Abstract
Background
Limited contemporary data compare the clinical and psychosocial characteristics and acute management of patients hospitalized with an initial versus a recurrent episode of acute coronary disease. We describe these factors in a cohort of patients recruited from six hospitals in Massachusetts and Georgia after an acute coronary syndrome.
Materials and Methods
We performed structured baseline in-person interviews and medical record abstractions for 2,174 eligible and consenting patients surviving hospitalization for an acute coronary syndrome between April, 2011 and May, 2013.
Results
The average patient age was 61 years, 64% were men, and 47% had a high school education or less; 29% had a low general quality of life and 1 in 5 were cognitively impaired. Patients with a recurrent coronary episode had a greater burden of previously diagnosed comorbidities. Overall, psychosocial burden was high, and more so in those with a recurrent versus those with an initial episode. Patients with an initial coronary episode were as likely to have been treated with all 4 effective cardiac medications (51.6%) as patients with a recurrent episode (52.3%), but were significantly more likely to have undergone cardiac catheterization (97.9% vs 92.9%) and a percutaneous coronary intervention (73.7% vs 60.9%) (p <0.001) during their index hospitalization.
Conclusions
Patients with a first episode of acute coronary artery disease have a more favorable psychosocial profile, less comorbidity, and receive more invasive procedures, but similar medical management than patients with previously diagnosed coronary disease. Implications of the high psychosocial burden on various patient-related outcomes requires investigation.
Keywords: prospective observational study, acute coronary syndrome, hospital treatment practices, psychosocial characteristics
Introduction
Despite encouraging declines in the short-term death rates of patients hospitalized with an acute coronary syndrome over the past several decades1–4, this clinical syndrome affects several million American men and women annually5,6. Moreover, despite extensive knowledge about the underlying pathophysiology, treatment, and natural history of patients who present with an acute coronary syndrome, relatively little contemporary data are available about possible differences in the descriptive characteristics and management of patients hospitalized with an initial, as compared to those hospitalized with a prior, episode of acute coronary heart disease7–11. Even less information is available about the psychosocial profile of these patients at the time of hospitalization for an acute coronary syndrome. Knowledge about these latter factors is particularly important since they can affect health care providers’ management practices and patient’s long-term outcomes.
We describe the baseline socio-demographic, lifestyle, psychosocial, and clinical characteristics, as well as hospital treatment practices, of patients who survived hospitalization for an initial, as compared to those hospitalized with a prior, acute coronary syndrome episode at 6 hospitals in Massachusetts and Georgia. This descriptive study uses data from the Transitions, Risks, and Actions in Coronary Events Center for Outcomes Research and Education (TRACE-CORE) study12, one of three Centers for Cardiovascular Outcomes Research funded by the National Heart, Lung and Blood Institute13.
Methods and Design
Details of the study design, patient recruitment practices, and data collection activities utilized in this longitudinal cohort study have been described previously12.
In brief, TRACE-CORE used a multi-site prospective cohort design to recruit and follow a cohort of adult men and women hospitalized with an acute coronary syndrome at three tertiary care and community medical centers in Worcester, MA, that capture the vast majority of all hospitalizations for acute coronary syndrome in Central Massachusetts, two hospitals in Atlanta, GA, that contract to admit and treat members of a major health maintenance organization network, and one hospital in Macon, GA, a large teaching hospital that serves all of Central Georgia. Participating study sites served a heterogeneous patient population and were purposely selected for their socio-demographic and socio-economic diversity. All eligible and consenting patients 21 years and older discharged alive from participating hospitals after an acute coronary syndrome were enrolled between April, 2011 and May, 2013.
Trained study staff abstracted an extensive amount of socio-demographic, clinical, laboratory, physiologic, and treatment related data from the medical records of patients hospitalized with an independently validated acute coronary syndrome. Standard definitions of acute coronary syndrome, including ST-segment elevation myocardial infarction, non-ST segment elevation myocardial infarction, and unstable angina were used7,12,14,15; questionable cases of acute coronary syndrome were adjudicated by a team of physicians. Patients were classified as having an initial acute coronary syndrome episode if, based on the careful review of hospital medical records by trained study abstractors, there was no mention of a prior hospitalization for coronary heart disease or receipt of a coronary interventional procedure in the past (e.g., percutaneous coronary intervention and/or coronary artery bypass graft surgery). Patients were classified as having a prior diagnosis of coronary heart disease if there had been either a prior hospitalization for coronary heart disease (e.g., angina or myocardial infarction) or receipt of either a percutaneous coronary intervention and/or coronary artery bypass graft surgery at any time in the past.
Information was collected by trained study staff about patient’s general quality of life, behavioral and lifestyle characteristics, including alcohol consumption and cigarette smoking, and a variety of social factors, such as marital and employment status, using standardized instruments during an extensive in-person baseline interview at the time of the patient’s index hospitalization for an acute coronary syndrome at participating medical centers12. We also collected information directly from patients during their standardized interview about a variety of psychosocial factors which would not be routinely available or collected and recorded in a standardized manner from the review of hospital charts. These factors included cognitive status, depression, anxiety, measures of perceived stress and social support, trust in physicians, and health literacy and numeracy12,16–18.
Information was also collected from the review of hospital charts about the inhospital use of several evidence-based cardiac medications, cardiac catheterization, percutaneous coronary intervention, and coronary artery bypass graft surgery. Quality control procedures were carried out through double abstraction of a continuing random sample of 5% of study patients at each study site.
IRB approval was obtained from the UMMS Committee for the Protection of Human Subjects in Research and participants provided written informed consent.
Data Analysis
Differences in the baseline socio-demographic, clinical, and treatment characteristics of participating study subjects according to history of acute coronary disease (e.g., initial vs. prior evidence of coronary heart disease) were examined through the use of chi-square and t-tests for discrete and continuous variables, respectively. Analyses were conducted using SAS (Version 9.3).
Results
The average age (±SD) of our 2,174 study participants was 61.3 (±11.3) years, approximately two thirds were men, and 81.2% were non-Hispanic white; for 1,034 patients this was their first documented episode of acute coronary disease. In the overall study population, 28.9% had a low general quality of life (more than 1.5 standard deviation less than the population-based norm for the physical component score of the SF-36 instrument), 20.3% were classified as cognitively impaired, and 23.8% were current smokers.
Baseline Socio-Demographic and Clinical Characteristics
In examining differences in the baseline demographic and clinical characteristics of our 2 primary comparison groups, namely those with an initial episode of acute coronary heart disease (n=1,034) compared to those with previously diagnosed coronary heart disease (1,140), patients with previously documented coronary heart disease were approximately four years older, on average, more likely to be male, and from a minority racial/ethnic group, but were significantly less likely to be married, have graduated from college, and be currently working at the time of their index hospitalization than patients with a first episode of coronary heart disease (Table 1). Patients with pre-existing coronary disease were heavier, on average, and significantly more likely to have been previously diagnosed with each of the comorbid conditions examined than patients with a first episode of acute coronary disease (Table 1).
Table 1.
Socio-Demographic and Clinical Characteristics of Study Patients According to Order of Acute Coronary Syndrome: TRACE-CORE
| Characteristic | First Episode* (n=1,034) | Recurrent Episode (n=1,140) | P value |
|---|---|---|---|
| Socio-Demographic | |||
| Age (mean, yrs) | 59.3 | 63.2 | <0.001 |
| Male (%) | 64.1 | 68.7 | <0.05 |
| Non-Hispanic white (%) | 83.3 | 79.0 | <.01 |
| Married (%) | 60.8 | 56.1 | <.05 |
| Education (%) | |||
| High school or less | 41.7 | 50.8 | |
| Some college | 27.7 | 29.9 | <.001 |
| College graduate | 30.6 | 19.3 | |
| Currently working (%) | 54.3 | 29.0 | <0.001 |
| Body mass index (mean) | 29.9 | 30.5 | 0.06 |
| Hospital length of stay (mean, days) | 4.8 | 5.1 | 0.83 |
| Comorbidities at admission (%) | |||
| Atrial fibrillation | 3.8 | 12.0 | <0.001 |
| Chronic kidney disease | 4.6 | 16.6 | <.001 |
| Chronic lung disease | 11.9 | 23.3 | <.001 |
| Depression | 10.4 | 14.7 | <0.005 |
| Diabetes | 22.1 | 39.9 | <0.001 |
| Heart failure | 4.3 | 22.9 | <0.001 |
| Hyperlipidemia | 53.2 | 82.8 | <0.001 |
| Hypertension | 62.7 | 88.1 | <0.001 |
| Stroke | 2.6 | 7.8 | <0.001 |
| Physiologic variables (mean, at admission) | |||
| Blood pressure (diastolic, mmHg) | 82.7 | 78.6 | <.001 |
| Blood pressure (systolic, mmHg) | 142.7 | 140.7 | 0.08 |
| Estimated GFR (ml/min/1.73m2) | 83.1 | 75.7 | <.001 |
| Heart rate (bpm) | 78.8 | 76.9 | <.05 |
| Serum cholesterol (mg/dl) | 182.4 | 162.1 | <.001 |
| Serum glucose (mg/dl) | 146.1 | 155.4 | <.005 |
| Troponin (mg/mL) | 21.9 | 12.5 | <0.001 |
GFR – glomerular filtration rate
History of angina, myocardial infarction, percutaneous coronary intervention, or coronary artery bypass graft surgery
Patients with an initial as compared to those with previously diagnosed coronary heart disease had higher blood pressure readings, better kidney function, and higher heart rate, serum cholesterol, and peak troponin findings than patients with previously diagnosed coronary heart disease; these patients also had significantly lower serum glucose levels (Table 1). The average ejection fraction findings were similar in the patients with (n=336) and without a history of previously diagnosed coronary heart disease (n=341) who had these values recorded and who underwent ejection fraction testing (mean ejection fraction’s = 48.6% and 52.1%, respectively).
Baseline Psychosocial and Lifestyle Characteristics
Important differences in several psychosocial and behavioral characteristics were present in relation to incident versus recurrent coronary disease (Table 2). Patients with previously diagnosed coronary heart disease were more likely to report moderate/severe anxiety and depression, higher rates of perceived stress, to have impaired cognition, to have low health literacy and numeracy, and to have a lower quality of life on the physical and mental health measures on the SF-36 health survey (Table 2). On the other hand, these individuals were less likely to report consuming moderate or heavy amounts of alcohol and be a current smoker at the time of hospital admission than patients with an initial episode of coronary heart disease (Table 2).
Table 2.
Psychosocial and Behavioral Characteristics of Study Patients According to Type of Acute Coronary Syndrome: TRACE-CORE
| Characteristic | First Episode* (n=1,034) | Recurrent Episode (n=1,140) | P Value |
|---|---|---|---|
| Psychosocial | |||
| Anxiety∞ | |||
| Mild | 24.2 | 25.9 | <0.001 |
| Moderate/Severe | 20.6 | 27.1 | |
| Depression∞∞ | |||
| Mild | 23.3 | 29.7 | <0.001 |
| Moderate/Severe | 18.4 | 26.0 | |
| Impaired cognition∞∞∞ | 15.2 | 24.4 | <0.001 |
| High perceived stress† | 34.5 | 45.3 | <0.001 |
| Lives alone | 19.9 | 23.8 | <0.10 |
| Low health literacy†† | 30.6 | 41.1 | <.001 |
| Low health numeracy††† | 45.2 | 51.4 | <0.05 |
| Social support (mean) | 20.2 | 20.0 | 0.16 |
| SF-36 Components∘ | |||
| MCS (mean) | 49.2 | 45.8 | <0.001 |
| PCS (mean) | 44.4 | 38.2 | <0.001 |
| Trust in physicians∘∘ | 64.4 | 65.8 | 0.23 |
| Behavioral | |||
| Alcohol consumption | |||
| Moderate | 13.3 | 10.4 | <0.001 |
| Heavy | 11.0 | 8.4 | |
| Current smoking | 24.9 | 21.9 | <0.005 |
GAD7 General Anxiety Disorder 7 item score: 5–9 mild, 10–14 moderate, >15 Severe anxiety
PHQ-9 Patient Health Questionnaire 9 item score: 5–9 mild, 10–14 moderate, 15–19 moderately severe, and ≥20 severe depression
TICS – telephone interview for cognitive status: ≤28 impaired cognition
Perceived stress scale: ≥20 high perceived stress
Somewhat/not at all confident/little confidence in filling out medical forms
Unable to answer both health numeracy questions correctly
SF-36 – mental health and physical health components
Trust in Physicians questions (all in all, you trust doctors completely: agree/strongly agree)
MCS – mental component summary measure
PCS – Physical component summary measure
Hospital Treatment Practices
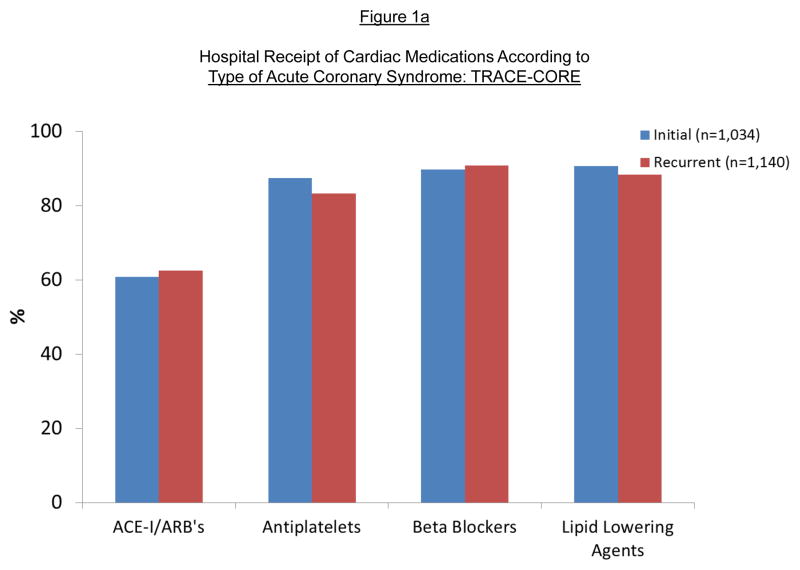
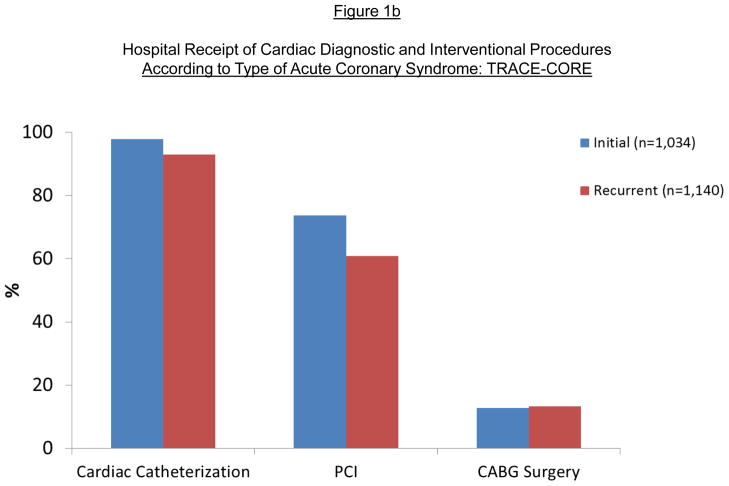
There were relatively minimal differences with regards to the receipt of effective cardiac medications during the patient’s index hospitalization for an acute coronary syndrome (Figure 1a). Patients with a history of prior coronary heart disease were no more likely to have been prescribed all 4 evidence-based cardiac medications (angiotensin converting enzyme inhibitors/angiotensin receptor blockers, aspirin, beta blockers, statins) during their acute hospital stay (51.6% vs. 52.3%) (p=0.76). Patients with an initial episode of coronary heart disease were significantly more likely to have been treated with anticoagulants during their acute hospital stay than patients with recurrent coronary disease (77.7% vs 66.3%) (p<.05). On the other hand, patients with a first episode of acute coronary disease were significantly more likely to have undergone cardiac catheterization and a percutaneous coronary intervention than patients with previously diagnosed coronary heart disease (Figure 1b K01AG033643).
Figure 1.
Figure 1a. Hospital Receipt of Cardiac Medications According to Initial Versus Recurrent Episode of Coronary Heart Disease: TRACE-CORE
Figure 1b. Hospital Receipt of Cardiac Diagnostic and Interventional Procedures According to Initial Versus Recurrent Episode of Coronary Heart Disease: TRACE-CORE
Essentially similar differences in patient’s baseline sociodemographic, clinical, and psychosocial characteristics and hospital treatment practices were observed between patients with an initial versus recurrent episode of coronary heart disease when we classified patients as having had either an episode of angina or acute myocardial infarction previously diagnosed or had received a prior coronary interventional procedure in separate subgroup analyses (data not shown).
Discussion
The results of the present study provide insights into the descriptive socio-demographic, clinical, and psychosocial characteristics of a contemporary, multi-racial, cohort of patients discharged from the hospital after an acute coronary syndrome and their hospital management practices. Although slightly less than one half of patients hospitalized with an acute coronary syndrome presented with a first episode of acute coronary disease, these patients were significantly younger compared with patients diagnosed with a previous episode of coronary heart disease and, for most factors, had a more favorable socio-demographic, comorbidity, and psychosocial profile.
Baseline Patient Characteristics
Patients in TRACE-CORE were relatively young, on average 61 years old, primarily male, married, had attended college, and a considerable proportion had been previously diagnosed with hyperlipidemia, diabetes, and chronic lung disease. In the population-based study of residents of Olmsted County, MN, patients with an incident (initial) episode of acute coronary syndrome were approximately 7 years older than our study population and had a relatively similar comorbidity profile1,19. In the community-based Worcester Heart Attack Study, the average age of central Massachusetts residents hospitalized at all 11 medical centers in this geographic region with independently confirmed acute myocardial infarction in 2003, 2005, and 2007 was 71 years, and the vast majority (87%) of these patients had at least one cardiac comorbid condition, and slightly more than half had at least one noncardiac comorbid condition, previously diagnosed20. In a prior analysis of data from the Worcester Heart Attack Study, older individuals, women, nonwhites, and widowed patients were more likely to have multiple cardiovascular comorbidities previously diagnosed than respective comparison groups21. In comparing the results of TRACE-CORE with these and other community-based investigations, the younger average may be explained by the fact that we only included patients who had survived their hospitalization for an acute coronary syndrome and who did not have psychiatric or other conditions which might have precluded their study enrollment and participation.
Baseline Psychosocial and Behavioral Characteristics
Patients with an initial acute coronary syndrome event were more likely to have smoked and consumed moderate/heavy amounts of alcohol compared to patients with previously diagnosed coronary heart disease. On the other hand, patients with a history of previously diagnosed coronary heart disease reported a lower quality of life and higher frequencies of impaired cognition, low health numeracy and literacy, perceived stress, and moderate/severe depression and anxiety as reflected by relevant measures. Some of these differences may have been attributable to patients with prior coronary heart disease being older and having more previously diagnosed comorbidities than patients with an initial episode of acute coronary heart disease.
Few studies have recently examined either the magnitude of, or factors associated with, various psychosocial factors in patients hospitalized with an acute coronary syndrome, with much of the published literature in this area being more than a decade old22–27. A review of studies carried out in patients with an acute coronary syndrome showed that the proportion of patients who either expressed symptoms of depression or who had a depressive disorder at the time of baseline enrollment ranged widely28. Anxiety is also a highly prevalent disorder in patients with an acute coronary syndrome affecting between 20 to 50% of these individuals28,29.
Patients with an acute coronary syndrome and symptoms of depression not only experience greater morbidity and mortality, but also report poorer quality of life than patients without symptoms of these underlying psychiatric disturbances. In a recent study of nearly 500 Dutch patients enrolled in the Depression After Myocardial Infarction Study, approximately one quarter of study patients showed signs of depression28.
In the present study of relatively young patients discharged from 6 hospitals in Massachusetts and Georgia after an acute coronary syndrome, we also showed relatively high rates of psychosocial problems and conditions including impaired cognition, low health literacy and numeracy, and perceived stress, characteristics that may be linked with worse long-term outcomes. This adverse psychosocial and cognitive profile was more pronounced in patients with previously diagnosed coronary heart disease. In addition to these factors, approximately one quarter of study patients admitted to being current cigarette smokers and more than 10% were classified as heavy drinkers.
These psychosocial, cognitive, lifestyle, and other related factors need to be considered in the short and long-term management of patients discharged from the hospital after an acute coronary syndrome, especially in persons with previously diagnosed coronary heart disease. These factors, and their possible treatment and modification, should be discussed with patients to enhance their adherence to prescribed treatment regimens, recommended lifestyle practices, and their long-term prognosis, including quality of life. Often times information on these important psychosocial factors is not collected or acted upon due to time constraints or other underlying medical issues. Discussions between patients and their providers should incorporate these factors since they may impact prescribed medication, patient self-management activities including lifestyle changes, and patient’s long-term prognosis and risk of hospital readmissions.
Hospital Treatment Practices
We observed a relatively high utilization of effective cardiac medications during their index hospitalization in this patient population, irrespective of a history of prior coronary disease, with the exception being ACE inhibitors and angiotensin receptor blockers. We were, however, unable to systematically classify patients in whom these medications may have been contraindicated, and, therefore, may have underestimated the use of currently recommended treatments in this patient population. In addition, the vast majority of patients underwent cardiac catheterization in the present study with some statistically significant, but modest, between group differences noted with regards to the receipt of cardiac catheterization and a percutaneous coronary intervention in patients with an initial versus recurrent episode of coronary heart disease. These findings need to be cautiously, interpreted, however, given the effects of assessing one acute illness episode in an often complex disease management history.
The present results suggest that approaches to optimize the medical management of patients hospitalized with an acute coronary syndrome continue to be needed, which would hopefully pay dividends to improvements in patient’s long-term survival and quality of life.
Study Strengths and Limitations
The strengths of the present study include the contemporary and diverse cohort of patients hospitalized with an acute coronary syndrome, use of standardized data collection instruments to ascertain various measures of psychosocial and lifestyle characteristics, and rigorous quality control measures. We collected information from patients about an abundance of psychosocial characteristics that are not usually available in studies of patients discharged from the hospital after an acute coronary syndrome, especially those that are primarily based on the review of information noted in hospital medical records. Nonetheless, our findings need to be interpreted with appropriate reservation due to a lack of broader geographic representation, though our sites were purposely selected to provide diversity in race/ethnicity and socioeconomic status.
Conclusions
The results of this cohort study provide insights into the baseline descriptive socio-demographic, lifestyle, psychosocial, and clinical characteristics of contemporary patients discharged from the hospital with different manifestations of acute coronary disease. Psychosocial vulnerability and burden of comorbidity appear to be high. It will be important to describe changes in factors, such as health-related quality of life and various clinical parameters, over the course of our longitudinal follow-up and examine the relation between baseline levels of these characteristics, and changes over time therein, to various patient-centered measures and clinical outcomes. Our findings also highlight the importance of considering these factors, especially certain psychosocial conditions, in the acute and long-term management of patients who present with an acute coronary syndrome.
Acknowledgments
We are indebted to the trained study staff at each of our participating study sites in Worcester, MA, Macon, GA, and Atlanta, GA. TRACE-CORE was supported by NIH grant U01HL105268. Support for Dr. Waring was provided by KL2TR000160, for Dr. Saczynski by K01AG033643 from the National Institute of Aging, and by KL2RR031981 for Dr. McManus.
Footnotes
There are no conflicts of interests with any of the authors.
All authors had access to the data and had a role in writing this manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Roger VL, Weston SA, Gerber Y, Killian JM, Dunlay SM, Jaffe AS, Bell MR, Kors J, Yawn BP, Jacobsen SJ. Trends in incidence, severity, and outcome of hospitalized myocardial infarction. Circulation. 2010;121:863–869. doi: 10.1161/CIRCULATIONAHA.109.897249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;362:2155–2165. doi: 10.1056/NEJMoa0908610. [DOI] [PubMed] [Google Scholar]
- 3.Rosamond WD, Chambless LE, Heiss G, Mosley TH, Coresh J, Whitsel E, Wagenknecht L, Ni H, Folsom AR. Twenty-two-year trends in incidence of myocardial infarction, coronary heart disease mortality, and case fatality in 4 US communities, 1987–2008. Circulation. 2012;125:1848–1857. doi: 10.1161/CIRCULATIONAHA.111.047480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Floyd KC, Yarzebski J, Spencer FA, Lessard D, Dalen JE, Alpert JS, Gore JM, Goldberg RJ. A 30-year perspective (1975–2005) into the changing landscape of patients hospitalized with initial acute myocardial infarction: Worcester Heart Attack Study. Circ Cardiovasc Qual Outcomes. 2009;2:88–95. doi: 10.1161/CIRCOUTCOMES.108.811828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Magid D, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, Moy CS, Mussolino ME, Nichol G, Paynter NP, Schreiner PJ, Sorlie PD, Stein J, Turan TN, Virani SS, Wong ND, Woo D, Turner MB. Heart disease and stroke statistics-2013 update: a report from the American Heart Association. Circulation. 2013;127:e6–e245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Heart, Lung and Blood Institute. Morbidity and Mortality Chartbook. 2012 [Google Scholar]
- 7.McManus DD, Gore J, Yarzebski J, Spencer F, Lessard D, Goldberg RJ. Recent Trends in the Incidence, Treatment, and Outcomes of Patients with ST and Non-ST-Segment Acute Myocardial Infarction. Am J Med. 2011;124:40–47. doi: 10.1016/j.amjmed.2010.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Montalescot G, Dallongeville J, Van Belle E, Rouanet S, Baulac C, Degrandsart A, Vicaut E OPERA Investigators. STEMI and NSTEMI: are they so different? 1 year outcomes in acute myocardial infarction as defined by the ESC/ACC definition (the OPERA registry) Eur Heart J. 2007;28:1409–1417. doi: 10.1093/eurheartj/ehm031. [DOI] [PubMed] [Google Scholar]
- 9.Chan MY, Sun JL, Newby LK, Shaw LK, Lin M, Peterson ED, Califf RM, Kong DF, Roe MT. Long-term mortality of patients under-going cardiac catheterization for ST-elevation and non-ST-elevation myocardial infarction. Circulation. 2009;119:3110–3117. doi: 10.1161/CIRCULATIONAHA.108.799981. [DOI] [PubMed] [Google Scholar]
- 10.Terkelsen CJ, Lassen JF, Nørgaard BL, Gerdes JC, Jensen T, Gøtzsche LB, Nielsen TT, Andersen HR. Mortality rates in patients with ST-elevation vs non-ST-elevation acute myocardial infarction: observations from an unselected cohort. Eur Heart J. 2005;26:18–26. doi: 10.1093/eurheartj/ehi002. [DOI] [PubMed] [Google Scholar]
- 11.Alpert JS, Thygesen K, Antman E, Bassand JP. Myocardial infarction redefined – a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol. 2000;36:959–969. doi: 10.1016/s0735-1097(00)00804-4. [DOI] [PubMed] [Google Scholar]
- 12.Waring ME, McManus RH, Saczynski JS, Anatchkova MD, McManus DD, Devereaux RS, Goldberg RJ, Allison JJ, Kiefe CI for the TRACE-CORE Investigators. Transitions, risks, and actions in coronary events – Center for outcomes research and education (TRACE-CORE): Design and rationale. Circ Cardiovasc Qual Outcomes. 2012;5:e44–e50. doi: 10.1161/CIRCOUTCOMES.112.965418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cook NL, Bonds DE, Kiefe CI, Curtis JP, Krumholz HM, Kressin NR, Peterson ED National Heart, Lung, and Blood Institute Centers for Cardiovascular Research (CCOR) Writing Group. Circ Cardiovasc Qual Outcomes. 2013;6:223–228. [Google Scholar]
- 14.O’Gara PT, Kushner FG, Ascheim DD, Casey DE, Jr, Chung MK, de Lemos JA, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;127:529–555. doi: 10.1161/CIR.0b013e3182742c84. [DOI] [PubMed] [Google Scholar]
- 15.Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE, Jr, Chavey WE, 2nd, et al. 2012 ACCF/AHA focused update incorporated into the ACCF/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;127:e863–864. doi: 10.1161/CIR.0b013e31828478ac. [DOI] [PubMed] [Google Scholar]
- 16.Dugan E, Trachtenberg F, Hall MA. Development of abbreviated measures to assess patient trust in a physician, a health insurer, and the medical profession. BMC Health Services Research. 2005;5:64. doi: 10.1186/1472-6963-5-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lipkus IM, Samsa G, Rimer BK. General performance on a numeracy scale among highly educated samples. Med Decis Making. 2001;21:37–44. doi: 10.1177/0272989X0102100105. [DOI] [PubMed] [Google Scholar]
- 18.Chew LD, Griffin JM, Partin MR, Noorbaloochi S, Grill JP, Snyder A, Bradley KA, Nugent SM, Baines AD, Vanryn M. Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med. 2008;23:561–566. doi: 10.1007/s11606-008-0520-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Roger VL, Jacobsen SJ, Weston SA, Goraya TY, Killian J, Reeder GS, Kottke TE, Yawn BP, Frye RL. Trends in the incidence and survival of patients with hospitalized myocardial infarction, Olmsted County, Minnesota, 1979 to 1994. Ann Intern Med. 2002;136:341–348. doi: 10.7326/0003-4819-136-5-200203050-00005. [DOI] [PubMed] [Google Scholar]
- 20.Chen H-Y, Saczynski JS, McManus DD, Lessard D, Yarzebski J, Lapane KL, Gore JM, Goldberg RJ. The impact of cardiac and noncardiac comorbidities on the short-term outcomes of patients hospitalized with acute myocardial infarction: a population-based perspective. Clin Epidemiol. 2013;5:439–448. doi: 10.2147/CLEP.S49485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McManus DD, Nguyen HL, Saczynski JS, Tisminetzky M, Bourell P, Goldberg RJ. Multiple cardiovascular comorbidities and acute myocardial infarction: temporal trends (1990–2007) and impact on death rates at 30 days and 1 year. Clin Epidemiol. 2012;4:115–123. doi: 10.2147/CLEP.S30883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ahern D, Godkin L, Anderson JL, Tierney C, Ahlstrom A, Wart C, Capone RJ, Schroon E, Kornfeld D, Herd JA, Richardson DW, Rollick MJ. Bio behavioral variables and mortality or cardiac arrest in the Cardiac Arrhythmia Pilot Study (CAPS) Am J Cardiol. 1990;66:59–62. doi: 10.1016/0002-9149(90)90736-k. [DOI] [PubMed] [Google Scholar]
- 23.Ludwig KH, Kiser M, Koenig J, Breithardt G. Affective disorders and survival after acute myocardial infarction. Results from the post-infarction late potential study. Eur Heart J. 1991;12:959–964. [PubMed] [Google Scholar]
- 24.Case RB, Moss AJ, Case N, McDermott M, Eberly S. Living alone after myocardial infarction: Impact on prognosis. JAMA. 1992;267:515–519. [PubMed] [Google Scholar]
- 25.Frasure-Smith N, Lespérance F, Talajic M. Depression following myocardial infarction. Impact on 6 month survival. JAMA. 1993;270:1819–1825. [PubMed] [Google Scholar]
- 26.Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation. 1999;99:2192–2217. doi: 10.1161/01.cir.99.16.2192. [DOI] [PubMed] [Google Scholar]
- 27.Thombs BD, Bass EB, Ford DE, Stewart KJ, Tsilidis KK, Patel U, Fauerbach JA, Bush DE, Ziegelstein RC. Prevalence of depression in survivors of acute myocardial infarction. Review of the evidence. J Gen Intern Med. 2006;21:30–38. doi: 10.1111/j.1525-1497.2005.00269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Meurs M, Zuidersma M, Dickens C, de Jonge P. Examining the relation between post myocardial infarction depression and cardiovascular prognosis using a validated prediction model for post myocardial mortality. Int J Cardiol. 2013;167:2533–2538. doi: 10.1016/j.ijcard.2012.06.042. [DOI] [PubMed] [Google Scholar]
- 29.Tisminetzky M, Bray BC, Miozzo R, Aupont O, McLaughlin T. Classes of depression, anxiety, and functioning in acute coronary syndrome patients. Am J Health Behav. 2012;36:20–30. doi: 10.5993/ajhb.36.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]