Abstract
Background
Primary care interventions addressing child traumatic stress exist but their range and effectiveness is unclear.
Objectives
To systematically assess the evidence base for prevention and treatment of child traumatic stress in primary care settings.
Data Sources
PubMed, Embase, PsycINFO, Scopus, Academic Search Complete, CINAHL, Web of Science, Cochrane Library, the National Registry of Evidence-based Programs and Practices, the National Child Traumatic Stress Network website, Google search.
Study Eligibility Criteria, Participants, and Interventions
Studies were eligible for inclusion if they described the results of intervention studies in a primary care setting addressing child traumatic stress. Study participants could include primary care providers, pediatric patients, and their parents or other caregivers.
Study Appraisal and Synthesis Methods
Each study was assessed for inclusion and each included study was assessed for risk of bias by two reviewers.
Results
We found 12 articles describing 10 different studies that met the inclusion criteria. The intervention approaches taken in the studies were diverse and included the implementation of screening programs/tools, training clinicians to recognize and discuss psychosocial issues with patients and their families, and providing primary care professionals with community resource lists. Nine out of 10 studies included in the review reported favorable results.
Limitations
Studies included in the review had relatively short follow-up periods and the diversity of studies identified precluded the possibility of conducting a meta-analysis.
Conclusions and Implications of Key Findings
Findings suggest that interventions in pediatric primary care settings are feasible and can favorably impact clinical practices and families’ outcomes.
MeSH Key Words: Stress Disorders, Post-Traumatic, Child, Infant, Infant, Newborn, Child, Preschool, Adolescent, Primary Health Care, Secondary Prevention, Tertiary Prevention, Primary Prevention
Introduction
Social scientists have long pointed out that humans’ social environment has a profound and sustained impact on emotional and physical health.1 Neuroscientists have extended this work to propose that the brain is responsible for regulating the behavioral, autonomic, and immune responses to the social environment, particularly for perceptions of relative safety and threat.2 An NIMH consensus panel suggested that there may be discrete brain circuits associated with both acute and chronic stressors.3 The brain’s response to threats can vary greatly by an individual’s developmental status and beliefs about the causes of the threat and ability to survive or overcome them.4 When threats are interpreted as significantly life-threatening or negatively life-changing, we often refer to them as traumatic and become concerned about both short and long-term impact on health.5–16
The National Child Traumatic Stress Network (NCTSN) separates these more serious threats into two main categories, acute and chronic. Acute traumatic events include witnessing violence, facing imminent threats of injury, or experiencing violation of personal physical integrity (e.g., school shootings, sudden or violent loss of loved one, sexual assault). Chronic traumatic situations occur repeatedly over long periods of time (e.g., living with abusive parents or in poverty). Using these and similar definitions, general population studies have found that more than two-thirds of children and adolescents report past or present exposure to at least one form of trauma.7,8,9
Response to stressors is highly variable and can be immediate or delayed. Predictors include both personal characteristics such as temperament and environmental characteristics such as social support.4 There is evidence that specific psychological interventions can help prevent or ameliorate the development of long-term consequences including post-traumatic stress disorder,16 which is associated with myriad mental and physical problems in adults.17 The American Academy of Pediatrics (AAP) advocates that pediatricians do more to address trauma, not only because of the developmental and behavioral support offered by primary care providers (PCPs), but also because of their ability to identify and treat early physiologic markers that may be associated with adverse physiologic responses (e.g., abnormal weight, blood pressure, and glucose and lipid metabolism).18
By building longitudinal and broadly-based relationships with families, PCPs can become part of an ongoing support system and serve as a point of entry and coordination for additional services.19,20 Primary care practices have long made referrals for emotional and behavioral problems, but it is only recently that PCPs have begun to consider the extent to which they can help to identify and address trauma-related physical and psychological problems. Given that the 2010 Patient Protection and Affordable Care Act requires coverage of screening for depression and that Medicaid’s Early and Periodic Screening, Diagnosis, and Testing requires children to be screened for mental health problems,21 the use of screening interventions within the pediatric medical home is likely to increase over time.
The challenge lies in determining which interventions are feasible, sustainable, and effective for use in the pediatric primary care setting. Pediatric providers face a number of challenges to providing more mental health services, such as limited training on how to address the psychosocial concerns of their patients.21 The goal of this systematic review was to examine the existing evidence base on preventing and addressing traumatic stress exposure in pediatric primary care to better understand what is effective in this setting. Specifically, we aimed to identify the types of interventions that have been implemented and assess their impact on a variety of outcomes including provider behavior and, where studied, clinical outcomes.
Methods
Database Search
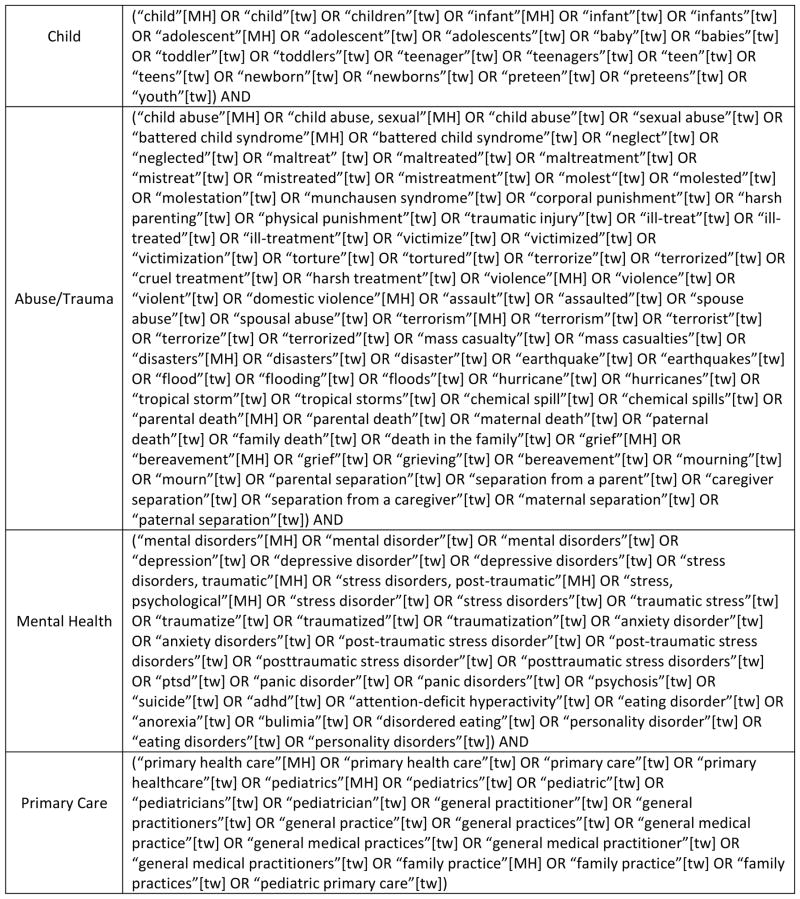
We searched the following databases: PubMed, Embase, PsycINFO, Scopus, Academic Search Complete, CINAHL, Web of Science, and the Cochrane Library. In addition, we searched the National Registry of Evidence-based Programs and Practices, the National Child Traumatic Stress Network website, and conducted a general web search using Google. The database search strategy was formulated around terms for “child” AND “abuse or trauma or violence or mass casualty or bereavement” AND “mental health” AND “primary care” (Figure 1). The earliest publication date was open while the search ended on December 31, 2013. Search results were exported from each database, and imported into RefWorks for de-duplication and review. Reference sections of included articles were searched, in addition, to identify articles published from January 1990 – December 2013.
Figure 1.
PubMed search string
Selection of Articles
The review was limited to peer-reviewed, original research articles in English. To be eligible for inclusion in the review, studies had to describe an intervention for the prevention of circumstances in which a child might experience traumatic stress, or for the treatment of child traumatic stress, and be carried out in a pediatric primary care setting. Studies carried out in specialty settings (e.g., emergency room, pediatric orthopedics) were excluded because we were interested specifically in interventions carried out in routine primary care. We also excluded studies of adult survivors of abuse and studies conducted in practice settings dissimilar to those encountered in the United States such as in developing countries. Included studies describe efficacy, effectiveness, or efficiency studies (there was no requirement that there be a control group or that group allocation be randomized); case reports, opinions, and reviews were excluded.
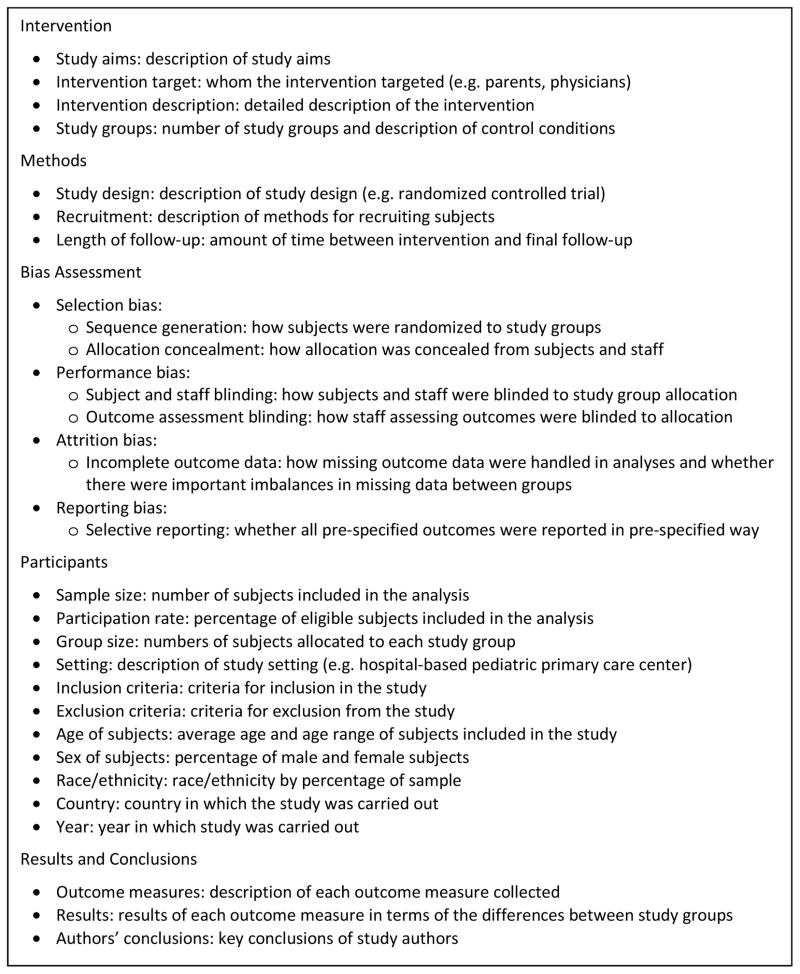
Each study was assessed for inclusion by two authors in a stepwise fashion, first by reading the title, then by reviewing the abstract, and finally by reviewing the full text of each study article as necessary. This was carried out first in independent assessments and then findings were compared and consensus was achieved on which studies to include in the next step. Data were extracted from included studies independently by two authors using a data extraction tool designed by the lead author. Variables for which data were sought are listed in Figure 2. Each of the studies included in the review was assessed for potential bias according to the Cochrane “Risk of Bias Tool”22 by two reviewers. We assessed selection bias (sequence generation, allocation concealment), performance bias (subject and staff blinding), detection bias (outcome assessment blinding), attrition bias (incomplete outcome data), and reporting bias (selective reporting) for the randomized controlled trials and attrition and reporting bias for observational studies. Possible ratings for each domain were “low,” “high,” or “unclear.”
Figure 2.
Variables for which data were sought from studies included in the review
Results
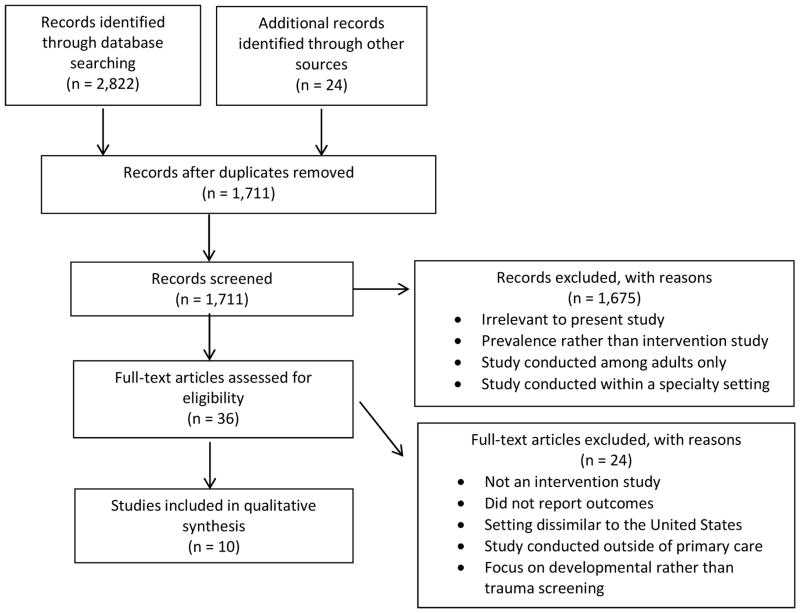
After removing duplicates, 1,711 articles were identified through database searches, and an additional 24 articles were identified by hand-searching the references of included full-text articles and review articles (Figure 3). We eliminated 1,675 records in the title and abstract reviews because they were 1) not relevant to the review topic, 2) focused on ascertaining prevalence of various disorders and exposures rather than on intervention evaluation, 3) focused on adults, or 4) carried out in a specialty setting. Thirty-six full-text articles were reviewed for eligibility. Twenty-four of the full-text articles were excluded because they did not describe intervention studies, did not report intervention outcomes, were conducted in settings too dissimilar to the United States, were not carried out in a primary care setting, or were focused on developmental rather than trauma screening. Twelve articles reporting the results of 10 separate studies were included the final review (Table 1).
Figure 3.
Table 1.
Intervention studies of child traumatic stress conducted in pediatric primary care settings, grouped by provider and patient (parents and/or children) outcomes
| Study | Subjects | Duration of follow-up |
Aim of study | Study Design | Intervention Description |
Control Condition Description |
Principal Outcomes Measured |
Conclusion of study |
|---|---|---|---|---|---|---|---|---|
| Provider Outcomes | ||||||||
| Berg et al 1983 | 2nd-year pediatric residents (n = 11) in the Phoenix Hospitals Affiliated Pediatric Program | 1–2 years | To study an 8-week rotation to increase knowledge, attitudes, and competence for pediatric residents | Non-randomized controlled trial | Residents examined patients in various settings (ambulatory clinic, psychiatry settings), visited community agencies and had didactic sessions. | A group of 3rd year residents who did not participate in the rotation served as controls (not randomly selected). | Residents’ attitudes, feelings of competence, factual knowledge | Rotation was successful in changing attitudes and knowledge |
| Berger et al 2002 | Pediatric residents, continuity clinic faculty, and nurse practitioners (n = 82) at Children’s Hospital of Pittsburgh | 2 months | To study whether an intervention would result in provider changes in screening for domestic violence (DV), identifying DV, and awareness of resources to address DV. | Pre-test/post-test | Didactic session on DV; DV articles and local DV resources; DV posters throughout the clinic; an additional session with a role play about how to ask parents and adolescents about DV | N/A | Clinicians’ knowledge, attitudes, and screening practices | It is possible to improve the frequency of routine DV screening among PCPs and pediatric staff. |
| Dubowitz et al 2011 Dubowitz et al 2012 Feigelman et al 2009 | Health professionals at 18 University of Maryland-affiliated private pediatric practices (n=95) | 1 year | To evaluate the effectiveness of the SEEK model in reducing child maltreatment in a suburban, middle income population | Cluster randomized controlled trial | The SEEK model consisted of primary care professionals training, the PSQ to screen parents for targeted risk factors, and a social worker to provide guidance, support, and referrals. | Practices assigned to the control condition received no training and provided standard care to subjects. | Attitudes, knowledge, feelings of competence, clinical practices | The SEEK model shows promise as a method of facilitating providers’ adoption of screening and referral practices |
| Feigelman et al 2011 | Resident physicians (n = 95) in primary care continuity clinics in a low-income urban area | 18 months | To evaluate the impact of the SEEK training model in pediatric residents and the families they care for. | Cluster randomized controlled trial | Residents were trained to identify psychosocial risk factors, use the PSQ screen, and work collaboratively with a social worker. | Residents assigned to the control group received no training and were not given SEEK materials. They were provided access to a human services worker. | Attitudes, knowledge, feelings of comfort, feelings of competence, clinical practices, parental satisfaction | Training improved resident comfort and perceived competence; small improvements in knowledge among parents, no difference in physical punishment |
| Forbes et al 2010 | Allied and primary care health practitioners (n = 342) working in bushfire zones in Australia | 0 – 3 months | To study the impact of “Skills for Psychological Recovery” modules for use by allied and primary care practitioners | pre-test/post-test | Health care workers were trained to use the “Skills for Psychological Recovery” manualized program, suitable for single or multiple sessions. | N/A | Provider perceptions, evaluation of workshops, use of Skills for Pyschological Recovery program | The workshops were well-received; generalists may need more support to address trauma |
| Garg et al 2007 | Pediatric residents (n = 45) in a large, urban hospital | 1 month | To evaluate the feasibility and impact of an intervention to improve the management of family psychosocial topics at well-child care visits at a medical home for low-income children | Randomized controlled trial | Providers were trained on the WE CARE program, administration of the WE CARE screening tool, and given access to a community resource book. | Residents in the control group received no training but were given the WE CARE Family Resource Book. | Provider attitudes about WE CARE | The We Care model was shown to be feasible in pediatric primary care in terms of provider comfort and duration of the patient visit. |
| Ishizaki et al 2005 | Pediatricians (n = 418) practicing throughout Japan | 1 year | To study the impact of disseminating a handbook for child psychosomatic disorders to pediatricians in Japan | Post-test | Providers were given a handbook with chapters on a wide range of mental health and behavioral issues. | N/A | Provider-reported handbook use, perceptions about usefulness, provider changes in thoughts and behaviors | Those with prior training used the handbook more but there was overall impact in PCP attitudes |
| Patient (parents and/or children) Outcomes | ||||||||
| Borowsky et al 2004 | Children ages 7 – 15 and their parents (n = 224) attending pediatric outpatient clinics in Minneapolis and St. Paul | 9 months | To evaluate the effectiveness of a primary care-based intervention directed at youths and their parents to reduce violence involvement and violence-related injuries | Randomized controlled trial | Children were screened with the PSC and the PCP was given the results to discuss with parents. The Positive Parenting program was available for parents. | PCPs were not given the results of the PSC for control group subjects. | Child and parent-reported CBCL scores (aggressive behavior), prevalence of bullying and being bullied | Psychosocial screening in primary care can result in decreases in injury and aggressive behaviors among children. |
| Dubowitz et al 2009 | Parents of children ages 0 – 5 years (n = 558) attending a resident-led pediatric primary care clinic in an urban, low-income setting | 3 – 4 years | To evaluate the effectiveness of the SEEK model in reducing child maltreatment in a high-risk population. | Randomized controlled trial | The SEEK model consisted of resident training, the PSQ to screen parents for targeted risk factors, and a social worker to provide guidance, support, and referrals. | Control group subjects received standard care. | Maltreatment rates determined by child protective services reports, child’s medical chart, and the Parent-Child Conflict Tactics Scale | The SEEK model showed promise as a practical strategy in primary care for helping prevent child maltreatment. |
| Dubowitz et al 2011 Dubowitz et al 2012 Feigelman et al 2009 | Mothers of children ages 0 – 5 years (n = 1,119) attending the practices | 1 year | To evaluate the effectiveness of the SEEK model in reducing child maltreatment in a suburban, middle income population | Cluster randomized controlled trial | The SEEK model consisted of primary care professionals training, the PSQ to screen parents for targeted risk factors, and a social worker to provide guidance, support, and referrals. | Practices assigned to the control condition received no training and provided standard care to subjects. | Child maltreatment determined by the Parent-Child Conflict Tactics Scale, children’s medical records, and child protective services reports | The SEEK model shows promise for preventing child maltreatment in a low-risk population |
| Garg et al 2007 | Parents of children aged 2 months to 10 years (n = 200) attending the pediatric clinic | 1 month | To evaluate the feasibility and impact of an intervention to improve the management of family psychosocial topics at well-child care visits at a medical home for low-income children | Randomized controlled trial | Providers were trained on the WE CARE program, administration of the WE CARE screening tool, and given access to a community resource book. | Residents in the control group received no training but were given the WE CARE Family Resource Book. | Rates of discussion and referral for family-level psychosocial problems at well-child care visits | The We Care model resulted in more discussion of psychosocial issues and more referrals during primary care visits |
| McFarlane et al 2005 | Women with children between the ages of 18 months and 18 years (n = 233) attending Women, Infants, and Children clinics in a large, urban city | 2 years | To evaluate whether a nurse case management program offered to abused mothers positively affects the behaviors of their children | Randomized controlled trial | The intervention group received abuse assessment, a wallet-size referral card, and nurse case management | The control group did not receive nurse case management but did receive abuse assessment and a wallet-size referral card. | Children’s internal, external, and total behavioral problems | nurse case management did not improve CBCL scores |
Studies included in the review fell into three categories: 1) those in which outcomes were reported among health professionals (5 studies), 2) those in which outcomes were reported among parents and/or children (3 studies), and 3) those in which outcomes were reported among both health professionals and parents or children (2 studies). Out of 10 studies, 6 were randomized controlled trials,23,24,25,26,27,28,29,30 and 4 were observational studies.31,32,33,34
Populations
The 10 included studies were carried out in diverse settings, including outpatient pediatric clinics of large urban teaching hospitals,31,32,29 pediatric primary care practices,23,25,26,27,33 primary care public health clinics,30 and Women, Infants & Children clinics.30 Seven studies targeted providers. Four of these were conducted among resident physicians,31,32,29,25,26,27 three were conducted among various health professionals working at primary care sites,23,34,30 and one was conducted among practicing pediatricians.33 Five studies targeted children, two based on parent’s/mother’s report of child behavior (parents of children ages 7–1523 and mothers of children ages 18 months to 18 years30) and three based on parent’s report and medical chart review (children ages 0–5 years old24,26 and children ages 2 months to 10 years29).
Interventions
There was a wide range of intervention types across the studies included in the review (Table 2). In most cases, interventions had multiple components so it was not possible to isolate the effects of individual components. In four studies, clinicians were taught to use a particular model/program or screening questionnaire with follow-up based on parent or caregiver responses. These included the Safe Environment for Every Kid (SEEK) Parent Screening Questionnaire (PSQ),24,25,26,27,28 the Pediatric Symptom Checklist (PSC),23 and the WE CARE family psychosocial screening tool.29 The SEEK version of the PSQ (for parents of children ages 0–5 years) has an emphasis on safety (number for poison control, fire alarms, gun in home), domestic violence exposure, parental/caregiver drug abuse, maternal depression, and major parental stress.24 The PSC is a psychosocial screen designed to facilitate the recognition of cognitive, emotional, and behavioral problems among children and teens with items pertaining to symptoms of internalizing, externalizing, and attentional disorders/behaviors.23 The WE CARE tool assesses parental drug use, parental depression, domestic violence exposure, child abuse, housing situation, education and employment among parents of children ages 2 months to 10 years.29 Following screening, various procedures were followed to address identified problems. Typically, clinicians were trained to discuss the results of screening with parents. Other intervention elements were implemented as well, including referrals to parenting programs such as Positive Parenting, a telephone-based parenting curriculum23 and referral to a social worker.24 In one study,30 the intervention consisted of giving out a wallet-size referral card and making nurse case-management sessions available to parents.
Table 2.
Types of Interventions Evaluated
| Study | Screening Use |
Didactic Training |
Experiential Training |
Social Worker |
Link to community services |
Telephone- based parenting program |
Handbook | Nurse case management |
Referral card/ Handout |
Office posters |
|---|---|---|---|---|---|---|---|---|---|---|
| Berg et al 1983 | X | X | ||||||||
| Berger et al 2002 | X | X | X | X | ||||||
| Borowsky et al 2004 | X | X | ||||||||
| Dubowitz et al 2009 | X | X | X | X | ||||||
| Dubowitz et al 2011 Dubowitz et al 2012 Feigelman et al 2009 | X | X | X | X | ||||||
| Feigelman et al 2011 | X | X | X | X | ||||||
| Forbes et al 2010 | X | X | X | |||||||
| Garg et al 2007 | X | X | X | X | ||||||
| Ishizaki et al 2005 | X | |||||||||
| McFarlane et al 2005 | X | X | X | |||||||
| Total | 6 | 7 | 2 | 3 | 2 | 1 | 2 | 1 | 6 | 1 |
Some studies involved training clinicians on how to recognize and address various issues (without the use of a screener) including child maltreatment, domestic violence, and psychosocial risk factors.31,32,34 Other intervention elements included having resident physicians spend a rotation with ambulatory clinic and psychiatry faculty and visit community agencies to learn about biosocial and developmental problems,31 providing clinicians with a list of local resources to improve their capacity to make referrals,32 placing posters related to domestic violence prevention throughout a primary care site,32 conducting role play sessions to improve communication with patients,32 training providers on how to work cooperatively with a social worker,28 and providing clinicians with a manual on psychosocial issues.33,34
Outcomes: Primary care providers
Table 4 reports the principal provider outcomes for each study. As a group, the studies found increased rates of screening and increased clinician confidence to carry out screening. Three studies reported changes in percentage of patients receiving screening. In one, screening rates for parent exposure to domestic violence increased from 21% pre-intervention to 46% after implementation of an education program on domestic violence.32 Two years after implementation of the SEEK model among health professionals, intervention group providers screened significantly more patients than did providers in the control group.25 After implementation of the SEEK model (provider training, screener use, coordination with social workers, handouts) among pediatric residents working in a primary care clinic, screening increased from 16% to 88% in the intervention group compared to almost no change in the control group.28
Table 4.
Principal study outcomes grouped by provider and patient (parents and/or children) outcomes
| Study | Outcome 1 | Outcome 2 | Outcome 3 |
|---|---|---|---|
| Provider Outcomes | |||
| Berg et al 1983 | Residents’ attitudes towards retardation, enuresis, physical handicaps, Down’s syndrome, bereavement, gynecology, deafness, and encopresis were significantly improved post-intervention (p<0.05). | Residents’ feelings of competence in the areas of physical handicaps, gynecology, hyperactivity, learning disabilities, enuresis, deafness, and childhood depression were significantly improved post-intervention (p<0.05). | Residents’ factual knowledge scores improved significantly post-intervention (p<0.005). |
| Berger et al 2002 | Knowledge of mandated reporting did not change significantly post-intervention among staff or trainees but did improve among interns (percentage giving correct answer increased from 64% to 100%, p<0.001). | No change in attitudes about role of pediatrician in discussing domestic violence (DV), comfort with talking about DV with patients, or having enough time to screen for DV. Clinicians and staff were more likely to report being aware of resources for DV victims: mean difference of 0.72, 95% confidence interval (0.46, 0.98), p<0.001. | No change in screening practices among clinicians and staff who attended just 1 training session. Percentage of clinicians and staff who routinely screened increased from 21% to 46% among those who attended 2 training sessions: difference of −0.25, 95% CI (−0.43, −0.08), p<0.005. |
| Dubowitz et al 2011 Dubowitz et al 2012 Feigelman et al 2009 | No difference between intervention and control groups on provider-reported knowledge, attitudes, practice behavior, and comfort discussing intimate partner violence and substance abuse with patients. Significant difference between groups on comfort level (p<0.05), perceived confidence (p<0.01), and comfort discussing depression (p=0.051) and stress (p<0.05) with patients. | Significant difference between intervention and control groups based on medical chart review in improvement in screening for depression (p<0.0001), intimate partner violence (p<0.0001), substance abuse (p<0.0001), and stress (p<0.0001). | No difference between groups based on observations of medical visits in improvement in screening for stress. Significant difference between groups in improvement in screening for depression (p<0.0001), intimate partner violence (p=0.0002), and substance abuse (p=0.0002) |
| Feigelman et al 2011 | Significant difference between intervention and control group residents in improvement of self-assessment on depression (p<0.01), intimate partner violence (p=0.03), and stress (p=0.04). Significant difference between groups in the opposite direction in improvement of self-assessment on corporal punishment (p=0.02). | Significant difference between groups according to medical chart review in screening for maternal depression (p<0.001), intimate partner violence (p<0.001), parental substance abuse (p<0.001), corporal punishment (p<0.001), stress/social support (p<0.001), and food insecurity (p<0.001). | Parents of children seen by intervention group residents were significantly more satisfied with their child’s doctor (score 17.4) than were control group parents (score 16.9)(p<0.01) at first visit. No difference between groups at 6-month follow-up. |
| Forbes et al 2010 | At baseline, 32% of providers agreed or strongly agreed that evidence-based treatments do not allow for clinical judgment and 20% agreed or strongly agreed that would not wish to use a manualized treatment program. | The workshop was rated as a positive experience on most items, with scores ranging from 2.08 to 3.48 on a 4-point scale. | 46% of log sheets returned by providers indicated that they had used Skills for Psychological Recovery among bushfire victims and 54% indicated the program had been used among victims of other traumatic events. |
| Garg et al 2007 | 100% of residents reported feeling comfortable with receiving the WE CARE survey from parents. | 77% of residents reported believing that conducting the WE CARE survey did not increase the duration of the visit. | 90.9% of residents said that conducting the WE CARE survey resulted in the addition of less than 5 minutes to the patient’s visit and 54.5% said that less than 2 minutes were added to the visit. |
| Ishizaki et al 2005 | 66.7% of providers said that they used the handbook at least once or twice per 2 or 3 months. | 63.2% of providers said that the handbook was at least relatively useful. | 34% of providers with limited training in children’s psychosomatic issues said their thoughts and behaviors about children’s psychosomatic disorders had changed (8% among trained providers). |
| Patient (parents and/or children) Outcomes | |||
| Borowsky et al 2004 | No difference between intervention and control groups in child-reported aggressive behavior. Significant difference at follow-up between groups in parent-reported aggressive behavior (p=0.005). | No difference between intervention and control groups in parent’s report of their child being bullied or in child’s report of bullying, either bullying or being bullied, physical fighting, or attitude toward violence. Significant difference at follow-up between groups on parent’s report of their child bullying other children (p<0.001), either bullying or being bullied (p=0.02), physical fighting (p=0.02), and fight-related injury (p=0.02) and in child’s report of being bullied (p<0.001). | |
| Dubowitz et al 2009 | There were significantly fewer instances of child abuse and neglect among intervention group children (13.3%) compared to control group children (19.2%) at follow-up: odds ratio 1.5, p=0.045. | There were significantly fewer instances of possible neglect among intervention group children compared to control group children based on review of child’s medical records (data not reported). | No difference between intervention and control groups on parent reported nonviolent discipline, psychological aggression, or minor physical assault. Significant difference between groups on parent reported severe or very severe physical assault: mean 0.11 vs. 0.33, p=0.04. |
| Dubowitz et al 2011 Dubowitz et al 2012 Feigelman et al 2009 | There were significant differences between intervention and control groups at 12-month follow-up on psychological aggression (effect estimate −0.12, 95% CI −0.24, −0.002, p=0.047) and minor physical assault (effect estimate −0.14, 95% CI −0.28, −0.005, p=0.043). | No significant difference between groups on abuse or neglect-related problems documented in children’s medical records. | No significant difference between groups on child protective services reports for neglect or physical abuse. |
| Garg et al 2007 | More psychosocial topics were discussed at well-child care visits among intervention group families (mean 2.9) than among control group families (mean 1.8) (p<0.01). | Intervention group parents received significantly more referrals than control group parent (mean 1.15 vs. 0.24, p<0.001). | |
| McFarlane et al 2005 | No significant difference between intervention and control groups on internal behavior problems. | No significant difference between groups on external behavior problems. | No significant difference between groups on total behavior problems. |
Six studies found improvements in self-assessments by clinicians. In one study, a rotation for residents resulted in increased perceived competence and more positive attitudes towards patients with psychosocial problems.31 Other findings included increased intentions to screen, improved comfort with screening, increased perceived usefulness of particular screening tools or handbooks, and increased awareness of community resources for patients.
Outcomes: Parents/children
Principal patient outcomes for each study are reported in Table 4. Five studies reported outcomes among parents and children, four of which provided evidence of reductions in risk or occurrence of trauma or increases in referrals to community resources. Two studies compared Child Behavior Checklist (CBCL) scores between intervention and control groups.23,30 In one of these, there was no significant difference in CBCL scores between children in the intervention group (family received nurse case-management after identification of exposure to maternal abuse) and the control group at 24 months after baseline.30 In the other study, significant improvement in CBCL scores for the intervention group (screening) compared to control groups was found for aggressive and delinquent behavior and attention problems but not anxiety/depression 9 months after baseline assessment.23 The two other studies finding a reduction in risk used the SEEK model as the intervention and child maltreatment as the outcome. In both low- and high-risk populations, the SEEK intervention group had lower rates of maltreatment by parents one year or more after baseline.24,26 These four studies were all randomized controlled trials.
Another study reporting outcomes among parents and children measured the occurrence of referral by clinical social workers through medical chart review; parents in the intervention group received more referrals than those in the control group.29 Other outcomes measured in studies among parents and children included instances of possible medical neglect, less harsh punishment reported by parents, unmet desires on the part of parents for discussion with the clinician, percent of parents reporting that their child needed to be hit or spanked, and fewer injuries resulting from physical fights with peers.
Study Quality
The 10 studies included in this review varied in terms of quality. Over half of the studies were randomized controlled trials. Research staff were blinded to allocation of subjects in only one study23 though this is understandable given the nature of the interventions; allocation concealment would have been impossible in many instances. Staff assessing outcomes from medical records were blinded in only two studies.23,29 Those studies for which methods of dealing with missing data were reported dropped subjects with missing outcomes data from the analysis.30,32 We assessed each of the studies specifically for potential for various forms of bias (see Table 3). Risk of bias was generally low overall though there were some exceptions. In particular, subject/staff blinding, outcome assessment blinding, and incomplete outcome reporting were areas of concern in a number of studies in that our ratings were either high or unclear. The four randomized trials reporting clinical outcomes (e.g. CBCL scores, child maltreatment as measured in the SEEK studies) were of mixed quality, with the two SEEK studies having low or unclear risk of bias and the two studies reporting CBCL scores having relatively high risk of bias (see Table 3).
Table 3.
Bias Risk Assessment (Low = low risk of bias) in randomized trials
| Key outcomes measured | Sequence Generation | Allocation Concealment | Subject/Staff Blinding | Outcome Assessment Blinding | Incomplete Outcome Data | Selective Reporting | |
|---|---|---|---|---|---|---|---|
| Randomized Controlled Trials | |||||||
| Borowsky, et al. 2004 | CBCL scores | Low | High | High | High | Low | Low |
| Dubowitz, et al. 2009 | Child maltreatment | Low | Low | Unclear | Unclear | Unclear | Low |
| Dubowitz, et al. 2011 | Child maltreatment | Low | Low | Low | Low | Low | Low |
| Feigelman, et al. 2011 | Resident self-assessment | Low | Low | Low | High | Low | Low |
| Garg, et al. 2007 | Psychosocial topics discussed, referrals | Low | Low | Unclear | Unclear | Unclear | Low |
| McFarlane, et al. 2005 | CBCL scores | Low | Low | Low | High | High | Low |
| Observational Studies | |||||||
| Berg, et al. 1983 | Perceived feelings of competence, attitudes, factual knowledge | n/a | n/a | n/a | n/a | Low | Low |
| Berger, et al. 2002 | Knowledge, attitudes, screening practices | n/a | n/a | n/a | n/a | Low | Low |
| Forbes, et al. 2010 | Perceptions of protocol, provider confidence | n/a | n/a | n/a | n/a | Low | Low |
| Ishizaki, et al. 2005 | Frequency of handbook use, perceptions, clinical behavior | n/a | n/a | n/a | n/a | Unclear | Low |
Discussion
There is a growing interest in integrating the prevention and management of trauma-related problems into pediatric primary care visits, yet very little is known about effective approaches to address trauma in this setting. According to an AAP policy statement, “the reduction of toxic stress in young children ought to be a high priority for medicine as a whole and for pediatrics in particular.”35 This paper reviewed the literature on evidence-based trauma interventions in pediatric primary care to improve our knowledge of different types of interventions and their effectiveness.
We identified ten studies implementing interventions in primary care settings to prevent or mitigate the impact of childhood traumatic stress. Over half (six) used randomized designs, and four were non-randomized intervention studies. Seven of the interventions targeted medical providers (including pediatric residents) and five targeted parents and children. The interventions combined included approximately 4000 health care providers. The interventions focused on training (to increase PCP’s knowledge, attitudes, confidence and competence), screening, linkage to social workers, nurse case management, and education materials (e.g., a handbook) and resource booklets for both doctors and families.
Authors of nine of the ten studies concluded that the interventions studied had a positive impact on their intended outcomes. The findings suggest that training/education and screening interventions in primary care settings can enhance a range of provider skills and increase provider knowledge and perceived competence. Reductions in adverse child outcomes such as child physical abuse and maltreatment (as assessed by parental and Child Protective Services report), domestic violence exposure, delinquent behavior, aggression, and injury were achieved by a majority of the interventions that measured these outcomes. The interventions also increased discussions about psychosocial issues during clinic visits and improved referral rates. In particular, in three out of four studies reporting clinical outcomes among children, significant changes were seen in the intervention group in terms of child maltreatment outcomes and change in CBCL scores. However, in the study by McFarlane and colleagues there was no significant impact of nurse case management on CBCL scores in the intervention group compared to the control group. It may be that the use of abuse assessments for both groups positively affected outcomes for all participants.30 It should be noted that iatrogenic effects of screening or the other interventions were not reported by any of the included studies.
These positive findings are tempered by the fact that, although they derive in part from four randomized trials, only one of the interventions (the SEEK model) has been replicated, and follow-up periods in some studies were very short. More research is needed on the long-term impact of these interventions on both parental and child outcomes. More also remains to be known about the feasibility and sustainability of the interventions in clinical practice settings. The SEEK24,25,26,27,28 and other studies23,29,30,31,32 used multicomponent, coordinated interventions that might not all be possible in some practices and service systems. Understandably, these initial studies were not implemented at a large enough scale to determine the individual effects or interactions of specific treatment components. Future research in this area should focus on replicating results, isolating the effects of individual intervention components, and reducing bias risk in study design by randomizing subjects to intervention and control groups and blinding study staff and patients to group allocation.
As noted by Dubowitz and colleagues.,24 although the role of pediatrics has evolved to include recognizing and addressing psychosocial problems such as trauma exposure in families, there has been only a modest shift in practice to proactively identify and treat trauma exposure.36,37,38,39 Part of this could be attributable to real and perceived barriers such as lack of time or training, lack of ease and efficiency in accessing community mental health resources, and discomfort addressing sensitive issues. The studies in this review were able to address many of these barriers. For example, to reduce screening time, Garg, et al.29 and Dubowitz, et al.24 administered the screen in the waiting room before the visit. These authors found that their programs did not add time to visits or added only 1–2 minutes.26,29 However, it is not known whether the discussion of family psychosocial problems may have displaced other recommended anticipatory guidance topics during the visit and healthcare providers who adopt screening programs should be mindful of this. Clinicians have cited lack of insurance reimbursement as a barrier to the incorporation of evidence-based strategies into the pediatric medical home.40 However, Lane and colleagues found that the SEEK cost about $5 per family but estimated that the dissemination of the model to 100,000 families could save $37 million in medical, mental health, and social services costs, which is highly relevant to both healthcare providers and policy makers.41
These findings should be discussed in the context of several limitations. The risk of publication bias is high as only one of the included studies had negative findings. We included only studies in the English language. The heterogeneity in screeners used, outcomes assessed, and age range targeted across the included studies precluded a meta-analysis. We are not aware of whether the interventions were sustained, and long-term impact (over three years) was not studied. A broad range of populations is represented by the studies included in this review, including both high and low income families, public and private hospital or clinic settings, and a diversity of geographical locations throughout the United States and other countries. While this indicates that approaches to preventing and treating child traumatic stress in primary care settings can be effective in a variety of settings, it should be noted that each individual study included in our review is generalizable only so far as the results are applied to populations similar to those studied. In addition, the training and qualifications of those delivering interventions was quite diverse across those studies that reported such information, including psychologists, social workers, pediatricians, pediatric residents, doctors, nurses, counsellors, occupational therapists, and case managers. Despite these limitations, this review fills a major gap in the literature. The group of included studies collectively demonstrates that interventions to prevent and treat child traumatic stress are feasible and can have a favorable impact on health professionals’ clinical practices and families’ outcomes.
The current evidence suggests that primary care may be well suited to implementing interventions related to prevention, detection, and early intervention of trauma-related problems. Our review highlights the impact and effectiveness of primary care-based trauma interventions. Issues of cost-effectiveness and sustainability of the interventions reviewed remain to be studied in depth.
What this Systematic Review Adds
Identification of interventions for child traumatic stress in primary care
Assessment of quality of studies of child traumatic stress interventions inprimary care
Promising evidence supporting further implementation and testing of interventions for child traumatic stress in primary care settings
How to Use this Systematic Review
Become familiar with the range of interventions addressing child traumatic stress in primary care settings
Consider implementing and further testing interventions for child traumatic stress in primary care
Acknowledgments
This work was supported by the Substance Abuse and Mental Health Service Administration (SAMHSA) (U79SM061259) for the Pediatric Integrated Care Collaborative (PICC). PICC is a component of the National Child Traumatic Stress Network (NCTSN) through the Donald J. Cohen National Child Traumatic Stress Initiative, which encourages collaboration among leaders in the field of child traumatic stress. The role of the funders for the systematic review was solely financial support. This research was supported in part by a grant from the National Institutes on Drug Abuse (T-32DA007292, awarded to C. Debra M. Furr-Holden).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Kate E. Fothergill, Email: kfother1@jhu.edu.
Holly C. Wilcox, Email: hwilcox1@jhmi.edu.
Elizabeth Coleclough, Email: ecolecl1@jhu.edu.
Russell Horwitz, Email: rhorwitz@jhmi.edu.
Anne Ruble, Email: aruble@jhmi.edu.
Matthew D. Burkey, Email: mburkey1@jhmi.edu.
Lawrence Wissow, Email: lwissow@jhmi.edu.
References
- 1.Link BG, Phelan J. Social conditions and fundamental causes of disease. Journal of Health and Social Behavior. 1995;35:80–94. [PubMed] [Google Scholar]
- 2.McEwan BS, Gianaros PJ. Central role of the brain in stress and adaptation: links to socioeconomic status, health, and disease. Annals of the New York Academy of Sciences. 2010;1186:190–222. doi: 10.1111/j.1749-6632.2009.05331.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Morris SE, Cuthbert BN. Research Domain Criteria: cognitive systems, neural circuits, and dimensions of behavior. Dialogues in Clinical Neuroscience. 2012;14:29–37. doi: 10.31887/DCNS.2012.14.1/smorris. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ungar M. Practitioner review: diagnosing childhood resilience – a systemic approach to the diagnosis of adaptation in adverse social and physical ecologies. Journal of Child Psychology and Psychiatry. 2015;56:4–17. doi: 10.1111/jcpp.12306. [DOI] [PubMed] [Google Scholar]
- 5.National Child Traumatic Stress Network. [Accessed on September 16, 2014];Defining Trauma and Child Traumatic Stress. Retrieved from http://www.nctsn.org/content/defining-trauma-and-child-traumatic-stress.
- 6.Odgers CL, Jaffee SR. Routine versus catastrophic influences on the developing child. Annual Review of Public Health. 2013;34:29–48. doi: 10.1146/annurev-publhealth-031912-114447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Copeland WE, Keeler G, Angold A, Costello EJ. Traumatic events and posttraumatic stress in childhood. Archives of General Psychiatry. 2007;64:577–584. doi: 10.1001/archpsyc.64.5.577. [DOI] [PubMed] [Google Scholar]
- 8.Costello EJ, Erkanli A, Fairbank JA, Angold A. The prevalence of potentially traumatic events in childhood and adolescence. Journal of Traumatic Stress. 2002;15:99–112. doi: 10.1023/A:1014851823163. [DOI] [PubMed] [Google Scholar]
- 9.Finkelhor D, Ormrod R, Turner H, Hamby SL. The victimization of children and youth: a comprehensive, national survey. Child Maltreatment. 2005;10:5–25. doi: 10.1177/1077559504271287. [DOI] [PubMed] [Google Scholar]
- 10.Edwards VJ, Anda RF, Dube SR, Dong M, Chapman DF, Felitti VJ. The wide-ranging health consequences of adverse childhood experiences. In: Kendall-Tackett K, Giacomoni S, editors. Child Victimization: Maltreatment, Bullying, and Dating Violence Prevention and Intervention. Kingston, NJ: Civic Research Institute; 2005. [Google Scholar]
- 11.Dube SR, Anda RF, Felitti VJ, Chapman D, Williamson DF, Giles WH. Childhood abuse, household dysfunction and the risk of attempted suicide throughout the life span: Findings from Adverse Childhood Experiences Study. JAMA. 2001;286:3089–3096. doi: 10.1001/jama.286.24.3089. [DOI] [PubMed] [Google Scholar]
- 12.Dube SR, Anda RF, Whitfield CL, Brown DW, Felitti VJ, Dong M, Giles WH. Long-term consequences of childhood sexual abuse by gender of victim. American Journal of Preventive Medicine. 2005;28:430–438. doi: 10.1016/j.amepre.2005.01.015. [DOI] [PubMed] [Google Scholar]
- 13.Jonson-Reid M, Kohl PL, Drake B. Child and adult outcomes of chronic child maltreatment. Pediatrics. 2012;129(5):839–45. doi: 10.1542/peds.2011-2529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gilbert R, Widom CS, Browne K, Fergusson D, Webb E, Janson S. Burden and consequences of child maltreatment in high-income countries. Lancet. 2009;373(9657):68–81. doi: 10.1016/S0140-6736(08)61706-7. [DOI] [PubMed] [Google Scholar]
- 15.Widom CS, Czaia SJ, Bentley T, Johnson MS. A prospective investigation of physical health outcomes in abused and neglected children: new findings from a 30-year follow-up. American Journal of Public Health. 2012;102(6):1135–44. doi: 10.2105/AJPH.2011.300636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Newman E, Pfefferbaum B, Kirlic N, Tett R, Nelson S, Liles B. Meta-analytic review of psychological interventions for children survivors of natural and man-made disasters. Current Psychiatry Reports. 2014;16:462. doi: 10.1007/s11920-014-0462-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sareen J. Posttraumatic stress disorder in adults: impact, comorbidity, risk factors, and treatment. Canadian Journal of Psychiatry. 2014;59:460. doi: 10.1177/070674371405900902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shonkoff JP, Garner AS the Committee on Psychosocial Aspects of Child and Family Health, Committee on Early Childhood, Adoption, and Dependent Care, and Sections on Developmental and Behavioral Pediatrics. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129:e232–e246. doi: 10.1542/peds.2011-2663. [DOI] [PubMed] [Google Scholar]
- 19.Finkel MA. I can tell you because you’re a doctor. Pediatrics. 2008;122(2):442. doi: 10.1542/peds.2008-1416. [DOI] [PubMed] [Google Scholar]
- 20.Flaherty EG, Stirling J the Committee on Child Abuse and Neglect. Clinical report - the pediatricians’ role in child maltreatment prevention. Pediatrics. 2010;126(4):833–841. doi: 10.1542/peds.2010-2087. [DOI] [PubMed] [Google Scholar]
- 21.Wissow LS, Brown J, Fothergill KE, Gadomski A, Hacker K, Salmon P, Zelkowitz R. Universal mental health screening in primary care: a systematic review. Journal of the American Academy of Child and Adolescent Psychiatry. 2013;52:1134–1147. doi: 10.1016/j.jaac.2013.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. The Cochrane Collaboration; 2011. [Accessed on September 16, 2014]. Retrieved from: http://handbook.cochrane.org/front_page.htm. [Google Scholar]
- 23.Borowsky IW, Mozayeny S, Stuenkel K, Ireland M. Effects of a primary care-based intervention on violent behavior and injury in children. Pediatrics. 2004;114:e392. doi: 10.1542/peds.2004-0693. [DOI] [PubMed] [Google Scholar]
- 24.Dubowitz H, Feigelman S, Lane W, Jeongeun K. Pediatric primary care to help prevent child maltreatment: The Safe Environment for Every Kid (SEEK) Model. Pediatrics. 2009;123:858–864. doi: 10.1542/peds.2008-1376. [DOI] [PubMed] [Google Scholar]
- 25.Dubowitz H, Lane WG, Semiatin JN, et al. The Safe Environment for Every Kid Model: Impact on Pediatric Primary Care Professionals. Pediatrics. 2011;127:e962–970. doi: 10.1542/peds.2010-1845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dubowitz H, Lane WG, Semiatin JN, Magder LS. The SEEK Model of Pediatric Primary Care: Can Child Maltreatment be Prevented in a Low-Risk Population? Academic Pediatrics. 2012;12:259–268. doi: 10.1016/j.acap.2012.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Feigelman S, Dubowitz H, Lane W, et al. Screening for harsh punishment in a pediatric primary care clinic. Child Abuse & Neglect. 2009;33:269–277. doi: 10.1016/j.chiabu.2008.09.011. [DOI] [PubMed] [Google Scholar]
- 28.Feigelman S, Dubowitz H, Lane W, et al. Training residents in a primary care clinic to help address psychosocial problems and prevent child maltreatment. Academic Pediatrics. 2011;11:474–480. doi: 10.1016/j.acap.2011.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Garg A, Butz AM, Dworkin PH, et al. Improving the management of family psychosocial problems at low-income children’s well-child care visits: the WE CARE Project. Pediatrics. 2007;120:547–58. doi: 10.1542/peds.2007-0398. [DOI] [PubMed] [Google Scholar]
- 30.McFarlane JM, Groff JY, O’Brien JA, Watson K. Behaviors of children following a randomized controlled treatment program for their abused mothers. Issues in Comprehensive Pediatric Nursing. 2005;28:195–211. doi: 10.1080/01460860500396708. [DOI] [PubMed] [Google Scholar]
- 31.Berg RA, Rimsza ME, Eisenberg N, Ganelin RS. Evaluation of a successful biosocial rotation. American Journal of Diseases of Children. 1983;137:1066–1068. doi: 10.1001/archpedi.1983.02140370028010. [DOI] [PubMed] [Google Scholar]
- 32.Berger RP, Bogen D, Dulani T, Broussard E. Implementation of a program to teach pediatric residents and faculty about domestic violence. Archives of Pediatric and Adolescent Medicine. 2002;156:804–810. doi: 10.1001/archpedi.156.8.804. [DOI] [PubMed] [Google Scholar]
- 33.Ishizaki Y, Kobayshi Y, Yamagata Z, et al. Research on promotion of management of children with psychosomatic and psychological disorders in Japan. Pediatrics International. 2005;47:352. doi: 10.1111/j.1442-200x.2005.02074.x. [DOI] [PubMed] [Google Scholar]
- 34.Forbes D, Fletcher S, Wolfgang B, et al. Practitioner perceptions of skills for psychological recovery: a training program for health practitioners in the aftermath of the Victorian bushfires. Australian and New Zealand Journal of Psychiatry. 2010;44:1105–1111. doi: 10.3109/00048674.2010.513674. [DOI] [PubMed] [Google Scholar]
- 35.Garner AS, Shonkoff JP, Siegel BS, et al. Early childhood adversity, toxic stress, and the role of the pediatrician: translating developmental science into lifelong health. Policy statement of the American Academy of Pediatrics. Pediatrics. 2012;129(1):e224–e231. doi: 10.1542/peds.2011-2662. [DOI] [PubMed] [Google Scholar]
- 36.Horwitz SM, Kelleher KJ, Stein RE, et al. Barriers to the identification and management of psychosocial issues in children and maternal depression. Pediatrics. 2007;119(1):e208–18. doi: 10.1542/peds.2005-1997. [DOI] [PubMed] [Google Scholar]
- 37.Fothergill KE, Gadomski A, Solomon BS, et al. Assessing the impact of a web-based comprehensive somatic and mental health screening tool in pediatric primary care. Academic Pediatrics. 2013;13:340–347. doi: 10.1016/j.acap.2013.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Marie-Mitchell A, O’Connor TG. Adverse childhood experiences: translating knowledge into identification of children at risk for poor outcomes. Academic Pediatrics. 2013;13:14–19. doi: 10.1016/j.acap.2012.10.006. [DOI] [PubMed] [Google Scholar]
- 39.Zenlea IS, Milliren CE, Mednick L, Rhodes ET. Depression screening in adolescents in the United States: a national study of ambulatory office-based practice. Academic Pediatrics. 2014;14:186–191. doi: 10.1016/j.acap.2013.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Morelli DL, Pati S, Butler A, et al. Challenges to implementation of developmental screening in urban primary care: a mixed methods study. BMC Pediatrics. 2014;14:16–26. doi: 10.1186/1471-2431-14-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lane WG, Frick K, Dubowitz H, et al. Cost-Effectiveness analysis of the SEEK (A Safe Environment for Every Kid) child maltreatment prevention program. American Public Health Association 139th Annual Meeting and Exposition; Washington, DC. November 1, 2011. [Google Scholar]