Abstract
Background/Aims:
Advanced human immunodeficiency virus (HIV) infection, despite sustained viral suppression by highly active antiretroviral therapy (HAART), is a risk factor for poor immunologic recovery. However, some patients with advanced infection do show immunologic recovery. In this study, predictive factors of immunologic recovery were analyzed in advanced HIV patients showing sustained viral suppression.
Methods:
A case-control study was conducted in HIV-infected adult patients with HIV-1 RNA < 50 copies/mL maintained for 4 years or longer and who were receiving HAART. Advanced HIV infection was defined as a baseline CD4 T cell count < 200/mm3. Immunologic responders were defined as patients showing immunologic recovery (CD4 T cell counts ≥ 500/mm3 at 4 years with HAART). To analyze the CD4 T cell kinetics, the CD4 slope (monthly changes in the CD4 T cell count) was estimated for each patient using a linear regression between the CD4 T cell count and the time since HAART initiation.
Results:
Of 102 eligible patients, 73 had advanced HIV, and 33 (45.2%) showed immunologic recovery. The median CD4 slopes (cells/mm3 per month) during 0 to 6 and 0 to 12 months of HAART in the 73 advanced patients were significantly higher in responders than in non-responders (0 to 6 months, 38.6 vs. 22.8; 0 to 12 months, 24.5 vs. 13.5). Multivariate analyses showed opportunistic infections at the start of HAART (adjusted odds ratio [OR], 0.28) and a CD4 slope ≥ 20 during 0 to 12 months of HAART (adjusted OR, 10.10) were independently associated with immunologic recovery.
Conclusions:
The CD4 slope can be an early predictor of long-term immunologic recovery in advanced HIV patients.
Keywords: Antiretroviral therapy, CD4 T lymphocyte, Immunologic response
INTRODUCTION
Although the number of newly diagnosed human immunodeficiency virus (HIV) infections each year is reducing, there were still 35.0 million people were living with HIV and 1.5 million who died of HIV-related infections in 2013 [1].
The key clinical features of untreated HIV patients are, impaired immune function and increased risk of disease progression and death [2,3]. Since zidovudine (ZDV) was first introduced as an antiretroviral therapy in 1987, treatment has greatly improved due to the advent of potent combination therapies in 1996 [3,4]. Combination therapies, known as highly active antiretroviral therapy (HAART), have been significantly effective in reducing and maintaining HIV loads at below detectable levels [2]. Despite the aviremic status achieved by HAART, HIV infection cannot be eradicated because of the persistence of the HIV in CD4 T cells [5,6]. Therefore, the primary goals of HAART are not only to suppress the plasma HIV load, but also to restore immunologic function, reduce opportunistic infections (OIs), and improve the survival of infected patients [3].
On receiving HAART, immunologic responses in patients are assessed by means of increases in their CD4 T cell counts. The immunologic response under HAART is a three-phase process. In the first phase, during 2 to 3 months after HAART initiation, the number of peripheral CD4 T cells increases rapidly, at an average rate of 20 to 30 cells/mm3/month [2,7-9]. This is due to the redistribution of memory CD4 T cells from the lymphoid tissue to the blood compartment. The second phase lasts until the end of the second year of HAART, during which CD4 T cells increase by 5 to 10 cells/mm3/month. Thereafter, in the third phase, the incremental pace of CD4 T cell count slows to 2 to 5 cells/mm3/month [8,10]. During the latter two phases, mostly naïve CD4 T cells increase by various mechanisms: de novo production of T cells in the thymus, homeostatic proliferation of residual CD4 T cells, and the extension of the half-life of CD4 T cells [2,11].
Despite successful virologic suppression, however, some patients fail to achieve an adequate immunologic response. Old age and coinfection with other viruses, such as hepatitis C virus (HCV), are among the factors associated with a poor immunologic response. A baseline CD4 T cell count < 200/mm3 when starting HAART is also a risk factor of poor immunologic response [2,9-16]. Nevertheless, some advanced patients with baseline CD4 T cell counts < 200/mm3 do achieve adequate immunologic recovery [15]. The predictive factors of immunologic recovery in advanced HIV-infected patients were investigated in this study.
METHODS
Study population
Adult HIV-infected patients who visited a university-affiliated hospital in 1991 to 2011 and had received HAART for ≥ 4 years were enrolled in the study. The HAART regimen was defined as a combination of three antiretroviral drugs, including a combination of two nucleoside reverse-transcriptase inhibitors (NRTIs) and one of following: either a non-NRTI, a protease inhibitor (PI), or an integrase strand transfer inhibitor [3]. The HAART regimen was classified as NNRTI-based, boosted PI-based, unboosted PI-based, and mixed, according to the backbone of antiretroviral drugs administered. A boosted PI-based regimen was defined as a ritonavirboosted PI-containing regimen. A mixed regimen was defined as a switch from one class to another [3].
Laboratory data were collected every 2 to 6 months to monitor patients after initiation of HAART. Because the objective of this study was to identify predictive factors of immunologic recovery in virologically suppressed patients, the analysis was restricted to those patients who achieved and maintained virologic suppression for ≥ 4 years with adequate medication adherence. Virologic suppression was defined as plasma HIV-1 RNA loads of < 50 copies/mL. Virologic failure was defined as two consecutive HIV-1 RNA loads > 200 copies/mL [3,17]. Intermittent viremia, defined as HIV-1 RNA loads being mostly < 50 copies/mL but only temporarily rising over 50 copies/mL, was not regarded as a virologic failure. To eliminate the effects of previous treatments, these patients were included only if the end of a previous treatment regimen had occurred at least 1 year from the start of the current treatment.
Immunologic responders (case group) were defined as patients showing CD4 T cell counts ≥ 500/mm3 at 4 years after HAART initiation, and immunologic non-responders (control group) were those who did not [10,18]. The two groups were compared for various clinical and laboratory parameters, including the “CD4 slope,” to assess factors associated with immunologic recovery. Medical records were reviewed, including age, sex, route of HIV transmission, time interval between HIV diagnosis and HAART initiation, comorbidities, HAART regimen, OIs, and clinical stage at the start of HAART. Clinical categories of HIV infection were classified according to the 1993 revised classification system of the Centers for Disease Control and Prevention (CDC), and OIs were defined as the clinical conditions listed in the surveillance case definitions for HIV infection and acquired immunodeficiency syndrome (AIDS) in the CDC [19]. Coinfections of hepatitis B virus (HBV) and of HCV were defined as being positive for HBV surface antigen, anti-HCV antibody, and HCV polymerase chain reaction, respectively.
The CD4 T cell count was measured using a Cytomics FC 500 (Beckman Coulter, Brea, CA, USA), and plasma HIV-1 RNA loads were measured by COBAS AmpliPrep/COBAS TaqMan HIV-1 Test (Roche Molecular Diagnostics, Pleasanton, CA, USA).
Statistical analysis
Univariate analysis of continuous variables was performed by t, Mann-Whitney U, or median tests, as appropriate. Categorical variables were compared between the case and control groups by a chi-square test. Multivariate analysis was performed using logistic regression. The CD4 slope, representing the CD4 T cell count change per month (cells/mm3/month), was calculated for each patient as the slope of a best-fit line obtained by linear regression of CD4 T cell counts during a certain treatment period, against the time since HAART initiation: If there were three CD4 T cell results during 0- to 12-month period; for example, (0 month, 100 cells/mm3; 4 months, 300 cells/mm3; and 10 months, 500 cells/mm3), a linear regression analysis was performed with these 3 data points. The best-fit line was calculated, and its slope was designated as the CD4 slope during 0 to 12 months.
All statistical analyses were performed using IBM SPSS version 20 (IBM Co., Armonk, NY, USA). A two-sided p < 0.05 was considered to indicate statistical significance.
Ethics statement
This study was approved by the Institutional Review Board of the Pusan National University Hospital (Protocol No. E-2013012) according to the Declaration of Helsinki. The requirement for informed consent was waived by the board.
RESULTS
A total of 102 patients met the inclusion criteria. Their mean age was 44.9 years, and 85.3% were male. The baseline CD4 T cell count (mean ± SD) was 129.9 ± 109.5/mm3. Fifty-nine (57.8%) were immunologic responders, and 43 (42.2%) were non-responders (Table 1). Baseline CD4 T cell counts (mean ± SD) were 173.4 ± 113.1/mm3 and 70.1 ± 69.6/mm3 in responders and non-responders, respectively (p < 0.001). OIs at the start of HAART were more frequent in non-responders than in responders (51.2% vs. 33.9%), but this was not statistically significant (p = 0.080). The most frequent OI was tuberculosis (TB) (8/58 in responders and 9/43 in non-responders). There were no differences between responders and non-responders in age, time from diagnosis of HIV infection to initiation of HAART, CDC HIV-1 categories, and HBV or HCV coinfection.
Table 1.
Clinical and laboratory characteristics of all 102 patients according to their immunologic responses to highly active antiretroviral therapy
| Characteristic | Responder (n = 59) | Non-responder (n = 43) | p value |
|---|---|---|---|
| Age, yr | 44.9 ± 9.3 | 44.8 ± 10.8 | 0.969 |
| Male sex | 49 (83.1) | 38 (88.4) | 0.454 |
| Route of HIV transmission | 0.328 | ||
| Heterosexual contact | 34 (57.6) | 28 (65.1) | |
| Male homosexual contact | 25 (42.4) | 14 (32.6) | |
| Transfusion | 0 | 1 (2.3) | |
| Time from diagnosis of HIV infection to initiation of HAART, day | 572.5 ± 895.2 | 746.6 ± 1,312.8 | 0.428 |
| Baseline CD4 T cell/mm3 | 173.4 ± 113.1 | 70.1 ± 69.6 | < 0.001 |
| Baseline CD4 T cell count < 200/mm3 | 33 (55.9) | 40 (93.0) | < 0.001 |
| Baseline CD4 T cell count < 50/mm3 | 10 (16.9) | 23 (53.5) | < 0.001 |
| Baseline viral load > 100,000 copies/mLa | 49 (83.1) | 35 (81.4) | 0.829 |
| CDC HIV-1 disease categoryb | 0.157 | ||
| A | 30 (50.8) | 15 (34.9) | |
| B | 11 (18.6) | 7 (16.3) | |
| C | 18 (30.5) | 21 (48.8) | |
| Hepatitis B or C coinfection | 6 (10.2) | 5 (11.6) | 0.815 |
| Syphilis | 30 (50.8) | 22 (51.2) | 0.975 |
| Opportunistic infections at the start of HAARTc | 20 (33.9) | 22 (51.2) | 0.080 |
| Tuberculosis | 8 (13.6) | 9 (20.9) | 0.324 |
| Pneumocystis pneumonia | 7 (11.9) | 8 (18.6) | 0.343 |
| Cytomegalovirus disease | 2 (3.4) | 2 (4.7) | 0.746 |
| Cryptococcal meningitis | 0 | 3 (7.0) | 0.039 |
| Esophageal candidiasis | 1 (1.7) | 2 (4.7) | 0.383 |
| Treatment-naïve when starting HAART | 57 (96.6) | 42 (97.7) | 0.753 |
| HAART regimend | 0.443 | ||
| Unboosted PI-based | 20 (33.9) | 13 (30.2) | |
| Boosted PI-based | 17 (28.8) | 18 (41.9) | |
| NNRTI-based | 16 (27.1) | 7 (16.3) | |
| Mixed | 6 (10.2) | 5 (11.6) | |
| HAART regimen including ZDV | 51 (86.4) | 39 (90.7) | 0.510 |
| TMP/SMX use | 29 (49.2) | 32 (74.4) | 0.010 |
| Duration of TMP/SMX use, mon | 0.001 | ||
| < 1 | 31 (52.5) | 14 (32.6) | |
| 1–6 | 15 (25.4) | 6 (14.0) | |
| 7–12 | 10 (16.9) | 6 (14.0) | |
| ≥ 13 | 3 (5.1) | 17 (39.5) |
Values are presented as mean ± SD or number (%).
HIV, human immunodeficiency virus; HAART, highly active antiretroviral therapy; CDC, Centers for Disease Control and Prevention; PI, protease inhibitor; NNRTI, non-nucleoside reverse transcriptase inhibitor; ZDV, zidovudine; TMP/SMX, trimethoprim/sulfamethoxazole.
There was one missing value in the responders and two in the non-responders.
According to the CDC classification [19].
Defined as the surveillance case definitions for HIV infection and acquired immunodeficiency syndrome (AIDS) of CDC [19].
According to the backbone antiretroviral drugs. The boosted PI-based regimen is defined as a ritonavir boosted PI-containing regimen. The mixed regimen is defined as switching from one class to another [19].
To exclude the influences of baseline CD4 T cell counts, factors associated with immunologic recovery were analyzed in 73 advanced patients with baseline CD4 cell counts < 200/mm3 (Table 2). Thirty-three patients (45.2%) were responders. Baseline CD4 T cell counts were 89.7 ± 57.8 and 57.1 ± 51.3/mm3 in responders and non-responders, respectively (p = 0.013). OIs at the start of HAART were more frequent in non-responders than in responders (50.5% vs. 27.3%, p = 0.048).
Table 2.
Clinical and laboratory characteristics of the 73 advanced patients according to their immunologic responses to highly active antiretroviral therapy
| Characteristic | Responder (n = 33) | Non-responder (n = 40) | p value |
|---|---|---|---|
| Age, yr | 44.0 ± 7.3 | 44.7 ± 11.1 | 0.754 |
| Male sex | 27 (81.8) | 35 (87.5) | 0.530 |
| Route of HIV transmission | 0.328 | ||
| Heterosexual contact | 17 (51.5) | 26 (65.0) | |
| Male homosexual contact | 16 (48.5) | 13 (32.5) | |
| Transfusion | 0 | 1 (2.5) | |
| Time from HIV diagnosis to HAART, day | 545.4 ± 1,017.6 | 737.8 ± 1,346.8 | 0.490 |
| Baseline CD4 T cell/mm3 | 89.7 ± 57.8 | 57.1 ± 51.3 | 0.013 |
| Baseline CD4 T cell count < 50/mm3 | 10 (30.3) | 23 (57.5) | 0.114 |
| Baseline viral load > 100,000 copies/mL | 31 (93.9) | 33 (82.5) | 0.171 |
| CDC HIV-1 disease categorya | 13 (39.4) | 12 (30.0) | 0.647 |
| A | 13 (39.4) | 12 (30.0) | |
| B | 4 (12.1) | 7 (17.5) | |
| C | 16 (48.5) | 21 (52.5) | |
| Hepatitis B or C coinfection | 2 (6.1) | 5 (12.5) | 0.446 |
| Syphilis | 16 (48.5) | 18 (45.0) | 0.766 |
| Opportunistic infections at the start of HAARTb | 9 (27.3) | 20 (50.0) | 0.048 |
| Tuberculosis | 7 (21.2) | 9 (22.5) | 0.895 |
| Pneumocystis pneumonia | 7 (21.2) | 8 (20.0) | 0.898 |
| Cytomegalovirus disease | 2 (6.1) | 2 (5.0) | 1.000 |
| Cryptococcal meningitis | 0 | 3 (7.5) | 0.247 |
| Esophageal candidiasis | 0 | 2 (5.1) | 0.498 |
| Treatment-naïve when starting HAART | 32 (97.0) | 39 (97.5) | 1.000 |
| HAART regimenc | 0.677 | ||
| Unboosted PI-based | 11 (33.3) | 12 (30.0) | |
| Boosted PI-based | 10 (30.3) | 16 (40.0) | |
| NNRTI-based | 9 (27.3) | 7 (17.5) | |
| Mixed | 3 (9.1) | 5 (12.5) | |
| HAART regimen including ZDV | 28 (84.8) | 36 (90.0) | 0.723 |
| TMP/SMX use | 27 (81.8) | 31 (77.5) | 0.650 |
| Duration of TMP/SMX use, mon | 0.002 | ||
| < 1 | 7 (21.2) | 12 (30.0) | |
| 1–6 | 13 (39.4) | 5 (12.5) | |
| 7–12 | 10 (30.3) | 6 (15.0) | |
| ≥ 13 | 3 (9.1) | 17 (42.5) |
Values are presented as mean ± SD or number (%).
HIV, human immunodeficiency virus; HAART, highly active antiretroviral therapy; CDC, Centers for Disease Control and Prevention; PI, protease inhibitor; NNRTI, non-nucleoside reverse transcriptase inhibitors; ZDV, zidovudine; TMP/SMX, trimethoprim/sulfamethoxazole.
According to the CDC classification [19].
Defined as the surveillance case definitions for HIV infection and acquired immunodeficiency syndrome (AIDS) of CDC [19].
According to the backbone antiretroviral drugs administered. The boosted PI-based regimen is defined as a ritonavir boosted PI-containing regimen. The mixed regimen is defined as switching from one class to another [19].
CD4 slope
We calculated the CD4 slopes during 0 to 6 and 0 to 12 months of HAART. Due to the large number of missing CD4 slope data during 6 to 12 months, CD4 slope during 6 to 12 months was not analyzed. For all 102 patients, the CD4 slopes during 0 to 6 and 0 to 12 months of HAART, respectively, were significantly higher in responders than in non-responders (Fig. 1): the medians for responders and non-responders were 36.8 cells/mm3/month vs. 21.3 cells/mm3/month (0 to 6 months, p = 0.024) and 20.9 cells/mm3/month vs. 13.5 cells/mm3/month (0 to 12 months, p < 0.001). This was also the case for the 73 advanced patients with baseline CD4 T cell counts < 200/mm3 (Fig. 2): the medians for responders and non-responders were 38.6 cells/mm3/month vs. 22.8 cells/mm3/month (0 to 6 months, p = 0.005) and 24.5 cells/mm3/month vs. 13.5 cells/mm3/month (0 to 12 months, p < 0.001).
Figure 1.
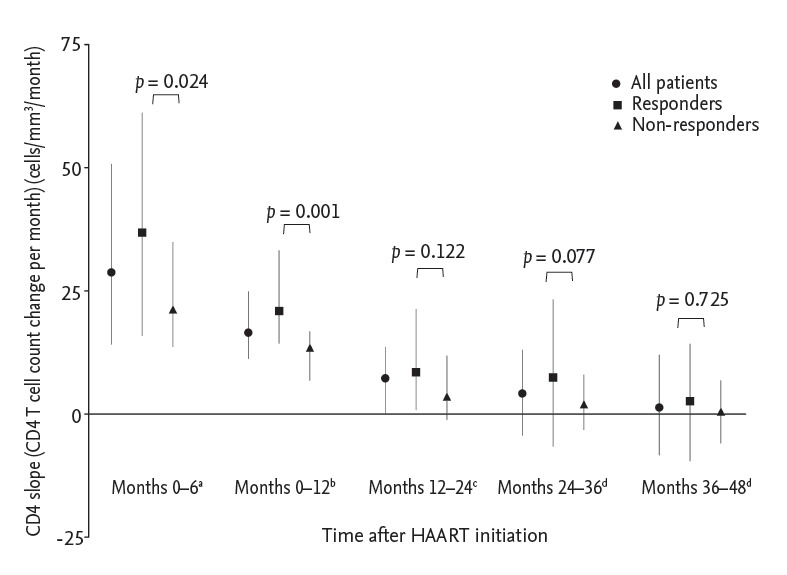
CD4 slopes in all patients during consecutive time intervals after highly active antiretroviral therapy (HAART) initiation. Data are medians and interquartile ranges. aThere were three missing values in the responders and one in the non-responders. bThere were two missing values in the responders. cThere were four missing values in both responders and non-responders. dThere were nine missing values in the responders and six in the non-responders.
Figure 2.
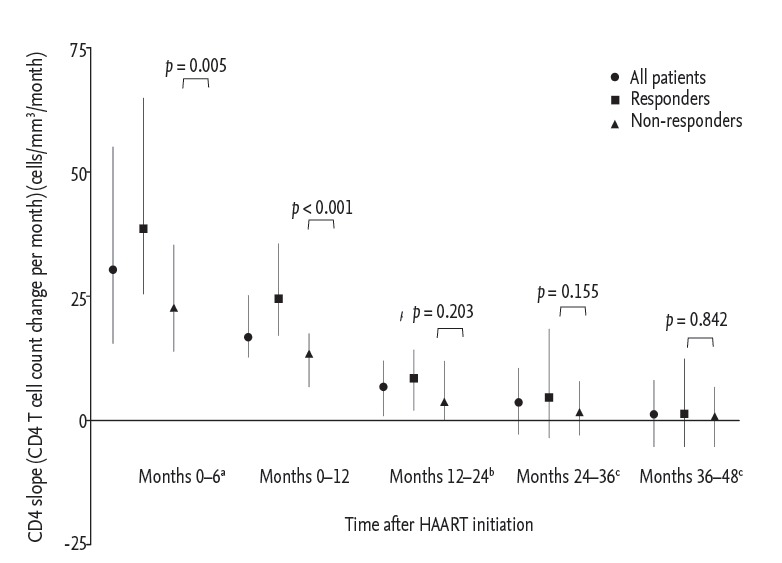
CD4 slopes in advanced patients with baseline CD4 T cell counts < 200/mm3 during consecutive time intervals after highly active antiretroviral therapy (HAART) initiation. Data are medians and interquartile ranges. aThere was one missing value in both responders and non-responders. bThere were four missing values for months 12 to 24 in the non-responders. cThere were four missing values in the responders and six in the non-responders.
The CD4 slope during 0 to 12 months of HAART was also analyzed as a dichotomous categorical variable with a cutoff of 20 cells/mm3/month. For all 102 patients, the proportion of those with a CD4 slope during 0 to 12 months ≥ 20 cells/mm3/month was significantly higher in responders (2 missing values; 30/57, 52.6%) than in non-responders (7/43, 16.3%), and the unadjusted odds ratio (OR) was 5.71 (95% confidence interval [CI], 3.32 to 32.61). Likewise, for the 73 advanced patients with baseline CD4 T cell counts < 200/mm3, the proportion was also significantly higher in responders (21/33, 63.6%) than in non-responders (7/40, 17.5%) with an unadjusted OR of 8.25 (95% CI, 2.80 to 24.31).
Multivariate analysis to identify independent predictors for immunologic recovery after HAART
Univariate analyses of all 102 patients showed that 20 of 59 responders (33.9%) and 22 of 43 non-responders (51.2%) had OIs when starting HAART, but this difference was not statistically significant (unadjusted OR, 0.49; 95% CI, 0.22 to 1.10). Multivariate analyses, however, showed that OIs at the start of HAART were independently associated with poor immunologic response (adjusted OR, 0.28; 95% CI, 0.10 to 0.83) (Table 3).
Table 3.
Multivariate logistic regression analysis to identify independent predictors of immunologic recovery
| Parameter | All 102 patients |
73 Advanced patients |
||
|---|---|---|---|---|
| Adjusted OR (95% CI) | p value | Adjusted OR (95% CI) | p value | |
| TMP/SMX use | 0.99 (0.28-3.51) | 0.985 | NA | NA |
| Opportunistic infections at the start of HAART | 0.28 (0.10-0.83) | 0.022 | 0.28 (0.08-0.94) | 0.039 |
| Baseline CD4 T cell count ≥ 200 cells/mm3 | 19.83 (3.73-105.48) | < 0.001 | NA | NA |
| Baseline CD4 T cell count ≥ 100 cells/mm3 | NA | NA | 2.61 (0.81-8.40) | 0.107 |
| CD4 slope ≥ 20/mm3/mon during 0−12 mon after HAART | 10.41 (3.32-32.61) | < 0.001 | 10.10 (3.06-33.30) | < 0.001 |
OR, odds ratio; CI, confidence interval; TMP/SMX, trimethoprim/sulfamethoxazole; NA, not applicable; HAART, highly active antiretroviral therapy.
Baseline CD4 T cell counts ≥ 200/mm3 (adjusted OR, 19.83; 95% CI, 3.73 to 105.48) and a CD4 slope ≥ 20 cells/mm3/month during 0 to 12 months (adjusted OR, 10.41; 95% CI, 3.32 to 32.61) were also independently associated with immunologic recovery (Table 3). Multivariate analysis of the 73 advanced HIV-infected patients with baseline CD4 T cell counts < 200/mm3, identified that independent predictors for immunologic recovery were an absence of OIs and a CD4 slope ≥ 20 cells/mm3/month during 0 to 12 months, but not a baseline CD4 T cell count ≥ 100/mm3 (Table 3).
DISCUSSION
HAART successfully suppressed HIV-1 replication and reduced HIV-associated morbidity and mortality [3]. However, in some patients, immunologic response after HAART was not adequate, despite their aviremic status. There is no definite consensus on the definition of non-responders, but generally, they are defined as patients with CD4 T cell counts < 500 cells/mm3 after 4 to 7 years of treatment, because CD4 T cell count of 500 cells/mm3 represents the lower limit of the physiological range [10,18]. In previous studies, 20% to 49.7% of patients receiving HAART did not achieve immunologic recovery [9,13-15,19,20]. This study showed that 42.2% (43/102) of patients were non-responders.
Our results also showed that trimethoprim/sulfamethoxazole (TMP/SMX) use was significantly less frequent in responders, but it was not an independent predictor for poor immunologic recovery in multivariate analysis (Table 3). Because TMP/SMX is primarily used for the prevention of Pneumocystis jirovecii pneumonia in patients with CD4 T cell counts < 200/mm3 and is taken until CD4 T cell counts reach and maintain > 200/mm3 [21], its use is more a consequence of poor immunologic recovery than a cause.
ZDV was previously a preferred and widely used choice for NRTI backbone, but ZDV is no longer recommended due to side effects including gastrointestinal intolerance, fatigue, and anemia [3]. In addition, ZDV may have a toxic effect to hematopoietic cells and could interrupt immunologic recovery [2]. In our results, most patients received ZDV-containing regimen, so there were no differences between responders and non-responders (Tables 1 and 2).
In the Australian HIV Observational Database, not having any prior AIDS-defined illness was a predictor of the time taken to achieve CD4 T cell counts > 500 cells/mm3 [16]. In this study, for all patients, OIs were more frequent in non-responders than in responders, but this was not statistically significant. However, in multivariate logistic regression analysis, OIs at the start of HAART were an independent predictive factor for immunologic recovery (adjusted OR, 0.28; 95% CI, 0.10 to 0.83; p = 0.022) (Table 3).
TB is an OI in HIV-infected patients, and it is known that treatment of TB before starting HAART, can lead to a slight increase in CD4 T cell counts [19,22]. In this study, few patients had TB (Tables 1 and 2) and the CD4 slope during 0 to 12 months of HAART was not significantly different between responders with TB and those without (data not shown, p = 0.658). Because HAART was initiated after a 2-month period of intensive TB treatment for these patients, it is conceivable that neither TB nor its treatment influenced the CD4 slope during the first year of HAART.
During the first phase of HAART, memory CD4 T cells sequestered within lymphoid tissues were redistributed into the peripheral blood. In the second and third phases, naïve CD4 T cells increased via production in the thymus [9,15,23,24]. Because thymic output is impaired in older patients, this represents a higher risk for reduced CD4 recovery than in younger patients [2,25]. In this study, however, age was not a predictive factor of immunologic recovery (Tables 1 and 2). This may be because the majority of patients were aged < 50 years. There were no differences in the CD4 slopes after 12 months of HAART (later phases) between responders and non-responders (Figs. 1 and 2), probably due to the similar age distribution in both groups.
In this study, we analyzed the CD4 slope during 0 to 12 months of HAART as a dichotomous categorical variable with a cutoff of 20 cells/mm3/month. In a previous study, failure to achieve a CD4 count increase > 100 cells/mm3 in 12 months on HAART is defined as immunologic failure [26]. However, because the objective of this study was to identify immunologic recovery in patients with virological suppression, we set the cutoff of CD4 slope during 0 to 12 months higher than in previous reports.
Within a group of similarly aged patients, the redistribution of memory CD4 T cells during the first phase would therefore be related to immunologic recovery, and the initial CD4 slope during the earlier phase of HAART could possibly be a predictor for this recovery. In this study, the CD4 slopes during 0 to 6 and 0 to 12 months were significantly higher in responders than in non-responders (Table 3, Figs. 1 and 2). These findings correspond with those in a previous study (the Swiss HIV Cohort Study), showing significant differences between the CD4 slopes of responders and non-responders [20].
Lower baseline CD4 T cell counts are associated with poor immunologic response [20,27]. In this study, the baseline CD4 T cell count was also a predictive factor for CD4 recovery in all 102 patients, but not in the 73 advanced patients with baseline CD4 T cell counts < 200/mm3. On the other hand, a CD4 slope ≥ 20/mm3/month at 0 to 12 months after HAART was a predictive factor for CD4 recovery in all patients, including the advanced HIV patients. Therefore, in patients with advanced HIV disease, a CD4 slope ≥ 20 cells/mm3/month during 0 to 12 months can be a better predictor for CD4 T cell recovery than a baseline CD4 T cell count. This result can be a useful indicator in countries where early diagnosis of HIV infection is not well-established due to limited resources, and where patients presenting with advanced HIV disease are common.
In conclusion, the CD4 slope can be calculated by linear regression with two or more CD4 T cell counts, enabling its use as a predictive factor for long-term immunologic recovery.
KEY MESSAGE
1. Opportunistic infections at the start of highly active antiretroviral therapy (HAART) and a CD4 slope ≥ 20 during 0 to 12 months of HAART were independently associated with immunologic recovery.
2. The CD4 slope can be a predictor of immunologic recovery in advanced human immunodeficiency virus patients.
Footnotes
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Joint United Nations Programme on HIV/AIDS (UNAIDS) The Gap Report. Geneva: Joint United Nations Programme on HIV/AIDS; 2014. [PubMed] [Google Scholar]
- 2.Corbeau P, Reynes J. Immune reconstitution under antiretroviral therapy: the new challenge in HIV-1 infection. Blood. 2011;117:5582–5590. doi: 10.1182/blood-2010-12-322453. [DOI] [PubMed] [Google Scholar]
- 3.Panel on Antiretroviral Guidelines for Adults and Adolescents . Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents [Internet] Rockville (MD): AIDSinfo; 2015. [cited 2015 Jul 6]. Available from: http://aidsinfo.nih.gov/ContentFiles/AdultandAdolescentGL.pdf. [Google Scholar]
- 4.Broder S. The development of antiretroviral therapy and its impact on the HIV-1/AIDS pandemic. Antiviral Res. 2010;85:1–18. doi: 10.1016/j.antiviral.2009.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chun TW, Stuyver L, Mizell SB, et al. Presence of an inducible HIV-1 latent reservoir during highly active antiretroviral therapy. Proc Natl Acad Sci U S A. 1997;94:13193–13197. doi: 10.1073/pnas.94.24.13193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chun TW, Engel D, Berrey MM, Shea T, Corey L, Fauci AS. Early establishment of a pool of latently infected, resting CD4(+) T cells during primary HIV-1 infection. Proc Natl Acad Sci U S A. 1998;95:8869–8873. doi: 10.1073/pnas.95.15.8869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guihot A, Tubiana R, Breton G, et al. Immune and virological benefits of 10 years of permanent viral control with antiretroviral therapy. AIDS. 2010;24:614–617. doi: 10.1097/QAD.0b013e32833556f3. [DOI] [PubMed] [Google Scholar]
- 8.Autran B, Carcelaint G, Li TS, et al. Restoration of the immune system with anti-retroviral therapy. Immunol Lett. 1999;66:207–211. doi: 10.1016/s0165-2478(98)00159-x. [DOI] [PubMed] [Google Scholar]
- 9.Guihot A, Bourgarit A, Carcelain G, Autran B. Immune reconstitution after a decade of combined antiretroviral therapies for human immunodeficiency virus. Trends Immunol. 2011;32:131–137. doi: 10.1016/j.it.2010.12.002. [DOI] [PubMed] [Google Scholar]
- 10.Kaufmann GR, Perrin L, Pantaleo G, et al. CD4 T-lymphocyte recovery in individuals with advanced HIV- 1 infection receiving potent antiretroviral therapy for 4 years: the Swiss HIV Cohort Study. Arch Intern Med. 2003;163:2187–2195. doi: 10.1001/archinte.163.18.2187. [DOI] [PubMed] [Google Scholar]
- 11.Tsukamoto H, Clise-Dwyer K, Huston GE, et al. Age-associated increase in lifespan of naive CD4 T cells contributes to T-cell homeostasis but facilitates development of functional defects. Proc Natl Acad Sci U S A. 2009;106:18333–18338. doi: 10.1073/pnas.0910139106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Viard JP, Mocroft A, Chiesi A, et al. Influence of age on CD4 cell recovery in human immunodeficiency virus-infected patients receiving highly active antiretroviral therapy: evidence from the EuroSIDA study. J Infect Dis. 2001;183:1290–1294. doi: 10.1086/319678. [DOI] [PubMed] [Google Scholar]
- 13.Egger M, May M, Chene G, et al. Prognosis of HIV-1-infected patients starting highly active antiretroviral therapy: a collaborative analysis of prospective studies. Lancet. 2002;360:119–129. doi: 10.1016/s0140-6736(02)09411-4. [DOI] [PubMed] [Google Scholar]
- 14.Nicastri E, Chiesi A, Angeletti C, et al. Clinical outcome after 4 years follow-up of HIV-seropositive subjects with incomplete virologic or immunologic response to HAART. J Med Virol. 2005;76:153–160. doi: 10.1002/jmv.20352. [DOI] [PubMed] [Google Scholar]
- 15.Lawn SD, Myer L, Bekker LG, Wood R. CD4 cell count recovery among HIV-infected patients with very advanced immunodeficiency commencing antiretroviral treatment in sub-Saharan Africa. BMC Infect Dis. 2006;6:59. doi: 10.1186/1471-2334-6-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rajasuriar R, Gouillou M, Spelman T, et al. Clinical predictors of immune reconstitution following combination antiretroviral therapy in patients from the Australian HIV Observational Database. PLoS One. 2011;6: doi: 10.1371/journal.pone.0020713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Havlir DV, Bassett R, Levitan D, et al. Prevalence and predictive value of intermittent viremia with combination hiv therapy. JAMA. 2001;286:171–179. doi: 10.1001/jama.286.2.171. [DOI] [PubMed] [Google Scholar]
- 18.Kelley CF, Kitchen CM, Hunt PW, et al. Incomplete peripheral CD4+ cell count restoration in HIV-infected patients receiving long-term antiretroviral treatment. Clin Infect Dis. 2009;48:787–794. doi: 10.1086/597093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.1993 Revised classification system for HIV infection and expanded surveillance case definition for AIDS among adolescents and adults. MMWR Recomm Rep. 1992;41(RR-17):1–19. [PubMed] [Google Scholar]
- 20.Kaufmann GR, Furrer H, Ledergerber B, et al. Characteristics, determinants, and clinical relevance of CD4 T cell recovery to <500 cells/microL in HIV type 1-infected individuals receiving potent antiretroviral therapy. Clin Infect Dis. 2005;41:361–372. doi: 10.1086/431484. [DOI] [PubMed] [Google Scholar]
- 21.Panel on Opportunistic Infections in HIV-Infected Adults and Adolescents . Guidelines for the prevention and treatment of opportunistic infections in HIV-infected adults and adolescents [Internet] Rockville (MD): AIDSinfo; 2015. [cited 2015 Jul 6]. Available from: http://aidsinfo.nih.gov/contentfiles/lvguidelines/adult_oi.pdf. [Google Scholar]
- 22.Morris L, Martin DJ, Bredell H, et al. Human immunodeficiency virus-1 RNA levels and CD4 lymphocyte counts, during treatment for active tuberculosis, in South African patients. J Infect Dis. 2003;187:1967–1971. doi: 10.1086/375346. [DOI] [PubMed] [Google Scholar]
- 23.Autran B, Carcelain G, Li TS, et al. Positive effects of combined antiretroviral therapy on CD4+ T cell homeostasis and function in advanced HIV disease. Science. 1997;277:112–116. doi: 10.1126/science.277.5322.112. [DOI] [PubMed] [Google Scholar]
- 24.Carcelain G, Debre P, Autran B. Reconstitution of CD4+ T lymphocytes in HIV-infected individuals following antiretroviral therapy. Curr Opin Immunol. 2001;13:483–488. doi: 10.1016/s0952-7915(00)00245-4. [DOI] [PubMed] [Google Scholar]
- 25.Pido-Lopez J, Imami N, Aspinall R. Both age and gender affect thymic output: more recent thymic migrants in females than males as they age. Clin Exp Immunol. 2001;125:409–413. doi: 10.1046/j.1365-2249.2001.01640.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hoffmann CJ, Schomaker M, Fox MP, et al. CD4 count slope and mortality in HIV-infected patients on antiretroviral therapy: multicohort analysis from South Africa. J Acquir Immune Defic Syndr. 2013;63:34–41. doi: 10.1097/QAI.0b013e318287c1fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kaufmann GR, Bloch M, Finlayson R, Zaunders J, Smith D, Cooper DA. The extent of HIV-1-related immunodeficiency and age predict the long-term CD4 T lymphocyte response to potent antiretroviral therapy. AIDS. 2002;16:359–367. doi: 10.1097/00002030-200202150-00007. [DOI] [PubMed] [Google Scholar]


