Abstract
Objectives
A rise in obstetric anal sphincter injuries (OASIS) has been observed and a preventive approach, originating in Finland, has been introduced in several European hospitals. The aim of this paper was to systematically evaluate the evidence behind the ‘Finnish intervention’.
Design
A systematic review of the literature conducted according to the Preferred Reporting for Systematic Reviews and Meta-analyses (PRISMA) guidelines.
Outcome measures
The primary outcome was OASIS. Secondary outcomes were (perinatal): Apgar scores, pH and standard base excess in the umbilical cord, and (maternal): episiotomy, intact perineum, first and second-degree perineal lacerations, duration of second stage, birth position and women's perceptions/birth experiences.
Methods
Multiple databases (Cochrane, Embase, Pubmed and SveMed) were systematically searched for studies published up to December 2014. Both randomised controlled trials and observational studies were eligible for inclusion. Studies were excluded if a full-text article was not available. Studies were evaluated by use of international reporting guidelines (eg, STROBE).
Results
Overall, 1042 articles were screened and 65 retrieved for full-text evaluation. Seven studies, all observational and with a level of evidence at 2c or lower, were included and consistently reported a significant reduction in OASIS. All evaluated episiotomy and found a significant increase. Three studies evaluated perinatal outcomes and reported conflicting results. No study reported on other perineal outcomes, duration of the second stage, birth positions or women's perceptions.
Conclusions
A reduction in OASIS has been contributed to the Finnish intervention in seven observational studies, all with a low level of evidence. Knowledge about the potential perinatal and maternal side effects and women's perceptions of the intervention is extremely limited and the biological mechanisms underlying the Finnish intervention are not well documented. Studies with a high level of evidence are needed to assess the effects of the intervention before implementation in clinical settings can be recommended.
Keywords: EPIDEMIOLOGY
Strengths and limitations of this study.
Complete, comprehensive and reproducible literature search based on the Population Intervention Comparison Outcome approach.
Transparency and reproducibility due to adherence of this study to Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) requirements and the Preferred Reporting for Systematic Reviews and Meta-analyses (PRISMA) guidelines.
Search of Finnish language studies would have strengthened our search strategy.
Background
The incidence of obstetric anal sphincter injuries (OASIS) is estimated to be as high as 11% in postpartum women, but the incidence depends on the studied population and the used method of identification.1–4 A number of studies conducted in Nordic countries have reported an increase in OASIS over the past decades.5–7 The underlying causes are unclear, but older, heavier mothers and a ‘hands off’ approach to the delivery of the fetal head have been presented as possible explanations. However, there is no evidence that these factors alone are responsible for the increasing incidence of OASIS.6–8 The fact that as many as 30–50% of women with OASIS will develop short-term or long-term symptoms such as chronic anal incontinence, faecal urgency, perineal pain and dyspareunia emphasises the importance of prevention9 as these conditions may compromise the quality of life for women and potentially lead to anxiety and depression.10 Despite this risk of severe sequelae, it remains unclear what factors provide the most effective protection against OASIS. A Cochrane review of techniques that may reduce perineal trauma in the second stage of labour found a significant beneficial effect of warm compressions and massage,2 while the effect of manual techniques for perineal support has yet to be determined. Despite this, manual techniques for perineal support have been widely used globally for decades.11 12 Box 1 presents some of these techniques.
Box 1. Manual support techniques.
The flexion technique11
Described by DeWees in 1889.
The manoeuvre involves maintenance of flexion of the emerging fetal head by exerting pressure on the occiput with one hand towards the perineum and thereby preventing extension until crowning has occurred. The other hand is placed on the perineum for support.
Ritgen's manoeuvre12
Described by Ritgen in Williams Obstetrics 1st Edition in 1903.
The manoeuvre is performed between contractions where two fingers are placed behind the anus and a forward and upward pressure is applied on the forehead through the perineum.
This was a modification from the original description, which instructed fingers to be placed into the rectum.
Modified Ritgen's manoeuvre12
Described in 1976 in Williams Obstetrics 15th Edition.
The manoeuvre is identical with Ritgen's manoeuvre but is performed during a contraction.
The Finnish manoeuvre5
The speed of crowning is controlled by exerting pressure on the occiput with one hand. Simultaneously, the thumb and index finger of the other hand are used to support the perineum while the flexed middle finger takes a grip on the baby's chin. When a good grip has been achieved, the woman is asked to stop pushing and to breathe rapidly, while the accoucheur slowly helps the baby's head through the vaginal introitus. When most of the head is out, the perineal ring is pushed under the baby's chin.
A search for effective interventions to reduce perineal trauma has led many obstetric units especially in Norway, Sweden and Denmark to introduce a protective procedure, featuring a manual support technique that is reported to be widely practised in Finland (the Finnish manoeuvre).13 The procedure, here subsequently refered to as ‘the Finnish intervention’, is a package of care introduced in Norway. It consists of four elements: (1) good communication between the accoucheur and the delivering woman; (2) the ‘Finnish manoeuvre’ (see box 1); (3) use of a delivery position that allows visual examination of the perineum during the last minutes of delivery; and (4) mediolateral episiotomy on indication.14 In Norway, for example, over 90% of obstetric units recommend the use of manual support techniques and in 48% of the units, the Finnish intervention is used.13 However, the Finnish intervention remains controversial and its use is strongly debated.15–19 Proponents of manual support techniques in general argue that pressure against the perineum protects the fragile tissue and that pressure against the fetal head before crowning aids presentation of the smallest diameter, and thus reduces the risk of laceration.2 20 Critics argue that the fetal head will naturally travel through the birth canal with the least resistance, thereby allowing the smallest diameter to crown. Pressure against the fetal head may disturb this natural orientation and lead the head towards the fragile perineum and thus increase the risk of OASIS.11 Other points of controversy are the use of episiotomy on indications such as rigid perineum and imminent perineal tear and restriction of birth position to positions that allow visual examination of the perineum (often interpreted as a semi-recumbent or side-lying position), as these run counter to recommendations based on randomised controlled trials.21 22 More knowledge is thus needed to inform decisions on the introduction of the Finnish intervention as prevention of OASIS. We therefore performed a systematic review of the literature and evidence regarding the Finnish intervention.
Methods
Aim
The primary objective was to identify the effect of the Finnish intervention on OASIS. The secondary objectives were to examine other effects and potential side effects, including perinatal outcomes such as Apgar scores and pH and standard base excess in the umbilical cord as well as maternal outcomes such as episiotomy, intact perineum, first and second-degree perineal lacerations, duration of the second stage, birth position, and women's perception and birth experiences. The secondary outcomes are chosen based on a Cochrane review evaluating methods to prevent perineal trauma.2
Study design
The systematic review of the literature was conducted according to the Preferred Reporting for Systematic Reviews and Meta-analyses (PRISMA) guidelines.23
Data sources and search strategy
A systematic search was performed in the electronic databases Cochrane, Embase, Pubmed and SveMed. On the basis of the Population Intervention Comparison Outcome (PICO)24 approach, the search was structured by combining MeSH terms/EMTREE terms and/or free-text form related to population (eg, parturition and vaginal birth), intervention (eg, perineum and perineal support) and outcomes (eg, OASIS, perineal trauma and Apgar scores), see online supplementary additional file 1. There were no restrictions on publication date or publication status. Studies published in the English, Danish, Norwegian and Swedish languages were included in the search. The reference lists of the included studies were hand searched for other relevant studies that may have been missed by our electronic searches. The latest literature search was performed on 8 December 2014 by the first three authors of this article.
Study selection
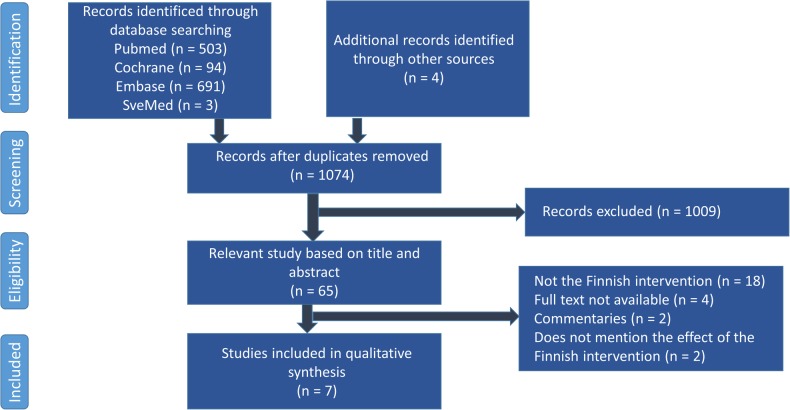
Studies were excluded if they (A) were duplicates, (B) were not relevant based on the title and abstract, (C) did not include the Finnish intervention, (D) did not focus on prevention of OASIS or any of the predefined primary or secondary outcomes of this study. We also excluded editorials, letters to editors, commentaries and studies where no full-text article was available. The study selection and subsequent information extraction was performed by the three aforementioned authors. Figure 1 presents a flow chart of the search process and study selection.
Figure 1.
Flow chart of literature search.
Data extraction
To extract relevant information and to assess the methodological quality of the studies, we used a predesigned data abstraction form based on the guidelines described in the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement25 and by National Institute for Health and Care Excellence.26 The data concerned study design, evidence level,27 study size, inclusion and exclusion criteria, outcomes, results, as well as study strengths and limitations, especially the risk of bias and confounding.26 The authors independently extracted the data from the included studies and compared and discussed them until consensus was reached.
Results
Our database searches identified 1295 articles, as presented in figure 1. After removal of duplicates, 1074 articles remained. Initial screening for relevant articles based on the title and abstract excluded 1009 articles. Of the remaining 65 articles, 18 articles involved techniques other than the Finnish intervention. Four records were excluded as full-text articles were not available, two because they were commentaries, and two because the effects of the intervention were not mentioned. Of the remaining articles, seven concerned the Finnish intervention reported on at least one of the predefined outcomes and were thus included in this review. All articles described non-randomised and non-blinded cross-sectional studies performed in a Nordic country. No randomised controlled trials or systematic review concerning the Finnish intervention or relating to the intervention were identified. An overview of the included studies is provided in table 1.
Table 1.
Included studies on the ‘Finnish intervention’
| Study | Study design | Data providers | Population | Comparator groups | Inclusion and exclusion criteria | Primary outcome | Secondary outcomes |
|---|---|---|---|---|---|---|---|
| Pirhonen et al 19985 | Register study | Skåne University Hospital, Malmö, Sweden, and Turku University Hospital, Finland | 30 933 births | 1990–1994 | Unknown | OASIS: Significantly lower frequency of OASIS in Finland (0.36%) compared to Sweden (2.69%) (p<0.001) | Apgar score after 5 min: Lower Apgar score in Finland compared to Sweden (p<0.01), caused by differences in the use of instrumental delivery |
| Length of second stage of labour: Prolonged second stage in Finland compared to Sweden (p<0.05) | |||||||
| Episiotomy: Significantly more usage of episiotomy in Finland (37.2%) compared to Sweden (24.3%) (p<0.001) | |||||||
| Laine et al 200828 | Before-and-after study | Oestfold Trust Hospital, Norway | 12 369 births | 2002–2007 | All births in one obstetric unit | OASIS: Significantly lower frequency of OASIS after implementation from 4.03% to 1.17% (p<0.001) | OASIS at instrumental deliveries: Significantly lower OASIS frequency after implementation from 16.26% to 4.90% (p<0.001) |
| Episiotomy: Significantly more use of episiotomy after implementation from 13.9% to 21.1% (p<0.001) | |||||||
| Laine et al 20096 | Register study | Finland: Hospital Discharge Register 1987–2007 and Medical Birth Register 2004–2007 Norway: Medical Birth Register, National Public Health Institute Sweden: Medical Birth Register, National Board of Health and Welfare Denmark: Medical Birth Register, National Board of Health |
1968–2007 | All vaginal births in Norway (1968–2007) Sweden (1973–2007) Denmark (1997–2007 Finland (1987–2007) |
OASIS: The frequency of OASIS is significantly higher in Denmark (3.6%), Norway (4.1%), and Sweden (4.2%) compared to Finland (0.6%) (p<0.001) The frequency is increasing in all four countries |
Episiotomy: Significantly decreasing frequency of episiotomy in all countries (no p value reported) | |
| Hals et al 201014 | Before-and-after study | Tromsø University Hospital, Stavanger University Hospital, Lillehammer Hospital, and Ålesund Hospital, Norway | 40 152 births | 2003–2009 | All vaginal births in 4 obstetric units | OASIS: Significantly lower frequency of OASIS after implementation from 4–5% to 1–2% (p<0.001) | OASIS at instrumental deliveries: Significantly lower frequency of OASIS after implementation from 12.81–16.45% to 6.0–6.7% (p<0.001) |
| Apgar score after 5 min: Improved Apgar score after 5 min (no p value reported) | |||||||
| Blood gas in umbilical cord: No changes | |||||||
| Episiotomy: Significantly more use of episiotomy in 2 units (p<0.001), but unchanged in two. | |||||||
| Laine et al 20128 | Before-and-after study | Oslo University Hospital, Norway | 31 709 births | 2003–2005 and 2008–2010 | All births in one obstetric unit Excluded: Sectio, preterm births (GA <32 weeks), and multiple pregnancies |
OASIS: Significantly lower OASIS frequency after implementation from 4.0% to 1.9% (p<0.01) The reduction was seen in all the groups. |
OASIS at instrumental deliveries: Reduction in the frequency of OASIS from 10.8% to 5.0% at instrumental deliveries (p<0.01) |
| Episiotomy: Significantly increased use of episiotomy in primiparous women from 31.4% to 36.2% (p<0.001) | |||||||
| Episiotomy at spontaneous deliveries: Significantly decreased use of episiotomy in primiparous women from 24.7% to 22.7% (p=0.006) | |||||||
| Episiotomy at instrumental deliveries: Significantly increased use of episiotomy in primiparous women from 60.8% to 85.1% (p<0.001) | |||||||
| Laine et al 20137 | Register study | Norway: Medical Birth Registry of Norway, National Institute of Public Health Sweden: Medical Birth Register, National Board of Health and Welfare Denmark: Medical Birth Register, National Board of Health Finland: Hospital Discharge Register 1987–2004 and Medical Birth Register 2004–2010 |
574 175 births | 2004–2010 | All vaginal births in Norway (1968–2010), Sweden (1973–2010), Denmark (1997–2010), and Finland (1987–2010) | OASIS: Finland had a lower frequency of OASIS (0.7–1.0%) compared to other Scandinavian countries (2.3–4.2%) (no p value reported) | Episiotomy: Frequency of episiotomy in Norway was increased from 17.8% in 2004 to 19.1% in 2010 (p<0.001) Frequency of episiotomy in Finland was decreased from 32.0% to 24.0% (p<0.001) |
| Stedenfeldt et al 201329 | Before-and-after study | Tromsø University Hospital, Stavanger University Hospital, Lillehammer Hospital, Ålesund Hospital, and Oestfold Hospital Trust, Norway. Same data as Laine et al 2008 28 and Hals et al 2010 14 | 40 154 births | 2003–2009 | All vaginal births in 5 obstetric units in Norway. Excluded: GA< 22 weeks and birth weight < 500 g | OASIS: Significantly reduced risk for OASIS after the intervention (59%; OR: 0.41; 95% CI 0.36 to 0.46). | Apgar score 5 min after birth: Significantly increased frequency of Apgar score <7 (p=0.02) |
| Episiotomy: Significantly increased frequency of episiotomy after the implementation (14.4–24.3%; OR: 1.92; 95% CI 1.82 to 2.02) |
GA, gestational age; OASIS, obstetric anal sphincter injuries.
Primary outcome
All seven articles reported on OASIS as the primary outcome. Despite observational designs and the general low level of evidence (see tables 1 and 2), all articles reported a decrease in the rate of OASIS after the implementation of the Finnish intervention. In Pirhonen et al's5 comparison of the frequency of OASIS in Turku, Finland, and Malmö, Sweden, the Finnish manoeuvre is conjectured to have caused the significant decrease. Several Norwegian studies have subsequently reached the same conclusion.7 8 14 28 29 The dominant design was observational before-and-after studies such as Laine et al's28 study of 12 369 vaginal births in the same obstetric unit between 2002 and 2007 in which they report a significant reduction from 4.03% to 1.17% (p<0.001) after the implementation of the intervention. This result was corroborated by Laine et al's8 study of 31 709 vaginal births, which also showed a significant reduction from 4.0% to 1.9%. In 2010, a study of 40 152 vaginal births in 2003 and 2009 by Hals et al14 likewise found a significantly reduced prevalence after the intervention was implemented in four Norwegian obstetric units, from 4–5% to 1–2% (p<0.001). Their results, as well as Laine et al's, were backed in Stedenfeldt et al's29 study of the same data. The occurrence of OASIS in Norway, Finland, Sweden and Denmark was also compared by Laine et al6 in 2009 and 2013 in two large register-based studies,7 both of which reported a lower rate for Finland, where the manoeuvre is more widely used (2.3–4.1% in Norway vs 0.7–1.0% in Finland).6 7 It is noticeable that five studies performed multivariate analysis to investigate potential confounders or competing risk factors for OASIS,5 8 14 28 29 but only two studies clearly stated which factors were included in the analysis.8 29
Table 2.
Comments on the included studies
| Study | Evidence level | Shortcomings of study design | Shortcomings of data provided | Limitations/strengths as presented by study authors |
|---|---|---|---|---|
| Pirhonen et al 19985 | 2c | The Finnish manoeuvre is not predefined as an outcome | – | No evaluation of the study design and its limitations regarding the interventions causality |
| Laine et al 200828 | 4 | Comparison of two groups not consistent in time | Same data as Stedenfeldt et al 201329 | No evaluation of the study design and its limitations regarding the interventions causality Missing key elements of study design |
| Laine et al 20096 | 2c | – | Overlapping data with Laine et al 20137 | Good integration of results with literature to date |
| Hals et al 201014 | 4 | Comparison of two groups not consistent in time | Same data as Stedenfeldt et al 201329 | No interpretation of the increased use of episiotomy. No evaluation of the study design and its limitations regarding the interventions causality No evaluation of the study's limitations |
| Laine et al 20128 | 4 | Comparison of two groups not consistent in time | – | Thorough evaluation of strengths of the study No evaluation of the study's limitations |
| Laine et al 20137 | 2c | – | Overlapping data with Laine et al 20096 | Thorough evaluation of strengths and limitations regarding study design |
| Stedenfeldt et al 201329 | 4 | – | Same data as Laine et al 2008 28 and Hals et al 201014 | Thorough evaluation of strengths and limitations regarding study design. Presentation of positive and negative results. Thorough presentation of relevant evidence |
Secondary outcomes: perinatal
Perinatal outcomes after the introduction of the Finnish intervention were evaluated in three studies. Table 1 shows their conflicting results. Hals et al14 found a slight improvement in Apgar scores 5 min after birth (no report of p values, ORs or 95% CIs), while blood gases from the umbilical cord showed no differences. In contrast, Stedenfeldt et al29 reported a significant increase in the number of neonates with Apgar scores below 7 points 5 min after birth (p<0.05). Pirhonen et al's5 comparative study of the frequency of OASIS in Turku and Malmö (mentioned above) found lower Apgar scores 5 min after birth in Turku (where the Finnish manoeuvre was reported to be widely used), but attributed this to the higher prevalence of instrumental deliveries in this area (p<0.01).
Secondary outcomes: maternal
The use of episiotomy was surveyed in all studies. The studies implementing the Finnish intervention showed a significant increase after the implementation 5 8 14 28 29 and the studies with comparisons of countries showed a higher prevalence in the clinics that used the Finnish intervention (table 1).5–7
Other outcomes
No study reported on intact perineum, first and second-degree perineal lacerations, duration of the second stage, birth position, and women's perception/birth experiences or any other outcomes or maternal effects/potential side effects of the intervention.
Evidence level
In table 2, the ecological studies are categorised as evidence level 2c as recommended. 27 The before-and-after studies are categorised as 4, as the studies cannot be classified as cohort or case-control studies. Furthermore, the studies failed to identify or appropriately control for known potential confounders, the comparison of the groups was not consistent in time, and exposures and outcomes were not measured in the same objective way in the exposed and non-exposed groups, as the data in the exposed group were collected prospectively, while the data of the non-exposed group were collected retrospectively.
Discussion
Key results
The aim of this study was to review the current literature regarding the Finnish intervention. Our systematic literature search identified seven studies evaluating the effect of the intervention, none of which were randomised or blinded. The evidence level was 2c or lower. They found that the implementation of the Finnish intervention was followed by significant reductions in OASIS and significant increases in the use of episiotomy.
Summary of evidence level
The evidence supporting the Finnish intervention is limited, as it is based on only seven studies with receding quality. The authors furthermore belong to a restricted group working on the basis of exclusively Nordic data, some of which were used in three studies.14 28 29 No causal effects can be established as none of the studies were randomised, blinded or compared the intervention to a concurrent controlled group. Furthermore, the intervention was not carried out in a standardised or controlled way. Despite these obvious limitations, the studies conclude that the occurrence of OASIS is reduced as a result of the Finnish intervention. 5–8 14 28 29 This is particularly worrying in the case of the frequently cited study by Pirhonen et al5 which aimed to compare frequencies of OASIS. This study was not predefined or designed to evaluate effects of the Finnish manoeuvre, but the authors suggested on the basis of educational books and personal experiences that the significantly lower frequency of OASIS in Finland compared to Sweden could be explained by the use of the manoeuvre in Finland.
Interpretation of the current evidence level
Methodological limitations related to the available studies of the Finnish intervention mean that the reported reduction of OASIS may potentially be accounted for by several other factors such as confounders or competing risk. A key point for consideration is that the Finnish intervention (see the background section and box 1) consists of four elements. One element with a negative influence on the outcome may thus have counteracted a positive effect of another element, and vice versa. Although none of the studies attempted to determine the effect of the individual elements, several of the studies claim that the manual support technique (the Finnish manoeuvre, box 1) is the most important part of the intervention and the one that constitutes the basis of the observed significant reduction in OASIS.8 14 28 29 Critics, however, argue that other manual support techniques could replace the Finnish manoeuvre provided that the other three elements of the Finnish intervention were retained.19 We maintain that the effect of the Finnish intervention remains unclear and that the theoretical basis for its main element, the Finnish manoeuvre, is questionable. We are concerned about the implications of a procedure that forces the infant's emerging neck to flex at crowning, whereby the presenting diameter is likely to increase. As the fetal head circumference is a well-known OASIS risk indicator, we urge further study of the Finnish manoeuvre's physiology before its use can be recommended.2 In assessing the Finnish intervention, it should also be considered that its introduction was accompanied by intense training and educational programmes.8 10 14 The Hawthorne effect is known to predict an independent effect of increasing the attention to a problem.30 Furthermore, since the Finnish intervention was not executed in a controlled way, the staff in hospitals and/or regions who had reduction of OASIS as a focus point may have combined the intervention with other common preventive techniques, such as warm compression or massage of the perineum, that have a documented effect on reduction of OASIS.2 Finally, episiotomy techniques have changed during the study periods. Hals et al14 reported that median episiotomy had been used before, while lateral or mediolateral episiotomy was used after the Finnish intervention was introduced. As median episiotomy is known to be a significant risk factor for OASIS,31 this shift may have contributed to the declining incidence.
Unexplored adverse effects and suggestions for research
Though the well-being of the infant should be considered before any intervention, little attention has been given to this aspect with only three studies reporting on fetal outcome. 5 14 29 Although the effect of the Finnish intervention on the length of the second stage has not been sufficiently evaluated,5 the intervention is likely to slow down the crowning of the fetus, at the same time slightly increasing the period of maximum pressure to the fetal head. The conflicting findings on the Apgar score 5 14 29 indicate a need for further studies of perinatal effects. Use of umbilical blood gases as a measurement would be a more objective indicator for infant well-being, but missing data could be a challenge as a test of umbilical blood gases is not routinely used in all birth settings.
The studies report an increase in the use of episiotomy after the implementation of the Finnish intervention. Although the evidence is contested, episiotomy is used to expedite birth, indicated, for example, by fetal distress, and to avert severe perineal trauma. Several studies have shown that an episiotomy is equally painful and involves tearing of the same structures as a second-degree spontaneous perineal laceration,32 33 and the literature generally recommends a restricted use of episiotomy.22 Episiotomy in the Finnish intervention should only be performed on indication.8 14 28 29 Although the use of episiotomy is thus restricted, indications include rigid perineum and imminent perineal tear. In a Nordic setting where episiotomy rates have for decades been low and routine use of episiotomy has been abandoned, this is a widening of the indications for episiotomy which may explain the increased use of episotomy following the implementation of the Finnish intervention. Laine et al7 suggest that as the episiotomy rate has increased, the incidence of OASIS has dropped, but limited evidence for this causal relationship is presented. Räisänen et al34 have estimated that 909 lateral episiotomies are needed to avert one anal sphincter injury. Although the perineal damage caused by episiotomy is less severe than the damage related to OASIS and therefore preferable, interventions that increase the use of episiotomy should be closely monitored.
The pain and discomfort of perineal trauma perceived by women essentialise efforts to minimise not only OASIS but also all traumas to the genital tract. We suggest that future research should investigate the effect of the Finnish intervention on first and second-degree perineal laceration as well as intact perineum; a favourable birth outcome with a positive influence in, for example, women's sexual life postpartum.35 36 Finally, future research should give more attention to the effects of the Finnish intervention on women's birth positions and perceptions of the intervention. Encouragement of women to use a delivery position that allows execution of the Finnish intervention and visual examination of the perineum during the last minutes of delivery could be problematic, as it may affect birth experiences and violate women's right to an informed choice in child birth. Moreover, it runs counter to recommendations in a Cochrane review.21
Finally, further research should take into account that factors such as episiotomy, duration of second stage of labour and birth position have the potential to be confounders or competing risk factors when evaluating the effect of the Finnish intervention to decrease the incidence of OASIS. The study designs and methods used in the current studies do not allow for determination of whether the factors had a positive, negative or neutral influence on the incidence of OASIS. In five of the included studies, an attempt to identify and remove potential risk factors for OASIS with multivariate analysis has been conducted,5 8 14 28 29 but as stated, only two studies describe which factors have been taken into account,8 29 and it is unclear if the decrease in OASIS is still significant in the multivariate analysis.
Strengths and limitations
The strength of this study lies in its foundation in the systematic, comprehensive and reproducible literature search based on the PICO approach24 and searches in the international English language as well as Scandinavian language article databases. A search of Finnish language studies would have further strengthened our strategy but to counter a potential oversight of relevant articles, the reference lists of the included studies were also searched. A rigorous appraisal of the included studies was performed and the transparency and reproducibility of this review is supported by its adherence to STROBE requirements25 and the PRISMA statement.23
What this study adds
This study adds to the understanding of a four-element approach to OASIS prevention that is rapidly being introduced in many obstetric units, especially in the Nordic countries and the UK. We suggest that the term, ‘the Finnish intervention’, should be used to ensure the clarity of concepts and increased generalisability of findings, as we find evidence in the literature that the intervention is confused with the general use of techniques for manual support of the perineum. Furthermore, our study is the first to offer an overview of the evidence underlying the Finnish intervention, based on a comprehensive and systematic approach in accordance with criteria for evidence-based medicine. Our study demonstrates that the theoretical foundation and causal relationship proposed in support of the Finnish intervention are as yet insufficient. We find that the evidence level underlying the intervention does not meet the requirements of evidence-based medicine and wish to voice our concern regarding the lack of investigation of potential adverse effects. Despite this, there is no indication in the literature that women are given an informed choice of the Finnish intervention and no exploration of women's experiences with the intervention seems to have been attempted as yet.
Implication for practice
The risk of severe potential short-term and long-term effects of OASIS for new mothers makes their prevention a priority in practice and research. Still, our findings in this systematic review do not support a broad-scale introduction of the Finnish intervention in clinical settings at this point. Uncertainty about the potential adverse effects and causation highlights the need for investigation of a broader range of maternal and perinatal effects in studies providing higher levels of evidence, such as randomised controlled trials (RCTs). RCTs may be difficult to carry out due to the four elements of the intervention that must all be taken into consideration and performed according to protocol. A question that arises is whether the Finnish interventions should be considered as a whole or if the elements should be investigated separately. We believe that since the Finnish manoeuvre is described as the most important element, this should be the focus of the trials. An RCT could be formed by comparing the Finnish intervention with another intervention such as applying the warm compressions instead of the Finnish manoeuvre and maintaining the other three elements. Conducting an RCT is likely to be challenging but not impossible as other manual perineal protection methods have already been tested using RCTs.2
In the absence of solid evidence, we encourage clinicians to monitor the occurrence of OASIS, to implement interventions with documented positive effects, including the use of warm perineal compressions and massage during the second stage of labour,2 and to stimulate discussions of best practice. Where the Finnish intervention has already been implemented, we urge management and staff to perform quality assessments and ensure that balanced information is offered to women.
Conclusions
A series of seven observational studies from Nordic countries have found a reduction inf OASIS after the introduction of the Finnish intervention for all vaginal births when compared to periods or settings in which it was not routinely used. The level of evidence of these studies is, however, low and the physiological mechanisms underlying the Finnish intervention are not well documented. The implementation of the Finnish intervention in clinical settings cannot be recommended before a wider range of maternal and perinatal effects have been further evaluated in randomised controlled trials.
Acknowledgments
The authors thank the university librarian and medical information specialist Mette Buje Grundsøe, cand.scient.bibl., for competent supervision and assistance in the systematic literature search.
Footnotes
Contributors: All four authors jointly developed the design of the study. MØP, MLM and A-CS-M carried out the systematic search, data extraction and made the first draft of the manuscript, while contributing equally to all aspects of the work. All authors took part in the interpretation of data and the critical revision of the manuscript for important intellectual content, read and approved the final version, and are accountable for all aspects of the work.
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Dudding TC, Vaizey CJ, Kamm MA. Obstetric anal sphincter injury: incidence, risk factors, and management. Ann Surg 2008;247:224–37. 10.1097/SLA.0b013e318142cdf4 [DOI] [PubMed] [Google Scholar]
- 2.Aasheim V, Nilsen AB, Lukasse M et al. Perineal techniques during the second stage of labour for reducing perineal trauma. Cochrane Database Syst Rev 2011:CD006672 10.1002/14651858.CD006672.pub2 [DOI] [PubMed] [Google Scholar]
- 3.Ramalingam K, Monga AK. Outcomes and follow-up after obstetric anal sphincter injuries. Int Urogynecol J 2013;24:1495–500. 10.1007/s00192-013-2051-9 [DOI] [PubMed] [Google Scholar]
- 4.Smith LA, Price N, Simonite V et al. Incidence of and risk factors for perineal trauma: a prospective observational study. BMC Pregnancy Childbirth 2013;13:59 10.1186/1471-2393-13-59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pirhonen JP, Grenman SE, Haadem K et al. Frequency of anal sphincter rupture at delivery in Sweden and Finland—result of difference in manual help to the baby's head. Acta Obstet Gynecol Scand 1998;77:974–7. 10.1080/j.1600-0412.1998.771005.x [DOI] [PubMed] [Google Scholar]
- 6.Laine K, Gissler M, Pirhonen J. Changing incidence of anal sphincter tears in four Nordic countries through the last decades. Eur J Obs Gynecol Reprod Biol 2009;146:71–5. 10.1016/j.ejogrb.2009.04.033 [DOI] [PubMed] [Google Scholar]
- 7.Laine K, Rotvold W, Staff AC. Are obstetric anal sphincter ruptures preventable?—large and consistent rupture rate variations between the Nordic countries and between delivery units in Norway. Acta Obstet Gynecol Scand 2013;92:94–100. 10.1111/aogs.12024 [DOI] [PubMed] [Google Scholar]
- 8.Laine K, Skjeldestad FE, Sandvik L et al. Incidence of obstetric anal sphincter injuries after training to protect the perineum: cohort study. BMJ Open 2012;2:e001649 10.1136/bmjopen-2012-001649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Samuelsson E, Ladfors L, Wennerholm UB et al. Anal sphincter tears: prospective study of obstetric risk factors. BJOG 2000;107:926–31. 10.1111/j.1471-0528.2000.tb11093.x [DOI] [PubMed] [Google Scholar]
- 10.Pirhonen T, Gissler M, Hartgill T et al. Experiences of expert midwives in a training program aimed at decreasing perineal tears. Int J Nurs Midwifery 2011;3:70–5. [Google Scholar]
- 11.Myrfield K, Brook C, Creedy D. Reducing perineal trauma: implications of flexion and extension of the fetal head during birth. Midwifery 1997;13:197–201. 10.1016/S0266-6138(97)80006-X [DOI] [PubMed] [Google Scholar]
- 12.Cunningham FG. The Ritgen maneuver: another sacred cow questioned. Obstet Gynecol 2008;112:210–11. 10.1097/AOG.0b013e318182a8d3 [DOI] [PubMed] [Google Scholar]
- 13.Fretheim A, Tanbo T, Vangen S et al. Use of manual techniques for perineal support in Norwegian maternity departments. Tidsskr Nor Legeforen 2011;131:2352–4. 10.4045/tidsskr.11.0643 [DOI] [PubMed] [Google Scholar]
- 14.Hals E, Øian P, Pirhonen T et al. A multicenter interventional program to reduce the incidence of anal sphincter tears. Obstet Gynecol 2010;116:901–8. 10.1097/AOG.0b013e3181eda77a [DOI] [PubMed] [Google Scholar]
- 15.Dahlen HG, Priddis H, Thornton C. Severe perineal trauma is rising, but let us not overreact. Midwifery 2015;31:1–8. 10.1016/j.midw.2014.09.004 [DOI] [PubMed] [Google Scholar]
- 16.Petrocnik P, Marshall JE. Hands-poised technique: The future technique for perineal management of second stage of labour? A modified systematic literature review. Midwifery 2015;31:274–9. 10.1016/j.midw.2014.10.004 [DOI] [PubMed] [Google Scholar]
- 17.Maimburg RD. Fagligt indstik: Evidensbaseret klinik ved caputs forløsning. Tidsskr Jordemødre 2015. [Google Scholar]
- 18.Rasmussen OB, Gommesen D, Christiansen AG et al. Kommentarer til artiklen “Evidensbaseret klinik ved caputs forløsning”, Tidsskrift for Jordemødre 1/2015. Tidsskr Jordemødre 2015;2. [Google Scholar]
- 19.Fretheim A. Fødselsrifter—vitenskapsteori og klinisk praksis. Tidsskr Nor Legeforen 2013;133:4. [Google Scholar]
- 20.Cheng YW, Hopkins LM, Caughey AB. How long is too long: does a prolonged second stage of labor in nulliparous women affect maternal and neonatal outcomes? Am J Obstet Gynecol 2004;191:933–8. 10.1016/j.ajog.2004.05.044 [DOI] [PubMed] [Google Scholar]
- 21.Gupta JK, Hofmeyr GJ, Shehmar M. Position in the second stage of labour for women without epidural anaesthesia. Cochrane Database Syst Rev 2012;5:CD002006 10.1002/14651858.CD002006.pub3 [DOI] [PubMed] [Google Scholar]
- 22.Eason E, Labrecque M, Wells G et al. Preventing perineal trauma during childbirth: a systematic review. Obstet Gynecol 2000;95:464–71. 10.1016/S0029-7844(99)00560-8 [DOI] [PubMed] [Google Scholar]
- 23.Liberati A, Altman DG, Tetzlaff J et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;339:b2700 10.1136/bmj.b2700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Richardson WS, Wilson MC, Nishikawa J et al. The well-built clinical question: a key to evidence-based decisions. ACP J Club 1995;123:A12–13. [PubMed] [Google Scholar]
- 25.Von Elm E, Altman DG, Egger M et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int J Surg 2014;12:1495–9. 10.1016/j.ijsu.2014.07.013 [DOI] [PubMed] [Google Scholar]
- 26.National Institute for Health and Clinical Excellence. London: Methods for development of NICE public health guidance, 2006. http://www.nice.org.uk/article/pmg4/resources/non-guidance-methods-for-the- development-of-nice-public-health-guidance-third-edition-pdf (accessed 23 May 2015). [PubMed] [Google Scholar]
- 27.OCEBM Levels of Evidence Working Group. The Oxford 2009 Levels of Evidence. Oxford Centre for Evidence-Based Medicine. http://www.cebm.net/index.aspx?o=5653 (accessed 23 may 2015).
- 28.Laine K, Pirhonen T, Rolland R et al. Decreasing the incidence of anal sphincter tears during delivery. Obstet Gynecol 2008;111:1053–7. 10.1097/AOG.0b013e31816c4402 [DOI] [PubMed] [Google Scholar]
- 29.Stedenfeldt M, Øian P, Gissler M et al. Risk factors for obstetric anal sphincter injury after a successful multicentre interventional programme. BJOG 2014;121:83–91. 10.1111/1471-0528.12274 [DOI] [PubMed] [Google Scholar]
- 30.Adair JG. The Hawthorne effect: A reconsideration of the methodological artifact. J Appl Psychol 1984;69:334–45. 10.1037/0021-9010.69.2.334 [DOI] [Google Scholar]
- 31.Gerdin E, Sverrisdottir G, Badi A et al. The role of maternal age and episiotomy in the risk of anal sphincter tears during childbirth. Aust N Z J Obstet Gynaecol 2007;47:286–90. 10.1111/j.1479-828X.2007.00739.x [DOI] [PubMed] [Google Scholar]
- 32.Sultan AH, Kamm MA, Hudson CN et al. Third degree obstetric anal sphincter tears: risk factors and outcome of primary repair. BMJ 1994;308:887–91. 10.1136/bmj.308.6933.887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Klein MC, Gauthier RJ, Robbins JM et al. Relationship of episiotomy to perineal trauma and morbidity, sexual dysfunction, and pelvic floor relaxation. Am J Obstet Gynecol 1994;171:591–8. 10.1016/0002-9378(94)90070-1 [DOI] [PubMed] [Google Scholar]
- 34.Räisänen S, Vehviläinen-Julkunen K, Cartwright R et al. Vacuum-assisted deliveries and the risk of obstetric anal sphincter injuries-a retrospective register-based study in Finland. BJOG 2012;119:1370–8. 10.1111/j.1471-0528.2012.03455.x [DOI] [PubMed] [Google Scholar]
- 35.McDonald E, Gartland D, Small R et al. Dyspareunia and childbirth: a prospective cohort study. BJOG 2015;122:672–9. 10.1111/1471-0528.13263 [DOI] [PubMed] [Google Scholar]
- 36.Rathfisch G, Dikencik BK, Kizilkaya Beji N et al. Effects of perineal trauma on postpartum sexual function. J Adv Nurs 2010;66:2640–9. 10.1111/j.1365-2648.2010.05428.x [DOI] [PubMed] [Google Scholar]