Abstract
Background
Serial interferon-gamma-release-assay (IGRA) result can show variance due to within-subject variation and difference in host immune status, and may be affected by latent tuberculosis infection (LTBI) treatment. We aimed to know the changes in QFT-IT (QuantiFERON-TB Gold In-Tube) results measured at a 4 month interval in end stage renal disease patients and whether these changes were influenced by dialysis method or LTBI treatment.
Methods
We prospectively performed serial QFT-IT tests at 4 month interval in 93 end stage renal disease (ESRD) patients on HD (hemodialysis) or PD (peritoneal dialysis). LTBI treatment was given to 18 of 39 patients with initial positive QFT-IT result. Agreement between the two results was estimated for all 93 patients and reversion rates were estimated among the 39 patients with initial positive QFT-IT.
Results
Positive QFT-IT at the first and 2nd tests were 41.9 and 34.4 %, respectively. The concordance rate between baseline QFT-IT and 2nd QFT in 93 ESRD patients was excellent (90.3 %, kappa = 0.80, p < 0.001). Agreement between the first QFT-IT and 2nd QFT-IT in HD (95.3 %, kappa = 0.91, p < 0.001) was higher than in PD patients (86.0 %, kappa = 0.69, p < 0.001). Among all ESRD patients, the odds of reversion of QFT-IT was not different in those who were, or were not treated for LTBI [odds ratio = 2.3 (0.5–11.4), p = 0.43].
Conclusions
In a group of 93 dialyzed ESRD patients 8.6 % showed reversion of initial positive QFT to negative within 4 months. Reversion seemed not to be associated with LTBI treatment. Further study with larger numbers of patients is needed to investigate the variation of QFT-IT tests in dialyzed ESRD patients.
Keywords: Interferon-gamma release assay, Latent tuberculosis, End stage renal disease, Dialysis, Reversion
Background
Tuberculosis (TB) remains an important global health issue, and is the single most significant infectious cause of morbidity and mortality in the world, with approximately 2 million deaths and around 9 million new cases each year [1–3]. LTBI diagnosis and treatment is a part of the strategy for TB elimination in countries with low or intermediate burden [4, 5].
There are several clinical conditions in which the risk for active TB is increased. ESRD patients as well as renal-transplant patients on immune suppressive agents who have LTBI have an increased risk for progressive active TB [6]. The annual incidence of active TB in South Korea where BCG vaccination is mandatory is intermediate (84/100,000) [7] and that of active TB in renal transplant patients is 0.5 %/year in South Korea [8]. Therefore, it would be better to treat LTBI in dialyzed ESRD patients before transplantation, because prophylactic TB drug like rifampicin can lead to drug interaction with immune suppression drug on kidney-transplantation recipients [9].
End stage renal disease (ESRD) is known to compromise cellular immune function, and patients on dialysis have been shown to have T cell dysfunction including abnormal IFN-gamma levels, considered to have a pivotal role in controlling latent TB infection [10, 11]. A high percentage of the ESRD patients show no skin reaction to tuberculin skin test (TST) as they are anergic [12, 13]. Interferon-gamma release assays (IGRAs) are useful tools for diagnosing LTBI, because they are more specific, particularly in BCG vaccinated populations [14], and may identify some additional patients with latent TB among kidney-transplantation (KT) recipients with a negative TST [15].
Therefore, IGRA may be useful in this patient population to detect TB infection, but the use of serial IGRA testing to detect new TB infection in these patients is controversial because of non-specific variation, conversions, and reversions. Lee et al. reported that QFT-IT test reversion occurred in 41.9 % of the subjects and IFN-gamma levels decreased in almost all subjects after LTBI treatment [16].
Although previous studies have proposed that conversions, reversions, and non-specific variations can occur with serial IGRA testing [17, 18], there are no studies about serial changes of IGRAs in patients with end stage renal disease who receive LTBI treatment. We prospectively evaluated QFT-IT tests on two occasions at a four month interval in dialyzed ESRD patients, some of whom received LTBI treatment, to estimate the variation of the QFT-IT on repeated testing, and the effect of dialysis type and LTBI therapy.
Methods
Study design
ESRD patients on Peritoneal dialysis (PD) or hemo-dialysis (HD) were enrolled in this study. QFT-IT test was performed initially for screening of LTBI, and the patients with positive QFT-IT started to receive 9 months of isoniazid treatment or 4 months of rifampicin treatment immediately. The QFT-IT test was repeated at 4 months interval for all the subjects including a sub-group who received Isoniazid for 9 months or rifampicin for 4 months- all of whom took > 80 % of doses. Chest radiographs were screened before LTBI treatment. Written informed consent was obtained from study participants, and the study was approved by the Institutional Review Board of the Inje University Busan Paik hospital.
QuantiFERON-TB Gold In-Tube test
All participants were tested with the QFT-IT test per the manufacturer’s instructions. An IFN-gamma response to the ESAT-6/CFP-10/TB7.7 mixture ≥0.35 IU/mL above the nil control value (and ≥25 % of the nil control) was considered a positive result for the QFT-IT test. QFT-IT test reversion was defined as a change from a positive (≥0.35 IU/mL) to a negative (<0.35 IU/mL) result, and conversion as a change from a negative (<0.35 IU/mL) to a positive (≥0.35 IU/mL) result.
Statistical analysis
All analyses were performed using SPSS software, version 12.0 (SPSS Inc., Chicago, IL, USA). Between-group comparisons were made with t-test and Mann–Whitney test for variables. Concordance between test results from first QFT-IT and 2nd QFT-IT test was assessed using kappa coefficients. The χ2 tests was used to test for difference between reversion group and non-reversion group, and paired changes of interferon-gamma levels was analyzed by Wilcoxon signed rank test. All tests for significance were two-sided and statistical significance was established at P values < 0.05.
Results
Demographics of the participants
A total of 150 ESRD patients were screened with QFT-IT and chest radiographs. The QFT-IT test was repeated for the initially screened patients, but both baseline QFT-IT and 2nd QFT-IT test results were available for 93 patients finally (Table 1). In other words, 2nd QFT-IT test could not be performed for 57 ESRD patients (HD:22, PD:35), because 6 patients (HD:2, PD:4) were in inpatient care for associated disease, 13 patients (HD:6, PD:7) were transferred out to other hospital, and 38 patients (HD:14, PD:24) refused to participate in further study. Old TB lesion on chest radiograph was found on 35 (37.6 %) patients among them. Hemodialysis was used for 43 ESRD patients, and peritoneal dialysis was used for 50 ESRD patients. The mean age was 51.6 years (range, 23–74 years) and the male-to-female ratio was 43:50. A BCG scar was present in 62 patients (66.7 %). The positive rates of the 1st QFT-IT at baseline testing and 2nd QFT-GIT testing at the 4 month follow-up were 41.9 and 34.4 %, respectively. Isoniazid was prescribed for 10 patients and rifampicin was prescribed for 8 patients for the treatment of patients with LTBI showing positive QFT-IT results. There were no differences between the HD group and PD group in age, gender, BMI, positive rate of QFT-IT except the presence of BCG scar and the rate of LTBI treatment (Table 1).
Table 1.
Clinical characteristics of the study population
| Clinical characteristics | Total (n = 93) | HD (n = 43) | PD (n = 50) | P-value |
|---|---|---|---|---|
| Mean age, years (range) | 51.6 (23–74) | 52.8 (31–74) | 50.6 (23–72) | 0.41 |
| Gender (Male : Female) | 43:50 | 19:24 | 24:26 | 0.71 |
| BMI, kg/m2, mean ± SD | 23.0 ± 3.7 | 22.6 ± 3.1 | 23.3 ± 4.3 | 0.44 |
| Cause for ESRD | ||||
| DM | 34 (36.6) | 19 (44.2) | 15 (30.0) | 0.23 |
| HTN | 44 (47.3) | 19 (44.2) | 25 (50.0) | 0.73 |
| aOthers | 15 (16.1) | 5 (11.6) | 10 (20.0) | 0.66 |
| Use of steroid | 2 (2.2) | 1 (2.3) | 1 (2) | 1.0 |
| Previous TB treatment (%) | 0 (0) | 0 (0) | 0 (0) | 1.0 |
| Presence of BCG scar (%) | 62/93 (66.7) | 19/43 (44.2) | 43/50 (86.0) | 0.001 |
| Baseline QFT-IT + (%) | 39/93 (41.9) | 19/43 (44.2) | 20/50 (40.0) | 0.68 |
| 2nd QFT-IT + (%) | 32/93 (34.4) | b19/43 (44.2) | 13/50 (26.0) | 0.07 |
| Old TB lesion (%) | 35/93 (37.6) | 14/43 (32.6) | 21/50 (42.0) | 0.35 |
| LTBI treatment among initial QFT-IT + (%) | 18/39 (46.2) | 5/19 (26.3) | 13/20 (65.0) | 0.02 |
| Isoniazid: Rifampicin | 10:8 | 3:2 | 7:6 | 1.0 |
aOthers include autoimmune diseases, glomerulonephritis, polycystic kidney diseases, and unknown diseases
bOne of 19 patients showed conversion from negative to positive result
HD Hemo-dialysis, PD peritoneal dialysis, BMI body mass index, TB tuberculosis, LTBI latent TB infection, BCG bacille Calmette-Guérin, QFT-IT QuantiFERON-TB Gold In-Tube, SD standard deviation
Changes in QFT-IT result in ESRD patients between 0 and 4 months
The agreement between baseline QFT-IT and 2nd QFT at 4 month interval in 93 ESRD patients was excellent (90.3 %, kappa = 0.80, p < 0.001) (Table 2). Agreement between baseline QFT-IT and 2nd QFT-IT in HD (95.3 %, kappa = 0.91, p <0.001) was higher than in PD patients (86.0 %, kappa = 0.69, p < 0.001).
Table 2.
1st QFT-IT and 2nd QFT-IT test results in 93 ESRD patients
| Dialysis | 1st QFT-IT positive (n = 39a) | 1st QFT-IT negative (n = 54a) | Total | Kappa | P value | ||
|---|---|---|---|---|---|---|---|
| 2nd QFT-IT positive | 2nd QFT-IT negative | 2nd QFT-IT positive | 2nd QFT-IT negative | (N) | (%) | ||
| HD | 18/43 (41.9 %) | 1/43 (2.3 %) | 1/43 (2.3 %) | 23/43 (53.5 %) | 43 | 0.91 (95.3 %) | <0.001* |
| PD | 13/50 (26.0 %) | 7/50 (14.0 %) | 0/50 (0 %) | 30/50 (60.0 %) | 50 | 0.69 (86.0 %) | <0.001* |
| Total | 31/93 (33.3 %) | 8/93 (8.6 %) | 1/93 (1.1 %) | 53/93 (57.0 %) | 93 | 0.80 (90.3 %) | <0.001* |
aAmong 93 ESRD patients, 39 patients showed QFT-IT positive results and 54 patients showed QFT-IT negative results on baseline QFT-IT tests, respectively
*Difference for concordance between 1st QFT-IT and 2nd QFT-IT
QFT-IT QuantiFERON-TB Gold In-Tube, PD peritoneal dialysis, HD hemodialysis
Changes in QFT-IT among ESRD patients with 1st QFT-positive results
Among 39 patients who showed positive QFT-IT result at first testing, QFT-IT test reversion occurred in 8 (20.5 %) patients, of whom seven (87.5 %) were on PD, and one patient (12.5 %) was on HD [odds ratio = 9.7 (1.1–88.7), p = 0.04] (Table 3). However, conversion rate was not different between them (0 vs. 2.3 %, p > 0.05). The median actual interferon-gamma levels of QFT-IT in HD group and PD group at baseline were; 1.55 (IQR 0.7–3.7) and 5.03 (IQR 0.9–15.4) respectively. The median values after 4 months were: HD = 0.87 (IQR 0.6–3.4), and PD = 1.31 (IQR 0.2–4.5). The change in median values of QFT-IT between baseline and 4 months was significantly different with HD = 8 % decrease, and PD = 76 % (p < 0.001)
Table 3.
Reversion and non-reversion of QFT-IT among ESRD patients with 1st QFT-IT positive result
| ESRD patients (N = 39) | Reversion | Non-reversion | OR (95 % CI) | P value | |
|---|---|---|---|---|---|
| Dialysis method | |||||
| PD | 7 (35.0 %) | 13 (65.0 %) | 9.7 (1.1–88.7) | 0.04 | |
| HD | 1 (5.3 %) | 18 (94.7 %) | 1 (Ref.) | ||
| Treatment | |||||
| LTBI treatment | 5 (27.8 %) | 13 (72.2 %) | 2.3 (0.5–11.4) | 0.43 | |
| No LTBI Treatment | 3 (14.3 %) | 18 (85.7 %) | 1 (Ref.) | ||
| Treatment drug | |||||
| Rifampin | 3 (37.5 %) | 5 (62.5 %) | 2.4 (0.3–19.8) | 0.61 | |
| INH | 2 (20.0 %) | 8 (80.0 %) | 1 (Ref.) | ||
OR odds ratio, PD peritoneal dialysis, HD hemodialysis, LTBI latent tuberculosis infection, RFP rifampicin, INH isoniazid
Among the 39 with baseline positive IGRA tests, there was no significant difference in the percent decline in interferon-gamma levels of QFT-IT tests over 4 months among the 18 who received LTBI treatment group and the 21 who were not treated (Decrease of 64 % among treated vs. 43 % among untreated, p > 0.05). However, as seen in Fig. 1, median values decreased significantly in both groups over the 4 month interval. Reversion odds of the QFT-IT test in the groups who received, or did not receive LTBI treatment were not significant [odds of reversion = 2.3 (0.5–11.4)]. Furthermore, there were no difference in reversion odds of the serial QFT-IT test between those treated with RIF or INH [odds ratio = 2.4 (0.3–19.8)].
Fig. 1.
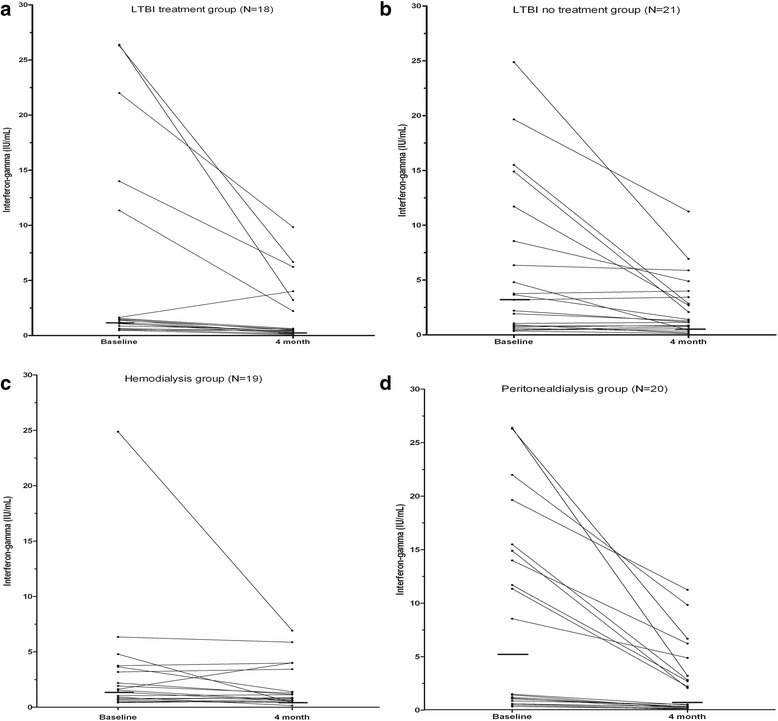
Changes of interferon-gamma levels over 4 months in those with positive QFT-IT at baseline. Paired changes of interferon-gamma levels in QFT-IT tests after 4 months in the LTBI treatment group (a) and in the LTBI no treatment group (b), as well as in the hemodialysis group (c) and in the peritoneal dialysis group (d). The horizontal bold lines at pre- and post-treatment values represent the median interferon-gamma values (a median 1.40 with IQR 0.8–12.0 and median 0.51 with IQR 0.3–3.4, b median 3.19 with IQR 0.8–10.1 and median 1.29 with IQR 0.7–3.7, c median 1.55 with IQR 0.7–3.7 and median 0.87 with IQR 0.6–3.4, d median 5.03 with IQR 0.9–15.4 and median 1.31 with IQR 0.2–4.5). QFT-IT: QuantiFERON-TB Gold In-Tube; IQR: interquartile range
Discussion
Within-subject variability of QFT-IT at 4 month interval in dialyzed ESRD patients was minimal. Reversion of QFT-IT after a 4 month interval was not related to LTBI treatment but was more frequent in PD patients than in HD patients.
QFT-IT in our study was checked in ESRD patients; the concordance rate in all ESRD patients was relatively high (90.3 %, kappa = 0.80), compared with previous study in which concordance rate at 1 year interval without LTBI treatment in ESRD patients was 70.4 % with T-SPOT-TB and 73.5 % with QFT-IT [19]. Furthermore, reversion rates after LTBI treatment in our study were relatively low (27.8 %, 5/18), compared with previous study in which IGRA reversion rates were 41.9 % with 4 months of rifampicin treatment [16]. Also, in case of conversion, only 1.9 % (1/54) HD patient showed conversion of QFT-IT in our study, which was relatively lower than 12.1 % in patients who was taking the immune-suppressive drugs at 8.5 month interval [20] and 6 % in ordinary patients with infectious disease at 3 month interval [21]. Compared with these studies, our result for ESRD patients with 4 month follow up showed low variance of IFN-gamma level. The reason why within-subject variability was low seems to be due to immune dysfunction of ESRD patients related to uremia and dialysis [11] as well as due to short term interval of QFT-IT follow up.
In our study, there is possibility that the LTBI treatment reduced the IFN-gamma level because 2nd IFN-gamma level decreased from baseline level more frequently in LTBI treatment group (17/18, 94.4 %) than in LTBI no treatment group (14/21, 66.7 %) (p = 0.049). However, the 2nd IFN-gamma level did not sufficiently decrease to reach to the defined cut-off level 0.35 IU/mL, and there were no difference in degree of decrease between two group (median value of percent decrease, 64.0 VS. 42.8 %, p > 0.05). Therefore, the threshold for IFN-gamma cut-off point must be considered to be re-defined which is optimal for distinguishing true reversion and non-specific variation.
The main reasons for the predominant reversion of QFT-IT in PD patients compared with HD patients may be the differences in immune activity and serum sampling time as well as in LTBI treatment rate (65.0 VS. 26.3 %, P = 0.02) between PD patients and HD patients. As seen in Fig. 1c and d, the median IFN-gamma levels on two time point were higher in PD patents than in HD patients, and the percent decrease in IFN-gamma level from baseline QFT-IT to sequential 4 month QFT-IT was significantly higher in PD patients than in HD patients (median value of percent decrease, 75.5 VS. 8.0 %, p < 0.001). This result could be occurred by accident, but T-SPOT TB which was reported to be equivalent to or inferior to QFT-IT in sensitivity [22] can be tested for reproducibility in PD patients to quantify the degree of decrease as another method. The explainable hypothesis for the difference of immune activity between HD and PD patients is that lymphopenia, decreased absolute counts of lymphocyte, and decreased production of interferon-gamma levels are more apparent in HD patients than in PD patients [23]. Circulating immune cells in PD patients may be more easily exhausted by chronic uremic activation [24]. Also, the timing in collecting the blood sample for QFT-IT could influence the variation of QFT-IT result of PD, because it was reported that the IFN-gamma level of post-dialysis could be reduced compared with that of pre-dialysis [25]. In our study, blood sampling was performed equally before dialysis in HD patients, but in PD patients, not equally before or after dialysis.
This study had some limitations. Firstly, the number of participants was small and the tuberculin skin tests were not performed in most of patients due to difficulty in follow up schedule for interpretation of TST results. Secondly, the timing for blood sampling in dialysis patients could not be equally conditioned for all subjects. Lastly, because the follow up interval is short, the serial extended follow up of QFT-IT at 9 months after LTBI treatment for more than 4 months is needed for confirming the variation of within-subject variability.
Conclusions
The concordance rate of QFT-IT for 4 month interval in dialyzed ESRD patients in a Korean population was excellent, and reversion seemed not to be associated with LTBI treatment. Further studies with extended follow up as well as with larger numbers of patients are needed to investigate the changes of QFT-IT including the effect of LTBI treatment in dialyzed ESRD patients.
Acknowledgements
We thank patients for their enthusiastic participation in this study. We gratefully acknowledge the technical support of two nurses, Jung-In Kim and Youn-Ju Lee, in the artificial kidney center. This study was helped by nephrology department in Busan Paik hospital and supported by a Korea University Grant (K1422351).
Footnotes
Yeong Hoon Kim and Dick Menzies contributed equally to this work.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
YHK and DM take responsibility for integrity of the data and the accuracy of the data analysis. SHL, YHK, and DM contributed to planning the study, collecting and analyzing the data, and writing the manuscript. HJK, SJP, THK, and SWK contributed to collecting the data. SJP contributed to performance of QFT-IT tests with interpretation. All authors read and approved the final version of the manuscript.
Contributor Information
Seung Heon Lee, Email: lee-sh@korea.ac.kr.
Hee Jin Kim, Email: hatchingbird@gmail.com.
Seok Ju Park, Email: psjgenesis@hanmail.net.
Tae Hee Kim, Email: thkim@paik.ac.kr.
So Jeong Park, Email: thwjd76@hanmail.net.
Sun Woo Kang, Email: kswnephrology@hotmail.com.
Yeong Hoon Kim, Email: yeonghnl@inje.ac.kr.
Dick Menzies, Email: Dick.Menzies@Mcgill.ca.
References
- 1.World Health Organization, Stop TB Partnership . The global plan to stop TB 2011–2015: transforming the fight towards elimination of tuberculosis. Geneva: World Health Organization; 2010. [Google Scholar]
- 2.Corbett EL, Watt CJ, Walker N, Maher D, Williams BG, Raviglione MC, et al. The growing burden of tuberculosis: global trends and interactions with the HIV epidemic. Arch Intern Med. 2003;163:1009–21. doi: 10.1001/archinte.163.9.1009. [DOI] [PubMed] [Google Scholar]
- 3.Dye C, Scheele S, Dolin P, Pathania V, Raviglione MC. Consensus statement. Global burden of tuberculosis: estimated incidence, prevalence, and mortality by country. WHO Global Surveillance and Monitoring Project. JAMA. 1999;282:677–86. doi: 10.1001/jama.282.7.677. [DOI] [PubMed] [Google Scholar]
- 4.Broekmans JF, Migliori GB, Rieder HL, Lees J, Ruutu P, Loddenkemper R, et al. European framework for tuberculosis control and elimination in countries with a low incidence. Recommendations of the World Health Organization (WHO), International Union Against Tuberculosis and Lung Disease (IUATLD) and Royal Netherlands Tuberculosis Association (KNCV) Working Group. Eur Respir J. 2002;19:765–75. doi: 10.1183/09031936.02.00261402. [DOI] [PubMed] [Google Scholar]
- 5.Jasmer RM, Nahid P, Hopewell PC. Clinical practice. Latent tuberculosis infection. N Engl J Med. 2002;347:1860–6. doi: 10.1056/NEJMcp021045. [DOI] [PubMed] [Google Scholar]
- 6.American Thoracic Society/Centers for Disease Control and Prevention. Targeted tuberculin testing and treatment of latent tuberculosis infection. Am J Respir Crit Care Med. 2000; 161:S221–47. [DOI] [PubMed]
- 7.World Health Organization . Global tuberculosis control: WHO report 2011. Geneva: World Health Organization; 2011. [Google Scholar]
- 8.Park SB, Suk J, Joo I, Kim HC, Cho WH, Park CH. Tuberculosis complicating kidney transplantation. J Korean Soc Transplant. 1995;9:95–102. [Google Scholar]
- 9.Abdel Halim M, Al-Otaibi T, Gheith O, El-Kholy O, Abdel Tawab K, Said T, et al. Toxic tacrolimus blood levels with rifampin administration in a renal transplant recipient. Ann Transplant. 2010;15:57–60. [PubMed] [Google Scholar]
- 10.Zamauskaite A, Perez-Cruz I, Yaqoob MM, Madrigal JA, Cohen SB. Effect of renal dialysis therapy modality on T cell cytokine production. Nephrol Dial Transplant. 1999;14:49–55. doi: 10.1093/ndt/14.1.49. [DOI] [PubMed] [Google Scholar]
- 11.Hauser AB, Stinghen AE, Kato S, Bucharles S, Aita C, Yuzawa Y, et al. Characteristics and causes of immune dysfunction related to uremia and dialysis. Perit Dial Int. 2008;28(Suppl 3):S183–7. [PubMed] [Google Scholar]
- 12.Shankar MS, Aravindan AN, Sohal PM, Kohli HS, Sud K, Gupta KL, et al. The prevalence of tuberculin sensitivity and anergy in chronic renal failure in an endemic area: tuberculin test and the risk of post-transplant tuberculosis. Nephrol Dial Transplant. 2005;20:2720–4. doi: 10.1093/ndt/gfi141. [DOI] [PubMed] [Google Scholar]
- 13.Poduval RD, Hammes MD. Tuberculosis screening in dialysis patients--is the tuberculin test effective? Clin Nephrol. 2003;59:436–40. doi: 10.5414/CNP59436. [DOI] [PubMed] [Google Scholar]
- 14.Diel R, Loddenkemper R, Nienhaus A. Predictive value of interferon-gamma release assays and tuberculin skin testing for progression from latent TB infection to disease state: a meta-analysis. Chest. 2012;142:63–75. doi: 10.1378/chest.1380697. [DOI] [PubMed] [Google Scholar]
- 15.Kim SH, Lee SO, Park JB, Park IA, Park SJ, Yun SC, et al. A prospective longitudinal study evaluating the usefulness of a T-cell-based assay for latent tuberculosis infection in kidney transplant recipients. Am J Transplant. 2011;11:1927–35. doi: 10.1111/j.1600-6143.2011.03625.x. [DOI] [PubMed] [Google Scholar]
- 16.Lee SH, Lew WJ, Kim HJ, Lee HK, Lee YM, Cho CH, et al. Serial interferon-gamma release assays after rifampicin prophylaxis in a tuberculosis outbreak. Respir Med. 2010;104:448–53. doi: 10.1016/j.rmed.2009.10.006. [DOI] [PubMed] [Google Scholar]
- 17.Ewer K, Millington KA, Deeks JJ, Alvarez L, Bryant G, Lalvani A. Dynamic antigen-specific T-cell responses after point-source exposure to Mycobacterium tuberculosis. Am J Respir Crit Care Med. 2006;174:831–9. doi: 10.1164/rccm.200511-1783OC. [DOI] [PubMed] [Google Scholar]
- 18.Wilkinson KA, Kon OM, Newton SM, Meintjes G, Davidson RN, Pasvol G, et al. Effect of treatment of latent tuberculosis infection on the T cell response to Mycobacterium tuberculosis antigens. J Infect Dis. 2006;193:354–9. doi: 10.1086/499311. [DOI] [PubMed] [Google Scholar]
- 19.Chung WK, Zheng ZL, Kim HS, Park JW, Lee HJ, Chang JH, et al. Serial testing of interferon-gamma-release assays for the diagnosis of latent tuberculosis in hemodialysis patients. J Infect. 2010;61:144–9. doi: 10.1016/j.jinf.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 20.Kim KH, Lee SW, Chung WT, Kim BG, Woo KS, Han JY, et al. Serial interferon-gamma release assays for the diagnosis of latent tuberculosis infection in patients treated with immunosuppressive agents. Korean J Lab Med. 2011;31:271–8. doi: 10.3343/kjlm.2011.31.4.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Perry S, Sanchez L, Yang S, Agarwal Z, Hurst P, Parsonnet J. Reproducibility of QuantiFERON-TB gold in-tube assay. Clin Vaccine Immunol. 2008;15:425–32. doi: 10.1128/CVI.00398-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Triverio PA, Bridevaus PO, Roux-Lombard P, Niksic L, Rochat T, Martin PY, et al. Interferon-gamma release assays versus tuberculin skin testing for detection of latent tuberculosis in chronic haemodialysis patients. Nephrol Dial Transplant. 2009;24:1952–6. doi: 10.1093/ndt/gfn748. [DOI] [PubMed] [Google Scholar]
- 23.Griveas I, Visvardis G, Fleva A, Papadopoulou D, Mitsopoulos E, Kyriklidou P, et al. Comparative analysis of immunophenotypic abnormalities in cellular immunity of uremic patients undergoing either hemodialysis or continuous ambulatory peritoneal dialysis. Ren Fail. 2005;27:279–82. doi: 10.1081/JDI-200056620. [DOI] [PubMed] [Google Scholar]
- 24.Ando M, Shibuya A, Yasuda M, Azuma N, Tsuchiya K, Akiba T, et al. Impairment of innate cellular response to in vitro stimuli in patients on continuous ambulatory peritoneal dialysis. Nephrol Dial Transplant. 2005;20:2497–503. doi: 10.1093/ndt/gfi048. [DOI] [PubMed] [Google Scholar]
- 25.Hursitoglu M, Cikrikcioglu MA, Tukek T, Beycan I, Ahmedova N, Karacuha S, et al. Acute effect of low-flux hemodialysis process on the results of the interferon-gamma-based QuantiFERON-TB Gold In-Tube test in end-stage renal disease patients. Transpl Infect Dis. 2009;11:28–32. doi: 10.1111/j.1399-3062.2008.00348.x. [DOI] [PubMed] [Google Scholar]


