Expression of IKKα in intestinal epithelial cells promotes IL-22 production by group 3 innate lymphoid cells, and this axis is essential for defense against Citrobacter rodentium infection and to limit intestinal inflammation in response to DSS treatment.
Abstract
Innate lymphoid cells (ILCs) are critical for maintaining epithelial barrier integrity at mucosal surfaces; however, the tissue-specific factors that regulate ILC responses remain poorly characterized. Using mice with intestinal epithelial cell (IEC)–specific deletions in either inhibitor of κB kinase (IKK)α or IKKβ, two critical regulators of NFκB activation, we demonstrate that IEC-intrinsic IKKα expression selectively regulates group 3 ILC (ILC3)–dependent antibacterial immunity in the intestine. Although IKKβΔIEC mice efficiently controlled Citrobacter rodentium infection, IKKαΔIEC mice exhibited severe intestinal inflammation, increased bacterial dissemination to peripheral organs, and increased host mortality. Consistent with weakened innate immunity to C. rodentium, IKKαΔIEC mice displayed impaired IL-22 production by RORγt+ ILC3s, and therapeutic delivery of rIL-22 or transfer of sort-purified IL-22–competent ILCs from control mice could protect IKKαΔIEC mice from C. rodentium–induced morbidity. Defective ILC3 responses in IKKαΔIEC mice were associated with overproduction of thymic stromal lymphopoietin (TSLP) by IECs, which negatively regulated IL-22 production by ILC3s and impaired innate immunity to C. rodentium. IEC-intrinsic IKKα expression was similarly critical for regulation of intestinal inflammation after chemically induced intestinal damage and colitis. Collectively, these data identify a previously unrecognized role for epithelial cell–intrinsic IKKα expression and TSLP in regulating ILC3 responses required to maintain intestinal barrier immunity.
Maintenance of epithelial barrier integrity at mucosal surfaces is essential to limit exposure to commensal and pathogenic microorganisms and to promote intestinal homeostasis (Artis, 2008; Hooper and Macpherson, 2010; Fung et al., 2014; Peterson and Artis, 2014). Defects in epithelial barrier function are associated with multiple infectious and inflammatory diseases, including inflammatory bowel disease (IBD; Pasparakis, 2008; Marchiando et al., 2010; Maloy and Powrie, 2011), and recent studies have highlighted a critical role for innate lymphoid cells (ILCs) in regulating immunity, inflammation, and tissue repair at barrier surfaces such as the intestine (Spits and Cupedo, 2012; Walker et al., 2013; McKenzie et al., 2014; Sonnenberg, 2014; Artis and Spits, 2015). ILCs represent a heterogeneous family of cells that, based on their expression of the transcription factors T-bet, GATA3, and RORγt, can be categorized into three groups with diverse effector functions. Group 1 ILCs (ILC1s) express IFNγ and T-bet and include NK cells (Spits and Cupedo, 2012), whereas ILC2s express GATA3, RORα, MHCII, IL-5, IL-13, and amphiregulin and regulate inflammation, barrier integrity, and/or tissue homeostasis in the skin, intestine, lung, and adipose tissue (Neill et al., 2010; Monticelli et al., 2011; Molofsky et al., 2013; Roediger et al., 2013; Oliphant et al., 2014; Brestoff et al., 2015; Lee et al., 2015). RORγt+ ILC3s express IL-17A, IFNγ, MHCII, lymphotoxin (LT)α1β2, and IL-22 and promote antibacterial immunity, secondary lymphoid structure formation, and the regulation of intestinal inflammation (Buonocore et al., 2010; Kiss et al., 2011; Tumanov et al., 2011; Sonnenberg et al., 2012; Hepworth et al., 2013, 2015; Goto et al., 2014). Although IL-17A and IFNγ production by ILC1s or ILC3s is implicated in the pathogenesis of colitis (Buonocore et al., 2010; Geremia et al., 2011; Spits and Di Santo, 2011), ILC3-derived IL-22 is associated with the promotion of epithelial barrier integrity at multiple tissue sites (Aujla et al., 2008; Satoh-Takayama et al., 2008; Sonnenberg et al., 2012; Goto et al., 2014). Ligation of the IL-22 receptor, expression of which is restricted to nonhematopoietic cell lineages such as epithelial cells, induces expression of host defense genes, mucins, and antimicrobial peptides (AMPs) that are critical for host-protective immunity after exposure to viruses and bacterial infections such as Klebsiella pneumoniae and Citrobacter rodentium (Aujla et al., 2008; Zheng et al., 2008; Kim et al., 2012; Klatt et al., 2012; Ivanov et al., 2013; Goto et al., 2014; Zhang et al., 2014; Muñoz et al., 2015). Although the influence of RORγt+ ILC3s on epithelial barrier function is well characterized, the molecular and cellular pathways that regulate ILC responses in mucosal tissue microenvironments remain poorly understood.
In addition to providing a physical barrier to microorganisms, intestinal epithelial cells (IECs) express cytokines, chemokines, pattern recognition receptors, inflammasomes, and AMPs that permit cross-talk with mucosal immune cells and maintenance of immune homeostasis (Strober, 1998; Pasparakis, 2008; Rescigno, 2011; Welz et al., 2011; Goto and Ivanov, 2013; Dannappel et al., 2014; Kagnoff, 2014; Peterson and Artis, 2014). For example, signals derived from IECs regulate proinflammatory cytokine secretion by DCs (Nenci et al., 2007; Zaph et al., 2007), enhancing their ability to promote regulatory and TH2-cytokine responses (Rimoldi et al., 2005a,b; Iliev et al., 2009). IECs also secrete cytokines that regulate macrophage function (Smythies et al., 2005) and B cell production of secretory IgA (Xu et al., 2007; Cerutti, 2008). Genetic approaches to interrogate the factors that regulate IEC function have identified a critical role for NFκB-associated genes, including inhibitor of κB kinase (IKK)β or IKKα, which control “canonical” versus “noncanonical” NFκB-dependent gene expression, respectively (Greten et al., 2004; Nenci et al., 2007; Zaph et al., 2007; Eckmann et al., 2008; Vlantis et al., 2011; Bonnegarde-Bernard et al., 2014; Takahashi et al., 2014; Vereecke et al., 2014). Although ILC3s are known to regulate IEC function via IL-17A and IL-22 expression (Aujla et al., 2008; Zheng et al., 2008; Hanash et al., 2012; Muñoz et al., 2015), whether tissue-resident nonhematopoietic cells such as IECs can reciprocally regulate intestinal ILC3 responses remains incompletely defined. In the present study, we demonstrate that mice with IEC-specific deletions in IKKα, but not IKKβ, exhibit impaired innate immunity to C. rodentium infection, identifying a previously unappreciated role for the noncanonical NFκB activation pathway in antibacterial immunity. Critically, mice with IEC-intrinsic IKKα deletions displayed impaired IL-22 production by RORγt+ ILC3s and delivery of recombinant IL-22 or IL-22–competent sort-purified ILCs was sufficient for restoration of protection against C. rodentium infection. IEC-intrinsic IKKα was also critical for regulation of intestinal inflammation after chemically induced intestinal damage and colitis. Mechanistically, the absence of IKKα expression resulted in elevated thymic stromal lymphopoietin (TSLP) production by colonic epithelial cells, which negatively regulated IL-22 production by ILC3s in vitro and innate immunity to C. rodentium in vivo. Furthermore, neutralization of TSLP in IKKαΔIEC mice could partially restore ILC3 responses and innate immunity to C. rodentium. Collectively, these data highlight a previously unrecognized mechanism by which IECs and ILC3s reciprocally regulate intestinal immune homeostasis.
RESULTS
IEC-intrinsic IKKα, but not IKKβ, expression is critical for immunity to C. rodentium infection
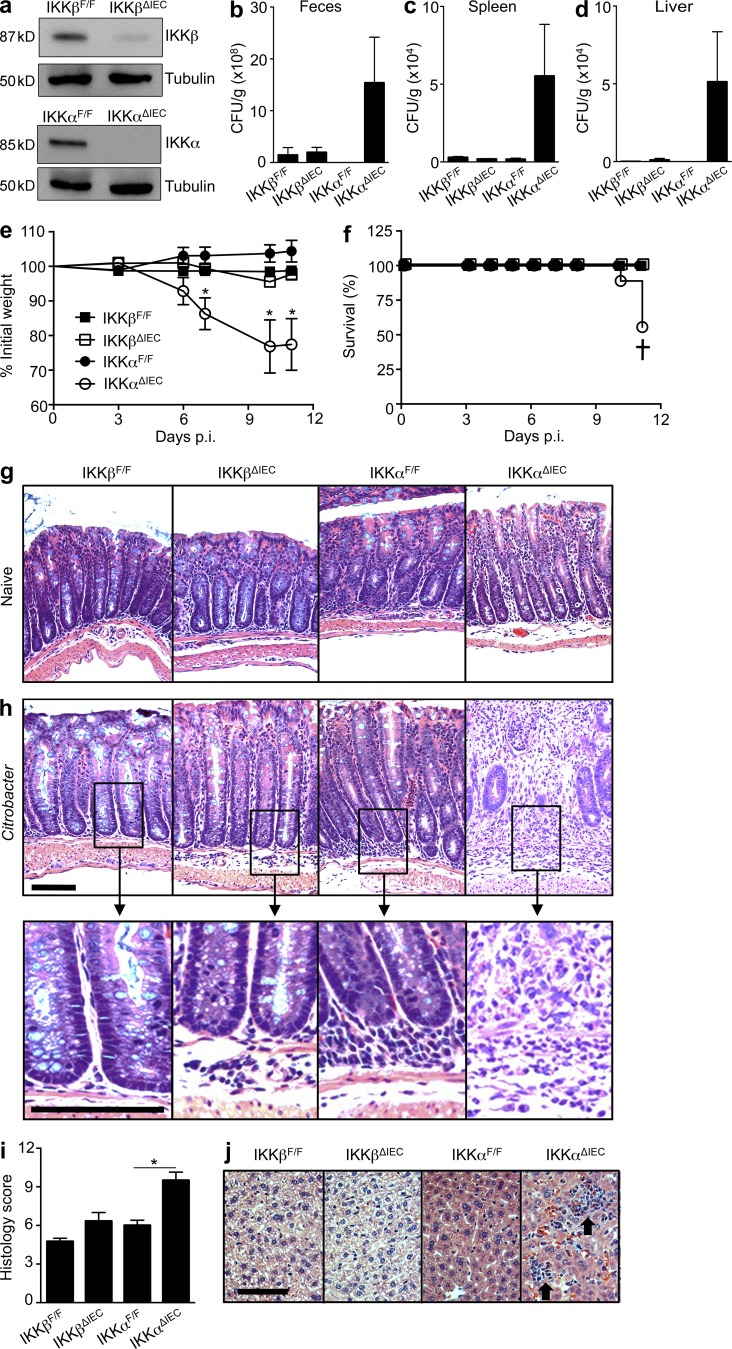
C. rodentium is a natural gram-negative extracellular bacterial pathogen of mice akin to the human pathogen enterohemorrhagic Escherichia coli that causes NFκB activation and colonic lesions after attachment to the epithelial surface (Mundy et al., 2005; Wang et al., 2006; Chandrakesan et al., 2010). Innate immunity to C. rodentium and regulation of intestinal barrier integrity is controlled, in part, by ILC3-dependent IL-22 responses (Satoh-Takayama et al., 2008; Zheng et al., 2008; Kiss et al., 2011; Sonnenberg et al., 2011b; Tumanov et al., 2011). However, the function of IEC-intrinsic NFκB activation and whether it regulates antibacterial immunity and tissue-protective ILC responses is unknown. Using mice with IEC-specific deletions in either IKKβ or IKKα, respectively, we assessed whether IEC-intrinsic canonical versus noncanonical NFκB activation regulates intestinal ILC responses. To do so, IKKβF/F or IKKαF/F mice in which either the Ikkβ or Ikkα genes are flanked by LoxP sites were crossed with mice expressing Cre recombinase under control of the IEC-specific villin promoter to generate IEC-specific IKKβ (IKKβΔIEC) or IKKα (IKKαΔIEC) knockout mice, as described previously (Nenci et al., 2007). Deletion of IKKβ in IECs from IKKβΔIEC mice and IKKα in IECs from IKKαΔIEC mice was confirmed by Western blotting (Fig. 1 a). To examine the potential influence of IECs on the functions of ILCs under inflammatory conditions, we infected IKKβΔIEC, IKKαΔIEC, and littermate control mice with C. rodentium. Although IKKβΔIEC mice exhibited equivalent fecal C. rodentium burdens to IKKβF/F mice at day 5 postinfection (p.i.), IKKαΔIEC mice displayed higher fecal bacterial titers (Fig. 1 b) and enhanced bacterial dissemination to peripheral organs, including the spleen and liver at day 11 p.i. compared with IKKαF/F controls (Fig. 1, c and d). Associated with an impaired ability to control C. rodentium infection, IKKαΔIEC, but not IKKβΔIEC, mice displayed exacerbated infection-induced weight loss (Fig. 1 e), and ∼50% of IKKαΔIEC mice succumbed to infection by day 11 p.i. (Fig. 1 f). IKKαΔIEC mice that survived beyond day 12 p.i. were able to resolve the infection and regain weight at a similar level to that of control mice (not depicted). Histological analyses demonstrated that deletion of IKKα or IKKβ in IECs was not associated with altered intestinal immune homeostasis in the steady state (Fig. 1 g), consistent with a previous study (Nenci et al., 2007). However, although C. rodentium–infected IKKβF/F, IKKβΔIEC, and IKKαF/F mice exhibited modest intestinal inflammation at day 11 p.i. (Fig. 1 h), infected IKKαΔIEC mice exhibited severe inflammation, characterized by disruption of normal epithelial crypt architecture, mucosal hyperplasia, and colonic ulceration (Fig. 1 h), resulting in a significantly higher colonic pathology score relative to control mice (Fig. 1 i). Associated with a loss of intestinal barrier integrity and bacterial dissemination, neutrophil-rich inflammatory foci were observed in the liver of IKKαΔIEC mice at day 11 p.i. (Fig. 1 j). Collectively, these data highlight the selective requirement for IEC-intrinsic expression of IKKα for regulation of antibacterial immune responses and intestinal barrier homeostasis.
Figure 1.
IEC-intrinsic IKKα, but not IKKβ, expression is critical for immunity to C. rodentium infection. (a) IKKβ and IKKα expression in IECs from naive IKKβF/F, IKKαF/F, IKKβΔIEC, and IKKαΔIEC mice as detected by Western blot. (b–j) Littermate control IKKβF/F and IKKαF/F mice and mutant IKKβΔIEC and IKKαΔIEC mice were infected with C. rodentium. (b–d) C. rodentium CFU in the feces on day 5 p.i. (b), spleen on day 11 p.i. (c), and liver on day 11 p.i. (d). (e and f) Percentage of initial body weight (e) and percent survival (f) at the indicated time points p.i. (g) H&E staining of colon tissue sections from naive mice. (h) H&E staining of colon tissue sections from C. rodentium–infected mice at day 11 p.i., including high-magnification insets (bottom). (i) Pathological score of colon histology. (j) H&E staining of liver tissue sections of day 11 infected mice. Arrows indicate neutrophil-rich inflammatory foci. All bars, 50 µm. Data for a are representative of two independent experiments using pooled IECs from three mice. Data for b–j are representative of three to four independent experiments (IKKβF/F, total n = 13; IKKαF/F, n = 18; IKKβΔIEC, n = 12; and IKKαΔIEC mice, n = 16). Data for f are pooled from three independent experiments. Data are shown as mean ± SEM. † indicates infection-induced mortality. *, P < 0.05 compared with IKKαF/F.
Colonic IL-22 and AMP expression are reduced in IKKαΔIEC mice in the steady state and after C. rodentium infection
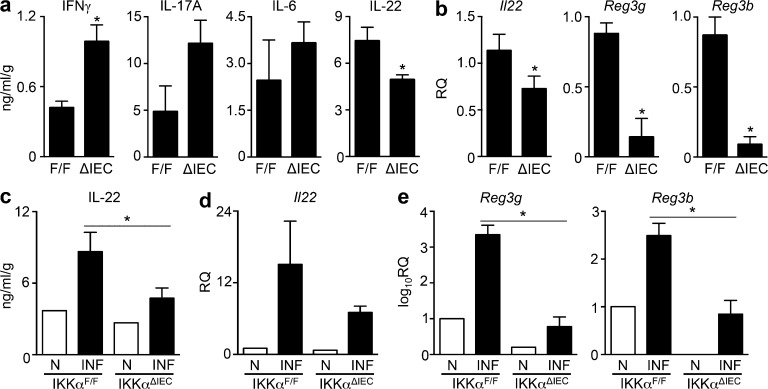
To investigate the mechanisms for dysregulated C. rodentium–induced intestinal inflammation in IKKαΔIEC mice, we first examined the expression levels of key cytokines involved in immunity to C. rodentium. Compared with littermate control IKKαF/F mice, protein levels of the proinflammatory cytokine IFNγ were significantly elevated in the colons of naive IKKαΔIEC mice, whereas expression levels of IL-17A and IL-6 were not significantly different (Fig. 2 a). In contrast, IL-22 protein (Fig. 2 a) and mRNA (Fig. 2 b) expression was significantly reduced in IKKαΔIEC mice in the steady state. This correlated with significant reductions in the mRNA expression levels of the IL-22–dependent AMPs Reg3g and Reg3b in the colon in the absence of IEC-intrinsic IKKα expression (Fig. 2 b). To assess whether the expression of IL-22 and AMPs was compromised after C. rodentium infection, we infected IKKαF/F control and mutant IKKαΔIEC mice with C. rodentium and analyzed mice at day 4 p.i., an early time point where IL-22 responses reach their peak after C. rodentium infection (Zheng et al., 2008; Ota et al., 2011; Sonnenberg et al., 2011b; Manta et al., 2013). Importantly, infection-induced IL-22 protein (Fig. 2 c) and mRNA (Fig. 2 d) expression was reduced in IKKαΔIEC mice, with concurrent significant reductions in Reg3g and Reg3b expression (Fig. 2 e). Together, these data highlight that IEC-intrinsic IKKα expression regulates both steady state and infection-induced IL-22 responses in the colon, suggesting a potential mechanism by which IECs may regulate barrier integrity in the intestine.
Figure 2.
Colonic IL-22 and AMP expression is reduced in IKKαΔIEC mice in the steady state and after C. rodentium infection. (a) IFNγ, IL-17A, IL-6, and IL-22 protein expression in colonic tissue homogenates from naive littermate control IKKαF/F and IKKαΔIEC mice, as measured by ELISA. (b) Il22, Reg3g, and Reg3b mRNA expression in colonic tissue homogenates from naive mice, as measured by RT-PCR. (c–e) IKKαF/F or IKKαΔIEC mice were infected with C. rodentium, and IL-22 protein expression (c) and Il22 mRNA (d) were measured in colonic tissue homogenates of naive (N) or infected (INF) mice at day 4 p.i. (e) Reg3g and Reg3b mRNA expression in colonic tissue homogenates from naive or day 4 C. rodentium–infected mice. Gene expression data in b, d, and e were normalized to naive IKKαF/F mice. Data for a and b are representative of two independent experiments (IKKαF/F, total n = 9; IKKαΔIEC, n = 8). Data for c–e are representative of three independent experiments (IKKαF/F, total n = 15; IKKαΔIEC, n = 14 + 1 naive mouse of each genotype per experiment). Data are expressed as mean ± SEM. *, P < 0.05 compared with IKKαF/F control.
Therapeutic delivery of recombinant IL-22 is sufficient to rescue IKKαΔIEC mice from C. rodentium–induced morbidity
IL-22 is critical for innate immunity to infection with C. rodentium (Zheng et al., 2008; Satoh-Takayama et al., 2008; Kiss et al., 2011; Sonnenberg et al., 2011b; Tumanov et al., 2011). In response to C. rodentium infection, IL-22–deficient mice exhibit rapid weight loss, intestinal barrier breakdown, and impaired control of bacterial dissemination resulting in death (Zheng et al., 2008), a phenotype consistent with C. rodentium–infected IKKαΔIEC mice (Fig. 1). Epithelial cells possess an array of mechanisms by which they can control mucosal immunity, and epithelial IKKα expression may have diverse effects on intestinal immune homeostasis beyond regulating IL-22 responses. To determine whether delivery of exogenous IL-22 was sufficient to restore protective immunity in IKKαΔIEC mice, IKKαΔIEC mice were infected with C. rodentium and treated with either PBS or rIL-22 every other day. Although IKKαΔIEC mice treated with PBS exhibited elevated bacterial titers in the feces at day 6 p.i. (Fig. 3 a) and enhanced bacterial dissemination to the liver at day 12 p.i. (Fig. 3 b) compared with control IKKαF/F mice, rIL-22–treated IKKαΔIEC mice displayed significant reductions in bacterial burdens (Fig. 3, a and b), indicating restoration of host-protective immunity. Consistent with this, although PBS-treated IKKαΔIEC mice underwent significant weight loss and infection-induced mortality, therapeutic administration of rIL-22 to IKKαΔIEC mice rescued mice from infection-induced weight loss and fatal C. rodentium infection (Fig. 3, c and d). Restoration of host-protective immunity correlated with reductions in colonic histopathology at day 12 p.i. (Fig. 3 e), lower colonic pathology score (Fig. 3 f), and reduced neutrophilic infiltrates in the liver at day 12 p.i. in rIL-22–treated IKKαΔIEC mice (Fig. 3 g). These data indicate that delivery of exogenous IL-22 is sufficient to restore antibacterial immunity in mice with IEC-specific deletion of IKKα, suggesting that defective IL-22 responses in IKKαΔIEC mice are a likely cause of C. rodentium–induced morbidity and mortality.
Figure 3.
Therapeutic delivery of recombinant IL-22 is sufficient to rescue IKKαΔIEC mice from C. rodentium–induced morbidity. IKKαΔIEC mice were infected with C. rodentium and injected i.p. with either PBS or 50 µg rIL-22 every 2 d (littermate control IKKαF/F mice received PBS only). (a and b) C. rodentium CFU in the feces on day 5 p.i. (a) and liver on day 12 p.i (b). (c and d) Percentage of initial body weight (c) and percent survival (d) at the indicated time points p.i. Data are pooled from three identical experiments. (e) H&E staining of colon tissue sections of C. rodentium–infected mice at day 12 p.i. (f) Pathological score of colon histology. (g) H&E staining in liver tissue sections of infected mice at day 12 p.i. Arrows indicate neutrophil-rich inflammatory foci. All bars, 50 µm. Data are representative of three independent experiments (IKKαF/F + PBS total n = 14; IKKαΔIEC + PBS, n = 14; IKKαΔIEC + rIL-22, n = 12) and expressed as mean ± SEM. *, P < 0.05. ND, not detected. † indicates infection-induced mortality.
C. rodentium infection–induced ILC-dependent IL-22 responses are diminished in IKKαΔIEC mice
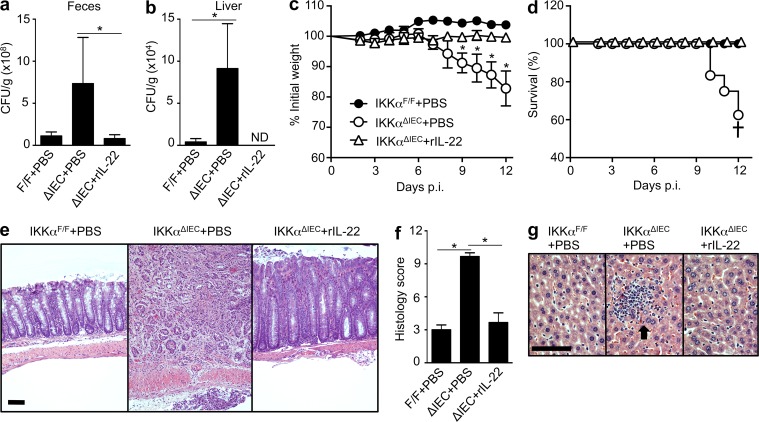
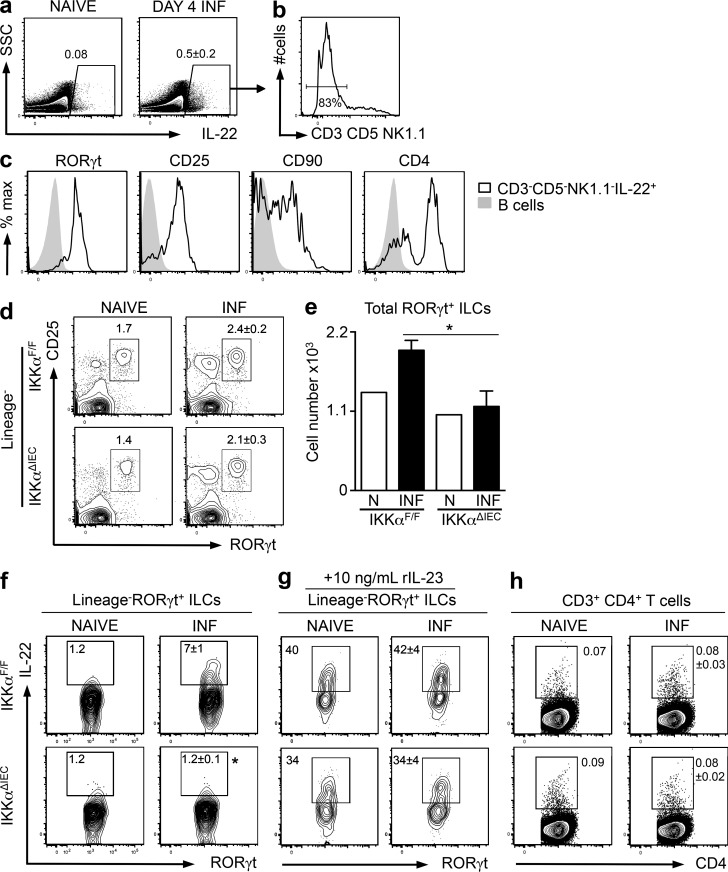
IL-22 can be produced by a variety of immune cells, including T cells, ILCs, neutrophils, and DCs (Zheng et al., 2008; Sonnenberg et al., 2011a; Zindl et al., 2013). However, previous studies have demonstrated that ILC3-dependent IL-22 responses are critical for innate immunity to C. rodentium infection (Sonnenberg et al., 2011b; Manta et al., 2013). Consistent with this, analysis of the predominant IL-22–expressing cells in the early stages of C. rodentium infection (day 4 p.i.) demonstrated that lineage-negative cells were the predominant source of IL-22 in the mesenteric LNs (mLNs) of control IKKαF/F mice (Fig. 4, a and b). Further characterization revealed that IL-22–expressing CD3−CD5−NK1.1− cells expressed RORγt, CD25, CD90, and CD4, a phenotype consistent with that of ILC3s (Fig. 4 c). Analysis of RORγt+ ILC responses (lineage−, RORγt+, CD25+ cells) in the mLNs of naive and day 4 C. rodentium–infected IKKαF/F and IKKαΔIEC mice revealed that although the frequencies of intestinal RORγt+ ILCs were not significantly different (Fig. 4 d), total numbers of RORγt+ ILCs were significantly reduced in C. rodentium–infected IKKαΔIEC mice compared with IKKαF/F control (Fig. 4 e). Strikingly, when RORγt+ ILCs were assessed for their functional capacity to produce IL-22 after PMA and ionomycin stimulation, we observed a significant reduction in infection-induced IL-22 responses in RORγt+ ILCs from IKKαΔIEC mice compared with IKKαF/F littermate controls (Fig. 4 f). Stimulation of cells with rIL-23 ex vivo revealed that RORγt+ ILCs from IKKαΔIEC mice were functionally capable of producing IL-22 if provided with adequate exogenous stimuli, and although the frequency of IL-22–producing ILC3s tended to be lower in rIL-23–stimulated cultures of IKKαΔIEC cells than cells from IKKαF/F mice (Fig. 4 g), these differences did not reach statistical significance. Importantly, frequencies of CD4+ T cells expressing IL-22 were not significantly altered in IKKαΔIEC mice (Fig. 4 h), indicating that IKKα-dependent regulation of IL-22 expression may be selective for ILCs. Collectively, these data indicate that IEC-intrinsic IKKα expression is necessary for optimal C. rodentium infection–induced ILC3-dependent IL-22 responses.
Figure 4.
C. rodentium infection–induced ILC-dependent IL-22 responses are diminished in IKKαΔIEC mice. IKKαF/F mice were infected (INF) with C. rodentium and sacrificed at day 4 p.i. (a) Representative plots displaying frequencies of IL-22+ cells in the mLNs. (b) Expression of T cell (CD3 and CD5) and NK cell (NK1.1) markers among IL-22+ cells. (c) Expression of ILC surface markers in gated CD3−CD5−NK1.1−IL-22+ cells (black, open histograms) compared with CD19+ B cells (gray, closed histograms). (d) Representative plots displaying frequencies of CD3−CD5−CD19−CD11c−NK1.1−, RORγt+CD25+ ILCs in the mLNs of naive and C. rodentium–infected littermate control IKKαF/F and IKKαΔIEC mice. (e) Total mLN ILC3s. (f) Frequencies of IL-22–expressing RORγt+ ILCs in the mLN after ex vivo PMA and ionomycin stimulation. (g) Frequencies of IL-22–expressing RORγt+ ILCs in the mLNs after stimulation with rIL-23, PMA, and ionomycin. (h) Frequencies of CD3+CD4+ T cells in the mLNs expressing IL-22 after ex vivo PMA and ionomycin stimulation. Data for a–f and h are representative of five experiments (IKKαF/F, total n = 21; IKKαΔIEC, n = 17 + 1 naive mouse of each genotype per experiment), and data for g are representative of three experiments (IKKαF/F, total n = 13; IKKαΔIEC, n = 11 + 1 naive mouse of each genotype per experiment). Data are expressed as mean ± SEM. *, P < 0.05 compared with IKKαF/F INF.
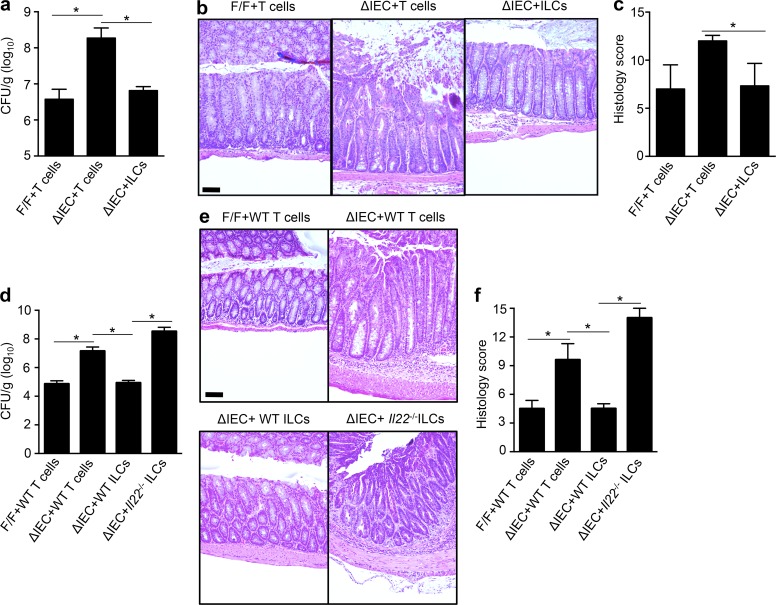
Delivery of sort-purified IL-22–competent ILCs restores immunity to C. rodentium infection in IKKαΔIEC mice
Although RORγt+ ILCs are the primary source of IL-22 in response to C. rodentium infection (Fig. 4, b and c), cells other than ILCs may contribute to IL-22–mediated immunity to C. rodentium. Therefore, we next assessed whether transfer of ILCs alone could restore immunity to C. rodentium infection in IKKαΔIEC mice. To do so, ILCs (lineage−CD90+CD25+CD127+) or T cells (CD3+CD90+) were sort purified from naive littermate control IKKαF/F mice and pulsed for 1 h ex vivo with rIL-23, rIL-1β, rIL-2, and rIL-7 to promote survival and cytokine production before adoptive transfer into recipient IKKαF/F or IKKαΔIEC mice. Although IKKαΔIEC mice that received T cells exhibited elevated bacterial titers in the feces at day 12 p.i. (Fig. 5 a) and exacerbated colonic inflammation and histology score compared with IKKαF/F control mice (Fig. 5, b and c), IKKαΔIEC mice that received cytokine-activated ILCs displayed significantly reduced bacterial burdens (Fig. 5 a) and improved intestinal pathology and colonic histology score at day 12 p.i. (Fig. 5, b and c), indicating that ILCs were more potent at restoring antibacterial immunity than T cells. To examine the cell-intrinsic mechanism by which ILCs confer protection against C. rodentium infection, analogous experiments were performed where recipient IKKαF/F or IKKαΔIEC mice were injected with either sort-purified ILCs or T cells from C57BL/6 WT mice or ILCs from C57BL/6 Il22−/− mice. Although IL-22–competent T cells were unable to confer protection against C. rodentium infection in IKKαΔIEC mice, transfer of IL-22–competent ILCs reduced fecal bacterial titers (Fig. 5 d) and intestinal pathology (Fig. 5, e and f) in IKKαΔIEC mice. Critically, Il22−/− ILCs were unable to confer similar protection (Fig. 5, d–f). Collectively, these data indicate that the provision of IL-22–competent ILCs is sufficient to restore immunity to C. rodentium infection in IKKαΔIEC mice, providing further evidence that defective ILC3–IL-22 responses are a likely cause of C. rodentium–induced immunopathology in IKKαΔIEC mice.
Figure 5.
Delivery of sort-purified IL-22–competent ILCs restores immunity to C. rodentium infection in IKKαΔIEC mice. (a–c) IKKαΔIEC mice were infected with C. rodentium and injected i.v. with either 104 sort-purified CD90+CD3+ T cells or 104 sort-purified lineage−CD90+CD25+CD127+ ILCs from IKKαF/F mice on days 0, 2, 4, and 7 p.i. (littermate control IKKαF/F mice received T cells only). T cells and ILCs were pulsed with rIL-23, rIL-1β, rIL-2, and rIL-7 for 1 h before injection. (a) C. rodentium CFU in the feces on day 6 p.i. (b) H&E staining of colon tissue sections at day 12 p.i. (c) Pathological score of colon histology. (d–f) Littermate IKKαF/F and IKKαΔIEC mice were infected with C. rodentium and injected i.v. with either 104 sort-purified T cells or 104 sort-purified ILCs (gating strategies as per a–c) from either C57BL/6 WT or C57BL/6 Il22−/− mice on days 0, 2, 4, and 7 p.i. (d) C. rodentium CFU in the feces on d 6 p.i. (e) H&E staining of colon tissue sections at day 12 p.i. All bars, 50 µm. (f) Pathological score of colon histology. Data for a–c are representative of two independent experiments (IKKαF/F + T cells, n = 8; IKKαΔIEC + T cells, n = 8; IKKαΔIEC + ILCs, n = 6). Data for d–f are representative of two experiments (IKKαF/F + WT T cells, n = 7; IKKαΔIEC + WT T cells, n = 7; IKKαΔIEC + WT ILCs, n = 6; IKKαΔIEC + IL-22−/− ILCs, n = 6). Data are expressed as mean ± SEM. *, P < 0.05.
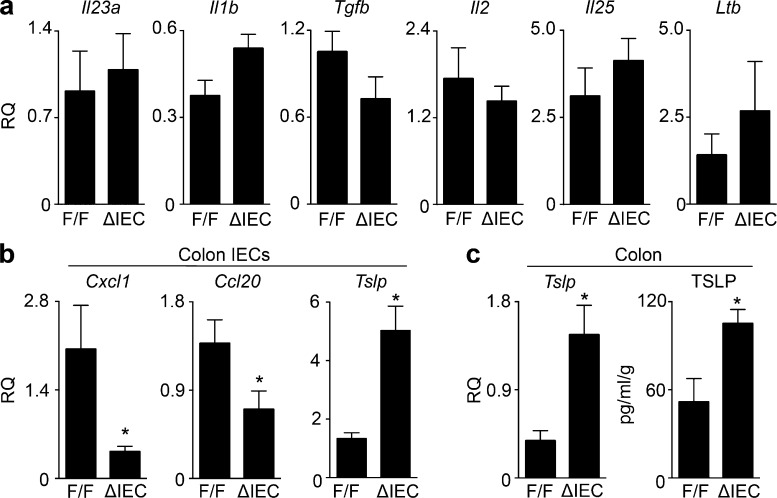
IKKαΔIEC mice exhibit dysregulated TSLP expression by colonic IECs
We next assessed the mechanisms by which IKKα expression within IECs regulates IL-22 production by ILC3. Production of IL-22 by intestinal ILCs is promoted by IL-23, IL-1β, IL-2, LTα1β2, and Ahr ligands (Cella et al., 2009; Hughes et al., 2010; Kiss et al., 2011; Reynders et al., 2011; Kinnebrew et al., 2012; Lee et al., 2012), whereas IEC-derived IL-25 is a negative regulator of ILC responses in the intestine (Sawa et al., 2011). Analysis of cytokine expression in whole colonic tissue isolated from day 4 C. rodentium–infected IKKαΔIEC versus littermate control IKKαF/F mice revealed no significant differences in expression of Il23a, Il1b, Tgfb, Il2, Il25, or Ltb mRNA (Fig. 6 a). Colonic IECs were isolated, and as expected, gene expression of the LTβR-dependent chemokines Cxcl1 and Ccl20 were significantly diminished in IECs from IKKαΔIEC mice (Fig. 6 b), given that LTβR signals through the noncanonical NFκB pathway (Matsushima et al., 2001; Dejardin et al., 2002). Notably, analysis of other IEC-intrinsic factors that may regulate ILC function revealed elevated expression of TSLP mRNA (Fig. 6 b) that correlated with significantly increased Tslp mRNA and TSLP protein levels in whole colonic tissue homogenates (Fig. 6 c).
Figure 6.
IKKαΔIEC mice exhibit dysregulated TSLP expression by colonic IECs. (a–c) Littermate IKKαF/F and IKKαΔIEC mice were infected with C. rodentium and sacrificed at day 4 p.i. (a) Relative mRNA expression of Il23a, Il1b, Tgfb, Il2, Il25, and Ltb in colon tissue homogenates. (b) Relative Cxcl1, Ccl20, and Tslp mRNA expression levels in colonic IECs. (c) Tslp mRNA and TSLP protein levels in colonic tissue homogenates. Gene expression data were normalized to naive IKKαF/F mice. Data for a and c are representative of three independent experiments (IKKαF/F, total n = 15; IKKαΔIEC, n = 14). Data for b is representative of two experiments (IKKαF/F, total n = 10; IKKαΔIEC, n = 8). Data are expressed as mean ± SEM. *, P < 0.05.
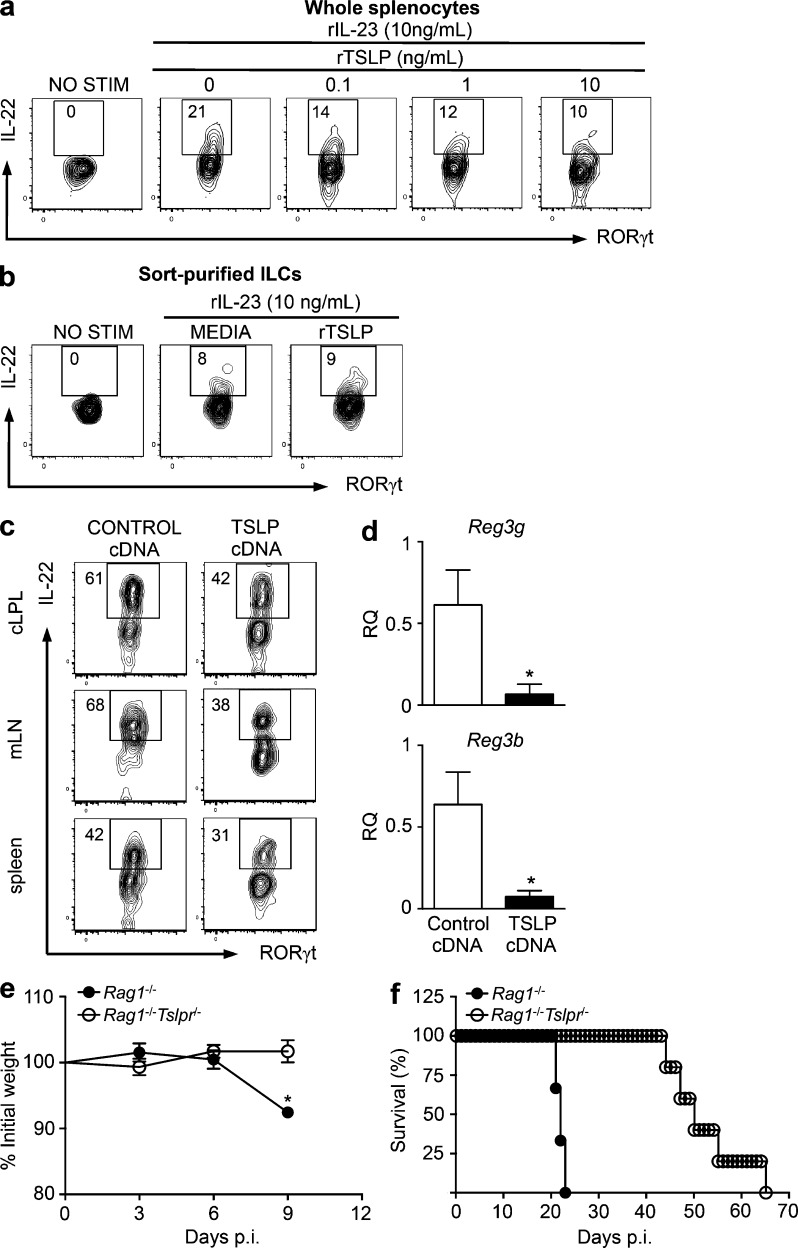
TSLP acts as a negative regulator of ILC-derived IL-22 production
Although TSLP has been shown to regulate the function of ILC2s (Mjösberg et al., 2012; Kim et al., 2013), a role for TSLP in influencing other ILC subsets has not been described. To assess whether TSLP regulates ILC3 function, we cultured splenocytes from WT C57BL/6 mice overnight with various concentrations of rTSLP, followed by 3-h stimulation with rIL-23, and examined IL-22 expression. Critically, although rIL-23 induced potent IL-22 expression in RORγt+ ILCs in the absence of TSLP, addition of rTSLP to splenocyte cultures limited IL-22 expression by ILCs in a dose-dependent manner (Fig. 7 a), suggesting that TSLP is a negative regulator of IL-22 production by ILCs. To assess whether TSLP acts directly on ILCs to regulate IL-22 production, we sort purified splenic lineage−CD90+CD127+ cells from C57BL/6 Rag1−/− mice and cultured cells overnight with various concentrations of rTSLP, followed by 3-h stimulation with rIL-23, and examined IL-22 expression. Notably, rIL-23 was able to induce equivalent IL-22 production in ILCs in the presence or absence of rTSLP, suggesting that the ability of TSLP to inhibit IL-22 production is indirect (Fig. 7 b). Next, we examined whether TSLP could regulate ILC–IL-22 responses in vivo. Hydrodynamic tail vein injection with gene-encoding plasmids has been used to induce protein overexpression in several settings (Sebestyén et al., 2006). Here, we treated C57BL/6 WT mice with either a control or TSLP overexpressing cDNA plasmid (as we have previously reported [Siracusa et al., 2011, 2013; Kim et al., 2013; Noti et al., 2014]), which has been shown to elevate circulating TSLP levels (Iseki et al., 2012), and examined IL-22 expression in ILCs 9 d later. Consistent with our in vitro findings using rIL-23 stimulation, TSLP overexpression led to diminished IL-22 production by RORγt+ ILCs isolated from the colonic lamina propria lymphocytes (cLPLs), mLNs, and spleen (Fig. 7 c), corresponding with significantly reduced expression levels of colonic Reg3g and Reg3b (Fig. 7 d). We next performed loss of function experiments to examine whether TSLP regulates innate immunity to C. rodentium. C57BL/6 Rag1−/− mice are highly susceptible to C. rodentium infection; however, IL-22 from ILCs does contribute to innate immunity (Zheng et al., 2008; Sonnenberg et al., 2011b). Although C57BL/6 Rag1−/− mice exhibited significant weight loss (Fig. 7 e) and succumbed to C. rodentium infection by days 20–22 p.i. (Fig. 7 f), C57BL/6 Rag1−/− mice deficient in TSLP responsiveness (Rag1−/−Tslpr−/− mice) lost less weight, and this correlated with prolonged survival, only succumbing to infection between days 45 and 65 p.i. (Fig. 7, e and f). Collectively, these data suggest that TSLP negatively regulates innate immunity to C. rodentium, potentially via regulation of the ILC3–IL-22 axis.
Figure 7.
TSLP acts as a negative regulator of ILC-derived IL-22 production. (a) C57BL/6 WT mouse splenocytes were cultured overnight in the presence of increasing doses of rTSLP and stimulated for 3 h with rIL-23 or were left unstimulated (NO STIM), and intracellular IL-22 expression was assessed in lineage−RORγt+CD90+ ILC populations. (b) ILCs were sort purified from C57BL/6 Rag1−/− mice and cultured overnight in the presence of rTSLP, followed by 3-h stimulation with rIL-23 or medium (NO STIM), and intracellular IL-22 expression was assessed. (c and d) WT C57BL/6 mice were injected with either a control cDNA plasmid or a TSLP-overexpressing cDNA plasmid for 9 d, and (c) IL-22 production by RORγt+ ILCs in the cLPLs, mLNs, and spleen was assessed after 3-h stimulation with rIL-23 in the presence of brefeldin A. (d) Reg3g and Reg3b mRNA expression in colonic tissue homogenates. (e and f) C57BL/6 Rag1−/− or double mutant Rag1−/−Tslpr−/− mice were infected with C. rodentium. Percentage of initial body weight (e) and percent survival (f) at the indicated time points p.i. Data for a and b are representative of two independent experiments (total n = 6/treatment), data for c and d are representative of two experiments (total n = 6/group), and data for e and f are representative of two experiments (Rag1−/−, n = 10; Rag1−/−Tslpr−/−, n = 8). Data are expressed as mean ± SEM. *, P < 0.05.
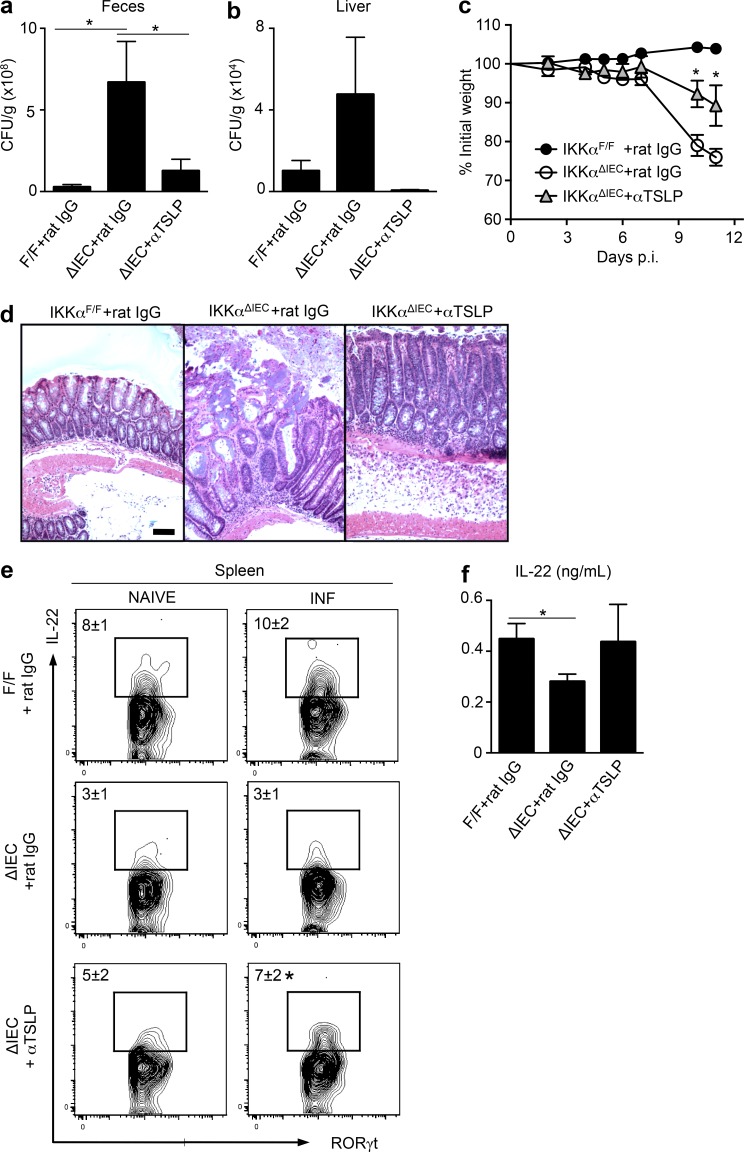
Neutralization of TSLP partially restores immunity to C. rodentium infection in IKKαΔIEC mice
To directly assess whether overexpression of TSLP in IKKαΔIEC mice is responsible for impaired immunity to C. rodentium infection, we treated IKKαΔIEC mice every 3 d p.i. with either a neutralizing anti-TSLP mAb or a control rat IgG. Littermate control IKKαF/F mice received rat IgG only. Critically, although IKKαΔIEC mice treated with rat IgG displayed increased C. rodentium CFU in the feces at day 6 p.i. (Fig. 8 a) and liver at day 11 p.i. (Fig. 8 b) compared with IKKαF/F mice, IKKαΔIEC mice treated with anti-TSLP mAb exhibited substantially reduced bacterial titers (Fig. 8, a and b). TSLP neutralization also partially protected IKKαΔIEC mice from infection-induced weight loss (Fig. 8 c) and diminished colonic pathology (Fig. 8 d). Importantly, antibody (Ab)-mediated neutralization of TSLP in IKKαΔIEC mice increased IL-22 production by splenic ILC3 at day 4 p.i. (Fig. 8 e) and restored IL-22 production in the colon to levels observed in IKKαF/F mice (Fig. 8 f). These data demonstrate that dysregulated TSLP expression in the absence of IEC-intrinsic IKKα expression is a potential mechanism by which ILC-dependent innate immunity to C. rodentium is impaired in IKKαΔIEC mice.
Figure 8.
Neutralization of TSLP partially restores immunity to C. rodentium infection in IKKαΔIEC mice. IKKαΔIEC mice were infected with C. rodentium and injected i.p. with either 0.5 mg rat IgG control or anti-TSLP mAb every 3 d (littermate control IKKαF/F mice received rat IgG only). (a and c) C. rodentium CFU in the feces on day 6 p.i. (a) and liver on day 11 p.i. (b). (c) Percentage of initial body weight. (d) H&E staining of colon tissue sections of day 11 C. rodentium–infected mice. Bar, 50 µm. (e) IL-22 expression by splenic ILCs at day 4 p.i., after ex vivo PMA and ionomycin stimulation. (f) IL-22 protein expression within colon homogenate tissue from day 4 infected mice. Data for a–d are representative of three experiments (IKKαF/F + rat IgG, n = 13; IKKαΔIEC + rat IgG, n = 10; IKKαΔIEC + anti-TSLP, n = 9), and data for e and f are representative of two experiments (IKKαF/F + rat IgG, n = 8; IKKαΔIEC + rat IgG, n = 6; IKKαΔIEC + anti-TSLP, n = 6). Data are expressed as mean ± SEM. *, P < 0.05 compared with IKKαΔIEC + rat IgG.
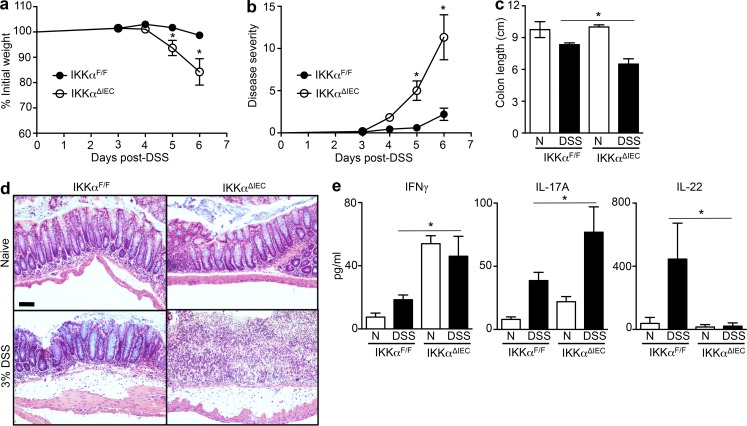
IEC-intrinsic IKKα expression regulates inflammation during chemically induced intestinal damage
To assess whether IKKα expression within IECs is protective in other models of intestinal inflammation, we examined the susceptibility of IKKαF/F mice and IKKαΔIEC mice to dextran sodium sulfate (DSS)–induced colitis. Inclusion of 3% DSS in the drinking water of control IKKαF/F mice caused only modest weight loss, increased disease severity score, and colon shortening (Fig. 9, a–c) compared with mice that received normal drinking water (naive). However, IKKαΔIEC mice experienced rapid weight loss from day 5 after DSS feeding (Fig. 9 a) and had to be sacrificed by day 6 because of escalating disease severity (Fig. 9 b). IKKαΔIEC mice displayed exacerbated colonic shortening (Fig. 9 c) and markedly increased colonic immunopathology compared with IKKαF/F littermate controls (Fig. 9 d). In line with increased pathology in IKKαΔIEC DSS-treated mice, levels of the proinflammatory cytokines IFNγ and IL-17A were elevated in IKKαΔIEC mice at day 4 after DSS treatment (Fig. 9 e). Consistent with what was observed after C. rodentium infection, IL-22 protein levels were significantly reduced in the colon of DSS-treated IKKαΔIEC mice compared with littermate IKKαF/F controls (Fig. 9 e). In conclusion, IEC-intrinsic IKKα expression can limit inflammation in experimental models of infection-induced colitis and chemical-induced intestinal inflammation.
Figure 9.
IEC-intrinsic IKKα expression regulates inflammation and pathology during chemically induced colitis. Littermate IKKαF/F and IKKαΔIEC mice were treated with either 3% DSS in the drinking water or maintained on normal drinking water (naive, N). (a) Percentage of original body weight. (b) Gross disease score. (c) Colon length at day 6 after DSS. (d) H&E staining of colon tissue sections of naive and DSS-treated mice at day 6 after DSS. Bar, 50 µm. (e) IFNγ, IL-17A, and IL-22 protein expression in overnight colonic organ culture supernatants at day 4 after DSS. Data for a–d are representative of three independent experiments (IKKαF/F, n = 17; IKKαΔIEC, n = 14 + 2 naive of each genotype per experiment). Data for e are representative of two independent experiments (IKKαF/F, n = 8; IKKαΔIEC, n = 8 + 2 naive of each genotype per experiment). Data are expressed as mean ± SEM. *, P < 0.05 compared with IKKαF/F + DSS.
DISCUSSION
RORγt+ ILCs are central for regulation of immunity and barrier function in the intestine by promoting secondary lymphoid structure formation (Kiss et al., 2011), preventing bacterial dissemination (Sonnenberg et al., 2012), controlling immune responses to commensal microbes (Hepworth et al., 2013, 2015), and regulating epithelial cell homeostasis in health and disease (Ota et al., 2011; Sawa et al., 2011; Sonnenberg et al., 2011b; Hanash et al., 2012; Qiu et al., 2012; Kirchberger et al., 2013; Goto et al., 2014). Although several studies have identified some of the transcription factors, microbial factors, and cytokines involved in the development and function of ILC3s (Cording et al., 2014), the cellular and molecular network involved in regulation of ILC3s remains incompletely defined. The present study identifies a previously unappreciated pathway by which IECs selectively regulate ILC3 function via IKKα expression. Ablation of IKKα, but not IKKβ, expression within IECs led to impaired antibacterial immunity and compromised intestinal barrier function that was associated with defective IL-22 production by ILC3s. Immunity to C. rodentium could be restored by therapeutic administration with rIL-22 or with ILCs from IL-22–competent mice that had been pre-primed for IL-22 production. Absence of IKKα expression by IECs led to the overexpression of TSLP, a cytokine that we demonstrate can suppress ILC3-derived IL-22 production in vitro and inhibit innate immunity to C. rodentium infection in vivo. Together, these findings highlight a previously unrecognized mechanism of immune–epithelial cell dialogue that regulates intestinal barrier homeostasis, tissue protection, and antimicrobial ILC3 responses.
The NFκB signaling pathway is fundamental for regulation of IEC function, and although absence of individual IKKα and IKKβ subunits does not result in spontaneous inflammation (Nenci et al., 2007), IEC-intrinsic IKKβ expression is critical for limiting intestinal inflammation in chemically induced models of colitis (Eckmann et al., 2008), ischemia-reperfusion injury (Chen et al., 2003), and helminth infection (Zaph et al., 2007). Furthermore, overexpression of IKKβ within IECs results in uncontrolled epithelial proliferation and intestinal tumorigenesis (Guma et al., 2011; Vlantis et al., 2011). In the present study, we identify a critical role for IKKα-mediated signaling pathways in regulating C. rodentium–induced colitis and demonstrate that IKKβ is dispensable, representing the first demonstration of a differential requirement for IKKβ- versus IKKα-dependent gene expression on IEC function. Furthermore, our findings are consistent with a previous study demonstrating that hyperactivation of the noncanonical NFκB pathway is associated with elevated immunity to C. rodentium (Hu et al., 2013), suggesting a pivotal role for IKKα-dependent signaling in immunity to bacterial infection.
IKKα-dependent noncanonical NFκB activation is associated with LTβR signaling (Schneider et al., 2004), and LTβR is a critical regulator of intestinal ILC-dependent IL-22 responses (Ota et al., 2011; Tumanov et al., 2011; Macho-Fernandez et al., 2015). Furthermore, mice with IEC-specific deletions in LTβR are highly susceptible to C. rodentium infection (Wang et al., 2010). Together, these data indicate a potential role for impaired LTβR signaling contributing to a reduction in host-protective immunity to C. rodentium in IKKαΔIEC mice. However, LT-mediated regulation of ILCs was primarily mediated through DCs, and the impact of IEC-specific LTβR deletion on ILCs and IL-22 was not assessed (Wang et al., 2010). We did observe significant reductions in expression of the LTβR-dependent genes Cxcl1 and Ccl20 in IECs recovered from IKKαΔIEC mice; hence it remains plausible that defective LTβR signaling may contribute to impaired IL-22 responses in the absence of IEC-intrinsic IKKα expression. This is consistent with a recent study showing that IEC-intrinsic LTβR expression regulates IL-22–dependent intestinal immune homeostasis during chemically induced colitis (Macho-Fernandez et al., 2015). Notably, despite impaired LTβR-dependent gene expression in IKKαΔIEC mice, we did not observe reductions in the presence of intestinal lymphoid tissues such as Peyer’s patches (PPs) or isolated lymphoid follicles in IKKαΔIEC mice (unpublished data), suggesting that in this context, other LTβ-responsive cells may have coordinated lymphoid organogenesis.
IL-22 production by ILC3s can be stimulated by several factors, chiefly IL-23 and IL-1β, but expression of these cytokines was not altered in IKKαΔIEC mice. In addition to factors that positively regulate ILC3 function, commensal bacteria–dependent expression of IL-25 has been reported to suppress ILC3 responses (Sawa et al., 2011). Although we did not observe significant increases in IL-25 in IKKαΔIEC mice, expression of the predominately IEC-derived cytokine TSLP was exaggerated in these mice. We demonstrate that exogenous TSLP suppressed IL-22 production by RORγt+ ILC3s in vitro and in vivo and that Ab-mediated neutralization of TSLP could partially restore innate immunity to C. rodentium infection in IKKαΔIEC mice. These data indicate that in addition to IL-25, TSLP acts as a negative regulator of ILC3 function in the context of bacterial-driven intestinal inflammation. Further studies are needed to illuminate whether additional IEC-dependent mechanisms, such as growth factors or the intestinal microbiota, may regulate ILC3 location, accumulation, or function.
Previous studies have demonstrated interactions between TSLP and ILC2s (Mjösberg et al., 2012; Kim et al., 2013) and that TSLPR signaling is dispensable for ILC3 development (Vonarbourg et al., 2010). How TSLP regulates IL-22 production by ILC3s remains unclear, but our data suggest that TSLP acts indirectly on ILCs to exert its function, possibly via an accessory TSLP-responsive cell such as a DC. It is becoming increasingly evident that TSLP has diverse cellular targets and biological functions, where TSLP may play both tissue-protective roles in the intestine (e.g., regulation of DC, ILC2, and granulocyte function; Ziegler et al., 2013), as well as nonprotective functions as illustrated in the current study. Thus, it remains possible that the protective effects we observed after TSLP neutralization during C. rodentium infection may be distinct from what would occur in DSS colitis where blocking TSLP–TSLPR interactions has been shown to exacerbate disease (Taylor et al., 2009; Reardon et al., 2011). Furthermore, it is unknown how and why TSLP expression by IECs is dysregulated in the absence of IKKα signaling. Given that TSLP is an IKKβ-dependent gene product (Lee and Ziegler, 2007; Zaph et al., 2007) and that the absence of IKKα and IKKβ can induce compensatory increases in canonical and noncanonical NFκB activation, respectively (Lawrence et al., 2005; Lam et al., 2008), it is possible that the elevated TSLP production in IKKαΔIEC mice is a result of increased IKKβ-dependent canonical NFκB activation. Indeed, we did observe increased expression of activated phospho-IKKβ/IKKα (Ser176/177) in colonic IECs from IKKαΔIEC mice compared with IKKαF/F mice (unpublished data), although it remains unclear whether this is sufficient to account for increased TSLP production.
Although deletion of IKKα and IKKβ within IECs does not cause spontaneous colitis (Nenci et al., 2007), the present study highlights multiple steady state defects in intestinal immune responses in IKKαΔIEC mice. Absence of IEC-intrinsic IKKα signaling led to increases in basal IFNγ expression in the intestine, with concurrent reductions in IL-22 and AMP expression. It is also possible that IEC-intrinsic NFκB signaling regulates the composition of the intestinal microbiota, which may have substantial impacts on inflammatory responses, but future studies will be required to investigate the interplay between immune responses and the microbiota in IKKαΔIEC mice. Thus, although IEC-specific deletion of IKKα signaling does not cause evident pathology in the steady state, developmental defects in these animals likely contributed to impaired immunity to infection, as well as increased susceptibility to chemically induced colitis. Further studies comparing the relative roles for IEC-intrinsic IKKα and IKKβ signaling in a variety of other infectious or inflammatory experimental models, potentially making use of inducible Cre-lox technology that could minimize the impact of altered immune development in constitutive ΔIEC mice, will contribute to our understanding of epithelial regulation of host-protective immunity and inflammation. In addition, given the multifaceted functions of IKKα in cell biology (Chariot, 2009), it remains possible that the ability of IKKα to regulate ILC3-dependent mucosal immunity may be independent of its ability to regulate noncanonical NFκB activation.
Collectively, these data identify a previously unrecognized pathway in which tissue-resident IECs selectively regulate the function of ILC3s in an IKKα-dependent fashion, thereby simultaneously promoting antibacterial immunity and maintenance of intestinal immune homeostasis. Elevated NFκB activation is associated with IBDs in humans, and NFκB inhibition therapies have been designed to treat multiple intestinal inflammatory diseases (Atreya et al., 2008). However, NFκB activation can have diverse effects within different cell lineages (Greten et al., 2007; Hsu et al., 2011), and humans carrying mutations in NFκB-related factors such as NOD1 or NOD2 develop intestinal inflammation (Strober et al., 2006). The present study and a previous one (Greten et al., 2007), demonstrate that some factors within the NFκB signaling pathway are critical for limiting intestinal inflammation, suggesting that more specific targeted therapies may be required for the design of optimal therapeutics. This, coupled with studies of dysregulated ILC responses in lesions isolated from IBD patients (Geremia et al., 2011; Bernink et al., 2013; Hepworth et al., 2015), indicates that targeted manipulation of the IEC–ILC axis could be beneficial for the treatment of chronic intestinal inflammatory disorders.
MATERIALS AND METHODS
Animals, cell isolations, and treatments.
IKKαF/F (Liu et al., 2008) and IKKβF/F (Pasparakis et al., 2002) mice used in this study were on a mixed genetic background and crossed with C57BL/6 villin-Cre mice (Pasparakis et al., 2002) to generate littermate controls and IKKαΔIEC and IKKβΔIEC mouse strains as described previously (Greten et al., 2004; Nenci et al., 2007). Mice were bred at the University of Pennsylvania or Weill Cornell Medical College and maintained in a specific pathogen–free environment. Male or female mice between the ages of 6 and 14 wk were used. Only cohoused littermate controls were used in experiments with F/F and ΔIEC mice. In some other experiments, C57BL/6 wild-type mice were used and obtained from the Jackson Laboratory. C57BL/6 Il22−/−, Rag1−/−, and Tslpr−/− mice were bred in-house. Experiments were terminated when mice lost a significant proportion of their original weight (>20%); however, mice that succumbed to infection died naturally. All experiments were performed according to guidelines of the Cornell University or University of Pennsylvania Institutional Animal Care and Use Committee–approved protocols. At necropsy, single cell suspensions of mLNs or PPs were prepared by passing through 70-µm nylon mesh filters. Splenocytes were isolated by homogenization followed by red blood cell lysis. IECs were isolated by thoroughly washing colon tissue in PBS and incubating for 10 min at 37°C with 5 ml of a 5 mM EDTA in PBS solution, shaking. The epithelial layer was then removed and passed through a 70-µm cell strainer. cLPLs were isolated as previously described (Zaph et al., 2007). Recombinant IL-22 (Pfizer), 50 µg/mouse in PBS, was injected i.p. into mice on days 0, 2, 4, 6, 8, and 10 after C. rodentium infection. Mice were injected i.v. by hydrodynamic tail vein injection with 10 µg control or TSLP encoding cDNA plasmid (Siracusa et al., 2011, 2013; Iseki et al., 2012; Kim et al., 2013; Noti et al., 2014). Previous studies have demonstrated that hydrodynamic injections with similar cDNA constructs have resulted in incorporation and gene expression primarily within hepatocytes (Yang et al., 2001; Sebestyén et al., 2006; Suda and Liu, 2007). Mice were treated with neutralizing mAb against mouse TSLP (Amgen) by i.p. injection with 0.5 mg Ab 4 h before infection and every 3 d p.i. Control mice received equivalent amounts of rat IgG.
Adoptive transfer of sort-purified ILCs.
ILCs (CD3−CD19−CD11c−NK1.1−CD90+CD127+CD25+) were sort purified from the spleen, PPs, and mLNs of naive IKKαF/F, C57BL/6 WT, or C57BL/6 Il22−/− mice using a FACSAria III sorter (BD). T cells (CD3+CD90+) were simultaneously sorted as a control cell population. Sorted ILCs and T cells were incubated for 1 h at 37°C with 10 ng/ml rIL-7, 10 ng/ml rIL-2, 10 ng/ml rIL-23, and 10 ng/ml rIL-1β (R&D Systems) to support cell viability and optimal IL-22 production before i.v. transfer into recipient IKKαΔIEC or IKKαF/F mice on days 0, 2, 4, and 7 after C. rodentium infection.
C. rodentium infection and assessment of CFU.
C. rodentium strain DBS100 (provided by B. Vallance, University of British Columbia, Vancouver, British Columbia, Canada) was prepared by selection of a single colony and culturing in LB broth overnight. Mice were inoculated with ∼1010 CFU in 200 µl by oral gavage. Analysis of CFU from overnight cultures or mechanically homogenized fecal pellets, livers, and spleens was determined via serial dilutions on MacConkey agar.
C. rodentium histological analyses and histopathological scoring.
Distal colon and liver were fixed in 4% PFA and embedded in paraffin, and 5-µm sections were stained with hematoxylin and eosin (H&E). For histological scoring, colonic tissue sections were blindly graded on a scale of 0–5 for each of the following parameters: (a) epithelial lesions (crypt elongation, hyperplasia, erosion, and ulceration/necrosis), (b) mural inflammation, and (c) edema for an overall maximal total histology score of 15.
Flow cytometry.
Single cell suspensions were stained with anti–mouse fluorochrome-conjugated mAbs against CD3e (145-2C11), CD4 (RM4-5), CD5 (53-7.3), CD11c (N418), CD19 (1D3), CD25 (PC61.5), CD90.2 (30-H12), CD127 (A7R34), and NK1.1 (PK136). Intranuclear RORγt staining was performed using a commercial kit (clone B2D; eBioscience). For intracellular IL-22 staining, cells were stimulated for 4 h with 50 ng/ml PMA and 750 ng/ml ionomycin in the presence of 10 µg/ml brefeldin A (Sigma-Aldrich), stained with cell surface Abs, fixed and permeabilized using a commercial kit (eBioscience), and stained with fluorochrome-labeled anti–IL-22 (IL22-02; Pfizer). Cells were analyzed by flow cytometry using an LSRII (BD), and further analysis was performed using FlowJo software (Tree Star).
Analysis of IKKα and IKKβ expression.
Whole cell extracts from IECs of naive mice were analyzed by SDS-PAGE, followed by immunoblotting with anti-IKKβ Ab (2684; Cell Signaling Technology), anti-IKKα Ab (14A231; EMD Millipore), or control tubulin Ab (T5168; Sigma-Aldrich).
RNA isolations and RT-PCR.
Colon tissue was homogenized in TRIzol using a TissueLyser (QIAGEN), and RNA was isolated by phenol chloroform extraction and isopropanol precipitation. cDNA was generated per standard protocol with Superscript II reverse transcription (Invitrogen) and used as input for RT-PCR using commercially available primer assays (QIAGEN), including Il22, Reg3g, Reg3b, IL23a, IL1b, Tgfb, Il2, Il25, Ltb, Cxcl1, Ccl20, and Tslp. Data were analyzed using the ΔΔCT method whereby β-actin served as the endogenous gene, and samples were normalized to naive controls. All reactions were run on an ABI 7500 Fast Real-Time PCR System (Applied Biosystems).
In vitro cell stimulations.
Whole splenocytes or sort-purified lineage−CD90+CD25+ ILCs from WT or Rag1−/− C57BL/6 mice were cultured overnight with 0, 0.1, 1, or 10 ng/ml rTSLP (Amgen) and stimulated with complete media only (RPMI 1640 containing 10% FBS, 100 U/ml penicillin, 100 µg/ml streptomycin, 2 mg/ml l-glutamine, 25 mM Hepes, and 5 × 10−5 M 2-ME) or complete media supplemented with 10 ng/ml recombinant murine IL-23 (eBioscience) for 3 h in the presence of 10 µg/ml brefeldin A, and intracellular IL-22 expression in lineage−CD90+RORγt+ cells was assessed as described in the section Flow cytometry.
ELISA.
For tissue homogenates, 1 cm of colonic tissue was mechanically homogenized in 0.5 ml PBS using a TissueLyser (QIAGEN). For organ cultures, 1 cm of colonic tissue was opened longitudinally and cultured overnight in complete media. Cell-free supernatants were analyzed for IL-22 using IL22-01 (Pfizer) as a capture Ab and biotin-conjugated IL22-03 (Pfizer) as a detection Ab. Cell-free supernatants were analyzed for IFNγ, IL-17A, IL-6 (all from eBioscience), and TSLP (R&D Systems) using standard techniques.
DSS-induced colitis and clinical disease scoring.
DSS (MP Biomedicals) was added to drinking water at 3% wt/vol. Mice were weighed regularly, and disease severity was scored as follows: (a) weight loss (no change = 0; <5% = 1; 6–10% = 2; 11–20% = 3; >20% = 4), (b) feces (normal = 0; pasty, semiformed = 2; liquid, sticky, or unable to defecate after 5 min = 4), (c) blood (no blood = 0; visible blood in rectum = 1; visible blood on fur = 2), and (d) general appearance (normal = 0; piloerection = 1; lethargy and piloerection = 2; motionless = 4).
Statistics.
Groups of animals were compared using Mann–Whitney U tests, Student’s t tests, or two-way ANOVA where applicable. P-values <0.05 were considered significant.
Acknowledgments
We thank members of the Artis laboratory for discussions and critical reading of manuscript drafts, the Matthew J. Ryan Veterinary Hospital Pathology Laboratory and the Abramson Cancer Center Flow Cytometry and Cell Sorting Resource Laboratory (partially supported by National Cancer Institute Comprehensive Cancer Center Support Grant [#2-P30 CA016520]) for technical advice and support, and K. Lam and A. Root (Pfizer) for purification of IL-22 diagnostic Abs. We thank M.R. Comeau (Amgen) for provision of TSLP-related reagents and mice.
Research in the Artis laboratory is supported by National Institutes of Health (NIH) grants AI061570, AI074878, AI087990, AI095466, AI095608, AI102942, AI106697, and AI097333 to D. Artis, T32-RR007063 and K08-DK093784 to T. Alenghat, and F32-AI72943 to A.E. Troy. This research is also supported by NIH grant DP5OD012116 to G.F. Sonnenberg, the Burroughs Wellcome Fund Investigator in Pathogenesis of Infectious Disease Award to D. Artis, Crohn’s and Colitis Foundation of America grant to D. Artis, the Australian National Health and Medical Research Council Overseas Biomedical Fellowship 613718 to P.R. Giacomin, the Swiss National Science Foundation grants PBBEP3_130438 and PA00P3_136468 to M. Noti, and the Irvington Institute Postdoctoral Fellowship of the Cancer Research Institute to L.C. Osborne.
L.A. Fouser and H.-L. Ma are employed by Pfizer. All other authors declare no competing financial interests.
Author contributions: P.R. Giacomin, R.H. Moy, M. Noti, L.C. Osborne, M.C. Siracusa, T. Alenghat, K.A. McCorkell, A.E. Troy, G.D. Rak, M.J. May, G.F. Sonnenberg, and D. Artis designed and performed the research. B. Liu, Y. Hu, H.-L. Ma, and L.A. Fouser provided reagents. P.R. Giacomin, G.F. Sonnenberg, and D. Artis analyzed the data. P.R. Giacomin and D. Artis wrote the paper.
Footnotes
Abbreviations used:
- Ab
- antibody
- AMP
- antimicrobial peptide
- cLPL
- colonic lamina propria lymphocyte
- DSS
- dextran sodium sulfate
- IBD
- inflammatory bowel disease
- IEC
- intestinal epithelial cell
- IKK
- inhibitor of κB kinase
- ILC
- innate lymphoid cell
- LT
- lymphotoxin
- mLN
- mesenteric LN
- p.i.
- postinfection
- PP
- Peyer’s patch
- TSLP
- thymic stromal lymphopoietin
References
- Artis D. 2008. Epithelial-cell recognition of commensal bacteria and maintenance of immune homeostasis in the gut. Nat. Rev. Immunol. 8:411–420. 10.1038/nri2316 [DOI] [PubMed] [Google Scholar]
- Artis D., and Spits H.. 2015. The biology of innate lymphoid cells. Nature. 517:293–301. 10.1038/nature14189 [DOI] [PubMed] [Google Scholar]
- Atreya I., Atreya R., and Neurath M.F.. 2008. NF-κB in inflammatory bowel disease. J. Intern. Med. 263:591–596. 10.1111/j.1365-2796.2008.01953.x [DOI] [PubMed] [Google Scholar]
- Aujla S.J., Chan Y.R., Zheng M., Fei M., Askew D.J., Pociask D.A., Reinhart T.A., McAllister F., Edeal J., Gaus K., et al. 2008. IL-22 mediates mucosal host defense against Gram-negative bacterial pneumonia. Nat. Med. 14:275–281. 10.1038/nm1710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernink J.H., Peters C.P., Munneke M., te Velde A.A., Meijer S.L., Weijer K., Hreggvidsdottir H.S., Heinsbroek S.E., Legrand N., Buskens C.J., et al. 2013. Human type 1 innate lymphoid cells accumulate in inflamed mucosal tissues. Nat. Immunol. 14:221–229. 10.1038/ni.2534 [DOI] [PubMed] [Google Scholar]
- Bonnegarde-Bernard A., Jee J., Fial M.J., Aeffner F., Cormet-Boyaka E., Davis I.C., Lin M., Tomé D., Karin M., Sun Y., and Boyaka P.N.. 2014. IKKβ in intestinal epithelial cells regulates allergen-specific IgA and allergic inflammation at distant mucosal sites. Mucosal Immunol. 7:257–267. 10.1038/mi.2013.43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brestoff J.R., Kim B.S., Saenz S.A., Stine R.R., Monticelli L.A., Sonnenberg G.F., Thome J.J., Farber D.L., Lutfy K., Seale P., and Artis D.. 2015. Group 2 innate lymphoid cells promote beiging of white adipose tissue and limit obesity. Nature. 519:242–246. 10.1038/nature14115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buonocore S., Ahern P.P., Uhlig H.H., Ivanov I.I., Littman D.R., Maloy K.J., and Powrie F.. 2010. Innate lymphoid cells drive interleukin-23-dependent innate intestinal pathology. Nature. 464:1371–1375. 10.1038/nature08949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cella M., Fuchs A., Vermi W., Facchetti F., Otero K., Lennerz J.K., Doherty J.M., Mills J.C., and Colonna M.. 2009. A human natural killer cell subset provides an innate source of IL-22 for mucosal immunity. Nature. 457:722–725. 10.1038/nature07537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerutti A. 2008. The regulation of IgA class switching. Nat. Rev. Immunol. 8:421–434. 10.1038/nri2322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandrakesan P., Ahmed I., Anwar T., Wang Y., Sarkar S., Singh P., Peleg S., and Umar S.. 2010. Novel changes in NF-kappaB activity during progression and regression phases of hyperplasia: role of MEK, ERK, and p38. J. Biol. Chem. 285:33485–33498. 10.1074/jbc.M110.129353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chariot A. 2009. The NF-kappaB-independent functions of IKK subunits in immunity and cancer. Trends Cell Biol. 19:404–413. 10.1016/j.tcb.2009.05.006 [DOI] [PubMed] [Google Scholar]
- Chen L.W., Egan L., Li Z.W., Greten F.R., Kagnoff M.F., and Karin M.. 2003. The two faces of IKK and NF-κB inhibition: prevention of systemic inflammation but increased local injury following intestinal ischemia-reperfusion. Nat. Med. 9:575–581. 10.1038/nm849 [DOI] [PubMed] [Google Scholar]
- Cording S., Medvedovic J., Cherrier M., and Eberl G.. 2014. Development and regulation of RORγt+ innate lymphoid cells. FEBS Lett. 588:4176–4181. 10.1016/j.febslet.2014.03.034 [DOI] [PubMed] [Google Scholar]
- Dannappel M., Vlantis K., Kumari S., Polykratis A., Kim C., Wachsmuth L., Eftychi C., Lin J., Corona T., Hermance N., et al. 2014. RIPK1 maintains epithelial homeostasis by inhibiting apoptosis and necroptosis. Nature. 513:90–94. 10.1038/nature13608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dejardin E., Droin N.M., Delhase M., Haas E., Cao Y., Makris C., Li Z.W., Karin M., Ware C.F., and Green D.R.. 2002. The lymphotoxin-β receptor induces different patterns of gene expression via two NF-κB pathways. Immunity. 17:525–535. 10.1016/S1074-7613(02)00423-5 [DOI] [PubMed] [Google Scholar]
- Eckmann L., Nebelsiek T., Fingerle A.A., Dann S.M., Mages J., Lang R., Robine S., Kagnoff M.F., Schmid R.M., Karin M., et al. 2008. Opposing functions of IKKβ during acute and chronic intestinal inflammation. Proc. Natl. Acad. Sci. USA. 105:15058–15063. 10.1073/pnas.0808216105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fung T.C., Artis D., and Sonnenberg G.F.. 2014. Anatomical localization of commensal bacteria in immune cell homeostasis and disease. Immunol. Rev. 260:35–49. 10.1111/imr.12186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geremia A., Arancibia-Cárcamo C.V., Fleming M.P., Rust N., Singh B., Mortensen N.J., Travis S.P., and Powrie F.. 2011. IL-23–responsive innate lymphoid cells are increased in inflammatory bowel disease. J. Exp. Med. 208:1127–1133. 10.1084/jem.20101712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goto Y., and Ivanov I.I.. 2013. Intestinal epithelial cells as mediators of the commensal-host immune crosstalk. Immunol. Cell Biol. 91:204–214. 10.1038/icb.2012.80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goto Y., Obata T., Kunisawa J., Sato S., Ivanov I.I., Lamichhane A., Takeyama N., Kamioka M., Sakamoto M., Matsuki T., et al. 2014. Innate lymphoid cells regulate intestinal epithelial cell glycosylation. Science. 345:1254009 10.1126/science.1254009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greten F.R., Eckmann L., Greten T.F., Park J.M., Li Z.W., Egan L.J., Kagnoff M.F., and Karin M.. 2004. IKKβ links inflammation and tumorigenesis in a mouse model of colitis-associated cancer. Cell. 118:285–296. 10.1016/j.cell.2004.07.013 [DOI] [PubMed] [Google Scholar]
- Greten F.R., Arkan M.C., Bollrath J., Hsu L.C., Goode J., Miething C., Göktuna S.I., Neuenhahn M., Fierer J., Paxian S., et al. 2007. NF-κB is a negative regulator of IL-1β secretion as revealed by genetic and pharmacological inhibition of IKKβ. Cell. 130:918–931. 10.1016/j.cell.2007.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guma M., Stepniak D., Shaked H., Spehlmann M.E., Shenouda S., Cheroutre H., Vicente-Suarez I., Eckmann L., Kagnoff M.F., and Karin M.. 2011. Constitutive intestinal NF-κB does not trigger destructive inflammation unless accompanied by MAPK activation. J. Exp. Med. 208:1889–1900. 10.1084/jem.20110242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanash A.M., Dudakov J.A., Hua G., O’Connor M.H., Young L.F., Singer N.V., West M.L., Jenq R.R., Holland A.M., Kappel L.W., et al. 2012. Interleukin-22 protects intestinal stem cells from immune-mediated tissue damage and regulates sensitivity to graft versus host disease. Immunity. 37:339–350. 10.1016/j.immuni.2012.05.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hepworth M.R., Monticelli L.A., Fung T.C., Ziegler C.G., Grunberg S., Sinha R., Mantegazza A.R., Ma H.L., Crawford A., Angelosanto J.M., et al. 2013. Innate lymphoid cells regulate CD4+ T-cell responses to intestinal commensal bacteria. Nature. 498:113–117. 10.1038/nature12240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hepworth M.R., Fung T.C., Masur S.H., Kelsen J.R., McConnell F.M., Dubrot J., Withers D.R., Hugues S., Farrar M.A., Reith W., et al. 2015. Group 3 innate lymphoid cells mediate intestinal selection of commensal bacteria-specific CD4+ T cells. Science. 348:1031–1035. 10.1126/science.aaa4812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooper L.V., and Macpherson A.J.. 2010. Immune adaptations that maintain homeostasis with the intestinal microbiota. Nat. Rev. Immunol. 10:159–169. 10.1038/nri2710 [DOI] [PubMed] [Google Scholar]
- Hsu L.C., Enzler T., Seita J., Timmer A.M., Lee C.Y., Lai T.Y., Yu G.Y., Lai L.C., Temkin V., Sinzig U., et al. 2011. IL-1β-driven neutrophilia preserves antibacterial defense in the absence of the kinase IKKβ. Nat. Immunol. 12:144–150. 10.1038/ni.1976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu H., Brittain G.C., Chang J.H., Puebla-Osorio N., Jin J., Zal A., Xiao Y., Cheng X., Chang M., Fu Y.X., et al. 2013. OTUD7B controls non-canonical NF-κB activation through deubiquitination of TRAF3. Nature. 494:371–374. 10.1038/nature11831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes T., Becknell B., Freud A.G., McClory S., Briercheck E., Yu J., Mao C., Giovenzana C., Nuovo G., Wei L., et al. 2010. Interleukin-1β selectively expands and sustains interleukin-22+ immature human natural killer cells in secondary lymphoid tissue. Immunity. 32:803–814. 10.1016/j.immuni.2010.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iliev I.D., Spadoni I., Mileti E., Matteoli G., Sonzogni A., Sampietro G.M., Foschi D., Caprioli F., Viale G., and Rescigno M.. 2009. Human intestinal epithelial cells promote the differentiation of tolerogenic dendritic cells. Gut. 58:1481–1489. 10.1136/gut.2008.175166 [DOI] [PubMed] [Google Scholar]
- Iseki M., Omori-Miyake M., Xu W., Sun X., Takaki S., Rawlings D.J., and Ziegler S.F.. 2012. Thymic stromal lymphopoietin (TSLP)-induced polyclonal B-cell activation and autoimmunity are mediated by CD4+ T cells and IL-4. Int. Immunol. 24:183–195. 10.1093/intimm/dxr113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivanov S., Renneson J., Fontaine J., Barthelemy A., Paget C., Fernandez E.M., Blanc F., De Trez C., Van Maele L., Dumoutier L., et al. 2013. Interleukin-22 reduces lung inflammation during influenza A virus infection and protects against secondary bacterial infection. J. Virol. 87:6911–6924. 10.1128/JVI.02943-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kagnoff M.F. 2014. The intestinal epithelium is an integral component of a communications network. J. Clin. Invest. 124:2841–2843. 10.1172/JCI75225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim B.S., Siracusa M.C., Saenz S.A., Noti M., Monticelli L.A., Sonnenberg G.F., Hepworth M.R., Van Voorhees A.S., Comeau M.R., and Artis D.. 2013. TSLP elicits IL-33–independent innate lymphoid cell responses to promote skin inflammation. Sci. Transl. Med. 5:170ra16 10.1126/scitranslmed.3005374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim C.J., Nazli A., Rojas O.L., Chege D., Alidina Z., Huibner S., Mujib S., Benko E., Kovacs C., Shin L.Y., et al. 2012. A role for mucosal IL-22 production and Th22 cells in HIV-associated mucosal immunopathogenesis. Mucosal Immunol. 5:670–680. 10.1038/mi.2012.72 [DOI] [PubMed] [Google Scholar]
- Kinnebrew M.A., Buffie C.G., Diehl G.E., Zenewicz L.A., Leiner I., Hohl T.M., Flavell R.A., Littman D.R., and Pamer E.G.. 2012. Interleukin 23 production by intestinal CD103+CD11b+ dendritic cells in response to bacterial flagellin enhances mucosal innate immune defense. Immunity. 36:276–287. 10.1016/j.immuni.2011.12.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirchberger S., Royston D.J., Boulard O., Thornton E., Franchini F., Szabady R.L., Harrison O., and Powrie F.. 2013. Innate lymphoid cells sustain colon cancer through production of interleukin-22 in a mouse model. J. Exp. Med. 210:917–931. 10.1084/jem.20122308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiss E.A., Vonarbourg C., Kopfmann S., Hobeika E., Finke D., Esser C., and Diefenbach A.. 2011. Natural aryl hydrocarbon receptor ligands control organogenesis of intestinal lymphoid follicles. Science. 334:1561–1565. 10.1126/science.1214914 [DOI] [PubMed] [Google Scholar]
- Klatt N.R., Estes J.D., Sun X., Ortiz A.M., Barber J.S., Harris L.D., Cervasi B., Yokomizo L.K., Pan L., Vinton C.L., et al. 2012. Loss of mucosal CD103+ DCs and IL-17+ and IL-22+ lymphocytes is associated with mucosal damage in SIV infection. Mucosal Immunol. 5:646–657. 10.1038/mi.2012.38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam L.T., Davis R.E., Ngo V.N., Lenz G., Wright G., Xu W., Zhao H., Yu X., Dang L., and Staudt L.M.. 2008. Compensatory IKKα activation of classical NF-κB signaling during IKKβ inhibition identified by an RNA interference sensitization screen. Proc. Natl. Acad. Sci. USA. 105:20798–20803. 10.1073/pnas.0806491106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence T., Bebien M., Liu G.Y., Nizet V., and Karin M.. 2005. IKKα limits macrophage NF-κB activation and contributes to the resolution of inflammation. Nature. 434:1138–1143. 10.1038/nature03491 [DOI] [PubMed] [Google Scholar]
- Lee H.C., and Ziegler S.F.. 2007. Inducible expression of the proallergic cytokine thymic stromal lymphopoietin in airway epithelial cells is controlled by NFκB. Proc. Natl. Acad. Sci. USA. 104:914–919. 10.1073/pnas.0607305104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J.S., Cella M., McDonald K.G., Garlanda C., Kennedy G.D., Nukaya M., Mantovani A., Kopan R., Bradfield C.A., Newberry R.D., and Colonna M.. 2012. AHR drives the development of gut ILC22 cells and postnatal lymphoid tissues via pathways dependent on and independent of Notch. Nat. Immunol. 13:144–151. 10.1038/ni.2187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee M.W., Odegaard J.I., Mukundan L., Qiu Y., Molofsky A.B., Nussbaum J.C., Yun K., Locksley R.M., and Chawla A.. 2015. Activated type 2 innate lymphoid cells regulate beige fat biogenesis. Cell. 160:74–87. 10.1016/j.cell.2014.12.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu B., Xia X., Zhu F., Park E., Carbajal S., Kiguchi K., DiGiovanni J., Fischer S.M., and Hu Y.. 2008. IKKα is required to maintain skin homeostasis and prevent skin cancer. Cancer Cell. 14:212–225. 10.1016/j.ccr.2008.07.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macho-Fernandez E., Koroleva E.P., Spencer C.M., Tighe M., Torrado E., Cooper A.M., Fu Y.X., and Tumanov A.V.. 2015. Lymphotoxin beta receptor signaling limits mucosal damage through driving IL-23 production by epithelial cells. Mucosal Immunol. 8:403–413. 10.1038/mi.2014.78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maloy K.J., and Powrie F.. 2011. Intestinal homeostasis and its breakdown in inflammatory bowel disease. Nature. 474:298–306. 10.1038/nature10208 [DOI] [PubMed] [Google Scholar]
- Manta C., Heupel E., Radulovic K., Rossini V., Garbi N., Riedel C.U., and Niess J.H.. 2013. CX3CR1+ macrophages support IL-22 production by innate lymphoid cells during infection with Citrobacter rodentium. Mucosal Immunol. 6:177–188. 10.1038/mi.2012.61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchiando A.M., Graham W.V., and Turner J.R.. 2010. Epithelial barriers in homeostasis and disease. Annu. Rev. Pathol. 5:119–144. 10.1146/annurev.pathol.4.110807.092135 [DOI] [PubMed] [Google Scholar]
- Matsushima A., Kaisho T., Rennert P.D., Nakano H., Kurosawa K., Uchida D., Takeda K., Akira S., and Matsumoto M.. 2001. Essential role of nuclear factor (NF)-κB–inducing kinase and inhibitor of κB (IκB) kinase α in NF-κB activation through lymphotoxin beta receptor, but not through tumor necrosis factor receptor I. J. Exp. Med. 193:631–636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKenzie A.N., Spits H., and Eberl G.. 2014. Innate lymphoid cells in inflammation and immunity. Immunity. 41:366–374. 10.1016/j.immuni.2014.09.006 [DOI] [PubMed] [Google Scholar]
- Mjösberg J., Bernink J., Golebski K., Karrich J.J., Peters C.P., Blom B., te Velde A.A., Fokkens W.J., van Drunen C.M., and Spits H.. 2012. The transcription factor GATA3 is essential for the function of human type 2 innate lymphoid cells. Immunity. 37:649–659. 10.1016/j.immuni.2012.08.015 [DOI] [PubMed] [Google Scholar]
- Molofsky A.B., Nussbaum J.C., Liang H.E., Van Dyken S.J., Cheng L.E., Mohapatra A., Chawla A., and Locksley R.M.. 2013. Innate lymphoid type 2 cells sustain visceral adipose tissue eosinophils and alternatively activated macrophages. J. Exp. Med. 210:535–549. 10.1084/jem.20121964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monticelli L.A., Sonnenberg G.F., Abt M.C., Alenghat T., Ziegler C.G., Doering T.A., Angelosanto J.M., Laidlaw B.J., Yang C.Y., Sathaliyawala T., et al. 2011. Innate lymphoid cells promote lung-tissue homeostasis after infection with influenza virus. Nat. Immunol. 12:1045–1054. 10.1038/ni.2131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mundy R., MacDonald T.T., Dougan G., Frankel G., and Wiles S.. 2005. Citrobacter rodentium of mice and man. Cell. Microbiol. 7:1697–1706. 10.1111/j.1462-5822.2005.00625.x [DOI] [PubMed] [Google Scholar]
- Muñoz M., Eidenschenk C., Ota N., Wong K., Lohmann U., Kühl A.A., Wang X., Manzanillo P., Li Y., Rutz S., et al. 2015. Interleukin-22 induces interleukin-18 expression from epithelial cells during intestinal infection. Immunity. 42:321–331. 10.1016/j.immuni.2015.01.011 [DOI] [PubMed] [Google Scholar]
- Neill D.R., Wong S.H., Bellosi A., Flynn R.J., Daly M., Langford T.K., Bucks C., Kane C.M., Fallon P.G., Pannell R., et al. 2010. Nuocytes represent a new innate effector leukocyte that mediates type-2 immunity. Nature. 464:1367–1370. 10.1038/nature08900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nenci A., Becker C., Wullaert A., Gareus R., van Loo G., Danese S., Huth M., Nikolaev A., Neufert C., Madison B., et al. 2007. Epithelial NEMO links innate immunity to chronic intestinal inflammation. Nature. 446:557–561. 10.1038/nature05698 [DOI] [PubMed] [Google Scholar]
- Noti M., Kim B.S., Siracusa M.C., Rak G.D., Kubo M., Moghaddam A.E., Sattentau Q.A., Comeau M.R., Spergel J.M., and Artis D.. 2014. Exposure to food allergens through inflamed skin promotes intestinal food allergy through the thymic stromal lymphopoietin-basophil axis. J. Allergy Clin. Immunol. 133:1390–1399. 10.1016/j.jaci.2014.01.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliphant C.J., Hwang Y.Y., Walker J.A., Salimi M., Wong S.H., Brewer J.M., Englezakis A., Barlow J.L., Hams E., Scanlon S.T., et al. 2014. MHCII-mediated dialog between group 2 innate lymphoid cells and CD4+ T cells potentiates type 2 immunity and promotes parasitic helminth expulsion. Immunity. 41:283–295. 10.1016/j.immuni.2014.06.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ota N., Wong K., Valdez P.A., Zheng Y., Crellin N.K., Diehl L., and Ouyang W.. 2011. IL-22 bridges the lymphotoxin pathway with the maintenance of colonic lymphoid structures during infection with Citrobacter rodentium. Nat. Immunol. 12:941–948. 10.1038/ni.2089 [DOI] [PubMed] [Google Scholar]
- Pasparakis M. 2008. IKK/NF-κB signaling in intestinal epithelial cells controls immune homeostasis in the gut. Mucosal Immunol. 1:S54–S57. 10.1038/mi.2008.53 [DOI] [PubMed] [Google Scholar]
- Pasparakis M., Courtois G., Hafner M., Schmidt-Supprian M., Nenci A., Toksoy A., Krampert M., Goebeler M., Gillitzer R., Israel A., et al. 2002. TNF-mediated inflammatory skin disease in mice with epidermis-specific deletion of IKK2. Nature. 417:861–866. 10.1038/nature00820 [DOI] [PubMed] [Google Scholar]
- Peterson L.W., and Artis D.. 2014. Intestinal epithelial cells: regulators of barrier function and immune homeostasis. Nat. Rev. Immunol. 14:141–153. 10.1038/nri3608 [DOI] [PubMed] [Google Scholar]
- Qiu J., Heller J.J., Guo X., Chen Z.M., Fish K., Fu Y.X., and Zhou L.. 2012. The aryl hydrocarbon receptor regulates gut immunity through modulation of innate lymphoid cells. Immunity. 36:92–104. 10.1016/j.immuni.2011.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reardon C., Lechmann M., Brüstle A., Gareau M.G., Shuman N., Philpott D., Ziegler S.F., and Mak T.W.. 2011. Thymic stromal lymphopoetin-induced expression of the endogenous inhibitory enzyme SLPI mediates recovery from colonic inflammation. Immunity. 35:223–235. 10.1016/j.immuni.2011.05.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rescigno M. 2011. The intestinal epithelial barrier in the control of homeostasis and immunity. Trends Immunol. 32:256–264. 10.1016/j.it.2011.04.003 [DOI] [PubMed] [Google Scholar]
- Reynders A., Yessaad N., Vu Manh T.P., Dalod M., Fenis A., Aubry C., Nikitas G., Escalière B., Renauld J.C., Dussurget O., et al. 2011. Identity, regulation and in vivo function of gut NKp46+RORγt+ and NKp46+RORγt− lymphoid cells. EMBO J. 30:2934–2947. 10.1038/emboj.2011.201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rimoldi M., Chieppa M., Larghi P., Vulcano M., Allavena P., and Rescigno M.. 2005a. Monocyte-derived dendritic cells activated by bacteria or by bacteria-stimulated epithelial cells are functionally different. Blood. 106:2818–2826. 10.1182/blood-2004-11-4321 [DOI] [PubMed] [Google Scholar]
- Rimoldi M., Chieppa M., Salucci V., Avogadri F., Sonzogni A., Sampietro G.M., Nespoli A., Viale G., Allavena P., and Rescigno M.. 2005b. Intestinal immune homeostasis is regulated by the crosstalk between epithelial cells and dendritic cells. Nat. Immunol. 6:507–514. 10.1038/ni1192 [DOI] [PubMed] [Google Scholar]
- Roediger B., Kyle R., Yip K.H., Sumaria N., Guy T.V., Kim B.S., Mitchell A.J., Tay S.S., Jain R., Forbes-Blom E., et al. 2013. Cutaneous immunosurveillance and regulation of inflammation by group 2 innate lymphoid cells. Nat. Immunol. 14:564–573. 10.1038/ni.2584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satoh-Takayama N., Vosshenrich C.A., Lesjean-Pottier S., Sawa S., Lochner M., Rattis F., Mention J.J., Thiam K., Cerf-Bensussan N., Mandelboim O., et al. 2008. Microbial flora drives interleukin 22 production in intestinal NKp46+ cells that provide innate mucosal immune defense. Immunity. 29:958–970. 10.1016/j.immuni.2008.11.001 [DOI] [PubMed] [Google Scholar]
- Sawa S., Lochner M., Satoh-Takayama N., Dulauroy S., Bérard M., Kleinschek M., Cua D., Di Santo J.P., and Eberl G.. 2011. RORγt+ innate lymphoid cells regulate intestinal homeostasis by integrating negative signals from the symbiotic microbiota. Nat. Immunol. 12:320–326. 10.1038/ni.2002 [DOI] [PubMed] [Google Scholar]
- Schneider K., Potter K.G., and Ware C.F.. 2004. Lymphotoxin and LIGHT signaling pathways and target genes. Immunol. Rev. 202:49–66. 10.1111/j.0105-2896.2004.00206.x [DOI] [PubMed] [Google Scholar]
- Sebestyén M.G., Budker V.G., Budker T., Subbotin V.M., Zhang G., Monahan S.D., Lewis D.L., Wong S.C., Hagstrom J.E., and Wolff J.A.. 2006. Mechanism of plasmid delivery by hydrodynamic tail vein injection. I. Hepatocyte uptake of various molecules. J. Gene Med. 8:852–873. 10.1002/jgm.921 [DOI] [PubMed] [Google Scholar]
- Siracusa M.C., Saenz S.A., Hill D.A., Kim B.S., Headley M.B., Doering T.A., Wherry E.J., Jessup H.K., Siegel L.A., Kambayashi T., et al. 2011. TSLP promotes interleukin-3-independent basophil haematopoiesis and type 2 inflammation. Nature. 477:229–233. 10.1038/nature10329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siracusa M.C., Saenz S.A., Wojno E.D., Kim B.S., Osborne L.C., Ziegler C.G., Benitez A.J., Ruymann K.R., Farber D.L., Sleiman P.M., et al. 2013. Thymic stromal lymphopoietin-mediated extramedullary hematopoiesis promotes allergic inflammation. Immunity. 39:1158–1170. 10.1016/j.immuni.2013.09.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smythies L.E., Sellers M., Clements R.H., Mosteller-Barnum M., Meng G., Benjamin W.H., Orenstein J.M., and Smith P.D.. 2005. Human intestinal macrophages display profound inflammatory anergy despite avid phagocytic and bacteriocidal activity. J. Clin. Invest. 115:66–75. 10.1172/JCI200519229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonnenberg G.F. 2014. Regulation of intestinal health and disease by innate lymphoid cells. Int. Immunol. 26:501–507. 10.1093/intimm/dxu052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonnenberg G.F., Fouser L.A., and Artis D.. 2011a. Border patrol: regulation of immunity, inflammation and tissue homeostasis at barrier surfaces by IL-22. Nat. Immunol. 12:383–390. 10.1038/ni.2025 [DOI] [PubMed] [Google Scholar]
- Sonnenberg G.F., Monticelli L.A., Elloso M.M., Fouser L.A., and Artis D.. 2011b. CD4+ lymphoid tissue-inducer cells promote innate immunity in the gut. Immunity. 34:122–134. 10.1016/j.immuni.2010.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonnenberg G.F., Monticelli L.A., Alenghat T., Fung T.C., Hutnick N.A., Kunisawa J., Shibata N., Grunberg S., Sinha R., Zahm A.M., et al. 2012. Innate lymphoid cells promote anatomical containment of lymphoid-resident commensal bacteria. Science. 336:1321–1325. 10.1126/science.1222551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spits H., and Cupedo T.. 2012. Innate lymphoid cells: emerging insights in development, lineage relationships, and function. Annu. Rev. Immunol. 30:647–675. 10.1146/annurev-immunol-020711-075053 [DOI] [PubMed] [Google Scholar]
- Spits H., and Di Santo J.P.. 2011. The expanding family of innate lymphoid cells: regulators and effectors of immunity and tissue remodeling. Nat. Immunol. 12:21–27. 10.1038/ni.1962 [DOI] [PubMed] [Google Scholar]
- Strober W. 1998. Interactions between epithelial cells and immune cells in the intestine. Ann. N. Y. Acad. Sci. 859:37–45. 10.1111/j.1749-6632.1998.tb11109.x [DOI] [PubMed] [Google Scholar]
- Strober W., Murray P.J., Kitani A., and Watanabe T.. 2006. Signalling pathways and molecular interactions of NOD1 and NOD2. Nat. Rev. Immunol. 6:9–20. 10.1038/nri1747 [DOI] [PubMed] [Google Scholar]
- Suda T., and Liu D.. 2007. Hydrodynamic gene delivery: its principles and applications. Mol. Ther. 15:2063–2069. 10.1038/sj.mt.6300314 [DOI] [PubMed] [Google Scholar]
- Takahashi N., Vereecke L., Bertrand M.J., Duprez L., Berger S.B., Divert T., Gonçalves A., Sze M., Gilbert B., Kourula S., et al. 2014. RIPK1 ensures intestinal homeostasis by protecting the epithelium against apoptosis. Nature. 513:95–99. 10.1038/nature13706 [DOI] [PubMed] [Google Scholar]
- Taylor B.C., Zaph C., Troy A.E., Du Y., Guild K.J., Comeau M.R., and Artis D.. 2009. TSLP regulates intestinal immunity and inflammation in mouse models of helminth infection and colitis. J. Exp. Med. 206:655–667. 10.1084/jem.20081499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tumanov A.V., Koroleva E.P., Guo X., Wang Y., Kruglov A., Nedospasov S., and Fu Y.X.. 2011. Lymphotoxin controls the IL-22 protection pathway in gut innate lymphoid cells during mucosal pathogen challenge. Cell Host Microbe. 10:44–53. 10.1016/j.chom.2011.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vereecke L., Vieira-Silva S., Billiet T., van Es J.H., Mc Guire C., Slowicka K., Sze M., van den Born M., De Hertogh G., Clevers H., et al. 2014. A20 controls intestinal homeostasis through cell-specific activities. Nat. Commun. 5:5103 10.1038/ncomms6103 [DOI] [PubMed] [Google Scholar]
- Vlantis K., Wullaert A., Sasaki Y., Schmidt-Supprian M., Rajewsky K., Roskams T., and Pasparakis M.. 2011. Constitutive IKK2 activation in intestinal epithelial cells induces intestinal tumors in mice. J. Clin. Invest. 121:2781–2793. 10.1172/JCI45349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vonarbourg C., Mortha A., Bui V.L., Hernandez P.P., Kiss E.A., Hoyler T., Flach M., Bengsch B., Thimme R., Hölscher C., et al. 2010. Regulated expression of nuclear receptor RORγt confers distinct functional fates to NK cell receptor-expressing RORγt+ innate lymphocytes. Immunity. 33:736–751. 10.1016/j.immuni.2010.10.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker J.A., Barlow J.L., and McKenzie A.N.. 2013. Innate lymphoid cells—how did we miss them? Nat. Rev. Immunol. 13:75–87. 10.1038/nri3349 [DOI] [PubMed] [Google Scholar]
- Wang Y., Xiang G.S., Kourouma F., and Umar S.. 2006. Citrobacter rodentium-induced NF-κB activation in hyperproliferating colonic epithelia: role of p65 (Ser536) phosphorylation. Br. J. Pharmacol. 148:814–824. 10.1038/sj.bjp.0706784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Koroleva E.P., Kruglov A.A., Kuprash D.V., Nedospasov S.A., Fu Y.X., and Tumanov A.V.. 2010. Lymphotoxin beta receptor signaling in intestinal epithelial cells orchestrates innate immune responses against mucosal bacterial infection. Immunity. 32:403–413. 10.1016/j.immuni.2010.02.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welz P.S., Wullaert A., Vlantis K., Kondylis V., Fernández-Majada V., Ermolaeva M., Kirsch P., Sterner-Kock A., van Loo G., and Pasparakis M.. 2011. FADD prevents RIP3-mediated epithelial cell necrosis and chronic intestinal inflammation. Nature. 477:330–334. 10.1038/nature10273 [DOI] [PubMed] [Google Scholar]
- Xu W., He B., Chiu A., Chadburn A., Shan M., Buldys M., Ding A., Knowles D.M., Santini P.A., and Cerutti A.. 2007. Epithelial cells trigger frontline immunoglobulin class switching through a pathway regulated by the inhibitor SLPI. Nat. Immunol. 8:294–303. 10.1038/ni1434 [DOI] [PubMed] [Google Scholar]
- Yang J., Chen S., Huang L., Michalopoulos G.K., and Liu Y.. 2001. Sustained expression of naked plasmid DNA encoding hepatocyte growth factor in mice promotes liver and overall body growth. Hepatology. 33:848–859. 10.1053/jhep.2001.23438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaph C., Troy A.E., Taylor B.C., Berman-Booty L.D., Guild K.J., Du Y., Yost E.A., Gruber A.D., May M.J., Greten F.R., et al. 2007. Epithelial-cell-intrinsic IKK-β expression regulates intestinal immune homeostasis. Nature. 446:552–556. 10.1038/nature05590 [DOI] [PubMed] [Google Scholar]
- Zhang B., Chassaing B., Shi Z., Uchiyama R., Zhang Z., Denning T.L., Crawford S.E., Pruijssers A.J., Iskarpatyoti J.A., Estes M.K., et al. 2014. Prevention and cure of rotavirus infection via TLR5/NLRC4-mediated production of IL-22 and IL-18. Science. 346:861–865. 10.1126/science.1256999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng Y., Valdez P.A., Danilenko D.M., Hu Y., Sa S.M., Gong Q., Abbas A.R., Modrusan Z., Ghilardi N., de Sauvage F.J., and Ouyang W.. 2008. Interleukin-22 mediates early host defense against attaching and effacing bacterial pathogens. Nat. Med. 14:282–289. 10.1038/nm1720 [DOI] [PubMed] [Google Scholar]
- Ziegler S.F., Roan F., Bell B.D., Stoklasek T.A., Kitajima M., and Han H.. 2013. The biology of thymic stromal lymphopoietin (TSLP). Adv. Pharmacol. 66:129–155. 10.1016/B978-0-12-404717-4.00004-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zindl C.L., Lai J.F., Lee Y.K., Maynard C.L., Harbour S.N., Ouyang W., Chaplin D.D., and Weaver C.T.. 2013. IL-22-producing neutrophils contribute to antimicrobial defense and restitution of colonic epithelial integrity during colitis. Proc. Natl. Acad. Sci. USA. 110:12768–12773. 10.1073/pnas.1300318110 [DOI] [PMC free article] [PubMed] [Google Scholar]