Abstract
Background
Low health literacy affects millions of Americans, putting those who are affected at a disadvantage and at risk for poorer health outcomes. Low health literacy can act as a barrier to effective disease self-management; this is especially true for chronic diseases such as heart failure (HF) that require complicated self-care regimens.
Purpose
This systematic review examined quantitative research literature published between 1999 and 2014 to explore the role of health literacy among HF patients. The specific aims of the systematic review are to (1) describe the prevalence of low health literacy among HF patients, (2) explore the predictors of low health literacy among HF patients, and (3) discuss the relationship between health literacy and HF self-care and common HF outcomes.
Methods
A systematic search of the following databases was conducted, PubMed, CINAHL Plus, Embase, PsycINFO, and Scopus, using relevant keywords and clear inclusion and exclusion criteria.
Conclusions
An average of 39% of HF patients have low health literacy. Age, race/ethnicity, years of education, and cognitive function are predictors of health literacy. In addition, adequate health literacy is consistently correlated with higher HF knowledge and higher salt knowledge.
Clinical Implications
Considering the prevalence of low health literacy among in the HF population, nurses and healthcare professionals need to recognize the consequences of low health literacy and adopt strategies that could minimize its detrimental effect on the patient's health outcomes.
Keywords: health literacy, health outcomes, heart failure, knowledge
Background
Approximately 5.1 million adult Americans have heart failure (HF).1 Each year, 825 000 new cases of HF are diagnosed, most of whom are people 65 years or older.1 The incidence of HF increases with age. Each year, an average of 5% of people 85 years or older develop HF compared with 1.4% of people between 65 and 74 years.1 With the oldest old (≥85 years) projected to reach 8.7 million by 2030,2 the incidence of HF and the subsequent cost of treating it will only exponentially increase. In 2012, the estimated cost of treating HF was $20.9 billion, 80% of which was attributed to hospitalizations; by 2030, the cost of treating HF is projected to reach $69.8 billion.3 To minimize hospitalizations and curb rising healthcare costs, effective implementation of HF self-care is vital. However, HF self-care clinical guidelines can be complicated, involving symptom monitoring, dietary and fluid restrictions, structured exercise regimens, and management of multiple medications.4 The complexity of HF self-care can pose a myriad of threats to patients’ adherence to self-care behaviors, particularly among those with low health literacy.
Health literacy is defined as “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.”5 On the basis of the 2003 National Assessment of Adult Literacy, 36% of adult Americans and 59% of adults 65 years or older have below basic or basic health literacy.6 People with low health literacy may have trouble processing information on disease management, such as reading appointment slips and medication labels, comprehending verbal information from their healthcare providers, and understanding educational materials.7,8 Studies have also shown that low health literacy is associated with poorer health-care knowledge,9—12 decreased medication adherence,11,13,14 diminished use of preventative services,15 poorer physical and mental health,16,17 and increased hospitalizations.18
Because health literacy can potentially affect the performance of HF self-care behaviors and other HF outcomes, a systematic review on the role of health literacy in the HF population is warranted. The purpose of this systematic review is to examine quantitative research literature exploring the role of health literacy in the HF population. Specifically, the review aims to (1) describe the prevalence of low health literacy among HF patients, (2) explore the predictors of low health literacy among HF patients, and (3) discuss the relationship between health literacy and HF self-care and common HF outcomes.
Methods
A systematic search for relevant quantitative studies in the following databases was conducted: PubMed, CINAHL Plus, Embase, PsycINFO, and Scopus. Keywords used in the search were health literacy, heart failure, congestive heart failure, and CHF. A medical librarian assisted in the database search. Studies were included if they met the following criteria: (1) assessed health literacy using a previously validated instrument, (2) included adult HF patients, and (3) published in English between 1999 and August 2014. This timeframe was chosen to coincide with the inception of the concept of health literacy, which was first defined by the American Medical Association in 1999.19,20 Studies were excluded if they were nonresearch articles (eg, commentaries, editorial, psychometric reports), measured health literacy but not in HF patients (eg, caregivers, healthcare professionals, informational materials), and had only abstracts available.
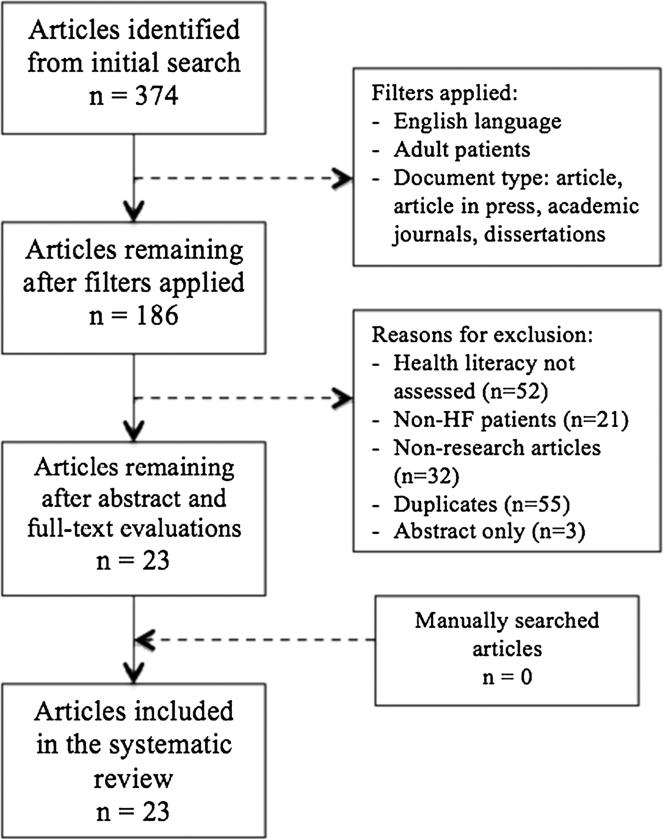
The initial database search yielded 374 citations. A total of 186 citations remained after filters were applied. Abstracts were then reviewed, and if inclusion could still not be determined after reviewing the abstracts, full-text evaluations were performed (n = 5). A total of 163 articles were excluded after the abstract and full-text evaluations. The references of the included articles were then manually searched for relevant studies (n = 0). Twenty-three articles were included in this systematic review, 22 published journal articles and 1 unpublished doctoral dissertation (Figure). Some of the articles used data from larger studies, which meant that their patient samples were not independent of each other. Therefore, in synthesizing the results, their health literacy assessments were grouped together. Of the 10 studies that used shared data, 4 used subsets of data from a larger randomized controlled trial testing a literacy-sensitive HF self-care training intervention (2 randomized controlled trials, 2 observational studies),21–24 2 used the Vanderbilt Inpatient Cohort Study (both used a prospective cohort design),25,26; and the remaining 4 used subsets of data from a larger randomized controlled trial testing a pharmacist-delivered patient education intervention (1 randomized controlled trial, 2 observational studies, 1 secondary analysis).27–30
FIGURE.
Diagram of search and retrieval process. HF indicates heart failure.
The Johns Hopkins Research Evidence Appraisal Tool, a generic evidence appraisal tool that can be used for any type of study design, was used to assess the quality of the included studies.* For this systematic review, studies with sample sizes that were sufficient for their study design and that used instruments with established validity and reliability were given high-quality ratings. Two reviewers assessed the quality of all the included studies independently, with an 87% agreement rate; disagreements were discussed and then reconciled. The first author performed data extraction using a data table and the second author reviewed the data table for accuracy.
Results
Table 1 summarizes the key characteristics of the included studies. The number of participants ranged from 26 to 1492. The average age of the study participants was 63.86 years, and an average of 59% was male. Of the 23 studies, 15 had a predominantly white sample (ranged from 39% to 98%), 6 had a predominantly African American sample (ranged from 39% to 68%), 1 had a predominantly Hispanic sample (64%), and the only study that was conducted outside the United States presumably had a 100% Asian sample. Of the 23 studies, 4 were experimental21,22,28,31 (2 studies explored the effect of the same intervention; however, they explored different HF outcomes21,22). On top of assessing health literacy, 5 of the 19 observational studies explored potential predictors of health literacy,27,32–35 5 explored the relationship between health literacy and HF outcomes (eg, hospitalization, mortality, quality of life),26,29,30,36,37 8 explored both the predictors of health literacy and the impact of health literacy on HF outcomes,23,24,38–42 and the remaining study merely assessed the health literacy of its sample.25
TABLE 1.
Patient Characteristics
| Study | Design | Sample Size | Age, Mean (SD), y | Sex, % Male | Race, % White | Quality Rating |
|---|---|---|---|---|---|---|
| Baker et al. (2011) | RCT | 531 | 60.7 (13.1) | 52 | 39 | High |
| Dewalt et al. (2012) | RCT | 605 | 60.7 (13.1) | 52 | 39 | High |
| Macabasco et al. (2011) | Observational, cross-sectional | 585 | 60.7 (13.1) | 52 | 39 | High |
| Wu et al. (2013) | Prospective cohort | 595 | 61 (13) | 52 | 39a | High |
| Meyers et al. (2014) | Prospective cohort | 1249 | 60 | 55 | 82.4 | High |
| Mixon et al. (2014) | Prospective cohort | 471 | 59.4 (12.5) | 52.1 | 80.7 | High |
| Morrow et al. (2006) | Observational, cross-sectional | 314 | 62.9 (8.5) | 33 | 49 | High |
| Morrow et al. (2007) | RCT | 236 | 64.5 | 32 | 47a | Good |
| Murray et al. (2009) | Observational, cross-sectional | 192 | 62.6 (8.8) | 33.9 | 52.1a | Good |
| Noureldin et al. (2012) | Secondary analysis | 281 | 63 (9) | 33 | 48a | Good |
| Chaudhry et al. (2011) | Secondary analysis | 1464 | 61 (15) | 58 | 56 | High |
| Chen et al. (2011) | Observational, cross-sectional | 49 | 72 (13.3) | 67.3 | 91.8 | Low |
| Chen et al. (2014) | Observational, cross-sectional | 63 | 62.1 (13.7) | 52.4 | 85.7 | Good |
| Cordasco et al. (2009) | Observational, cross-sectional | 399 | 55 | 64 | 64b | Good |
| Daley (2010) | Quasi-experimental | 89 | 73 | 63 | 98 | Low |
| Dennison et al. (2011) | Observational, cross-sectional | 95 | 59 (14) | 51 | 68a | Good |
| Hawkins (2012) | Secondary analysis | 26 | 65.3 (8.2) | 96 | 74.1 | Low |
| Kollipara et al. (2008) | Observational, cross-sectional | 48 | 56 (11) | 67 | 67a | Low |
| Laramee et al. (2007) | Observational, cross-sectional | 998 | 65 | 46 | 97 | High |
| McNaughton et al. (2013) | Prospective cohort | 709 | 61.4 | 56.1 | 52.9 | Good |
| Peterson et al. (2011) | Prospective cohort | 1494 | 74.9 (10.7) | 46.8 | 82 | Good |
| Robinson et al. (2011) | Observational, cross-sectional | 609 | 66 (13) | 58.5 | 88.7 | High |
| Tung et al. (2014) | Observational, cross-sectional | 98 | 67.4 | 75.5 | 100c | Good |
Abbreviation: RCT, randomized controlled trial.
African American.
Hispanic.
Asian.
Prevalence of Low Health Literacy Among Heart Failure Patients
The prevalence of low health literacy ranged from 17.5% to 97%, with an average of 39% of the study participants found to have low health literacy. The Test of Functional Health Literacy in Adults–Short Form (S-TOFHLA)43 was the most commonly used health literacy instrument. The full-length TOFHLA44 was used in 2 of the studies. The studies that used the S-TOFHLA and TOFHLA reported that an average of 31% and 45% of their study participants, respectively, had low health literacy (inadequate and marginal health literacy). The proportions of study participants who had low health literacy in the studies that used the Subjective Health Literacy Scale,45 Rapid Estimate of Adult Literacy in Medicine–Revised,46 Newest Vital Sign,47 and Taiwan Health Literacy Scale48 were 28%, 34%, 97%, and 60%, respectively. A mean score of less than 3 on the Taiwan Health Literacy Scale defined inadequate health literacy (moderate to low).42 The other 3 health literacy instruments had dichotomized (low vs adequate health literacy) scoring. A score of less than 4 on the Newest Vital Sign,47 6 or less on the Rapid Estimate of Adult Literacy in Medicine–Revised,46 and greater than 10 on the Subjective Health Literacy Scale40 implied that someone had low health literacy.
Predictors of Low Health Literacy Among Heart Failure Patients
A number of variables were explored in relation to health literacy among patients with HF: age, gender, race/ethnicity, educational attainment, and cognitive function (Table 2). All 8 studies that explored the relationship between age and health literacy reported that as age increased, health literacy decreased. Age remained negatively correlated with health literacy even after controlling for years of education, race/ethnicity, gender, and immigration status.33 However, after controlling for cognitive function, the independent relationship between age and health literacy became nonsignificant.27 Gender was found to be a predictor of health literacy in 2 high-quality studies, with the female gender associated with higher health literacy levels (β = 3.59, P <.001, for 1 study27 and β = 7.941, P <.001, for the other41). Gender remained a significant predictor of health literacy even after adjusting for age, race, education, income, health status, sensory function, and cognitive function.27,41 However, in another set of 4 studies with good to high quality ratings, no significant association was found between gender and health literacy.23,24,40,49 It should be noted that these 4 studies analyzed the differences in gender composition between low and adequate health literacy using χ2 tests and no adjustment for potential covariates (eg, age, education) was performed. Among the 4 studies that explored the association between race/ethnicity and health literacy, 2 (using the same participant sample) reported that those with low health literacy tended to be Hispanics,23,24 whereas the other 2 studies reported that those participants with low health literacy were more likely to be African Americans.27,32 African Americans were found to have lower S-TOFHLA scores than the other races combined even after controlling for age, gender, years of education, health status, sensory function, and cognitive function.27 Educational attainment was also found to have a positive correlation with health literacy.23,24,35,39,40 Participants who had less than a high school education were more likely to have low health literacy even after controlling for age, gender, race/ethnicity, income, marital status, and insurance status (odds ratio, 5.04; 95% confidence interval, 3.31–7.69; P <.001).35
TABLE 2.
Health Literacy Trends and Correlations
| Statistically Significant
Correlates |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | HL Instrument |
% Low HL |
Age | Gender | Race/ Ethnicity |
Education | Cognitive Function |
Healthcare Utilization |
Mortality | Quality of Life |
Knowledge | Self-efficacy/ Self-care |
Medication Adherence |
| Baker et al. | S-TOFHLA | 37 | |||||||||||
| Dewalt et al. | |||||||||||||
| Macabasco et al. | ↑Age:↓HL | No significant difference | Hispanics:↓HL African Americans:↓HL |
↓Education: ↓HL | ↓HL: ↑HFQOL | ↓HL: ↓HF and salt knowledge | ↑HL: ↑self-efficacy and ↑self-care | ||||||
| Wu et al. | ↑Age:↓HL | No significant difference | Hispanics:↓HL | ↓Education: ↓HL | ↓HL: ↑admissions | ↓HL: ↓HF and salt knowledge | ↓HL: ↓self-care behaviors | ||||||
| Meyers et al. | S-TOFHLA | 19.2 | |||||||||||
| Mixon et al. | ↑HL:↓cardiac medication misunderstanding | ||||||||||||
| Morrow et al. (2006) | S-TOFHLA | 28 | ↑Age:↓HL | Women: ↑HL | African Americans:↓HL | ↑Cognitive function: ↑HL | |||||||
| Morrow et al. (2007) | |||||||||||||
| Murray et al. | ↑HL:↓HF-related admissions | ||||||||||||
| Noureldin et al. | ↑HL: ↑taking adherence and ↑scheduling adherence | ||||||||||||
| Chaudhry et al. | REALM-R | 34 | African Americans:↓HL | ||||||||||
| Chen et al. (2011) | S-TOFHLA | 28.5 | ↑HL: ↓self-care maintenance and ↓ self-care management | ||||||||||
| Chen et al. (2014) | S-TOFHLA | 31.8 | ↓Education: ↓HL | ↑HL: ↑HF knowledge | No significant association | ||||||||
| Cordasco et al. | TOFHLA | 41.6 | ↑Age:↓HL | ||||||||||
| Daley | NVS | 97 | |||||||||||
| Dennison et al. | S-TOFHLA | 61 | ↑Age:↓HL | No significant difference | ↑HL: THF knowledge | No significant association (maintenance/management) | |||||||
| Hawkins | S-TOFHLA | 19.2 | ↑Age:↓HL | ↑Cognitive function: ↓HL | |||||||||
| Kollipara et al. | TOFHLA | 47.9 | ↓HL: ↓salt knowledge | ||||||||||
| Laramee et al. | S-TOFHLA | 27 | ↓Education: ↓HL | ||||||||||
| SHLS | 38 | ||||||||||||
| McNaughton et al. | No significant association | ||||||||||||
| Peterson et al. | SHLS | 17.5 | ↑Age:↓HL | No significant difference | ↓Education: ↓HL | No significant association | ↓HL: ↓Mortality | ||||||
| Robinson et al. | S-TOFHLA | - | Women: ↑HL | ↑HL: ↑HF knowledge | No significant association | ||||||||
| Tung et al. | THLS | 60.2 | ↑Age:↓HL | ↑HL: ↑social-QOL | ↑HL: ↑self-care maintenance and ↑self-care confidence | ||||||||
Abbreviations: HF, heart failure; HFQOL, heart failure quality of life; HL, health literacy; NVS, Newest Vital Sign; REALM-R, Rapid Estimate of Adult Literacy in Medicine-Revised; SHLS, Subjective Health Literacy Scale; S-TOFHLA, Test of Functional Health Literacy in Adults-Short Form; THLS, Taiwan Health Literacy Scale.
Cognitive function was examined in 2 studies that targeted older HF patients. The studies yielded a strong positive correlation between cognitive function and health literacy (r = 0.545, P <.01).27,34 Study participants with better cognitive function showed higher health literacy. Cognitive ability remained a strong predictor of health literacy even after adjusting for age, gender, race/ethnicity, educational attainment, comorbidity, and sensory function (β = 0.39, P <.001).27
Health Literacy, Heart Failure Self-care, and Common Heart Failure Outcomes
The findings pertaining to the relationship between health literacy and HF self-care were inconclusive. Of the 4 studies that used the Self-care of Heart Failure Index, 1 found no direct or indirect association between health literacy and HF self-care,39 2 found no significant association between health literacy and self-care management,42,49 1 found a significant correlation between lower health literacy and better self-care management (r = −0.573, P = .001),38 2 found a significant association between higher health literacy and better self-care maintenance (r = 0.357, P = .006, for 1 study38 and β = 5.933, P = .002, for the other study42), whereas 1 study found no significant correlation49 and 2 studies found significant associations between higher health literacy and higher self-care confidence (β = 9.834, P <.001, for both42,49), while 1 study did not.38 Two studies that used the same participant sample used the adapted version of the Improving Chronic Illness Care Evaluation survey to measure HF self-care behaviors, and both reported significant associations (β = 0.81; 95% confidence interval, 0.43–1.19; P <.001).23,24 Both studies found that lower health literacy was associated with poorer self-care behaviors. 23,24 Finally, 1 study used the European HF Self-care Behavior Scale and found no significant relationship between health literacy and HF self-care.41
The following HF outcomes were explored in the studies included in this systematic review: HF-related hospitalizations, all-cause hospitalizations, 30-day rehospitalizations, mortality, quality of life, HF knowledge, dietary sodium knowledge, and medication adherence. Low health literacy was found to be associated with increased incidence of HF-related hospitalizations (incidence rate ratio, 1.42; 95% confidence interval, 1.11–1.83) even after controlling for age, race, gender, socioeconomic status, education level, insurance coverage, clinical characteristics, and self-management skills.24 Participants with adequate health literacy had 64% fewer HF-related admissions (incidence rate ratio, 0.34; 95% confidence interval, 0.15–0.76).29 The as sociation between health literacy and all-cause hospitalizations was inconclusive. One high-quality study reported that low health literacy was associated with increased all-cause hospital admissions (incidence rate ratio, 1.43; 95% confidence interval, 1.00–2.05). However, 2 good-quality studies found no association between health literacy and all-cause hospitalizations.29,40 One of these studies initially found that low health literacy was associated with increased risk of all-cause hospitalization (unadjusted hazard ratio, 1.45; 95% confidence interval 1.13–1.86; P <.001); however, after adjusting for age, gender, race, socioeconomic status, educational attainment, comorbidity, and left ventricular ejection fraction, health literacy was no longer significantly associated with an increased risk of all-cause hospitalization (adjusted hazard ratio, 1.05; 95% confidence interval, 0.8–1.37; P = .73).40 One study also found that low health literacy was not associated with an increased odds of 30-day rehospitalizations (odds ratio, 1.17; 95% confidence interval, 0.83–1.65; P = .37).37 On the other hand, low health literacy was found to be associated with increased risk of mortality even after controlling for possible confounders (adjusted hazard ratio, 1.97; 95% confidence interval, 1.3–2.97; P = .001).40
Health literacy was positively associated with HF-related quality of life. In 1 study, participants with adequate health literacy had higher quality of life scores even after adjustment for race/ethnicity, age, insurance coverage, and subjective socioeconomic status (adjusted difference, 8.20; 95% confidence interval, 4.14–12.27; P <.001).23 In another study, health literacy was positively associated with social-related quality of life even after controlling for comorbid condition (β = 2.499; F = 16.702; P <.01); however, there were no significant associations found between health literacy and physical-related quality of life (β = 2.193; F = 3.203; P = .077) and emotional-relatedqualityof life (β = 1.597; F = 0.978; P = .610).42
Five studies found significant positive correlations between health literacy and HF knowledge.23,24,39,41,49 Participants with adequate health literacy had better HF knowledge compared with participants with low health literacy. The same was true for salt knowledge, with 3 studies reporting significant positive associations between health literacy and salt knowledge.23,24,36
The 2 studies that explored the relationship between health literacy and medication adherence both reported significant associations. One study found that higher health literacy was associated with lower odds of misunderstanding cardiac medication indication, dose, and frequency (odds ratio, 0.84; 95% confidence interval, 0.74–0.95).26 And the other study found that participants with adequate health literacy had higher medication taking adherence and medication scheduling adherence.30
Discussion
Based on the studies included in this systematic review, an average of 39% of HF patients have low health literacy. It should be noted that this number is only an estimate of the magnitude of low health literacy among HF patients. Considering that 2 of the studies included patients diagnosed with acute coronary syndrome and only the total low health literacy prevalence was reported and not the prevalence for each diagnosis, the pooled estimate might overestimate the actual prevalence of low health literacy within the HF population. However, 4 of the studies noted that a portion of their study participants failed to take/complete the health literacy measure. Cordasco et al33 posited that some of the noncompleters likely refused to answer the health literacy questions to hide their limited health literacy, which would underestimate the prevalence of low health literacy. In addition, the studies required signed informed consents, which could have discouraged HF patients with low health literacy from participating in the studies given that most consent forms are written at a 10th-grade reading level.50 Lastly, most of the studies excluded patients who could not speak/understand English and those with cognitive impairment, which, according to the findings of this review, are predictors of low health literacy. These exclusions further underestimate the prevalence of low health literacy in this population. In addition, the potential selection bias imposed by the studies’ inclusion criteria could have systematically excluded HF patients with low health literacy.
Consistent with previous studies on non-HF patients, age, race/ethnicity, years of education, and cognitive function were found to be independent predictors of health literacy among HF patients. On the other hand, there was conflicting evidence regarding the association between gender and health literacy. In a study of community-dwelling older adults, age was found to be a significant predictor of health literacy even after adjusting for sex, race/ethnicity, and educational attainment.51 Similarly, race/ethnicity was also found to be associated with health literacy. Cho and colleagues52 reported that African Americans had lower health literacy compared with whites. Sentell and Braun,53 in their study involving 48 427 adults, found that the prevalence of low health literacy was higher in Latinos compared with whites. In a systematic review of health literacy in the chronic kidney disease population, education was reported to be positively associated with health literacy. Finally, in a study involving 414 community-dwelling seniors, poor cognitive function was associated with low health literacy even after adjusting for age, sex, race/ethnicity, education, English proficiency, monthly income, and health status.54
There was consistent evidence from multiple studies that suggested a positive correlation between health literacy and knowledge. Study participants with adequate health literacy had significantly higher scores on HF and salt knowledge measures. Similarly, there was consistent evidence supporting the association between adequate health literacy and better medication adherence. Conversely, the relationship between health literacy and HF self-care cannot be supported (or refuted) because of conflicting evidence. The heterogeneity of HF self-care measures used further complicates the synthesis of findings. Among the HF outcomes, an association between adequate health literacy and lower risk for HF-related hospitalization was reported; however, only 2 studies explored these associations. There was also a paucity of studies that explored the relationship between health literacy and mortality in the HF population. However, the single study that explored the relationship between health literacy and all-cause mortality had a large sample size (n = 1494) and adjusted for possible confounders, and it reported a correlation between low health literacy and higher risk of mortality. Finally, adequate health literacy was found to be associated with better HF-related quality of life.
It should be noted that the studies included in this review conceptually defined health literacy in a variety of ways. Eight of the studies failed to provide a conceptual definition of health literacy; 2 of the studies simply defined health literacy as the ability to read and comprehend health-related information; and the rest recognized the multifaceted nature of health literacy that goes beyond the ability to read and comprehend health-related information. The heterogeneity of conceptual definition provided was not surprising given that health literacy experts have not reached a consensus on how to define health literacy.19,55 Regardless of differing opinions, most experts do agree that health literacy is more than just the ability to read and comprehend health information.56 Consequently, this calls into question the adequacy of current measures of health literacy. As previously stated, S-TOFHLA was the most frequently used health literacy measure among the studies included in this review; however, only 2 studies acknowledged that the S-TOFHLA does not completely capture all the dimensions of health literacy.27,49 The potential measurement bias created from using nonspecific or generic health literacy instruments might have contributed to some of the inconsistent findings reported in the HF literature.
Similar to other systematic reviews, the quality of this review is dependent upon the quality of the included studies. It should be noted that studies with low quality ratings, primarily because of small sample size, were included in this review; however, most of the studies earned good and high quality ratings. Another limitation is that most of the studies were observational; hence, causation cannot be established. The heterogeneity of the measures used, both for health literacy and the HF outcomes, limited the synthesis of the findings. Lastly, all but 1 of the studies were conducted in the United States, which limits the generalizability of the findings of this review to other countries with different healthcare systems and social structures. Among the strengths of this systematic review is that it was not limited to published studies, which eliminates publication bias. Another strength was the use of an extensive search strategy involving multiple databases searched under the guidance of an expert medical librarian.
Conclusion
Age, race/ethnicity, years of education, and cognitive function were found to be independent predictors of low health literacy. In particular, HF patients who were older, were African American or Latino, had less years of education, and had cognitive impairment were more likely to have low health literacy. Adequate health literacy was consistently correlated with higher HF knowledge and higher salt knowledge.
Implications for Practice and Future Research
Nurses and other healthcare professionals should recognize that low health literacy is prevalent and start to adopt strategies that can potentially mitigate the impact of low health literacy when communicating with HF patients. Communication strategies, such as those outlined in the Agency for Healthcare Research and Quality Health Literacy Universal Toolkit,57 can be a good starting point. The use of teach-back method, literacy-sensitive education materials, videos, and easy-to-read signs are just some of the strategies outlined in the toolkit.57 Future studies should consider the use of a more complete measure of health literacy, one that measures all the dimensions of health literacy and not just reading comprehension. Instrument developers should consider using item response theory, as opposed to classical test theory, because it provides item-level information (item difficulty and item discrimination). It also allows one to perform differential item functioning analysis to ensure that the instrument performs the same way for different groups of people. It is possible that independent predictors of low health literacy identified in this systematic review could just be the result of an instrument that functions differently for different groups. Lastly, in the future, researchers should use theoretical frameworks to guide their studies and examine potential mediators and moderators of health literacy.
What's New and Important.
■ An average of 39% of HF patients have low health literacy.
■ Predictors of low heath literacy among HF patients include increased age, being African American/Hispanic, low educational attainment, and cognitive impairment.
■ Adequate health literacy is consistently associated with higher HF knowledge.
Acknowledgments
The primary author is supported by a predoctoral fellowship in Interdisciplinary Training in Cardiovascular Health Research (NIH/NINR T32 NR012704).
Footnotes
Author contributions: M.I.C. and T.R.C., review of papers and manuscript preparation; H.H., manuscript preparation and review.
The authors have no conflicts of interest to disclose.
The tool is available at http://www.hopkinsmedicine.org/institute_nursing/continuing_education/ebp/ebp_books_consultations.html
Contributor Information
Maan Isabella Cajita, School of Nursing, Johns Hopkins University, Baltimore, Maryland..
Tara Rafaela Cajita, Advocate Health Care, Park Ridge, Illinois..
Hae-Ra Han, School of Nursing, Department of Community-Public Health, Johns Hopkins University, Baltimore, Maryland..
REFERENCES
- 1.Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics–2014 update: a report from the American Heart Association. Circulation. 2014;129(3):e28–e292. doi: 10.1161/01.cir.0000441139.02102.80. doi:10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vincent GK, Velkoff VA. [September 9, 2014];The Older Population in the United States: 2010 to 2050. 2010 :25–1138. http://www.census.gov/prod/2010pubs/p25-1138.pdf.
- 3.Heidenreich PA, Albert NM, Allen LA, et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6(3):606–619. doi: 10.1161/HHF.0b013e318291329a. doi:10.1161/HHF.0b013e318291329a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;128(16):e240–e327. doi: 10.1161/CIR.0b013e31829e8776. doi:10.1161/CIR.0b013e31829e8776. [DOI] [PubMed] [Google Scholar]
- 5.Nielsen-Bohlman L, Panzer AM, Kindig DA, editors. Health Literacy: A Prescription to End Confusion. The National Academies Press; Washington, DC: 2004. [PubMed] [Google Scholar]
- 6.Kutner M, Greenberg E, Jin Y, Paulsen C. The Health Literacy of America’s Adults: Results From the 2003 National Assessment of Adult Literacy (NCES 2006 -483) U.S. Department of Education. National Center for Education Statistics; Washington, DC: 2006. [Google Scholar]
- 7.Schillinger D, Grumbach K, Piette J, et al. Association of health literacy with diabetes outcomes. JAMA. 2002;288(4):475–482. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- 8.Mayeaux EJ, Murphy PW, Arnold C, Davis TC, Jackson RH, Sentell T. Improving patient education for patients with low literacy skills. Am Fam Physician. 1996;53(1):205–211. [PubMed] [Google Scholar]
- 9.Williams MV, Baker DW, Parker RM, Nurss JR. Relationship of functional health literacy to patients’ knowledge of their chronic disease. Arch Intern Med. 1998;158:166–172. doi: 10.1001/archinte.158.2.166. [DOI] [PubMed] [Google Scholar]
- 10.Williams MV, Parker RM, Baker DW, et al. Inadequate functional health literacy among patients at two public hospitals. [March 21, 2014];JAMA. 1995 274(21):1677–1682. http://www.ncbi.nlm.nih.gov/pubmed/7474271. [PubMed] [Google Scholar]
- 11.Kalichman SC, Benotsch E, Suarez T, Catz S, Miller J, Rompa D. Health literacy and health-related knowledge among persons living with HIV/AIDS. [August 30, 2014];Am J Prev Med. 2000 18(4):325–331. doi: 10.1016/s0749-3797(00)00121-5. http://www.ncbi.nlm.nih.gov/pubmed/10788736. [DOI] [PubMed] [Google Scholar]
- 12.Gazmararian JA, Williams MV, Peel J, Baker DW. Health literacy and knowledge of chronic disease. Patient Educ Couns. 2003;51(3):267–275. doi: 10.1016/s0738-3991(02)00239-2. doi:10.1016/S0738-3991(02)00239-2. [DOI] [PubMed] [Google Scholar]
- 13.Williams MV, Baker DW, Honig EG, Lee TM, Nowlan A. Inadequate literacy is a barrier to asthma knowledge and self-care. [August 30, 2014];Chest. 1998 114(4):1008–1015. doi: 10.1378/chest.114.4.1008. http://www.ncbi.nlm.nih.gov/pubmed/9792569. [DOI] [PubMed] [Google Scholar]
- 14.Persell SD, Osborn CY, Richard R, Skripkauskas S, Wolf MS. Limited health literacy is a barrier to medication reconciliation in ambulatory care. J Gen Intern Med. 2007;22(11):1523–1526. doi: 10.1007/s11606-007-0334-x. doi:10.1007/s11606-007-0334-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Scott TL, Gazmararian JA, Williams MV, Baker DW. Health literacy and preventive health care use among Medicare enrollees in a managed care organization. [August 30, 2014];Med Care. 2002 40(5):395–404. doi: 10.1097/00005650-200205000-00005. http://www.ncbi.nlm.nih.gov/pubmed/11961474. [DOI] [PubMed] [Google Scholar]
- 16.Wolf MS, Gazmararian JA, Baker DW. Health literacy and functional health status among older adults. Arch Intern Med. 2005;165:1946–1952. doi: 10.1001/archinte.165.17.1946. doi:10.1111/j.1365-2702.2008.02739.x. [DOI] [PubMed] [Google Scholar]
- 17.Baker DW, Parker RM, Williams MV, Clark WS, Nurss J. The relationship of patient reading ability to self-reported health and use of health services. [August 30, 2014];Am J Public Health. 1997 87(6):1027–1030. doi: 10.2105/ajph.87.6.1027. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1380944&tool=pmcentrez&render-type=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baker DW, Parker RM, Williams MV, Clark WS. Health literacy and the risk of hospital admission. [August 30, 2014];J Gen Intern Med. 1998 13(12):791–798. doi: 10.1046/j.1525-1497.1998.00242.x. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1497036&tool=pmcentrez&rendertype=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Berkman ND, Davis TC, McCormack L. Health literacy: what is it? J Health Commun. 2010;15(suppl 2):9–19. doi: 10.1080/10810730.2010.499985. doi:10.1080/10810730.2010.499985. [DOI] [PubMed] [Google Scholar]
- 20.AMA Health literacy: report of the Council on Scientific Affairs. JAMA. 1999;281(6):552–557. [PubMed] [Google Scholar]
- 21.Baker DW, Dewalt DA, Schillinger D, et al. The effect of progressive, reinforcing telephone education and counseling versus brief educational intervention on knowledge, self-care behaviors and heart failure symptoms. J Card Fail. 2011;17(10):789–796. doi: 10.1016/j.cardfail.2011.06.374. doi:10.1016/j.cardfail.2011.06.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.DeWalt DA, Schillinger D, Ruo B, et al. Multisite randomized trial of a single-session versus multisession literacy-sensitive self-care intervention for patients with heart failure. Circulation. 2012;125(23):2854–2862. doi: 10.1161/CIRCULATIONAHA.111.081745. doi:10.1161/CIRCULATIONAHA.111.081745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Macabasco-O'Connell A, DeWalt DA, Broucksou KA, et al. Relationship between literacy, knowledge, self-care behaviors, and heart failure-related quality of life among patients with heart failure. J Gen Intern Med. 2011;26(9):979–986. doi: 10.1007/s11606-011-1668-y. doi:10.1007/s11606-011-1668-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wu J-R, Holmes GM, DeWalt DA, et al. Low literacy is associated with increased risk of hospitalization and death among individuals with heart failure. J Gen Intern Med. 2013;28(9):1174–1180. doi: 10.1007/s11606-013-2394-4. doi:10.1007/s11606-013-2394-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Meyers AG, Salanitro A, Wallston KA, et al. Determinants of health after hospital discharge: rationale and design of the Vanderbilt Inpatient Cohort Study ( VICS ). BMC Health Serv Res. 2014;14(10):1–10. doi: 10.1186/1472-6963-14-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mixon AS, Myers AP, Leak CL, et al. Characteristics associated with postdischarge medication errors. Mayo Clin Proc. 2014;89(8):1042–1051. doi: 10.1016/j.mayocp.2014.04.023. doi:10.1016/j.mayocp.2014.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Morrow D, Clark D, Tu W, et al. Correlates of health literacy in patients with chronic heart failure. [March 21, 2014];Gerontologist. 2006 46(5):669–676. doi: 10.1093/geront/46.5.669. http://www.ncbi.nlm.nih.gov/pubmed/17050758. [DOI] [PubMed] [Google Scholar]
- 28.Morrow DG, Weiner M, Steinley D, Young J, Murray MD. Patients’ health literacy and experience with instructions: influence preferences for heart failure medication instructions. J Aging Health. 2007;19(4):575–593. doi: 10.1177/0898264307304448. doi:10.1177/0898264307304448. [DOI] [PubMed] [Google Scholar]
- 29.Murray MD, Tu W, Wu J, Morrow D, Smith F, Brater DC. Factors associated with exacerbation of heart failure include treatment adherence and health literacy skills. Clin Pharmacol Ther. 2009;85(6):651–658. doi: 10.1038/clpt.2009.7. doi:10.1038/clpt.2009.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Noureldin M, Plake KS, Morrow DG, Tu W, Wu J, Murray MD. Effect of health literacy on drug adherence in patients with heart failure. [March 15, 2014];Pharmacotherapy. 2012 32(9):819–826. doi: 10.1002/j.1875-9114.2012.01109.x. http://www.scopus.com/inward/record.url?eid=2-s2.0-84867622247&partnerID=40&md5=0692e4d41a999bb7602388424667cb14. [DOI] [PubMed] [Google Scholar]
- 31.Daley CM. A hybrid transitional care program. Crit Pathw Cardiol. 2010;9(4):231–234. doi: 10.1097/HPC.0b013e3182018838. doi:10.1097/HPC.0b013e318 2018838. [DOI] [PubMed] [Google Scholar]
- 32.Chaudhry SI, Herrin J, Phillips C, et al. Racial disparities in health literacy and access to care among patients with heart failure. J Card Fail. 2011;17(2):122–127. doi: 10.1016/j.cardfail.2010.09.016. doi:10.1016/j.cardfail.2010.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cordasco KM, Asch SM, Franco I, Mangione CM. Health literacy and English language comprehension among elderly inpatients at an urban safety-net hospital. J Health Hum Serv Adm. 2009;32(1):30–50. [PubMed] [Google Scholar]
- 34.Hawkins LA. [August 26, 2014];Health literacy, cognitive impairment, and medication adherence in veterans with heart failure. 2012 Nov;:1–103. http://gradworks.umi.com/35/38/3538789.html.
- 35.Laramee AS, Morris N, Littenberg B. Relationship of literacy and heart failure in adults with diabetes. BMC Health Serv Res. 2007;7:98. doi: 10.1186/1472-6963-7-98. doi:10.1186/1472-6963-7-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kollipara UK, Jaffer O, Amin A, et al. Relation of lack of knowledge about dietary sodium to hospital readmission in patients with heart failure. Am J Cardiol. 2008;102(9):1212–1215. doi: 10.1016/j.amjcard.2008.06.047. doi:10.1016/j.amjcard.2008.06.047. [DOI] [PubMed] [Google Scholar]
- 37.Mcnaughton CD, Collins S, Kripalani S, Arbogast P, Naftilan A, Dittus RS. Lower numeracy is associated with increased odds of 30-day emergency department and hospital recidivism for patients with acute heart failure. Circ Hear Fail. 2013;6(1):40–46. doi: 10.1161/CIRCHEARTFAILURE.112.969477. doi:10.1161/CIRCHEARTFAILURE.112.969477.Lower. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chen AMH, Yehle KS, Plake KS, Murawski MM, Mason HL. Health literacy and self-care of patients with heart failure. J Cardiovasc Nurs. 2011;26(6):446–451. doi: 10.1097/JCN.0b013e31820598d4. doi:10.1097/JCN.0b013e31820598d4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chen AMH, Yehle KS, Albert NM, et al. Relationships between health literacy and heart failure knowledge, self-efficacy, and self-care adherence. Res Soc Adm Pharm. 2014;10(2):378–386. doi: 10.1016/j.sapharm.2013.07.001. doi:10.1016/j.sapharm.2013.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Peterson PN, Shetterly SM, Clarke CL, et al. Health literacy and outcomes among patients with heart failure. JAMA. 2011;305(16):1695–1701. doi: 10.1001/jama.2011.512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Robinson S, Moser D, Pelter MM, Nesbitt T, Paul SM, Dracup K. Assessing health literacy in heart failure patients? J Card Fail. 2011;17(11):887–892. doi: 10.1016/j.cardfail.2011.06.651. doi:10.1016/j.cardfail.2011.06.651.Assessing. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tung H-H, Lu T-M, Chen L-K, Liang S-Y, Wu S-F, Chu K-H. Health literacy impact on elderly patients with heart failure in Taiwan. J Clin Gerontol Geriatr. 2014;5(3):72–76. doi:10.1016/j.jcgg.2014.01.005. [Google Scholar]
- 43.Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. [August 30, 2014];Patient Educ Couns. 1999 38(1):33–42. doi: 10.1016/s0738-3991(98)00116-5. http://www.ncbi.nlm.nih.gov/pubmed/14528569. [DOI] [PubMed] [Google Scholar]
- 44.Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: a new instrument for measuring patients’ literacy skills. [March 21, 2014];J Gen Intern Med. 1995 10(10):537–541. doi: 10.1007/BF02640361. http://www.ncbi.nlm.nih.gov/pubmed/8576769. [DOI] [PubMed] [Google Scholar]
- 45.Chew LD, Griffin JM, Partin MR, et al. Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med. 2008;23(5):561–566. doi: 10.1007/s11606-008-0520-5. doi:10.1007/s11606-008-0520-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bass PF, Wilson JF, Griffith CH. A shortened instrument for literacy screening. J Gen Intern Med. 2003;18:1036–1038. doi: 10.1111/j.1525-1497.2003.10651.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Weiss BD, Mays MZ, Martz W, et al. Quick assessment of literacy in primary care: the Newest Vital Sign. Ann Fam Med. 2005;3(6):514–522. doi: 10.1370/afm.405. doi:10.1370/afm.405.College. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Su C, Chang S, Chen R, Pan F, Chen C, Liu W. A preliminary study of Taiwan Health Literacy Scale. J Formos Med Assoc. 2008;12:525–536. [Google Scholar]
- 49.Dennison CR, McEntee ML, Samuel L, et al. Adequate healthliteracyisassociatedwithhigherheartfailureknowledgeand self care confidence in hospitalized patients. J Cardiovasc Nurs. 2011;26(5):359–367. doi: 10.1097/JCN.0b013e3181f16f88. doi:10.1097/JCN.0b013e3181f16f88.Adequate. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Malik L, Kuo J, Yip D, Mejia A. How well informed is the informed consent for cancer clinical trials? [September 10, 2014];Clin Trials. 2014 doi: 10.1177/1740774514548734. doi:10.1177/1740774514548734. http://ctj.sagepub.com/content/early/2014/08/18/1740774514548734. [DOI] [PubMed]
- 51.Baker DW, Gazmararian JA, Sudano J, Patterson M. The association between age and health literacy among elderly persons. J Gerontol. 2000;55(6):S368YS374. doi: 10.1093/geronb/55.6.s368. [DOI] [PubMed] [Google Scholar]
- 52.Cho YI, Lee SD, Arozullah AM, Crittenden KS. Effects of health literacy on health status and health service utilization amongst the elderly. Soc Sci Med. 2008;66:1809–1816. doi: 10.1016/j.socscimed.2008.01.003. doi:10.1016/j.socscimed.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 53.Sentell T, Braun K. Low health literacy, limited English proficiency, and health status in Asians, Latinos and other racial/ethnic groups in California. J Health Commun. 2012;17(suppl 3):82–99. doi: 10.1080/10810730.2012.712621. doi:10.1080/10810730.2012.712621.Low. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Federman AD, Sano M, Wolf MS, Siu AL, Halm EA. Health literacy and cognitive performance among older adults. J Am Geriatr Soc. 2009;57(8):1475–1480. doi: 10.1111/j.1532-5415.2009.02347.x. doi:10.1111/j.1532-5415.2009.02347.x.Health. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.SLrensen K, Van den Broucke S, Fullam J, et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. 2012;12(1):80. doi: 10.1186/1471-2458-12-80. doi:10.1186/1471-2458-12-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pleasant A, McKinney J, Rikard RV. Health literacy measurement: a proposed research agenda. J Health Commun. 2011;16(suppl 3):11–21. doi: 10.1080/10810730.2011.604392. doi:10.1080/10810730.2011.604392. [DOI] [PubMed] [Google Scholar]
- 57.Dewalt D, Callahan L, Hawk V, et al. Health Literacy Universal Precautions. (Prepared by North Carolina Network Consortium, The Cecil G. Sheps Center for Health Services Research, The University of North Carolina at Chapel Hill, under Contract No. HHSA290200710014.) AHRQ Publication No. 10-0046-EF. Agency for Healthcare Research and Quality; Rockville, MD: 2010. [Google Scholar]