Abstract
Patient: Male, 31
Final Diagnosis: Acute cholecystitis complicated with portal vein thrombosis
Symptoms: Abdominal discomfort • fever • vomiting
Medication: —
Clinical Procedure: Abdominal ultrasound and MRI
Specialty: Gastroenterology and Hepatology
Objective:
Rare co-existance of disease or pathology
Background:
Portal vein thrombosis (PVT) is an infrequent clinical condition usually associated with multiple etiological factors and diseases. In some cases, PVT remains undiagnosed and is incidentally detected during routine examination for a known etiology.
Case Report:
Here, we present a rare case of portal vein thrombosis associated with acute cholecystitis in a 31-year-old man.
Conclusions:
Conservative treatment may be a feasible and safe approach for the management of PVT with acute cholecystitis, if treated at an early stage. Moreover, initial diagnosis based on radiological evaluation is possible only if the surgeons are familiar with this unusual condition. Therefore, a high index of suspicion is required for early diagnosis and management of patients with acute cholecystitis-associated PVT.
MeSH Keywords: Cholecystitis, Acute; Diagnosis; Portal Vein
Background
Acute portal vein thrombosis (PVT) is an unusual clinical condition resulting from a combination of acquired, inherited, and local precipitating factors [1]. Although the diagnosis of inherited coagulation disorder does not influence the management of VTE, there is increased risk of recurrence in such patients with homozygotes gain-of-function mutations [2]. The most frequent local thrombotic risk factors are cholecystitis, cholangitis, appendicitis, splenectomy, pancreatitis, and liver cirrhosis or tumors [3]. The signs and symptoms of PVT are often non-specific, and these patients mainly present with acute febrile illness and abdominal pain [4]. Unfortunately, abdominal pain is not considered as the primary indication of PVT; therefore, it might be neglected in some cases [5]. The use of Doppler ultrasonography and CT scan has improved the rate of radiological diagnosis of PVT [6], but PVT remains undiagnosed in some cases and is incidentally detected during routine examination for other reasons [7]. In such cases, the specific underlying pathological condition related with PVT manifested the initial clinical presentation, time course, and prognosis [8]. Particularly, the presentation of PVT with acute cholecystitis is an unusual event and only a few cases have been reported in the literature. Here, we present a rare case of portal vein thrombosis associated with acute cholecystitis.
Case Report
A 31-year-old man presented with right upper-quadrant abdominal pain, fever, and vomiting for 7 days but had no history of jaundice. The laboratory findings revealed impaired liver function profile with high alanine aminotransferase (65 U/l), aspartate aminotransferase (65 U/l), total bilirubin (90 umol/l) and alkaline phosphatase (312 U/l). Anti-thrombin III was slightly raised at 122% (reference range: 80–120%). The coagulation profile was unremarkable, with no deficiency of protein C and S, negative finding for factor V Leiden, and complement component 3 (C3 and 4) was 156 and 51 mg/dl, respectively. Anti-smooth muscle antibody, anti-mitochondrial antibody, anti-nuclear antibody, anti-LKM antibody, and viral hepatitis screens were negative. The blood culture report was also negative. Our case had no history of splenectomy. Abdominal ultrasonography showed features of acute cholecystitis and right portal vein thrombosis. Moreover, the magnetic resonance imaging (MRI) study confirmed the diagnosis of PVT (Figures 1, 2). The patient was managed conservatively with intravenous antibiotics and anticoagulation. Within few days, the patient started recovering with normalization of the liver function profile and subsequently, he was discharged home on the 8th day post hospitalization.
Figure 1.
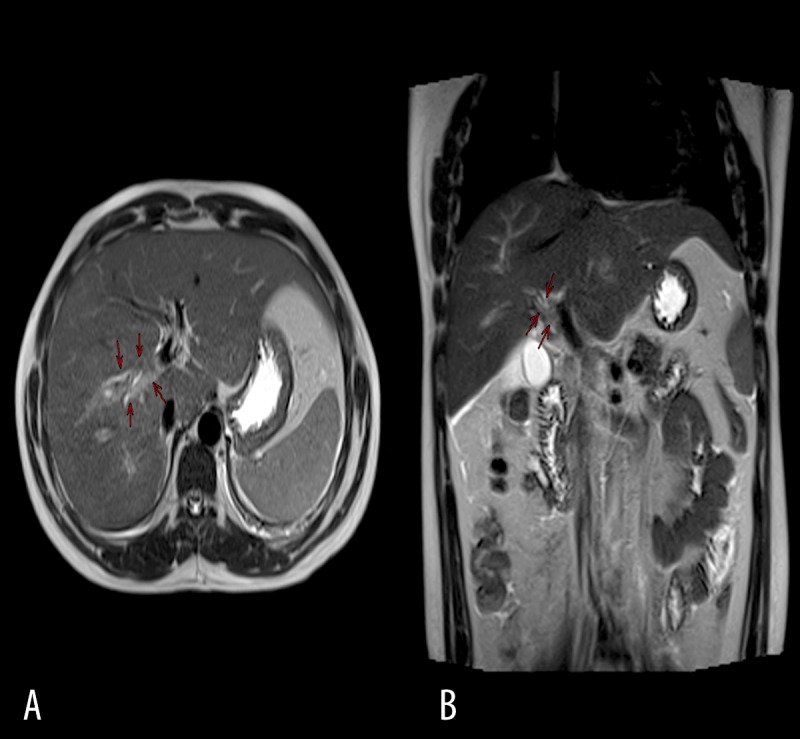
Axial T2 (A) and coronal T2 (B) images of the upper abdomen showing a thrombus involving the right portal vein (red arrows).
Figure 2.
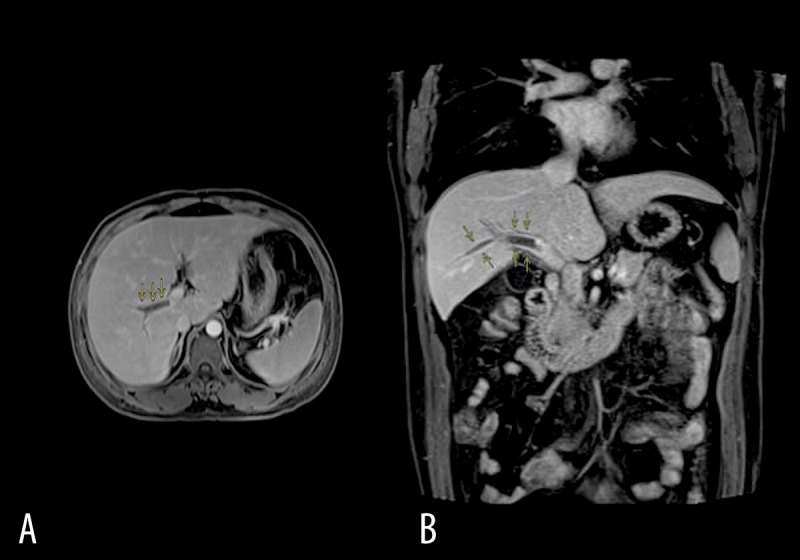
Axial (A) and coronal (B) post-contrast T1 fat saturation images showing a filling defect involving the right portal vein and extending to its segmental branches with associated minor perfusion geographical changes.
Discussion
The present case report describes a rare case of portal vein thrombosis (PVT) secondary to acute cholecystitis. The association of acute cholecystitis with PVT is considered relatively rare and is usually presented as case series and reports [9]. The pathogenesis of PVT is multifactorial and is primarily associated with liver or pancreatic malignancies, with an overall frequency of 21–24% [10]. In contrast, local thrombotic risk factors such as cholecystitis, cholangitis, appendicitis, splenectomy, and pancreatitis are commonly observed [11–13]. However, we did not observe any association of local risk factors in our case with no history of splenectomy or other complications. The most frequent symptoms include abdominal pain, nausea, vomiting, diarrhea, or constipation [12]. The clinical signs are usually non-specific and patients often present with abdominal tenderness and distension, diminished bowel sounds, fever, and shock.
Moreover, patients with PVT have differential presentation depending upon the site of the thrombosis (portal vein or portal vein territory), acute or chronic, and collateral veins development. These collateral veins develop in few days after portal vein obstruction, and get completed within 3 to 5 weeks [14,15]. Several causes of PVT have been reported in the literature, however, PVT post acute cholecystits is rare event and only few cases have been reported so far (Table 1) [3,8,16–20]. This could be attributed to the subclinical course of the disease, which is only detected incidentally during radiological examination. Orgen et al. [11] reported the rate of incidental detection of PVT is around 1% of the general population based on 23 796 consecutive autopsies from Sweden. Choi et al. [20] reported 6 cases of PVT associated with acute cholecystitis in a retrospective radiological evaluation of patients with transiently increased hepatic attenuation on CT scan. These authors observed no etiological factors associated with PVT and speculated that the occurrence of PVT post-acute cholecystitis could be due to inflammation or an infectious process that involves the cystic vein. Similarly, we did not observe any coexistent clinical conditions responsible for PVT and there was no abscess collection to indicate any involvement of inflammation or infectious process in our case.
Table 1.
Summary of the literature review.
| Authors | Year | Cases | Clinical presentation | Management |
|---|---|---|---|---|
| Harch et al. [16] | 1987 | 1 | Abdominal pain | Anticoagulation |
| Kidney et al. [17] | 1998 | 1 | Severe right upper quadrant and epigastric pain | Conservative management |
| Inoguchi et al. [18] | 2004 | 1 | Abdominal pain, nausea | Percutaneous transhepatic gallbladder drainage |
| Choi et al. [20] | 2004 | 6 | – | – |
| El-Wahsh [8] | 2006 | 1 | Abdominal pain, nausea | Conservative management followed by bowel rest and anticoagulation |
| Menéndez-Sánchez et al. [19] | 2010 | 1 | Abdominal pain | Surgery and antibiotic treatment |
| Hsu et al. [3] | 2012 | 1 | Abdominal pain, fever | Anti-coagulation and laparoscopic cholecystectomy |
| Present case | 2014 | 1 | Abdominal pain, fever, vomiting | Conservative management |
The treatment goal in PVT is to prevent extension of the thrombus and to attain portal vein patency. The various treatment approaches for PVT include the management of the underlying disease, use of antibiotics, hydration, anticoagulation therapy, and (infrequently) thrombolytic therapy or surgical embolectomy [21]. However, some studies suggested spontaneous resolution of the PVT [22,23]. The time interval between thrombosis formation and start of the anticoagulation treatment dictates the outcome of recanalization [21]. It has been reported that in case of acute PVT, early anticoagulation treatment results in favorable outcome. For instance, Turnes and colleagues [24] showed that the rate of recanalization was greater in patients who received anticoagulation early in the first week post diagnosis in comparison to the second week anticoagulation therapy (69% vs. 25%).
In our case, the patient was treated conservatively with sub-cutaneous heparin injection. We treated the primary condition “acute cholecystitis” that improved patient condition, in terms of liver derangement normalization. However, the therapeutic management should also aim to resolve extensive portal vein obstruction and to avoid serious complications [10].
Our report is limited in that the patient did not undergo follow-up abdominal CT imaging after conservative management to look for any change in imaging results. We only followed clinical and laboratory findings for resolving the disease manifestations of the patient until complete recovery.
Conclusions
Conservative treatment could be a feasible and safe approach for the management of PVT with acute cholecystitis, if treated at an early stage. The occurrence of PVT secondary to acute cholecystitis could possibly be explained by the pericholecystic inflammation that affects the portal vein, which resulted in PVT. Moreover, initial diagnosis based on Doppler ultrasonography and CT scan is possible only if the surgeons are familiar with this uncommon condition. Therefore, the diagnosis of such patients requires a high index of suspicion and early management of associated etiology to achieve better outcomes.
Acknowledgments
The authors thank all the general surgery staff for their cooperation.
Footnotes
Conflicts of interests
The authors have no conflicts of interests and no financial issues to disclose.
References:
- 1.Sogaard KK, Astrup LB, Vilstrup H, Gronbaek H. Portal vein thrombosis; risk factors, clinical presentation and treatment. BMC Gastroenterol. 2007;7:34. doi: 10.1186/1471-230X-7-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Martinelli I, De Stefano V, Mannucci PM. Inherited risk factors for venous thromboembolism. Nat Rev Cardiol. 2014;11(3):140–56. doi: 10.1038/nrcardio.2013.211. [DOI] [PubMed] [Google Scholar]
- 3.Hsu SC, Hsieh CH, Wu SC, et al. Successful staged treatment for acute cholecystitis complicated by portal vein thrombosis. Am Surg. 2012;78:E19–21. [PubMed] [Google Scholar]
- 4.de Cleva R, Herman P, Saad WA, et al. Postoperative portal vein thrombosis in patients with hepatosplenic mansonic schistosomiasis: relationship with intraoperative portal pressure and flow. A prospective study. Hepatogastroenterology. 2005;52:1529–33. [PubMed] [Google Scholar]
- 5.Famularo G, Minisola G, Nicotra GC, De Simone C. Mesenteric and portal vein thrombosis associated with hyperhomocysteinemia and heterozygosity for factor V Leiden mutation. World J Gastroenterol. 2005;11:7700–1. doi: 10.3748/wjg.v11.i48.7700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Condat B, Pessione F, Hillaire S, et al. Current outcome of portal vein thrombosis in adults: risk and benefit of anticoagulant therapy. Gastroenterology. 2001;120:490–97. doi: 10.1053/gast.2001.21209. [DOI] [PubMed] [Google Scholar]
- 7.Pasiri S, Pirathvisuth T. Review of 336 patients with hepatocellular carcinoma. World J Gastroenterol. 2000;6:339–43. doi: 10.3748/wjg.v6.i3.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.El-Wahsh M. A case of portal vein thrombosis associated with acute cholecystitis/pancreatitis or coincidence. Hepatobiliary Pancreat Dis Int. 2006;5:308–10. [PubMed] [Google Scholar]
- 9.Amitrano L, Guardascione MA, Brancaccio V, et al. Risk factors and clinical presentation of portal vein thrombosis in patients with liver cirrhosis. J Hepatol. 2004;40:736–41. doi: 10.1016/j.jhep.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 10.Ponziani FR, Zocco MA, Campanale C, et al. Portal vein thrombosis: Insight into physiopathology, diagnosis, and treatment. World J Gastroenterol. 2010;16:143–55. doi: 10.3748/wjg.v16.i2.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ogren M, Bergqvist D, Björck M, et al. Portal vein thrombosis: prevalence, patient characteristics and lifetime risk: a population study based on 23,796 consecutive autopsies. World J Gastroenterol. 2006;12:2115–19. doi: 10.3748/wjg.v12.i13.2115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Condat B, Valla D. Nonmalignant portal vein thrombosis in adults. Nat Clin Pract Gastroenterol Hepatol. 2006;3:505–15. doi: 10.1038/ncpgasthep0577. [DOI] [PubMed] [Google Scholar]
- 13.Denninger MH, Chaït Y, Casadevall N, et al. Cause of portal or hepatic venous thrombosis in adults: the role of multiple concurrent factors. Hepatology. 2000;31:587–91. doi: 10.1002/hep.510310307. [DOI] [PubMed] [Google Scholar]
- 14.Ohnishi K, Okuda K, Ohtsuki T, et al. Formation of hilar collaterals or cavernous transformation after portal vein obstruction by hepatocellular carcinoma. Observations in ten patients. Gastroenterology. 1984;87:1150–53. [PubMed] [Google Scholar]
- 15.De Gaetano AM, Lafortune M, Patriquin H, et al. Cavernous transformation of the portal vein: patterns of intrahepatic and splanchnic collateral circulation detected with Doppler sonography. Am J Roentgenol. 1995;165:1151–55. doi: 10.2214/ajr.165.5.7572494. [DOI] [PubMed] [Google Scholar]
- 16.Harch JM, Radin RD, Yellin AE, Donovan AJ. Pylethrombosis. Serendipitous radiologic diagnosis. Arch Surg. 1987;122:1116–19. doi: 10.1001/archsurg.1987.01400220026003. [DOI] [PubMed] [Google Scholar]
- 17.Kidney DD, Forino MT, Cohen AJ, Hunter V. Case report: Portal venous thrombosis in acute cholecystitis. CT, ultrasound, Doppler and power Doppler findings. Clin Radiol. 1998;53:459–61. doi: 10.1016/s0009-9260(98)80279-1. [DOI] [PubMed] [Google Scholar]
- 18.Inoguchi H, Nakata K, Sugimachi K. Portal vein thrombosis complicated with disseminated intravascular coagulation due to acute cholecystitis. Hepatogastroenterology. 2004;51:661–63. [PubMed] [Google Scholar]
- 19.Menéndez-Sánchez P, Gambí-Pisonero D, Villarejo-Campos P, et al. Septic thrombophlebitis of the portal vein due to acute cholecystitis. Cir Cir. 2010;78:439–41. [PubMed] [Google Scholar]
- 20.Choi SH, Lee JM, Lee KH, et al. Relationship between various patterns of transient increased hepatic attenuation on CT and portal vein thrombosis related to acute cholecystitis. Am J Roentgenol. 2004;183:437–42. doi: 10.2214/ajr.183.2.1830437. [DOI] [PubMed] [Google Scholar]
- 21.Thomas RM, Ahmad SA. Management of acute post-operative portal venous thrombosis. J Gastrointest Surg. 2010;14:570–77. doi: 10.1007/s11605-009-0967-7. [DOI] [PubMed] [Google Scholar]
- 22.Condat B, Pessione F, Helene Denninger M, et al. Recent portal or mesenteric venous thrombosis: increased recognition and frequent recanalization on anticoagulant therapy. Hepatology. 2000;32:466–70. doi: 10.1053/jhep.2000.16597. [DOI] [PubMed] [Google Scholar]
- 23.Baril N, Wren S, Radin R, et al. The role of anticoagulation in pylephlebitis. Am J Surg. 1996;172:449–52. doi: 10.1016/S0002-9610(96)00220-6. discussion 452–53. [DOI] [PubMed] [Google Scholar]
- 24.Turnes J, García-Pagán JC, González M, et al. Portal hypertension-related complications after acute portal vein thrombosis: impact of early anticoagulation. Clin Gastroenterol Hepatol. 2008;6:1412–17. doi: 10.1016/j.cgh.2008.07.031. [DOI] [PubMed] [Google Scholar]


