Abstract
Pneumomediastinum is a rare condition, and mostly occurs following traumatic or iatrogenic tracheal and oesophageal perforation, but spontaneous pneumomediastinum has also been described. We report a case of a 17-year-old woman who presented with a penetrating neck wound after a fall down the stairs. She had an extensive pneumomediastinum without signs of tracheal or oesophageal laceration, rib fractures, pneumothorax or haematothorax. The contaminated wound was surgically explored and extensively lavaged. Prophylactic antibiotic treatment was given and the patient recovered without complications. Direct perforating trauma to the mediastinum is a severe entity, but can be treated by lavage and prophylactic antibiotic therapy.
Background
Pneumomediastinum, a rare condition, is defined as the presence of free air in the mediastinal cavity, or mediastinal emphysema. Laënnec1 first described this diagnosis following chest trauma. However, primary pneumomediastinum, as first described by Hamman2, may also occur spontaneously. Further clinical work up is recommended, since pneumomediastinum may be life-threatening. We report a unique case of a 17-year-old woman with pneumomediastinum following penetrating neck trauma, with no signs of tracheal or oesophageal laceration, rib fractures, pneumothorax or haematothorax.
Case presentation
A 17-year-old woman with no medical or medication-use history, slipped and fell down a 3 m flight of stairs. She landed head first on a reed basket at the bottom of the stairs. She regained consciousness after a few seconds, and only experienced bleeding and pain in the anterior aspect of the neck.
At presentation to the emergency department, she was screened according to the principles of Advanced Trauma Life Support. Patients Glasgow Coma Scale was 15 on arrival. The airway was not compromised and cervical spine was protected. Examination of the chest revealed no signs of subcutaneous emphysema. Respiratory sounds were normal, and all vital signs were normal and stable. What was remarkable, however, was a small 2 cm wound, directly cranial to the right clavicle, with small pieces of reed within it (figure 1). The patient was checked for circulation and disabilities, and showed no abnormalities.
Figure 1.

A penetrating wound with corpus alienum directly above the right clavicle.
Investigations
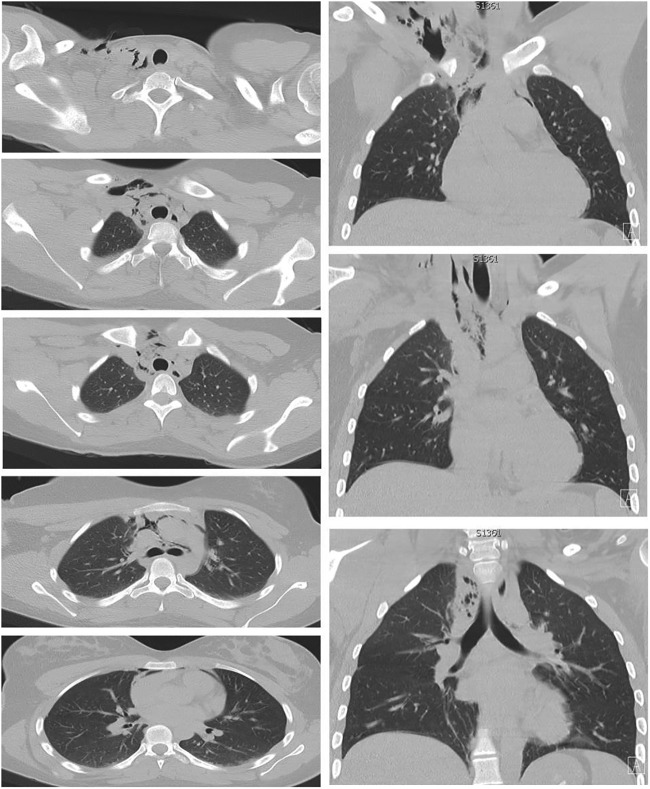
Laboratory examination was normal. X-ray of the chest and right clavicle demonstrated no signs of fractures, pneumothorax, haematothorax or extrapleural signs (figure 2). Cerebral CT scan did not reveal any cerebral abnormalities or fractures. There were also no signs of fractures on the cervical spine CT scan, but minimal subcutaneous emphysema was seen above the right clavicle, without signs of a pneumothorax (figure 3). In addition, a CT of the chest was performed, which revealed a large amount of subcutaneous emphysema starting from the wound above the right clavicle to the mediastinum with pneumomediastinum and without signs of pneumothorax or haematothorax, fractures, or tracheal or oesophageal laceration (figure 4).
Figure 2.
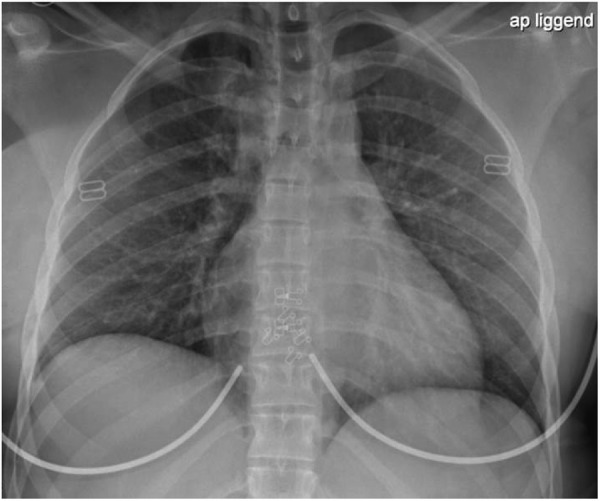
Chest X-ray performed in the emergency department.
Figure 3.

Cervical spine CT scan at presentation, with subcutaneous emphysema.
Figure 4.
Chest CT scan at presentation.
Differential diagnosis
The differential diagnoses are pneumomediastinum due to a penetrating injury, forceful straining during the fall and spontaneous or traumatic tracheal or oesophageal laceration.
Treatment
Our main aim was to clear any obvious airway injury, so we decided to perform bronchoscopy to exclude tracheal perforation, along with surgical exploration, in a combined session in the operating room. CT scan confirmed no obvious oesophageal injuries, therefore we discussed with the trauma team, and it was decided not to investigate the oesophagus prior to surgery. During intubation and ventilation, vital signs remained stable and within normal range, and there was no tension pneumothorax. Prophylactic intravenous antibiotics were administered before surgery. Bronchoscopy showed no signs of tracheal or bronchial injury. Local wound exploration (digital and blunt instrumental exploration) revealed a narrow but long 15 cm wound trajectory from cranial to right clavicle to mediastinum directly retrosternal. There was no major bleeding. Many fragments from the reed basket were removed from the subcutaneous tissue and from the wound trajectory to the mediastinum (figure 5). The wound was extensively lavaged. A small surgical drain was placed without closure of the wound due to contamination of the wound. The patient was extubated after surgery and transferred to the intensive care unit for 24 h of observation. Postoperatively, we prescribed antibiotics intravenously for 7 days to prevent mediastinitis.
Figure 5.

Drainage of the wound during surgery. Notice the large pieces of reed removed from the wound.
Outcome and follow-up
Follow-up chest X-ray at day 1 showed no extension of subcutaneous emphysema and pneumomediastinum (figure 6). There was no need for administration of oxygen, and pain was well controlled with analgetics. Food was prohibited for 24 h, followed by a liquid diet for a few days. Haemoglobin levels remained stable. C reactive protein and leucocyte count were checked daily and remained low. The wound was lavaged daily. The surgical drain was removed after 5 days. The patient recovered without complications and was discharged from the hospital 7 days following surgery. Oral antibiotic treatment was continued for 1 week. Wound lavage was continued daily after discharge. The small neck wound was almost closed, showed no evidence of infection and healed after 1 month (figure 7). At follow-up 2 months after discharge, the postoperative course remained uncomplicated.
Figure 6.
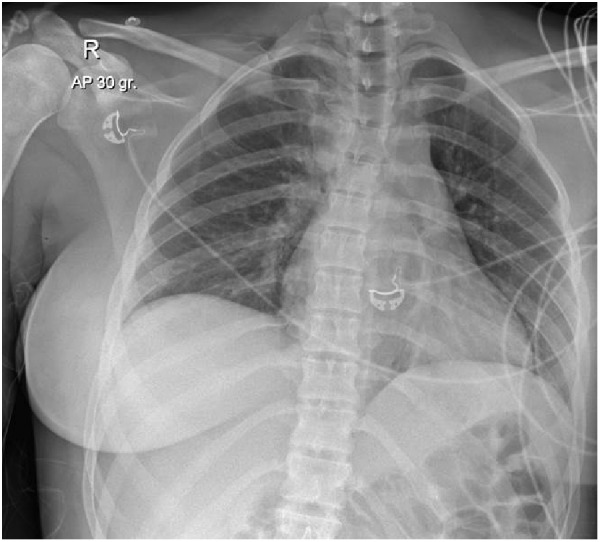
Chest X-ray performed at day 1 after surgery.
Figure 7.

Healing of the neck wound.
Discussion
We described a unique case with pneumomediastinum following perforating neck trauma, without obvious organ damage.
The aetiology of pneumomediastinum is extensive. Air from outside may enter the mediastinum after (penetrating) trauma or through iatrogenic causes (ie, cardiothoracic or thoracoscopic/mediastinal surgery, manipulation following tonsillectomy, thyroidectomy or dental procedures). Air leakage to the mediastinum may also result from the inside. Increased alveolar pressure (ie, due to positive pressure ventilation, airway obstruction, vomiting, coughing, Valsalva manoeuver, blunt chest trauma) or weak lung parenchyma (as in infection, emphysema, sarcoidosis, acute respiratory distress syndrome) may result in alveolar rupture. As a result, air may leak into the pulmonary interstitium with subsequent accumulation of free air along the sheath of the bronchi or pulmonary vessels going towards the mediastinum. This physiological phenomenon is called the ‘Macklin effect’, and is the most common cause in both traumatic and spontaneous pneumomediastinum.3 4 In a minority of cases, air may leak from a rupture of air-containing mediastinal structures, including the trachea, bronchi and oesophagus. Also, pneumomediastinum has been described after perforation of the nasopharynx and larynx or after air leakage from abnormal air collections in the abdomen. Furthermore, some organisms in the mediastinum or adjacent chest may also cause entry of gas into the mediastinum. Trauma is responsible for about 80% of cases with pneumomediastinum and more common due to blunt chest trauma than to perforating or iatrogenic trauma.4–6
Chest X-ray is usually the first diagnostic tool when patients present with chest symptoms, but it may be false negative for pneumomediastinum. Chest CT scan may be more effective.4 7 8 The Macklin effect can often be seen on chest CT scan and may help in the differentiation of aetiology of pneumomediastinum.7 The differentiation in aetiology is important since spontaneous pneumomediastinum is mostly self-limiting,8 while other more serious causes may require adjacent diagnostic tests and, often, surgical treatment.
In our case, subcutaneous emphysema was seen starting from the wound above the right clavicle to the mediastinum with pneumomediastinum. However, signs of perforating injury of the adjacent organs (trachea, oesophagus, lungs) or rib fractures were lacking. There were also no signs of pneumothorax or haematothorax. The patient only reported pain on the right side of her neck, but showed no other symptoms, and all ventilatory and haemodynamic vital signs were normal and stable. Therefore, the differential diagnosis was difficult. The perforating injury itself may have been the cause of pneumomediastinum, but this would be extremely rare. Furthermore, we did not want to miss other serious injuries, including unrecognised tracheal or oesophageal laceration. However, there were no clear signs of oesophageal or tracheal laceration on CT scan.
After discussion in the multidisciplinary team, with a trauma and lung surgeon, and an intensivist and pulmonologist, we decided to explore the wound in the operating room. The consideration not to perform a thoracoscopy was owing to the lack of intrathoracic abnormalities on chest CT scan, such as pneumothorax, haematothorax or lung contusion. In case of an unrecognised pneumothorax, this would be clearer during intubation and positive pressure ventilation. Therefore, chest tubes were available and prepared in the operating room, but no tension pneumothorax occurred. We performed a bronchoscopy directly after intubation to be sure not to miss tracheal laceration, and no abnormalities were seen, after which the wound was explored and extensively lavaged. It was suggested that the pneumomediastinum was the result of air entering from outside, due to negative intrathoracic pressure during breathing.
After surgery, the patient went to the intensive care unit for close observation, but remained stable during the first 24 h. It is open to discussion whether or not to perform chest X-rays during follow-up, as was performed in our patient. As mentioned before, outcome of chest X-rays may be false-negative and, also, if pneumothorax existed in our patient, it would have been seen during the artificial respiration in the operating room. However, with improvement of the clinical course and the absence of new findings on chest X-ray, it was likely that the pneumomediastinum did not result in mediastinitis or other complications. Furthermore, follow-up of bronchoscopy was unnecessary, since there was no evidence of tracheal laceration. Therefore, the patient was also extubated directly after surgery. As described before in the literature, there is no evidence for placing a chest tube in patients with only pneumomediastinum, unless they have concomitant pneumothorax.9 Mediastinal drainage is indicated after cardiothoracic surgery and when extensive mediastinitis is suspected.10 In our case, there were no signs of mediastinitis and therefore drainage was not indicated. Antibiotics were given to our patient as prophylaxis. In patients with spontaneous pneumomediastinum, antibiotics are not necessary, and there have been no reported cases of infection secondary to spontaneous pneumomediastinum.11 However, in our case, a reed basket perforated the skin barrier and pieces of reed were found in the mediastinum, resulting in a contaminated wound. To decrease the risk of mediastinitis, broad spectrum antibiotic treatment was given. Since the patient recovered well within a few days following surgery, there was no need for new interventions. Discharge criteria should include normalisation of vital signs, normal laboratory studies and relief of pain.
Learning points.
The differential diagnosis of pneumomediastinum is extensive and may include traumatic and spontaneous causes.
Direct penetrating trauma to the mediastinum itself can be a rare cause of pneumomediastinum. Wound lavage with antibiotic treatment is the first choice in such trauma.
Chest X-ray may be false negative for pneumomediastinum.
The Macklin effect seen on chest CT scan is an important finding and may help in the differentiation of aetiology.
Antibiotic treatment to prevent mediastinitis is not indicated for spontaneous pneumomediastinum, but it should be strongly considered for contaminated wounds.
Footnotes
Contributors: All the authors participated in the design of the study and performed a literature study of this subject. VK drafted the manuscript, but all the authors edited, read and approved the final manuscript. VK treated the patient at the emergency department and assisted during the operation. R Krol performed the surgery and treated the patient in the outpatient clinic. HMR was the anaesthesiologist on call, and treated the patient in the intensive care unit. PEJMS reported the CT scan. LMvR treated the patient during hospital stay.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Laënnec RT. De L'auscultation Médiate ou Traité du Diagnostic des Maladies des Poumon et du Coeur. Brosson & Chaudé, 1819. [Google Scholar]
- 2.Hamman L. Spontaneous mediastinal emphysema. Bull Johns Hopkins Hosp 1939;64:1–21. [Google Scholar]
- 3.Macklin MT, Macklin CC. Malignant interstitial emphysema of the lungs and mediastinum as an important occult complication in many respiratory diseases and other conditions: interpretation of the clinical literature in the light of laboratory experiment. Medicine 1944;23:281–358. 10.1097/00005792-194412000-00001 [DOI] [Google Scholar]
- 4.Wintermark M, Schnyder P. The Macklin effect: a frequent etiology for pneumomediastinum in severe blunt chest trauma. Chest 2001;120:543–7. 10.1378/chest.120.2.543 [DOI] [PubMed] [Google Scholar]
- 5.Banki F, Estrera AL, Harrison RG et al. Pneumomediastinum: etiology and a guide to diagnosis and treatment. Am J Surg 2013;206:1001–6. 10.1016/j.amjsurg.2013.08.009 [DOI] [PubMed] [Google Scholar]
- 6.Sahni S, Verma S, Grullon J et al. Spontaneous pneumomediastinum: time for consensus. N Am J Med Sci 2013;5:460–4. 10.4103/1947-2714.117296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Murayama S, Gibo S. Spontaneous pneumomediastinum and Macklin effect: overview and appearance on computed tomography. World J Radiol 2014;6:850–4. 10.4329/wjr.v6.i11.850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Okada M, Adachi H, Shibuya Y et al. Diagnosis and treatment of patients with spontaneous pneumomediastinum. Respir Investig 2014;52:36–40. 10.1016/j.resinv.2013.06.001 [DOI] [PubMed] [Google Scholar]
- 9.Iyer VN, Joshi AY, Ryu JH. Spontaneous pneumomediastinum: analysis of 62 consecutive adult patients. Mayo Clin Proc 2009;84:417–21. 10.1016/S0025-6196(11)60560-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Merrill WH, Akhter SA, Wolf RK et al. Simplified treatment of postoperative mediastinitis. Ann Thorac Surg 2004;78:608–12. 10.1016/j.athoracsur.2004.02.089 [DOI] [PubMed] [Google Scholar]
- 11.Al-Mufarrej F, Badar J, Gharagozloo F et al. Spontaneous pneumomediastinum: diagnostic and therapeutic interventions. J Cardiothorac Surg 2008;3:59 10.1186/1749-8090-3-59 [DOI] [PMC free article] [PubMed] [Google Scholar]