Abstract
Study Design Case report.
Objective To describe a patient with a recurrent spontaneous spinal epidural hematoma (SSEH) during pregnancy that had spontaneous remission.
Methods A 27-year-old primigravida at 37 weeks' gestation suddenly felt a strong left shoulder pain without any trauma. She had a history of fenestration for a spontaneous cervical hematoma when she was 18 years old. An emergency magnetic resonance imaging revealed a recurrence of the cervical epidural hematoma at the C4–T1 level, but she had no paralysis.
Results The patient subsequently underwent a cesarean section and delivered a healthy male infant. Her spinal epidural hematoma disappeared. Multislice computed tomography showed no evidence for a vascular malformation or tumor. Three years after the initial cesarean section, she underwent a second one and delivered another male infant.
Conclusions We report on a rare case of recurrent SSEH during pregnancy with no neurologic deficits that was treated nonoperatively with close observation and resulted in spontaneous resolution. In such patients with no neurologic deficits, nonoperative management with close observation may be a reasonable alternative.
Keywords: recurrent, cervical, epidural hematoma, spontaneous resolution, pregnancy, spontaneous spinal epidural hematoma, cesarean section
Introduction
Spontaneous spinal epidural hematoma (SSEH) is a rare condition of unknown origin typically produced by the rupture of an epidural vein. It usually presents when a healthy adult engaged in a normal activity suddenly develops back or neck pain.1 There have been many reports of SSEH,2 3 4 but few during pregnancy.5 6 7 8 9 10 11 12 13 14 15 16 In general, recurrent SSEHs are uncommon.17 18 19 20 We report a case of SSEH recurrence during pregnancy and its spontaneous resolution.
Case Report
A 27-year-old primigravida at 37 weeks' gestation suddenly felt a strong pain in her left shoulder and was admitted to the hospital emergency room. She denied any history of trauma and cited neither hypertensive disorders nor comorbidities during the term of her pregnancy. However, she had a history of fenestration surgery for SSEH (Frankel A) at 18 years old (Figs. 1 and 2) with complete recovery. Her laboratory test results including the clotting parameters were normal. Her blood pressure was 177/97 mmHg, pulse rate was 83 beats per minute, and temperature was 36.4°C. The first doctor she met in the emergency room was a neurosurgeon. He performed a full physical examination. Her sole symptom remained severe pain without neurologic deficit. He suspected a recurrence of the SSEH from her past medical history and her recollection of a similarly intense pain experienced only once before during her first SSEH.
Fig. 1.
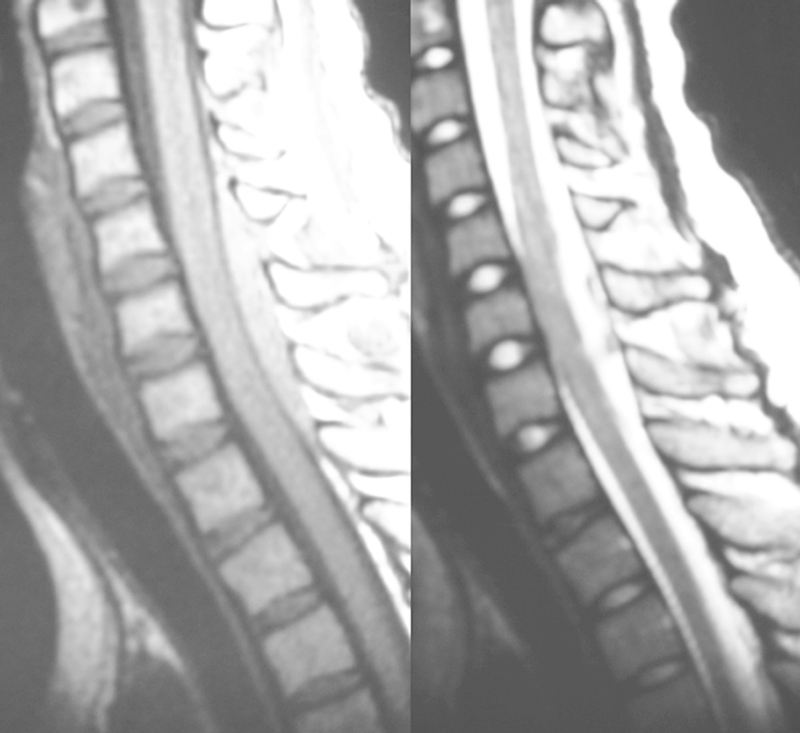
T1W1-weighted (left) and T2W1-weighted (right) magnetic resonance imaging showing the cervical epidural hematoma at the C4–T1 level at 18 years old.
Fig. 2.
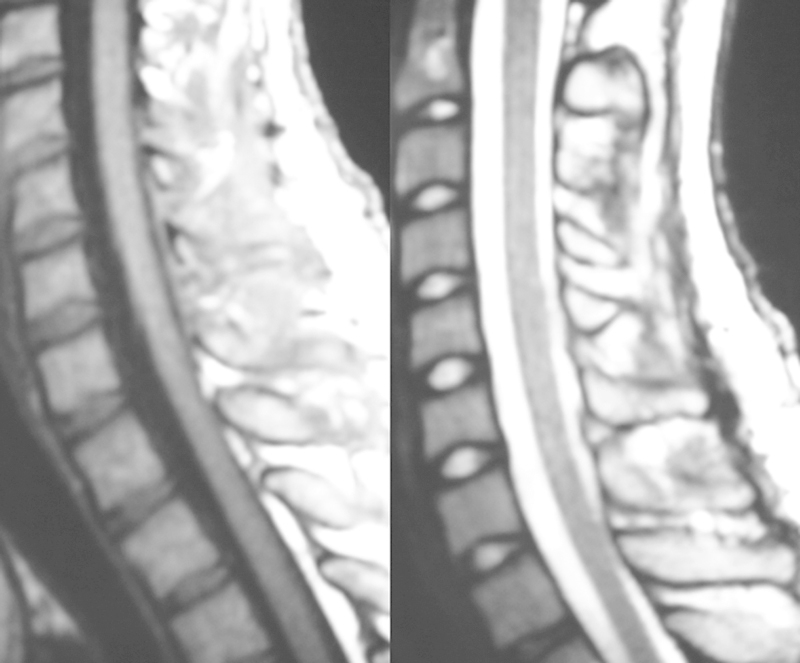
T1W1-weighted (left) and T2W1-weighted (right) magnetic resonance imaging showing that the cervical epidural hematoma disappeared after operation at 18 years old.
An emergency magnetic resonance imaging (MRI) revealed a cervical epidural hematoma at the C4–T1 level (Fig. 3). The orthopedic and obstetric doctors recommended a cesarean section for delivery and observation without steroids for the SSEH. On the day following admission, a cesarean section was performed under general anesthesia and a healthy male infant weighing 3,256 g was delivered. During recovery, her neurologic status did not deteriorate. She was discharged with no pain or neurologic deficit 7 days later.
Fig. 3.

T1W1-weighted (left) and T2W1-weighted (right) magnetic resonance imaging showing the epidural hematoma at the C4–T1 level at 27 years old. Sagittal view and axial view (C6 level).
At her 1-month follow-up, an MRI showed that the epidural hematoma had disappeared (Fig. 4). Multislice computed tomography showed no evidence of a vascular malformation or tumor. Three years later, she underwent a second cesarean section and gave birth to a male infant without recurrence of SSEH.
Fig. 4.
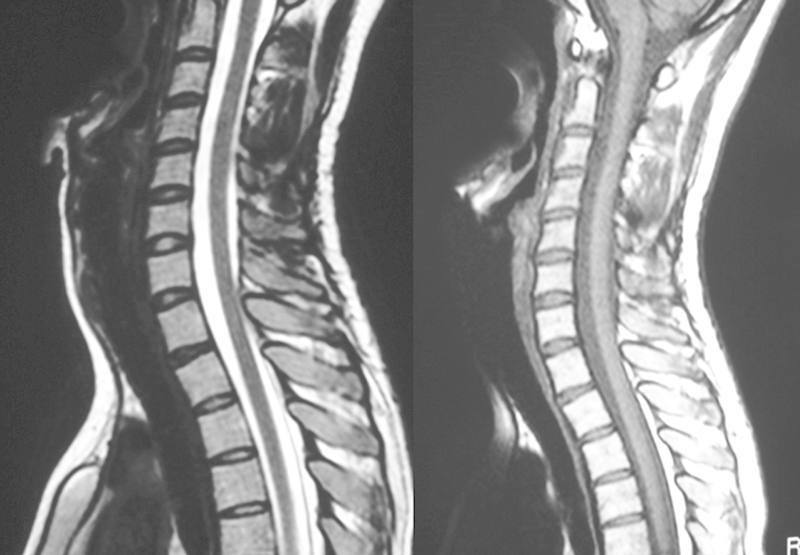
T1W1-weighted (left) and T2W1-weighted (right) magnetic resonance imaging showing that the epidural hematoma at the C4–T1 level disappeared at 1-month follow-up.
Discussion
Our case of recurrent SSEH with spontaneous resolution during pregnancy is unusual. The recommended treatment for this medical condition is commonly a surgical decompression to prevent neurologic deficit.21 Previous reports suggest that the prognostic factors were strongly correlated with the timing of the surgical decompression; therefore, an immediate decompression was recommended.21 The outcomes were better if the surgery was performed within 48 hours (in cases with incomplete spinal cord dysfunction) or 36 hours (in cases with complete spinal cord dysfunction).3
Several authors have reported cases of spontaneous resolution of SSEH without an operative intervention.4 22 23 24 However, the conservative treatment has often resulted in a poor clinical outcome. We have no definitive tools to identify the patients who may recover spontaneously.22 If there is no motor function improvement, the treatment in most cases should be an immediate decompression.22 23 24
The strategies must be determined for both the mother's neurologic disorder and the fetus' well-being. Babies born before 37 weeks of pregnancy are defined as extremely preterm (<28 weeks), very preterm (28 to <32 weeks), and moderate to late preterm (32 to <37 weeks).25 Any child born at 36 weeks or earlier is considered a preemie. The organ function of the fetus is still immature, specifically the pulmonary capacity.26 There have been a small number of reports of pregnant women with an SSEH.5 6 7 8 9 10 11 12 13 14 15 16 Three cases before 31 weeks' gestation were carried through term, but almost all infants born after 32 weeks were delivered by cesarean section. From 32 to 36 weeks, it is very difficult to decide if the best course of action is to deliver the baby or to continue the pregnancy. The prone position for the spine operation as well as the general anesthesia required have associated risks for the fetus; however, if the pregnancy is sustained, the risk for respiratory distress syndrome and other respiratory morbidity can be reduced.26 In the studies reviewed, all of the women experienced neurologic deficits and were managed operatively5 6 7 8 9 10 11 12 13 14 15 16; therefore, this is the first case of spontaneous resolution. We chose nonoperative management with close observation for this patient because she had no neurologic deficit, only pain.
SSEH during pregnancy is an acute neurologic emergency, and a universally accepted idea is that this condition may be a consequence of venous bleeding. During pregnancy, women are in a hypercoagulable state, making it less likely for hematomas to develop. However, sudden changes in the central venous pressure can be transmitted directly from the visceral cavities to the epidural veins.15 According to Steinmetz et al,9 as the uterus and fetus enlarge during the late stages of pregnancy, the abdominal and pelvic venous dynamics are altered.15 This fluctuation in the venous pressures may lead to the rupture of a pre-existing pathologic venous wall.6 15
Hypertension is a major cause of hematoma. Hypertensive disorders associated with pregnancy are one of the most common obstetric problems. Upon arrival in the emergency room, our patient's blood pressure was elevated, although after admission it was monitored strictly and returned to normal. We cannot definitively conclude if temporary high blood pressure caused the bleeding or if pain made her blood pressure higher.
Cases of relapse have rarely been reported, and at initial presentation, all cases were treated conservatively, achieving a spontaneous resolution.17 18 19 20 The recurrent intervals were a few minutes to 3 years.18 19 This patient's recurrence interval was about 10 years. The hospital that operated on her at age 18 for the initial SSEH performed the fenestration and aspirated the hematoma. Many patients undergo a cervical laminectomy or laminoplasty, and these operations might be needed to prevent recurrences.
Conclusion
We report on a rare case of recurrent SSEH during pregnancy with no neurologic deficits that was treated nonoperatively with close observation and resulted in spontaneous resolution. In such patients with no neurologic deficits, nonoperative management with close observation may be a reasonable alternative.
Footnotes
Disclosures Katsuyuki Iwatsuki, none Masao Deguchi, none Hitoshi Hirata, none Toshihisa Kanamono, none
References
- 1.McQuarrie I G. Recovery from paraplegia caused by spontaneous spinal epidural hematoma. Neurology. 1978;28(3):224–228. doi: 10.1212/wnl.28.3.224. [DOI] [PubMed] [Google Scholar]
- 2.Foo D, Rossier A B. Preoperative neurological status in predicting surgical outcome of spinal epidural hematomas. Surg Neurol. 1981;15(5):389–401. doi: 10.1016/0090-3019(81)90178-6. [DOI] [PubMed] [Google Scholar]
- 3.Groen R J van Alphen H A Operative treatment of spontaneous spinal epidural hematomas: a study of the factors determining postoperative outcome Neurosurgery 1996393494–508., discussion 508–509 [DOI] [PubMed] [Google Scholar]
- 4.Groen R J. Non-operative treatment of spontaneous spinal epidural hematomas: a review of the literature and a comparison with operative cases. Acta Neurochir (Wien) 2004;146(2):103–110. doi: 10.1007/s00701-003-0160-9. [DOI] [PubMed] [Google Scholar]
- 5.Bidzinski J. Spontaneous spinal epidural hematoma during pregnancy. Case report. J Neurosurg. 1966;24(6):1017. doi: 10.3171/jns.1966.24.6.1017. [DOI] [PubMed] [Google Scholar]
- 6.Yonekawa Y, Mehdorn H M, Nishikawa M. Spontaneous spinal epidural hematoma during pregnancy. Surg Neurol. 1975;3(6):327–328. [PubMed] [Google Scholar]
- 7.Mahieu X, Kridelka F, Pintiaux A. et al. [Spontaneous cervical extradural hematoma in a pregnant woman] J Gynecol Obstet Biol Reprod (Paris) 1994;23(1):99–102. [PubMed] [Google Scholar]
- 8.Carroll S G, Malhotra R, Eustace D, Sharr M, Morcos S. Spontaneous spinal extradural hematoma during pregnancy. J Matern Fetal Med. 1997;6(4):218–219. doi: 10.1002/(SICI)1520-6661(199707/08)6:4<218::AID-MFM6>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 9.Steinmetz M P, Kalfas I H, Willis B, Chalavi A, Harlan R C. Successful surgical management of a case of spontaneous epidural hematoma of the spine during pregnancy. Spine J. 2003;3(6):539–542. [PubMed] [Google Scholar]
- 10.Masski G, Housni B, Ibahiouin K, Miguil M. Spontaneous cervical epidural haematoma during pregnancy. Int J Obstet Anesth. 2004;13(2):103–106. doi: 10.1016/j.ijoa.2003.09.006. [DOI] [PubMed] [Google Scholar]
- 11.Jea A Moza K Levi A D Vanni S Spontaneous spinal epidural hematoma during pregnancy: case report and literature review Neurosurgery 2005565E1156, discussion E1156 [PubMed] [Google Scholar]
- 12.Kelly M E, Beavis R C, Hattingh S. Spontaneous spinal epidural hematoma during pregnancy. Can J Neurol Sci. 2005;32(3):361–365. doi: 10.1017/s0317167100004297. [DOI] [PubMed] [Google Scholar]
- 13.Consolo D, Vadala A A, Rollin P, Merle B, Girard C. [Spontaneous spinal epidural haematoma during pregnancy] Ann Fr Anesth Reanim. 2007;26(5):455–458. doi: 10.1016/j.annfar.2007.01.019. [DOI] [PubMed] [Google Scholar]
- 14.Singh D P, Lamtha S C, Kumar S. Spontaneous spinal epidural haematoma during pregnancy. J Assoc Physicians India. 2009;57:540–542. [PubMed] [Google Scholar]
- 15.Wang P, Xin X T, Lan H, Chen C, Liu B. Spontaneous cervical epidural hematoma during pregnancy: case report and literature review. Eur Spine J. 2011;20 02:S176–S179. doi: 10.1007/s00586-010-1484-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Matsubara S, Inoue H, Takamura K. et al. Spontaneous spinal epidural hematoma at the 16th week of a twin pregnancy. J Obstet Gynaecol Res. 2011;37(10):1466–1469. doi: 10.1111/j.1447-0756.2010.01522.x. [DOI] [PubMed] [Google Scholar]
- 17.Abram H S, DeLaHunt M J, Merinbaum D J, Hammond D N. Recurrent spontaneous spinal epidural hematoma in a child: first case report. Pediatr Neurol. 2007;36(3):177–180. doi: 10.1016/j.pediatrneurol.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 18.Hernandez D, Vinuela F, Feasby T E. Recurrent paraplegia with total recovery from spontaneous spinal epidural hematoma. Ann Neurol. 1982;11(6):623–624. doi: 10.1002/ana.410110611. [DOI] [PubMed] [Google Scholar]
- 19.Matsumae M, Shimoda M, Shibuya N, Ueda M, Yamamoto I, Sato O. Spontaneous cervical epidural hematoma. Surg Neurol. 1987;28(5):381–384. doi: 10.1016/0090-3019(87)90062-0. [DOI] [PubMed] [Google Scholar]
- 20.Sano H, Satomi K, Hirano J. Recurrent idiopathic epidural hematoma: a case report. J Orthop Sci. 2004;9(6):625–628. doi: 10.1007/s00776-004-0821-4. [DOI] [PubMed] [Google Scholar]
- 21.Liao C C Lee S T Hsu W C Chen L R Lui T N Lee S C Experience in the surgical management of spontaneous spinal epidural hematoma J Neurosurg 2004100(1, Suppl Spine ):38–45. [DOI] [PubMed] [Google Scholar]
- 22.Aoki Y, Yamagata M, Shimizu K. et al. An unusually rapid spontaneous recovery in a patient with spinal epidural hematoma. J Emerg Med. 2012;43(2):e75–e79. doi: 10.1016/j.jemermed.2009.08.031. [DOI] [PubMed] [Google Scholar]
- 23.Davies K G, Weeks R D. Acute spontaneous spinal epidural haematoma with temporary resolution. Br J Neurosurg. 1992;6(1):63–66. doi: 10.3109/02688699209002903. [DOI] [PubMed] [Google Scholar]
- 24.Duffill J, Sparrow O C, Millar J, Barker C SK. Can spontaneous spinal epidural haematoma be managed safely without operation? A report of four cases. J Neurol Neurosurg Psychiatry. 2000;69(6):816–819. doi: 10.1136/jnnp.69.6.816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Blencowe H, Cousens S, Oestergaard M Z. et al. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet. 2012;379(9832):2162–2172. doi: 10.1016/S0140-6736(12)60820-4. [DOI] [PubMed] [Google Scholar]
- 26.Hibbard J U, Wilkins I, Sun L. et al. Respiratory morbidity in late preterm births. JAMA. 2010;304(4):419–425. doi: 10.1001/jama.2010.1015. [DOI] [PMC free article] [PubMed] [Google Scholar]


