Abstract
Background:
Lithium disilicate ceramic system consists of glass ceramic ingots with different grades of translucence which may influence its flexural strength.
Aims:
To assess the three-point flexural strength of the different lithium disilicate-based ceramic ingots (IPS e.max Press/Ivoclar Vivadent) with different levels of translucence and shade.
Materials and Methods:
Six groups of ceramic ingots were selected to represent different levels of translucence and shade (HTA1, HTBL2, LTA2, LTB2, MO2, and HO). They measured 25 mm × 5 mm × 2 mm (n = 10), according to ISO 6872 specifications, and tested on a universal test machine (EMIC).
Statistical Analysis Used:
A one-way analysis of variance (ANOVA) was used (α = 0.05).
Results:
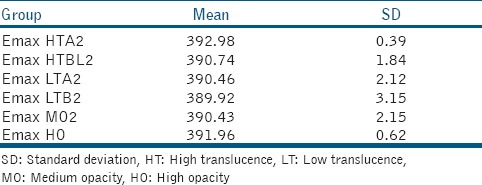
The results (in MPa) were: HTA1 = 392.98; HTBL2 = 390.74; LTA2 = 390.46; LTB2 = 389.92; MO2 = 390.43; HO = 391.96. ANOVA showed no significant difference among groups (P = 0.1528).
Conclusions:
Different levels of translucence, opacity and shade of ingots did not affect their mechanical strength, and the use of these ceramics should be guided by the esthetic demands of each clinical situation.
Keywords: Ceramics, compressive strength, lithium compounds
INTRODUCTION
The new ceramic systems have provided esthetic quality in terms of translucence. With increased translucency, light is able to pass the surface and is scattered within the restoration. Optically, the translucent materials usually are more esthetic than the layered and opaque materials. By the use of different ceramic translucencies, the restoration can match the enamel variations of patients' age, surface luster, and level of dehydration.[1,2,3,4]
IPS e.max Press is one of the lithium disilicate systems which is susceptible to acid etching, and shows excellent mechanical properties, but above all, high esthetic quality.[3,5] One example of such technology is the IPS e.max system (Ivoclar Vivadent), which is available in the form of ingots (IPS e.max Press)[6] that present different grades of translucence, opacity and shade.[6,7] Four translucence and opacity options are available (ingots of high translucence [HT], low translucence [LT], medium opacity [MO], and high opacity [HO]) and each of them presents a variety of shades, as well as a specific shade scale for each type of pressed ceramic ingot, therefore allowing the selection of an ideal shade with the patient.[7] The HT ingots are recommended for small restorations (inlays, onlays, and veneers), whereas the LT ingots are ideal to conduct restorations based on make-up and “cut-back” techniques. These consist of customization of restorations at the incisal edge, leading to a reduction in the area to achieve final stratification and highly esthetic restorations. MO and HO ingots are used for lightly discolored vital teeth or severely discolored nonvital teeth, or for masking metal posts, respectively.[7]
The higher the opacity the higher the quantity of oxides or pigments in the crystalline phase of dental ceramics,[8] which could enhance their flexural strength,[9] despite a lack of microstructural differences in their composition.[7,8] Restorations with adequate flexural strength can be used in areas of high mastication forces, such as fixed bridges of up to three units, without the need for a metal framework. In addition, individual crowns in posterior teeth can be fitted with adhesive systems.[10] The IPS Empress 2 lithium disilicate ceramic system has a flexural strength of 350 MPa,[11] and some authors believe that the addition of lithium orthodisilicate, in higher density and lower size compared to Empress 1, gives the IPS e.max Press system higher the flexural strength (approximately 400 MPa) for all ingots.[12,13] However, there have been no studies investigating grades of translucence, opacity, and ingot shade with flexural strength. Therefore, the aim of this study was to assess the flexural strength of lithium disilicate ceramic ingots according to the different grades of translucence/opacity and shade (HTA2, HTBL2, LTA2, LTB2, MO2, and HO). The null hypothesis was that there was no difference in flexural strength among ceramic ingots of different translucence/opacity and shades.
MATERIALS AND METHODS
Experimental design
Sixty lithium disilicate bars were made and randomly distributed in groups (n = 10), according to the number of variables in the study. The variables were the grade of translucence/opacity and ceramic shade, in 6 levels:
HTA2: HT ceramic, shade A2 (IPS e.max Press HT A2).
HTBL2: HT ceramic for bleached teeth, shade 2 (IPS e.max Press HT BL2).
LTA2: LT ceramic, shade A2 (IPS e.max Press LT A2).
LTB2: LT ceramic, shade B2 (IPS e.max Press LT B2).
MO2: MO ceramic, shade 2 (IPS e.max Press MO 2).
HO: HO ceramic (IPS e.max Press HO).
Flexural strength was assessed quantitatively in MPa.
Test specimen preparation
Pressed lithium disilicate ceramic (IPS e.max Press, Ivoclar Vivadent AG, Schaan, Liechtenstein, Germany) was used, containing SiO2 with additional Li2O, K2O, MgO, ZnO2, Al2O3, P2O5, and other oxides. Six combinations were selected, which presented different grades of translucence/opacity/shades, based on those most used in dental studies, where two were HT (HTA2 and HTBL2), two were LT (LTA2 and LTB2), one MO (MO2) and one HO (Ivoclar Vivadent AG, 2009).
For each grade of translucence/opacity/shade of the ceramic ingots, 10 test specimens were made in the shape of a 25 mm × 5 mm × 2 mm bar, according to ISO 6872 guidelines.
The test specimens were obtained via lost wax casting. Models of the test specimens were made in “blender,” an open-source language software. The file was then transferred onto “nesting,” the running software of the milling unit. With the finalized CNC file, the specimens were built in wax using the computer-aided design and computer-aided manufacturing system (Zirkonzahn, Talmax, Italy). Wax sprue guides were positioned and fixed onto the ring base provided by the manufacturer. The investment was carried out using IPS Press VEST Speed Investment (Ivoclar Vivadent AG, Schaan, Liechtenstein, Germany) for day use. The material was prepared in a vacuum mixer (Elite Mix, Zhermack Technical, Italy) for 40 s. A silicone ring with its specific ring gauge was used for this purpose. The investment ring (IPS Silicone Ring, Ivoclar Vivadent AG, Schaan, Liechtenstein, Germany) was carefully positioned over its base and filled with investment material respecting the manufacturer's guiding marks. The ring gauge was rotated into place. The investment was left untouched to set for 30–45 min.
The set-up was placed in a preheated furnace at 850°C (Forno de Anel F3000 3P Microprocessado, EDG, Sao Paulo, Brazil) to eliminate the wax and expand the mold. The ceramic ingots and the plunge shaft were not preheated.
The ceramic ingot was positioned over the sprues of the investment ring set and placed in the furnace (EP-500, Ivoclar Vivadent AG, Schaan, Liechtenstein, and Germany). It was heated automatically at a rate of 60°C per minute to an initial temperature of 700°C and up to 920°C, maintaining it for 20 min. At the end of this cycle, with the ingot already plasticized, the ceramic was pressed into the investment mold using an alumina plunger at 0.4 MPa. The set was removed from the furnace immediately after pressing, allowing to the slowly cooling down to room temperature. The specimens were removed and blasted with 100 μm aluminum oxide using a sandblaster (Biojato Master, Bioart, Sao Carlos, SP, and Brazil).
Investment residue was removed by immersing the specimens into 1% hydrofluoric acid (Invex Liquid, Ivoclar Vivadent AG, Schaan, Liechtenstein, and Germany) for 10 min in an ultrasound bath (Cristofoli, Campo Mourao, PR, Brazil).
The sprues were removed using diamond disks (Disco flexivel diamantado KG Sorensen, Sumare, Sao Paulo, Brazil). Aluminum oxide stone (Edenta AG Dental Produkt, Hauptstrasse, Switzerland) was used to finish the specimens, which were then measured using a digital caliper (Absolute Digimatic, Mitutoyo Sul Americana, Santo Amaro, SP, Brazil), excluding those with the dimensions 0.5 mm greater or lower than the preestablished 25 mm × 5 mm × 2 mm.
Three-point flexural strength test
The three-point flexural strength test was assessed in a universal test machine (EMIC DL 2000, Sao Jose dos Pinhais, PR, Brazil), using a 10 N cell and 0.5 mm/min constant loading speed. Specimens were positioned on the equipment's specific platform, which was composed by two supporting levers, 20 mm apart, onto which the specimen would rest, with both ends hanging 2.5 mm over the supporting edges. Force was applied onto the central aspect of the test specimen, using a blunt tip until specimen fracture occurred.
The test machine registered the highest force in Newton (N). For flexural strength calculations, values in MPa were used. As the test specimens had a rectangular shape, this calculation was carried out using the equation S = 3FD/2 LH2, where F is the highest centralized load in N applied onto the specimen at the moment of its rupture; D is the distance in millimeters between the supporting marks; L and H are the width and height of the specimens measured in millimeters.
A one-way analysis of variance (ANOVA) was used, accepting a significance level of 5%. The analyses were performed on SAS software (SAS Institute Inc., Release 9.2, 2008, Cary, NC, USA).
RESULTS
ANOVA demonstrated no significant difference found among groups (P = 0.1528), showing that differences in translucence/opacity and shade did not affect flexural strength in lithium disilicate ceramics [Table 1 and Graph 1].
Table 1.
Mean three-point flexural strength values (MPa) and SD for the studied groups
Graph 1.
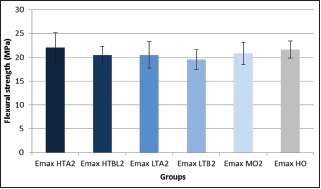
Bar diagram of the mean three-point flexural strength values (MPa) and standard deviation for the studied groups
DISCUSSION
Suitable ceramics for anterior veneers or crowns should be the conventional feldspathic or glass ceramics reinforced with leucite or lithium disilicate, as they allow for substrate's shade control (hue, chroma, and value) as well as translucence.[10,14] Ceramic optical properties are more important than its flexural strength in anterior restorations, contrary to what is desired for posterior teeth, where the flexural strength to bear higher mastication loads is paramount.[1,15] Higher crystalline phase ceramics have improved mechanical properties and therefore, are indicated for posterior restorations. On the other hand, high glass ceramics have better optical properties and therefore, more suitable for anterior teeth.[11,16,17]
The ideal esthetic material for indirect restorations should allow control of shade in all its dimensions (hue, chroma, and value) as well as translucence. Pressed lithium disilicate ceramics (as per the IPS e.max Press system) are found as ingots in a variety of translucence and opacity levels,[6,7,8,18] also containing zirconia, which shows a lower grade of translucence, thus limiting its use in anterior restorations.[8,19]
During manipulation of the lithium disilicate ceramics, heat-aided pressing depends on the external pressure in order to sinter and mold the ceramic at high temperatures. This process prevents the formation of large pores and promotes dispersion of the high crystalline phase within the glass matrix.[5,7] Some studies have demonstrated high flexural strength and fracture resistance in lithium disilicate reinforced ceramics,[9,20,21] due to their improved mechanical properties, based on particles with a low diameter and homogenous distribution.[10,21]
The IPS e.Max system represents a step forward from the Empress 2 system, with a flexural strength of 400 MPa, according to the manufacturer,[7] which corroborates the results obtained in this study. This system is a result of the addition of lithium orthodisilicate to the material in higher density and lower-sized particles, making it very similar to the tooth's microstructure. Furthermore, ceramics containing fluorapatite nanoparticles (IPS e.max Ceram) provide good esthetic results and excellent flexural strength.[8,11] The mean flexural strength values presented in this study were close to 400 MPa, as demonstrated by the manufacturer.[7] The lower results could be attributed to the lack of surface glaze of the test specimens, which would have otherwise increased surface smoothness and reduced porosity.
Translucence is strongly affected by the materials' composition and by the concentration of crystals.[6,8] It has been observed that ceramics with a high crystal content have improved mechanical properties.[22,23,24] When assessing the relationship between relative translucence and flexural strength of different ceramic systems, Chen et al.[24] concluded that zircona-based ceramics and yttria-stabilized zircona show the highest flexural strength values and the highest levels of opacity; however, lithium disilicite ceramics show lower strength and HT. According to the information supplied by the manufacturer, the composition and concentration of the crystalline phase within the IPS e.max Press ingots do not differ in terms of translucence or opacity. Furthermore, the material added to lithium disilicate ceramics, which is capable of causing different levels of shade and translucence, has not been released by the manufacturer, who has owned the patent for over 20 years.[7]
The present study demonstrated that there was no difference in flexural strength between ceramics of different grades of opacity/translucence. The null hypothesis has been accepted. The choice of the ceramic ingot is related to the esthetic need of each individual case, since the strength is similar across all IPS e.max Press ceramics, with different opacity/translucence types. Furthermore, clinical studies have demonstrated a considerable longevity for lithium disilicate pressed ceramics, with durability rates of 96% over 3 years for full coverage crowns, 96% over 6 years for three-unit fixed prosthodontics[12] and 100% over 3 years for onlays.[25] Over a 5 year time period, 99% of full coverage crowns on anterior and posterior teeth were successful.[26] After 10 years, from a total of 261 anterior and posterior lithium disilicate crowns, 95.5% survived, while four showed small chips in the ceramic and two suffered core fractures.[16] A systematic review[27] indicated that the 5-year cumulative estimated survival for etchable nonfeldspathic porcelain veneers was over 90%. Fabbri et al.[28] showed cumulative survival rates of lithium disilicate restorations ranging from approximately 95.39–100%, with anterior veneer monolithic restorations showing the lowest number of mechanical complications.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Giordano RA, 2nd, Pelletier L, Campbell S, Pober R. Flexural strength of an infused ceramic, glass ceramic, and feldspathic porcelain. J Prosthet Dent. 1995;73:411–8. doi: 10.1016/s0022-3913(05)80067-8. [DOI] [PubMed] [Google Scholar]
- 2.Della Bona A, Mecholsky JJ, Jr, Anusavice KJ. Fracture behavior of lithia disilicate-and leucite-based ceramics. Dent Mater. 2004;20:956–62. doi: 10.1016/j.dental.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 3.Shenoy A, Shenoy N. Dental ceramics: An update. J Conserv Dent. 2010;13:195–203. doi: 10.4103/0972-0707.73379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pollington S. Novel glass-ceramics for dental restorations. J Contemp Dent Pract. 2011;12:60–7. doi: 10.5005/jp-journals-10024-1011. [DOI] [PubMed] [Google Scholar]
- 5.Schwieger M. IPS Empress 2: A new pressable high-strength glass-ceramic for esthetic all-ceramic restorations. Quintessence Dent Technol. 1999;22:143–51. [Google Scholar]
- 6.Tysowsky GW. The science behind lithium disilicate: A metal-free alternative. Dent Today. 2009;28:112–3. [PubMed] [Google Scholar]
- 7.Ivoclar Vivadent AG. IPS Emax Press. Ivoclar. 2009. [Last cited on 2013 Feb 03]. Available from: http://www.ivoclarvivadent.us/en-us/download-center/instructions-foruse-for-dental-technicians/#I .
- 8.Yuan K, Wang F, Gao J, Sun X, Deng ZX, Wang H, et al. Effect of zircon-based tricolor pigments on the color, microstructure, flexural strength and translucency of a novel dental lithium disilicate glass-ceramic. J Biomed Mater Res B Appl Biomater. 2014;102:98–107. doi: 10.1002/jbm.b.32986. [DOI] [PubMed] [Google Scholar]
- 9.Fradeani M, Barducci G. Versatility of IPS Empress restorations. Part II: Veneers, inlays, and onlays. J Esthet Dent. 1996;8:170–6. doi: 10.1111/j.1708-8240.1996.tb00421.x. [DOI] [PubMed] [Google Scholar]
- 10.Sorensen JA. The IPS Empress 2 system: Defining the possibilities. Quintessence Dent Technol. 1999;22:153–63. [Google Scholar]
- 11.Höland W, Schweiger M, Frank M, Rheinberger V. A comparison of the microstructure and properties of the IPS Empress 2 and the IPS Empress glass-ceramics. J Biomed Mater Res. 2000;53:297–303. doi: 10.1002/1097-4636(2000)53:4<297::aid-jbm3>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 12.Wolfart S, Eschbach S, Scherrer S, Kern M. Clinical outcome of three-unit lithium-disilicate glass-ceramic fixed dental prostheses: Up to 8 years results. Dent Mater. 2009;25:e63–71. doi: 10.1016/j.dental.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 13.Ting S, Long QS, Yan LW, Yuan FY, Bin D, Ning W. Affection of post-core materials on the resultant color of lithium disilicate ceramic restorations. Key Eng Mater. 2012;6:512–5. [Google Scholar]
- 14.Ge J, Wang XZ, Feng HL. Influence of different postcore materials on the color of Empress 2 full ceramic crowns. Chin Med J (Engl) 2006;119:1715–20. [PubMed] [Google Scholar]
- 15.Chong KH, Chai J, Takahashi Y, Wozniak W. Flexural strength of In-Ceram alumina and In-Ceram zirconia core materials. Int J Prosthodont. 2002;15:183–8. [PubMed] [Google Scholar]
- 16.Valenti M, Valenti A. Retrospective survival analysis of 261 lithium disilicate crowns in a private general practice. Quintessence Int. 2009;40:573–9. [PubMed] [Google Scholar]
- 17.Höland W, Rheinberger V, Apel E, Ritzberger C, Rothbrust F, Kappert H, et al. Future perspectives of biomaterials for dental restoration. J Eur Ceram Soc. 2009;29:1291–8. [Google Scholar]
- 18.Stappert CF, Att W, Gerds T, Strub JR. Fracture resistance of different partial-coverage ceramic molar restorations: An in vitro investigation. J Am Dent Assoc. 2006;137:514–22. doi: 10.14219/jada.archive.2006.0224. [DOI] [PubMed] [Google Scholar]
- 19.Heffernan MJ, Aquilino SA, Diaz-Arnold AM, Haselton DR, Stanford CM, Vargas MA. Relative translucency of six all-ceramic systems. Part I: Core materials. J Prosthet Dent. 2002;88:4–9. [PubMed] [Google Scholar]
- 20.Pallis K, Griggs JA, Woody RD, Guillen GE, Miller AW. Fracture resistance of three all-ceramic restorative systems for posterior applications. J Prosthet Dent. 2004;91:561–9. doi: 10.1016/j.prosdent.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 21.Lin WS, Ercoli C, Feng C, Morton D. The effect of core material, veneering porcelain, and fabrication technique on the biaxial flexural strength and weibull analysis of selected dental ceramics. J Prosthodont. 2012;21:353–62. doi: 10.1111/j.1532-849X.2012.00845.x. [DOI] [PubMed] [Google Scholar]
- 22.Tinschert J, Zwez D, Marx R, Anusavice KJ. Structural reliability of alumina-, feldspar-, leucite-, mica-and zirconia-based ceramics. J Dent. 2000;28:529–35. doi: 10.1016/s0300-5712(00)00030-0. [DOI] [PubMed] [Google Scholar]
- 23.Albakry M, Guazzato M, Swain MV. Biaxial flexural strength, elastic moduli, and x-ray diffraction characterization of three pressable all-ceramic materials. J Prosthet Dent. 2003;89:374–80. doi: 10.1067/mpr.2003.42. [DOI] [PubMed] [Google Scholar]
- 24.Chen YM, Smales RJ, Yip KH, Sung WJ. Translucency and biaxial flexural strength of four ceramic core materials. Dent Mater. 2008;24:1506–11. doi: 10.1016/j.dental.2008.03.010. [DOI] [PubMed] [Google Scholar]
- 25.Guess PC, Stappert CF, Strub JR. Preliminary clinical results of a prospective study of IPS e.max Press- and Cerec ProCAD-partial coverage crowns. Schweiz Monatsschr Zahnmed. 2006;116:493–500. [PubMed] [Google Scholar]
- 26.Giordano R., 2nd A comparison of all-ceramic restorative systems: Part 2. Gen Dent. 2000;48:38. [PubMed] [Google Scholar]
- 27.Layton DM, Clarke M. A systematic review and meta-analysis of the survival of non-feldspathic porcelain veneers over 5 and 10 years. Int J Prosthodont. 2013;26:111–24. doi: 10.11607/ijp.3202. [DOI] [PubMed] [Google Scholar]
- 28.Fabbri G, Zarone F, Dellificorelli G, Cannistraro G, De Lorenzi M, Mosca A, et al. Clinical evaluation of 860 anterior and posterior lithium disilicate restorations: Retrospective study with a mean follow-up of 3 years and a maximum observational period of 6 years. Int J Periodontics Restorative Dent. 2014;34:165–77. doi: 10.11607/prd.1769. [DOI] [PubMed] [Google Scholar]


