Abstract
Background
Overweight and obese older adults have high sedentary time. We tested the feasibility and preliminary effects of a sedentary time reduction intervention among adults over age 60 with a body mass index over 27 kg/m2 using a nonrandomized one arm design.
Methods
Participants (N = 25, Mean Age = 71.4, Mean BMI = 34) completed an 8-week theory-based intervention targeting reduced total sitting time and increased sit-to-stand transitions. An inclinometer (activPAL™) measured the primary outcomes, change in total sitting time and sit-to-stand transitions. Secondary outcomes included physical activity (ActiGraph GT3X+ accelerometer), self-reported sedentary behaviors, physical function (Short Physical Performance Battery), depressive symptoms (PHQ-8), quality of life (PROMIS), and study satisfaction. Paired t-tests examined pre-post test changes in sitting time, sit-to-stand transitions, and secondary outcomes.
Results
Inclinometer measured sitting time decreased by 27 minutes/day (p < .05) and sit-to-stand transitions increased by 2 per day (p > .05) while standing time increased by 25 minutes/day p < .05). Accelerometer measured sedentary time, light-intensity and moderate-to-vigorous physical activity improved (all p values ≤ .05). Self-reported sitting time, gait speed, and depressive symptoms also improved (all p values < .05). Effect sizes were small. Study satisfaction was high.
Conclusions
Reducing sitting time is feasible and the intervention shows preliminary evidence of effectiveness among older adults with overweight and obesity. Randomized trials of sedentary behavior reduction in overweight and obese older adults, most of whom have multiple chronic conditions, may be promising.
Keywords: aging, physical activity, intervention
Introduction
Sedentary behaviors are characterized by a sitting or lying posture and low energy expenditure (Sedentary Behaviour Research Network, 2012). In older adults, sedentary time is related to obesity, cardiovascular disease, diabetes, and mortality even after adjustment moderate-to-vigorous physical activity (Leon-Munoz et al., 2013; Proper, Singh, van Mechelen, & Chinapaw, 2011; Wilmot et al., 2012). Overweight and obese older adults have low levels of physical activity, high sedentary time, and often have multiple chronic conditions (Evenson, Buchner, & Morland, 2012; Morrato, Hill, Wyatt, Ghushchyan, & Sullivan, 2007; Seguin et al., 2012). A variety of physical, motivational, and environmental barriers to exercise may hinder older adults with obesity from engaging in sufficient physical activity compared to their normal weight peers (Godin, Amireault, Belanger-Gravel, Vohl, & Perusse, 2009; Lee, Ory, Yoon, & Forjuoh, 2013; Schutzer & Graves, 2004). Reduction of sedentary time could be a more achievable goal for modifying chronic disease risk factors (Davis et al., 2011; Evenson et al., 2012; Matthews et al., 2008). To date, no randomized trials have documented the health benefits of reducing sedentary time in older adults with overweight and obesity, but before randomized trials can be conducted, the feasibility of reducing sedentary time in this population needs to be assessed.
There are two previous short-term pilot studies examining the feasibility of reducing sedentary time in adults over age 60 (neither focused on adults who were overweight or obese). In a four week pre-test post-test study (N = 24), participants had a 24 minute/day reduction in sitting/lying time measured by inclinometers (activPAL™) and a 13 minute/day increase in stepping time (mean baseline participant body mass index [BMI] = 26.2 kg/m2) (Fitzsimons et al., 2013). Gardiner and colleagues conducted a 2-week intervention and found a 30 minute/day decrease in sedentary activity measured by Actigraph accelerometer (Gardiner, Eakin, Healy, & Owen, 2011).
Feasibility testing has been limited to short-term interventions with only 1 or 2 intervention contacts (Fitzsimons et al., 2013; Gardiner et al., 2011). In addition, previous intervention studies have only reported changes in sedentary behavior and have not examined impacts on other health outcomes such as depressive symptoms and physical function. The purpose of our study was to examine the feasibility of a longer (8 week) theory-based intervention to reduce sitting time in older adults with overweight and obesity. We also explored the effect of the intervention on our primary outcomes, reduction in total sitting time and increase in sit-to-stand transitions, and secondary outcomes including physical function and depressive symptoms.
Methods
We conducted a one-arm pre-test post-test study called Take Active Breaks from Sitting (TABS) Pilot Study in Seattle, WA during 2013-2014. Study procedures were approved by the Group Health Research Institute Institutional Review Board.
Participants and Setting
Participants were recruited from March 2013-May 2014 through the patient panels of a primary care clinic located within a large integrated health system in Washington State, USA. We used electronic health records to randomly select a group of patients over age 60 and with a body mass index (BMI) ≥ 27 kg/m2. Recruitment letters were sent and interested individuals were invited to call a study line to discuss the study with a member of the research staff. During the telephone call, participants were screened for eligibility criteria, provided oral informed consent, and scheduled a baseline in-person assessment. Eligibility criteria were: self-report sitting time over 7 hours per day (confirmed with objective monitoring at baseline, described below), able to stand, and able to walk one block.
Procedures
A study research specialist conducted in-person assessments at the participants' primary care clinic at baseline (pre-test) and post-test (8 weeks). During the visit, participants completed several tasks (e.g. height, weight, physical function) and completed a survey. Participants were fit with activity monitoring devices (thigh worn inclinometer and waist worn accelerometer) to wear for 7 days at baseline and 8 weeks. They were instructed to wear the devices for 7 days, only removing them to go to sleep, bathe/shower, or swim. They were given a log to record device wear time and instructed to return the devices by mail using pre-stamped addressed envelopes. In addition to in-person measurement visits at baseline and 8 weeks, participants were mailed the inclinometer to wear for 7 days at the mid-point of the study (about 3 weeks into the intervention),. Participants received $15 after completing the baseline visit, $10 after the mid-point inclinometer wear, and $15 after the post-test visit.
Intervention
The Take Active Breaks from Sitting (TABS) intervention consisted of five phone calls delivered over an 8 week period by a health coach using social cognitive theory constructs adapted from Gardiner's Stand Up For Your Health intervention (Gardiner et al., 2011; McAlister, Perry, & Parcel, 2008). Social cognitive theory emphasizes the dynamic interaction among personal, behavioral, and environmental influences on behavior (reciprocal determinism) (McAlister et al., 2008). Specific strategies used in the TABS intervention are described according to the behavior change technique taxonomy in Table 1 (Michie et al., 2011; Michie et al., 2013). The initial phone call lasted about 30 minutes with follow-up calls 2, 3, 5 and 7 weeks later each of which lasted about 20 minutes. A motivational interviewing style was used by the phone coaches in order to support self-efficacy and engage participants in working on their goals in a manner that is non-threatening and supportive of participant values and preferences (Miller & Rose, 2009). Participants set personalized goals to help them ultimately achieve two goals: 1) a decrease in total sitting time by 2 hours per day through more standing and moving; and, 2) an additional 15 breaks from sitting (i.e. increase in the number of sit-to-stand transitions) throughout the day. Participants were also mailed graphical feedback charts depicting their sitting time, standing time, stepping time, and sit-to-stand transitions after each week they wore the inclinometer. After the baseline devices were received, the first feedback chart was mailed along with a study workbook, and self-monitoring logs. Health coaches were masters' level research assistants and post-doctoral fellows who were trained and received on-going supervision from the study PI who is a clinical health psychologist.
Table 1. Take Active Breaks from Sitting Intervention Theoretical Underpinnings and Techniques.
| Social cognitive theory constructs | Behavior Change Techniques (from Michie's taxonomy) |
|---|---|
| Self-regulation strategies |
|
| Facilitation |
|
| Self-efficacy |
|
| Outcome expectations |
|
Measurement
Primary outcomes
The primary outcomes were total sitting time and sit-to-stand transitions as measured by a thigh worn inclinometer worn for one-week at baseline, 3 weeks, and post-test (8 weeks) (activPAL™, Glasgow, Scotland). The device is small, lightweight and unobtrusive and was affixed to the front of the thigh with a mild gel. The activPAL has been tested for reliability and validity, has been used with older adults, and is considered the current most valid objective measure of sedentary behavior (Grant, Dall, Mitchell, & Granat, 2008; Hart, Ainsworth, & Tudor-Locke, 2011; Kozey-Keadle, Libertine, Lyden, Staudenmayer, & Freedson, 2011; Kozey-Keadle, Libertine, Staudenmayer, & Freedson, 2012). Time spent sitting/lying and sit-to-stand transitions per day were calculated using proprietary activPAL3™ software. Non-wear time was determined by log entries and removed from analysis. Other inclinometer outcomes included time spent standing and stepping and the percent of the day spent sitting, standing, and stepping while wearing the device (to adjust for wear time).
Secondary outcomes
Objective physical activity was measured with a waist worn accelerometer (Actigraph wGT3X+, Pensalcola, FL). The Actigraph is reliable (Esliger & Tremblay, 2006; Santos-Lozano et al., 2012) and valid among older adults (Buman et al., 2010; Pruitt et al., 2008), people with mobility limitations (Pruitt et al., 2008), and obese adults (Colbert, Matthews, Havighurst, Kim, & Schoeller, 2011; Kozey-Keadle et al., 2011; Lopes, Magalhaes, Bragada, & Vasques, 2009). Accelerometer data were processed using ActiLife Version 6.8.0 with data captured in 60 second epochs with the low frequency extension enabled. Sedentary activity was considered as time spent at < 100 counts per minute, light activity as counts between 100 and 1951, and moderate or higher intensity activity at counts above 1951 (Freedson, Melanson, & Sirard, 1998). We also classified the number of breaks from sedentary time as the number of times counts went above the 100 cut point threshold for one minute or more.
The Short Physical Performance Battery (SPPB) was used to assess lower extremity balance, gait speed (time to walk a 3 meter course), and strength (time it takes to complete 5 chair stands) (Guralnik, Ferrucci, Simonsick, Salive, & Wallace, 1995; Guralnik et al., 1994). Participants had their height (inches) and weight (pounds) measured using a portable digital scale (Tanita HD-35, Arlington Heights, IL) and stadiometer (Seca 213, Chino, CA). BMI was calculated as [weight/(height2)] × 703.
The survey assessed self-reported sitting time using the International Physical Activity Questionnaire (IPAQ) and sedentary behavior with items from the Sedentary Behavior Questionnaire both of which have adequate reliability and validity (Rosenberg, Bull, Marshall, Sallis, & Bauman, 2008; Rosenberg et al., 2010). The 8-item Patient Health Questionnaire (PHQ-8) measured depressive symptoms; higher scores represent more depressive symptoms and scores ≥ 10 indicate a depressive disorder (Kroenke et al., 2009). The 10-item PROMIS Global Health short form version 1.1 was used to capture physical and mental health quality of life (Hays, Bjorner, Revicki, Spritzer, & Cella, 2009). Raw scores are translated into T-scores such that a score of 50 represents the average for the US general population with a standard deviation of 10 points. Higher scores indicate better physical and mental health quality of life.
The baseline survey also assessed demographic characteristics and chronic conditions (a checklist of 9 conditions including arthritis, high cholesterol, lung disease, high blood pressure, diabetes, stroke, arthritis, cancer, and osteoporosis). The post-test survey also asked several items to assess helpfulness of TABS materials and components on a 0 to 3 scale (0 = did not use, 1 = not helpful; 2 = somewhat helpful, 3 = very helpful) as well as study satisfaction on a 0 to 3 scale (0 = not at all satisfied, 1 = not very satisfied, 2 = somewhat satisfied, 3 = very satisfied).
Data Analysis
We conducted paired t-tests using SPSS Version 22 (IBM, 2013) to assess change from baseline to mid-point and baseline to post-test among those who had complete data (resulting in different sample sizes between primary and secondary outcomes). The level of significance was set at .05. Due to the small sample size, we calculated Cohen's D values as an estimate of the effect sizes (interpreted as small, .20, medium, .50, and large, .80) (Cohen, 1988).
Results
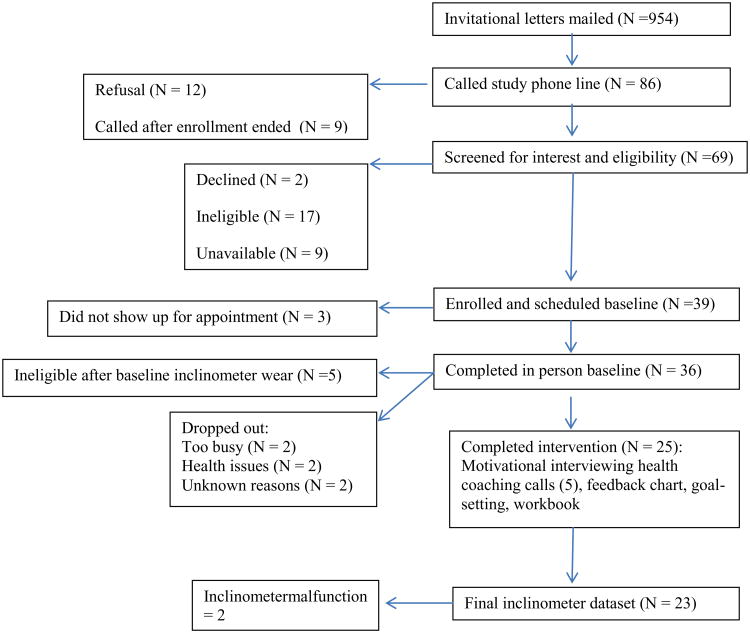
A total of 36 participants were consented to participate and completed baseline measures (see Figure 1). Non-completers (N = 12) did not differ from completers based on BMI, age, gender, physical function or self-reported ST. Completers had an average of 2.65 chronic conditions including hypertension (N = 12), high cholesterol (N = 12), diabetes (n = 7), arthritis (N = 10), and cancer (N = 8; 4 prostate and 3 breast; 1 unknown type). The mean age was 71.4 years (range 60-84, standard deviation 6.4), 70% were female, 91% were non-Hispanic white, 74% had a college degree or higher, 61% were retired, 13% worked full time, 13% used an assistive device, 61% were married, and mean BMI was 34 kg/m2 (range = 27 to 47). No study-related adverse events were reported.
Figure 1. Take Active Breaks from Sitting Pilot Study Flow Diagram.
Primary Inclinometer Outcomes
Mean inclinometer wear time was 6.4 days and 13.7 hours per day at baseline and 6.6 days and 13.7 hours per day at post-test. Inclinometer measured sitting time ranged from 7.2 to 13.8 hours/day at baseline and 4.2 to 12.9 hours/day at post-test. From baseline to post-test, there were improvements in inclinometer measured sitting time (27 minutes/day), standing time (24.6 minutes/day), percent of the day spent standing (3%) and a decrease in percent of the day spent sitting (-3%) from baseline to post-test (see Table 2). While not meeting statistical significance, there were increases in sit-to-stand transitions (2.17/day), stepping time (6.6 minutes/day), steps (574/day), and percent of the day stepping (1%) from baseline to post-test. The mid-point analysis suggested that most changes were made by the mid-term evaluation and sustained at post-test (see Table 2).
Table 2. Changes in Primary (Inclinometer) Outcomes at Baseline, Mid-Point, and Post-Test (N=23).
| Baseline Mean (SD) | Mid-point Mean(SD) a | p-value (baseline-mid) | Post-test Mean (SD) | p-value (mid-post) | p-value (pre-post) | Effect size (d; pre-post)b | |
|---|---|---|---|---|---|---|---|
| Sitting time (hours/day) | 9.22 (1.70) | 8.79 (1.76) | .05 | 8.77 (1.86) | .88 | .04 | .25 |
| Sit to stand transitions (per day) | 37.06 (9.81) | 36.48 (7.49) | .98 | 39.23 (10.34) | .19 | .13 | .22 |
| Standing time (hours/day) | 3.28 (1.14) | 3.78 (1.47) (1.50) | .01 | 3.69 (1.27) | .60 | .04 | .34 |
| Stepping (hours/day) | 1.18 (.50) | 1.26 (.44) | .26 | 1.29 (.68) | .61 | .13 | .16 |
| Steps per day | 5400.6 (2491.47) | 5834.42 (3258.80) | .17 | 5974.02 (3456.20) | .67 | .13 | .16 |
| Sitting (% of day while worn) | .67 (.10) | .64 (.13) | .01 | .64 (.12) | .85 | .02 | .34 |
| Standing (% of day while worn) | .24 (.08) | .27 (.10) | .01 | .27 (.09) | .60 | .03 | .33 |
| Stepping (% of day while worn) | .09 (.04) | .09 (.05) | .52 | .10 (.05) | .34 | .11 | .15 |
N = 22
Effect sizes of .20 are considered small, .50 medium, and .80 large
Based on the inclinometer data, 19 out of 23 participants (83%) improved either total sitting time or sit-to-stand transitions. For sitting time, 16 out of 23 participants (70%) had a reduction from baseline to post-test. Among the 16 participants that reduced their sitting time, the decrease in sitting time was 53 minutes/day on average (9.23 hours/day at baseline; 8.35 hours/day at post-test; p < .01; baseline percent of day sitting = 66% and 60% at post-test; p < .01). However only 1 participant met the goal of reducing sitting time by 2 hours or more per day. Fourteen out of 23 participants (61%) increased sit-to-stand transitions; the average increase in sit-to-stand transitions among these 14 participants was 6 per day (36 at baseline and 42 at post-test, p < .01). However, no one achieved 15 or more additional sit-to-stand transitions per day.
Secondary Outcomes
Accelerometer measures of sedentary time, light activity, and moderate-to-vigorous activity also improved from baseline to post-test (see Table 3). According to the accelerometer, sedentary time decreased by 23.25 minutes/day, light-intensity activity increased by 21.32 minutes/day, and moderate-to-vigorous activity increased by 3.7 minutes/day.
Table 3. Changes in Secondary Outcomes at Baseline and Post-test.
| Self-reportedSedentary Behavior N = 23 |
Pre-test Mean (SD) | Post-test Mean (SD) | p-value | Effect size (d) a |
|---|---|---|---|---|
| TV (hours/day) | 3.04 (1.93) | 3.33 (2.41) | .49 | .13 |
| Computer (hours/day; N = 22) | 2.91 (2.65) | 2.01 (1.64) | .08 | .39 |
| Week day sitting (hours/day) | 8.38 (2.54) | 6.57 (2.89) | .01 | .66 |
| Weekend day sitting (hours/day) | 7.48 (2.50) | 6.52 (2.80) | .02 | .36 |
|
Actigraph N = 22 |
||||
| Sedentary time(hours/day) | 9.55 (1.74) | 9.17 (1.78) | .02 | .22 |
| Sedentary time (% of day) | .67 (.09) | .64 (.10) | .02 | .29 |
| Sedentary Breaks Per Day | 75.51 (16.12) | 78.50 (12.68) | .30 | .20 |
| Light activity (% of day) | .31 (.08) | .34 (.09) | .02 | .30 |
| Light PA (hours/day) | 4.41 (1.14) | 4.77 (1.18) | .05 | .31 |
| Moderate-to-vigorous PA (hours/week) | 1.59 (1.90) | 2.02 (2.64) | .03 | .10 |
|
Short Physical Performance Battery N = 23 |
||||
| Chair stands (seconds) | 11.26 (3.36) | 10.91 (2.77) | .46 | .11 |
| Gait speed (seconds) | 3.80 (.64) | 3.38 (.64) | .01 | .52 |
| SPPB total score | 10.52 (1.73) | 10.74 (1.57) | .37 | .14 |
|
BMI (N = 23) (kg/m2) |
34.07 (4.85) | 33.97 (4.74) | .53 | .02 |
|
Weight (N = 23) (pounds) |
204.64 (29.85) | 203.37 (29.73) | .07 | .04 |
| PHQ-8 score (N = 20)b | 3.10 (2.63) | 2.10 (2.20) | .03 | .37 |
| Quality of life- Mental health (N = 23) | 51.97 (8.06) | 52.24 (8.89) | .84 | .03 |
| Quality of life- Physical health (N = 23) | 48.86 (6.80) | 48.90 (7.59) | .97 | .01 |
Effect sizes of .20 are considered small, .50 medium, and .80 large
Due to non-normality, the natural log transform of the PHQ8 was analyzed for significance tests. Means and standard deviations are in the standard metric.
Self-reported weekday and weekend sitting time was lower at post-test compared to baseline (see Table 3). There was no change in television or computer time. While physical function overall was high, gait speed improved. Depressive symptoms, while below cut-offs indicating any mild-to-moderate depression, also improved. Neither mental nor physical quality of life measures significantly improved.
Acceptability
Satisfaction ratings were high with 100% of completers reporting they were somewhat or very satisfied with the number, length and content of calls as well as the study as a whole for helping them to decrease their sitting time. The workbook and self-monitoring logs had lower ratings of helpfulness with 19% reporting they did not use the workbook and 28.5% reporting they did not use the logs. Among those that used the workbook and logs, 100% found the workbook somewhat or very helpful while 87% of those that used the logs reported them to be somewhat or very helpful. Phone calls were rated highly (95% reported finding them somewhat or very helpful) as were the feedback charts (100% reported them to be somewhat or very helpful).
Discussion
We found preliminary evidence that a behavioral sedentary time reduction program is feasible and acceptable among older adults with overweight and obesity, most of whom had multiple chronic conditions. Furthermore, 83% improved sitting time, sit-to-stand transitions, or both. However, our goals of a 2 hour per day reduction or an increase of 15 sit-to-stand transitions was not achievable given the current intervention strategies. Additionally, we observed the most change during the first few weeks of the study (mid-point) with maintenance at the 8 week post-test. This suggests that change in sedentary time can occur fairly quickly and can continue to improve and/or be maintained over a 2 month period. However, additional adaptive strategies may be necessary to support larger improvements in sitting time and sit-to-stand transitions after the one-month mark. Overall, we found a modest 27 minute per day decrease in sitting time, or a 3% decrease in sitting time, and a small overall improvement in sit-to-stand transitions. Those that improved sitting time or sit-to-stand transitions had larger improvements on both outcomes. We also found improvements in light and moderate-to-vigorous physical activity.
Our 27 minute decrease in sitting time in a more overweight population than previously researched represents a small effect size which is comparable to previous studies in the general older adult population (Fitzsimons et al., 2013; Gardiner et al., 2011). Compared to Fitzsimons et al. (2013), we found larger effect sizes for increased standing time (.34 vs. .15) but smaller effect sizes for stepping time (.16 vs. .39) suggesting that our participants decreased sitting time by standing more whereas Fitzsimons' participants decreased sitting time by stepping more. Fitzsimons (2013) and Gardiner (2011) found decreases in TV viewing while we did not. More research to understand the best types of goal targets for older adults with overweight and obesity and the health benefits of small amounts of increased standing time is needed.
We found that gait speed significantly improved by almost 0.5 seconds. Perera et al. noted that a change of .05 m/s indicates a small change and .10 m/s indicates a substantial change in gait speed on the 6-meter usual pace gait speed task (Perera et al., 2014). While we used a shorter course, this could suggest a small but clinically meaningful improvement in gait speed (from 0.79 m/s at baseline to 0.89 m/s at follow-up).
Satisfaction with the study appeared high. Participants found the feedback charts most helpful followed by phone coaching calls. Those that used self-monitoring logs found them helpful but there were many reports that these were too burdensome. We also conducted qualitative exit-interviews with the participants and those findings provide additional evidence of the acceptability and feasibility of reducing sedentary behavior in this population highlighting barriers and motivators (Greenwood-Hickman, Renz, & Rosenberg, 2014).
Overall, effect sizes for sedentary behavior reduction in our study, as well as previously published studies, are small. Of note, a recent 6 month randomized controlled pilot study among sedentary adults found a non-significant 16 minute per day reduction in sitting time among the intervention group (Aadahl et al., 2014). However, there were significant improvements in fasting insulin levels and measured waist circumference for those receiving the intervention in that study (Aadahl et al., 2014). A clear threshold for achieving sedentary behavior reductions which will promote health improvements is unclear at this time. However, our results showing improved function as well as results by Aadahl et al. (2014) suggest that small changes may be meaningful to health.
Key strengths of our study were the longer study duration, additional intervention contacts compared to earlier studies, and the focus on a more overweight and obese participant sample than prior studies. Additionally, the intervention was delivered by phone in order to reduce barriers to behavior change and support future dissemination efforts based on prior work in smoking cessation (Lichtenstein, Zhu, & Tedeschi, 2010), physical activity in older adults (Muller & Khoo, 2014), and cardiac rehabilitation (Kotb, Hsieh, & Wells, 2014). Our study used multiple indicators of sitting time (e.g. self-report, inclinometer, accelerometer). The two objective measures yielded similar estimates of total sitting time and decreases in sitting time. Self-reported decreases in sitting time were much larger than the inclinometer or accelerometer data suggested. An important limitation of our study is that participants comprised a volunteer sample which was predominantly white and highly educated and who may differ in their motivation and behaviors compared to the general population of older adults with overweight and obesity. In addition, our study lacked a comparison group which would have enabled a better understanding of the effects of measurement and would have better controlled for events that could disrupt sedentary time (e.g. illness, vacation, retirement). Finally, we conducted a large number of analyses given our small study sample so our significant findings must be interpreted with caution and should be confirmed in future studies with larger samples.
In conclusion, we found that a theory-based intervention to reduce sitting time and increase sit-to-stand transitions in a convenience sample of older adults with overweight and obesity was feasible and acceptable. In addition, our brief intervention shows preliminary evidence of effectiveness. Given our results and the high prevalence of sedentary behaviors among older adults with overweight and obesity and low levels of physical activity, interventions to improve sedentary behaviors may be a practical behavioral target.
References
- Aadahl M, Linneberg A, Moller TC, Rosenorn S, Dunstan DW, Witte DR, Jorgensen T. Motivational Counseling to Reduce Sitting Time: A Community-Based Randomized Controlled Trial in Adults. Am J Prev Med. 2014 doi: 10.1016/j.amepre.2014.06.020. [DOI] [PubMed] [Google Scholar]
- Buman MP, Hekler EB, Haskell WL, Pruitt L, Conway TL, Cain KL, et al. King AC. Objective light-intensity physical activity associations with rated health in older adults. Am J Epidemiol. 2010;172(10):1155–1165. doi: 10.1093/aje/kwq249. doi:kwq249[pii]10.1093/aje/kwq249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- Colbert LH, Matthews CE, Havighurst TC, Kim K, Schoeller DA. Comparative validity of physical activity measures in older adults. Med Sci Sports Exerc. 2011;43(5):867–876. doi: 10.1249/MSS.0b013e3181fc7162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis MG, Fox KR, Hillsdon M, Sharp DJ, Coulson JC, Thompson JL. Objectively measured physical activity in a diverse sample of older urban UK adults. Med Sci Sports Exerc. 2011;43(4):647–654. doi: 10.1249/MSS.0b013e3181f36196. [DOI] [PubMed] [Google Scholar]
- Esliger DW, Tremblay M. Technical reliability assessment of three accelerometer models in a mechanical setup. Med Sci Sports Exerc. 2006;38(12):2173–2181. doi: 10.1249/01.mss.0000239394.55461.08. [DOI] [PubMed] [Google Scholar]
- Evenson KR, Buchner DM, Morland KB. Objective measurement of physical activity and sedentary behavior among US adults aged 60 years or older. Prev Chronic Dis. 2012;9:E26. Comparative Study Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S. doi:E26[pii] [PMC free article] [PubMed] [Google Scholar]
- Fitzsimons CF, Kirk A, Baker G, Michie F, Kane C, Mutrie N. Using an individualised consultation and activPAL feedback to reduce sedentary time in older Scottish adults: results of a feasibility and pilot study. Prev Med. 2013;57(5):718–720. doi: 10.1016/j.ypmed.2013.07.017. doi:S0091-7435(13)00269-7[pii]10.1016/j.ypmed.2013.07.017. [DOI] [PubMed] [Google Scholar]
- Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications, Inc. accelerometer. Med Sci Sports Exerc. 1998;30(5):777–781. doi: 10.1097/00005768-199805000-00021. [DOI] [PubMed] [Google Scholar]
- Gardiner PA, Eakin EG, Healy GN, Owen N. Feasibility of reducing older adults' sedentary time. Am J Prev Med. 2011;41(2):174–177. doi: 10.1016/j.amepre.2011.03.020. doi:S0749-3797(11)00266-2[pii]10.1016/j.amepre.2011.03.020. [DOI] [PubMed] [Google Scholar]
- Godin G, Amireault S, Belanger-Gravel A, Vohl MC, Perusse L. Prediction of leisure-time physical activity among obese individuals. Obesity (Silver Spring) 2009;17(4):706–712. doi: 10.1038/oby.2008.599. Research Support, Non-U.S. Gov't. [DOI] [PubMed] [Google Scholar]
- Grant PM, Dall PM, Mitchell SL, Granat MH. Activity-monitor accuracy in measuring step number and cadence in community-dwelling older adults. J Aging Phys Act. 2008;16(2):201–214. doi: 10.1123/japa.16.2.201. [DOI] [PubMed] [Google Scholar]
- Greenwood-Hickman MA, Renz A, Rosenberg D. Motivators and barriers to reducing sedentary behavior among overweight and obese older adults. Gerontologist. 2014 doi: 10.1093/geront/gnu163. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332(9):556–561. doi: 10.1056/NEJM199503023320902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. Wallace RB. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85–M94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- Hart TL, Ainsworth BE, Tudor-Locke C. Objective and subjective measures of sedentary behavior and physical activity. Med Sci Sports Exerc. 2011;43(3):449–456. doi: 10.1249/MSS.0b013e3181ef5a93. [DOI] [PubMed] [Google Scholar]
- Hays RD, Bjorner JB, Revicki DA, Spritzer KL, Cella D. Development of physical and mental health summary scores from the patient-reported outcomes measurement information system (PROMIS) global items. Qual Life Res. 2009;18(7):873–880. doi: 10.1007/s11136-009-9496-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IBM. IBM SPSS Statistics for Windows (Version 22.0) Armonk, NY: IBM Corp; 2013. [Google Scholar]
- Kotb A, Hsieh S, Wells GA. The Effect of Telephone Support Interventions on Coronary Artery Disease (CAD) Patient Outcomes during Cardiac Rehabilitation: A Systematic Review and Meta-Analysis. PLoS One. 2014;9(5):e96581. doi: 10.1371/journal.pone.0096581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozey-Keadle S, Libertine A, Lyden K, Staudenmayer J, Freedson PS. Validation of wearable monitors for assessing sedentary behavior. Med Sci Sports Exerc. 2011;43(8):1561–1567. doi: 10.1249/MSS.0b013e31820ce174. Research Support, Non-U.S. Gov't Validation Studies. [DOI] [PubMed] [Google Scholar]
- Kozey-Keadle S, Libertine A, Staudenmayer J, Freedson P. The feasibility of reducing and measuring sedentary time among overweight, non-exercising office workers. J Obes. 2012;2012:282303. doi: 10.1155/2012/282303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009;114(1-3):163–173. doi: 10.1016/j.jad.2008.06.026. Comparative Study. [DOI] [PubMed] [Google Scholar]
- Lee C, Ory MG, Yoon J, Forjuoh SN. Neighborhood walking among overweight and obese adults: age variations in barriers and motivators. J Community Health. 2013;38(1):12–22. doi: 10.1007/s10900-012-9592-6. [DOI] [PubMed] [Google Scholar]
- Leon-Munoz LM, Martinez-Gomez D, Balboa-Castillo T, Lopez-Garcia E, Guallar-Castillon P, Rodriguez-Artalejo F. Continued sedentariness, change in sitting time, and mortality in older adults. Med Sci Sports Exerc. 2013;45(8):1501–1507. doi: 10.1249/MSS.0b013e3182897e87. Research Support, Non-U.S. Gov't. [DOI] [PubMed] [Google Scholar]
- Lichtenstein E, Zhu SH, Tedeschi GJ. Smoking cessation quitlines: an underrecognized intervention success story. Am Psychol. 2010;65(4):252–261. doi: 10.1037/a0018598. Research Support, N.I.H., Extramural Research Support, U.S. Gov't, Non-P.H.S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopes VP, Magalhaes P, Bragada J, Vasques C. Actigraph calibration in obese/overweight and type 2 diabetes mellitus middle-aged to old adult patients. J Phys Act Health. 2009;6(Suppl 1):S133–140. doi: 10.1123/jpah.6.s1.s133. [DOI] [PubMed] [Google Scholar]
- Matthews CE, Chen KY, Freedson PS, Buchowski MS, Beech BM, Pate RR, Troiano RP. Amount of time spent in sedentary behaviors in the United States, 2003-2004. Am J Epidemiol. 2008;167(7):875–881. doi: 10.1093/aje/kwm390. doi:kwm390[pii]10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAlister AL, Perry CL, Parcel GS. How individuals, environments, and health behaviors interact. In: Glanz K, Rimer BK, Viswanath K, editors. Health Behavior and Health Education. San Francisco: Josey-Bass; 2008. pp. 169–188. [Google Scholar]
- Michie S, Ashford S, Sniehotta FF, Dombrowski SU, Bishop A, French DP. A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: the CALO-RE taxonomy. Psychol Health. 2011;26(11):1479–1498. doi: 10.1080/08870446.2010.540664. [DOI] [PubMed] [Google Scholar]
- Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. Wood CE. The Behavior Change Technique Taxonomy (v1) of 93 Hierarchically Clustered Techniques: Building an International Consensus for the Reporting of Behavior Change Interventions. Ann Behav Med. 2013 doi: 10.1007/s12160-013-9486-6. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rose GS. Toward a theory of motivational interviewing. Am Psychol. 2009;64(6):527–537. doi: 10.1037/a0016830. Research Support, N.I.H., Extramural Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrato EH, Hill JO, Wyatt HR, Ghushchyan V, Sullivan PW. Physical activity in U.S. adults with diabetes and at risk for developing diabetes, 2003. Diabetes Care. 2007;30(2):203–209. doi: 10.2337/dc06-1128. [DOI] [PubMed] [Google Scholar]
- Muller AM, Khoo S. Non-face-to-face physical activity interventions in older adults: a systematic review. Int J Behav Nutr Phys Act. 2014;11(1):35. doi: 10.1186/1479-5868-11-35. Research Support, Non-U.S. Gov't. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perera S, Studenski S, Newman A, Simonsick E, Harris T, Schwartz A, et al. for the Health, A. B. C. S. Are Estimates of Meaningful Decline in Mobility Performance Consistent Among Clinically Important Subgroups? (Health ABC Study) J Gerontol A Biol Sci Med Sci. 2014 doi: 10.1093/gerona/glu033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proper KI, Singh AS, van Mechelen W, Chinapaw MJ. Sedentary behaviors and health outcomes among adults: a systematic review of prospective studies. Am J Prev Med. 2011;40(2):174–182. doi: 10.1016/j.amepre.2010.10.015. doi:S0749-3797(10)00608-2[pii]10.1016/j.amepre.2010.10.015. [DOI] [PubMed] [Google Scholar]
- Pruitt LA, Glynn NW, King AC, Guralnik JM, Aiken EK, Miller G, Haskell WL. Use of accelerometry to measure physical activity in older adults at risk for mobility disability. J Aging Phys Act. 2008;16(4):416–434. doi: 10.1123/japa.16.4.416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg DE, Bull FC, Marshall AL, Sallis JF, Bauman AE. Assessment of sedentary behavior with the International Physical Activity Questionnaire. J Phys Act Health. 2008;5(Suppl 1):S30–S44. doi: 10.1123/jpah.5.s1.s30. [DOI] [PubMed] [Google Scholar]
- Rosenberg DE, Norman GJ, Wagner N, Patrick K, Calfas KJ, Sallis JF. Reliability and validity of the Sedentary Behavior Questionnaire (SBQ) for adults. J Phys Act Health. 2010;7(6):697–705. doi: 10.1123/jpah.7.6.697. [DOI] [PubMed] [Google Scholar]
- Santos-Lozano A, Marin PJ, Torres-Lugue G, Ruiz JR, Lucia A, Garatachea N. Technical variability of the GT3X accelerometer. Med Eng Phys. 2012;34(6):787–790. doi: 10.1016/j.medengphy.2012.02.005. [DOI] [PubMed] [Google Scholar]
- Schutzer KA, Graves BS. Barriers and motivations to exercise in older adults. Prev Med. 2004;39(5):1056–1061. doi: 10.1016/j.ypmed.2004.04.003. doi:S0091743504002026[pii]10.1016/j.ypmed.2004.04.003. [DOI] [PubMed] [Google Scholar]
- Sedentary Behaviour Research Network. Letter to the editor: standardized use of the terms “sedentary” and “sedentary behaviours”. Appl Physiol Nutr Metab. 2012;37(3):540–542. doi: 10.1139/h2012-024. [DOI] [PubMed] [Google Scholar]
- Seguin R, Lamonte M, Tinker L, Liu J, Woods N, Michael YL, et al. Lacroix AZ. Sedentary Behavior and Physical Function Decline in Older Women: Findings from the Women's Health Initiative. J Aging Res. 2012;2012:271589. doi: 10.1155/2012/271589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilmot EG, Edwardson CL, Achana FA, Davies MJ, Gorely T, Gray LJ, et al. Biddle SJ. Sedentary time in adults and the association with diabetes, cardiovascular disease and death: systematic review and meta-analysis. Diabetologia. 2012;55(11):2895–2905. doi: 10.1007/s00125-012-2677-z. Meta-Analysis Research Support, Non-U.S. Gov't Review. [DOI] [PubMed] [Google Scholar]