 pw (95% CI 15.4, 15.7) in the last three seasons (2010/11, 2011/12 and 2012/13). This decline occurred prior to 2002/3 (S3 Table). After this date ILI consultation rates remained largely stable, apart from year-on-year variations and the peak in consultations during the 2009/10 pandemic (Fig 1). In contrast, consultation rates for non-specific cough or fever symptoms increased by 40% from 169.4/100,000 pw (95% CI 168.6, 170.3) to 237.7/100,000 pw (95% CI 237.2, 238.2) between the first three and the last three seasons (Fig 2, S3 Table).
Fig 1. Consultation rates for ILI (per 100,000 person-weeks) by age group and winter season, 1995–2013.
Fig 2. Consultation rates for cough or fever symptoms (per 100,000 person-weeks) by age group and winter season, 1995–2013*.
*Note difference in scale on y-axis cf. Fig 1.
A cubic spline with four internal knots at 2002/03, 2004/05, 2007/08 and 2009/10 best explained the time trend in ILI consultations, based on minimisation of the AIC. Including the age group: season, and age group: pandemic indicator interaction terms significantly improved model fit, implying that the observed trends over time in ILI recorded consultations vary significantly by age group. S1 Fig shows the fit of the final models. An overall decline prior to 2002/3 in ILI consultations was observed in all age groups, but the largest declines were observed in individuals aged 65 years or above. Children aged less than 15 years experienced the highest peak in consultations during the 2009–2010 pandemic.
Recent recoding of ILI according to socio-demographic characteristics, 2010–2013
Overall, ILI consultation rates were higher among women than men, but this difference varied by age group (an age group: gender interaction term significantly improved model fit based on minimisation of AIC). Consultation rates were higher in women than in men among individuals aged between 15 and 74 years. Only small gender differences in consultation rates were observed in children aged less than 15 years and persons aged over 75 years (Table 1). Individuals living in more deprived areas had higher consultation rates (incidence rate ratio comparing highest versus lowest Townsend deprivation quintile 1.25 (1.14, 1.37).
Table 1. Observed consultation rates and adjusted incidence rate ratios by age group, gender, winter season and Townsend quintile, 2010–2013*.
| Variable | Consultation rates/100,000 pw (95% CI) | Adjusted incidence rate ratios † (95% CI) |
|---|---|---|
| Townsend quintile | ||
| 1st (least deprived) | 14.1 (13.9, 14.4) | 1 (baseline) |
| 2nd | 14.6 (14.3, 14.8) | 1.04 (0.99, 1.09) |
| 3rd | 15.8 (15.5, 16.1) | 1.13 (1.05, 1.20) |
| 4th | 16.6 (16.3, 16.9) | 1.18 (1.09, 1.28) |
| 5th (most deprived) | 17.8 (17.4, 18.2) | 1.25 (1.14, 1.37) |
| Season | ||
| 2010/11 | 23.5 (23.2, 23.8) | 1 (baseline) |
| 2011/12 | 9.2 (9.0, 9.3) | 0.39 (0.37, 0.41) |
| 2012/13 | 13.9 (13.7, 14.1) | 0.59 (0.56, 0.62) |
| Men | ||
| Age group (years) | ||
| <1 year | 11 (9.6, 12.5) | 0.66 (0.49, 0.88) |
| 1–4 years | 12.3 (11.6, 13.1) | 0.73 (0.65, 0.83) |
| 5–14 years | 11.2 (10.8, 11.7) | 0.66 (0.61, 0.72) |
| 15–24 years | 13.5 (13.0, 14.0) | 0.80 (0.76, 0.84) |
| 25–44 years | 16.7 (16.3, 17.0) | 1 (baseline) |
| 45–64 years | 13.5 (13.1, 13.8) | 0.84 (0.80, 0.87) |
| 65–74 years | 9.1 (8.6, 9.6) | 0.57 (0.53, 0.60) |
| 75–84 years | 9.5 (8.8, 10.1) | 0.59 (0.53, 0.65) |
| 85–99 years | 12.5 (11.2, 13.9) | 0.77 (0.65, 0.92) |
| Women | ||
| Age group | ||
| <1 year | 9.1 (7.8, 10.6) | 0.39 (0.30, 0.51) |
| 1–4 years | 12.2 (11.4, 12.9) | 0.52 (0.46, 0.59) |
| 5–14 years | 11.4 (11.0, 11.9) | 0.49 (0.45, 0.52) |
| 15–24 years | 19.8 (19.2, 20.4) | 0.85 (0.82, 0.88) |
| 25–44 years | 23.3 (22.8, 23.7) | 1 (baseline) |
| 45–64 years | 19.2 (18.8, 19.5) | 0.84 (0.81, 0.87) |
| 65–74 years | 11.7 (11.2, 12.2) | 0.53 (0.50, 0.56) |
| 75–84 years | 10.4 (9.9, 11.0) | 0.47 (0.43, 0.51) |
| 85–99 years | 13.7 (12.7, 14.7) | 0.61 (0.47, 0.79) |
*Model included 507 practices with data from the seasons 2010/11-2012/13.
†Model included linear predictors for age group, gender, Townsend score, season and an age group:gender interaction term.
Only 0.5% of the registered population had a record of at least one ILI consultation during the last three winters (combined) of the study period. Even in the age, gender and deprivation groups with the highest consultation rates, the proportion with one or more ILI consultations during a winter season did not exceed 1% (S2 Fig).
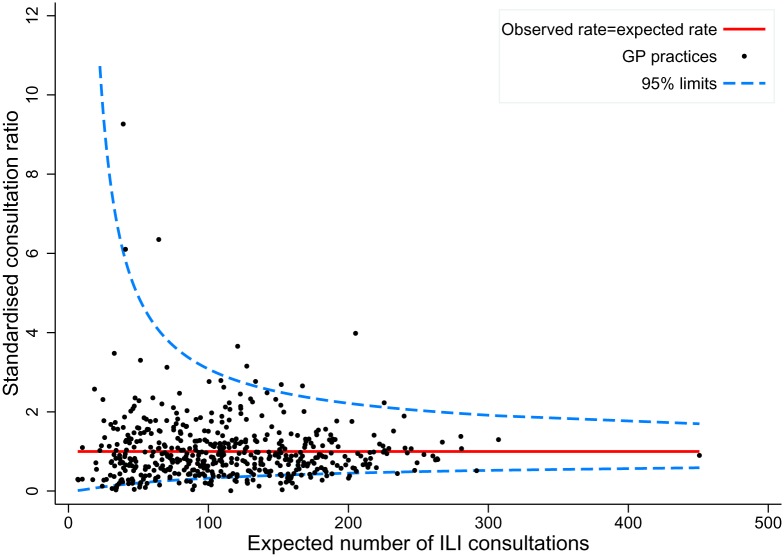
Practice-level variation in ILI recorded consultations, 2010–2013
Practice-level ILI consultation rates varied between 0.1/100,000 pw to 154.3/100,000 pw. Of 507 practices contributing data in the three year period, 60 (11.8%) had SCRs which fell outside the 95% control limits of the funnel plot, whereas only 25 practices would be expected to by chance (Fig 3). Ten of 60 of the outlier practices had rates above the 95% control limit (17%) and 50 below.
Fig 3. Funnel plot of standardised ILI consultation ratios (SCRs) by practice, 2010/11-2012/13*.
*SCRs are adjusted for age group, sex, Townsend quintile and winter season.
Discussion
ILI consultation rates in UK primary care declined during the late 1990s and early 2000s, leading to a halving of consultation rates during the study period. In contrast, recording of less specific symptoms of respiratory tract infections increased by 40% during the same period. The decline in ILI consultation rates was observed across all age groups. Women aged between 15 and 75 years were more likely than men to have an ILI consultation recorded, and older children and adults had the highest ILI consultation rates. We also identified substantial between-practice variation in ILI consultation rates.
Strength and limitations
This was a large study of over seven million individuals, demographically representative of the UK population, across 18 winters. The large study size and long period of data collection allowed examination of consultation rates according to population subgroups, between practices and over time.
THIN is a database collected for clinical management, not research. This leads to some limitations. THIN only covers individuals who present to their GP. However a substantial proportion of people with ILI do not consult their GP,[11] therefore the ILI burden seen and recorded in primary care is an underestimate of the true population burden. We used the Townsend score, a small-area level indicator of deprivation, and not an individual level measure of a person’s socio-economic circumstances. This could result in misclassification of an individual’s deprivation status, in turn leading the observed association between deprivation level and ILI consultation rates to be underestimated.
Interpretation
There are few studies of temporal trends in ILI consultations in the UK, and no repeated community or seroprevalence studies of influenza covering the whole study period. Declining ILI consultation rates have been observed in a sentinel surveillance network in England between 1966 and 2006, including during the late 1990s, but the magnitude of the decline was not reported, with no age-specific analyses.[16] Contemporary surveillance reports noted a reduction in influenza activity in England and Wales in the early 2000s compared to the late 1990s based on both primary care surveillance and laboratory data. [40] Declines in ILI consultation rates during the 1990s and 2000s have also been observed in primary care or outpatient settings in the Netherlands,[14] New Zealand [13] and Taiwan.[41]
Since not only influenza causes ILI, factors unrelated to influenza activity are also likely to contribute to the observed decline in ILI consultations. One likely explanation for the reduction in ILI consultation rates is changes coding by GPs, in favour of less specific codes. This is supported by our finding of a concurrent 40% increase in coding of cough or fever symptoms, indicating that it is not the propensity to consult GPs with common symptoms of respiratory tract infections which are driving the trends. Universal influenza vaccination for individuals aged 65 years and over was introduced in the UK in 2000.[42] It is possible that the introduction of influenza vaccine could lead GPs to be more reluctant to use codes specifically mentioning influenza and (such as the codes for ‘influenza-like’ or ‘flu-like’ illness) in vaccinated individuals. However, since declines in ILI consultation rates were observed in all age groups, with the main decline observed during the late 1990s, this is an unlikely explanation of our findings.
An increase in the use of non-specific codes in primary care databases has also been observed for certain chronic conditions.[43] In addition, UK public health information campaigns since the late 1990s encouraged self-management of symptoms of respiratory tract infections in order to reduce antibiotic prescribing.[44] An increase in the use of codes for less specific respiratory tract infections and ill-defined symptoms in children have been linked to GPs’ decision making regarding whether to describe antibiotics for symptoms of likely viral origin.[45]
We observed large between-practice differences in ILI coded consultation rates, most likely reflecting differences in GP recording preferences in the absence of standard diagnostic criteria for ILI. Local variation in the propensity to consult primary care or variation in local population infection rates may also contribute to the observed variation. More detailed data on practice locations and their proximity are required to determine the potential role of local outbreaks of respiratory infection in driving these differences.
Only a very minor proportion of registered individuals have an ILI recorded in their GP records during a winter season. This is to be expected from a recent community study, where even among confirmed, symptomatic influenza cases, only 21% consult their GP.[11] Apart from the 2009/10 pandemic, the highest ILI recorded consultation rates were observed in adults. This finding was also reported by Meier et al for UK primary care [17], but in New Zealand [13] and the Netherlands [14] ILI consultation rates were highest in children. Lower ILI consultation rates in children than adults are in contrast to community and seroepidemiological studies of influenza, in which children tend to have the highest infection rates.[11, 46, 47] Similarly, studies estimating the impact of influenza on hospital admissions in a number of countries have found the highest impact among young children as well as older adults.[48, 49] This discrepancy reflects differences in GPs’ willingness to assign specific ILI codes in young children with respiratory symptoms in whom competing diagnoses are harder to rule out. In contrast clear diagnostic guidelines had been issued during the 2009/10 pandemic; this is also when ILI consultation rates were highest among children. The reluctance to code ILI in children could lead to an underestimate of the burden of ILI, and therefore also the severity of influenza epidemics in children. A qualitative or questionnaire study examining why GPs decide to enter a specific ILI code in the absence of standard diagnostic criteria is required to understand these differences by age group.
Women were more likely to have an ILI diagnosis recorded than men among older children and adults. A higher ILI consultation rate in women than men has also been reported in a previous study.[15] In the UK, adult women are more likely to present to primary care than men. [50] However, women were also more likely to report ILI symptoms in an internet based community survey, even after adjusting for contact with children, suggesting other contributing factors including sex-based immunological differences. [51]
Rates of recorded ILI in primary care have declined in all age groups in the UK since 1995, whilst recording of less specific symptoms, cough or fever, has increased. The age pattern of ILI recorded in primary care differs from the age pattern of ILI and influenza observed in community settings in the UK. Our results suggest that differences in GP coding habits may explain these results. Policy makers and researchers need to be aware of the importance of GP coding behaviour. Observed differences in ILI consultations rates in electronic primary care records over time and between groups may not reflect true variability in the severity of influenza epidemics in the population.
Supporting Information
Prediction is for men in the least deprived Townsend quintile.
(TIF)
(TIF)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Data Availability
Please note that the data are not freely available and some access restrictions will apply. THIN data were purchased from IMS Health (previously CSD Medical Research, see: http://www.epic-uk.org/) by UCL for use in public health research. The data are under license which prevents UCL from distributing the data to third parties. The data can be obtained by contacting IMS Health by phone at +44(0) 20 7388 8215 or email on hbhullar@uk.imshealth.com.
Funding Statement
PH is funded by a National Institute for Health Research postdoctoral fellowship (number PDF-2013-06-004). This article represents independent research funded by the National Institute for Health Research (NIHR). The views expressed are those of the authors and not those of the NHS, the NIHR or the Department of Health. RG and PH are members of the Farr Institute of Health Informatics Research London. The funders had no role in study design, collection, analysis, interpretation of data, or writing of the report.
References
- 1. Nicholson KG, Wood JM, Zambon M. Influenza. Lancet. 2003;362(9397):1733–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Storms AD, Van Kerkhove MD, Azziz-Baumgartner E, Lee WK, Widdowson MA, Ferguson NM, et al. Worldwide transmission and seasonal variation of pandemic influenza A(H1N1)2009 virus activity during the 2009–2010 pandemic. Influenza Other Respir Viruses. 2013;7(6):1328–35. Epub 2013/04/05. 10.1111/irv.12106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Zhou H, Thompson WW, Viboud CG, Ringholz CM, Cheng PY, Steiner C, et al. Hospitalizations associated with influenza and respiratory syncytial virus in the United States, 1993–2008. Clin Infect Dis. 2012;54(10):1427–36. Epub 2012/04/13. 10.1093/cid/cis211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hardelid P, Pebody R, Andrews N. Mortality caused by influenza and respiratory syncytial virus by age group in England and Wales 1999–2010. Influenza Other Respir Viruses. 2013;7(1):35–45. Epub 2012/03/13. 10.1111/j.1750-2659.2012.00345.x . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Green HK, Charlett A, Moran-Gilad J, Fleming D, Durnall H, Thomas DR, et al. Harmonizing influenza primary-care surveillance in the United Kingdom: piloting two methods to assess the timing and intensity of the seasonal epidemic across several general practice-based surveillance schemes. Epidemiol Infect. 2014:1–12. Epub 2014/07/16. 10.1017/S0950268814001757 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Harcourt SE, Smith GE, Elliot AJ, Pebody R, Charlett A, Ibbotson S, et al. Use of a large general practice syndromic surveillance system to monitor the progress of the influenza A(H1N1) pandemic 2009 in the UK. Epidemiol Infect. 2012;140(1):100–5. Epub 2011/04/09. 10.1017/S095026881100046X . [DOI] [PubMed] [Google Scholar]
- 7.European Centre for Disease Prevention and Control. Influenza case definitions 2014. Available: http://ecdc.europa.eu/en/activities/surveillance/eisn/surveillance/pages/influenza_case_definitions.aspx. Accessed 14 May 2014.
- 8. Hirve S, Chadha M, Lele P, Lafond KE, Deoshatwar A, Sambhudas S, et al. Performance of case definitions used for influenza surveillance among hospitalized patients in a rural area of India. Bull World Health Organ. 2012;90(11):804–12. Epub 2012/12/12. 10.2471/BLT.12.108837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dierig A, Heron LG, Lambert SB, Yin JK, Leask J, Chow MY, et al. Epidemiology of respiratory viral infections in children enrolled in a study of influenza vaccine effectiveness. Influenza Other Respir Viruses. 2014;8(3):293–301. Epub 2014/02/04. 10.1111/irv.12229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Falchi A, Turbelin C, Andreoletti L, Arena C, Blanchon T, Bonmarin I, et al. Nationwide surveillance of 18 respiratory viruses in patients with influenza-like illnesses: a pilot feasibility study in the French Sentinel Network. J Med Virol. 2011;83(8):1451–7. Epub 2011/06/04. 10.1002/jmv.22113 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hayward AC, Fragaszy EB, Bermingham A, Wang L, Copas A, Edmunds WJ, et al. Comparative community burden and severity of seasonal and pandemic influenza: results of the Flu Watch cohort study. Lancet Respir Med. 2014. 10.1016/S2213-2600(14)70034-7 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Department of Health. The Use of antivirals in an influenza pandemic: Scientific Evidence Based Review. 2014 Available: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/316206/Use_of_antivirals_Evidence_Review.pdf
- 13. Sue Huang Q, Lopez L, McCallum L, Adlam B. Influenza surveillance and immunisation in New Zealand, 1997–2006. Influenza and Other Respiratory Viruses. 2008;2(4):139–45. 10.1111/j.1750-2659.2008.00050.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Dijkstra F, Donker GA, Wilbrink B, Van Gageldonk-Lafeber AB, Van Der Sande MAB. Long time trends in influenza-like illness and associated determinants in The Netherlands. Epidemiology & Infection. 2009;137(04):473–9. 10.1017/S095026880800126X [DOI] [PubMed] [Google Scholar]
- 15. Ross AM, Kai J, Salter R, Ross J, Fleming DM. Presentation with influenza-like illness in general practice: implications for use of neuraminidase inhibitors. Commun Dis Public Health. 2000;3(4):256–60. Epub 2001/03/31. . [PubMed] [Google Scholar]
- 16. Elliot AJ, Fleming DM. Surveillance of influenza-like illness in England and Wales during 1966–2006. Euro Surveill. 2006;11(10):249–50. Epub 2006/11/30. . [PubMed] [Google Scholar]
- 17. Meier CR, Napalkov PN, Wegmuller Y, Jefferson T, Jick H. Population-based study on incidence, risk factors, clinical complications and drug utilisation associated with influenza in the United Kingdom. Eur J Clin Microbiol Infect Dis. 2000;19(11):834–42. Epub 2001/01/11. . [DOI] [PubMed] [Google Scholar]
- 18. Lis Y, Mann RD. The VAMP Research multi-purpose database in the U.K. J Clin Epidemiol. 1995;48(3):431–43. Epub 1995/03/01. . [DOI] [PubMed] [Google Scholar]
- 19.CSD Medical Research. The Health Improvement Network 2014. Available: http://csdmruk.cegedim.com/our-data/our-data.shtml. Accessed 16 April 2014.
- 20. Bourke A, Dattani H, Robinson M. Feasibility study and methodology to create a quality-evaluated database of primary care data. Inform Prim Care. 2004;12(3):171–7. Epub 2004/12/21. . [DOI] [PubMed] [Google Scholar]
- 21. Blak BT, Thompson M, Dattani H, Bourke A. Generalisability of The Health Improvement Network (THIN) database: demographics, chronic disease prevalence and mortality rates. Inform Prim Care. 2011;19(4):251–5. Epub 2011/01/01. . [DOI] [PubMed] [Google Scholar]
- 22. Benson T. The history of the Read Codes: the inaugural James Read Memorial Lecture 2011. Inform Prim Care. 2011;19(3):173–82. Epub 2012/06/13. . [DOI] [PubMed] [Google Scholar]
- 23. Herrett E, Thomas SL, Schoonen WM, Smeeth L, Hall AJ. Validation and validity of diagnoses in the General Practice Research Database: a systematic review. Br J Clin Pharmacol. 2010;69(1):4–14. Epub 2010/01/19. 10.1111/j.1365-2125.2009.03537.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Khan NF, Harrison SE, Rose PW. Validity of diagnostic coding within the General Practice Research Database: a systematic review. Br J Gen Pract. 2010;60(572):e128–36. Epub 2010/03/06. 10.3399/bjgp10X483562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Joint Formulary Committee. British National Formulary 66. London: BMJ Group; 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Rutter PD, Mytton OT, Mak M, Donaldson LJ. Socio-economic disparities in mortality due to pandemic influenza in England. Int J Public Health. 2012;57(4):745–50. Epub 2012/02/03. 10.1007/s00038-012-0337-1 . [DOI] [PubMed] [Google Scholar]
- 27. Mayoral JM, Alonso J, Garin O, Herrador Z, Astray J, Baricot M, et al. Social factors related to the clinical severity of influenza cases in Spain during the A (H1N1) 2009 virus pandemic. BMC Public Health. 2013;13(1):118 Epub 2013/02/09. 10.1186/1471-2458-13-118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Millett ER, Quint JK, Smeeth L, Daniel RM, Thomas SL. Incidence of community-acquired lower respiratory tract infections and pneumonia among older adults in the United Kingdom: a population-based study. PLOS One. 2013;8(9):e75131 Epub 2013/09/17. 10.1371/journal.pone.0075131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Maguire A, Blak BT, Thompson M. The importance of defining periods of complete mortality reporting for research using automated data from primary care. Pharmacoepidemiol Drug Saf. 2009;18(1):76–83. Epub 2008/12/10. 10.1002/pds.1688 . [DOI] [PubMed] [Google Scholar]
- 30. Horsfall L, Walters K, Petersen I. Identifying periods of acceptable computer usage in primary care research databases. Pharmacoepidemiol Drug Saf. 2013;22(1):64–9. Epub 2012/11/06. 10.1002/pds.3368 . [DOI] [PubMed] [Google Scholar]
- 31.Public Health England. Surveillance of influenza and other respiratory viruses, including novel respiratory viruses, in the United Kingdom: winter 2012/2013. 2013 Available: http://www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1317139321787
- 32. Dave S, Petersen I. Creating medical and drug code lists to identify cases in primary care databases. Pharmacoepidemiol Drug Saf. 2009;18(8):704–7. Epub 2009/05/21. 10.1002/pds.1770 . [DOI] [PubMed] [Google Scholar]
- 33. Frank AL, Taber LH, Wells JM. Individuals infected with two subtypes of influenza A virus in the same season. J Infect Dis. 1983;147(1):120–4. Epub 1983/01/01. . [DOI] [PubMed] [Google Scholar]
- 34. Molbak K, Espenhain L, Nielsen J, Tersago K, Bossuyt N, Denissov G, et al. Excess mortality among the elderly in European countries, December 2014 to February 2015. Euro Surveill. 2015;20(11):pii: 21065. Epub 2015/03/27. . [DOI] [PubMed] [Google Scholar]
- 35. Zhao H, Green H, Lackenby A, Donati M, Ellis J, Thompson C, et al. A new laboratory-based surveillance system (Respiratory DataMart System) for influenza and other respiratory viruses in England: results and experience from 2009 to 2012. Euro Surveill. 2014;19(3): pii: 20680. Epub 2014/02/01. . [DOI] [PubMed] [Google Scholar]
- 36.Royal College of General Practitioners Research Surveillance Centre. Weekly Returns Service Annual Report 2010. Available: http://www.rcgp.org.uk/pdf/ANNUAL%20REPORT%202010%20FINAL.pdf
- 37. Harrell FE. Regression Modeling Strategies: With Applications to Linear Models, Logistic Regression, and Survival Analysis. New York: Springer; 2001. [Google Scholar]
- 38. Spiegelhalter DJ. Funnel plots for comparing institutional performance. Stat Med. 2005;24(8):1185–202. Epub 2004/11/30. 10.1002/sim.1970 . [DOI] [PubMed] [Google Scholar]
- 39.StataCorp. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP.; 2013.
- 40. Goddard NL, Joseph CA, Watson JM, Ellis JS, Zambon MC. Three years of low influenza activity—no reason for complacency. Commun Dis Public Health. 2003;6(2):128–32. Epub 2003/08/02. . [PubMed] [Google Scholar]
- 41. Lian I-B, Wu H-DI, Chang W-T, Chao D-Y. The Temporal Trend of Influenza-Associated Morbidity and the Impact of Early Appearance of Antigenic Drifted Strains in a Southeast Asian Country. PLOS ONE. 2014;9(1):e84239 10.1371/journal.pone.0084239 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Salisbury D, Ramsay M, Noakes K. Immunisation against Infectious Disease: The Green Book. London: The Stationery Office; 2006. [Google Scholar]
- 43. Rait G, Walters K, Griffin M, Buszewicz M, Petersen I, Nazareth I. Recent trends in the incidence of recorded depression in primary care. Br J Psychiatry. 2009;195(6):520–4. Epub 2009/12/02. 10.1192/bjp.bp.108.058636 . [DOI] [PubMed] [Google Scholar]
- 44. McNulty C, Joshi P, Butler CC, Atkinson L, Nichols T, Hogan A, et al. Have the public's expectations for antibiotics for acute uncomplicated respiratory tract infections changed since the H1N1 influenza pandemic? A qualitative interview and quantitative questionnaire study. BMJ Open. 2012;2(2). 10.1136/bmjopen-2011-000674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Thompson PL, Spyridis N, Sharland M, Gilbert RE, Saxena S, Long PF, et al. Changes in clinical indications for community antibiotic prescribing for children in the UK from 1996 to 2006: will the new NICE prescribing guidance on upper respiratory tract infections just be ignored? Arch Dis Child. 2009;94(5):337–40. Epub 2008/12/11. 10.1136/adc.2008.147579 . [DOI] [PubMed] [Google Scholar]
- 46. Monto AS, Koopman JS, Longini IM. Tecumseh Study of Illness. XIII. Influenza Infection and Disease, 1976–1981. Am J of Epidemiol. 1985;121(6):811–22. [DOI] [PubMed] [Google Scholar]
- 47. Hoschler K, Thompson C, Andrews N, Galiano M, Pebody R, Ellis J, et al. Seroprevalence of influenza A(H1N1)pdm09 virus antibody, England, 2010 and 2011. Emerg Infect Dis. 2012;18(11):1894–7. Epub 2012/10/25. 10.3201/eid1811.120720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Thompson WW, Shay DK, Weintraub E, Brammer L, Bridges CB, Cox NJ, et al. Influenza-associated hospitalizations in the United States. JAMA. 2004;292(11):1333–40. Epub 2004/09/16. 10.1001/jama.292.11.1333 . [DOI] [PubMed] [Google Scholar]
- 49. Khieu TQ, Pierse N, Barnard LF, Huang QS, Baker MG. Estimating the contribution of influenza to hospitalisations in New Zealand from 1994 to 2008. Vaccine. 2015. Epub 2015/07/06. 10.1016/j.vaccine.2015.06.080 . [DOI] [PubMed] [Google Scholar]
- 50. Wang Y, Hunt K, Nazareth I, Freemantle N, Petersen I. Do men consult less than women? An analysis of routinely collected UK general practice data. BMJ Open. 2013;3(8):e003320 Epub 2013/08/21. 10.1136/bmjopen-2013-003320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Adler AJ, Eames KT, Funk S, Edmunds WJ. Incidence and risk factors for influenza-like-illness in the UK: online surveillance using Flusurvey. BMC Infect Dis. 2014;14:232 Epub 2014/06/03. 10.1186/1471-2334-14-232 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Prediction is for men in the least deprived Townsend quintile.
(TIF)
(TIF)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
Please note that the data are not freely available and some access restrictions will apply. THIN data were purchased from IMS Health (previously CSD Medical Research, see: http://www.epic-uk.org/) by UCL for use in public health research. The data are under license which prevents UCL from distributing the data to third parties. The data can be obtained by contacting IMS Health by phone at +44(0) 20 7388 8215 or email on hbhullar@uk.imshealth.com.