Abstract
Background
Opioids are the most frequently used drugs to treat pain in cancer patients. In some patients, however, opioids can cause adverse effects and drug–drug interactions. No advice concerning the combination of opioids and other drugs is given in the current European guidelines.
Objective
To identify studies that report clinically significant drug–drug interactions involving opioids used for pain treatment in adult cancer patients.
Design and data sources
Systematic review with searches in Embase, MEDLINE, and Cochrane Central Register of Controlled Trials from the start of the databases (Embase from 1980) through January 2014. In addition, reference lists of relevant full-text papers were hand-searched.
Results
Of 901 retrieved papers, 112 were considered as potentially eligible. After full-text reading, 17 were included in the final analysis, together with 15 papers identified through hand-searching of reference lists. All of the 32 included publications were case reports or case series. Clinical manifestations of drug–drug interactions involving opioids were grouped as follows: 1) sedation and respiratory depression, 2) other central nervous system symptoms, 3) impairment of pain control and/or opioid withdrawal, and 4) other symptoms. The most common mechanisms eliciting drug–drug interactions were alteration of opioid metabolism by inhibiting the activity of cytochrome P450 3A4 and pharmacodynamic interactions due to the combined effect on opioid, dopaminergic, cholinergic, and serotonergic activity in the central nervous system.
Conclusion
Evidence for drug–drug interactions associated with opioids used for pain treatment in cancer patients is very limited. Still, the cases identified in this systematic review give some important suggestions for clinical practice. Physicians prescribing opioids should recognize the risk of drug–drug interactions and if possible avoid polypharmacy.
Keywords: opioids, pain, cancer patients, drug–drug interactions
Introduction
Opioid analgesics are the most frequently used drugs to treat pain in patients with cancer.1 In some patients, however, opioids cause adverse effects.2 The most frequent adverse effects in cancer patients treated for pain with opioids are sedation, nausea/vomiting, and constipation, but other infrequent adverse effects, such as myoclonus, hallucination, and respiratory depression, are also feared.1–3 Adverse drug reactions from opioids are most often caused by the opioid itself, but can also be a result of the combination of the opioid and another drug, a drug–drug interaction (DDI).4 The risk of DDIs is high in cancer patients because of the large number of concomitant drugs.5
DDIs can be categorized as pharmacokinetic, that is, one drug influences the pharmacokinetic properties – absorption, distribution, metabolism, or excretion – of another drug. DDIs can also be pharmacodynamic, when the effects of two drugs either potentiate or antagonize each other.6
DDIs are reported to lead to serious adverse drug reactions in patients treated with opioids for pain.7,8 Still, no advice concerning the combination of opioids and other drugs is given in the current guidelines.2 Some studies have assessed the number of potentially harmful drug combinations in cancer pain patients, but do not report the number of clinically observed adverse drug reactions actually resulting from such combinations.5,9 Thus, the real risk of clinically important DDIs related to opioid therapy in cancer patients is not established.
The lack of advice on drug combinations in current guidelines may be a result of this limited clinical information. Therefore, a systematic review of the literature is indicated to identify studies that report clinically relevant DDIs associated with opioid analgesics used for the treatment of pain in patients with cancer.
Methods
Search strategy
Systematic searches were performed in Embase and MEDLINE through OvidSP and in the Cochrane Central Register of Controlled Trials, from set up of the databases (Embase from 1980) through January 2014. The last day searched was March 14, 2014. The full search string for Embase is presented in Table 1. Titles and abstracts of the retrieved citations were reviewed independently by two of the researchers (DFH, AKL), and potentially relevant papers were read in full text (DFH, AKL). In cases of doubt or disagreement, papers were reassessed by all three investigators (DFH, AKL, PK).
Table 1.
Search strategy
| Search strategy in Embase for drug–drug interactions (DDIs) involving opioid analgesics used for pain treatment in cancer patients (#1 or #2 or #3) |
|---|
| #1 (exp opiate agonist/it or exp narcotic analgesic agent/it or exp narcotic agent/it or exp morphine derivative/it) and exp neoplasm/ |
| #2 (exp opiate agonist/or exp narcotic analgesic agent/or exp narcotic agent/or exp morphine derivative/) and exp neoplasm/and (drug interaction/or drug antagonism/or drug competition/or drug inhibition/or drug potentiation/) and (exp pain/or analgesia/or analgesic activity/or pain relief/) |
| #3 (exp opiate agonist/or exp narcotic analgesic agent/or exp narcotic agent/or exp morphine derivative/) and exp neoplasm/and polypharmacy/ |
Additionally, reference lists of all the papers read in full text were hand-searched for relevant papers.
Inclusion criteria
– Publications reporting clinically significant DDIs involving WHO step II or step III opioids, as assessed by the authors.
– The DDI observed in one or more adult patients with a diagnosis of malignant disease and treated with an opioid for pain.
– Any type of publication: randomized controlled trial, other controlled study, observational study, case report, case series, or letter to the Editor, except for publications available only in abstract form.
– Publications in English language.
Exclusion criteria
– Experimental studies.
– Nonhuman studies.
– Only pharmacokinetic investigations (no clinical outcome).
– Studies in noncancer patients.
– Opioids used for indications other than pain or perioperatively.
– Duplicate publications.
Content analysis
The identified publications were grouped according to clinical presentation and probable underlying mechanism of the DDI. The DDIs and underlying mechanisms were presented as assessed and interpreted by the authors in each publication.
Results
Systematic review of the literature
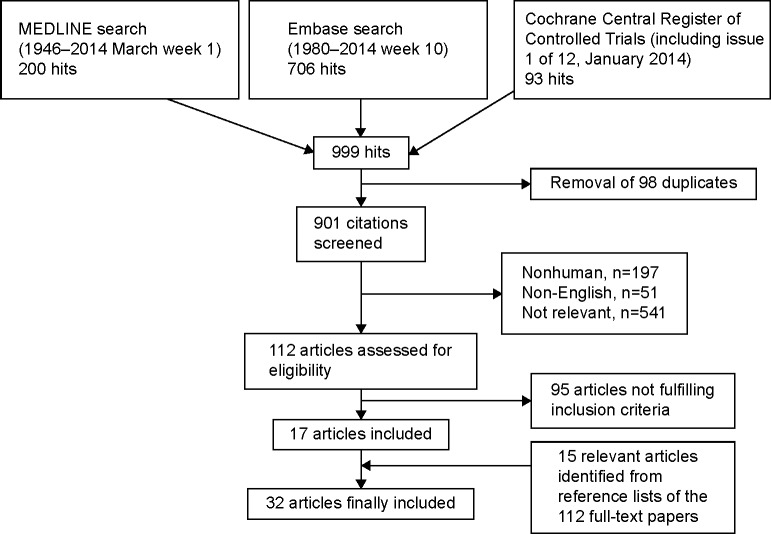
After removal of duplicates, 901 papers were retrieved (Figure 1). A total of 112 of these papers were considered potentially eligible for inclusion. After reading the full-text papers, 17 publications were included in the final analysis. In addition, 15 relevant papers were identified through hand-searching the reference lists of the articles read in full text, adding up to a total number of 32 included publications (Table 2).10–41 Additionally, two papers that commented on two of the included publications were identified,42,43 but not included as cases in the review.
Figure 1.
PRISMA flow chart showing the selection of papers.
Table 2.
Overview of included publications reporting drug–drug interactions (DDIs) involving opioids used for pain treatment in cancer patients
| Author (year) | Study design (number of patients) | Patients | Primary treatment (dose, route of administration) | Coadministered drug (dose, route of administration) | Clinical presentation | Underlying mechanism as proposed by the authors | Additional information provided by the authors of the included papers and the present review |
|---|---|---|---|---|---|---|---|
| Tramadol | |||||||
| Huang et al10 (2007) | Case report | 39-year-old woman with lymphoma | IV tramadol (150 mg/day) | Pethidine (25 mg injection) | Confusion with agitation and visual hallucinations 2 hours after pethidine injection, followed by catatonia with mutism and immobile standing, for 2 days | Anticholinergic and serotonergic effects; imbalance between cholinergic and dopaminergic systems in the CNS | Other drugs (pantoprazole, cyclophosphamide, prednisolone) could have contributed to the symptoms |
| Dextropropoxyphene/propoxyphene | |||||||
| Yu et al11 (1986) | Case series (one patient) | 69-year-old woman with myelofibrosis | Carbamazepine (600 mg/day) | Dextro-propoxyphene (32 mg q4h) | Drowsiness progressing to coma on the fifth day of the co-treatment | Inhibition of carbamazepine metabolism | Two other cases of patients with nonmalignant diseases are also reported |
| Oles et al12 (1989) | Case series (two patients) | Two patients; 60-year-old man and 23-year-old woman with brain tumors | Carbamazepine (~9–23 mg/kg/day) | Propoxyphene | Lightheadedness, blurred vision, double/triple vision, ataxia, nausea and vomiting after 2–3 days of co-treatment | Inhibition of carbamazepine metabolism (CYP450) | Six other cases of patients with nonmalignant diseases are also reported |
| Tapentadol | |||||||
| Sanders13 (2013) | Case report | 58-year-old woman with endometrial carcinoma | PO clonidine (400 mg/day) | PO tapentadol (50 mg per dose) | Blood pressure increase within 24 hours after tapentadol initiation. Similar episode 2 hours after tapentadol was resumed | Inhibition of norepinephrine reuptake | |
| Morphine | |||||||
| Potter et al14 (1989) | Case series (seven patients) | Nineteen patients; ten men and nine women aged 34–75; with malignant disease, and high dose of morphine or morphine-related side effects | PO morphine (120–1,200 mg/day), SC morphine (210–800 mg/day) | Antidepressants (TCA), antipsychotics (phenothiazines and haloperidol), antiemetics, NSAIDs | Side effects in 13 of the 19 patients (myoclonus in 12, and hyperalgesia in 1). Antidepressants and antipsychotics were used only in patients with side effects (7/13). A greater proportion of patients with side effects used thiethylperazine and NSAIDs | Antagonistic effect on dopamine receptors (phenothiazines); inhibition of catecholamines release (NSAIDs); promotion of proconvulsant properties of opioids | Abnormal concentrations of electrolytes in some patients could have contributed to the symptoms |
| Smith and Guly15 (2004) | Case report | 60-year-old woman with metastatic renal cell carcinoma | SR morphine (90 mg q12h) | IV nalbuphine (30 mg) | Symptoms of opioid withdrawal, resistance to additional doses of intravenous morphine | Antagonistic effect on mu opioid receptors | |
| Hartree16 (2005) | Case series (one patient) | 49-year-old man with metastatic prostate cancer | SR morphine (360 mg q12h) | IM nalbuphine (10 mg) | Increased pain and symptoms of opioid withdrawal | Antagonistic effect on mu opioid receptors | Another patient (treated with methadone and nalbuphine) is reported below |
| Ripamonti et al17 (1998) | Case series (three patients) | Three patients; one man and two women aged 20–58; with sarcomas and cervical carcinoma | PO, SC, spinal morphine (in increasing doses; 20–2,000 mg MEDD) | SC or IV somatostatin (3 mg) | Increased pain, difficulty in controlling pain | Opioid antagonistic properties of somatostatin | One patient initially on oral methadone with poor analgesic effect, switched to morphine |
| Piquet et al18 (1998) | Case series (one patient) | 72-year-old man with metastatic bladder carcinoma | IT morphine (10 mg) | IT bupivacaine (7.5 mg) with epinephrine | Coma and respiratory depression 10 minutes after IT injection of morphine and bupivacaine (morphine was resumed in the same dose after 4 days) | Inhibition of the stimulating effect of pain on respiration | A case of a patient with nonmalignant disease is also reported |
| Upadhyay et al19 (2008) | Case report | 80-year-old man with metastatic lung cancer | PO morphine (dose increased from 15 mg to 30 mg q4h) | PO amitriptyline (dose increased from 25 mg/day to 50 mg/day), ranitidine (300 mg/day) | Deep and prolonged sedation, not responding to painful stimuli with respiratory rate eight per minute during titration rate of the analgesic dose | Sedating effect of amitriptyline; inhibition of morphine metabolism (amitryptyline and ranitidine) | Patient with hypoalbuminemia |
| Martinez-Abad et al20 (1988) | Case report | 42-year-old man with cancer of the larynx | IV ranitidine (150 mg q8h) | IV morphine (50 mg/day) | Three episodes of confusion with agitation after three subsequent doses of ranitidine during morphine infusion | Mechanism not clear (according to the authors) | Inhibition of morphine metabolism by ranitidine has been demonstrated45,46 |
| Guo et al21 (2006) | Case report | 18-year-old woman with nasopharyngeal carcinoma | IM haloperidol (4 mg/day), IV morphine (up tô10 mg/h) and ED injection of morphine (2 mg) | IV naloxone (3 injections of 0.1–0.2 mg at 30-minute intervals) | Three episodes of extrapyramidal symptoms (restlessness, torticollis, oculogyric response) 5 minutes after each naloxone injection | Reversal of opioid-related protection from haloperidol-induced extrapyramidal side effects | |
| Bortolussi et al22 (1994) | Case series (four patients) | Four patients; three men and one woman aged 53–56; with metastatic renal cell carcinoma | SR morphine | IV recombinant interleukin-2 (rIL-2) | Coma and/or respiratory depression | Toxic synergy on CNS; accumulation of morphine metabolites due to acute renal failure (induced by rIL-2) | |
| Hydromorphone | |||||||
| Fainsinger et al23 (1993) | Case report | 85-year-old woman with breast cancer | PO hydromorphone (24 mg q4h, 12 mg prn) | Captopril (50 mg/day) | Confusion with agitation and hallucinations, after a few days of co-treatment | Accumulation of hydromorphone metabolites due to renal failure (induced by captopril) | |
| Oxycodone | |||||||
| Watanabe et al24 (2011) | Case series (seven patients) | Nine patients; two men and seven women aged 39–82; with maxillary tumor or hematologic malignancies | PO oxycodone (~0.2–2.0 mg/kg/day) | PO or IV voriconazole (~2.2–8.0 mg/kg/day) coadministered or discontinued | Adverse events (vomiting, drowsiness, hypopnea, delirium, sweating, hypotension, uncontrolled pain) in seven of nine patients; after 1–10 days of co-treatment | Inhibition of CYP3A4 | Commented in Hagelberg et al42 |
| Walter et al25 (2012) | Case report | 77-year-old woman with lung cancer | SR oxycodone (50 mg q12h), IR oxycodone (5 mg prn) | Citalopram (20 mg/day) | Tremor, weakness, inability to coordinate motor movements, confusion (serotonin syndrome). The symptoms resolved within 48 hours after oxycodone was changed to morphine | Hyperstimulation of central 5-HT1A and 2A receptors (citalopram); disinhibition of serotonergic neuronal activity by suppressing GABA-mediated inhibition (oxycodone) | The patient also used esomeprazole, which could have inhibited citalopram clearance |
| Rosebraugh et al26 (2001) | Case report | 34-year-old man with lymphoma | PO sertraline (50 mg/day) | PO oxycodone (200 mg over 48 hours) | Severe tremor and visual hallucinations (probable serotonin syndrome). The symptoms resolved within 12 hours after sertraline was stopped and cyproheptadine administered | Hyperstimulation of central 5-HT1A and 2A receptors (sertraline); disinhibition of neuronal activity by suppressing GABA-mediated inhibition (oxycodone) | |
| Fentanyl | |||||||
| Takane et al27 (2005) | Case report | 61-year-old man with parotid gland adenocarcinoma | TD fentanyl (dose increased from 2.5 mg to 7.5 mg; every 3 days) | PO rifampin (300 mg/day) | Severe pain after rifampin initiation. Patient continued to have pain despite three-fold increase in fentanyl dose | Induction of CYP3A4 | The ratio of serum fentanyl concentration/dose decreased to 20%–50% of baseline value |
| Morii et al28 (2007) | Case report | 64-year-old man with colon cancer | Rifampicin (450 mg/day) | TD fentanyl (dose increased from 0.6 mg/day to 2.5 mg/day) | Poor analgesia | Induction of CYP3A4 | |
| Mercadante et al29 (2002) | Case report | 67-year-old man with head and neck cancer | TD fentanyl (50 µg/h) | PO itraconazole (400 mg/day) | Agitated delirium with myoclonus 24 hours after starting itraconazole | Inhibition of CYP3A4 | Patient also used omeprazole and ibuprofen, which could have contributed to the event (by inhibition of fentanyl metabolism and renal excretion) |
| Hallberg et al30 (2006) | Case report | 46-year-old man with tonsillar cancer | TD fentanyl (150 µg/h) | PO fluconazole (50 mg/day) | Death after 3 days of co-treatment | Inhibition of CYP3A4 | Postmortem blood analysis showed toxic concentration of fentanyl. Patient used also other drugs that could have contributed to the event (morphine, oxazepam, zolpidem) |
| Levin et al31 (2010) | Case report | 85-year-old man with lung cancer | IV fentanyl (25 µg/h) | Diltiazem | Hypoactive delirium, somnolence, miosis after 3 days of coadministration | Inhibition of CYP3A4 | Patient with chronic renal insufficiency |
| Cronnolly and Pegrum32 (2012) | Case report | 72-year-old woman with metastatic breast cancer | TD fentanyl (87 µg/h) | PO clarithromycin (1 g/day) | Coma and respiratory depression 2 days after clarithromycin initiation | Inhibition of CYP3A4 | Patient with kidney disease on hemodialysis |
| Tsutsumi et al33 (2006) | Case report | 47-year-old woman with leukemia | TD fentanyl (25 µg/h), discontinued | Cyclosporine | Opioid withdrawal syndrome 1 day following fentanyl cessation. Symptoms disappeared after fentanyl was resumed | Inhibition of CYP3A4 | |
| Morita et al34 (2004) | Case report | 67-year-old man with esophageal cancer | IV fentanyl (500 µg/day) | IV haloperidol (2.5–7.5 mg/day) | Worsening of pre-existing delirium (days 3–6). On day 7 muscle rigidity, fever, severe diaphoresis, tachycardia, hypertension, tachypnea, and coma (neuroleptic malignant syndrome) | Antagonistic effect on dopamine receptors (haloperidol); modification of dopamine metabolism in the CNS (fentanyl) | Hypocalcemia, hypophosphatemia and hypomagnesemia in this patient could have contributed to the symptoms |
| Ailawadhi et al35 (2007) | Case report | 65-year-old woman with myeloproliferative disease | Citalopram | TD fentanyl (25 µg/h) | Confusion, agitation, tremors, hyperreflexia, myoclonus, unsteady gait, tachycardia (serotonin syndrome) within 24 hours of fentanyl initiation. The symptoms resolved within 24–36 hours after fentanyl was replaced by oxycodone | Overstimulation of serotonin receptors (citalopram); inhibition of serotonin reuptake and increase of serotonin release in the CNS (fentanyl) | |
| Buprenorphine | |||||||
| Moro et al36 (2006) | Case report | 34-year-old man with metastatic osteosarcoma | Ifosfamide (2 g/m2/day for 3 days) | TD buprenorphine (35–52.5 µg/h) | Confusion, miosis, respiratory depression and bradycardia within 36 hours of the co-treatment | Inhibition of CYP3A4 (due to saturation of the enzyme by ifosfamide) | Commented by Davis (best interpretation for the event was rapid increase in buprenorphine dose)43 |
| Methadone | |||||||
| Hartree16 (2005) | Case series (one patient) | 54-year-old man with rectal carcinoma | PO methadone (20 mg/day) | IM nalbuphine (10 mg) | Increased pain and symptoms of opioid withdrawal | Antagonistic effect on mu opioid receptors | Another patient (treated with morphine and nalbuphine) is reported above |
| Benítez-Rosario et al37 (2006) | Case report | 61-year-old woman with metastatic lung cancer | PO methadone (210 mg/day) | Carbamazepine (1,200 mg/day), discontinued | Loss of consciousness and respiratory depression eleven days after carbamazepine discontinuation | Disappearance of carbamazepine inducing effect on metabolizing enzymes | The dose of methadone was increased within a week before the incident |
| Tarumi et al38 (2002) | Case report | 60-year-old man with gastric cancer | PO methadone (45–75 mg/day) | IV fluconazole (100 mg/day) | Unresponsiveness and respiratory depression 4 days after fluconazole initiation | Inhibition of CYP3A4 and 2C9 | Patient also used omeprazole, which could have contributed to the accumulation of methadone (by inhibition of CYP2C19 and CYP3A4) |
| Sorkin and Ogawa39 (1983) | Case report | 76-year-old man with metastatic lung cancer | PO methadone (5 mg q8h), SC morphine (8 mg prn) | IV cimetidine (1.2 g/day) | Respiratory depression 6 days after cimetidine initiation, 3 h after the rescue dose of morphine | Inhibition of liver enzymes | Cimetidine is a weak CYP3A4 inhibitor44 |
| Elsayem and Bruera40 (2005) | Case report | 70-year-old man with gastric cancer | Methadone (10 mg q8h, 2 mg prn) | Sertraline (100 mg/day) | Coma and respiratory depression 3 days after sertraline dose was increased from 50 mg/day to 100 mg/day | Inhibition of CYP3A4 | Severely malnourished patient with a history of alcoholism |
| Walker et al41 (2003) | Case series (one patient) | 61-year-old woman with rectal cancer | PO methadone (600–700 mg/day) | Sertraline (50 mg/day), midazolam, IV fentanyl (prn) | Two episodes of ventricular tachycardia (torsades de pointes) | Interference with methadone metabolism (sertraline, midazolam, and fentanyl, substrates of CYP3A4); increase in methadone blood levels | High dose of methadone and preexisting cardiac disease in the patient Two other cases of patients with nonmalignant disease are also reported |
Abbreviations: PO, oral; IR, immediate release; SR, slow release; SC, subcutaneous; IV, intravenous; TD, transdermal; ED, epidural; IT, intrathecal; q4h, every four hours; q12h, every 12 hours; prn, as required; MEDD, morphine equivalent daily dose; NSAIDs, nonsteroidal anti-inflammatory drugs; TCA, tricyclic antidepressants; CNS, central nervous system; BP, blood pressure.
No randomized controlled trials or other controlled studies were found. All of the included publications were case reports or case series, reporting on 2–19 patients. Nine of the papers were published in the period 1983–2000, and 23 in the period 2001–January 2014 (Table 2). In some case series, DDIs in both cancer patients and patients with nonmalignant diseases were reported.11,12,18,41 From these case series, only cases of DDIs due to opioids in patients with a diagnosis of malignant disease treated for pain were included in the review.
Opioids involved in DDIs
The majority of included publications report DDIs related to opioids that are in common clinical use (Table 2):
– morphine, administered by various routes; oral, subcutaneous, intravenous, epidural, and intrathecal (nine publications),14–22
– fentanyl, transdermal, and intravenous (nine publications,27–35 of which seven described DDIs associated with transdermal preparations),
– tramadol combined with pethidine,10 tapentadol,13 hydromorphone,23 and buprenorphine36 was reported in one paper each.
Four publications report DDIs associated with opioids of minor current clinical relevance: propoxyphene, dextro-propoxyphene, and nalbuphine.11,12,15,16
Clinical presentation of DDIs
Eleven papers reported DDIs resulting in sedation and respiratory depression.18,19,22,24,30,32,36–40 Fifteen papers reported DDIs causing various other central nervous system (CNS) symptoms, including delirium,10,20,23–25,29,31,34–36 serotonin syndrome,25,26,35 myoclonus,14,29,35 hyperalgesia,14 extrapyramidal symptoms,21 catatonia,10 neuroleptic malignant syndrome,34 or carbamazepine toxicity.11,12 Seven papers reported DDIs causing impairment of pain control and/or opioid withdrawal.15–17,24,27,28,33 Finally, in three publications, other symptoms believed to be associated with opioid-related DDIs were reported: hypertension,13 hypotension,24 vomiting,24 sweating,24 ventricular tachycardia/torsades de pointes.41
Mechanisms underlying DDIs of opioids used for pain treatment in cancer patients
The mechanisms underlying DDIs involving opioid analgesics used for pain treatment in patients with cancer in the publications included in this review are presented in Table 3.
Table 3.
Mechanisms underlying DDIs involving opioid analgesics used for pain treatment in patients with cancer
| Mechanisms underlying DDIs of opioid analgesics |
|---|
| Pharmacokinetic DDIs |
| 1) Inhibition or induction of opioid metabolism through CYP450 or other metabolizing enzymes19,20,24,27–33,36–41 |
| 2) Decreased renal elimination of an opioid22,23 |
| 3) Inhibition of the metabolism of other drugs exerted by an opioid11,12 |
| Pharmacodynamic DDIs |
| 1) Potentiation of analgesic efficacy and toxicity through opioid and nonopioid mechanisms18,19 |
| 2) Inhibition or reversal of the effect of an opioid by antagonism at opioid receptors, or by other mechanisms15–17 |
| 3) Modification of cholinergic, adrenergic, dopaminergic, and serotoninergic activity in the CNS10,13,14,25,26,34,35 |
| Others (including DDIs with unknown mechanism)21 |
Abbreviations: CNS, central nervous system; DDI, drug–drug interactions.
Quality of evidence
The included studies have several limitations. Only case reports and case series were identified (Table 2). Most of the reports included in this review provide poor level of evidence. Some may also not represent true DDIs, but other opioid-related complications. However, we decided to include the reports as they were clinically evaluated and presented by the authors and published by the respective journals.
Discussion
Evidence for DDIs involving opioids used for pain treatment in cancer patients is very limited. This systematic review of publications on clinically significant DDIs involving opioid analgesics used for pain treatment in patients with cancer identified only case reports and case series (Table 2).10–41 As no systematic studies were identified, it was not possible to do any statistical analysis.
The three major categories of DDIs identified in the review were increased opioid effects causing sedation and respiratory depression, other CNS toxicities, and decreased opioid effects causing more pain and/or acute withdrawal symptoms. The lack of controlled studies precludes specific conclusions on the risk of DDIs associated with opioids. Still, based upon the reported cases, it can be concluded that physicians treating patients for cancer pain should be aware of and closely monitor patients for DDIs.
The DDIs with increased opioid efficacy, resulting in sedation and respiratory depression, were caused by decreased opioid metabolism,19,24,30,32,36–40 impaired renal excretion,22 or an additional therapy that also relieves pain and possesses sedative and respiratory depressant effect (eg, amitriptyline or intrathecal bupivacaine added to morphine)18,19 (Tables 2 and 3). Most examples identified in the review refer to opioids metabolized by cytochrome P450 (CYP450), and cytochrome P450 izoenzyme CYP3A4 (CYP3A4) in particular, such as fentanyl, methadone, oxycodone, or buprenorphine, either by concomitant use of CYP3A4 substrates and inhibitors (voriconazole, fluconazole, clarithromycin, cimetidine, and sertraline) or by discontinuation of a CYP3A4 inducer (carbamazepine) (Tables 2 and 4).24,30,32,36–40,44 Morphine pharmacokinetics were reported to be affected by a DDI leading to sedation and respiratory depression only in two case reports.19,22 In one of these publications, morphine was coadministered with amitriptyline and ranitidine,19 two drugs which can affect morphine glucuronidation45,46 (Table 2). Morphine may also indirectly be affected by renal failure caused by another drug.22 Additionally, other drugs with sedative effects can cause pharmacodynamic DDIs with an opioid. A typical observation in clinical practice is the combination of an opioid and a benzodiazepine, both contributing to sedation.
Table 4.
CYP3A4 enzyme inhibitors and inducers reported to have caused clinically significant drug–drug interactions with opioids metabolized by CYP3A4 (oxycodone, methadone, fentanyl) in papers included in the present review24,27–33,37–39,44
| Drugs | Effect on CYP3A4 activity | Resulting effects when coadministered with opioid | Resulting effects after withdrawal of interacting drug |
|---|---|---|---|
| CYP3A4 inhibitors | |||
| Voriconazole | Strong | ||
| Itraconazole | Strong | ||
| Fluconazole Clarithromycin Diltiazem |
Moderate Strong Moderate |
Decreased rate of opioid metabolism, increased opioid effect, increased risk of opioid toxicity | Increased opioid metabolism, decreased clinical effect of opioid |
| Cyclosporine | Weak | ||
| Cimetidine | Weak | ||
| CYP3A4 inducers | |||
| Rifampin Carbamazepine |
Strong Strong |
Increased metabolism of opioid, requirement for higher opioid doses, deterioration of pain control | Decreased rate of opioid metabolism, increased risk of opioid overdose |
CNS symptoms (other than sedation and respiratory depression) associated with opioids included hyperactive or hypoactive delirium with or without hallucinations, serotonin toxicity, myoclonus, hyperalgesia, extrapyramidal symptoms, catatonia, and neuroleptic malignant syndrome (Table 2). CNS symptoms were related both to decreased clearance of an opioid due to decreased metabolism20,24,29,31,36 or impaired renal elimination23 and to a variety of interactions influencing several biological systems in the CNS10,14,21,25,26,34,35 (Table 3). Additionally, two reports presented cases of carbamazepine neurotoxicity related to inhibition of its metabolism by propoxyphene and dextropropoxyphene, opioids with an inhibitory effect on cytochrome P450 enzymes (Table 2).11,12,47
DDIs involving opioids can cause acute exacerbations of pain, or withdrawal symptoms (Table 2). In the identified cases, these symptoms resulted from the addition of an opioid with a mixed agonist–antagonist effect (nalbuphine),15,16 and increased or decreased metabolism of an opioid due to the coadministration of a CYP3A4 inducer (rifampin)27,28 or inhibitor (cyclosporine)33 or cessation of CYP3A4 inhibition (voriconazole)24 (Table 3). Nalbuphine, which is an agonist at kappa opioid receptors and an antagonist at mu opioid receptors,48 reverses the analgesic effect of mu opioid agonists when used concomitantly.15,16 Rifampin is a potent inducer of metabolizing enzymes, including CYP3A4, and may enhance clearance and attenuate the clinical effects of opioids.27,28,49–53 The withdrawal syndrome reported after discontinuation of a low dose of transdermal fentanyl (25 µg/h) was attributed to increased blood concentration of fentanyl (and increased effect) due to coadministration of cyclosporine, a CYP3A4 inhibitor.33 Additionally, one case series described impaired pain control in three patients who were given somatostatin as part of their antineoplastic treatment.17 The exact mechanism for this DDI is not certain. The authors suggest opioid antagonistic effect of somatostatin, demonstrated in animal studies.17,54
Finally, some other important DDIs were identified (Table 2). Prolonged QT time and ventricular arrhythmias (torsades de pointes) were seen in a patient receiving a high dose of methadone, and at the same time, three drugs that were CYP3A4 substrates. The authors suggest that these coadministered drugs may have interfered with methadone metabolism and caused elevation of its level in the blood.41
Multiple complex mechanisms, often not fully understood, underlie DDIs involving opioid analgesics (Table 3). In this review, we refer to the mechanisms of DDIs as they were understood and presented by the authors. In some cases, alternative causes for the observed complications may be found.
The most frequently reported mechanism of DDIs was associated with cytochrome P450 enzyme activity. In our review, the implicated opioids were fentanyl, methadone, oxycodone, and buprenorphine.24,27–33,36–41 Of these, orally administered oxycodone and methadone have been shown to be more susceptible to DDIs related to CYP3A4 or other CYP enzymes in studies in volunteers,49,50,55–58 while fentanyl pharmacokinetics were less affected in volunteer studies.51,59–62 Still, DDIs of fentanyl associated with CYP3A4 activity were reported in seven publications identified by this review.27–33
Buprenorphine metabolism can be increased by strong CYP3A4 inducers as demonstrated in a study with rifampin,52 while the effect of CYP3A4 inhibitors is limited due to complex metabolism (conversion to norbuprenorphine by CYP3A4 and CYP2C8, and glucuronidation) as well as renal and extrarenal elimination of the parent drug and metabolites.50,63 As noted by Davis, the case report involving buprenorphine36 should probably be best interpreted as a result of rapid dose increase before time to maximum concentration or steady state was reached, and not a DDI.43
In our review, most drugs that precipitated serious CYP3A4-mediated DDIs (voriconazole, itraconazole, fluconazole, clarithromycin, diltiazem) are also drugs relevant for patients with advanced cancer, supporting the clinical importance of this finding. The vast majority of DDIs occur after a precipitating drug is introduced. The opposite effect of a decreased or increased opioid action may be caused if the use of a CYP3A4 inhibitor or inducer is stopped,24,37 thereby decreasing or increasing the serum concentration of the drug (Table 4). Defining a consequence of stopping a drug as an interaction, is perhaps counterintuitive, but it still represents symptoms related to a pharmacokinetic DDI. Interactions are less frequent if an opioid is introduced in a patient already using another drug. This may be related to titration of the opioid dose to obtain the desired clinical effect. Thus, a DDI may change the dose, but not the clinical outcome.
In cancer patients, the coexistence of other clinical factors can increase the risk of DDIs (Table 2). Impaired renal function is a common predisposing factor of DDIs31,32 and has added importance in cancer pain management because the incidence of renal impairment in patients with advanced cancer is high.64,65 Also, the concomitant use of other drugs and the frequent need to change coadministered drugs and their doses add to the complexity of DDIs of opioids in these patients.5,9
The presence of DDIs seems to be underreported. This lack of formal evidence may have several explanations. First, the DDI may not be detected, or the symptoms are believed to be caused by the cancer disease and, therefore, not recognized as drug related. Second, DDIs are mostly observed by clinicians, who often do not have the time, the experience, or the interest to publish clinical observations. Third, several DDIs, even if not reported in the literature, may be considered as frequent and part of common knowledge, and therefore, not reported. Finally, many journals only occasionally publish case reports and, perhaps, case reports are more often published in national journals and therefore not identified by a search strategy excluding non-English papers.
Conclusion
For obvious ethical reasons, there are no randomized controlled trials or other well-designed controlled studies exploring DDIs. Recommendations must therefore be based upon cases reporting serious adverse drug reactions and basic knowledge about drug mechanisms. The cases identified in this systematic review can give some suggestions for clinical practice:
The combined use of an opioid and another drug with CNS depressant effect (eg, amitriptyline) increases the risk of acute opioid toxicity and respiratory depression. Such drugs should be carefully titrated according to effect.
Opioids with antagonistic effects at the mu opioid receptor (eg, nalbuphine) should not be coadministered with another opioid analgesic.
The concomitant use of an opioid and a drug, which affects the activity of cholinergic, dopaminergic, and/or serotonergic systems in the CNS (eg, selective serotonin inhibitors), can cause CNS-related complications (eg, delirium and serotonin syndrome) and should, therefore, be monitored carefully.
Introduction of a CYP3A4 inhibitor in a patient treated with fentanyl, oxycodone, or methadone may result in opioid overdose and increased opioid toxicity (Table 4). Caution has to be undertaken when such drugs are implemented. The use of a major CYP450 inducer may impair pain treatment (Table 4). Opposite effects should be expected when these drugs are stopped (Table 4).
Finally, the physician should recognize the risk for DDIs of opioids, monitor the patients carefully for interactions, and if possible avoid polypharmacy.
Acknowledgments
This systematic review was performed as part of the work to update the European Association for Palliative Care Guidelines for Cancer Pain Management. We thank Ingrid Riphagen for help with electronic database searches.
Footnotes
Disclosure
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. The authors report no other conflicts of interest in this work.
References
- 1.World Health Organization . Cancer Pain Relief: With a Guide to Opioid Availability. 2nd ed. Geneva: WHO; 1996. [Google Scholar]
- 2.Caraceni A, Hanks G, Kaasa S, et al. European Palliative Care Research Collaborative (EPCRC) European Association for Palliative Care (EAPC) Use of opioid analgesics in the treatment of cancer pain: evidence-based recommendations from the EAPC. Lancet Oncol. 2012;13(2):e58–e68. doi: 10.1016/S1470-2045(12)70040-2. [DOI] [PubMed] [Google Scholar]
- 3.Laugsand EA, Kaasa S, Klepstad P. Management of opioid-induced nausea and vomiting in cancer patients: systematic review and evidence-based recommendations. Palliat Med. 2011;25(5):442–453. doi: 10.1177/0269216311404273. [DOI] [PubMed] [Google Scholar]
- 4.Bernard SA, Bruera E. Drug interactions in palliative care. J Clin Oncol. 2000;18(8):1780–1799. doi: 10.1200/JCO.2000.18.8.1780. [DOI] [PubMed] [Google Scholar]
- 5.Kotlinska-Lemieszek A, Paulsen Ø, Kaasa S, Klepstad P. Polypharmacy in patients with advanced cancer and pain: a European cross-sectional study of 2282 patients. J Pain Symptom Manage. 2014;48(6):1145–1159. doi: 10.1016/j.jpainsymman.2014.03.008. [DOI] [PubMed] [Google Scholar]
- 6.Osterhoudt KC, Pening TM. Drug toxicity and poisoning. In: Brunton LL, Chabner BA, Knollmann BC, editors. Goodman and Gilman’s the Pharmacological Basis of Therapeutics. 12th ed. New York: McGraw-Hill; 2010. pp. 73–88. [Google Scholar]
- 7.Butts M, Jatoi A. A systematic compilation of reports published on opioid-related problems. J Opioid Manag. 2011;7(1):35–45. doi: 10.5055/jom.2011.0047. [DOI] [PubMed] [Google Scholar]
- 8.Dahan A, Overdyk F, Smith T, Aarts L, Niesters M. Pharmacovigilance: a review of opioid-induced respiratory depression in chronic pain patients. Pain Physician. 2013;16(2):E85–E94. [PubMed] [Google Scholar]
- 9.Gaertner J, Ruberg K, Schlesiger G, Frechen S, Voltz R. Drug interactions in palliative care – it’s more than cytochrome P450. Palliat Med. 2012;26(6):813–825. doi: 10.1177/0269216311412231. [DOI] [PubMed] [Google Scholar]
- 10.Huang SS, Jou SH, Chiu NY. Catatonia associated with coadministration of tramadol and meperidine. J Formos Med Assoc. 2007;106(4):323–326. doi: 10.1016/s0929-6646(09)60260-6. [DOI] [PubMed] [Google Scholar]
- 11.Yu YL, Huang CY, Chin D, Woo E, Chang CM. Interaction between carbamazepine and dextropropoxyphene. Postgrad Med J. 1986;62(725):231–233. doi: 10.1136/pgmj.62.725.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oles KS, Mirza W, Penry JK. Catastrophic neurologic signs due to drug interaction: Tegretol and Darvon. Surg Neurol. 1989;32(2):144–151. doi: 10.1016/0090-3019(89)90203-6. [DOI] [PubMed] [Google Scholar]
- 13.Sanders P. Tapentadol analgesic interaction with clonidine. Pain Med. 2013;14(6):943–944. doi: 10.1111/pme.12134. [DOI] [PubMed] [Google Scholar]
- 14.Potter JM, Reid DB, Shaw RJ, Hackett P, Hickman PE. Myoclonus associated with treatment with high doses of morphine: the role of supplemental drugs. BMJ. 1989;299(6692):150–153. doi: 10.1136/bmj.299.6692.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smith J, Guly H. Nalbuphine and slow release morphine. BMJ. 2004;328(7453):1426. doi: 10.1136/bmj.328.7453.1426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hartree C. Caution with nalbuphine in patients on long-term opioids. Palliat Med. 2005;19(2):168. doi: 10.1177/026921630501900218. [DOI] [PubMed] [Google Scholar]
- 17.Ripamonti C, De Conno F, Boffi R, Ascani L, Bianchi M. Can somatostatin be administered in association with morphine in advanced cancer patients with pain? Ann Oncol. 1998;9(8):921–923. doi: 10.1023/a:1008416621421. [DOI] [PubMed] [Google Scholar]
- 18.Piquet CY, Mallaret MP, Lemoigne AH, Barjhoux CE, Danel VC, Vincent FH. Respiratory depression following administration of intrathecal bupivacaine to an opioid-dependent patient. Ann Pharmacother. 1998;32(6):653–655. doi: 10.1345/aph.17182. [DOI] [PubMed] [Google Scholar]
- 19.Upadhyay S, Jain R, Chauhan H, Gupta D, Mishra S, Bhatnagar S. Oral morphine overdose in a cancer patient antagonized by prolonged naloxone infusion. Am J Hosp Palliat Care. 2008;25(5):401–405. doi: 10.1177/1049909108319260. [DOI] [PubMed] [Google Scholar]
- 20.Martinez-Abad M, Delgado Gomis F, Ferrer JM, Morales-Olivas FJ. Ranitidine-induced confusion with concomitant morphine. Drug Intell Clin Pharm. 1988;22(11):914–915. doi: 10.1177/106002808802201124. [DOI] [PubMed] [Google Scholar]
- 21.Guo SL, Lin CJ, Huang HH, Chen LK, Sun WZ. Reversal of morphine with naloxone precipitates haloperidol-induced extrapyramidal side effects. J Pain Symptom Manage. 2006;31(5):391–392. doi: 10.1016/j.jpainsymman.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 22.Bortolussi R, Fabiani F, Savron F, et al. Acute morphine intoxication during high-dose recombinant interleukin-2 treatment for metastatic renal cell cancer. Eur J Cancer. 1994;30A(12):1905–1907. doi: 10.1016/0959-8049(94)00257-6. [DOI] [PubMed] [Google Scholar]
- 23.Fainsinger R, Schoeller T, Boiskin M, Bruera E. Palliative care round: cognitive failure and coma after renal failure in a patient receiving captopril and hydromorphone. J Palliat Care. 1993;9(1):53–55. [PubMed] [Google Scholar]
- 24.Watanabe M, Homma M, Momo K, et al. Effects of voriconazole co-administration on oxycodone-induced adverse events: a case in the retrospective survey. Eur J Clin Pharmacol. 2011;67(8):859–861. doi: 10.1007/s00228-010-0968-1. [DOI] [PubMed] [Google Scholar]
- 25.Walter C, Ball D, Duffy M, Mellor JD. An unusual case of serotonin syndrome with oxycodone and citalopram. Case Rep Oncol Med. 2012;2012:261787. doi: 10.1155/2012/261787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rosebraugh CJ, Flockhart DA, Yasuda SU, Woosley RL. Visual hallucination and tremor induced by sertraline and oxycodone in a bone marrow transplant patient. J Clin Pharmacol. 2001;41(2):224–227. doi: 10.1177/00912700122009926. [DOI] [PubMed] [Google Scholar]
- 27.Takane H, Nosaka A, Wakushima H, Hosokawa K, Ieiri I. Rifampin reduces the analgesic effect of transdermal fentanyl. Ann Pharmacother. 2005;39(12):2139–2140. doi: 10.1345/aph.1G370. [DOI] [PubMed] [Google Scholar]
- 28.Morii H, Chiba M, Konishi H, Endo Y, Yamaji A. Failure of pain control using transdermal fentanyl during rifampicin treatment. J Pain Symptom Manage. 2007;33(1):5–6. doi: 10.1016/j.jpainsymman.2006.08.005. [DOI] [PubMed] [Google Scholar]
- 29.Mercadante S, Villari P, Ferrera P. Itraconazole-fentanyl interaction in a cancer patient. J Pain Symptom Manage. 2002;24(3):284–286. doi: 10.1016/s0885-3924(02)00477-3. [DOI] [PubMed] [Google Scholar]
- 30.Hallberg P, Martén L, Wadelius M. Possible fluconazole-fentanyl interaction–a case report. Eur J Clin Pharmacol. 2006;62(6):491–492. doi: 10.1007/s00228-006-0120-4. [DOI] [PubMed] [Google Scholar]
- 31.Levin TT, Bakr MH, Nikolova T. Case report: delirium due to a diltiazem-fentanyl CYP3A4 drug interaction. Gen Hosp Psychiatry. 2010;32(6):648.e9–648.e10. doi: 10.1016/j.genhosppsych.2010.08.003. [DOI] [PubMed] [Google Scholar]
- 32.Cronnolly B, Pegrum H. Fentanyl-clarithromycin interaction. BMJ Case Rep. 2012. [Accessed June 30, 2014]. published online. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3417012/ [DOI] [PMC free article] [PubMed]
- 33.Tsutsumi Y, Kanamori H, Tanaka J, Asaka M, Imamura M, Masauzi N. Withdrawal symptoms from transdermal fentanyl (TDF) after an allogeneic peripheral blood stem cell transplant (PBSCT) Pain Med. 2006;7(2):164–165. doi: 10.1111/j.1526-4637.2006.00107.x. [DOI] [PubMed] [Google Scholar]
- 34.Morita T, Shishido H, Tei Y, Inoue S, Nagayama K. Neuroleptic malignant syndrome after haloperidol and fentanyl infusion in a patient with cancer with severe mineral imbalance. J Palliat Med. 2004;7(6):861–864. doi: 10.1089/jpm.2004.7.861. [DOI] [PubMed] [Google Scholar]
- 35.Ailawadhi S, Sung KW, Carlson LA, Baer MR. Serotonin syndrome caused by interaction between citalopram and fentanyl. J Clin Pharm Ther. 2007;32(2):199–202. doi: 10.1111/j.1365-2710.2007.00813.x. [DOI] [PubMed] [Google Scholar]
- 36.Moro C, Taino R, Mandalà M, Labianca R. Buprenorphine-induced acute respiratory depression during ifosfamide-based chemotherapy. Ann Oncol. 2006;17(9):1466–1467. doi: 10.1093/annonc/mdl059. [DOI] [PubMed] [Google Scholar]
- 37.Benítez-Rosario MA, Salinas Martín A, Gómez-Ontañón E, Feria M. Methadone-induced respiratory depression after discontinuing carbamazepine administration. J Pain Symptom Manage. 2006;32(2):99–100. doi: 10.1016/j.jpainsymman.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 38.Tarumi Y, Pereira J, Watanabe S. Methadone and fluconazole: respiratory depression by drug interaction. J Pain Symptom Manage. 2002;23(2):148–153. doi: 10.1016/s0885-3924(01)00368-2. [DOI] [PubMed] [Google Scholar]
- 39.Sorkin EM, Ogawa GS. Cimetidine potentiation of narcotic action. Drug Intell Clin Pharm. 1983;17(1):60–61. doi: 10.1177/106002808301700120. [DOI] [PubMed] [Google Scholar]
- 40.Elsayem A, Bruera E. Methadone-induced respiratory depression in a patient with a history of alcoholism. J Palliat Med. 2005;8(5):1062–1066. doi: 10.1089/jpm.2005.8.1062. [DOI] [PubMed] [Google Scholar]
- 41.Walker PW, Klein D, Kasza L. High dose methadone and ventricular arrhythmias: a report of three cases. Pain. 2003;103(3):321–324. doi: 10.1016/S0304-3959(02)00461-X. [DOI] [PubMed] [Google Scholar]
- 42.Hagelberg NM, Nieminen TH, Saari TI, et al. Interaction of oxycodone and voriconazole–a case series of patients with cancer pain supports the findings of randomised controlled studies with healthy subjects. Eur J Clin Pharmacol. 2011;67(8):863–864. doi: 10.1007/s00228-010-0969-0. [DOI] [PubMed] [Google Scholar]
- 43.Davis MP. Buprenorphine-ifosfamide interactions? Another reason for respiratory depression. Ann Oncol. 2006. [Accessed June 30, 2014]. E-letter. Available from: http://www.annonc.oxfordjournals.org/content/17/9/1466.extract/reply#annonc_el_86.
- 44.U.S. Food and Drug Administration Drug Development and Drug Interactions: Table of Substrates, Inhibitors and Inducers. 2014. [Accessed June 30, 2014]. Available from: http://www.fda.gov/drugs/developmentapprovalprocess/developmentresources/DrugInteractionsLabeling/ucm093664.htm.
- 45.McQuay HJ, Carroll D, Faura CC, Gavaghan DJ, Hand CW, Moore RA. Oral morphine in cancer pain: influences on morphine and metabolite concentration. Clin Phaermacol Ther. 1990;48(3):236–244. doi: 10.1038/clpt.1990.145. [DOI] [PubMed] [Google Scholar]
- 46.Aasmundstad TA, Størset P. Influence of ranitidine on the morphine-3-glucuronide to morphine-6-glucuronide ratio after oral administration of morphine in humans. Hum Exp Toxicol. 1998;17(6):347–352. doi: 10.1177/096032719801700611. [DOI] [PubMed] [Google Scholar]
- 47.U.S. Food and Drug Administration Professional Drug Information. 2014. [Accessed June 30, 2014]. Available from: http://www.drugs.com/pro/darvon-n.html.
- 48.U.S. Food and Drug Administration Professional Drug Information. 2014. [Accessed June 30, 2014]. Available from: http://www.drugs.com/pro/nalbuphine.html.
- 49.Nieminen TH, Hagelberg NM, Saari TI, et al. Rifampin greatly reduces the plasma concentrations of intravenous and oral oxycodone. Anesthesiology. 2009;110(6):1371–1378. doi: 10.1097/ALN.0b013e31819faa54. [DOI] [PubMed] [Google Scholar]
- 50.McCance-Katz EF, Sullivan LE, Nallani S. Drug interactions of clinical importance among the opioids, methadone and buprenorphine, and other frequently prescribed medications: a review. Am J Addict. 2010;19(1):4–16. doi: 10.1111/j.1521-0391.2009.00005.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kharasch ED, Whittington D, Hoffer C. Influence of hepatic and intestinal cytochrome P4503A activity on the acute disposition and effects of oral transmucosal fentanyl citrate. Anesthesiology. 2004;101(3):729–737. doi: 10.1097/00000542-200409000-00022. [DOI] [PubMed] [Google Scholar]
- 52.McCance-Katz EF, Moody DE, Prathikanti S, Friedland G, Rainey PM. Rifampin, but not rifabutin, may produce opiate withdrawal in buprenorphine-maintained patients. Drug Alcohol Depend. 2011;118(2–3):326–334. doi: 10.1016/j.drugalcdep.2011.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fromm MF, Eckhardt K, Li S, et al. Loss of analgesic effect of morphine due to coadministration of rifampin. Pain. 1997;72(1–2):261–267. doi: 10.1016/s0304-3959(97)00044-4. [DOI] [PubMed] [Google Scholar]
- 54.Terenius L. Somatostatin and ACTH are peptides with partial antagonist-like selectivity for opiate receptors. Eur J Pharmacol. 1976;38(1):211–213. doi: 10.1016/0014-2999(76)90221-1. [DOI] [PubMed] [Google Scholar]
- 55.Hagelberg NM, Nieminen TH, Saari TI, et al. Voriconazole drastically increases exposure to oral oxycodone. Eur J Clin Pharmacol. 2009;65(3):263–271. doi: 10.1007/s00228-008-0568-5. [DOI] [PubMed] [Google Scholar]
- 56.Saari TI, Grönlund J, Hagelberg NM, et al. Effects of itraconazole on the pharmacokinetics and pharmacodynamics of intravenously and orally administered oxycodone. Eur J Clin Pharmacol. 2010;66(4):387–397. doi: 10.1007/s00228-009-0775-8. [DOI] [PubMed] [Google Scholar]
- 57.Kharasch ED, Walker A, Whittington D, Hoffer C, Bedynek PS. Methadone metabolism and clearance are induced by nelfinavir despite inhibition of cytochrome P4503A (CYP3A) activity. Drug Alcohol Depend. 2009;101(3):158–168. doi: 10.1016/j.drugalcdep.2008.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kharasch ED, Stubbert K. Role of cytochrome P4502B6 in methadone metabolism and clearance. J Clin Pharmacol. 2013;53(3):305–313. doi: 10.1002/jcph.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ibrahim AE, Feldman J, Karim A, Kharasch ED. Simultaneous assessment of drug interactions with low- and high-extraction opioids: application to parecoxib effects on the pharmacokinetics and pharmacodynamics of fentanyl and alfentanil. Anesthesiology. 2003;98(4):853–861. doi: 10.1097/00000542-200304000-00011. [DOI] [PubMed] [Google Scholar]
- 60.Palkoma VJ, Neuvonen PJ, Olkkola KT. The CYP 3A4 inhibitor itraconazole has no effect on the pharmacokinetics of i.v. fentanyl. Br J Anaesth. 1998;81(4):598–600. doi: 10.1093/bja/81.4.598. [DOI] [PubMed] [Google Scholar]
- 61.Saari TI, Laine K, Neuvonen M, Neuvonen PJ, Olkkola KT. Effect of voriconazole and fluconazole on the pharmacokinetics of intravenous fentanyl. Eur J Clin Pharmacol. 2008;64(1):25–30. doi: 10.1007/s00228-007-0398-x. [DOI] [PubMed] [Google Scholar]
- 62.Olkkola KT, Palkama VJ, Neuvonen PJ. Ritonavir’s role in reducing fentanyl clearence and prolonging its half-life. Anesthesiology. 1999;91(3):681–685. doi: 10.1097/00000542-199909000-00020. [DOI] [PubMed] [Google Scholar]
- 63.Kapil RP, Cipriano A, Michels GH, et al. Effect of ketoconazole on the pharmacokinetic profile of buprenorphine following administration of a once weekly buprenorphine transdermal system. Clin Drug Investig. 2012;32(9):583–592. doi: 10.1007/BF03261913. [DOI] [PubMed] [Google Scholar]
- 64.Janus N, Launay-Vacher V, Byloos E, et al. Cancer and renal insufficiency results of the BIRMA study. Br J Cancer. 2010;103(12):1815–1821. doi: 10.1038/sj.bjc.6605979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Deskur-Smielecka E, Kotlinska-Lemieszek A, Niemir ZI, Wieczorowska-Tobis K. Prevalence of renal impairment in palliative care inpatients: a retrospective analysis. J Palliat Med. 2015;18(7):613–617. doi: 10.1089/jpm.2014.0421. [DOI] [PubMed] [Google Scholar]