Abstract
Purpose:
Neck of Femur (NOF) fracture is a common injury with high mortality that all orthopaedic departments must contend with [1]. The aim of this study was to report incidence and mortality of NOF fractures occurring while patients were being admitted to hospital for other conditions.
Methods:
A retrospective review was performed of all NOF fracture admissions between 1st of Jan 2010 to 31st of Dec 2012 at a University Hospital trauma centre. Fractures were divided according to the location where the fracture occurred, either in the community (acute NOF) or in-hospital (in-hospital NOF).
Results:
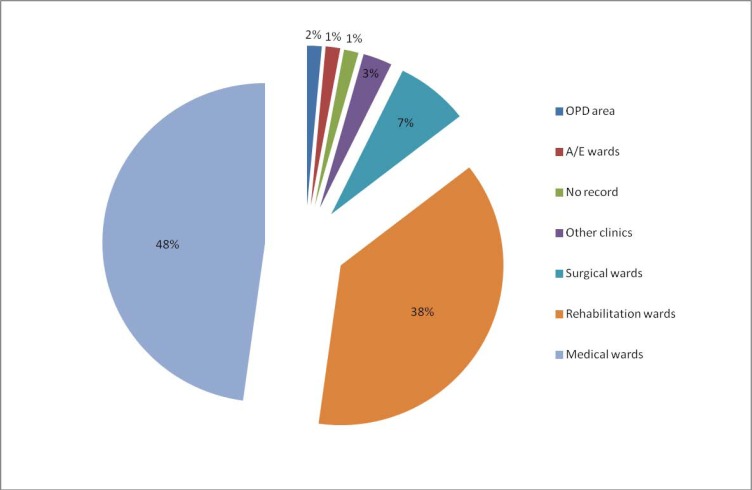
In-hospital mortality, 30-day, 90-day and 1 year mortality were recorded. There were 1086 patients in the acute NOF fracture group (93.9%) and 70 patients in the in-hospital group (6.1%) over three years. The odds of inpatient death was 2.25 times higher for inpatient NOFs (p=0.012). 86% of all in-hospital NOF fractures occurred on medical and rehabilitation wards. NOF fractures result in increased mortality and morbidity.
Conclusion:
All patients in hospital should be assessed to identify those at high risk of falls and implemented measures should be taken to reduce this.
Keywords: ASA grade, hospital fractures, mortality, neck of femur fracture
INTRODUCTION
A neck of femur (NOF) fracture is a common injury with high mortality that all orthopaedic departments must contend with [1]. There are 75,000 NOF fractures a year, costing the NHS £2 billion annually. The mortality of patients sustaining a NOF fracture is reported to be 10% at 30 days and 30% at 1 year post operatively [2]. There are many factors that can affect mortality following a NOF fracture which include gender, time for surgery and age [3]. Though the majority of NOF fractures occur within the community, there are incidences of in-patient NOFs, and the differences between these groups of patients lead to significantly different outcomes. Existing research carried out by Hamilton et al. shows an increased mortality for patients who suffered their NOF fracture as an in-patient. It also noted a longer mean waiting time for surgery and increased in-patient stay [4, 5]. This same study highlighted that the reasons for admission of patients who suffered in-patient NOFs were recurrent falls/confusion, cardiac disease and stroke. Another study highlighted that in-patient NOF fractures make up 7% of all NOF fractures and showed that patients with this type of injury are usually more medically unfit pre-operatively, which raises both the length of stay post-operatively and the mortality [6]. It was also noted that in-patient NOF fractures had a significantly longer delay to surgery and that post-operatively they were swiftly transferred from surgical wards specialising in NOF fracture rehabilitation to the ward the patients were originally from, in spite of the fact that the wards did not require any further active treatment or diagnostics to be performed on these patients at the time of their injury, and that their care should have been focussed NOF fracture post-surgical rehabilitation [6]. It was found in an analysis of 2 million patients that a NOF fracture occurring as a complication of admission was 6 times higher on general medical wards than on post-surgical wards, and that the main consequence of this was a doubly long length of stay and cost of admission and a tripled mortality. As with other studies previously mentioned, it was noted that these injuries occurred mostly in elderly medical wards with fragile, cognitively impaired patients with multiple co-morbidities, frequent risk factors being the presence of dementia, delirium or confusional syndrome and malnutrition [7]. An aside to this were those patients living in assisted living housing were almost twice as likely to sustain NOF fractures compared to patients of the same age living in their own residence, and that those who lived in assisted living had greater co-morbidities such as chronic illness, cognitive and visual impairment, frailty and polypharmacy [7-9]. Although the increased mortality of in-patient NOF has been clearly demonstrated, it was also seen that after discharge, there was a higher rate of referral to social care providers and a reduction in activities of daily living compared to pre-fracture states [10]. The aim of this study was to report the incidence and mortality of NOF fractures occurring while patients are being admitted for other medical conditions, and given the reasons mentioned above consider what can be done in order to target these patients and prevent falls or how to best optimise treatment after in-patient NOFs.
METHOD
This study was a retrospective review of referrals and admissions of all NOF fractures between 1st of January 2010 to 31st of December 2012 at a University Hospital. Case notes and X-rays (reported by radiologist) were reviewed and analysed by MM and MB. Patient demographics were documented which included age, gender, side of injury, American Society for Anaesthesiologist (ASA) grade and Abbreviated Mental Test (AMT). Patients were in two categories; Acute NOF fracture patient group, in which the injury occurred outside the hospital, and the In-hospital NOF fracture group in which the injury occurred while the patient was admitted and being an in-patient for other medical conditions. Surgical data regarding the classification of the injury, the type of fracture, the type of operation and pre-injury mobility status was also collected. In the in-hospital group, the type of ward (i.e. medical, surgical, or rehabilitation ward) in which the injury occurred was also documented. The in-hospital mortality, 30-day, 90-day and 1 year mortality were also recorded. Following discharge, patients are normally contacted by a specialist nurse practitioner to enquire on progress of patients (whether they have been discharged to their own home or other destinations; if they were referred to a rehabilitation ward or an external hospital and mortality recorded if so).
Statistical analysis was performed using STATA12. Data was tested for normality of distribution using the skewness-kurtosis test. Comparison between groups was performed using chi-squared, Student’s t-test and Mann-Whitney U test for categorical, parametric and non-parametric data, respectively. Univariable logistic regression was performed to assess predictors of mortality outcomes. Age and gender adjusted logistic regression was used to assess whether mortality outcomes were different between in-patient and acute NOF fractures.
RESULTS
A total of 1156 patients with NOF fractures were identified and referred to the department for treatment in the study period. There were 1086 patients in the acute NOF fracture admissions group (93.9%) and 70 in the in-hospital NOF fracture group (6.1%). Over the three year period, the mean number of NOF fractures, a year was 385 and of these approximately 23 were in-hospital NOF fractures. The demographics of both groups are shown in Table 1. The mean age for acute NOF fractures was 78.3 years compared to 80.5 years for in-hospital NOF patients with no statistical difference. There was a statistically higher number of females in the acute admissions. The mean ASA grade was significantly higher in the in-hospital group (3.3 vs 2.8. P<0.001). The Abbreviated Mental Test (AMT) between groups was not significantly different.
Table 1.
Demographics table.
| Acute NOFs | In-Patients NOFs | P-Value | ||
|---|---|---|---|---|
| Mean Age (±sd) | 78.3 ± 11.6 | 80.5 ± 11.2 | 0.128 | |
| Gender | Male | 317 (29.2%) | 33 (47.1%) | 0.002 |
| Female | 769 (70.8%) | 37 (52.9%) | ||
| Side | Right | 507 | 30 | 0.534 |
| Left | 579 | 40 | ||
| ASA | Mean | 2.8 ± 0.7 | 3.3 ± 0.7 | <0.001 |
| 1 | 38 (3.6%) | 1 (1.5%) | ||
| 2 | 248 (23.4%) | 4 (6.2%) | ||
| 3 | 628 (59.2%) | 36 (55.4%) | ||
| 4 | 145 (13.7%) | 23 (35.4%) | ||
| 5 | 2 (0.2%) | 1 (1.5%) | ||
| Unknown | 25 | 5 | ||
| Walking Indoor | One aid | 210 (19.3%) | 21 (30%) | |
| Two aids or frame | 230 (21.2%) | 26 (22.1%) | ||
| Without aids | 606 (55.8%) | 15 (21.4%) | ||
| Unknown | 9 (0.8%) | 6 (8.6%) | ||
| Wheelchair or bedbound | 31 (2.9%) | 2 (2.9%) | ||
| Walking outdoors | One aid | 180 (16.6%) | 16 (22.9%) | |
| Two aids or frame | 113 (10.4%) | 7 (10%) | ||
| Without aids | 489 (24%) | 11 (15.7%) | ||
| Unknown | 43 (4%) | 15 (21.4%) | ||
| Wheelchair or bedbound | 163 (15%) | 9 (12.9%) | ||
| Never goes outdoors | 91 (8.4%) | 11 (15.7%) | ||
| Electric buggy | 7 (0.6%) | 0 | ||
| Median AMT (IQR) | 7.8 ± 3.4 | 7.3 ± 3.5 | p=0.333 | |
SD: standard deviation; IQR: interquartile range.
There was no difference between groups in the classification of fracture but the in-hospital group had a higher number of pathological fractures compared to the acute NOF fracture group (Table 2). The in-hospital NOF fracture group was less mobile in-doors using one or two walking sticks compared to the acute NOF fracture group.
Table 2.
Surgical details for both groups.
| Acute NOFs | In-patients NOFs | ||
|---|---|---|---|
| Time from admission to NOF # (median) | n/a | 16.3 (0.45 to 89.24 ) | |
| Time to surgery (hours) | 25.5 (3.83 to 147.4 ) | 26.6 (2.35 to 156.5 ) | |
| Classification of fracture | InterTroch | 443 | 26 |
| IC- displaced | 469 | 31 | |
| IC- undisplaced | 108 | 8 | |
| Sub T | 66 | 5 | |
| Type of operation | DHS | 388 | 27 |
| CHS | 82 | 5 | |
| Cemented hemi | 374 | 22 | |
| Uncemented hemi | 15 | 3 | |
| IM nail (long) | 83 | 4 | |
| IM nail (short) | 48 | 1 | |
| THR (uncemented) | 1 | 0 | |
| THR (cemented) | 60 | 2 | |
| Bipolar hemi (cemented) | 3 | 0 | |
| Bipolar hemi (uncemented) | 10 | 0 | |
| No operation | 15 (1.4%) | 5 (7.1%) | |
| Other | 7 | 1 | |
| Type of fracture | Pathological | 18 (1.6%) | 4 (5.7%) |
| Traumatic | 1066 (98.2%) | 66 (94.2%) | |
| Unknown | 2 | 0 | |
The type of operation patients received was not statistically different between groups. However, the number of patients not being operated due to poor medical condition was higher in the in-hospital NOF fracture group. In-hospital NOF fracture patients were in hospital for a mean of 16.3 days before sustaining their injury (range 0.5 to 89.2 days). The median time of length of stay post-surgery was 17.8 days (range 0.2-157.6 days) for acute NOF fracture and 27 days (0.6-107.5 days) for in-patient NOF fracture (p=0.008).
In univariable logistic regression ASA grade and fracture type were not associated with mortality outcomes. Age was significantly associated with all outcomes of mortality as expected. Age and gender adjusted logistic regression showed that the odds of mortality outcomes were significantly increased in the inpatient NOFs (Table 4). The odds of inpatient mortality was 2.25 times higher for inpatient compared to acute NOFs. Similarly, odds of 90-day and 1 year mortality were approximately 1.8 times higher for inpatient NOFs. Odds ratios were not significantly changed when adjusted for AMTS and the presence of pathological fractures (data not shown).
Table 4.
Age and gender adjusted logistic regression for inpatient compared to acute neck of femur fractures.
| Inpatient vs Acute NOF | Odds Ratio | 95% Confidence Interval | P-Value |
|---|---|---|---|
| Inpatient death | 2.25 | 1.19 - 4.26 | 0.012 |
| 30-day | 1.63 | 0.77 - 3.45 | 0.200 |
| 90-day | 1.83 | 1.02 - 3.29 | 0.043 |
| 1-year | 1.87 | 1.11 - 3.13 | 0.018 |
Ninety two patients (8.5%) in the acute NOF fracture group died whilst being an in-patient compared to 14 patients (20%) in the other group (p=0.001) (Table 3). The 90-day and 1 year mortality rate was significantly higher in the in-hospital NOF fracture group (p=0.014 and 0.006, respectively). In addition 86% of all in-hospital NOF fractures occurred on medical and rehabilitation wards.
Table 3.
NOF mortality.
| Acute NOFs | In-Patients NOFs | P-Value | ||
|---|---|---|---|---|
| Mortality | In-hospital mortality | 92 (8.5%) | 14 (20%) | 0.001 |
| 30-day mortality | 73 (6.7%) | 8 (11.4%) | 0.135 | |
| 90-day mortality | 137 (12.6%) | 16 (22.6%) | 0.014 | |
| 1 year mortality | 234 (21.5%) | 25 (35.7%) | 0.006 | |
| Medain LOS post-surgery (range) | 17.8 (0.2 to 157.6) | 27 (0.6 to 107.5) | 0.008 | |
DISCUSSION
Comparison of community NOF fractures and in-hospital NOF fractures mortality shows that on the whole, a worse outcome is associated with in-hospital NOF fractures. The in-hospital mortality of an acute NOF fracture was 8.5%, compared to 20% for in-patient NOF. The odds of inpatient mortality was 2.25 times higher for inpatient NOFs, adjusted for age and gender. The odds were similarly raised for 90-days and 1 year mortality. The in-hospital NOF fracture group also remained in hospital longer post-operatively. This suggests a worse outcome for NOF fractures that occur during in-patient stays than those that occur acutely within the community. A limitation within this study is that it does not compare like type of fractures or like types of fixation methods. However we have enough evidence from our existing studies to suggest there is a greater mortality for in-patient NOF fractures.
In the study by Hamilton et al., the mean age of patients with in-patient NOF fractures was 84.1 compared to our 80.5, and the percentage of patients who sustained a fracture as an in-patient was 4% compared to our 6.1%. The mortality figures from our study are lower than that quoted in other literature; mortality at 30 days, 90 days and 1 year were 11.4%, 22.6% and 35.7% respectively for our in-patient NOF fractures. The potential reasons for this are that the mean waiting time for surgery for all patients who required it was 25.5 and 26.6 hours for community NOF fractures and in-patient NOF fractures respectively compared to 2.29 days in Hamilton et al. It was noted by Green et al. that the most common cause of delay for surgery was obtaining a medical review pre-operatively, with 87.5% of their in-patient NOF fractures being reviewed by an orthogeriatrician [11]. Because this study took place at a trauma centre with a dedicated orthogeriatrician service it meant that all patients were reviewed and optimised pre-operatively before surgery. Also all NOF fracture patients were started on an enhanced recovery program lead by physiotherapists as part of a multi-disciplinary team approach to encourage post-op rehabilitation as fast possible to reduce chances of hospital acquired pneumonia, pulmonary emboli and other post-operative complications.
The post-operative length of stay for this group of patients was also found to be increased. We found in our study that 48% of falls occurred on medical wards and 38% of falls occurred on geriatric/elderly medicine/rehab wards (Fig. 1). Noting the reasons for admission for in-patient NOF fractures in Hamilton et al., a point to be noted is that patients admitted with recurrent falls, confusion and strokes would be sent to elderly medicine/rehab wards, which is the second most common location for falls to occur in our study. Again, it has been noted in the literature that medical and rehabilitation wards are the common areas for in-patient falls to occur with 77.5% occurring there [12]. This shows the need to be more vigilant regarding NOF fracture prevention on the wards stated above; one study showed that none of the patients who suffered an in-patient NOF fracture had any preventative measures taken prior to their injury despite a history of falls in half of these patients and even a fall during their current admission for a third of these patients [7]. The prevalence of this finding should alert NHS trusts to realise that this is a nationwide issue which affects a range of trusts from district general hospitals to trauma centres and should be a catalyst for promoting more rigorous falls prevention and assessment methods on these wards. With regards to NOF fracture prevention, the interventions can be broadly separated into falls prevention and fracture prevention. Falls prevention assessment tools have been shown to be predictive and useful to identify high risk patients [13, 14]. While data on fracture prevention through the use of external hip protectors is not definitive, with no clear evidence of reducing fractures through their usage noted [15, 16], reviews have shown that implementing fall prevention can reduce the incidence of falls; despite there being no clear number in the reduction of falls it is still considered best practice to implement falls prevention programmes for in-patients at risk of falls [17-19].
Fig. (1).
Wards where the in-hospital NOF fracture occurred.
Our study also collected data regarding several other variables as mortality needs to be considered as a multi-factorial event. The mobility of patients who suffered NOF fractures was collected. This shows that the acute NOF fracture group is more mobile both in-doors and out-doors compared to the in-hospital NOF fracture group where a higher proportion of patients (15.7% compared to 8.4%) never goes out-doors. Though it is ultimately only an inference, these differences in mobility indicate that patients who suffered a NOF fracture in the community had fewer mobility issues than in-patient NOF fracture patients. The implication behind this is that a reduced mobility or difficulty mobilising makes those patients more prone to falls and thus injury. Studies regarding co-morbidities and their effect on in-patient NOF fractures have found that patients who suffer falls in hospital tend to be frailer and have impaired cognitive functions with greater co-morbidity, which cumulatively results in worse outcomes and raised mortality, a finding mirrored by our data. This same study also found, like ours, that most falls occurred in elderly patient wards and stressed on importance of fall prevention in these wards [20].
CONCLUSION
NOF fractures will continue to result in an increase in mortality and morbidity within patients. NOF fractures associated with patients already in hospital have been associated with an increase in mortality. These patients are typically older, higher ASA grades and have prolonged hospital stays. More has to be done to identify patients when admitted to hospital to identify those at risk of falls and measures implemented to reduce the number of these in hospital NOF fractures, which can be done in part by looking at their baseline mobility and co-morbidities. All patients who require NOF fracture surgery should be optimised by an orthogeriatrician team before their surgery to reduce post-operative mortality due to medical management of co-morbidities. Hospital should take an active role auditing which ward a fall occurred on and a NOF fracture occurs. Following this a root course analyses should take place in order to identify any factors which may have contributed to the fall and measure implemented to prevent these from occurring in the future.
ACKNOWLEDGEMENTS
All contribution in this manuscript was solely by the listed authors and no funding was required for this research. There are no conflicts of interest and there are no financial disclosures to be made from the authors for this manuscript.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
REFERENCES
- 1.Keene G.S., Parker M.J., Pryor G.A. Mortality and morbidity after hip fractures. BMJ. 1993;307(6914):1248–1250. doi: 10.1136/bmj.307.6914.1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.NICE NICE: National Institute for Health and Care Excellence [Internet]. [cited 2014 May 05]; Available from: http://guidance.nice.org.uk/CG124/NICEGuidance/pdf/English .
- 3.Casaletto J.A., Gatt R. Post-operative mortality related to waiting time for hip fracture surgery. Injury. 2004;35(2):114–120. doi: 10.1016/S0020-1383(03)00210-9. [DOI] [PubMed] [Google Scholar]
- 4.Hamilton P.D., Whelan A., Isaacs D., Mestha P., Armitage A., Skyrme A. Increased mortality among patients sustaining hip fractures requiring surgery in a district general hospital. Hip Int. 2007;17(3):160–163. doi: 10.1177/112070000701700307. [DOI] [PubMed] [Google Scholar]
- 5.Zapatero A., Barba R., Canora J., Losa J.E., Plaza S., San Roman J., Marco J. Hip fracture in hospitalized medical patients. BMC Musculoskelet. Disord. 2013;14:15. doi: 10.1186/1471-2474-14-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Foss N.B., Palm H., Kehlet H. In-hospital hip fractures: prevalence, risk factors and outcome. Age Ageing. 2005;34(6):642–645. doi: 10.1093/ageing/afi198. [DOI] [PubMed] [Google Scholar]
- 7.Chen J.S., Sambrook P.N., Simpson J.M., Cameron I.D., Cumming R.G., Seibel M.J., Lord S.R., March L.M. Risk factors for hip fracture among institutionalised older people. Age Ageing. 2009;38(4):429–434. doi: 10.1093/ageing/afp051. [DOI] [PubMed] [Google Scholar]
- 8.Butler M., Norton R., Lee-Joe T., Cheng A., Campbell A.J. The risks of hip fracture in older people from private homes and institutions. Age Ageing. 1996;25(5):381–385. doi: 10.1093/ageing/25.5.381. [DOI] [PubMed] [Google Scholar]
- 9.Norton R., Campbell A.J., Reid I.R., Butler M., Currie R., Robinson E., Gray H. Residential status and risk of hip fracture. Age Ageing. 1999;28(2):135–139. doi: 10.1093/ageing/28.2.135. [DOI] [PubMed] [Google Scholar]
- 10.Murray G.R., Cameron I.D., Cumming R.G. The consequences of falls in acute and subacute hospitals in Australia that cause proximal femoral fractures. J. Am. Geriatr. Soc. 2007;55(4):577–582. doi: 10.1111/j.1532-5415.2007.01102.x. [DOI] [PubMed] [Google Scholar]
- 11.Green C.M., Zeiton M., Foulkes K., Barrie J. The inpatient fracture neck of femur: an important subgroup of patients. Injury. 2014;45(12):1946–1949. doi: 10.1016/j.injury.2014.09.022. [DOI] [PubMed] [Google Scholar]
- 12.Green C.M., Zeiton M., Foulkes K., Barrie J. Acute fracture neck of femur among inpatients: severe injuries which need to be taken seriously. J Patient Saf. 2015 doi: 10.1097/PTS.0000000000000193. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 13.Perell K.L., Nelson A., Goldman R.L., Luther S.L., Prieto-Lewis N., Rubenstein L.Z. Fall risk assessment measures: an analytic review. J. Gerontol. A Biol. Sci. Med. Sci. 2001;56(12):M761–M766. doi: 10.1093/gerona/56.12.M761. [DOI] [PubMed] [Google Scholar]
- 14.Vassallo M., Stockdale R., Sharma J.C., Briggs R., Allen S. A comparative study of the use of four fall risk assessment tools on acute medical wards. J. Am. Geriatr. Soc. 2005;53(6):1034–1038. doi: 10.1111/j.1532-5415.2005.53316.x. [DOI] [PubMed] [Google Scholar]
- 15.Parker M.J., Gillespie L.D., Gillespie W.J. Hip protectors for preventing hip fractures in the elderly. Cochrane Database Syst. Rev. 2004;3(3):CD001255. doi: 10.1002/14651858.CD001255.pub2. [DOI] [PubMed] [Google Scholar]
- 16.O’Halloran P.D., Cran G.W., Beringer T.R., Kernohan G., O’Neill C., Orr J., Dunlop L., Murray L.J. A cluster randomised controlled trial to evaluate a policy of making hip protectors available to residents of nursing homes. Age Ageing. 2004;33(6):582–588. doi: 10.1093/ageing/afh200. [DOI] [PubMed] [Google Scholar]
- 17.Gillespie L.D., Gillespie W.J., Robertson M.C., Lamb S.E., Cumming R.G., Rowe B.H. Interventions for preventing falls in elderly people. Cochrane Database Syst. Rev. 2003;4(4):CD000340. doi: 10.1002/14651858.CD000340. [DOI] [PubMed] [Google Scholar]
- 18.Guideline for the prevention of falls in older persons. American Geriatrics Society, British Geriatrics Society, and American Academy of Orthopaedic Surgeons Panel on Falls Prevention. J. Am. Geriatr. Soc. 2001;49(5):664–672. [PubMed] [Google Scholar]
- 19.Haines T.P., Bennell K.L., Osborne R.H., Hill K.D. Effectiveness of targeted falls prevention programme in subacute hospital setting: randomised controlled trial. BMJ. 2004;328(7441):676. doi: 10.1136/bmj.328.7441.676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Johal K.S., Boulton C., Moran C.G. Hip fractures after falls in hospital: a retrospective observational cohort study. Injury. 2009;40(2):201–204. doi: 10.1016/j.injury.2008.06.036. [DOI] [PubMed] [Google Scholar]