Abstract
Background and Purpose
This American Heart Association (AHA) scientific statement provides a comprehensive overview of current evidence on the burden cardiovascular disease (CVD) among Hispanics in the United States. Hispanics are the largest minority ethnic group in the United States, and their health is vital to the public health of the nation and to achieving the AHA’s 2020 goals. This statement describes the CVD epidemiology and related personal beliefs and the social and health issues of US Hispanics, and it identifies potential prevention and treatment opportunities. The intended audience for this statement includes healthcare professionals, researchers, and policy makers.
Methods
Writing group members were nominated by the AHA’s Manuscript Oversight Committee and represent a broad range of expertise in relation to Hispanic individuals and CVD. The writers used a general framework outlined by the committee chair to produce a comprehensive literature review that summarizes existing evidence, indicate gaps in current knowledge, and formulate recommendations. Only English-language studies were reviewed, with PubMed/MEDLINE as our primary resource, as well as the Cochrane Library Reviews, Centers for Disease Control and Prevention, and the US Census data as secondary resources. Inductive methods and descriptive studies that focused on CVD outcomes incidence, prevalence, treatment response, and risks were included. Because of the wide scope of these topics, members of the writing committee were responsible for drafting individual sections selected by the chair of the writing committee, and the group chair assembled the complete statement. The conclusions of this statement are the views of the authors and do not necessarily represent the official view of the AHA. All members of the writing group had the opportunity to comment on the initial drafts and approved the final version of this document. The manuscript underwent extensive AHA internal peer review before consideration and approval by the AHA Science Advisory and Coordinating Committee.
Results
This statement documents the status of knowledge regarding CVD among Hispanics and the sociocultural issues that impact all subgroups of Hispanics with regard to cardiovascular health. In this review, whenever possible, we identify the specific Hispanic subgroups examined to avoid generalizations. We identify specific areas for which current evidence was less robust, as well as inconsistencies and evidence gaps that inform the need for further rigorous and interdisciplinary approaches to increase our understanding of the US Hispanic population and its potential impact on the public health and cardiovascular health of the total US population. We provide recommendations specific to the 9 domains outlined by the chair to support the development of these culturally tailored and targeted approaches.
Conclusions
Healthcare professionals and researchers need to consider the impact of culture and ethnicity on health behavior and ultimately health outcomes. There is a need to tailor and develop culturally relevant strategies to engage Hispanics in cardiovascular health promotion and cultivate a larger workforce of healthcare providers, researchers, and allies with the focused goal of improving cardiovascular health and reducing CVD among the US Hispanic population.
Keywords: AHA Scientific Statements, cardiovascular disease, Hispanic, Latino, stroke
More than 53 million Hispanics currently live in the United States, which constitutes 17% of the total US population. They represent the fastest-growing racial or ethnic population in the United States and are expected to constitute 30% of the total US population by 2050. Hispanics are a diverse ethnic population, varying in race, national origin, immigration status, and other socioeconomic characteristics. Despite the growing numbers of US Hispanics, many continue to face health disparities. Moreover, the diversity among US Hispanics presents many challenges. In particular, comprehensive research data on the prevalence of risk factors for cardiovascular disease (CVD) among Hispanic subgroups have been lacking.1 An incomplete understanding of Hispanic populations in academic research has produced a lack of comprehensive data addressing Hispanic health and CVD, discordant literature regarding CVD risk factors and its prevalence, and a decreased understanding of health status and risk factors contributing to health disparities for US Hispanics.
Cardiovascular research has relied heavily on national surveys of US Hispanics such as the National Health and Nutrition Examination Surveys (NHANES), the National Health Interview Survey (NHIS), and the Behavioral Risk Factor Surveillance System (BRFSS). Yet many of these surveys have examined Hispanics as an aggregated group without identifying their background of origin. It was only in 2007 that NHANES revised its sampling methodology to oversample all Hispanics and not just Mexican Americans. The greater availability of data on Mexican Americans than on other Hispanic groups may simply reflect their larger numerical presence within the United States, but it may not be appropriate to extrapolate these data to the other Hispanic groups. Additional limitations, particularly regarding Hispanic Health and Nutrition Examination Survey (HHANES) data collected 3 decades ago, may not accurately reflect the current burden of CVD risk factors among present-day US Hispanics. Despite these limitations, the aforementioned studies have described a sizeable burden of CVD risk factors among US Hispanics, which suggests a need for further examination and study.2,3 Recent findings from the Hispanic Communities Health Study–Study of Latinos (HCHS/SOL) emphasize the importance of examining the heterogeneity within the Hispanic population and confirm markedly different adverse CVD risk profiles for Hispanic subgroups.1
Because of a lack of comprehensive data and limited interventions addressing Hispanic health, disparities, and CVD, this writing group has conducted a comprehensive review to summarize findings from a variety of sources, including historical, interventional, and observational studies that focused on Hispanic populations. We also conducted our literature search to report, when available, on specific Hispanic subgroups examined, to avoid generalizations. In studies in which the Hispanic background group was not specified, we simply refer to the participants as Hispanics. We include these specific details in an effort to show the heterogeneity and sometimes contradictory information present within the existing data, as well as the need to modify research methodologies to be more inclusive of Hispanics.
Additionally, this review provides a brief background in immigration history, socioeconomic status (SES) factors, psychosocial characteristics, and other information concerning the Hispanic population not often learned by healthcare professionals in their education or training. Understanding the diversity among Hispanics may (1) help promote cultural sensitivity and competency, which is important in addressing the burden of CVD in the Hispanic population; (2) clarify the need for disaggregation of Hispanic subgroup categories in the health research and academic literature; (3) better inform the relationship of CVD/cardiovascular health (CVH) in the US Hispanic population; (4) impact intervention and future study design; and (5) improve the understanding of factors that contribute to health disparities for US Hispanics.
Who are US Hispanics? Demographics and SES
The 1970 census introduced the term Hispanic to refer to individuals of any race who have origins in Mexico, the Caribbean, Central America, South America, or other Spanish-speaking countries.4,5 The term Hispanic was institutionalized in 1976 when the US Congress passed Public Law 94-311, which mandated the collection of information about these same populations. The term Latino has grown in popularity recently and has been adopted as a term by some members of the Hispanic community (similar to the origins of the term African American). Hispanic and Latino are often used synonymously and interchangeably. Both terms are uniquely American labels.6 However, with increased globalization of Spanish language media in the United States and abroad, Latin America has begun to adopt (or least become familiar with) the terms Hispanic/Latino in reference to a broader Spanish-speaking population. For the purposes of this report, the term Hispanic will be used from here forward. The use of Hispanic throughout this report refers specifically to US Hispanics.
It is also important to note that among Hispanics, the term Hispanic is preferred over Latino by a 2 to 1 margin; however, an overwhelming majority (88%) also prefer to identify themselves with their country of origin.7 Because Hispanic groups and subgroups (by various backgrounds of origin) have different sociocultural practices, environmental experiences, genetic backgrounds, and cultural histories that shape their predispositions to certain chronic conditions, including CVD, the use of the aggregated label of Hispanic likely leads to misclassification with respect to true associations with CVD risk factors and incident disease. In recognition of these differences, as well as the growing relevance of these diverse Hispanic subgroups to national public health, there have been increasing efforts (including the National Heart, Lung, and Blood Institute’s HCHS/SOL, the National Eye Institute’s Los Angeles Latino Eye Study, the National Cancer Institute’s Understanding and Preventing Breast Cancer Disparities in Latinas, and the National Institute on Minority Health and Health Disparities’ San Diego Partnership to Reduce Diabetes and CVD in Latinos) to explore disease risk factors among the different Hispanic subgroups.8,9 Such studies provide an opportunity to examine unique risk factors in collective and disaggregated Hispanic groups. The HCHS/SOL is, to date, the largest cohort study of CVD in US Hispanics, with 16 415 Hispanic participants aged 18 to 74 years who self-identified as being of Mexican, Cuban, Puerto Rican and Dominican, or Central and South American descent in 4 US communities: Bronx, NY; Chicago, IL; Miami, FL; and San Diego, CA.8,9
Current Demographic Profile
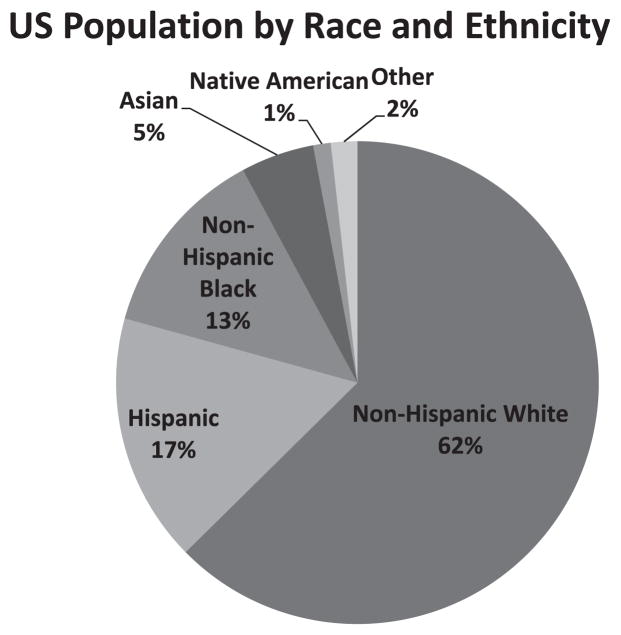
In 2013, 53 million Hispanic individuals represented 17% of the US population, which made them the largest racial/ethnic minority in the United States (Figure 1).10 Moreover, between 2000 and 2010, the Hispanic population increased by 3%, which represented more than half of the nation’s population growth during that decade. Hispanic individuals also represent the largest US immigrant population; among the nation’s 40 million immigrants, nearly half (47%) are Hispanic. A large majority of Hispanic people (74%) are US citizens, either naturalized or by birth.11 Most Hispanic immigrants who were US residents as of 1990 or later (83.6%) had not yet obtained US citizenship by 2011,12 and thus, it is reasonable to anticipate increasing numbers of Hispanic citizens in the future as this recent immigrant population becomes naturalized. Because of the sensitivity of immigration status, data are very limited for unauthorized immigrants, a fact that limits any research on the US Hispanic population.13 Thus, data presented on foreign-born Hispanics residing in the United States may not include those who are not legal immigrants.
Figure 1.
US population by race and ethnicity. Racial groups include only non-Hispanics. Hispanics may be of any race. Source: Tabulations of US Census Bureau Statistics; 2012 population estimates.10
Projected to grow to 30.2% of the US population (132.7 million) by 2050, Hispanics are one of the country’s fastest-growing populations.14 The 2050 projected growth for each Hispanic subgroup will likely vary substantially, as it did from 2000 to 2010 (Table 1). Mexicans increased by 54% and accounted for ≈75% of the 15.2 million person increase in the US Hispanic population. Puerto Ricans grew by 36%, whereas the Cuban population increased by 44%.
Table 1.
The 10 Largest US Hispanic Groups by Origin, 2000 and 2010
| 2000, in Millions | 2010, in Millions | % Change 2000–2010 | % of Total Hispanics, 2010 | |
|---|---|---|---|---|
| Colombian | 0.47 | 0.97 | 106 | 1.9 |
| Cuban | 1.2 | 1.8 | 44 | 3.7 |
| Dominican | 0.76 | 1.5 | 97 | 3.0 |
| Ecuadorian | 0.26 | 0.67 | 73 | 1.3 |
| Guatemalan | 0.37 | 1.1 | 197 | 2.2 |
| Honduran | 0.22 | 0.73 | 231 | 1.4 |
| Mexican | 20.6 | 31.8 | 54 | 64.9 |
| Peruvian | 0.23 | 0.61 | 165 | 1.2 |
| Puerto Rican | 3.4 | 4.6 | 36 | 9.2 |
| Salvadoran | 0.66 | 1.8 | 172 | 3.6 |
Forty-seven percent of Hispanics aged ≥18 years were married; 36.1% were never married.17 By comparison, non-Hispanic whites (NHWs) of the same age were somewhat more likely to be married (55.4%) and less likely never to have married (23.6 %).17 Foreign-born Hispanic women were more likely to be married (56.2%) than US-born Hispanic women (38.8%).18 Hispanic households are generally larger, consisting of 3.4 people on average, compared with 2.5 people in NHW households.19 Compared with NHWs, a larger proportion of Hispanics are young. The median age of Hispanic individuals residing in the United States was 27 years, which is 10 years younger than the median age of the US population.15 Among Hispanic individuals, those of Mexican background had the lowest median age (25 years) and Cuban Americans the highest (40 years).15 Only 6% of Hispanics people are ≥65 years of age compared with 15% of NHWs. Of note, the aging growth trend is greater for Hispanic individuals than for NHW Americans. That is, although the NHW population aged >65 years is expected to grow by 83% between 2000 and 2030, Hispanic individuals of this same age group are projected to grow by 328%. This makes Hispanics the fastest-growing aging population in the United States,20,21 with potential implications to healthcare costs for the Centers for Medicare and Medicaid Services.
The geographic distribution of the US Hispanic population has also changed substantially within the past decade. Although more than half of all US Hispanic individuals live in 5 states (California, Texas, Florida, New York, and Illinois), the Hispanic population in 8 states in the South (Alabama, Arkansas, Kentucky, Maryland, Mississippi, North Carolina, South Carolina, and Tennessee) and South Dakota more than doubled in size between 2000 and 2010.22 South Carolina has the fastest-growing Hispanic population, increasing from 95 000 in 2000 to 236 000 in 2010 (a 148% increase), whereas Alabama showed the second-fastest rate of growth at 145%, increasing from 76 000 to 186 000.
SES Characteristics
Lower SES is associated with increased cardiovascular morbidity and mortality,23,24 possibly related to people with lower SES being exposed to more frequent and severe psychosocial stressors,25 as well as via reduced healthcare access and worsened preventative healthcare practices. According to the US Census, the SES of Hispanic individuals is comparable to that of non-Hispanic blacks (NHBs) and significantly lower than that of NHWs,26 regardless of a variety of SES measures, including personal and family income, poverty rates, educational attainment, occupation, and wealth.
Education
Education has been shown to be the most reliable socioeconomic predictor of CVD.27 In 2000, 53.2% of all Hispanic individuals had an educational attainment of high school or greater, compared with 90.1% of the US population as a whole.28 In 2010, 62.9% of Hispanic adults aged ≥25 years had obtained at least a high school degree and 13.9% had completed at least a bachelor’s degree compared with 87.1% and 29.9% of the total US population, respectively.29 Despite this increase in educational attainment over time, Hispanics had the lowest percentages of those with at least a high school diploma (60.9%) compared with NHWs (90.4%) and NHBs (81.4%).30 Many Hispanic immigrants have received little or none of their education in the United States; however, according to 2012 statistics, first- and second-generation US-born Hispanics complete all of their education in the United States and are generally the first in their families to graduate high school or attend college.31 Furthermore, educational attainment differed by nativity, with foreign-born Hispanics having less educational attainment than US-born Hispanics regardless of Hispanic subgroup. In fact, the educational attainment of foreign-born Hispanics remained lower than all other US racial/ethnic groups.30
Income and Wealth
In 2011, 25.3% of the Hispanic population lived below poverty level compared with 15% of the total US population.32 Between 2006 and 2010, the poverty rate among Hispanics increased by 5%, more than for any other US group. In contrast, poverty rates decreased among NHWs from 10.4% to 9.9% and increased among NHBs by 2.3%, from 25.3% to 27.6%.33,34 The proportion of Hispanic families with annual income >$50 000 was 37.9 % compared with 50.1 % for the total population.32 Approximately 50.9% of Hispanic families have total income <$35 000 per year compared with 26.3% of NHW families.35 Notably, Puerto Ricans on the US mainland face some of the highest rates of poverty seen among all racial/ethnic groups.21,36
The housing crisis and economic recession between 2005 and 2009 affected the wealth profile of minorities more than the NHW population. In 2009, the median wealth (assets minus debts) of NHW households was 18 times that of Hispanic households. Median wealth between 2005 and 2009 decreased substantially for both Hispanic and NHB households (by 66% and 53%, respectively) compared with the 16% decline in wealth for NHW households (Figure 2).37 These wealth differences by race/ethnicity highlight a greater margin of inequity than seen when household income is compared across groups, because income is distributed more evenly across groups.38 Very little research has examined the impact of income versus wealth inequity on cardiovascular outcomes among the Hispanic population.
Figure 2.
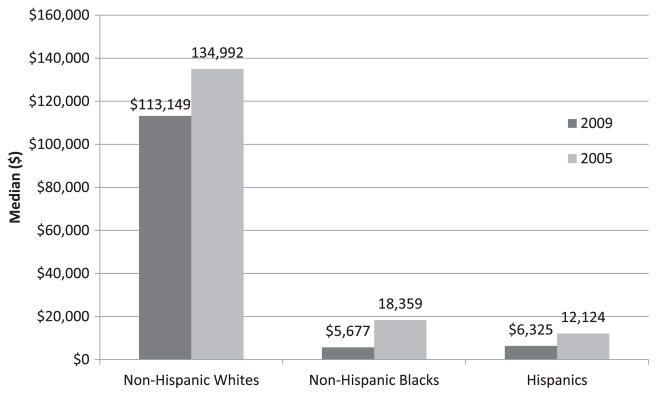
Pew Research analysis of median household wealth across racial and ethnic groups, from 2005 to 2009. Data derived from Pew Research Center tabulations of survey of income and program participation data.37
Occupation
The majority of Hispanics in the United States are employed (66.4%), similar to the 64.0% rate for NHWs.39 Despite this, Hispanic workers have the lowest median earnings of all US racial and ethnic groups.40 The 2 major occupation categories41 are high-risk/low-social-position occupations (including service occupations; precision production, craft, and repair occupations; operators, fabricators, and laborers; and farming, forestry, and fishing occupations) and low-risk/high-social-position occupations (including both managerial and professional occupations and technical, sales, and administrative support occupations). In 2010, Hispanics (59.0%) were disproportionately represented in high-risk/low-social-position occupations compared with NHBs (45.9%) and NHWs (38.1%; Figure 3).42 Because of lower levels of education, limited English proficiency, and documentation status, foreign-born Hispanics are more likely to be employed in low-skill jobs and to have substantially lower incomes than their US-born counterparts.43–45
Figure 3.
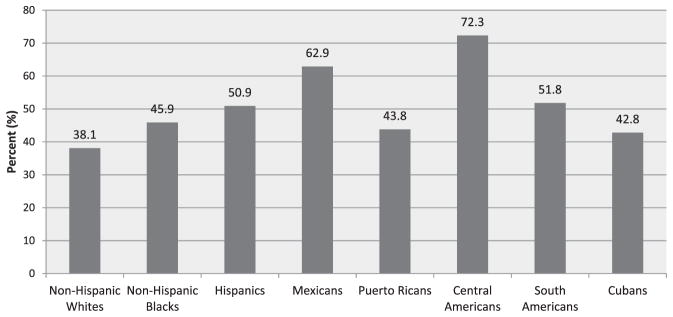
Percent composition of racial and ethnic groups in high-risk/low-social-position occupations. Source: Tabulations of US Census Bureau statistics.42
Insurance Status
Access to healthcare services in the United States is highly dependent on availability and access to health insurance. Those who lack insurance either must independently pay for healthcare services or seek healthcare services from safety net facilities such as free clinics, hospital emergency rooms, and community health centers. Because uninsured rates are higher among people with lower SES, and a large proportion of the Hispanic population lives in poverty, a large proportion of Hispanics lack healthcare insurance coverage. In 2011, Hispanics disproportionately represented 30.1% of the US uninsured population and fared worse than NHWs (11.1%) and NHBs (19.5%) with regard to being uninsured.32 Employment does not necessarily guarantee insurance. Although Hispanics are employed at similar rates as NHWs, they are disproportionately uninsured compared with their NHW peers because of their more frequent employment in occupations that do not provide health insurance. The proportion of uninsured Hispanics directly influences their access to health care.
The 2010 Patient Protection and Affordable Care Act is anticipated to substantially increase the number of US citizens and legal immigrants with health insurance by expanding Medicaid eligibility to adults with incomes up to 138% of the federal poverty level. Although millions of uninsured US Hispanics will be eligible for coverage under the 2010 Patient Protection and Affordable Care Act, undocumented immigrants will continue to be ineligible for coverage under its provisions. Noncitizens or undocumented immigrants who lack continuous, comprehensive, and preventive care will continue to depend on episodic or emergency healthcare services.
Not only are Hispanics at a disadvantage because of low insurance coverage, but research by the US Centers for Disease Control and Prevention has also shown that Hispanics are twice as likely as NHBs and 3 times as likely as NHWs to lack a regular healthcare provider.46 One in 3 Hispanic adults in the United States lacks a regular healthcare provider, regardless of nativity status (US born or foreign born).46,47 The profile of a Hispanic individual most likely to lack a regular healthcare provider is similar to that of the general US population without health care: male, young (between ages 18 and 29 years), and less educated (with less than a high school diploma).47 Although Hispanic women are more likely to have a regular healthcare provider than their Hispanic male counterparts (36% versus 17%, respectively), Hispanic women remain less likely to have a usual source of health care (80.0%) than NHW women (91.7%) and all US women (89.6%).47,48
SES Heterogeneity
SES varies significantly among US Hispanic groups (Table 2). Hispanic individuals of Cuban and Puerto Rican background had the highest proportion with at least a high school diploma, and those of Colombian and Peruvian origin had the highest proportions with a bachelor’s degree or more education and the highest median household income. Hispanic individuals of Dominican, Honduran, Mexican, and Puerto Rican backgrounds are among the groups with the lowest median household incomes and are more likely to live in poverty.
Table 2.
Demographic and Socioeconomic Characteristics for Hispanics, 2010
| Median Age, y | High School Diploma, % | Bachelor’s Degree or More, % | Without Health Insurance, % | Living in Poverty, % | Median Household Income (in Thousands) | |
|---|---|---|---|---|---|---|
| Colombian | 34 | 27 | 32 | 28 | 13 | 49.5 |
| Cuban | 40 | 29 | 24 | 25 | 18 | 40 |
| Dominican | 29 | 26 | 15 | 22 | 26 | 34 |
| Ecuadorian | 31 | 26 | 18 | 36 | 18 | 50 |
| Guatemalan | 28 | 22 | 8 | 48 | 26 | 39 |
| Honduran | 28 | 26 | 10 | 50 | 27 | 38 |
| Mexican | 25 | 26 | 9 | 34 | 27 | 38.7 |
| Peruvian | 34 | 27 | 30 | 30 | 14 | 48 |
| Puerto Rican | 27 | 30 | 16 | 15 | 27 | 36 |
| Salvadoran | 29 | 24 | 7 | 41 | 20 | 43 |
| All Hispanics | 27 | 26 | 13 | 31 | 25 | 40 |
Data derived from Motel and Patten.15
Racial Admixture and Inclusion History Among US Hispanics
Race as a social or biological construct has important CVH implications. Hypertension, cardiac hypertrophy, and cardiovascular disparities are more prevalent among NHBs than NHWs,49–51 yet race among Hispanic subgroups remains largely unexplored. Hispanics with greater African admixture may have more similarity to NHBs with regard to CVH and CVD risk factors than appreciated previously. Studies suggest that Hispanics of Caribbean descent have a similar prevalence of hypertension,52 abnormal 24-hour blood pressure,53 and cardiac hypertrophy54 as NHBs. Furthermore, some Hispanics may be at risk for not only ethnic discrimination but also racial discrimination because of their non-European appearance.55–57 Research exploring these constructs reported that dark-skinned US Hispanics experience more discrimination than their light-skinned counterparts.58,59 The interaction of darker skin color and SES among Puerto Ricans was associated with higher systolic blood pressure than genetic ancestry alone.60 This section examines some of the rationale that contributes to a greater attention to racial admixture and ethnic group disaggregation among US Hispanics.
Histories of Race in Latin America
Latin America is a region in which extensive racial and cultural mixing occurred through a process of colonization that began in the 15th century. Slavery was abolished in most Latin American countries and interracial marriage was legal and socially accepted by the 1800s, which resulted in an intermixed Latin America.61 As a result, Hispanics are not just geographically and culturally diverse but also racially diverse.62 Specific Amerindian populations differed throughout Latin America so that, for example, the Amerindian population in Mexico is distinct from the indigenous population in the Caribbean, Peru, or Guatemala.63 These indigenous populations shrunk to less than half of their size before Spanish conquest in some Latin American countries and became nearly became extinct in others.64 Countries such as the Dominican Republic, Cuba, Puerto Rico, Brazil, Panama, Colombia, and Venezuela imported larger numbers of West African slaves, and intermixed populations of African descent constitute a sizeable segment of the Hispanic population in these respective countries. Not only did the size of the Amerindian or African population vary across Latin America, but the practices of intermarriage also varied substantially depending on region and country. Genetic studies have confirmed that Mexican-origin Hispanics have varying proportions of European and Amerindian ancestry, whereas Hispanics from the Caribbean have varying proportions of European and African ancestry.65,66 Central/South Americans have varying proportions of European, Amerindian, and African ancestry depending on the country of origin. Thus, the Latin American country of origin does correspond somewhat to the racially admixed background among Hispanics.63 Asian immigrants have embraced Hispanic culture, intermarried, and made a notable impact on Latin American society. There is also a large population of Chinese ancestry in the Dominican Republic, Puerto Rico, Cuba, and Panama that has existed since migration to Latin America began in the 19th century. Four and a half million Latin Americans (almost 1% of the total population) are also of recent Asian descent. A significant number of Japanese, along with East Asian Indians and Southeast Asians, have established residency in certain countries, notably Paraguay, Argentina, and Peru.
This long history of cultural and racial admixture in Latin America has resulted in a sociocultural, sociopolitical structure that categorizes and recognizes race differently from how race is conceptualized within the United States. Consequently, the accurate identification of race among US Hispanics is problematic. Whereas the racial classification system prominent in the United States reflects only a black or white, Latin America has racially mixed categorizations that are more complex and more closely representative of mixed Amerindian-European or African-European heritage.58,67–69
Immigration/Inclusion Patterns of Different Hispanic Subgroups
Ten Hispanic subgroups represent 92% of the total US Hispanic population (Table 1). There is a distinct and diverse pattern of immigration and inclusion into the United States among each Hispanic subgroup. This, in turn, has had a significant impact on the concentrations of these groups in different US geographic areas, as well as an influence on their health-related characteristics. In broad terms, 4 sociopolitical profiles21 exist among US Hispanics: (1) US born and US educated (includes first-generation* or higher Hispanic people born to immigrant parents; Puerto Ricans; and Mexicans from annexed portions of the Southwest United States); (2) educated professionals who immigrated to the United States, some from large urban cities from Latin America; (3) other documented immigrants; and (4) undocumented immigrants. Profiles 2, 3, and 4 include those immigrants who moved for better economic or educational opportunities or as political refugees. Notably, generational distinctions add to the complexity of Hispanic identity; for example, within the first generation of immigrants, there are fundamental differences between those who arrive as children and those who arrive as adults.70,71 Such generational categories have been found to have direct implications for language, literacy, and economic earnings and consequently, the demographic characteristics associated with health outcomes.70–72
Mexico
Compared with other Hispanic subgroups, Mexican-origin Hispanics probably have the oldest history with the United States. The first era, from 1520 until 1821, covers the period from the Spanish colonization until the beginning of Mexico’s revolution against Spanish rule. A cultural synthesis (mestizaje) of European and indigenous Amerindian cultures took place during these 300 years. During this same period, what is now the Southwest United States was part of Colonial New Spain and later became Mexico when Mexico won its independence from Spain. The second era began in 1822 and ended in 1848 with the Mexican-American War. As a result of that war, the United States annexed the Mexican territories and the inhabitants of what is now the Southwest United States, including California, Nevada, Utah, New Mexico, Texas, Arizona, Colorado, and parts of Oklahoma, Kansas, and Wyoming. Large-scale urbanization and industrialization, occurring between 1849 and 1920, marked a third era. The lure of employment opportunities during the labor shortages of World War I, as well as the opportunity for escape from the Mexican Revolution (1910–1917) ensured a steady stream of millions of Mexican immigrants until the Great Depression of the 1930s. When the United States entered World War II, it turned to Mexico to address wartime labor shortages. The Bracero program (1943–1964) allowed for the temporary importation of contract laborers from Mexico and marked a fourth era of immigration from Mexico to the United States. In the decades after World War II, Mexicans’ migration shifted to longer-term settlement patterns, and Hispanic individuals of Mexican background began to emerge as a distinct and visible social group in the United States. This marked the beginning of the fifth era with the passage of immigration reforms in 1965, including legalization programs for those who had entered the United States before 1982. Indeed, by the early 1990s, >90% of Mexican Americans were living in or near urban cities and assimilating to the dominant cultural norms.73 Monolingual speakers of indigenous languages now represent a growing number of the more recent immigrants from Mexico.
Puerto Rico
Whether they were born in their homeland, Borinquen (the indigenous name of the island colonized by Spain in the 1400s), or in the US mainland, Puerto Ricans are citizens of the United States by birth. Some 4.6 million Puerto Ricans live in the mainland United States, and 3.9 million live in the Commonwealth of Puerto Rico. Puerto Rico was ceded to the United States by Spain in 1898 after an invasion of American forces and subsequent defeat during the Spanish American War.
Puerto Ricans began a northward migration in the late 1940s and 1950s as part of Operation Bootstrap after World War II. In an effort to improve the island’s severe economic problems, Puerto Rico prompted a migration of thousands of Puerto Ricans into the agricultural farmlands and manufacturing centers of the northeast United States. The plan had mixed results. Despite their status as citizens, both mainland and island-dwelling Puerto Ricans continue to face tremendous economic challenges. Although the mainland Puerto Rican population has historically been concentrated in the New York/New Jersey/Connecticut area, an increasing number of individuals of Puerto Rican background can also be found in Florida, Illinois (Chicago), and Massachusetts.36
Cuba
The oldest wave of migration of Cubans to the United States can be traced back to the 1800s. When the Ten Years War (1868–1878), a Cuban attempt to become independent from Spain, failed and resulted in a more oppressive Spanish rule, thousands of Cubans left the island and went to nearby Florida. Cuban immigration to the United States continued into Florida and reached new heights between 1896 and 1910, after 1918, and during the Great Depression with the fluctuations of the Florida cigar-making industry. During the Batista regime and before the arrival of Castro’s government, many Cubans fled to Florida in political protest.74 Once the Cuban revolution ended and Fidel Castro rose to power in 1959, some Cubans initially returned to their country in hopes of a better government, but by the early 1960s, the period of modern Cuban emigration began. During this time, Cubans who had their livelihood taken by the government, faced incarceration, or had their freedom of speech repressed, left the island seeking political and economic freedom in the United States. During the same period (1960–1962), >14 000 unaccompanied Cuban youths arrived in the United States; Operación Pedro Pan was the largest recorded exodus of unaccompanied minors in the Western Hemisphere.75
Before 1985, the US government facilitated Cuban immigration with the 1966 Cuban Refugee Act and offered financial support and educational training to facilitate economic and social adaptation into US culture with a degree of acceptance and assistance that no other Hispanic group has experienced. However, this unrestricted immigration changed with the 1980 Mariel Boatlift, which brought 125 000 Cubans, many of whom had been imprisoned for opposition to the Cuban government and called antisocial, to the United States.76,77 This new wave of immigrants faced more discrimination and SES difficulties than previous Cuban immigrants. The US government sought to reduce the number of Cuban immigrants allowed into the United States with the 1980 Refugee Act. In 1984, Congress reenacted the Cuban Refugee Act of 1966 and restored the favorable status Cuban refugees had previously enjoyed. By the end of 1985, most Cubans had received permanent residency status in the United States, which enabled them to apply for citizenship.73
Dominican Republic
Since the early 17th century, the island La Española has been divided into 2 sides, 1 colonized by the French (Haiti) and 1 by the Spanish (Dominican Republic). During the period of colonization, many of the indigenous Caribbean Amerindian population of Cuba, Puerto Rico, and the Dominican Republic died. By the end of the 17th century, Spanish law allowed slaves in the Dominican Republic to buy their own freedom. As black freemen in La Española began to outnumber slaves, they began to intermarry with Spaniards. This intermarriage has created, over several hundred years, a large mixed-ancestry population and a synthesis of mostly Spanish and African cultures.
The first wave of emigration from the Dominican Republic to the United States was in large part the product of political and social instability in 1963 after a US-supported military coup of the dictator Rafael Trujillo. Those who opposed the new regime and those who were fleeing violence throughout the 1960s came to the United States in notable numbers. Before this time, the possibilities for leaving the island had been very limited. As such, at the time of the 1980 US Census, only 6.1% of all Dominicans had arrived in the United States before 1960.78 Even as the political situation in the Dominican Republic stabilized over time, Dominicans continued to emigrate, mostly because of limited employment and poor economic conditions on the island. Dominicans now account for 3% of the total US Hispanic population, increasing by 85%, from 765 000 in 2000 to 1.4 million in 2010.22 Thus, relative to other Hispanics, the Dominican community is primarily composed of recent immigrants over the past 30 to 40 years. Most Dominican-origin individuals have settled in the Northeast, primarily in New York City, but growing numbers are now found in Massachusetts, Pennsylvania, Florida, and across the United States.80
Central and South America
Immigrants from both Central and South America began arriving in larger numbers in the 1970s when those countries suffered political instability, economic turmoil, and violence.44 For example, during the 1980s and 1990s, approximately 1 million refugees from El Salvador sought asylum in the United States. In the 1980s, the Guatemalan government began a process of modernizing their indigenous population in an attempt to unify a country divided by >20 different languages, traditions, and religious practices. In this process, the military clashed with local resistance groups and forced many indigenous people, mostly women and children, to cross the border into Mexico or seek asylum in the United States. Similar political turmoil also motivated migration from South America. Although small numbers of Ecuadorians began entering the United States on tourist and work visas during the 1960s and 1970s, most Ecuadorians now living in the United States are economic refugees who fled during Ecuador’s political and banking crisis of the 1990s. These also include a large number of undocumented workers from the rural Andes who work in low-paying, unskilled service and manufacturing industries.
In contrast to their South American peers, Peruvian immigrants began migrating to the United States during the California Gold Rush (1848–1855).81 After World War II, migration increased in response to rising US demand for industrial labor. During the 1970s, mostly upper- and middle-class Peruvian residents, as well as highly skilled professionals and technicians, fled the military regime. In the early 1980s, political violence and economic crisis spurred indigenous people from rural regions and individuals of lower SES to leave Peru. Intensification of violence and the economic crisis, which continued through the 1990s, also forced highly educated, middle class, and professional Peruvians to emigrate.
In general, Central American and South American immigrants are more recent additions to the United States. In recent decades, the Central American population in the United States has grown rapidly, from 345 655 in 1980 to 1.1 million by 1990 and nearly doubling to 2.0 million in 2000. Similarly, the Central American immigrant population grew by nearly 890 000 between 2000 and 2009, and by 910 000 during 1990 to 2000.43 Immigrants from El Salvador and Guatemala accounted for 41.2% and 28.7%, respectively, of the total increase. Although Colombian immigrants are relative newcomers, Colombians were the largest South American immigrant group in the United States in 2010, accounting for 23% of all South Americans in the United States.82 Central Americans from Guatemala and Honduras are more likely than any other US Hispanic group to lack health insurance.
Documenting Race Among US Hispanics
The histories of migration, immigration, and the processes of colonization have resulted in unique racial admixture among Hispanics. Hispanics can be of any race or combination of races and may self-identify as Asian, Amerindian, black, or white, but in the United States they are all considered Hispanics. Despite this reality, the US Census defines race by 6 categories: NHW, NHB, American Indian, Alaska Native, Asian, and Other; ethnicity is only subdivided as Hispanic or non-Hispanic. The discordance between the understanding of race among Hispanics and the US conceptualizations of this construct affects how Hispanics respond to the discrete racial categories that appear on the US Census. Among Hispanics, the question of race in the United States is frequently confused with that of ethnicity. There is a perception that for Hispanics to identify as racially black or white in the United States, they are negating their ethnic Hispanic identity. Moreover, acculturation among Hispanics, which is dependent on length of time in the United States, age of arrival, immigrant generation, educational levels, and even geographic residence, also influences understanding of the US racial taxonomy.83,84 As a result, national attempts at racial data collection among Hispanics have often been unfruitful, revealing little about this population. A growing proportion of Hispanics self- identify as “other race.”67,85,86 Yet it would be incorrect to merge the concepts of race and ethnicity when it comes to Hispanics.87–89 What is needed is better educating of Hispanics on the societal differences of the concept of race between the United States and Latin America and on what can be learned from racial self-identification under the current US framework.
Genetic admixture analysis is another method to investigate potential genetic factors that contribute to racial differences in complex phenotypes.90,91 The technique is based on the knowledge that individuals can be classified, on the basis of genetic markers, into clusters that correspond to continental lines and to commonly identified racial groups. Genetic admixture analysis quantifies the proportion of an individual’s genome that is of a given ancestral origin (eg, European, African, Asian) using ancestry-informative markers (those with large frequency differences between the ancestral populations). Genetic admixture analysis may provide a more sophisticated and informative method of studying race and the ways in which race affects CVD among Hispanics, rather than the cruder self-reporting into categorical racial groups.65,66,92
Commonalities in Language and Cultural Beliefs Among US Hispanics
Although Hispanics are not bonded by shared physical characteristics, the fusion of Spanish, African, and Amerindian culture, religion, and histories has given rise to a rich cultural heritage, an intertwined history, a common language,93 and several cultural characteristics that are common across the varied Hispanic subgroups, including familismo, respeto, personalismo, simpatía, personas de confianza, religiosidad, fatalismo (destino).94
Language
Spanish is the predominant language throughout Latin America (except for Brazil) and has had far greater generational longevity than other non-English languages in the United States.95 A continuous flow of Latin American immigrants makes it easier for US Hispanic residents to retain their Spanish tongue and provides greater opportunities and incentives for bilingualism.95 The spoken Spanish language varies among diverse Hispanic subgroups, and slight regional variations in Spanish dialect and accents are present across Latin America. Among a minority of foreign-born Hispanics, particularly migrant workers from some rural parts of Mexico and South America, indigenous languages such as Mixtec, Chinantec, and Mayan are more common; limited formal Spanish literacy skills and lack of written indigenous languages are further significant barriers to healthcare services, education, and other social services.96,97 Although proficiency in English is often a measurement of acculturation, its use among US Hispanics is influenced by multiple factors, including generational patterns, SES, sex (more so in females), and family communication dynamics.98 Preference for and ability in the English language vary widely among Hispanics. Among many Hispanics, English is commonly used for business and official domains, as a means of achieving social mobility, whereas Spanish is used mostly in familiar and personal environments.99,100 Among US-born Hispanics, according to self-report, 38.7% spoke only English and 61.2% were bilingual, of whom 12.2% spoke English less than “very well.”101 Foreign-born Hispanics are mostly a population with limited English proficiency; 4.2% spoke English only, and 95.8% were bilingual, of whom 68.4% spoke English less than “very well.” By the second and third generations, estimates of English fluency jumped to 88% and 94%, respectively.102 Immigrants who arrived in the United States as young adults are more likely to report not speaking/reading English well than those who arrived before the age of 10 years.102 Furthermore, English language proficiency may differ across Hispanic subgroups. A recent Pew Hispanic Center report found that Hispanics of Mexican and Puerto Rican backgrounds had the highest proportions of individuals who spoke only English at home, whereas those of Dominican, Guatemalan, Honduran, and Salvadoran background had the smallest proportion of English-proficient speakers.15
Among Hispanic populations, language preference and proficiency have profound effects on health services utilization, perception of healthcare quality, and even risk of poor health.103–105 In the 2003 Medical Expenditure Panel Survey, speaking a language other than English at home identified Hispanics who were at risk for not receiving recommended healthcare services.106 However, researchers using the BRFSS noted that Spanish-speaking Hispanics ate fruit more times per day but consumed significantly fewer vegetables than English-speaking Hispanics.107
Preference for and use of the Spanish language influenced perceived health status, as well as health knowledge. BRFSS data (2003–2005) from 45 076 Hispanic adults in 23 states showed that Spanish-speaking Hispanics reported far worse health status and less access to preventive health care than did English-speaking Hispanics; these findings were not attenuated by adjustment for SES factors.103 Furthermore, these data showed that although almost half of all Spanish-speaking Hispanics had a personal physician, 1 in 4 were unable to afford needed health care in the past year and were less likely to receive preventive health services.105 Spanish-speaking Hispanics were far less likely to be knowledgeable of heart attack and stroke symptoms than English-speaking Hispanics, NHBs, and NHWs.108
Language and Health Literacy
There is an important role for health literacy, because it influences the ability to negotiate health systems, understand and act on health treatment and advice, and seek timely and appropriate health care.77,78 Lower health literacy predicted increased all-cause mortality among patients with heart failure.109 Although low health literacy can impact all populations, health literacy is particularly relevant for Hispanics. The education, income profile, and English proficiency characteristics of the Hispanic population heighten the health literacy challenges. There are 3 aspects of health literacy: (1) Functional health literacy refers to basic skills in reading, writing, and comprehension, and some research has indicated that health disparities are attenuated by increasing functional literacy.110 (2) Interactive health literacy focuses on personal skills that increase self-efficacy and motivation. (3) Critical health literacy is defined as a range of skills that enable individuals to obtain, understand, use, and evaluate health information with the goal of reducing their own health risks, exerting greater health decision making, and making informed health choices.111–114 Patient-level health literacy potentially influences a patient’s willingness to engage their physicians in discussions about health issues. Almost twice as many Spanish-speaking compared with English-speaking patients have poor functional health literacy that results in a significantly diminished capacity to function in the healthcare system.115 Moreover, 3 times the number of Hispanics as NHWs lack the functional health literacy required to understand medical instructions and healthcare information such as reading their medication bottles.116 There has been very little examination of the recent accessibility of health information available online or via social media and the health literacy disparities produced or exacerbated because of the “digital divide.”
Language and Patient-Provider Relationships
Language discordance, when patients and providers do not share a common language or have limited proficiency in one another’s languages, is one of the greatest barriers faced by Hispanic patients in accessing health care. Communication challenges include the physician’s inability to listen to everything communicated by the patient, patients not fully understanding their doctor, and patients having questions during the visit that they were unable to ask. These problems are worse among Spanish-speaking patients than among those whose primary language is English.117–119 Often, Hispanic patients with limited English-speaking abilities find translation services to be inadequate and thus question the accuracy of the health information they are receiving.120,121 As a result, these patients often rely on family members as translators.122,123 Even after controlling for SES and demographic characteristics, Spanish-speaking patients report perceived differences in the type and quality of information that clinicians provide and receiving health education information that is less detailed and less empathetic.105,120,124–127 Cultural competence and literacy among providers, a significant factor for effective patient-provider communication, has been linked with improved patient decision making, patient communication, and adherence to treatment.128 Training for providers in cultural competence and cultural literacy includes knowledge and skill development in the use of patient beliefs, customs, and world views to frame health information.129 Provider cultural competence is perceived to be high when the practitioner is able to speak even some Spanish and can affect the content of the interaction.58,67 In these cases, Hispanic patients’ recall of the information exchanged and the patients’ satisfaction with the interaction are high.130,131 One recent study examined the role of culture and healthcare interaction among Mexican immigrants and found that adherence decisions were associated with patients’ beliefs about the physician’s cultural literacy and identity.128
Familism
Familism or familismo is considered an important part of Hispanic culture132 and is characterized when family members are a source of financial or emotional support.133 Foreign-born, less acculturated Mexicans for whom Spanish is the primary language spoken at home have higher family support than NHWs.134 Family members are often a source of financial or emotional support, which in turn can facilitate access to health services,135 promoting preventive practices and better medical treatment adherence. The main elements of familism include the perceived obligation to provide family members with material and emotional support, reliance on family members for assistance, and the perception of family members as attitudinal and behavioral referents.136 Studies on familism suggest that its salutary effects may help explain the better-than-expected health outcomes (ie, Hispanic paradox) observed in Hispanics.137,138 In fact, familism is often the basis for studies on CVD risk factors and social support among Hispanics.
Hispanic families in Latin America have been described as amplified or extended families consisting of a nuclear family and aunts, uncles, cousins, and godparents, as well as non-blood relatives such as friends and neighbors who have grown up together (often referred to as additional aunts, uncles, and cousins) who are also extensions of the family.139 As a result of this strongly held cultural value, Hispanic patients tend to respond better to messages with emphasis on “doing the right thing for the family” rather than “doing the right thing for yourself.”136 A focus on the family enables Hispanic immigrants to retain aspects of their culture, which may protect them from negative behaviors found in the mainstream culture140 and promote better psychological well-being.141 However, familism might attenuate over time as Hispanic immigrants assimilate into the more individualistic US culture. As a result, US-born Hispanics report lower familial social support than foreign-born Hispanics.134 Nevertheless, the attitudes of even more acculturated Hispanics remain more familistic than those of NHWs.142 Because familism can be broadly defined as placing one’s family above oneself, emphasizing interdependence over independence,143 familism can also contribute to stressful situations, particularly during the acculturative process. For example, an individual who agrees that an aging parent should live with relatives may experience distress if he or she is unable to provide such living arrangements for his or her parent(s).
Personalismo
Another characteristic of the Hispanic culture is personalismo, described as a “formal friendliness.”130 The concept suggests that adequate time is taken to establish an intimate and sustained relationship by communicating with patients in an open and a caring manner.130,144 Personalismo repeatedly has been found to be an important element in culturally competent encounters.119 A major aspect of personalismo is respeto, which refers to a tendency to respect generational hierarchies, giving more value to the opinions of elders; it is a broader construct in which respectful behavior toward peers is also important. Respeto influences parenting practices, because Hispanic parents tend to perceive the autonomy and individualism within Anglo-American culture as being in direct opposition to those cultural values of respect and generational deference.145 Similarly, Hispanic patients may not make a decision without having family present when the doctor speaks and may cede autonomy to family members or even to the doctor in important life decisions.
Marianismo and Machismo (Gender Roles)
Among most Hispanic subgroups, gender roles are clearly defined and often originate from the influence of Catholicism. The patriarchal authority characterizes the male role along a spectrum of machismo. On the one hand, machismo carries with it a positive quality of the honorable and responsible man who must always provide for and protect his family, friends, and community. This interpretation of the concept has been used to underpin spouse/partner leadership in risk reduction behavior.146–148 On the other hand, the negative consequences of machismo include domestic violence, infidelity, and high-risk behaviors.146
Matriarchal female roles are very prominent and important in Hispanic culture and are governed by norms conveyed through the concept of marianismo. Marianismo presents an idealized concept in which women are supposed to be virtuous, humble, and spiritually superior to men while also being submissive to the demands of men and to withstand extreme sacrifices and suffering for the sake of the family, frequently prioritizing family responsibilities over self-care.149–151 Hispanic adolescent females generally have positive perceptions of their ethnic background.152 This strong identification of Hispanic gender roles may play an important role in engaging in health behaviors that reduce CVD risk factors.
Faith, Spirituality, and Religious Values
Religion remains an important part of the Hispanic community.153 Ninety-one percent of Hispanics report some religious affiliation, with Roman Catholic affiliation being the most common (56%), although Protestant denominations are embraced by 23%.154 Hispanics value having a sense of spirituality and often prioritize achieving spiritual goals over material satisfaction. As such, Hispanics are often religious, and their way of expressing religious worship is often different from that of the US dominant culture.139 Hispanics are more likely to see a link between body, mind, and spiritual health. A consequence of spirituality is a sense of fatalism or destino in which life experiences, events, and adversities are inevitable and cannot be controlled or prevented. Such thinking leads to the fatalistic attitude that “whatever God wants, shall be” (“lo que Dios quiera”). Fatalistic beliefs have been correlated with a variety of negative health outcomes, including CVD,155 as well as protective factors that reduce drug abuse among Hispanic youths.139,156,157 Because religious networks and norms sometimes help to guide health behaviors, there is evidence that the deployment of interventions at Hispanic churches can serve as a motivating source of health education and fellowship, similar to what has occurred in the NHB community.158,159
Psychosocial Factors Affecting CVD Risks and Health Behaviors
Acculturation
Acculturation is defined as the process of adaptation to a new culture assessed by the integration into the new country’s cultural values, behaviors, beliefs, and attitudes.160 Researchers have categorized acculturation into 4 components,161 as follows: (1) Integration—maintaining attitudes and behaviors from the original culture but also adopting values and behaviors of the dominant culture; (2) assimilation–entirely adopting the values and behaviors of the dominant culture; (3) separation—rejecting the ways of the dominant culture and keeping the cultural practices and behaviors of the original culture; and (4) marginalization—not identifying with the original culture or the dominant/mainstream culture.162 The associated stress of cultural adaptation, as well as the concomitant behavioral changes, renders acculturation a significant explanatory variable related to CVH among Hispanics.163 Within the US Hispanic population, increasing numbers experience the acculturative process to US society, with the potential for a large impact on CVH and CVD risk.
The measurement of acculturation in research is challenging and thus far has been criticized for being too linear, relying heavily on English language use and acquisition and failing to consider the social and cultural experiences, such as living in economically deprived areas or racially/ethnically segregated neighborhoods that modify health behaviors as Hispanics acculturate.162,164–169 Additionally, most acculturation measures do not capture the fluidity of the acculturative process or the psychosocial components, such as vulnerability (eg, stress) or resilience factors (eg, social support), that may operate throughout. Given that several acculturation scales were created for or tested only in individual Hispanic subgroups (eg, the Acculturation Rating Scale for Mexican Americans II170), they may not capture the diversity of cultures within the Hispanic population and may not be generalizable to other Hispanic subgroups. Measurement of the level of acculturation is also challenging because as the United States becomes more diverse and multicultural, the “mainstream” society becomes more diverse and complex.168,171 The global dissemination and incorporation of Western lifestyle and behaviors throughout the globe further complicate our understanding and measurement of acculturation within the United States.
Despite these difficulties, a wealth of data shows that there are relationships between acculturation and coronary heart disease (CHD) risk factors. Epidemiological studies rely on proxy markers for acculturation, which include English language fluency, place of birth, length of time in the United States, age at time of immigration, generational status, and language spoken at home. Comprehensive reviews of health outcomes show strong negative effects of increasing acculturation on cardiovascular risk factors but positive effects on use of preventive health services, including screening.172–180 Some survey data show worsening CVD risk factors, including obesity, that increase with length of residency in the United States.172,180–182 Additionally, Spanish-speaking, less acculturated Hispanics report less use of preventive healthcare services and poorer heath.103,126,183 For example, among Mexican women, the highly acculturated had higher body mass index (BMI), fat mass, fasting insulin, and diastolic blood pressure than less acculturated women.179
Acculturation and Nutritional Behaviors
A healthy diet is essential to the promotion of CVH and the prevention of chronic illness, yet diet and nutrition are culturally bound. As a result, each Hispanic group has its own distinct nutritional habits and key dishes from its country of origin, based on customs and traditional foods that are readily available in its geographic area. Overall, Hispanic diets tend to be high on fiber, relying heavily on beans and grains. Results from the 2002 BRFSS showed that NHWs consumed a higher percentage of the daily recommended allowance of fruits and vegetables, followed by Hispanics and NHBs (23.4%, 22.9%, and 21.4%, respectively).184 Among Hispanic families, 15.8% have low food security, with less access to nutritious and safe foods.185 The risks associated with food insecurity include poor dietary quality and overweight/obesity.186 Perceptions, beliefs, and attitudes about foods characterize energy intake patterns and are influenced by assimilation of the mainstream culture’s dietary patterns.187 Using nationally representative data, it was shown that US-born Hispanics consumed more unhealthy foods and had greater caloric intake than foreign-born Hispanics.188 Qualitative work suggests that Hispanic immigrants struggle to retain their cultural food traditions and consume more high-fat, high-sugar foods than they did in their home countries.189 Among less acculturated Hispanics, energy intake has repeatedly been documented as more nutritious, with less fat and more fiber consumption, lower in saturated fats and simple sugars; highly acculturated Hispanics eat fewer fruit and vegetable servings.175,190–195 Other reviews suggest that the process of acculturation does not influence food choices among Hispanic subgroups and is not related to percent fat intake or percent energy from fat.195 Inconsistencies in the relationship between acculturation and diet among Hispanics are likely confounded or misclassified because of the variety of measures of acculturation used, potential differences between Hispanic subgroups, and the relationship of SES to food choices and healthy food availability. However, research documenting changing food practices resulting from immigration shows that the primary differences between the United States and the immigrants’ native countries stem from food access: greater amounts of poor quality foods available in the United States, whereas fruits and vegetables are more accessible and more affordable in many Latin American countries.
Acculturation and Acculturative Stress
Acculturative stress, an inability to successfully navigate the immigrant process and make decisions on retaining one’s native culture while adapting to a new culture, may exert a remarkable stress on CVH behaviors and subsequent health risks.196 Recent research shows that problems such as a lack of healthcare access and social marginalization produce significant distress.197–199 Furthermore, as Hispanic individuals attempt to acculturate to the economic, social, and cultural challenges of life in the United States, they experience a high burden of stress, depression, and anxiety.175,200 For some Hispanics, Americanization includes “upstream” contributors to CVD such as an abundance of fast foods, social isolation, and increased sedentary behaviors.201–204
A contributing healthcare barrier for some Hispanics is the belief that a healthcare provider is unnecessary because they are seldom sick.27 Some of this belief originates from the payer structure of healthcare systems in parts of Latin America, along with the perceived complexity of navigating the US healthcare system. Higher levels of acculturation are not only associated with higher levels of insurance coverage, they are also associated with greater use of preventive screening.175,205,206 The mechanism through which healthcare information is obtained may pose an additional barrier to care. Although >25% report obtaining no healthcare information from medical personnel in the past year, >8 in 10 Hispanics report receiving health information from alternative sources, such as television and radio.47
The available data also illustrate the heterogeneity of effects, sometimes conflicting, when one examines the role of acculturation in CVD risk. These conflicting findings suggest that the effects of sociocultural and economic factors should not be examined in isolation.198,207 Cultural and economic assimilation into mainstream society is associated with more positive health perceptions and greater levels of physical activity.172 Healthcare disparities experienced by recent immigrants or those who are less acculturated are underpinned by the lack of insurance, poverty, and legal status.183,201 Furthermore, the increasing consumption of fast foods and the rising burden of obesity globally calls into question the “better” health of immigrants on arrival in the United States.208 Additionally, prevalence rates of adult congenital heart disease and rheumatic heart disease may be higher among immigrant populations, but this has not been well studied.
Perceived Discrimination
Research has shown that perceived discrimination or unfair treatment conceptualized as a form of social stress may be associated with health outcomes.209–211 Most studies that examined perceived racial discrimination and CVH have focused on NHBs,212–214 whereas studies on discrimination among Hispanics have focused mostly on mental health outcomes.215–217 Despite this focus, an association of perceived discrimination with CVH outcomes among Hispanics may also exist.60,218 Prevalence estimates of perceived discrimination (those who experienced some form of unfair treatment attributed to race or ethnicity) among the US Hispanic population is ≈30% to 40% but may vary by Hispanic subgroup and Hispanic race.59,102,219,220 In 1 study, perceived everyday discrimination was detrimental to the physical health of Puerto Ricans and Mexicans, but the stress-buffering effects of marriage attenuated the associations among Mexicans only.221 Another study found that there were no variations between NHBs, NHWs, and Hispanics in the inverse associations of perceived discrimination and self-reported general health.210 Coping mechanisms in response to perceived discrimination among the total Hispanic population or certain subpopulations may have similarities to or differences from those of NHBs, but this has not been studied. Validation of existing perceived discrimination instruments (mostly developed for NHBs) in Hispanics is also needed.
Social Support
Social support is the extent and conditions in which interpersonal ties and relationships are linked to the broader environmental determinants of well-being222,223 and describes both the structure of a person’s social environment (social networks and network adequacy) and the resources such environments provide (financial, instrumental, and emotional support). Social support may influence CVD/CVH factors via the pathways of influencing health behaviors and facilitating adherence to medical regimens.142,224 Social support may also buffer the adverse effects of sociocontextual factors that may contribute to both increased stress and poor cardiovascular outcomes.225,226 Although greater levels of CVD risk factors are linked to lower social support among NHBs,227–229 most studies of social support among Hispanics have inexplicably been limited to the context of physical activity, particularly among Hispanic women.230–234 In pregnant and postpartum Mexican-born women, social support is essential to the maintenance of physical activity, especially compared with women of other ethnic groups.235 Strong networks of social support are hypothesized to be instrumental in influencing Hispanic CVD/CVH outcomes, but further study is needed to support this claim.
Use of Alternative Medicines
The use and influence of complementary and alternative medicines (CAMs) on adherence to conventional medicine is complex and poorly understood. Part of the complexity stems from the fact that CAMs encompass a broad variety of treatments not typically prescribed by a medical doctor, including (1) the use of vitamins and nutritional supplements or special diets; (2) medicinal herbs or teas, homeopathic remedies, and manual therapies (sobadores); and (3) energy therapies (Reiki, biofeedback), acupuncture, and prayer. Studies suggest that the use of CAMs among Hispanics as a form of health care appears to be because of its affordability, accessibility, and familiarity, as well as concerns of patients that they were not receiving a correct diagnosis or treatment through conventional medical practice.236–238 Often, patients using CAM or folk therapies do not inform their healthcare providers about these practices.239–241 It is common to find treatments that combine CAM and mainstream medicine.242–245 This is a concern because some CAM treatments may interact with prescribed medications,237,246,247 and this can put patients at increased risk, for lack of the expected therapeutic effects or an adverse reaction.245,248
CAM studies among Hispanics reveal mixed findings. Some studies have found lower CAM use among Hispanics compared to NHWs and NHBs or minimal racial and ethnic differences in CAM use, whereas other studies have found that CAM use, particularly the use of herbal teas and plant-based substances, was the most frequently reported treatment among Hispanics.238,240,249–253 A more recent study found that CAM use was lower among NHWs and NHBs than among all Hispanics (Figure 4).254 Some studies have reported lower CAM use among foreign-born Hispanic women compared to US-born counterparts, whereas other studies found that foreign-born Mexicans had higher CAM use.251,255 Such mixed results speak to the limitations of the studies (small sample sizes or administration of surveys in English language only), but they also suggest that CAM use among Hispanics is more complex and nuanced than is currently understood.253
Figure 4.
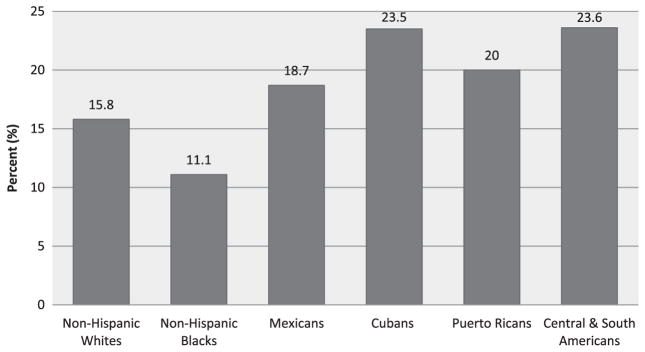
Recent use of complementary and alternative medicines across racial and ethnic groups. Data derived from the National Longitudinal Study of Adolescent Health.254
There are several cultural folk beliefs related to the origins of illnesses across diverse Hispanic subgroups that influence the use of CAM.21,256,257 There is a humoral approach to illness/ healing that emphasizes the hot-cold equilibrium in both diagnosis and treatments.183 This is expressed by the folk belief in pasmo (spasm), in which illness or death can be brought on by exposure to cold air when the body is overheated.21 One study found that 70% of the parents of Mexican descent believed in mal de ojo (evil eye), 64% in empacho, 52% in mollera caida (fallen fontanel), and 37% in susto (fright) as folk causes of illness and that 20% had taken their children to curanderos (traditional healers) for treatment of these folk illnesses.258
Prevalence of CVD Risk Factors in Hispanics
In 2010, the American Heart Association declared 2020 health strategy goals to reduce deaths attributable to CVD and stroke by 20% and to improve the CVH of all Americans by 20% by focusing on 7 key risk factors: smoking, BMI, diet, physical activity, blood pressure, blood glucose, and total cholesterol.259 In this section, we review several of these key risk factors with respect to US Hispanics. Hispanics are significantly less aware of CVD as the leading cause of death and their personal risk factors for CVD than are NHWs.260 This is important, because the first step toward prevention is awareness.
As mentioned previously in the limitations to the present report, most of the cohorts referenced below have included predominantly Mexicans as the representative Hispanic population. Despite this limitation, studies do suggest that CVD risk factor prevalence varies across Hispanic subgroups. When available, this review specifies the Hispanic subgroups examined; when Hispanic background group was not specified, we simply refer to the participants as Hispanics.
Traditional Risk Factors
Hypercholesterolemia and Hypertension
According to 2007 to 2010 NHANES data, among Mexicans ≥20 years of age, 48.1% of men and 44.7% of women have total cholesterol levels ≥200 mg/dL (of these, 15.2% and 13.5%, respectively, had levels ≥240 mg/dL), and 39.9% and 30.4% had low-density lipoprotein cholesterol (LDL-C) levels ≥130 mg/dL.261 Data from the 1982 to 1984 HHANES demonstrate variation in prevalence of hypercholesterolemia (defined by abnormal total cholesterol or LDL-C) among 3 Hispanic subgroups: Mexicans, Cubans, and Puerto Ricans. Women in each subgroup had the highest prevalence of hypercholesterolemia, with Puerto Rican women having a prevalence of 20.6%.262 In the Study of Women’s Health Across the Nation (which included 277 total Hispanics), Puerto Rican women had the highest prevalence of smoking (26.8%) but the lowest mean levels of LDL-C.263 Among 1437 Hispanic participants (56% Mexicans, 12% Dominicans, 14% Puerto Ricans, and 18% Central/South Americans) from the Multi-Ethnic Study of Atherosclerosis (MESA), Mexicans had the highest prevalence of dyslipidemia.264 For HCHS/SOL, the overall prevalence of hypercholesterolemia among Hispanic men was 51.7% and ranged from 47.6% among Dominican and Puerto Rican men to 54.9% among Central American men. Among women, the prevalence of hypercholesterolemia was 36.9% overall and ranged from 31.4% among South American women to 41% among Puerto Rican women.1,265
Despite high prevalence rates of hypercholesterolemia, disparities related to sex and race/ethnicity exist and result in substantially lower rates of treatment and control among Mexicans than among NHWs.266,267 Fewer than half of all Mexicans had been screened for high cholesterol in the previous 5 years compared with 65.2% of NHWs and 57.7% of NHBs, with fewer than half of Mexicans actually being aware that they had high cholesterol.267 The Insulin Resistance Atherosclerosis Study (IRAS) found that Hispanics tended to have more mixed dyslipidemia, with lower high-density lipoprotein cholesterol levels, higher triglyceride levels, and similar LDL-C levels compared with NHWs.268 This pattern of low high-density lipoprotein cholesterol and high triglyceride levels is a major risk factor for CVD because of its association with insulin resistance and smaller, dense, more atherogenic LDL-C particles. Adequate screening measures and treatment for this type of dyslipidemia are warranted for Hispanics.265
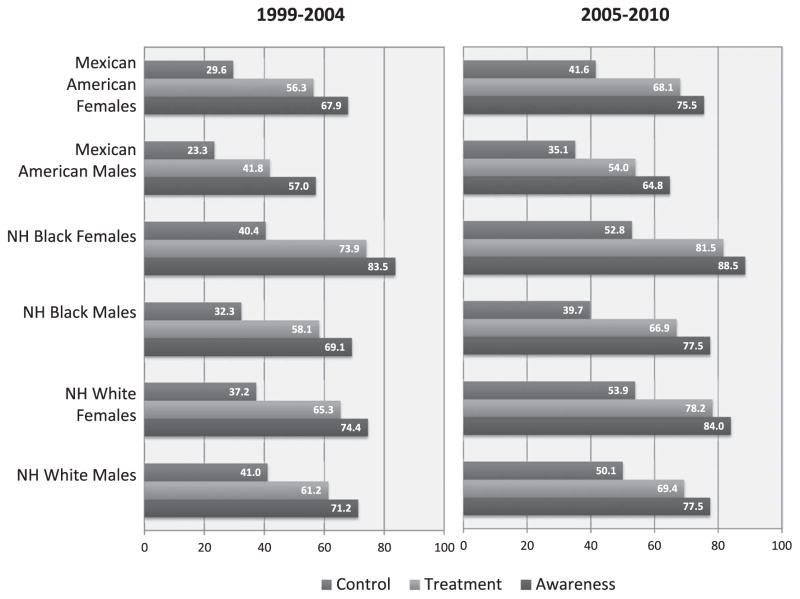
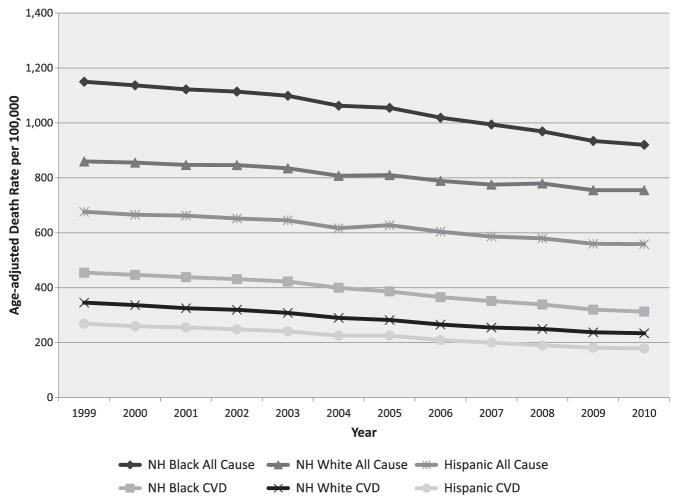
Although hypertension-related mortality rates have increased among Hispanics, and differences by Hispanic subgroup are evident,269,270 there is a remarkable lack of consistent information regarding the prevalence of hypertension among US Hispanics. Studies suggest that the prevalence of hypertension is highest in NHBs and lowest in Mexican Americans.271,272 The prevalence of hypertension among Mexicans (30.1% in males, 28.8% in females) is lower than the prevalence of hypertension in the general American population (33.0%).261 Comparison between NHANES examinations273 conducted in 1988 to 1992 and 1999 to 2000 revealed that among Mexicans, age-adjusted rates of prehypertension increased from 33.2% to 35.1%, rates of stage 1 hypertension increased from 12.4% to 14.8%, and rates of stage 2 hypertension increased from 4.2% to 5.3%. Similarly, the age-adjusted prevalence of hypertension among Mexicans increased from 17.2% in 1988 to 1991 to 20.7% in 1999 to 2000 and to 27.8% in 2003 to 2004.271,274 Over a 10-year time span, Hispanic individuals remained more likely to have undiagnosed, untreated, or uncontrolled hypertension than other ethnic groups (Figure 5).276–278
Figure 5.
Rates of hypertension awareness, treatment, and control by race/ethnicity and sex, National Health and Nutrition Examination Survey 1999 to 2004 and 2005 to 2010. NH indicates non-Hispanic. Data derived from Go et al.275
Little has been published about the prevalence of hypertension in other Hispanic subgroups. Among NHIS 1997 to 2005 respondents, in multivariate-adjusted analyses that controlled for sociodemographic and health-related factors, odds of self-reported hypertension were 67% higher among Dominicans and 20% to 27% lower among Mexicans/Mexican Americans and Central/South Americans than among NHWs.279 Among Northern Manhattan Study (NOMAS) participants (predominantly Dominican), objectively measured hypertension was similarly substantially higher in Hispanics (59%) than in NHWs (42%).54 These findings suggest that Hispanics of Dominican origin may be at particularly high risk of hypertension. Among Mexicans ≥20 years of age, 27.8% of men and 28.9% of women have high blood pressure, with Puerto Rican Americans having the highest hypertension-related death rate of all Hispanic-background groups (154.0/100 000) and Cuban Americans having the lowest (82.5/100 000).269 Among foreign-born Hispanics who responded to the NHIS, those of Puerto Rican and Dominican origin had higher hypertension prevalence than those of Mexican origin.280 Among MESA participants, Dominicans had the highest rates of hypertension.264 Similar high rates of hypertension among Dominicans have been documented in HCHS/SOL. The overall prevalence of hypertension among Hispanic men was 25.4%, with the highest proportion among Dominicans (32.6%) and the lowest among South American men (19.9%). Among Hispanic women, the prevalence of hypertension was slightly lower (23.5%) and was highest among Puerto Rican women (29.1%) and lowest among South American women (15.9%).1 In the HCHS/SOL, of those with hypertension, 82% were aware of their hypertension, 50% were receiving treatment, and only 32% of those treated had their hypertension under control.281
A country-of-origin effect on hypertension and hypercholesterolemia remained regardless of nativity (US versus foreign born) among Hispanics. Crimmins and colleagues,282 using data from the NHANES with adjustment for SES, found that US-born Mexican Americans had worse CVD risk profiles than NHWs and foreign-born Mexican Americans (the latter 2 groups had similar risk profiles). A report examining the cross-sectional relationships between acculturation measures and cholesterol levels among Hispanic MESA participants showed that preferential Spanish-speaking Hispanics had a significantly higher LDL-C than preferential English-speaking Hispanics and that those who had lived a greater proportion of their life in the United States also had higher LDL-C.163
Diabetes Mellitus
Type 2 diabetes mellitus prevalence is found to be consistently higher among Hispanics than among NHWs.283 Major surveys (NHANES, BRFSS) show that the prevalence of diabetes mellitus is twice as high among Hispanics as among NHWs.283 Hispanics are also 1.5 times more likely to die of diabetes mellitus than NHWs.284 People of Hispanic descent currently lead the epidemic of diabetes mellitus in the United States, particularly in areas of south Florida, Texas, and California.285 The prevalence of physician-diagnosed diabetes mellitus was 11% in Mexican men and 12.7% in Mexican women; an additional 6.3% and 3.8% were estimated to have undiagnosed diabetes mellitus (fasting plasma glucose ≥126 mg/dL).269 The higher incidence of diabetes mellitus among Mexicans is attributable to a large extent to a higher prevalence of insulin resistance.286 Among HHANES participants, the age-standardized prevalence of diagnosed and undiagnosed diabetes was similar for Mexicans and Puerto Ricans (≈13%) but lower among Cubans (9.3%).287 In the NHIS, rates of self-reported diabetes mellitus were higher among Puerto Ricans and Mexicans (11% and 10%), whereas Cubans, Dominicans, and Central/South Americans had a lower prevalence.280 Among MESA participants, Mexicans had the highest prevalence of diabetes mellitus.264 HCHS/SOL documented a higher prevalence of diabetes mellitus among Hispanic women (17.2%) than among Hispanic men (16.7%).1 The prevalence of diabetes mellitus was highest among Mexican men, Mexican women, and Puerto Rican women (19%); both South American men and women had the lowest prevalence of diabetes mellitus (10%).
Glycemic control is worse in Hispanics than in NHWs, and Hispanics are more likely to have undiagnosed diabetes mellitus than NHBs and NHWs.288 Although diabetes mellitus prevalence also varied by educational attainment among all Hispanic subgroups, it remained higher among Mexican participants compared with NHWs irrespective of their level of education.289 Not only is the burden of diabetes mellitus higher for Hispanics, the profile of diabetes mellitus-related complications in Hispanics (compared with NHWs) is variable: Chronic kidney disease and retinopathy are more prevalent, whereas CVD morbidity and mortality are lower, although increasing acculturation leads to higher mortality.283 Although inadequate healthcare insurance in part explains the diagnosis rates and glycemic control rates among Hispanics, the lack of glycemic control may be influenced by additional factors such as health literacy levels, poor access to culturally appropriate educational materials, and inadequate patient-provider communication.
Using American Diabetes Association criteria of fasting plasma glucose of 100 to <126 mg/dL, among Mexicans, the prevalence of prediabetes is currently 44.9% in men and 34.3% in women.269 One explanation for the high rates of diabetes mellitus and prediabetes among certain Hispanic subgroups is the possibility of a genetic predisposition to insulin resistance283,290 among Hispanics compared with NHWs. A higher prevalence of insulin resistance and diabetes mellitus has been found among relatively healthy community populations of young Hispanics and Hispanic children.291–293 The Corpus Christi Child Heart Study found significantly higher fasting insulin and glucose concentrations among Mexican children compared with NHW children.265,294 The high prevalence of diabetes mellitus and insulin resistance found in Native American populations has led some to propose a unifying genetic explanation attributable to the Amerindian ancestral composition of Mexicans,296 but such genetic associations have not yet been confirmed and remain somewhat controversial.143 Existing evidence suggests that possible lifestyle and gene-environment interactions may contribute to the higher insulin resistance and diabetes mellitus rates among Hispanics.297
Obesity
The prevalence of obesity among Hispanic populations is generally higher than among NHW populations in the United States298,299 and has increased from 1999 to 2002.300 Among Mexican participants in NHANES 2005 to 2008, 77.5% of men and 75.1% of women were overweight/obese (BMI ≥25 kg/m2), and 31.4% of men and 43.4% of women were obese (BMI ≥30 kg/m2).269 More recent NHANES 1999 to 2010 data show even higher rates of overweight/obesity and obesity among Mexicans (81.3% and 35.6% for men and 78.5% and 44.3% for women, respectively), with significant increases in overweight and obesity from 1999 through 2010.301 Mexican HHANES participants had a higher mean BMI and higher age-adjusted prevalence of being overweight compared with Puerto Ricans and Cubans.262 Contrary to what was seen in HHANES, the prevalence of obesity (BMI ≥30 kg/m2) among HCHS/SOL participants was higher for Hispanic women (42.6%) than for men (36.5%), whereas the highest prevalence of obesity occurred among Puerto Rican men (40.9%) and women (51.4%) compared to the other Hispanic groups.1
There is limited research regarding the efficacy of dietary and weight-loss intervention in Hispanics. An important review by Lindberg and Stevens302 discussed weight-loss interventions that targeted Hispanics and concluded that most studies were limited in differentiation of Hispanic subgroups, level of acculturation, and SES. Collectively, however, these studies emphasize the importance of integrating cultural values, social support, and literacy to construct appropriate dietary interventions for Hispanics.160,304–307 Using resources from the Clinica Campesina Family Health Services, 200 Hispanic participants received an intervention that deployed a social ecological and cognitive approach to self-management of diet, physical activity, and multilevel support for behavior change.308 Short-term (6 weeks) and medium-term (6 months) outcomes showed the intervention as effective and practical in improving health behavior among low-income, preferentially Spanish-speaking participants with multiple chronic conditions.308 Secretos de la Buena Vida was a communication intervention developed for Latinas that included weekly home visits with promotoras (lay health advisors or community members who are turned to for advice or information) along with tailored mailed newsletters.309 The intervention targeted awareness and assistance with adoption of fat and fiber intake recommendations. Perceived effort, perceived support, and intervention length predicted adoption of a low-fat/high-fiber diet at 15-month follow-up, with married women being 4 times more likely to be adopters of dietary changes than single women.309 Perhaps most promising, Lindberg and colleagues310 conducted a feasibility study targeting obese, preferentially Spanish-speaking Mexican women to change diet intake behaviors. The culturally appropriate behavioral intervention included promotoras, was based on cultural adaptations, and used minimal written materials, with an emphasis on group activities, a focus on Mexican traditions and beliefs, and a skill-building approach to food measurement. Mean weight loss at 6 and 12 months was 5.3 and 7.2 kg, respectively, with a mean reduction in BMI of 4.0 and 5.5 kg/m2 from baseline to 6 and 12 months, respectively.
Smoking
Overall, the prevalence of cigarette smoking is lower for US Hispanics than for NHWs and NHBs.311,312 In 2012, among Hispanics aged ≥18 years, 16.6% of males and 7.5% of females smoked cigarettes.261 Although NHIS data from 2005 and 2010 showed significant declines in current smoking prevalence among Hispanic men and women (from 21.1% to 15.8% in men and from 11.8% to 9.0% in women),313 smoking among Hispanic men and certain Hispanic subgroups approximates or exceeds the national average.314,315 Among HHANES participants, prevalence of current cigarette smoking was highest among Mexican and Cuban men (≈43% and 42%, respectively) and Puerto Rican women (31%).262,316 Nevertheless, findings from a telephone-administered survey conducted in 1993 to 1994 were generally consistent with HHANES reports on cigarette smoking: Among US Hispanics, Puerto Rican men and women had the highest rates of current smoking, and Cuban men and women had the highest prevalence of heavy smoking (≥20 cigarettes per day).314 Only ≈26% of the survey respondents who were current smokers reported smoking ≥20 cigarettes (ie, a pack) per day, which casts doubt on the presence of substantial nicotine dependence among Hispanics.314 Moreover, the survey found no association of education and income with heavy smoking.314 Among MESA participants, Puerto Ricans had the highest rates of ever smoking.264 In HCHS/SOL, smoking prevalence was 25.7% for men, ranging from 11.1% among Dominicans to 34.7% among Puerto Ricans.1 Although smoking prevalence was lower for women (15.2%), the ranges varied widely, from 8.7% for Central American women to 31.7% among Puerto Rican women.1 Prevalence of smoking also increased with acculturation among women but not among men.317 Central American women smoked significantly less than Puerto Rican or Cuban women.263 Hispanic smokers were half as likely as NHW smokers to be advised on or offered assistance with smoking cessation.21 Biochemical verification with cotinine levels may be important for future studies of tobacco use among Hispanics, because light smokers and nondaily smokers may be particularly prevalent among Hispanics, and this particular subgroup tends to underreport cigarette consumption.318
Physical Activity
Hispanic respondents of the 2003 BRFSS had significantly lower rates of self-reported physical activity than NHWs (24.7% of Hispanics engaged in ≥30 minutes of moderate physical activity daily versus 37.3% of NHWs).311 In NHANES III, 33% and 46% of Mexican men and women, respectively, reported not participating in any leisure time physical activity.319 A report from the 2001 BRFSS examined physical activity performed during leisure time, during household activities, or for transportation; 41.6% of Hispanics met recommended activity levels, whereas 21.8% did not engage in regular moderate or vigorous activity.320 Although all Hispanics were less active than NHWs, self-reported physical activity in NHIS did vary among the Hispanic subgroups. For example, Cubans and Dominicans reported less leisure time physical activity than did Mexicans and Central/South Americans.321
These previous studies suggest Hispanics remain the most physically inactive ethnic group in the United States despite an increase in their level of leisure time physical activity during the past decade.322 In 2010, only 14.4% of Hispanics aged ≥18 years met the 2008 Federal Physical Activity Guidelines.275 Data from the NHIS showed that Hispanics were 2.09 times more likely to report inadequate levels of physical activity than NHWs.323 Older Hispanic women were classified as among the least physically active groups in the country.324,325 However, these prior studies did not account for the physical activity that occurs during normal working hours or for transportation-related physical activity. Occupational physical activity may be more important among Hispanics, because many more of them work in blue-collar than white-collar jobs, which tend to be more physically demanding.326 Although the BRFSS does not assess frequency and duration of occupational physical activity, employed respondents were asked whether their work entailed mostly standing or sitting, walking, or heavy labor or physically demanding work. With inclusion of such occupation-related activity, the prevalence ratio for meeting physical activity guidelines increased from 0.85 to 0.97 of Hispanic men and from 0.88 to 0.93 for Hispanic women compared with NHW men and women, respectively.201 Thus, previous studies that have only assessed leisure time physical activity may have underestimated levels of physical activity among Hispanic/Latino individuals. Acculturation may also play an important yet complex role. Previous research suggests that as immigrants become more acculturated, their lifestyle patterns approximate the pattern of US-born populations, experiencing a decline in physical activity, an increase in sedentary behavior, and greater consumption of calorie-rich foods.327
Combined Risk Factor Profile
Data from the 1999 to 2002 NHANES reports combined CVD risk profiles (blood pressure, metabolic and inflammatory risk) and found that although foreign-born Mexicans and NHWs had similar combined risk profiles, US-born Mexicans were at higher risk.282 HCHS/SOL recently examined the prevalence of combined adverse CVD risk factors (including hypercholesterolemia, hypertension, diabetes mellitus, obesity, and smoking) and found that the prevalence was highest among Puerto Ricans, lower SES Hispanics, and those with higher acculturation levels.1 The prevalence of ≥3 major CVD risk factors was higher for Hispanic men (21.3%) than women (17.4%). Among Hispanic subgroups, both Puerto Rican men (24.9%) and women (25.0%) had the highest prevalence of having ≥3 major CVD risk factors. Similarly, ideal CVH among Hispanics is low. Among Mexican NHANES participants, the prevalence of low CVD risk factor burden was only 7.5% in 1988 to 1994 and declined to 5.3% in 1999 to 2004.328 A Hispanic cohort of mostly Caribbean Hispanics also showed lower ideal CVH among Hispanics (3.2%) than NHWs (7.7%).329,330 Although recent results from HCHS/SOL are better than what has been documented previously, only 20.2% of Hispanic men and 29.3% of Hispanic women met ideal CVH targets.1 Table 3 presents a summary of the proportion of Hispanics who engaged in ideal CVH behaviors.
Table 3.
Prevalence of Ideal Cardiovascular Health in the US Hispanic Population
| Ideal Cardiovascular Health | Prevalence of US Hispanics Meeting Ideal Cardiovascular Health Targets |
|---|---|
| No tobacco | 76.6% Are nonsmokers331 |
| Healthy weight | 23% Have a BMI <25 kg/m2 331 |
| Healthy dietary practices | 2.5% Meet 4–5 of the 5 AHA ideal dietary components332 |
| Physically active lifestyle | 51.3% Perform ≥150 min/wk of moderate or vigorous activity combined331 |
| Adherence to healthcare recommendations (eg, hyperlipidemia/hypertension/ diabetes mellitus) | |
| Hypertension: >140/>90 mm Hg | 53.4% Ideal with BP <120/<80 mm Hg331 |
| High TC: >200 mg/dL | 59% Ideal with TC <200 mg/dL331 |
| Diabetes mellitus: >126 mg/dL | FPG: 68.9% Ideal with FPG <100 mg/dL331 |
| Early recognition and treatment of symptomatic disease | 27% Of acute Mexican American stroke patients obtain treatment within 3 h333 |
| 35% Of Hispanics recognized all 5 heart attack warning symptoms108 | |
| 46% Of Hispanics recognized all 5 stroke symptoms334 | |
| Hispanics arriving at an ED with stroke symptoms had longer waiting times to see a physician334 |
AHA indicates American Heart Association; BMI, body mass index; BP, blood pressure; ED, emergency department; FPG, fasting plasma glucose; and TC, total cholesterol.
Nontraditional Risk Factors
Coronary Artery Calcium
More than half of the Hispanic men and a third of the women from MESA were found to have some coronary calcification (Agatston score >0), although prevalence was significantly lower than in NHWs (56.5% and 34.9% for Hispanic men and women versus 70.4% and 44.6% for NHW men and women).335 With adjustment for age, education, and CVD risk factors, Hispanics had a 15% lower risk of coronary artery calcium (CAC) than NHWs, and the amount of CAC among Hispanic participants with any CAC was 74% that of NHWs.335 Similar findings were reported in a physician-referred population, that is, relative risk (RR) for any CAC among Hispanics was 0.88 (95% confidence interval [CI], 0.67–1.15) compared with NHWs.336
Data from MESA suggest that prevalence of any CAC may be higher among Mexicans than Dominicans, Puerto Ricans, or other Hispanic subgroups.264 Moreover, foreign-born Hispanics have lower CAC scores than US-born Hispanics.337 This difference was independent of SES and standard CVD risk factors (smoking, BMI, lipids, hypertension, and diabetes mellitus). Among the least acculturated people, these data found an inverse association of higher incomes with lower CAC scores, but this was reversed to a positive association (higher SES with higher CAC scores) among the more highly acculturated individuals.198 Finally, CAC scores have been found to be independent predictors of incident CHD, with magnitudes of association that are similar for NHW (hazard ratio for a major coronary event, 1.15 [95% CI, 1.02–1.29]) and Hispanic (hazard ratio, 1.17 [95% CI, 1.06–1.30]) participants.338
Carotid Intimal-Medial Thickness
Nondiabetic Hispanic participants in IRAS were found to have lower mean common carotid artery intimal-medial thickness (IMT) than NHWs (749.4 versus 776.2 μm, respectively); these differences remained significant with adjustment for CVD risk factors. However, no differences in internal carotid artery IMT were seen for Hispanics versus NHWs.339 Conversely, among MESA participants, Hispanics had similar common carotid artery IMT as NHWs (0.86 versus 0.87 mm, respectively) but slightly lower internal carotid artery IMT (1.04 versus 1.13 mm, respectively).340 Among 786 college students, Hispanics had slightly lower common carotid artery IMT values than NHWs (588.5 versus 607.5 μm, respectively).341 Regarding Hispanic subgroups in MESA, Dominicans had the lowest carotid IMT (0.89 mm) among Hispanic subgroups; values were similar for Mexicans, Puerto Ricans, and other Hispanics (0.94–0.96 mm).264
Left Ventricular Hypertrophy
Among Hispanic NHANES III participants, the prevalence of left ventricular hypertrophy (LVH) determined by ECG was lower than for other racial/ethnic groups regardless of blood pressure levels: 1.4% of Hispanic participants had LVH (versus 1.7% of NHWs and 3.8% of NHBs). Nevertheless, ECG-determined LVH was strongly and significantly associated with 10-year CVD mortality among Hispanics (hazard ratio, 2.11; 95% CI, 1.35–3.30).342 However, electrocardiography has a low sensitivity for detecting LVH (compared with echocardiography and magnetic resonance imaging), and its utility in detecting LVH has been shown to vary by ethnicity.343 The prevalence of echocardiogram-determined LVH among the mostly Caribbean Hispanic participants in NOMAS was 35.7%, significantly higher than NHWs and approximating that of NHBs.54 A small study found lower echocardiographic left ventricular mass among Mexicans than NHWs, although these differences disappeared after multivariate adjustment.344 In MESA, Caribbean Hispanics, Mexicans, and Central/South Americans were all more likely to have magnetic resonance imaging–determined LVH than NHWs (in analyses adjusted for hypertension, SES, and other covariates); the odds ratios (95% CIs) for having LVH were 1.8 (1.1–3.0), 2.2 (1.4–3.3), and 1.5 (0.7–3.1), respectively, compared with NHWs.345
CVD Risk Factors in Hispanic Youth
Since the late 1950s, when the first observations of lesions compatible with atherosclerosis in youth were made, several cohort studies made important contributions to the field by relating the presence of cardiovascular risk factors during childhood to increased risk of subclinical atherosclerosis and diabetes mellitus in young adulthood and an increased risk of premature death (before 55 years of age).346–351 In addition, racial/ethnic disparities in the distribution of CVD risk factors in youth have been described.352 In 2011, among Hispanics in grades 9 to 12, 19.5% of males and 15.2% of females smoked cigarettes. Mexican American youths were significantly more susceptible to start smoking than other racial/ethnic groups.269 Rates of smoking were higher among Hispanic 8th graders (28.0%) than among NHWs (23.7%) or NHBs (25.3%).353 The epidemic of childhood obesity has not escaped Hispanic youth.354–358 In particular, the prevalence of obesity among Hispanic children 6 to 11 years old is twice as high as the prevalence for non-Hispanic children of the same age, but among those 2 to 5 years old, it is 4 times higher than for their non-Hispanic counterparts.358 Individuals who are obese during their childhood are more likely to develop CVD and diabetes mellitus as young adults351,359 and have an increased risk for premature death.360 Compared with NHW youth, Hispanic children have higher abdominal adiposity but no differences in abnormal blood pressure, triglycerides, or high-density lipoprotein cholesterol.361 Conversely, Hispanic youth are more likely to develop glucose dysregulation than youth of other ethnicities.362 Existing data suggest that overweight and obese Hispanic children are at risk of developing metabolic syndrome, and the presence of metabolic syndrome in this higher-risk group is associated with higher IMT.363 Yet studies that follow Hispanic youth into adulthood to assess the long-term CVH implications are lacking. We could observe a greater number of Hispanics living with chronic conditions throughout their lifespans, once the generation of Hispanic children affected by the obesity epidemic reaches their adult ages.
The factors that put Hispanic children at risk of obesity are complex. Hispanic youth born outside of the United States have a lower risk of obesity than those who are US born or who moved to the United States at a very young age.364–367 To this effect, prolonged exposure to an obesogenic environment may be more relevant. Studies indicate that cost and availability of healthy foods, as well as access to resources that promote physical activity, might be important factors to curtail obesity risk in Hispanic youth.368–370 Lower parental educational achievement and living in poverty have been documented as risk factors for increased cardiometabolic burden in youth.371,372 The joint influence of parental acculturation and youth acculturation on the health risk profile of Hispanic youth needs to be evaluated in future studies.
Hispanic CVD Incidence and Prevalence
CVD is the leading cause of death among Hispanics, as it is among the rest of the US population. CVD includes coronary artery disease (CAD), also known as CHD, and incorporates other cardiac conditions (congenital heart disease, arrhythmias, and congestive heart failure). CAD or CHD is broadly referred to as ischemic heart disease and consists of conditions such as myocardial infarction, sudden cardiac death (SCD), and angina pectoris. Atherosclerotic cerebrovascular disease is a common pathogenesis of stroke. Peripheral vascular disease (PVD) includes carotid artery disease, aortic aneurysms, and intermittent claudication.
Most of the studies on the prevalence and incidence of CVD in US Hispanics have included primarily Mexicans. The greater availability of data on Mexican Americans compared with other Hispanic groups may simply reflect their larger numerical presence within the United States, but it may not be appropriate to extrapolate these data to the other Hispanic groups. Recent estimates show that the overall prevalence of CVD is 33.4% for Mexican males and 30.7% for Mexican females. This is lower than the overall prevalence for NHWs (36.6% for males and 32.4% for females) and the prevalence for NHBs (44.4% for males and 48.9% for females).275 The lack of data among the other Hispanic groups does not allow for an accurate picture regarding the overall prevalence of CVD in all Hispanics.
Ischemic Heart Disease
Incidence
A prospective study inclusive of Mexicans aged ≥65 years from 5 Southwestern states found that the 1-year age-adjusted rates for hospitalization for myocardial infarction among Mexican men and women were 427.4 and 606.1 per 100 000 people, respectively. These rates were significantly higher among Mexican males and females than among NHW males and females (276.9 and 502.6 per 100 000, respectively).373
Prevalence
The prevalence of ischemic heart disease is estimated to be 5.2% for adult Hispanics, and the prevalence of angina pectoris is estimated to be 3.5%.261,374 In the San Antonio Heart Study, the age-specific prevalence of myocardial infarction was 4.0% for Hispanic males and 2.5% for Hispanic women (versus 5.5% and 1.4%, respectively, for NHWs).375 A cross-sectional study across 5 Southwestern states estimated the prevalence of heart attacks to be 7.9% for Hispanics aged 65 to 74 years and 11.2% for those ≥75 years of age.376 The rates were higher for males (11.7%) than for females (7.6%).376 The prevalence of angiographic CAD among Hispanics aged ≥40 years ranged from 10% for those without CVD risk factors to 70% for those who had a history of diabetes mellitus, smoking, and dyslipidemia.377 In a cohort of patients referred for angiography (in the ACC-NCDR, or American College of Cardiology–National Cardiovascular Data Registry), Hispanic women had lower rates of significant CAD (45.3%) than NHWs (59%) and slightly higher rates than NHBs (41.7%).378 The prevalence of premature CAD (<40 years old) appears to be lower in the Hispanic population (20%) than among NHBs (30%) and NHWs (50%).377 HCHS/SOL found self-reported CHD prevalence for Hispanic men and women of 4.2% and 2.4%, respectively.1 Puerto Ricans reported the highest prevalence of CHD (5.0%) compared with other Hispanic subgroups.
Stroke
Incidence
The BASIC (Brain Attack Surveillance in Corpus Christi) project showed an increased incidence of stroke among Mexicans compared with NHWs in this southeast Texas community. The crude 2-year cumulative incidence (2000–2002) was 168 per 10 000 in Mexicans and 136 per 10 000 in NHWs. Specifically, Mexicans had a higher cumulative incidence of ischemic stroke at younger ages (45–59 years of age: crude rate 76 per 10 000; RR, 2.10 [95% CI, 1.64–2.69]; 60–74 years of age: crude rate 224 per 10 000; RR, 1.59 [95% CI, 1.34–1.90]). However, no difference was observed at older ages (>75 years of age: crude rate 468 per 10 000; RR, 1.15 [95% CI, 0.98–1.34]). Mexicans also had a higher incidence of intracerebral hemorrhage (25/10 000 versus 19/10 000; RR, 1.37; 95% CI, 1.04–1.80) than NHWs but nonsignificantly different rates of subarachnoid hemorrhage (5/10 000 versus 4/10 000), adjusted for age.269,379 The age-adjusted incidence of first ischemic stroke in Hispanics was 149 per 10 000 compared with 88/10 000 in NHWs according to data from NOMAS for the years 1993 to 1997. There were also significant differences in the mechanism for ischemic stroke (stroke subtypes). Intracranial atherosclerosis (atherothrombotic subtype) and lacunar (small-vessel subtype) stroke mechanisms were more common among Hispanics than cardioembolic stroke.380,381 In NOMAS, which included Hispanics of primarily Dominican, Cuban, and Puerto Rican origin, the relative rate of intracranial atherosclerotic stroke was 5.00 (95% CI, 1.69–14.76) and the relative rate of lacunar stroke was 2.32 (95% CI, 1.48–3.63) compared with NHWs.269,380 The total cost of stroke from 2005 to 2050 (in 2005 dollars) is projected to be $313 billion for Hispanics and $379 billion for NHBs.269
Prevalence
The age-adjusted prevalence of stroke among Hispanics ≥18 years of age is estimated to be 2.5%, 275 which is similar to the 2.5% prevalence rate for NHWs but lower than the 3.9% for NHBs. These rates for Hispanics are similar to those recently reported among HCHS/SOL participants (2.0% for Hispanic males, 1.2% for Hispanic females).1 The prevalence of stroke among Hispanics has remained stable during the past 5 years.382 A study among subjects aged ≥60 years found that the prevalence of stroke was higher among US-born Hispanics (6.6%) than among foreign-born Hispanic participants (4.5%).383
Heart Failure
Incidence
There are few data on incident heart failure in Hispanics. A report from MESA estimated the incidence of heart failure in Hispanics to be 3.5 per 1000 person-years compared with 2.4 per 1000 person-years in NHWs and 4.6 per 1000 person-years in NHBs.384,385 In a study in a long-term facility, 67 of 257 elderly Hispanics (26%) developed congestive heart failure at 43-month follow-up.386 Among Medicare enrollees, hospitalization for heart failure was higher among Hispanics than among NHWs.269 The age-adjusted rate for hospitalization for Hispanics was 22.4 per 10 000 per year for males and 17.6/10 000 for females.387
Prevalence
The community prevalence of heart failure among Mexicans was 1.9% for males and 1.1% for females. 275 Using the large database of hospitalized patients from the AHA’s Get With The Guidelines–Heart Failure, 1 study noted 46% of Hispanic inpatients had heart failure with preserved ejection fraction, whereas 54% had heart failure with reduced ejection fraction, compared with 55% and 45% of NHWs, respectively. Relative to NHWs, Hispanics with heart failure were more likely to be younger, to have diabetes mellitus or hypertension, and to be overweight/obese. In multivariate analysis, a 45% lower mortality risk was observed among Hispanics with heart failure with preserved ejection fraction, but not among Hispanics with heart failure with reduced ejection fraction, compared with NHWs (P=0.63).388
Peripheral Vascular Disease
Incidence
The rate of peripheral vascular revascularization procedures is lower in Hispanics than in NHWs (4 per versus 6 per 10 000 person-years).389 Of course, this could be more reflective of healthcare utilization disparities than of true differences in incident disease. Conversely, the rate of admission for lower-limb amputations is higher in Hispanics than in NHWs (3 versus 2 per 10 000 person-years).389 Only 1 study examined a relation of lower-limb amputations and diabetes mellitus prevalence among a select group of Hispanics.390 This is an area that requires further study.
Prevalence
In the community-based MESA cohort, the prevalence of an ankle-brachial index <0.9 (to define PVD) was substantially higher in NHBs (7.2%) than in NHWs (3.6%), Hispanics (2.4%), or Chinese (2.0%), with Hispanics having 51% lower odds of having PVD than NHWs after adjustment for multiple risk factors, including diabetes mellitus, smoking, and SES.391 Among primary care clinic patients, the prevalence of PVD was reported to be as high as 13.7% among Mexicans, similar to NHWs (13.5%) and less than NHBs (22.8%).392 PVD prevalence was 16% among older Hispanics in an academic hospital–based geriatric practice.393 The AHA practice guidelines for PVD do not report prevalence by ethnicity.394 A higher percentage of Native American ancestry among Hispanics was associated with lower odds of PVD compared with European ancestry.395
Sudden Cardiac Death
Incidence and Survival Rates
SCD is often a difficult outcome to study, particularly without a prior CHD diagnosis.396,397 In general, the overall age-adjusted rate for SCD was 50% higher in men than in women.396 Both SCD and lower survival rates after cardiac arrest are more common among NHBs.398 Little is known about SCD in Hispanics, and further research is needed to determine the incidence and survival rates in this population. Hispanics appear to experience lower rates of SCD than non-Hispanics.396,397 Among Hispanic subgroups, the percentages of those dying outside of the hospital or in emergency rooms of CHD were lower in Mexicans (54.0%) and Cubans (54.3%) than in Puerto Ricans (58.8%).397 Despite potential race and sex differences in incidence, SCD remains poorly understood.398 It is surprising that Hispanics appear to have less SCD despite their adverse cardiovascular risk profile. These paradoxical findings reflect the fact that there are incomplete data on Hispanics and SCD.
Hispanic Paradox
Despite the distressingly poor SES profile and cardiovascular risk profile discussed previously, some studies suggest that CVD mortality and overall mortality are lower in Hispanics than in NHWs. National Vital Statistics past and present399,400 (Figure 6) have shown that Hispanics have longer life expectancies than NHWs or NHBs, along with lower heart disease mortality.183,184 A recent study showed lower overall incident CVD rates for Hispanics than for the other racial/ethnic groups regardless of the number of ideal CVH metrics,329 with the differential cardiovascular benefit of having ideal versus poor CVH being somewhat less for Hispanics than for other racial/ethnic groups.330 This epidemiological paradox for Hispanic health outcomes was first reported in 1969 by Karno and Edgerton,402 who observed low mortality rates for Hispanics among psychiatric patients, whereas Teller and Clyburn403 in 1974 described favorable birth outcomes among Mexicans. In the early 1980s, Markides404 reinvigorated the concept of the epidemiological paradox when he focused on more favorable mortality outcomes among Hispanics than would have been expected given their risk factor profiles. In the 1990s, Sorlie et al405 coined the term Hispanic paradox, which has since been cited by many. The notion of the Hispanic paradox has become controversial and complex.406 Attempts to explain the paradox have included the salmon bias hypothesis, or the idea that Hispanics return to their country of origin to die, and consequently, US Hispanic death numbers are underestimated.407 Another perspective is the healthy migrant hypothesis, whereby Hispanics who migrate to the United States are generally healthy.408 Yet neither of these ideas fully explains the paradox.409 The current prevailing notion is that the Hispanic paradox may be moderated by psychosocial factors, including social support, optimism, and strong familial and social ties among Hispanics, all of which are thought to be stress buffering and potentially protective among Hispanics despite their higher risk profile. This remains to be clarified in further studies.
Figure 6.
Age-adjusted all-cause and cardiovascular disease (CVD) mortality rates by race/ethnicity and sex, 1999 to 2010. NH indicates non-Hispanic. CVD is defined as International Classification of Diseases, 10th Revision codes I00 through I99. Source: Centers for Disease Control and Prevention, National Center for Health Statistics, data from Compressed Mortality File 1999–2010 Series 20 No. 2P.401
The notion of the Hispanic paradox is problematic for the health of Hispanics. In the past, concerns about CVD among Hispanics in the United States were allayed by the perception that Hispanic individuals were less susceptible to CVD than the general population. Thus, the Hispanic paradox confuses risk assessment and delays the development of interventions that address the problems presented by poor CVH among the Hispanic population. However, prospective cohort studies that included Mexicans, such as the San Antonio Heart Study and the Corpus Christi Heart Project, refuted the perception of a Hispanic paradox, because evidence showed not only that the paradox may be untrue but also that mortality rates may actually be higher within the Hispanic community than for NHWs.410,411
The Hispanic paradox, if it really exists, may not apply to every Hispanic subgroup equally.406 Studies that have disaggregated the Hispanic population by national subgroup have reported varying degrees of support for the Hispanic paradox. For example, using the National Longitudinal Mortality Study, Abraído-Lanza et al409 found lower mortality hazard ratios for each of the Hispanic subgroups relative to NHWs after they accounted for age, education, and family income. Hummer412 compared all-cause mortality outcomes for 5 major Hispanic subgroups and found that only Mexicans and Central/South Americans had significantly lower mortality than NHWs. These data highlight the significant heterogeneity within the Hispanic population and demonstrate that the unique socio-cultural characteristics of the diverse Hispanic subgroups may contribute to these differential outcomes. As a result, health research that lumps all Hispanic-origin individuals into 1 category potentially masks substantial differences among the diverse Hispanic subgroups, particularly with regard to the notion of the Hispanic paradox.413
Another important consideration is the impact of acculturation on the Hispanic paradox. Data show that the longer Hispanic immigrants reside in the United States, the worse some CVD risk factors become.414 For this reason, some argue that with increasing acculturation and assimilation, this potential epidemiological paradox may attenuate over time. As Hispanic immigrants begin to resemble the host culture with regard to a number of social, economic, and health indicators, more are exposed to the increased stress of living in US communities and may adopt high-risk behaviors from the host culture such as smoking, poor diet, alcohol consumption, and substance abuse.161,415
Recommendations for Future Action
Because racial and ethnic minority groups will constitute an increasingly larger proportion of the US population in coming years, improving the CVH of these groups will support reaching the AHA’s 2020 goals. Because Hispanic individuals are the largest ethnic minority in the United States (a fact that is not expected to change within the next 20–40 years), they are uniquely important to the public health of the United States. In spite of the recognized diversity among Hispanic subgroups, relatively little research evidence is available about the cultural values and behavior that influence CVH promotion, prevention, and acceptance of treatment recommendations. In Table 4, we outline recommendations as part of a call to action around the key themes presented in the previous sections of the present statement. We also outline suggestions for healthcare providers of patients of Hispanic ethnicity in Table 5.
Table 4.
Recommendations to Improve Cardiovascular Health in Hispanics
| Recommendations for Finding Solutions | |
|---|---|
| Hispanic demographics | |
| Increase awareness of changing demographics, including diversity of Hispanic background groups |
|
| SES of the Hispanic population | |
| Reduce health disparities |
|
| Language, health literacy, and patient-provider relationships | |
| Reduce barriers in health care |
|
| Hispanics and race | |
| Increase awareness of racial diversity among Hispanics |
|
| Improve measurement of race and ethnicity to support a greater understanding of Hispanic diversity | |
| Prevalence of CVD risk factors; Hispanic CVD incidence and prevalence | |
| Increase awareness of health disparities for CVD and stroke |
|
| Emphasize workforce development to improve CVD prevention and promote CVH | |
| Hispanic paradox | |
| Highlights how little we know about Hispanics |
|
| Psychosocial factors and health behaviors | |
| Advance our understanding of the acculturative process and its potential impact on CVH of the Hispanic population |
|
| Commonalities in culture and beliefs | |
| Increase awareness of the influence of culture, including Hispanic subgroup diversity |
|
| Emphasize workforce development for a culturally competent healthcare system | |
CAM indicates complementary and alternative medicine; CVD, cardiovascular disease; CVH, cardiovascular health; SES, socioeconomic status; and USPSTF, US Preventive Services Task Force.
Table 5.
Suggestions for Care Providers of Patients of Hispanic Ethnicity
| Common Problems | Suggested Instruction |
|---|---|
| Logistical barriers to care (eg, arriving late to appointments) |
|
| Racial-language assumptions |
|
| Aggregation and stereotyping of Hispanics |
|
| Lack of accurate communication during patient interaction with Spanish-speaking patients |
|
| Patient use of alternative/folk medicine |
|
| Impact of personalismo and respeto |
|
| Impact of familism |
|
| Delivering medical news and end-of-life decisions |
|
| Counteracting fatalism during healthcare decisions |
|
The Hispanic population within the United States adds complexity to health research and healthcare delivery. The present statement has described the diversity and complexity of the Hispanic population and assessed the multiple issues that affect CVD and CVH among all subgroups of Hispanics. Our recommendations respond to the need to tailor and develop culturally relevant strategies to engage Hispanic individuals in CVH-promoting behaviors and to engage and educate healthcare providers regarding the Hispanic population for the goal of CVD risk reduction and deployment of culturally competent CVH interventions and care for Hispanics. The reduction of CVH disparities among all Americans is a centerpiece of the AHA’s 2020 goals,259 Healthy People 2020,417 the National Prevention Strategy,418 and others. As described previously, the Hispanic population aged ≥65 years is projected to grow by 328%, making Hispanics the fastest-growing aging population in the United States.20,21 There are projected growth estimates for CVD prevalence and US healthcare costs based on the changing demographics of an aging population and the increasing proportion of Hispanic individuals.419 Understanding and overcoming the challenges of successfully implementing the AHA’s 2020 Impact Goals among the US Hispanic population would result in an overall benefit in CVH nationwide and could help reduce CVD disparities for all Americans.
Footnotes
Those not born in the United States were considered generation zero, and those with 1 or both parents not born in the United States were considered first generation.
The American Heart Association makes every effort to avoid any actual or potential conflicts of interest that may arise as a result of an outside relationship or a personal, professional, or business interest of a member of the writing panel. Specifically, all members of the writing group are required to complete and submit a Disclosure Questionnaire showing all such relationships that might be perceived as real or potential conflicts of interest.
Expert peer review of AHA Scientific Statements is conducted by the AHA Office of Science Operations. For more on AHA statements and guidelines development, visit http://my.americanheart.org/statements and select the “Policies and Development” link.
Disclosures
| Writing Group Member | Employment | Research Grant | Other Research Support | Speakers’ Bureau/Honoraria | Expert Witness | Ownership Interest | Consultant/Advisory Board | Other |
|---|---|---|---|---|---|---|---|---|
| Carlos J. Rodriguez | Wake Forest University School of Medicine | NHLBI†; Robert Wood Johnson Foundation† | None | None | None | None | None | None |
| Matthew Allison | University of California San Diego | None | None | None | None | None | None | None |
| Martha L. Daviglus | Northwestern University | NIH/NHLBI† | None | None | None | None | None | None |
| Carmen R. Isasi | Albert Einstein College of Medicine | None | None | None | None | None | None | None |
| Colleen Keller | Arizona State University | None | None | None | None | None | None | None |
| Enrique C. Leira | University of Iowa | NINDS† | None | None | None | None | None | None |
| Latha Palaniappan | Palo Alto Medical Foundation Research Initiative | NIH/NIDDK† | None | None | None | None | None | None |
| Ileana L. Piña | Montefiore Einstein Medical Center | None | None | None | None | None | None | None |
| Sarah M. Ramirez | Public Health Institute | None | None | None | None | None | None | None |
| Beatriz Rodriguez | University of Hawaii | None | None | None | None | None | None | None |
| Mario Sims | University of Mississippi Medical Center | None | None | None | None | None | None | None |
| Reviewer | Employment | Research Grant | Other Research Support | Speakers’ Bureau/Honoraria | Expert Witness | Ownership Interest | Consultant/Advisory Board | Other |
|---|---|---|---|---|---|---|---|---|
| Hector Gonzalez | Michigan State University | NIH† | None | None | None | None | None | None |
| Walter Palmas | Columbia University | None | None | None | None | None | None | None |
| Rey Vivo | UCLA | None | None | None | None | None | None | None |
References
- 1.Daviglus ML, Talavera GA, Avilés-Santa ML, Allison M, Cai J, MH, Gellman M, Giachello AL, Gouskova N, Kaplan RC, LaVange L, Penedo F, Perreira K, Pirzada A, Schneiderman N, Wassertheil-Smoller S, Sorlie PD, Stamler J. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. JAMA. 2012;308:1775–1784. doi: 10.1001/jama.2012.14517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wei M, Gaskill SP, Haffner SM, Stern MP. Effects of diabetes and level of glycemia on all-cause and cardiovascular mortality: the San Antonio Heart Study. Diabetes Care. 1998;21:1167–1172. doi: 10.2337/diacare.21.7.1167. [DOI] [PubMed] [Google Scholar]
- 3.Wei M, Mitchell BD, Haffner SM, Stern MP. Effects of cigarette smoking, diabetes, high cholesterol, and hypertension on all-cause mortality and cardiovascular disease mortality in Mexican Americans: the San Antonio Heart Study. Am J Epidemiol. 1996;144:1058–1065. doi: 10.1093/oxfordjournals.aje.a008878. [DOI] [PubMed] [Google Scholar]
- 4.Office of Management and Budget. Revisions to the standards for the classification of federal data on race and ethnicity. [Accessed August 4, 2012];Federal Register Notice. 1997 Oct 30; http://www.whitehouse.gov/omb/fedreg_1997standards.
- 5.Waterston A. Are Latinos becoming “white” folk? And what that still says about race in America. Transforming Anthropol. 2006;14:133–150. [Google Scholar]
- 6.Tienda M, Mitchell F, editors. National Research Council. Multiple Origins, Uncertain Destinies: Hispanics and the American Future. Washington, DC: National Academies Press; 2006. [PubMed] [Google Scholar]
- 7.Taylor P, Lopez MH, Martínez JH, Velasco G. When Labels Don’t Fit: Hispanics and Their Views of Identity. Washington, DC: Pew Research Center; Apr 4, 2012. Pew Research Hispanic Trends Project. [Google Scholar]
- 8.Lavange LM, Kalsbeek WD, Sorlie PD, Avilés-Santa LM, Kaplan RC, Barnhart J, Liu K, Giachello A, Lee DJ, Ryan J, Criqui MH, Elder JP. Sample design and cohort selection in the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010;20:642–649. doi: 10.1016/j.annepidem.2010.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sorlie PD, Avilés-Santa LM, Wassertheil-Smoller S, Kaplan RC, Daviglus ML, Giachello AL, Schneiderman N, Raij L, Talavera G, Allison M, Lavange L, Chambless LE, Heiss G. Design and implementation of the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010;20:629–641. doi: 10.1016/j.annepidem.2010.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.US Census Bureau. [Accessed August 4, 2012];2012 Population estimates. 2013 http://www.census.gov/popest/data/national/asrh/2012/index.html.
- 11.US Census Bureau. [Accessed November 16, 2012];B05003I: Sex by age by nativity and citizenship status (Hispanic or Latino): 2009–2011 American Community Survey 3-year estimates. 2011 http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_11_3YR_B05003I&prodType=table.
- 12.US Census Bureau. [Accessed November 16, 2012];B05007: Place of birth by year of entry by citizenship status for the foreign-born population: 2009–2011 American Community Survey 3-year estimates. 2011 http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_11_3YR_B05007&prodType=table.
- 13.Passel JS, Cohn D. Unauthorized Immigrant Population: National and State Trends, 2010. Washington, DC: Pew Research Center; Feb 1, 2011. Pew Research Hispanic Trends Project. [Google Scholar]
- 14.Population Division, US Census Bureau; [Accessed October 26, 2012]. Table 4: Projections of the population by sex, race, and Hispanic origin for the United States: 2010 to 2050. NP2008-T4. Release date: August 14, 2008. http://www.census.gov/population/projections/files/summary/np2008-t4.xls. [Google Scholar]
- 15.Motel S, Patten E. The 10 Largest Hispanic Origin Groups: Characteristics, Rankings, Top Counties. Washington, DC: Pew Research Center; Jun 27, 2012. Pew Research Hispanic Trends Project. [Google Scholar]
- 16.Guzmán B. The Hispanic Population: Census 2000 Brief. Washington DC: US Census Bureau; 2001. [Google Scholar]
- 17.Motel S. Statistical Portrait of Hispanics in the United States, 2010. Washington, DC: Pew Research Center; Feb 21, 2012. [Accessed October 26, 2012]. Pew Research Hispanic Trends Project. http://www.pewhispanic.org/2012/02/21/statistical-portrait-of-hispanics-in-the-united-states-2010/ [Google Scholar]
- 18.Copen CE, Daniels K, Vespa J, Mosher WD. First marriages in the United States: data from the 2006–2010 National Survey of Family Growth. Natl Health Stat Report. 2012;49:1–21. [PubMed] [Google Scholar]
- 19.US Census Bureau. [Accessed December 3, 2012];Table AVG1: Average number of people per household, by race and Hispanic origin, marital status, age, and education of householder. 2010 http://www.census.gov/population/www/socdemo/hh-fam/cps2010.html.
- 20.He W, Sengupta M, Velkoff VA, DeBarros KA. 65+ in the United States: 2005. Washington, DC: US Government Printing Office; 2005. US Census Bureau, Current Population Reports. P23–209. [Google Scholar]
- 21.National Alliance for Hispanic Health. Delivering Health Care To Hispanics: A Manual for Providers. 3. Washington, DC: National Alliance for Hispanic Health; 2003. [Google Scholar]
- 22.Ennis SR, Ríos-Vargas M, Albert NG. The Hispanic Population: 2010. Washington DC: US Census Bureau; 2011. 2010 Census Briefs. [Google Scholar]
- 23.Kaplan GA, Keil JE. Socioeconomic factors and cardiovascular disease: a review of the literature. Circulation. 1993;88:1973–1998. doi: 10.1161/01.cir.88.4.1973. [DOI] [PubMed] [Google Scholar]
- 24.Pappas G, Queen S, Hadden W, Fisher G. The increasing disparity in mortality between socioeconomic groups in the United States, 1960 and 1986 [published correction appears in N Engl J Med. 1993;329:1139] N Engl J Med. 1993;329:103–109. doi: 10.1056/NEJM199307083290207. [DOI] [PubMed] [Google Scholar]
- 25.Everson SA, Lynch JW, Kaplan GA, Lakka TA, Sivenius J, Salonen JT. Stress-induced blood pressure reactivity and incident stroke in middle-aged men. Stroke. 2001;32:1263–1270. doi: 10.1161/01.str.32.6.1263. [DOI] [PubMed] [Google Scholar]
- 26.DeNavas-Walt C, Proctor BD, Mills RJ. Income, Poverty, and Health Insurance Coverage in the United States: 2003. Washington, DC: US Government Printing Office; 2004. pp. 60–226. US Census Bureau, Current Population Reports. P60–226. [Google Scholar]
- 27.Winkleby MA, Jatulis DE, Frank E, Fortmann SP. Socioeconomic status and health: how education, income, and occupation contribute to risk factors for cardiovascular disease. Am J Public Health. 1992;82:816–820. doi: 10.2105/ajph.82.6.816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Niner DA, Rios M. Hispanics in the United States, Puerto Rico, and the US Virgin Islands: 2000. Washington, DC: US Census Bureau; 2004. Working Paper No. 84. [Google Scholar]
- 29.US Census Bureau. Statistical Abstract of the United States: 2012. 131. Washington, DC: US Census Bureau; 2011. [Accessed October 9, 2012]. http://www.census.gov/compendia/statab. [Google Scholar]
- 30.Ryan CL, Siebens J. Educational Attainment in the United States: 2009: Population Characteristics. Washington, DC: US Government Printing Office; 2012. US Census Bureau, Current Population Reports. P20–566. [Google Scholar]
- 31.Baum S, Flores SM. Higher education and children in immigrant families. Future Child. 2011;21:171–193. doi: 10.1353/foc.2011.0000. [DOI] [PubMed] [Google Scholar]
- 32.DeNavas-Walt C, Proctor BD, Smith JC. Income, Poverty, and Health Insurance Coverage in the United States: 2011. Washington, DC: US Government Printing Office; 2012. US Census Bureau, Current Population Reports. P60–243. [Google Scholar]
- 33.Webster BH, Jr, Bishaw A. Income, Earnings, and Poverty Data From the 2006 American Community Survey. Washington, DC: US Census Bureau; 2007. US Census Bureau, American Community Survey Reports. ACS-08. [Google Scholar]
- 34.DeNavas-Walt C, Proctor BD, Smith Income JC. Poverty, and Health Insurance Coverage in the United States: 2010. Washington, DC: US Government Printing Office; 2011. US Census Bureau, Current Population Reports. P60–239. [Google Scholar]
- 35.Hispanics in the United States. US Census Bureau; [Accessed October 16, 2012]. Hispanic population of the United States: 1970 to 2050. Web site. http://www.census.gov/population/hispanic/publications/hispanics_2006.html. [Google Scholar]
- 36.Collazo SG, Ryan CL, Bauman KJ. Profile of the Puerto Rican population in United States and Puerto Rico: 2008. Paper presented at: Annual Meeting of the Population Association of America; April 15–17, 2010; Dallas, TX. [Google Scholar]
- 37.Kochhar R, Fry R, Taylor P. Wealth Gap Rises to Record Highs Between Whites, Blacks, Hispanics: Twenty-to-One. Washington, DC: Pew Research Center; Jul 26, 2011. Pew Research Social & Demographic Trends. [Google Scholar]
- 38.Oliver ML, Shapiro TM. Black Wealth/White Wealth: A New Perspective on Racial Inequality. New York, NY: Routledge; 2006. [Google Scholar]
- 39.US Department of Labor, Bureau of Labor Statistics. 2012 Civilian labor force participation rates by sex, age, race, and Hispanic origin. Dec, 2013. [Accessed June 19, 2014]. [Google Scholar]
- 40.Bergad LW, Klein HS. Hispanics in the United States: A Demographic, Social, and Economic History, 1980–2005. New York, NY: Cambridge University Press; 2010. [Google Scholar]
- 41.Friedman-Jimenez G, Ortiz J. Latino health and the work environment. In: Molina CW, Aguirre-Molina M, editors. Latino Health in the US: A Growing Challenge. Washington, DC: American Public Health Association; 1994. [Google Scholar]
- 42.Table 16: Labor force and employment status of the civilian population 16 years and over by sex and Hispanic origin type: 2010. Release date: June 2011. US Census Bureau. [Accessed October 28, 2012];Current Population Survey, Annual Social and Economic Supplement. 2010 http://www.census.gov/population/hispanic/data/2010.html.
- 43.Terrazas A. Central American immigrants in the United States. [Accessed December 3, 2012];Migr Inf Source. 2011 Jan 10; http://www.migrationpolicy.org/article/central-american-immigrants-united-states-0.
- 44.Pellegrino A. Trends in international migration in Latin America and the Caribbean. Int Soc Sci J. 2000;52:395–408. [Google Scholar]
- 45.Rosenblum MR, Brick K. US Immigration Policy and Mexican/Central American Migration Flows. Washington, DC: Migration Policy Institute; Aug, 2011. [Google Scholar]
- 46.Bloom B, Cohen RA. Summary Health Statistics for US Children: National Health Interview Survey, 2006. Hyattsville, MD: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; 2007. Vital and Health Statistics: Series 10, No. 234. DHHS publication No. (PHS) 2007-1562. [Google Scholar]
- 47.Livingston G, Minushkin S, Cohn D. Hispanics and Health Care in the United States: Access, Information and Knowledge: A Joint Pew Hispanic Center and Robert Wood Johnson Foundation Report. Washington, DC: Pew Hispanic Center; 2008. [Google Scholar]
- 48.DeVoe JE, Fryer GE, Phillips R, Green L. Receipt of preventive care among adults: insurance status and usual source of care. Am J Public Health. 2003;93:786–791. doi: 10.2105/ajph.93.5.786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gretler DD, Fumo MT, Nelson KS, Murphy MB. Ethnic differences in circadian hemodynamic profile. Am J Hypertens. 1994;7:7–14. doi: 10.1093/ajh/7.1.7. [DOI] [PubMed] [Google Scholar]
- 50.Mayet J, Chapman N, Li CK, Shahi M, Poulter NR, Sever PS, Foale RA, Thom SA. Ethnic differences in the hypertensive heart and 24-hour blood pressure profile. Hypertension. 1998;31:1190–1194. doi: 10.1161/01.hyp.31.5.1190. [DOI] [PubMed] [Google Scholar]
- 51.Magalski A, Maron BJ, Main ML, McCoy M, Florez A, Reid KJ, Epps HW, Bates J, Browne JE. Relation of race to electrocardiographic patterns in elite American football players. J Am Coll Cardiol. 2008;51:2250–2255. doi: 10.1016/j.jacc.2008.01.065. [DOI] [PubMed] [Google Scholar]
- 52.Sacco RL, Roberts JK, Boden-Albala B, Gu Q, Lin IF, Kargman DE, Berglund L, Hauser WA, Shea S, Paik MC. Race-ethnicity and determinants of carotid atherosclerosis in a multiethnic population: the Northern Manhattan Stroke Study. Stroke. 1997;28:929–935. doi: 10.1161/01.str.28.5.929. [DOI] [PubMed] [Google Scholar]
- 53.Rodriguez CJ, Jin Z, Schwartz JE, Turner-Lloveras D, Sacco RL, Di Tullio MR, Homma S. Socioeconomic status, psychosocial factors, race and nocturnal blood pressure dipping in a Hispanic cohort. Am J Hypertens. 2013;26:673–682. doi: 10.1093/ajh/hpt009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rodriguez CJ, Sciacca RR, Diez-Roux AV, Boden-Albala B, Sacco RL, Homma S, DiTullio MR. Relation between socioeconomic status, race-ethnicity, and left ventricular mass: the Northern Manhattan study. Hypertension. 2004;43:775–779. doi: 10.1161/01.HYP.0000118055.90533.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Brondolo E, Rieppi R, Kelly KP, Gerin W. Perceived racism and blood pressure: a review of the literature and conceptual and methodological critique. Ann Behav Med. 2003;25:55–65. doi: 10.1207/S15324796ABM2501_08. [DOI] [PubMed] [Google Scholar]
- 56.Contrada RJ, Ashmore RD, Gary ML, Coups E, Egeth JD, Sewell A, Ewell K, Goyal TM, Chasse V. Ethnicity-related sources of stress and their effects on well-being. Curr Dir Psychol Sci. 2000;9:136–139. [Google Scholar]
- 57.Williams D, Sternthal M. Understanding racial-ethnic disparities in health: sociological contributions. J Health Soc Behav. 2010;51(suppl):S15–S27. doi: 10.1177/0022146510383838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Golash-Boza T, Darity W. Latino racial choices: the effects of skin colour and discrimination on Latinos’ and Latinas’ racial self-identifications. Ethn Racial Stud. 2008;31:899–934. [Google Scholar]
- 59.Todorova IL, Falcon LM, Lincoln AK, Price LL. Perceived discrimination, psychological distress and health. Sociol Health Illn. 2010;32:843–861. doi: 10.1111/j.1467-9566.2010.01257.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gravlee C, Non A, Mulligan C. Genetic ancestry, social classification, and racial inequalities in blood pressure in southeastern Puerto Rico. PLoS One. 2009;4:e6821. doi: 10.1371/journal.pone.0006821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Chasteen JC. Born in Blood and Fire: A Concise History of Latin America. 1. New York, NY: Norton; 2001. [Google Scholar]
- 62.Choudhry S, Coyle NE, Tang H, Salari K, Lind D, Clark SL, Tsai HJ, Naqvi M, Phong A, Ung N, Matallana H, Avila PC, Casal J, Torres A, Nazario S, Castro R, Battle NC, Perez-Stable EJ, Kwok PY, Sheppard D, Shriver MD, Rodriguez-Cintron W, Risch N, Ziv E, Burchard EG Genetics of Asthma in Latino Americans (GALA) Study. Population stratification confounds genetic association studies among Latinos. Hum Genet. 2006;118:652–664. doi: 10.1007/s00439-005-0071-3. [DOI] [PubMed] [Google Scholar]
- 63.Manichaikul A, Palmas W, Rodriguez CJ, Peralta CA, Divers J, Guo X, Chen WM, Wong Q, Williams K, Kerr KF, Taylor KD, Tsai MY, Goodarzi MO, Sale MM, Diez-Roux AV, Rich SS, Rotter JI, Mychaleckyj JC. Population structure of Hispanics in the United States: the Multi-Ethnic Study of Atherosclerosis. PLoS Genet. 2012;8:e1002640. doi: 10.1371/journal.pgen.1002640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Newson LA. Indian population patterns in colonial Spanish America. Latin Am Res Rev. 1985;20:41–74. [Google Scholar]
- 65.Bonilla C, Parra EJ, Pfaff CL, Dios S, Marshall JA, Hamman RF, Ferrell RE, Hoggart CL, McKeigue PM, Shriver MD. Admixture in the Hispanics of the San Luis Valley, Colorado, and its implications for complex trait gene mapping. Ann Hum Genet. 2004;68:139–153. doi: 10.1046/j.1529-8817.2003.00084.x. [DOI] [PubMed] [Google Scholar]
- 66.Bonilla C, Shriver MD, Parra EJ, Jones A, Fernández JR. Ancestral proportions and their association with skin pigmentation and bone mineral density in Puerto Rican women from New York city. Hum Genet. 2004;115:57–68. doi: 10.1007/s00439-004-1125-7. [DOI] [PubMed] [Google Scholar]
- 67.Almaguer T. Race, racialization, and Latino populations in the United States. In: HoSang DM, LaBennett O, Pulido L, editors. Racial Formation in the Twenty-First Century. Berkeley and Los Angeles, CA: University of California Press; 2012. pp. 143–161. [Google Scholar]
- 68.Itzigsohn J, Dore-Cabral C. Competing identities? Race, ethnicity and panethnicity among Dominicans in the United States. Sociol Forum. 2000;15:225–247. [Google Scholar]
- 69.Marrow HB. To be or not to be (Hispanic or Latino): Brazilian racial and ethnic identity in the United States. Ethnicities. 2003;3:427–464. [Google Scholar]
- 70.Duncan B, Trejo SJ. The Complexity of Immigrant Generations: Implications for Assessing the Socioeconomic Integration of Hispanics and Asians. Bonn, Germany: Institute for the Study of Labor (IZA); 2012. Discussion paper No. 6276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Fry R, Lowell BL. The wage structure of Latino-Origin groups across generations. Ind Relations. 2006;45:147–168. [Google Scholar]
- 72.Oropesa RS, Landale NS. In search of the new second generation: alternative strategies for identifying second generation children and understanding their acquisition of English. Sociol Perspect. 1997;40:429–455. [Google Scholar]
- 73.Guisepi RA, editor. Hispanic Americans. International World History Project/World History Center; 2007. The story of Hispanics in the Americas. [Google Scholar]
- 74.Cabanas Abella O. Cubatey: Crónicas de mi inolvidable Cuba. Madrid, Spain: Cultiva Libros; 2012. [Google Scholar]
- 75.Conde YM. Operation Pedro Pan: The Untold Exodus of 14,048 Cuban Children. New York, NY: Routledge; 1999. [Google Scholar]
- 76.Ojito M. Finding Mañana: A Memoir of a Cuban Exodus. New York, NY: Penguin Press; 2005. [Google Scholar]
- 77.Treaster JB. New York Times. 1987 May 2; Downward spiral for U.S.-CUBA Ties. Times and Topics. [Google Scholar]
- 78.Buffington ST. Gale Encyclopedia of Multicultural America. Farmington Hills, MI: Gale Group; 2000. Dominican Americans. [Google Scholar]
- 79.Deleted in proof.
- 80.Motel S, Patten E. Hispanics of Dominican Origin in the United States, 2010: Statistical Profile. Washington, DC: Pew Research Center; Jun 27, 2012. Hispanic Trends Project. [Google Scholar]
- 81.Marrow HB. South America: Ecuador, Peru, Brazil, Argentina, Venezuela. In: Waters MC, Ueda R, editors. The New Americans: A Guide to Immigration Since 1965. Cambridge, MA: Harvard University Press; 2007. pp. 593–611. [Google Scholar]
- 82.Acosta YD, de la Cruz GP. The Foreign Born From Latin America and the Caribbean: 2010. Washington, DC: US Census Bureau; 2011. American Community Survey Briefs. ACSBR/10–15. [Google Scholar]
- 83.Smedley BD, Stith AY, Nelson AR, editors. Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 84.Vaquera E, Kao G. The implications of choosing “no race” on- the lience of Hispanic identity: how racial and ethnic backgrounds intersect among Hispanic adolescents. Sociol Q. 2006;47:375–396. [Google Scholar]
- 85.Stokes-Brown AK. America’s shifting color line? Reexamining determinants of Latino racial self-identification. Soc Sci Q. 2012;93:309–332. [Google Scholar]
- 86.Allen VC, Jr, Lachance C, Rios-Ellis B, Kaphingst KA. Issues in the assessment of “race” among Latinos: implications for research and policy. Hisp J Behav Sci. 2011;33:411–424. doi: 10.1177/0739986311422880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Duany J. Reconstructing racial identity: ethnicity, color, and class among Dominicans in the United States and Puerto Rico. Latin Am Perspect. 1998;25:147–172. [Google Scholar]
- 88.Nutini HG. Class and ethnicity in Mexico: somatic and racial considerations. Ethnology. 1997;36:227. [Google Scholar]
- 89.Rodriguez CE, Castro A, Garcia O, Torres A. Latino racial identity: In the eye of the beholder? Latino Stud J. 1991;2:33–48. [Google Scholar]
- 90.Karter AJ. Commentary: Race, genetics, and disease: in search of a middle ground. Int J Epidemiol. 2003;32:26–28. doi: 10.1093/ije/dyg033. [DOI] [PubMed] [Google Scholar]
- 91.Arnett DK, Rautaharju P, Crow R, Folsom AR, Ekelund LG, Hutchinson R, Tyroler HA, Heiss G. Black-white differences in electrocardiographic left ventricular mass and its association with blood pressure (the ARIC study): Atherosclerosis Risk in Communities. Am J Cardiol. 1994;74:247–252. doi: 10.1016/0002-9149(94)90365-4. [DOI] [PubMed] [Google Scholar]
- 92.González Burchard E, Borrell LN, Choudhry S, Naqvi M, Tsai HJ, Rodriguez-Santana JR, Chapela R, Rogers SD, Mei R, Rodriguez-Cintron W, Arena JF, Kittles R, Perez-Stable EJ, Ziv E, Risch N. Latino populations: a unique opportunity for the study of race, genetics, and social environment in epidemiological research. Am J Public Health. 2005;95:2161–2168. doi: 10.2105/AJPH.2005.068668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Bayles BP, Katerndahl DA. Culture-bound syndromes in Hispanic primary care patients. Int J Psychiatry Med. 2009;39:15–31. doi: 10.2190/PM.39.1.b. [DOI] [PubMed] [Google Scholar]
- 94.Falicov CJ. Commentary: on the wisdom and challenges of culturally attuned treatments for Latinos. Fam Process. 2009;48:292–309. doi: 10.1111/j.1545-5300.2009.01282.x. [DOI] [PubMed] [Google Scholar]
- 95.Linton A, Jiménez TR. Contexts for bilingualism among US-born Latinos. Ethn Racial Stud. 2009;32:967–995. [Google Scholar]
- 96.Bade BL. Is There a Doctor in the Field? Underlying Conditions Affecting Access to Health Care for California Farmworkers and Their Families. Oakland, CA: California Policy Research Center; 1999. [Google Scholar]
- 97.Kresge L. Indigenous Oaxacan Communities in California: An Overview. California Institute for Rural Studies; Nov, 2007. [Accessed November 16, 2012]. Pub 1107. http://www.cirsinc.org/publications/farm-labor. [Google Scholar]
- 98.Arriagada PA. Family context and Spanish-language use: a study of Latino children in the United States. Soc Sci Q. 2005;86:599–619. [Google Scholar]
- 99.Clément R, Noels KA, Deneault B. Interethnic contact, identity, and psychological adjustment: the mediating and moderating roles of communication. J Soc Issues. 2001;57:559–577. [Google Scholar]
- 100.Proctor CP, August D, Carlo M, Barr C. Language maintenance versus language of instruction: Spanish reading development among Latino and Latina bilingual learners. J Soc Issues. 2010;66:79–94. [Google Scholar]
- 101.Table B16005I: Nativity by language spoken at home by ability to speak English for the population 5 years and over (Hispanic or Latino): 2009–2011 American Community Survey 3-year estimates. [Accessed October 28, 2012];United States Census Web site. 2011 http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_11_3YR_B16005I&prodType=table.
- 102.Hakimzadeh S, Cohn D. English usage among Hispanics in the United States. Washington, DC: Pew Research Center; Nov 29, 2007. Pew Research Hispanic Trends Project. [Google Scholar]
- 103.DuBard C, Gizlice Z. Language spoken and differences in health status, access to care, and receipt of preventive services among US Hispanics. Am J Public Health. 2008;98:2021–2028. doi: 10.2105/AJPH.2007.119008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ponce NA, Hays RD, Cunningham WE. Linguistic disparities in health care access and health status among older adults. J Gen Intern Med. 2006;21:786–791. doi: 10.1111/j.1525-1497.2006.00491.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Pearson WS, Ahluwalia IB, Ford ES, Mokdad AH. Language preference as a predictor of access to and use of healthcare services among Hispanics in the United States. Ethn Dis. 2008;18:93–97. [PubMed] [Google Scholar]
- 106.Cheng EM, Chen A, Cunningham W. Primary language and receipt of recommended health care among Hispanics in the United States. J Gen Intern Med. 2007;22(suppl 2):283–288. doi: 10.1007/s11606-007-0346-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Grimm KA, Blanck HM. Survey language preference as a predictor of meeting fruit and vegetable objectives among Hispanic adults in the United States, Behavioral Risk Factor Surveillance System, 2009. Prev Chronic Dis. 2011;8:A133. [PMC free article] [PubMed] [Google Scholar]
- 108.DuBard CA, Garrett J, Gizlice Z. Effect of language on heart attack and stroke awareness among U.S. Hispanics. Am J Prev Med. 2006;30:189–196. doi: 10.1016/j.amepre.2005.10.024. [DOI] [PubMed] [Google Scholar]
- 109.Peterson PN, Shetterly SM, Clarke CL, Bekelman DB, Chan PS, Allen LA, Matlock DD, Magid DJ, Masoudi FA. Health literacy and outcomes among patients with heart failure. JAMA. 2011;305:1695–701. doi: 10.1001/jama.2011.512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Sentell TL, Halpin HA. Importance of adult literacy in understanding health disparities. J Gen Intern Med. 2006;21:862–866. doi: 10.1111/j.1525-1497.2006.00538.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Nutbeam D. Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promot Int. 2000;15:259–267. [Google Scholar]
- 112.Zarcadoolas C, Pleasant A, Greer DS. Understanding health literacy: an expanded model. Health Promot Int. 2005;20:195–203. doi: 10.1093/heapro/dah609. [DOI] [PubMed] [Google Scholar]
- 113.Chinn D. Critical health literacy: a review and critical analysis. Soc Sci Med. 2011;73:60–67. doi: 10.1016/j.socscimed.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 114.Nutbeam D. Defining and measuring health literacy: what can we learn from literacy studies? Int J Public Health. 2009;54:303–5. doi: 10.1007/s00038-009-0050-x. [DOI] [PubMed] [Google Scholar]
- 115.Williams MV, Parker RM, Baker DW, Parikh NS, Pitkin K, Coates WC, Nurss JR. Inadequate functional health literacy among patients at two public hospitals. JAMA. 1995;274:1677–1682. [PubMed] [Google Scholar]
- 116.Kaestle CF, Campbell A, Finn JD, Johnson ST, Mikulecky LJ. Adult Literacy and Education in America: Four Studies Based on the National Adult Literacy Survey. Washington, DC: US Department of Education, National Center for Education Statistics; 2001. NCES 2001-534. [Google Scholar]
- 117.Anderson LM, Scrimshaw SC, Fullilove MT, Fielding JE, Normand J Task Force on Community Preventive Services. Culturally competent healthcare systems: a systematic review. Am J Prev Med. 2003;24(suppl):68–79. doi: 10.1016/s0749-3797(02)00657-8. [DOI] [PubMed] [Google Scholar]
- 118.Castro A, Ruiz E. The effects of nurse practitioner cultural competence on Latina patient satisfaction. J Am Acad Nurse Pract. 2009;21:278–286. doi: 10.1111/j.1745-7599.2009.00406.x. [DOI] [PubMed] [Google Scholar]
- 119.Clark L, Redman RW. Mexican immigrant mothers’ expectations for children’s health services. West J Nurs Res. 2007;29:670–690. doi: 10.1177/0193945906297375. [DOI] [PubMed] [Google Scholar]
- 120.Gany F, Leng J, Shapiro E, Abramson D, Motola I, Shield DC, Changrani J. Patient satisfaction with different interpreting methods: a randomized controlled trial. J Gen Intern Med. 2007;22(suppl 2):312–318. doi: 10.1007/s11606-007-0360-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Cristancho S, Garces DM, Peters KE, Mueller BC. Listening to rural Hispanic immigrants in the Midwest: a community-based participatory assessment of major barriers to health care access and use. Qual Health Res. 2008;18:633–646. doi: 10.1177/1049732308316669. [DOI] [PubMed] [Google Scholar]
- 122.Derose KP. Networks of care: How Latina immigrants find their way to and through a county hospital. J Immigr Health. 2000;2:79–87. doi: 10.1023/A:1009533901752. [DOI] [PubMed] [Google Scholar]
- 123.Harari N, Davis M, Heisler M. Strangers in a strange land: health care experiences for recent Latino immigrants in Midwest communities. J Health Care Poor Underserved. 2008;19:1350–1367. doi: 10.1353/hpu.0.0086. [DOI] [PubMed] [Google Scholar]
- 124.Lopez-Quintero C, Berry EM, Neumark Y. Limited English proficiency is a barrier to receipt of advice about physical activity and diet among Hispanics with chronic diseases in the United States. J Am Diet Assoc. 2009;109:1769–74. doi: 10.1016/j.jada.2009.07.003. [DOI] [PubMed] [Google Scholar]
- 125.Tortolero-Luna G, Byrd T, Groff JY, Linares AC, Mullen PD, Cantor SB. Relationship between English language use and preferences for involvement in medical care among Hispanic women. J Womens Health (Larchmt) 2006;15:774–785. doi: 10.1089/jwh.2006.15.774. [DOI] [PubMed] [Google Scholar]
- 126.O’Brien M, Shea J. Disparities in patient satisfaction among Hispanics: the role of language preference. J Immigr Minor Health. 2011;13:408–412. doi: 10.1007/s10903-009-9275-2. [DOI] [PubMed] [Google Scholar]
- 127.Wallace LS, DeVoe JE, Heintzman JD, Fryer GE. Language preference and perceptions of healthcare providers’ communication and autonomy making behaviors among Hispanics. J Immigr Minor Health. 2009;11:453–459. doi: 10.1007/s10903-008-9192-9. [DOI] [PubMed] [Google Scholar]
- 128.Villagran M, Hajek C, Zhao X, Peterson E, Wittenberg-Lyles E. Communication and culture: predictors of treatment adherence among Mexican immigrant patients. J Health Psychol. 2012;17:443–452. doi: 10.1177/1359105311417194. [DOI] [PubMed] [Google Scholar]
- 129.Cross TL, Bazron BJ, Dennis KW, Isaccs MR. Towards a Culturally Competent System of Care. Vol. 1. Washington, DC: National Institute of Mental Health Child and Adolescent Service System Program (CASSP); 1989. [Google Scholar]
- 130.Warda MR. Mexican Americans’ perceptions of culturally competent care. West J Nurs Res. 2000;22:203–224. doi: 10.1177/01939450022044368. [DOI] [PubMed] [Google Scholar]
- 131.Pérez-Stable EJ, Nápoles-Springer A, Miramontes JM. The effects of ethnicity and language on medical outcomes of patients with hypertension or diabetes. Med Care. 1997;35:1212–1219. doi: 10.1097/00005650-199712000-00005. [DOI] [PubMed] [Google Scholar]
- 132.Sabogal F, Marín G, Otero-Sabogal R, Marín BV, Perez-Stable E. Hispanic familism and acculturation: what changes and what doesn’t. Hisp J Behav Sci. 1987;9:397–412. [Google Scholar]
- 133.Schwartz SJ. The applicability of familism to diverse ethnic groups: a preliminary study. J Soc Psychol. 2007;147:101–118. doi: 10.3200/SOCP.147.2.101-118. [DOI] [PubMed] [Google Scholar]
- 134.Almeida J, Molnar BE, Kawachi I, Subramanian SV. Ethnicity and nativity status as determinants of perceived social support: testing the concept of familism. Soc Sci Med. 2009;68:1852–1858. doi: 10.1016/j.socscimed.2009.02.029. [DOI] [PubMed] [Google Scholar]
- 135.Abraído-Lanza AF, Guier C, Revenson TA. Coping and social support resources among Latinas with arthritis. Arthritis Care Res. 1996;9:501–508. doi: 10.1002/art.1790090612. [DOI] [PubMed] [Google Scholar]
- 136.Davila YR, Reifsnider E, Pecina I. Familismo: influence on health behaviors. Appl Nurs Res. 2011;24:e67–e72. doi: 10.1016/j.apnr.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 137.Sherraden MS, Barrera RE. Prenatal care experiences and birth weight among Mexican immigrant women. J Med Syst. 1996;20:329–350. doi: 10.1007/BF02257044. [DOI] [PubMed] [Google Scholar]
- 138.Suarez L. Pap smear and mammogram screening in Mexican-American women: the effects of acculturation. Am J Public Health. 1994;84:742–746. doi: 10.2105/ajph.84.5.742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Torres V. La familia as locus theologicus and religious education in lo cotidiano [daily life] Relig Educ. 2010;105:444–461. [Google Scholar]
- 140.Ramirez JR, Crano WD, Quist R, Burgoon M, Alvaro EM, Grandpre J. Acculturation, familism, parental monitoring, and knowledge as predictors of marijuana and inhalant use in adolescents. Psychol Addict Behav. 2004;18:3–11. doi: 10.1037/0893-164X.18.1.3. [DOI] [PubMed] [Google Scholar]
- 141.Rodriguez N, Mira CB, Paez ND, Myers HF. Exploring the complexities of familism and acculturation: central constructs for people of Mexican origin. Am J Community Psychol. 2007;39:61–77. doi: 10.1007/s10464-007-9090-7. [DOI] [PubMed] [Google Scholar]
- 142.Uchino BN. Social support and health: a review of physiological processes potentially underlying links to disease outcomes. J Behav Med. 2006;29:377–387. doi: 10.1007/s10865-006-9056-5. [DOI] [PubMed] [Google Scholar]
- 143.Santisteban DA, Muir-Malcolm JA, Mitrani VB, Szapocznik J. Integrating the study of ethnic culture and family psychology intervention science. In: Liddle HA, Levant RF, Santisteban DA, Bray JH, editors. Family Psychology: Science-Based Interventions. Washington, DC: American Psychological Association; 2002. pp. 331–352. [Google Scholar]
- 144.Bermúdez JM, Kirkpatrick DR, Hecker L, Torres-Robles C. Describing Latinos families and their help-seeking attitudes: challenging the family therapy literature. Contemp Fam Ther. 2010;32:155–172. [Google Scholar]
- 145.Calzada EJ, Fernandez Y, Cortes DE. Incorporating the cultural value of respeto into a framework of Latino parenting. Cultur Divers Ethnic Minor Psychol. 2010;16:77–86. doi: 10.1037/a0016071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Galanti GA. The Hispanic Family and Male-Female Relationships: An Overview. J Transcult Nurs. 2003;14:180–185. doi: 10.1177/1043659603014003004. [DOI] [PubMed] [Google Scholar]
- 147.Keller C, Records K, Ainsworth B, Belyea M, Permana P, Coonrod D, Vega-Lopez S, Nagle-Williams A. Madres para la Salud: design of a theory-based intervention for postpartum Latinas. Contemp Clin Trials. 2011;32:418–427. doi: 10.1016/j.cct.2011.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Torres JB, Solberg VS, Carlstrom AH. The myth of sameness among Latino men and their machismo. Am J Orthopsychiatry. 2002;72:163–181. doi: 10.1037/0002-9432.72.2.163. [DOI] [PubMed] [Google Scholar]
- 149.D’Alonzo KT. The influence of marianismo beliefs on physical activity of immigrant Latinas. J Transcult Nurs. 2012;23:124–133. doi: 10.1177/1043659611433872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Castillo LG, Caver KA. Expanding the concept of acculturation in Mexican American rehabilitation psychology research and practice. Rehabil Psychol. 2009;54:351–362. doi: 10.1037/a0017801. [DOI] [PubMed] [Google Scholar]
- 151.Castillo LG, Cano M. Mexican American psychology: theory and clinical application. In: Negy C, editor. Cross-Cultural Psychotherapy: Toward a Critical Understanding of Diverse Client Populations. Reno, NV: Bent Tree Press; 2007. pp. 85–102. [Google Scholar]
- 152.Charmaraman L, Grossman JM. Importance of race and ethnicity: an exploration of Asian, Black, Latino, and multiracial adolescent identity. Cultur Divers Ethnic Minor Psychol. 2010;16:144–151. doi: 10.1037/a0018668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Edwards LM, Haglund K, Fehring RJ, Pruszynski J. Religiosity and sexual risk behaviors among Latina adolescents: trends from 1995 to 2008. J Womens Health (Larchmt) 2011;20:871–877. doi: 10.1089/jwh.2010.1949. [DOI] [PubMed] [Google Scholar]
- 154.Kelly NJ, Kelly JM. Religion and Latino partisanship in the United States. Polit Res Q. 2005;58:87–95. [Google Scholar]
- 155.Urizar GG, Jr, Sears SF., Jr Psychosocial and cultural influences on cardiovascular health and quality of life among Hispanic cardiac patients in South Florida. J Behav Med. 2006;29:255–268. doi: 10.1007/s10865-006-9050-y. [DOI] [PubMed] [Google Scholar]
- 156.Heathcote JD, West JH, Hall PC, Trinidad DR. Religiosity and utilization of complementary and alternative medicine among foreign-born Hispanics in the United States. Hisp J Behav Sci. 2011;33:398–408. [Google Scholar]
- 157.Hodge DR, Marsiglia FF, Nieri T. Religion and substance use among youths of Mexican heritage: a social capital perspective. Soc Work Res. 2011;35:137–146. doi: 10.1093/swr/35.3.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Jurkowski JM, Kurlanska C, Ramos BM. Latino women’s spiritual beliefs related to health. Am J Health Promot. 2010;25:19–25. doi: 10.4278/ajhp.080923-QUAL-211. [DOI] [PubMed] [Google Scholar]
- 159.Castro F, Elder J, Coe K, Tafoya-Barraza HM, Moratto S, Campbell N, Talavera G. Mobilizing churches for health promotion in Latino communities: Compañeros en la Salud. J Natl Cancer Inst Monogr. 1995;1995:127–135. [PubMed] [Google Scholar]
- 160.Giachello AL. The health of Latinas. In: Aguirre-Molina M, Molina CW, Zambrana RE, editors. Health Issues in the Latino Community. San Francisco, CA: Jossey-Bass; 2001. [Google Scholar]
- 161.Berry JW. Conceptual approaches to acculturation. In: Chun KM, Organista PB, Marin G, editors. Acculturation: Advances in Theory, Measurement and Applied Research. Washington, DC: American Psychological Association; 2003. pp. 17–38. [Google Scholar]
- 162.Thomson MD, Hoffman-Goetz L. Defining and measuring acculturation: a systematic review of public health studies with Hispanic populations in the United States. Soc Sci Med. 2009;69:983–991. doi: 10.1016/j.socscimed.2009.05.011. [DOI] [PubMed] [Google Scholar]
- 163.Eamranond PP, Legedza AT, Diez-Roux AV, Kandule NR, Palmas W, Siscovick DS, Makamal KJ. Association between language and risk factor levels among Hispanic adults with hypertension, hypercholesterolemia, or diabetes. Am Heart J. 2009;157:53–59. doi: 10.1016/j.ahj.2008.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Acevedo-Garcia D, Sanchez-Vaznaugh EV, Viruell-Fuentes EA, Almeida J. Integrating social epidemiology into immigrant health research: a cross-national framework. Soc Sci Med. 2012;75:2060–2068. doi: 10.1016/j.socscimed.2012.04.040. [DOI] [PubMed] [Google Scholar]
- 165.Viruell-Fuentes EA. Beyond acculturation: immigration, discrimination, and health research among Mexicans in the United States. Soc Sci Med. 2007;65:1524–1535. doi: 10.1016/j.socscimed.2007.05.010. [DOI] [PubMed] [Google Scholar]
- 166.Viruell-Fuentes EA, Miranda PY, Abdulrahim S. More than culture: structural racism, intersectionality theory, and immigrant health. Soc Sci Med. 2012;75:2099–2106. doi: 10.1016/j.socscimed.2011.12.037. [DOI] [PubMed] [Google Scholar]
- 167.Zambrana RE, Carter-Pokras O. Role of acculturation research in advancing science and practice in reducing health care disparities among Latinos. Am J Public Health. 2010;100:18–23. doi: 10.2105/AJPH.2008.138826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Hunt LM, Schneider S, Comer B. Should “acculturation” be a variable in health research? A critical review of research on US Hispanics. Soc Sci Med. 2004;59:973–86. doi: 10.1016/j.socscimed.2003.12.009. [DOI] [PubMed] [Google Scholar]
- 169.Hazuda HP, Haffner SM, Stern MP, Eifler CW. Effects of acculturation and socioeconomic status on obesity and diabetes in Mexican Americans: the San Antonio Heart Study. Am J Epidemiol. 1988;128:1289–1301. doi: 10.1093/oxfordjournals.aje.a115082. [DOI] [PubMed] [Google Scholar]
- 170.Cuellar I, Arnold B, Maldonado R. Acculturation rating scale for Mexican Americans-II: a revision of the original ARSMA scale. Hisp J Behav Sci. 1995;17:275–304. [Google Scholar]
- 171.Abraído-Lanza AF, Armbrister AN, Flórez KR, Aguirre AN. Toward a theory-driven model of acculturation in public health research. Am J Public Health. 2006;96:1342–1346. doi: 10.2105/AJPH.2005.064980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Abraído-Lanza AF, Chao MT, Flórez KR. Do healthy behaviors decline with greater acculturation? Implications for the Latino mortality paradox. Soc Sci Med. 2005;61:1243–1255. doi: 10.1016/j.socscimed.2005.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Ghaddar S, Brown CJ, Pagán JA, Díaz V. Acculturation and healthy lifestyle habits among Hispanics in United States-Mexico border communities. Rev Panam Salud Publica. 2010;28:190–197. doi: 10.1590/s1020-49892010000900009. [DOI] [PubMed] [Google Scholar]
- 174.Jurkowski JM, Mosquera M, Ramos B. Selected cultural factors associated with physical activity among Latino women. Womens Health Issues. 2010;20:219–226. doi: 10.1016/j.whi.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 175.Lara M, Gamboa C, Kahramanian MI, Morales LS, Bautista DE. Acculturation and Latino health in the United States: a review of the literature and its sociopolitical context. Annu Rev Public Health. 2005;26:367–97. doi: 10.1146/annurev.publhealth.26.021304.144615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Morales LS, Leng M, Escarce JJ. Risk of cardiovascular disease in first and second generation Mexican-Americans. J Immigr Minor Health. 2011;13:61–68. doi: 10.1007/s10903-009-9262-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Moran A, Diez Roux AV, Jackson SA, Kramer H, Manolio TA, Shrager S, Shea S. Acculturation is associated with hypertension in a multiethnic sample. Am J Hypertens. 2007;20:354–363. doi: 10.1016/j.amjhyper.2006.09.025. [DOI] [PubMed] [Google Scholar]
- 178.Pichon LC, Arredondo EM, Roesch S, Sallis JF, Ayala GX, Elder JP. The relation of acculturation to Latinas’ perceived neighborhood safety and physical activity: a structural equation analysis. Ann Behav Med. 2007;34:295–303. doi: 10.1007/BF02874554. [DOI] [PubMed] [Google Scholar]
- 179.Vella CA, Ontiveros D, Zubia RY, Bader JO. Acculturation and metabolic syndrome risk factors in young Mexican and Mexican-American women. J Immigr Minor Health. 2011;13:119–126. doi: 10.1007/s10903-009-9299-7. [DOI] [PubMed] [Google Scholar]
- 180.Wolin KY, Colangelo LA, Chiu BC, Gapstur SM. Obesity and immigration among Latina women. J Immigr Minor Health. 2009;11:428–431. doi: 10.1007/s10903-007-9115-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Koya D, Egede LE. Association between length of residence and cardiovascular disease risk factors among an ethnically diverse group of United States immigrants. J Gen Intern Med. 2007;22:841–846. doi: 10.1007/s11606-007-0163-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Yeh MC, Viladrich A, Bruning N, Roye C. Determinants of Latina obesity in the United States: the role of selective acculturation. J Transcult Nurs. 2009;20:105–115. doi: 10.1177/1043659608325846. [DOI] [PubMed] [Google Scholar]
- 183.Askim-Lovseth M, Aldana A. Looking beyond “affordable” health care: cultural understanding and sensitivity-necessities in addressing the health care disparities of the U.S. Hispanic population. Health Mark Q. 2010;27:354–387. doi: 10.1080/07359683.2010.519990. [DOI] [PubMed] [Google Scholar]
- 184.Behavioral Risk Factor Surveillance System: BRFSS 2002 survey data and documentation. Centers for Disease Control and Prevention; [Accessed August 4, 2012]. Web site http://www.cdc.gov/brfss/annual_data/annual_2002.htm. [Google Scholar]
- 185.Coleman-Jensen A, Nord M, Singh A. Household food security in the United States in 2012. Washington, DC: US Department of Agriculture, Economic Research Service; 2013. Report No. ERR-155. [Google Scholar]
- 186.Dhokarh R, Himmelgreen DA, Peng YK, Segura-Pérez S, Hromi-Fiedler A, Pérez-Escamilla R. Food insecurity is associated with acculturation and social networks in Puerto Rican households. J Nutr Educ Behav. 2011;43:288–294. doi: 10.1016/j.jneb.2009.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Lin H, Bermudez OI, Tucker KL. Dietary patterns of Hispanic elders are associated with acculturation and obesity. J Nutr. 2003;133:3651–3657. doi: 10.1093/jn/133.11.3651. [DOI] [PubMed] [Google Scholar]
- 188.Mainous AG, 3rd, Diaz VA, Geesey ME. Acculturation and healthy lifestyle among Latinos with diabetes. Ann Fam Med. 2008;6:131–137. doi: 10.1370/afm.814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.McArthur LH, Anguiano RPV, Nocetti D. Maintenance and change in the diet of Hispanic immigrants in eastern North Carolina. Fam Consum Sci Res J. 2001;29:309–335. [Google Scholar]
- 190.Bermúdez OI, Falcón LM, Tucker KL. Intake and food sources of macro-nutrients among older Hispanic adults: association with ethnicity, acculturation, and length of residence in the United States. J Am Diet Assoc. 2000;100:665–673. doi: 10.1016/s0002-8223(00)00195-4. [DOI] [PubMed] [Google Scholar]
- 191.Dixon LB, Sundquist J, Winkleby M. Differences in energy, nutrient, and food intakes in a US sample of Mexican-American women and men: findings from the Third National Health and Nutrition Examination Survey, 1988–1994. Am J Epidemiol. 2000;152:548–557. doi: 10.1093/aje/152.6.548. [DOI] [PubMed] [Google Scholar]
- 192.Guendelman S, Abrams B. Dietary intake among Mexican-American women: generational differences and a comparison with white non-Hispanic women. Am J Public Health. 1995;85:20–25. doi: 10.2105/ajph.85.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Neuhouser ML, Thompson B, Coronado GD, Solomon CC. Higher fat intake and lower fruit and vegetables intakes are associated with greater acculturation among Mexicans living in Washington State. J Am Diet Assoc. 2004;104:51–57. doi: 10.1016/j.jada.2003.10.015. [DOI] [PubMed] [Google Scholar]
- 194.Pérez-Escamilla R. Acculturation, nutrition, and health disparities in Latinos. Am J Clin Nutr. 2011;93:1163–1167. doi: 10.3945/ajcn.110.003467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Ayala GX, Baquero B, Klinger S. A systematic review of the relationship between acculturation and diet among Latinos in the United States: implications for future research. J Am Diet Assoc. 2008;108:1330–1344. doi: 10.1016/j.jada.2008.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Guarnaccia P, Martinez I. Comprehensive In-Depth Literature Review and Analysis of Hispanic Mental Health Issues With Specific Focus on Members of the Following Ethnic Groups: Cubans, Dominicans, Mexicans and Puerto Ricans. Mercerville, NJ: New Jersey Mental Health Institute; 2002. [Google Scholar]
- 197.Cervantes RC, Goldbach JT, Padilla AM. Using Qualitative Methods for Revising Items in the Hispanic Stress Inventory. Hisp J Behav Sci. 2012;34:208–331. [Google Scholar]
- 198.Gallo LC, de Los Monteros KE, Allison M, Diez Roux A, Polak JF, Watson KE, Morales LS. Do socioeconomic gradients in subclinical atherosclerosis vary according to acculturation level? Analyses of Mexican-Americans in the Multi-Ethnic Study of Atherosclerosis. Psychosom Med. 2009;71:756–762. doi: 10.1097/PSY.0b013e3181b0d2b4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Jurkowski JM, Leckman EL, Rossy-Millan J. Latina self-reported mental health and delay in health care in a new Latino destination. Women Health. 2010;50:213–228. doi: 10.1080/03630242.2010.482007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Vega WA, Rodriguez MA, Gruskin E. Health disparities in the Latino population. Epidemiol Rev. 2009;31:99–112. doi: 10.1093/epirev/mxp008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Sussner KM, Lindsay AC, Greaney ML, Peterson KE. The influence of immigrant status and acculturation on the development of overweight in Latino families: a qualitative study. J Immigr Minor Health. 2008;10:497–505. doi: 10.1007/s10903-008-9137-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Lindberg NM, Stevens VJ. Immigration and weight gain: Mexican-American women’s perspectives. J Immigr Minor Health. 2011;13:155–160. doi: 10.1007/s10903-009-9298-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Himmelgreen D, Romero Daza N, Cooper E, Martinez D. “I don’t make the soups anymore”: Pre- to post-migration dietary and lifestyle changes among Latinos living in West-Central Florida. Ecol Food Nutr. 2007;46:427–444. [Google Scholar]
- 204.Guarnaccia PJ, Vivar T, Bellows AC, Alcaraz GV. “We eat meat every day”: ecology and economy of dietary change among Oaxacan migrants from Mexico to New Jersey. Ethn Racial Stud. 2012;35:104–119. [Google Scholar]
- 205.Goel MS, Wee CC, McCarthy EP, Davis RB, Ngo-Metzger Q, Phillips RS. Racial and ethnic disparities in cancer screening: the importance of foreign birth as a barrier to care. J Gen Intern Med. 2003;18:1028–1035. doi: 10.1111/j.1525-1497.2003.20807.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Rodríguez MA, Ward LM, Pérez-Stable EJ. Breast and cervical cancer screening: impact of health insurance status, ethnicity, and nativity of Latinas. Ann Fam Med. 2005;3:235–241. doi: 10.1370/afm.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Eamranond PP, Wee CC, Legedza AT, Marcantonio ER, Leveille SG. Acculturation and cardiovascular risk factor control among Hispanic adults in the United States. Public Health Rep. 2009;124:818–824. doi: 10.1177/003335490912400609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.United Nations, Food and Agriculture Organization. The State of Food and Agriculture, 2013: Food Systems for Better Nutrition. Rome, Italy: Food and Agriculture Organization of the United Nations; 2013. [Google Scholar]
- 209.Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32:20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Brondolo E, Hausmann LR, Jhalani J, Pencille M, Atencio-Bacayon J, Kumar A, Kwok J, Ullah J, Roth A, Chen D, Crupi R, Schwartz J. Dimensions of perceived racism and self-reported health: examination of racial/ethnic differences and potential mediators. Ann Behav Med. 2011;42:14–28. doi: 10.1007/s12160-011-9265-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Sims M, Wyatt SB, Gutierrez ML, Taylor HA, Williams DR. Development and psychometric testing of a multidimensional instrument of perceived discrimination among African Americans in the Jackson Heart Study. Ethn Dis. 2009;19:56–64. [PMC free article] [PubMed] [Google Scholar]
- 212.Sims M, Diez-Roux AV, Dudley A, Gebreab S, Wyatt SB, Bruce MA, James SA, Robinson JC, Williams DR, Taylor HA. Perceived discrimination and hypertension among African Americans in the Jackson Heart Study. Am J Public Health. 2012;102(suppl 2):S258–S265. doi: 10.2105/AJPH.2011.300523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Lewis TT, Everson-Rose SA, Powell LH, Matthews KA, Brown C, Karavolos K, Sutton-Tyrrell K, Jacobs E, Wesley D. Chronic exposure to everyday discrimination and coronary artery calcification in African-American women: the SWAN Heart Study. Psychosom Med. 2006;68:362–368. doi: 10.1097/01.psy.0000221360.94700.16. [DOI] [PubMed] [Google Scholar]
- 214.Wyatt SB, Williams DR, Calvin R, Henderson FC, Walker ER, Winters K. Racism and cardiovascular disease in African Americans. Am J Med Sci. 2003;325:315–331. doi: 10.1097/00000441-200306000-00003. [DOI] [PubMed] [Google Scholar]
- 215.Finch BK, Kolody B, Vega WA. Perceived discrimination and depression among Mexican-origin adults in California. J Health Soc Behav. 2000;41:295–313. [PubMed] [Google Scholar]
- 216.Ryff CD, Keyes CL, Hughes DL. Status inequalities, perceived discrimination, and eudaimonic well-being: do the challenges of minority life hone purpose and growth? J Health Soc Behav. 2003;44:275–291. [PubMed] [Google Scholar]
- 217.Borrell LN, Diez Roux AV, Jacobs DR, Jr, Shea S, Jackson SA, Shrager S, Blumenthal RS. Perceived racial/ethnic discrimination, smoking and alcohol consumption in the Multi-Ethnic Study of Atherosclerosis (MESA) Prev Med. 2010;51:307–312. doi: 10.1016/j.ypmed.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Brondolo E, Libby DJ, Denton EG, Thompson S, Beatty DL, Schwartz J, Sweeney M, Tobin JN, Cassells A, Pickering TG, Gerin W. Racism and ambulatory blood pressure in a community sample. Psychosom Med. 2008;70:49–56. doi: 10.1097/PSY.0b013e31815ff3bd. [DOI] [PubMed] [Google Scholar]
- 219.Pérez DJ, Fortuna L, Alegria M. Prevalence and correlates of everyday discrimination among U.S. Latinos. J Community Psychol. 2008;36:421–433. doi: 10.1002/jcop.20221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Pew Hispanic Center. Between Two Worlds: How Young Latinos Come of Age in America. Washington, DC: Pew Research Center; Dec 11, 2009. Pew Research Hispanic Trends Project. [Google Scholar]
- 221.Lee MA, Ferraro KF. Perceived discrimination and health among Puerto Rican and Mexican Americans: buffering effect of the Lazo matrimonial? Soc Sci Med. 2009;68:1966–1974. doi: 10.1016/j.socscimed.2009.02.052. [DOI] [PubMed] [Google Scholar]
- 222.Barrera M., Jr . Social support research in community psychology. In: Rappaport J, Seidman E, editors. Handbook of Community Psychology. New York, NY: Kluwer Academic/Plenum Publishers; 2000. [Google Scholar]
- 223.Heller K, Thompson MG, Trueba PE, Hogg JR, Vlachos-Weber I. Peer support telephone dyads for elderly women: was this the wrong intervention? Am J Community Psychol. 1991;19:53–74. doi: 10.1007/BF00942253. [DOI] [PubMed] [Google Scholar]
- 224.Lett HS, Blumenthal JA, Babyak MA, Strauman TJ, Robins C, Sherwood A. Social support and coronary heart disease: epidemiologic evidence and implications for treatment. Psychosom Med. 2005;67:869–878. doi: 10.1097/01.psy.0000188393.73571.0a. [DOI] [PubMed] [Google Scholar]
- 225.Lora CM, Gordon EJ, Sharp LK, Fischer MJ, Gerber BS, Lash JP. Progression of CKD in Hispanics: potential roles of health literacy, acculturation, and social support. Am J Kidney Dis. 2011;58:282–290. doi: 10.1053/j.ajkd.2011.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Uchino BN, Garvey TS. The availability of social support reduces cardiovascular reactivity to acute psychological stress. J Behav Med. 1997;20:15–27. doi: 10.1023/a:1025583012283. [DOI] [PubMed] [Google Scholar]
- 227.Clark R. Self-reported racism and social support predict blood pressure reactivity in Blacks. Ann Behav Med. 2003;25:127–136. doi: 10.1207/S15324796ABM2502_09. [DOI] [PubMed] [Google Scholar]
- 228.Yan LL, Liu K, Matthews KA, Daviglus ML, Ferguson TF, Kiefe CI. Psychosocial factors and risk of hypertension: the Coronary Artery Risk Development in Young Adults (CARDIA) study. JAMA. 2003;290:2138–2148. doi: 10.1001/jama.290.16.2138. [DOI] [PubMed] [Google Scholar]
- 229.Romano PS, Bloom J, Syme SL. Smoking, social support, and hassles in an urban African-American community. Am J Public Health. 1991;81:1415–1422. doi: 10.2105/ajph.81.11.1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Eyler AA, Baker E, Cromer L, King AC, Brownson RC, Donatelle RJ. Physical activity and minority women: a qualitative study. Health Educ Behav. 1998;25:640–652. doi: 10.1177/109019819802500510. [DOI] [PubMed] [Google Scholar]
- 231.Hovell M, Sallis J, Hofstetter R, Barrington E, Hackley M, Elder J, Castro F, Kilbourne K. Identification of correlates of physical activity among Latino adults. J Community Health. 1991;16:23–36. doi: 10.1007/BF01340466. [DOI] [PubMed] [Google Scholar]
- 232.Keller C, Fleury J. Factors related to physical activity in Hispanic women. J Cardiovasc Nurs. 2006;21:142–145. doi: 10.1097/00005082-200603000-00012. [DOI] [PubMed] [Google Scholar]
- 233.Barrera M, Jr, Toobert DJ, Angell KL, Glasgow RE, MacKinnon DP. Social support and social-ecological resources as mediators of lifestyle intervention effects for type 2 diabetes. J Health Psychol. 2006;11:483–495. doi: 10.1177/1359105306063321. [DOI] [PubMed] [Google Scholar]
- 234.Marquez DX, McAuley E, Overman N. Psychosocial correlates and outcomes of physical activity among Latinos: a review. Hisp J Behav Sci. 2004;26:195–229. [Google Scholar]
- 235.Thornton PL, Kieffer EC, Salabarria-Peña Y, Odoms-Young A, Willis SK, Kim H, Salinas MA. Weight, diet, and physical activity-related beliefs and practices among pregnant and postpartum Latino women: the role of social support. Matern Child Health J. 2006;10:95–104. doi: 10.1007/s10995-005-0025-3. [DOI] [PubMed] [Google Scholar]
- 236.Chao MT, Wade C, Kronenberg F, Kalmuss D, Cushman LF. Women’s reasons for complementary and alternative medicine use: racial/ethnic differences. J Altern Complement Med. 2006;12:719–722. doi: 10.1089/acm.2006.12.719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Trangmar P, Diaz VA. Investigating complementary and alternative medicine use in a Spanish-speaking Hispanic community in South Carolina. Ann Fam Med. 2008;6(suppl 1):S12–S15. doi: 10.1370/afm.736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Graham RE, Ahn AC, Davis RB, O’Connor BB, Eisenberg DM, Phillips RS. Use of complementary and alternative medical therapies among racial and ethnic minority adults: results from the 2002 National Health Interview Survey. J Natl Med Assoc. 2005;97:535–545. [PMC free article] [PubMed] [Google Scholar]
- 239.Shelley BM, Sussman AL, Williams RL, Segal AR, Crabtree BF Rios Net Clinicians. “They don’t ask me so I don’t tell them”: patient-clinician communication about traditional, complementary, and alternative medicine. Ann Fam Med. 2009;7:139–147. doi: 10.1370/afm.947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Kuo GM, Hawley ST, Weiss LT, Balkrishnan R, Volk RJ. Factors associated with herbal use among urban multiethnic primary care patients: a cross-sectional survey. BMC Complement Altern Med. 2004;4:18. doi: 10.1186/1472-6882-4-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Howell L, Kochhar K, Saywell R, Jr, Zollinger T, Koehler J, Mandzuk C, Sutton B, Sevilla-Martir J, Allen D. Use of herbal remedies by Hispanic patients: do they inform their physician? J Am Board Fam Med. 2006;19:566–578. doi: 10.3122/jabfm.19.6.566. [DOI] [PubMed] [Google Scholar]
- 242.Ailinger RL. Folk beliefs about high blood pressure in Hispanic immigrants. [DOI] [PubMed] [Google Scholar]
- 243.Flaskerud JH, Calvillo ER. Beliefs about AIDS, health, and illness among low-income Latina women. Res Nurs Health. 1991;14:431–438. doi: 10.1002/nur.4770140607. [DOI] [PubMed] [Google Scholar]
- 244.Gordon SM. Hispanic cultural health beliefs and folk remedies. J Holist Nurs. 1994;12:307–322. doi: 10.1177/089801019401200308. [DOI] [PubMed] [Google Scholar]
- 245.Ortiz BI, Shields KM, Clauson KA, Clay PG. Complementary and alternative medicine use among Hispanics in the United States. Ann Pharmacother. 2007;41:994–1004. doi: 10.1345/aph.1H600. [DOI] [PubMed] [Google Scholar]
- 246.Izzo AA, Ernst E. Interactions between herbal medicines and prescribed drugs: a systematic review. Drugs. 2001;61:2163–2175. doi: 10.2165/00003495-200161150-00002. [DOI] [PubMed] [Google Scholar]
- 247.Eisenberg DM, Davis RB, Ettner SL, Appel S, Wilkey S, Van Rompay M, Kessler RC. Trends in alternative medicine use in the United States, 1990–1997. JAMA. 1998;280:1569–1575. doi: 10.1001/jama.280.18.1569. [DOI] [PubMed] [Google Scholar]
- 248.Pachter LM, Bernstein B, Osorio A. Clinical implications of a folk illness: empacho in mainland Puerto Ricans. Med Anthropol. 1992;13:285–299. doi: 10.1080/01459740.1992.9966053. [DOI] [PubMed] [Google Scholar]
- 249.Factor-Litvak P, Cushman LF, Kronenberg F, Wade C, Kalmuss D. Use of complementary and alternative medicine among women in New York City: a pilot study. J Altern Complement Med. 2001;7:659–666. doi: 10.1089/10755530152755216. [DOI] [PubMed] [Google Scholar]
- 250.Villa-Caballero L, Morello CM, Chynoweth ME, Prieto-Rosinol A, Polonsky WH, Palinkas LA, Edelman SV. Ethnic differences in complementary and alternative medicine use among patients with diabetes. Complement Ther Med. 2010;18:241–248. doi: 10.1016/j.ctim.2010.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Upchurch DM, Chyu L. Use of complementary and alternative medicine among American women. Womens Health Issues. 2005;15:5–13. doi: 10.1016/j.whi.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 252.White B, Knox L, Zepeda M, Mull D, Nunez F. Impact of immigration on complementary and alternative medicine use in Hispanic patients. J Am Board Fam Med. 2009;22:337–338. doi: 10.3122/jabfm.2009.03.080210. [DOI] [PubMed] [Google Scholar]
- 253.Kronenberg F, Cushman LF, Wade CM, Kalmuss D, Chao MT. Race/ethnicity and women’s use of complementary and alternative medicine in the United States: results of a national survey [published correction appears in Am J Public Health. 2006;96:1340] Am J Public Health. 2006;96:1236–42. doi: 10.2105/AJPH.2004.047688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Upchurch DM, Rainisch BKW. Racial and ethnic profiles of complementary and alternative medicine use among young adults in the United States: findings from the National Longitudinal Study of Adolescent Health. J Evid Based Complementary Altern Med. 2012;17:172–9. doi: 10.1177/2156587212450713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Loera JA, Reyes-Ortiz C, Kuo YF. Predictors of complementary and alternative medicine use among older Mexican Americans. Complement Ther Clin Pract. 2007;13:224–231. doi: 10.1016/j.ctcp.2007.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Baer R, Ackerman A. Toxic Mexican folk remedies for the treatment of empacho: the case of azarcon, greta, and albayalde. J Ethnopharmacol. 1988;24:31–39. doi: 10.1016/0378-8741(88)90137-7. [DOI] [PubMed] [Google Scholar]
- 257.Weller SC, Pachter LM, Trotter RT, 2nd, Baer RD, Klein RE, Garcia JEG, Glazer M, Castillo Z. Empacho in four Latino groups: a study of intra- and inter-cultural variation in beliefs. Med Anthropol. 1993;15:109–136. doi: 10.1080/01459740.1993.9966085. [DOI] [PubMed] [Google Scholar]
- 258.Risser AL, Mazur LJ. Use of folk remedies in a Hispanic population. Arch Pediatr Adolesc Med. 1995;149:978–981. doi: 10.1001/archpedi.1995.02170220044006. [DOI] [PubMed] [Google Scholar]
- 259.Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, Arnett DK, Fonarow GC, Ho PM, Lauer MS, Masoudi FA, Robertson RM, Roger V, Schwamm LH, Sorlie P, Yancy CW, Rosamond WD on behalf of the American Heart Association Strategic Planning Task Force and Statistics Committee. . Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 260.Mosca L, Ferris A, Fabunmi R, Robertson RM. Tracking women’s awareness of heart disease: an American Heart Association national study. Circulation. 2004;109:573–579. doi: 10.1161/01.CIR.0000115222.69428.C9. [DOI] [PubMed] [Google Scholar]
- 261.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Magid D, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, Moy CS, Mussolino ME, Nichol G, Paynter NP, Schreiner PJ, Sorlie PD, Stein J, Turan TN, Virani SS, Wong ND, Woo D, Turner MB on behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. . Heart disease and stroke statistics: 2013 update: a report from the American Heart Association [published corrections appear in Circulation 2013;127:doi:10.1161/CIR.0b013e31828124ad and Circulation. 2013;127:e841] Circulation. 2013;127:e6–e245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Crespo C, Loria C, Burt V. Hypertension and other cardiovascular disease risk factors among Mexican Americans, Cuban Americans, and Puerto Ricans from the Hispanic Health and Nutrition Examination Survey. Public Health Rep. 1996;111(suppl 2):7–10. [PMC free article] [PubMed] [Google Scholar]
- 263.Derby CA, Wildman RP, McGinn AP, Green RR, Polotsky AJ, Ram KT, Barnhart J, Weiss G, Santoro N. Cardiovascular risk factor variation within a Hispanic cohort: SWAN, the Study of Women’s Health Across the Nation. Ethn Dis. 2010;20:396–402. [PMC free article] [PubMed] [Google Scholar]
- 264.Allison MA, Budoff MJ, Wong ND, Blumenthal RS, Schreiner PJ, Criqui MH. Prevalence of and risk factors for subclinical cardiovascular disease in selected US Hispanic ethnic groups: the Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol. 2008;167:962–969. doi: 10.1093/aje/kwm402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Davidson JA, Kannel WB, Lopez-Candales A, Morales L, Moreno PR, Ovalle F, Rodriguez CJ, Rodbard HW, Rosenson RS, Stern M. Avoiding the looming Latino/Hispanic cardiovascular health crisis: a call to action. Ethn Dis. 2007;17:568–573. [PubMed] [Google Scholar]
- 266.Ford ES, Li C, Pearson WS, Zhao G, Mokdad AH. Trends in hypercholesterolemia, treatment and control among United States adults. Int J Cardiol. 2010;140:226–235. doi: 10.1016/j.ijcard.2008.11.033. [DOI] [PubMed] [Google Scholar]
- 267.Nelson K, Norris K, Mangione CM. Disparities in the diagnosis and pharmacologic treatment of high serum cholesterol by race and ethnicity: data from the third National Health and Nutrition Examination Survey. Arch Intern Med. 2002;162:929–935. doi: 10.1001/archinte.162.8.929. [DOI] [PubMed] [Google Scholar]
- 268.Haffner SM, D’Agostino R, Jr, Goff D, Howard B, Festa A, Saad MF, Mykkänen L. LDL size in African Americans, Hispanics, and non-Hispanic whites: the Insulin Resistance Atherosclerosis Study. Arterioscler Thromb Vasc Biol. 1999;19:2234–2240. doi: 10.1161/01.atv.19.9.2234. [DOI] [PubMed] [Google Scholar]
- 269.Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Soliman EZ, Sorlie PD, Sotoodehnia N, Turan TN, Virani SS, Wong ND, Woo D, Turner MB on behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. . Heart disease and stroke statistics: 2012 update: a report from the American Heart Association [published correction appears in Circulation. 2012;125:e1002] Circulation. 2012;125:e2–e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Centers for Disease Control and Prevention. Hypertension-related mortality among Hispanic subpopulations: United States, 1995–2002. MMWR Morb Mortal Wkly Rep. 2006;55:177–180. [PubMed] [Google Scholar]
- 271.Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. JAMA. 2003;290:199–206. doi: 10.1001/jama.290.2.199. [DOI] [PubMed] [Google Scholar]
- 272.Haffner SM, Mitchell BD, Stern MP, Hazuda HP, Patterson JK. Decreased prevalence of hypertension in Mexican-Americans. Hypertension. 1990;16:225–232. doi: 10.1161/01.hyp.16.3.225. [DOI] [PubMed] [Google Scholar]
- 273.Qureshi AI, Suri MF, Kirmani JF, Divani AA. Prevalence and trends of prehypertension and hypertension in United States: National Health and Nutrition Examination Surveys 1976 to 2000. Med Sci Monit. 2005;11:CR403–CR409. [PubMed] [Google Scholar]
- 274.Ong KL, Cheung BM, Man YB, Lau CP, Lam KS. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension. 2007;49:69–75. doi: 10.1161/01.HYP.0000252676.46043.18. [DOI] [PubMed] [Google Scholar]
- 275.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Judd SE, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Mackey RH, Magid DJ, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, 3rd, Moy CS, Mussolino ME, Neumar RW, Nichol G, Pandey DK, Paynter NP, Reeves MJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Wong ND, Woo D, Turner MB on behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. . Heart disease and stroke statistics: 2014 update: a report from the American Heart Association. Circulation. 2014;129:e28–e292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Burt VL, Whelton P, Roccella EJ, Brown C, Cutler JA, Higgins M, Horan MJ, Labarthe D. Prevalence of hypertension in the US adult population: results from the Third National Health and Nutrition Examination Survey, 1988–1991. Hypertension. 1995;25:305–313. doi: 10.1161/01.hyp.25.3.305. [DOI] [PubMed] [Google Scholar]
- 277.Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;303:2043–2050. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- 278.Cutler JA, Sorlie PD, Wolz M, Thom T, Fields LE, Roccella EJ. Trends in hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988–1994 and 1999–2004. Hypertension. 2008;52:818–827. doi: 10.1161/HYPERTENSIONAHA.108.113357. [DOI] [PubMed] [Google Scholar]
- 279.Borrell LN, Crawford ND. Disparities in self-reported hypertension in Hispanic subgroups, non-Hispanic black and non-Hispanic white adults: the National Health Interview Survey. Ann Epidemiol. 2008;18:803–812. doi: 10.1016/j.annepidem.2008.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Pabon-Nau LP, Cohen A, Meigs JB, Grant RW. Hypertension and diabetes prevalence among U.S. Hispanics by country of origin: the National Health Interview Survey 2000–2005. J Gen Intern Med. 2010;25:847–852. doi: 10.1007/s11606-010-1335-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Sorlie PD, Allison MA, Aviles-Santa ML, Cai J, Daviglus ML, Howard AG, Kaplan R, Lavange LM, Raij L, Schneiderman N, Wassertheil-Smoller S, Talavera GA. Prevalence of hypertension, awareness, treatment, and control in the Hispanic Community Health Study/Study of Latinos. Am J Hypertens. 2014;27:793–800. doi: 10.1093/ajh/hpu003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Crimmins E, Kim J, Alley D, Karlamangla A, Seeman T. Hispanic paradox in biological risk profiles. Am J Public Health. 2007;97:1305–1310. doi: 10.2105/AJPH.2006.091892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Caballero AE. Type 2 diabetes in the Hispanic or Latino population: challenges and opportunities. Curr Opin Endocrinol Diabetes Obes. 2007;14:151–157. doi: 10.1097/MED.0b013e32809f9531. [DOI] [PubMed] [Google Scholar]
- 284.Diabetes and Hispanic Americans. US Department of Health & Human Services, Office of Minority Health; [Accessed June 19, 2012]. Web site. http://minorityhealth.hhs.gov/templates/content.aspx?ID=3324. [Google Scholar]
- 285.Narayan KM, Boyle JP, Thompson TJ, Sorensen SW, Williamson DF. Lifetime risk for diabetes mellitus in the United States. JAMA. 2003;290:1884–1890. doi: 10.1001/jama.290.14.1884. [DOI] [PubMed] [Google Scholar]
- 286.Lorenzo C, Hazuda HP, Haffner SM. Insulin resistance and excess risk of diabetes in Mexican-Americans: the San Antonio Heart Study. J Clin Endocrinol Metab. 2012;97:793–799. doi: 10.1210/jc.2011-2272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Flegal K, Ezzati T, Harris M, Haynes SG, Juarez RZ, Knowler WC, Pérez-Stable EJ, Stern MP. Prevalence of diabetes in Mexican Americans, Cubans, and Puerto Ricans from the Hispanic Health and Nutrition Examination Survey, 1982–1984. Diabetes Care. 1991;14:628–638. doi: 10.2337/diacare.14.7.628. [DOI] [PubMed] [Google Scholar]
- 288.Boltri JM, Okosun IS, Davis-Smith M, Vogel RL. Hemoglobin A1c levels in diagnosed and undiagnosed black, Hispanic, and white persons with diabetes: results from NHANES 1999–2000. Ethn Dis. 2005;15:562–567. [PubMed] [Google Scholar]
- 289.Borrell LN, Crawford ND, Dallo FJ, Baquero MC. Self-reported diabetes in Hispanic subgroup, non-Hispanic black, and non-Hispanic white populations: National Health Interview Survey, 1997–2005. Public Health Reports. 2009;124:702–710. doi: 10.1177/003335490912400512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Neel JV. Diabetes mellitus: a “thrifty” genotype rendered detrimental by “progress”? Am J Hum Genet. 1962;14:353–362. [PMC free article] [PubMed] [Google Scholar]
- 291.Haffner SM, D’Agostino R, Saad MF, Rewers M, Mykkänen L, Selby J, Howard G, Savage PJ, Hamman RF, Wagenknecht LE, Bergman RN. Increased insulin resistance and insulin secretion in nondiabetic African-Americans and Hispanics compared with non-Hispanic whites: the Insulin Resistance Atherosclerosis Study. Diabetes. 1996;45:742–8. doi: 10.2337/diab.45.6.742. [DOI] [PubMed] [Google Scholar]
- 292.Chiu KC, Cohan P, Lee NP, Chuang LM. Insulin sensitivity differs among ethnic groups with a compensatory response in beta-cell function. Diabetes Care. 2000;23:1353–1358. doi: 10.2337/diacare.23.9.1353. [DOI] [PubMed] [Google Scholar]
- 293.Goran MI, Bergman RN, Cruz ML, Watanabe R. Insulin resistance and associated compensatory responses in African-American and Hispanic children. Diabetes Care. 2002;25:2184–2190. doi: 10.2337/diacare.25.12.2184. [DOI] [PubMed] [Google Scholar]
- 294.Davidson JA, Moreno PR, Badimon JJ, Lopez-Candales A, Maisonet Giachello AL, Ovalle F, Rodriguez CJ, Rosenson RS, Rodbard HW, Kannel WB. Cardiovascular disease prevention and care in Latino and Hispanic subjects. Endocr Pract. 2007;13:77–85. doi: 10.4158/EP.13.1.77. [DOI] [PubMed] [Google Scholar]
- 295.Deleted in proof.
- 296.Tian C, Hinds DA, Shigeta R, Adler SG, Lee A, Pahl MV, Silva G, Belmont JW, Hanson RL, Knowler WC, Gregersen PK, Ballinger DG, Seldin MF. A genomewide single-nucleotide-polymorphism panel for Mexican American admixture mapping. Am J Hum Genet. 2007;80:1014–1023. doi: 10.1086/513522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Neel JV. The “thrifty genotype” in 19981. Nutr Rev. 1999;57:2–9. doi: 10.1111/j.1753-4887.1999.tb01782.x. [DOI] [PubMed] [Google Scholar]
- 298.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 299.Nichaman MZ, Garcia G. Obesity in Hispanic Americans. Diabetes Care. 1991;14:691–694. doi: 10.2337/diacare.14.7.691. [DOI] [PubMed] [Google Scholar]
- 300.Flegal KM, Ogden CL, Carroll MD. Prevalence and trends in overweight in Mexican-American adults and children. Nutr Rev. 2004;62(pt 2):S144–S148. doi: 10.1111/j.1753-4887.2004.tb00085.x. [DOI] [PubMed] [Google Scholar]
- 301.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307:491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 302.Lindberg NM, Stevens VJ. Review: weight-loss interventions with Hispanic populations. Ethn Dis. 2007;17:397–402. [PubMed] [Google Scholar]
- 303.Poston WS, Reeves RS, Haddock CK, Stormer S, Balasubramanyam A, Satterwhite O, Taylor JE, Foreyt JP. Weight loss in obese Mexican Americans treated for 1-year with orlistat and lifestyle modification. Int J Obes Relat Metab Disord. 2003;27:1486–1493. doi: 10.1038/sj.ijo.0802439. [DOI] [PubMed] [Google Scholar]
- 304.Trevino RP, Pugh JA, Hernandez AE, Menchaca VD, Ramirez RR, Mendoza M. Bienestar: a diabetes risk-factor prevention program. J Sch Health. 1998;68:62–67. doi: 10.1111/j.1746-1561.1998.tb07192.x. [DOI] [PubMed] [Google Scholar]
- 305.Fitzgibbon ML, Gapstur SM, Knight SJ. Results of Mujeres Felices por ser Saludables: a dietary/breast health randomized clinical trial for Latino women. Ann Behav Med. 2004;28:95–104. doi: 10.1207/s15324796abm2802_4. [DOI] [PubMed] [Google Scholar]
- 306.Thompson B, Coronado G, Chen L, Islas I. Celebremos la salud! A community randomized trial of cancer prevention (United States) Cancer Causes Control. 2006;17:733–746. doi: 10.1007/s10552-006-0006-x. [DOI] [PubMed] [Google Scholar]
- 307.Rosal MC, Olendzki B, Reed GW, Gumieniak O, Scavron J, Ockene I. Diabetes self-management among low-income Spanish-speaking patients: a pilot study. Ann Behav Med. 2005;29:225–235. doi: 10.1207/s15324796abm2903_9. [DOI] [PubMed] [Google Scholar]
- 308.Eakin EG, Bull SS, Riley KM, Reeves MM, McLaughlin P, Gutierrez S. Resources for health: a primary-care-based diet and physical activity intervention targeting urban Latinos with multiple chronic conditions. Health Psychol. 2007;26:392–400. doi: 10.1037/0278-6133.26.4.392. [DOI] [PubMed] [Google Scholar]
- 309.Baquero B, Ayala GX, Arredondo EM, Campbell NR, Slymen DJ, Gallo L, Elder JP. Secretos de la Buena Vida: processes of dietary change via a tailored nutrition communication intervention for Latinas. Health Educ Res. 2009;24:855–866. doi: 10.1093/her/cyp022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Lindberg NM, Stevens VJ, Vega-López S, Kauffman TL, Calderón MR, Cervantes MA. A weight-loss intervention program designed for Mexican-American women: cultural adaptations and results. J Immigr Minor Health. 2012;14:1030–1039. doi: 10.1007/s10903-012-9616-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Chowdhury PP, Balluz L, Okoro C, Strine T. Leading health indicators: a comparison of Hispanics with non-Hispanic whites and non-Hispanic blacks, United States 2003. Ethn Dis. 2006;16:534–41. [PubMed] [Google Scholar]
- 312.Centers for Disease Control and Prevention (CDC). . Cigarette smoking among adults and trends in smoking cessation: United States, 2008. MMWR Morb Mortal Wkly Rep. 2009;58:1227–1232. [PubMed] [Google Scholar]
- 313.Centers for Disease Control and Prevention (CDC). . Vital signs: current cigarette smoking among adults aged ≥18 years: United States, 2005–2010. MMWR Morb Mortal Wkly Rep. 2011;60:1207–1212. [PubMed] [Google Scholar]
- 314.Pérez-Stable EJ, Ramirez A, Villareal R, Talavera GA, Trapido E, Suarez L, Marti J, McAlister A. Cigarette smoking behavior among US Latino men and women from different countries of origin. Am J Public Health. 2001;91:1424–1430. doi: 10.2105/ajph.91.9.1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Centers for Disease Control and Prevention (CDC). . Tobacco use among adults: United States, 2005. 2006;55:1145–1148. [Google Scholar]
- 316.Marks G, Garcia M, Solis JM. Health risk behaviors of Hispanics in the United States: findings from HHANES, 1982–84. Am J Public Health. 1990;80(suppl):20–26. doi: 10.2105/ajph.80.suppl.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Bethel JW, Schenker MB. Acculturation and smoking patterns among Hispanics: a review. Am J Prev Med. 2005;29:143–148. doi: 10.1016/j.amepre.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 318.Pérez-Stable EJ, Marín BV, Marín G, Brody DJ, Benowitz NL. Apparent underreporting of cigarette consumption among Mexican American smokers. Am J Public Health. 1990;80:1057–1061. doi: 10.2105/ajph.80.9.1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.Crespo CJ, Keteyian SJ, Heath GW, Sempos CT. Leisure-time physical activity among US adults: results from the Third National Health and Nutrition Examination Survey. Arch Intern Med. 1996;156:93–98. [PubMed] [Google Scholar]
- 320.Macera CA, Ham SA, Yore MM, Jones DA, Ainsworth BE, Kimsey CD, Kohl HW., 3rd Prevalence of physical activity in the United States: Behavioral Risk Factor Surveillance System, 2001. Prev Chronic Dis. 2005;2:A17. [PMC free article] [PubMed] [Google Scholar]
- 321.Neighbors CJ, Marquez DX, Marcus BH. Leisure-time physical activity disparities among Hispanic subgroups in the United States. Am J Public Health. 2008;98:1460–1464. doi: 10.2105/AJPH.2006.096982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.Ham SA, Yore MM, Kruger J, Heath GW, Moeti R. Physical activity patterns among Latinos in the United States: putting the pieces together. Prev Chronic Dis. 2007;4:A92. [PMC free article] [PubMed] [Google Scholar]
- 323.McGruder HF, Malarcher AM, Antoine TL, Greenlund KJ, Croft JB. Racial and ethnic disparities in cardiovascular risk factors among stroke survivors: United States 1999 to 2001. Stroke. 2004;35:1557–1561. doi: 10.1161/01.STR.0000130427.84114.50. [DOI] [PubMed] [Google Scholar]
- 324.Brownson RC, Eyler AA, King AC, Brown DR, Shyu YL, Sallis JF. Patterns and correlates of physical activity among US women 40 years and older. Am J Public Health. 2000;90:264–70. doi: 10.2105/ajph.90.2.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Dergance JM, Mouton CP, Lichtenstein MJ, Hazuda HP. Potential mediators of ethnic differences in physical activity in older Mexican Americans and European Americans: results from the San Antonio Longitudinal Study of Aging. J Am Geriatr Soc. 2005;53:1240–1247. doi: 10.1111/j.1532-5415.2005.53363.x. [DOI] [PubMed] [Google Scholar]
- 326.Centers for Disease Control and Prevention (CDC). . Contribution of occupational physical activity toward meeting recommended physical activity guidelines: United States, 2007. MMWR Morb Mortal Wkly Report. 2011;60:656–660. [PubMed] [Google Scholar]
- 327.Bowie JV, Juon HS, Cho J, Rodriguez EM. Factors associated with overweight and obesity among Mexican Americans and Central Americans: results from the 2001 California Health Interview Survey. Prev Chronic Dis. 2007;4:A10. [PMC free article] [PubMed] [Google Scholar]
- 328.Ford ES, Li C, Zhao G, Pearson WS, Capewell S. Trends in the prevalence of low risk factor burden for cardiovascular disease among United States adults. Circulation. 2009;120:1181–1188. doi: 10.1161/CIRCULATIONAHA.108.835728. [DOI] [PubMed] [Google Scholar]
- 329.Dong C, Rundek T, Wright CB, Anwar Z, Elkind MS, Sacco RL. Ideal cardiovascular health predicts lower risks of myocardial infarction, stroke, and vascular death across whites, blacks, and Hispanics: the Northern Manhattan Study. Circulation. 2012;125:2975–2984. doi: 10.1161/CIRCULATIONAHA.111.081083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330.Rodriguez CJ. Disparities in ideal cardiovascular health: a challenge or an opportunity? Circulation. 2012;125:2963–2964. doi: 10.1161/CIRCULATIONAHA.112.112680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331.González HM, Tarraf W, Mosley T, Wright C, Rundek T, Lutsey PL, Gouskova N, Grober E, Pirzada A, Daviglus M. Life’s Simple 7s of Cardiovascular Health Among Hispanic/Latinos: the Hispanic Community Health Study/Study of Latinos (HCHS/SOL) Circulation. 2012;126:A17624. [Google Scholar]
- 332.Burke JP, Williams K, Haffner SM, Villalpando CG, Stern MP. Elevated incidence of type 2 diabetes in San Antonio, Texas, compared with that of Mexico City, Mexico. Diabetes Care. 2001;24:1573–1578. doi: 10.2337/diacare.24.9.1573. [DOI] [PubMed] [Google Scholar]
- 333.Smith MA, Lisabeth LD, Bonikowski F, Morgenstern LB. The role of ethnicity, sex, and language on delay to hospital arrival for acute ischemic stroke. Stroke. 2010;41:905–9. doi: 10.1161/STROKEAHA.110.578112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334.Lacy CR, Suh DC, Bueno M, Kostis JB. Delay in presentation and evaluation for acute stroke: Stroke Time Registry for Outcomes Knowledge and Epidemiology (S.T.R.O.K.E.) Stroke. 2001;32:63–69. doi: 10.1161/01.str.32.1.63. [DOI] [PubMed] [Google Scholar]
- 335.Bild DE, Detrano R, Peterson D, Guerci A, Liu K, Shahar E, Ouyang P, Jackson S, Saad MF. Ethnic differences in coronary calcification: the Multi-Ethnic Study of Atherosclerosis (MESA) Circulation. 2005;111:1313–1320. doi: 10.1161/01.CIR.0000157730.94423.4B. [DOI] [PubMed] [Google Scholar]
- 336.Budoff MJ, Nasir K, Mao S, et al. Ethnic differences of the presence and severity of coronary atherosclerosis. Atherosclerosis. 2006;187:343–350. doi: 10.1016/j.atherosclerosis.2005.09.013. [DOI] [PubMed] [Google Scholar]
- 337.Diez Roux AV, Detrano R, Jackson S, Jacobs DR, Jr, Schreiner PJ, Shea S, Szklo M. Acculturation and socioeconomic position as predictors of coronary calcification in a multiethnic sample. Circulation. 2005;112:1557–1565. doi: 10.1161/CIRCULATIONAHA.104.530147. [DOI] [PubMed] [Google Scholar]
- 338.Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, Folsom AR, Liu K, Shea S, Szklo M, Bluemke DA, O’Leary DH, Tracy R, Watson K, Wong ND, Kronmal RA. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008;358:1336–1345. doi: 10.1056/NEJMoa072100. [DOI] [PubMed] [Google Scholar]
- 339.D’Agostino RB, Burke G, O’Leary D, Rewers M, Selby J, Savage PJ, Saad MF, Bergman RN, Howard G, Wagenknecht L, Haffner SM. Ethnic differences in carotid wall thickness: the Insulin Resistance Atherosclerosis Study. Stroke. 1996;27:1744–1749. doi: 10.1161/01.str.27.10.1744. [DOI] [PubMed] [Google Scholar]
- 340.Manolio TA, Arnold AM, Post W, Bertoni AG, Schreiner PJ, Sacco RL, Saad MF, Detrano RL, Szklo M. Ethnic differences in the relationship of carotid atherosclerosis to coronary calcification: the Multi-Ethnic Study of Atherosclerosis. Atherosclerosis. 2008;197:132–138. doi: 10.1016/j.atherosclerosis.2007.02.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341.Breton CV, Wang X, Mack WJ, Berhane K, Lopez M, Islam TS, Feng M, Hodis HN, Künzli N, Avol E. Carotid artery intima-media thickness in college students: race/ethnicity matters. Atherosclerosis. 2011;217:441–446. doi: 10.1016/j.atherosclerosis.2011.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.Havranek EP, Froshaug DB, Emserman CD, Hanratty R, Krantz MJ, Masoudi FA, Dickinson LM, Steiner JF. Left ventricular hypertrophy and cardiovascular mortality by race and ethnicity. Am J Med. 2008;121:870–875. doi: 10.1016/j.amjmed.2008.05.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343.Jain A, Tandri H, Dalal D, Chahal H, Soliman EZ, Prineas RJ, Folsom AR, Lima JA, Bluemke DA. Diagnostic and prognostic utility of electrocardiography for left ventricular hypertrophy defined by magnetic resonance imaging in relationship to ethnicity: the Multi-Ethnic Study of Atherosclerosis (MESA) Am Heart J. 2010;159:652–658. doi: 10.1016/j.ahj.2009.12.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344.Gardin JM, Allebban Z, Wong ND, Sklar SK, Bess RL, Spence MA, Pershadsingh HA, Detrano R. Do differences in subclinical cardiovascular disease in Mexican Americans versus European Americans help explain the Hispanic paradox? Am J Cardiol. 2010;105:205–209. doi: 10.1016/j.amjcard.2009.08.673. [DOI] [PubMed] [Google Scholar]
- 345.Rodriguez CJ, Diez-Roux AV, Moran A, Jin Z, Kronmal RA, Lima J, Homma S, Bluemke DA, Barr RG. Left ventricular mass and ventricular remodeling among Hispanic subgroups compared with non-Hispanic blacks and whites: MESA (Multi-Ethnic Study of Atherosclerosis) J Am Coll Cardiol. 2010;55:234–242. doi: 10.1016/j.jacc.2009.08.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346.Bao W, Threefoot SA, Srinivasan SR, Berenson GS. Essential hypertension predicted by tracking of elevated blood pressure from childhood to adulthood: the Bogalusa Heart Study. Am J Hypertens. 1995;8:657–665. doi: 10.1016/0895-7061(95)00116-7. [DOI] [PubMed] [Google Scholar]
- 347.Freedman DS, Patel DA, Srinivasan SR, Chen W, Tang R, Bond MG, Berenson GS. The contribution of childhood obesity to adult carotid intima-media thickness: the Bogalusa Heart Study. Int J Obes (Lond) 2008;32:749–756. doi: 10.1038/sj.ijo.0803798. [DOI] [PubMed] [Google Scholar]
- 348.Juonala M, Magnussen CG, Berenson GS, Venn A, Burns TL, Sabin MA, Srinivasan SR, Daniels SR, Davis PH, Chen W, Sun C, Cheung M, Viikari JS, Dwyer T, Raitakari OT. Childhood adiposity, adult adiposity, and cardiovascular risk factors. N Engl J Med. 2011;365:1876–1885. doi: 10.1056/NEJMoa1010112. [DOI] [PubMed] [Google Scholar]
- 349.Magnussen CG, Koskinen J, Chen W, Thomson R, Schmidt MD, Srinivasan SR, Kivimäki M, Mattsson N, Kähönen M, Laitinen T, Taittonen L, Rönnemaa T, Viikari JS, Berenson GS, Juonala M, Raitakari OT. Pediatric metabolic syndrome predicts adulthood metabolic syndrome, subclinical atherosclerosis, and type 2 diabetes mellitus but is no better than body mass index alone: the Bogalusa Heart Study and the Cardiovascular Risk in Young Finns Study. Circulation. 2010;122:1604–1611. doi: 10.1161/CIRCULATIONAHA.110.940809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 350.Saydah S, Bullard KM, Imperatore G, Geiss L, Gregg EW. Cardiometabolic risk factors among US adolescents and young adults and risk of early mortality. Pediatrics. 2013;131:e679–e686. doi: 10.1542/peds.2012-2583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351.Attard SM, Herring AH, Howard AG, Gordon-Larsen P. Longitudinal trajectories of BMI and cardiovascular disease risk: the National Longitudinal Study of Adolescent Health. Obesity (Silver Spring) 2013;21:2180–2188. doi: 10.1002/oby.20569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 352.Daviglus ML, Pirzada A, Van Horn L. Ethnic disparities in cardiovascular risk factors in children and adolescents. Curr Cardiovasc Risk Rep. 2014;8:376. [Google Scholar]
- 353.Johnston LD, O’Malley PM, Bachman JG, Scholenberg JE. Monitoring the Future: National Survey Results on Drug Use, 1975–2006: Volume 1: Secondary School Students. Bethesda, MD: National Institute on Drug Abuse; 2007. NIH publication No 07-6205. [Google Scholar]
- 354.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity in the United States, 2009–2010. NCHS Data Brief. 2012;(82):1–8. [PubMed] [Google Scholar]
- 355.Harrington S. Overweight in Latino/Hispanic adolescents: scope of the problem and nursing implications. Pediatr Nurs. 2008;34:389–394. [PubMed] [Google Scholar]
- 356.Lindsay AC, Sussner KM, Greaney ML, Peterson KE. Latina mothers’ beliefs and practices related to weight status, feeding, and the development of child overweight. Public Health Nurs. 2011;28:107–118. doi: 10.1111/j.1525-1446.2010.00906.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 357.Baughcum AE, Burklow KA, Deeks CM, Powers SW, Whitaker RC. Maternal feeding practices and childhood obesity: a focus group study of low-income mothers. Arch Pediatr Adolesc Med. 1998;152:1010–1014. doi: 10.1001/archpedi.152.10.1010. [DOI] [PubMed] [Google Scholar]
- 358.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311:806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359.The NS, Richardson AS, Gordon-Larsen P. Timing and duration of obesity in relation to diabetes: findings from an ethnically diverse, nationally representative sample. Diabetes Care. 2013;36:865–872. doi: 10.2337/dc12-0536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 360.Franks PW, Hanson RL, Knowler WC, Sievers ML, Bennett PH, Looker HC. Childhood obesity, other cardiovascular risk factors, and premature death. N Engl J Med. 2010;362:485–493. doi: 10.1056/NEJMoa0904130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 361.Messiah SE, Arheart KL, Lopez-Mitnik G, Lipshultz SE, Miller TL. Ethnic group differences in cardiometabolic disease risk factors independent of body mass index among American youth. Obesity (Silver Spring) 2013;21:424–428. doi: 10.1002/oby.20343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362.Marcus MD, Baranowski T, DeBar LL, Edelstein S, Kaufman FR, Schneider M, Siega-Riz AM, Staten MA, Virus A, Yin Z. Severe obesity and selected risk factors in a sixth grade multiracial cohort: the HEALTHY study. J Adolesc Health. 2010;47:604–607. doi: 10.1016/j.jadohealth.2010.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 363.Toledo-Corral CM, Ventura EE, Hodis HN, Weigensberg MJ, Lane CJ, Li Y, Goran MI. Persistence of the metabolic syndrome and its influence on carotid artery intima media thickness in overweight Latino children. Atherosclerosis. 2009;206:594–598. doi: 10.1016/j.atherosclerosis.2009.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 364.Ahn MK, Juon HS, Gittelsohn J. Association of race/ethnicity, socioeconomic status, acculturation, and environmental factors with risk of overweight among adolescents in California, 2003. Prev Chronic Dis. 2008;5:A75. [PMC free article] [PubMed] [Google Scholar]
- 365.Gordon-Larsen P, Harris KM, Ward DS, Popkin BM National Longitudinal Study of Adolescent Health. . Acculturation and overweight-related behaviors among Hispanic immigrants to the US: the National Longitudinal Study of Adolescent Health. Soc Sci Med. 2003;57:2023–2034. doi: 10.1016/s0277-9536(03)00072-8. [DOI] [PubMed] [Google Scholar]
- 366.Popkin BM, Udry JR. Adolescent obesity increases significantly in second and third generation U.S. immigrants: the National Longitudinal Study of Adolescent Health. J Nutr. 1998;128:701–706. doi: 10.1093/jn/128.4.701. [DOI] [PubMed] [Google Scholar]
- 367.Liu JH, Chu YH, Frongillo EA, Probst JC. Generation and acculturation status are associated with dietary intake and body weight in Mexican American adolescents. J Nutr. 2012;142:298–305. doi: 10.3945/jn.111.145516. [DOI] [PubMed] [Google Scholar]
- 368.Caprio S, Daniels SR, Drewnowski A, Kaufman FR, Palinkas LA, Rosenbloom AL, Schwimmer JB. Influence of race, ethnicity, and culture on childhood obesity: implications for prevention and treatment: a consensus statement of Shaping America’s Health and the Obesity Society. Diabetes Care. 2008;31:2211–2221. doi: 10.2337/dc08-9024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 369.Monsivais P, Drewnowski A. The rising cost of low-energy-density foods. J Am Diet Assoc. 2007;107:2071–2076. doi: 10.1016/j.jada.2007.09.009. [DOI] [PubMed] [Google Scholar]
- 370.Ayala GX, Carnethon M, Arredondo E, Delamater AM, Perreira K, Van Horn L, Himes JH, Eckfeldt JH, Bangdiwala SI, Santisteban DA, Isasi CR. Theoretical foundations of the Study of Latino (SOL) Youth: implications for obesity and cardiometabolic risk. Ann Epidemiol. 2014;24:36–43. doi: 10.1016/j.annepidem.2013.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 371.Goodman E, McEwen BS, Huang B, Dolan LM, Adler NE. Social inequalities in biomarkers of cardiovascular risk in adolescence. Psychosom Med. 2005;67:9–15. doi: 10.1097/01.psy.0000149254.36133.1a. [DOI] [PubMed] [Google Scholar]
- 372.Kakinami L, Seguin L, Lambert M, Gauvin L, Nikiema B, Paradis G. Comparison of three lifecourse models of poverty in predicting cardiovascular disease risk in youth. Ann Epidemiol. 2013;23:485–491. doi: 10.1016/j.annepidem.2013.05.012. [DOI] [PubMed] [Google Scholar]
- 373.Nichaman MZ, Wear ML, Goff DC, Jr, Labarthe DR. Hospitalization rates for myocardial infarction among Mexican-Americans and non-Hispanic whites: the Corpus Christi Heart Project. Ann Epidemiol. 1993;3:42–48. doi: 10.1016/1047-2797(93)90008-r. [DOI] [PubMed] [Google Scholar]
- 374.Eamranond PP, Davis RB, Phillips RS, Wee CC. Patient-physician language concordance and primary care screening among Spanish-speaking patients. Med Care. 2011;49:668–672. doi: 10.1097/MLR.0b013e318215d803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 375.Mitchell BD, Hazuda HP, Haffner SM, Patterson JK, Stern MP. Myocardial infarction in Mexican-Americans and non-Hispanic whites: the San Antonio Heart Study. Circulation. 1991;83:45–51. doi: 10.1161/01.cir.83.1.45. [DOI] [PubMed] [Google Scholar]
- 376.Otiniano ME, Du XL, Maldonado MR, Ray L, Markides K. Effect of metabolic syndrome on heart attack and mortality in Mexican-American elderly persons: findings of 7-year follow-up from the Hispanic established population for the Epidemiological Study of the Elderly. J Gerontol A Biol Sci Med Sci. 2005;60:466–470. doi: 10.1093/gerona/60.4.466. [DOI] [PubMed] [Google Scholar]
- 377.Amin AP, Nathan S, Evans AT, Attanasio S, Mukhopadhyay E, Mehta V, Kelly RF. The effect of ethnicity on the relationship between premature coronary artery disease and traditional cardiac risk factors among uninsured young adults. Prev Cardiol. 2009;12:128–135. doi: 10.1111/j.1751-7141.2009.00025.x. [DOI] [PubMed] [Google Scholar]
- 378.Shaw LJ, Shaw RE, Merz CN, Brindis RG, Klein LW, Nallamothu B, Douglas PS, Krone RJ, McKay CR, Block PC, Hewitt K, Weintraub WS, Peterson ED on behalf of the American College of Cardiology-National Cardiovascular Data Registry Investigators. . Impact of ethnicity and gender differences on angiographic coronary artery disease prevalence and in-hospital mortality in the American College of Cardiology-National Cardiovascular Data Registry. Circulation. 2008;117:1787–1801. doi: 10.1161/CIRCULATIONAHA.107.726562. [DOI] [PubMed] [Google Scholar]
- 379.Smith MA, Risser JM, Lisabeth LD, Moye LA, Morgenstern LB. Access to care, acculturation, and risk factors for stroke in Mexican Americans: the Brain Attack Surveillance in Corpus Christi (BASIC) project. Stroke. 2003;34:2671–2675. doi: 10.1161/01.STR.0000096459.62826.1F. [DOI] [PubMed] [Google Scholar]
- 380.White H, Boden-Albala B, Wang C, Elkind MS, Rundek T, Wright CB, Sacco RL. Ischemic stroke subtype incidence among whites, blacks, and Hispanics: the Northern Manhattan Study. Circulation. 2005;111:1327–1331. doi: 10.1161/01.CIR.0000157736.19739.D0. [DOI] [PubMed] [Google Scholar]
- 381.Rodriguez CJ, Homma S, Sacco RL, Di Tullio MR, Sciacca RR, Mohr JP for the PICSS Investigators. . Race-ethnic differences in patent foramen ovale, atrial septal aneurysm, and right atrial anatomy among ischemic stroke patients. Stroke. 2003;34:2097–2102. doi: 10.1161/01.STR.0000085828.67563.42. [DOI] [PubMed] [Google Scholar]
- 382.Centers for Disease Control and Prevention (CDC). . Prevalence of stroke: United States, 2006–2010. MMWR Morb Mortal Wkly Rep. 2012;61:379–382. [PubMed] [Google Scholar]
- 383.Moon JR, Capistrant BD, Kawachi I, Avendaño M, Subramanian SV, Bates LM, Glymour MM. Stroke incidence in older US Hispanics: is foreign birth protective? Stroke. 2012;43:1224–1229. doi: 10.1161/STROKEAHA.111.643700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 384.Bahrami H, Kronmal R, Bluemke DA, Olson J, Shea S, Liu K, Burke GL, Lima JA. Differences in the incidence of congestive heart failure by ethnicity: the Multi-Ethnic Study of Atherosclerosis. Arch Intern Med. 2008;168:2138–2145. doi: 10.1001/archinte.168.19.2138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 385.Vivo RP, Krim SR, Cevik C, Witteles RM. Heart failure in Hispanics. J Am Coll Cardiol. 2009;53:1167–1175. doi: 10.1016/j.jacc.2008.12.037. [DOI] [PubMed] [Google Scholar]
- 386.Aronow WS, Ahn C, Kronzon I. Comparison of incidences of congestive heart failure in older African-Americans, Hispanics, and whites. Am J Cardiol. 1999;84:611–612. A9. doi: 10.1016/s0002-9149(99)00392-6. [DOI] [PubMed] [Google Scholar]
- 387.Alexander M, Grumbach K, Remy L, Rowell R, Massie BM. Congestive heart failure hospitalizations and survival in California: patterns according to race/ethnicity. Am Heart J. 1999;137:919–927. doi: 10.1016/s0002-8703(99)70417-5. [DOI] [PubMed] [Google Scholar]
- 388.Vivo RP, Krim SR, Krim NR, Zhao X, Hernandez AF, Peterson ED, Piña IL, Bhatt DL, Schwamm LH, Fonarow GC. Care and outcomes of Hispanic patients admitted with heart failure with preserved or reduced ejection fraction: findings from Get With The Guidelines–Heart Failure. Circ Heart Fail. 2012;5:167–175. doi: 10.1161/CIRCHEARTFAILURE.111.963546. [DOI] [PubMed] [Google Scholar]
- 389.Morrissey J, Giacovelli J, Egorova N, Gelijns A, Moskowitz A, McKinsey J, Kent KC, Greco G. Disparities in the treatment and outcomes of vascular disease in Hispanic patients. J Vasc Surg. 2007;46:971–978. doi: 10.1016/j.jvs.2007.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 390.Lavery LA, Ashry HR, van Houtum W, Pugh JA, Harkless LB, Basu S. Variation in the incidence and proportion of diabetes-related amputations in minorities. Diabetes Care. 1996;19:48–52. doi: 10.2337/diacare.19.1.48. [DOI] [PubMed] [Google Scholar]
- 391.Allison MA, Criqui MH, McClelland RL, Scott JM, McDermott MM, Liu K, Folsom AR, Bertoni AG, Sharrett AR, Homma S, Kori S. The effect of novel cardiovascular risk factors on the ethnic-specific odds for peripheral arterial disease in the Multi-Ethnic Study of Atherosclerosis (MESA) J Am Coll Cardiol. 2006;48:1190–1197. doi: 10.1016/j.jacc.2006.05.049. [DOI] [PubMed] [Google Scholar]
- 392.Collins TC, Petersen NJ, Suarez-Almazor M, Ashton CM. The prevalence of peripheral arterial disease in a racially diverse population. Arch Intern Med. 2003;163:1469–1474. doi: 10.1001/archinte.163.12.1469. [DOI] [PubMed] [Google Scholar]
- 393.Mendelson G, Aronow WS, Ahn C. Prevalence of coronary artery disease, atherothrombotic brain infarction, and peripheral arterial disease: associated risk factors in older Hispanics in an academic hospital-based geriatrics practice. J Am Geriatr Soc. 1998;46:481–483. doi: 10.1111/j.1532-5415.1998.tb02470.x. [DOI] [PubMed] [Google Scholar]
- 394.Hirsch AT, Haskal ZJ, Hertzer NR, Bakal CW, Creager MA, Halperin JL, Hiratzka LF, Murphy WR, Olin JW, Puschett JB, Rosenfield KA, Sacks D, Stanley JC, Taylor LM, Jr, White CJ, White J, White RA. ACC/AHA 2005 practice guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease. Circulation. 2006;113:e463–e654. doi: 10.1161/CIRCULATIONAHA.106.174526. [DOI] [PubMed] [Google Scholar]
- 395.Allison MA, Peralta CA, Wassel CL, Aboyans V, Arnett DK, Cushman M, Eng J, Ix J, Rich SS, Criqui MH. Genetic ancestry and lower extremity peripheral artery disease in the Multi-Ethnic Study of Atherosclerosis. Vasc Med. 2010;15:351–359. doi: 10.1177/1358863X10375586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 396.Zheng ZJ, Croft JB, Giles WH, Mensah GA. Sudden cardiac death in the United States, 1989 to 1998. Circulation. 2001;104:2158–2163. doi: 10.1161/hc4301.098254. [DOI] [PubMed] [Google Scholar]
- 397.Gillum RF. Sudden cardiac death in Hispanic Americans and African Americans. Am J Public Health. 1997;87:1461–1466. doi: 10.2105/ajph.87.9.1461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 398.Deo R, Albert CM. Epidemiology and genetics of sudden cardiac death. Circulation. 2012;125:620–637. doi: 10.1161/CIRCULATIONAHA.111.023838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 399.Murphy SL, Xu J, Kochanek KD. National Vital Statistics Reports. 4. Vol. 60. Hyattsville, MD: National Center for Health Statistics; 2012. Deaths: preliminary data for 2010. [Google Scholar]
- 400.Hoyert DL, Kung HC, Smith BL. National Vital Statistics Reports. 15. Vol. 53. Hyattsville, MD: National Center for Health Statistics; 2005. Deaths: preliminary data for 2003. [PubMed] [Google Scholar]
- 401.Centers for Disease Control and Prevention, National Center for Health Statistics. Compressed mortality data. Series 20 No. 2P. [Accessed February 12, 2014];CDC WONDER Online Database [database online] Released January 2013. http://wonder.cdc.gov/cmf-icd10.html.
- 402.Karno M, Edgerton RB. Perception of mental illness in a Mexican-American community. Arch Gen Psychiatry. 1969;20:233–238. doi: 10.1001/archpsyc.1969.01740140105013. [DOI] [PubMed] [Google Scholar]
- 403.Teller CH, Clyburn S. Trends in infant mortality. Tex Bus Rev. 1974;48:240–246. [Google Scholar]
- 404.Markides KS. Mortality among minority populations: a review of recent patterns and trends. Public Health Reports. 1983;98:252–260. [PMC free article] [PubMed] [Google Scholar]
- 405.Sorlie PD, Backlund E, Johnson NJ, Rogot E. Mortality by Hispanic status in the United States. JAMA. 1993;270:2464–2468. [PubMed] [Google Scholar]
- 406.Borrell LN, Lancet EA. Race/ethnicity and all-cause mortality in US adults: revisiting the Hispanic paradox. Am J Public Health. 2012;102:836–843. doi: 10.2105/AJPH.2011.300345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 407.Pablos-Méndez A. Mortality among Hispanics. JAMA. 1994;271:1237. [PubMed] [Google Scholar]
- 408.Marmot MG, Adelstein AM, Bulusu L. Lessons from the study of immigrant mortality. Lancet. 1984;1:1455–1457. doi: 10.1016/s0140-6736(84)91943-3. [DOI] [PubMed] [Google Scholar]
- 409.Abraído-Lanza AF, Dohrenwend BP, Ng-Mak DS, Turner JB. The Latino mortality paradox: a test of the “salmon bias” and healthy migrant hypotheses. Am J Public Health. 1999;89:1543–1548. doi: 10.2105/ajph.89.10.1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 410.Hunt KJ, Resendez RG, Williams K, Haffner SM, Stern MP, Hazuda HP. All-cause and cardiovascular mortality among Mexican-American and non-Hispanic White older participants in the San Antonio Heart Study: evidence against the “Hispanic paradox”. Am J Epidemiol. 2003;158:1048–1057. doi: 10.1093/aje/kwg249. [DOI] [PubMed] [Google Scholar]
- 411.Pandey DK, Labarthe DR, Goff DC, Chan W, Nichaman MZ. Community-wide coronary heart disease mortality in Mexican Americans equals or exceeds that in non-Hispanic whites: the Corpus Christi Heart Project. Am J Med. 2001;110:81–87. doi: 10.1016/s0002-9343(00)00667-7. [DOI] [PubMed] [Google Scholar]
- 412.Hummer RA. Adult mortality differentials among Hispanic subgroups and non-Hispanic whites. Soc Sci Q. 2000;81:459–476. [PubMed] [Google Scholar]
- 413.Hajat A, Lucas JB, Kington R. Health outcomes among Hispanic subgroups: data from the National Health Interview Survey, 1992–95. Adv Data. 2000;(310):1–14. [PubMed] [Google Scholar]
- 414.Goel MS, McCarthy EP, Phillips RS, Wee CC. Obesity among US immigrant subgroups by duration of residence. JAMA. 2004;292:2860–2867. doi: 10.1001/jama.292.23.2860. [DOI] [PubMed] [Google Scholar]
- 415.Wolf CB, Portis M. Smoking, acculturation, and pregnancy outcome among Mexican Americans. Health Care Women Int. 1996;17:563–573. [PubMed] [Google Scholar]
- 416.NHLBI Working Group. Epidemiologic Research in Hispanic Populations Opportunities, Barriers and Solutions: Working Group, July 31–August 1, 2003, Bethesda, MD: Summary and Recommendations. Bethesda, MD: National Heart, Lung, and Blood Institute; 2003. [Google Scholar]
- 417.HHS announces the nation’s new health promotion and disease prevention agenda [news release] Washington, DC: US Department of Health and Human Services; Dec 2, 2010. [Accessed December 8, 2012]. http://www.healthypeople.gov/2020/about/DefaultPressRelease.pdf. [Google Scholar]
- 418.National Prevention Council, US Department of Health and Human Services. National Prevention Strategy. Washington, DC: Office of the Surgeon General; 2011. [Accessed November 16, 2012]. http://www.surgeongeneral.gov/initiatives/prevention/strategy/ [Google Scholar]
- 419.Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, Finkelstein EA, Hong Y, Johnston SC, Khera A, Lloyd-Jones DM, Nelson SA, Nichol G, Orenstein D, Wilson PW, Woo YJ on behalf of the American Heart Association Advocacy Coordinating Committee; Stroke Council; Council on Cardiovascular Radiology and Intervention; Council on Clinical Cardiology; Council on Epidemiology and Prevention; Council on Arteriosclerosis; Thrombosis and Vascular Biology; Council on Cardiopulmonary;CriticalCare;PerioperativeandResuscitation;Councilon Cardiovascular Nursing; Council on the Kidney in Cardiovascular Disease; Council on Cardiovascular Surgery and Anesthesia, and Interdisciplinary Council on Quality of Care and Outcomes Research. . Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123:933–944. doi: 10.1161/CIR.0b013e31820a55f5. [DOI] [PubMed] [Google Scholar]